Abstract
Free full text

Appearance of immature/transitional B cells in HIV-infected individuals with advanced disease: Correlation with increased IL-7
Abstract
Progression of HIV disease is associated with the appearance of numerous B cell defects. We describe herein a population of immature/transitional B cells that is overly represented in the peripheral blood of individuals with advancing HIV disease. These B cells, identified by the expression of CD10, were unresponsive by proliferation to B cell receptor triggering and possessed a phenotype and an Ig diversity profile that confirmed their immature/transitional stage of differentiation. Consistent with an immature status, their lack of proliferation to B cell receptor triggering was reversed with CD40 ligand, but not B cell activation factor. Finally, levels of CD10 expression on B cells were directly correlated with serum levels of IL-7, suggesting that increased levels of IL-7 modulate human B cell maturation either directly or indirectly by means of a homeostatic effect on lymphopenia. Taken together, these data offer insight into human B cell development as well as B cell dysfunction in advanced HIV disease that may be linked to IL-7-dependent homeostatic events.
HIV infection is associated with numerous immunologic aberrancies that result from direct and indirect effects of ongoing viral replication and eventually lead to a state of profound immunodeficiency (1, 2). Although CD4+ T cells are the major targets of the insult exacted by HIV, a broad array of abnormalities are observed in most immune competent cells and lymphoid compartments of infected individuals. We and others have described a wide range of B cell dysfunctions in the setting of HIV infection, several of which have been associated with cellular hyperactivation induced by ongoing viral replication, including hypergammaglobulinemia (3), increased expression of cellular markers of B cell activation (4, 5), appearance of B cell subpopulations associated with cellular activation and terminal differentiation (6, 7), increased B cell turnover (8), and increased incidence of B cell malignancies (9). In addition, certain B cell deficiencies occur whether or not patients control HIV viremia; these changes include loss of memory B cells as measured by the expression of CD27 (10) and reduced expression of surface markers, such as CD25, that are induced by mitogenic stimulation (5).
We recently reported a reduction in influenza-specific memory B cell function that was most pronounced in HIV-infected individuals who were profoundly lymphopenic and had maintained a high viral burden (11). Lymphopenia in HIV disease is thought to induce compensatory homeostatic mechanisms, including increased levels of IL-7 (12, 13), a cytokine that plays a critical role in both the maturation and maintenance of T cells (14). With regard to B cells, IL-7 is essential for maturation in mice but not in humans (15, 16). However, whereas the effect of IL-7 on human B cell survival and proliferation has not been fully delineated, human pre-B cells express IL-7 receptors and, in the presence of stromal cells, respond to IL-7 (17). Furthermore, IL-7 transgenic mice have increased numbers of immature B cells (18), and similar increases in immature B cells