Paper:
Development of Intraoperative Plantar Pressure Measurement System Considering Weight Bearing Axis and Center of Pressure
Izumu Hosoi*1, Takumi Matsumoto*2, Song Ho Chang*3, Qi An*4, Ichiro Sakuma*1, and Etsuko Kobayashi*1
*1Schoool of Engineering, The University of Tokyo
7-3-1 Hongo, Bunkyo-ku, Tokyo 113-8656, Japan
*2School of Medicine, The University of Tokyo
7-3-1 Hongo, Bunkyo-ku, Tokyo 113-8656, Japan
*3Department of Orthopedic Surgery, JCHO Tokyo Shinjuku Medical Center
5-1 Tsukudo-cho, Shinjuku-ku, Tokyo 162-8543, Japan
*4School of Frontier Sciences, The University of Tokyo
5-1-5 Kashiwanoha, Kashiwa-shi, Chiba 277-0882, Tokyo
To prevent postoperative complications in corrective surgery for foot deformities such as hallux valgus and pes planus, it is critical to quantitatively predict the postoperative standing-position plantar pressure distribution during the operation. The authors have previously proposed an intraoperative plantar pressure measurement system (IPPM) that allows for the measurement of a supine patient’s plantar pressure distribution that is equivalent to that in the standing position. This system consists of an IPPM device comprising of a force plate and pressure distribution sensor, an optical three-dimensional position measurement device, a navigation monitor, and a PC. The plantar pressure distribution in the standing position is reproduced by navigating the operator, as he or she presses the IPPM device against the patient’s sole so that the weight-bearing axis (floor reaction force vector) and femoral head center are as close to each other as possible. However, in our previous study, the reproducibility of the standing position plantar pressure distribution was insufficient. Therefore, in the present study, we add a navigational function that can be used to bring the centers of pressure in the standing position and under measurement, as well as to correct the IPPM’s self-weight in the measured force. The improved device was used in an experiment with nine healthy subjects, and the similarity of the plantar pressure distribution in the standing and supine positions was evaluated using normalized cross-correlation, yielding an average of 0.90. Furthermore, in an evaluation experiment with ten orthopedic surgeons, it was observed that using the system reproduced the plantar pressure distribution significantly better than when the system was not used. These results indicate that the present system can predict the plantar pressure distribution in the standing position. We believe that this system can contribute to reducing complications after foot surgery.
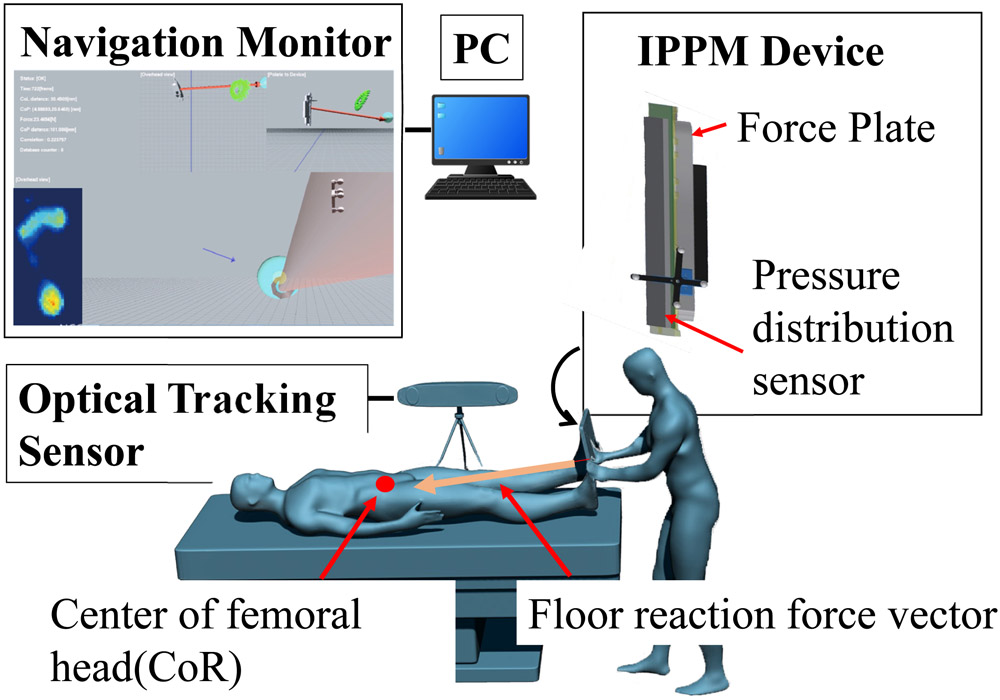
Overview of intraoperative planter pressure measurement (IPPM) system
- [1] G. Bonney and I. Macnab, “Hallux Valgus and Hallux Rigidus,” The J. of Bone and Joint Surgery, Vol.34-B, No.3, pp. 366-385, doi: 10.1302/0301-620X.34B3.366, 1952.
- [2] E. Roddy, W. Zhang, and M. Doherty, “Prevalence and associations of hallux valgus in a primary care population,” Arthritis Care and Research, Vol.59, No.6, pp. 857-862, doi: 10.1002/art.23709, 2008.
- [3] T. Matsumoto, J. Higuchi, Y. Maenohara, S. H. Chang, T. Iidaka, C. Horii et al., “The discrepancy between radiographically-assessed and self-recognized hallux valgus in a large population-based cohort,” BMC Musculoskelet. Disord., Vol.23, No.1, Article No.31, doi: 10.1186/s12891-021-04978-z, 2022.
- [4] K. J. Mickle, B. J. Munro, S. R. Lord, H. B. Menz, and J. R, Steele, “Gait, balance and plantar pressures in older people with toe deformities,” Gait and Posture, Vol.34, No.3, pp. 347-351, doi: 10.1016/j.gaitpost.2011.05.023, 2011.
- [5] H. B. Menz and S. R. Lord, “Foot pain impairs balance and functional ability in community-dwelling older people,” J. Am. Podiatr. Med. Assoc., Vol.91, No.5, pp. 222-229, doi: 10.7547/87507315-91-5-222, 2001.
- [6] H. B. Menz and S. R. Lord, “Gait instability in older people with hallux valgus,” Foot Ankle Int., Vol.26, No.6, pp. 483-489, doi: 10.1177/107110070502600610, 2005.
- [7] R. A. Mann and M. J. Coughlin, “Hallux valgus – etiology, anatomy, treatment and surgical considerations,” Clin. Orthop. Relat. Res., Vol.157, pp. 31-41, 1981.
- [8] K. Tóth, I. Huszanyik, P. Kellermann, K. Boda, and L. Róde, “The effect of first ray shortening in the development of metatarsalgia in the second through fourth rays after metatarsal osteotomy,” Foot. Ankle. Int., Vol.28, No.1, pp. 61-63, doi: 10.3113/FAI.2007.0011, 2007.
- [9] G. Zheng and L. P. Nolte, “Computer-Assisted Orthopedic Surgery: Current State and Future Perspective,” Front. Surg., Vol.2, Article No.66, 10.3389/fsurg.2015.00066, 2015.
- [10] F. A. Casari, N. Navab, L. A. Hruby, P. Kriechling, R. Nakamura, R. Tori, F. L. S. Nunes, M. C. Queiroz, P. Fúrnstahl, and M. Farshad, “Augmented Reality in Orthopedic Surgery Is Emerging from Proof of Concept Towards Clinical Studies: a Literature Review Explaining the Technology and Current State of the Art,” Current Reviews in Musculoskeletal Medicine, Vol.14, pp. 192-203, doi: 10.1007/s12178-021-09699-3, 2021.
- [11] N. Sugano, “Computer-assisted orthopedic surgery,” J. of Orthopaedic Science, Vol.8, pp. 442-448, 2003.
- [12] R. H. Taylor et al., “An image-directed robotic system for precise orthopaedic surgery,” IEEE Trans. on Robotics and Automation, Vol.10, No.3, pp. 261-275, doi: 10.1109/70.294202, 1994.
- [13] S. D. Werner, M. Stonestreet, and D. J. Jacofsky, “Makoplasty and the accuracy and efficacy of robotic-assisted arthroplasty,” Surgical Technology Int., Vol.24, pp. 302-306, 2014.
- [14] T. Nakano, N. Sugita, T. Kato, K. Fujiwara, N. Abe, T. Ozaki, M. Suzuki, and M. Mitsuishi, “Interference Free Tool Path Generation in Multi-Axis Milling Machine for Orthopedic Surgery,” Int. J. Automation Technol., Vol.3, No.5, pp. 514-521, 2009.
- [15] M. Richter, M. Frink, S. Zech, N. Vanin, J. Geerling, P. Droste, and C. Krettek, “Intraoperative pedography: A validated method for static intraoperative biomechanical assessment,” Foot and Ankle Int., Vol.27, No.10, pp. 833-842, doi: 10.1177/107110070602701014, 2006.
- [16] S. J. Ellis, H. Hillstrom, R. Cheng, J. Lipman, G. Garrison, and J. T. Deland, “The development of an intraoperative plantar pressure assessment device,” Foot and Ankle Int., Vol.30, No.4, pp. 333-340, doi: 10.3113/FAI.2009.0333, 2009.
- [17] Y. S. Lee, B. K. Lee, S. H. Lee, H. G. Park, D. S. Jun, and D. H. Moon, “Effect of foot rotation on the mechanical axis and correlation between knee and whole leg radiographs,” Knee Surgery, Sports Traumatology, Arthroscopy, Vol.21, No.11, pp. 2542-2547, doi: 10.1007/s00167-013-2419-x, 2013.
- [18] I. Hosoi, E. Kobayashia, S. Chang, T. Matsumoto, Q. An, E. Anzai, Y. Ohta, and I. Sakuma, “Development of Intraoperative Plantar Pressure Measuring System considering weight bearing axis,” Int. J. of Computer Assisted Radiology and Surgery, Vol.14, pp. 385-395, doi: 10.1007/s11548-018-1862-z, 2018.
- [19] S. Holzreiter, “Calculation of the instantaneous centre of rotation for a rigid body,” J. of Biomechanics, Vol.24, No.7, pp. 643-647, doi: 10.1016/0021-9290(91)90297-z, 1991.
- [20] S. Kajita, “Humanoid Robot,” Ohmusha, 2005.
- [21] Welfare Statistics Handbook, “Ministry of Health,” Labour and Welfare, 2021.
- [22] Research and development of infrastructure equipment planning for the elderly, “Part 2 Database Equipment – dynamics/audiovisual characteristics –,” Research Inssitute of Human Engineering for Quality Life, 2000.
 This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.
This article is published under a Creative Commons Attribution-NoDerivatives 4.0 Internationa License.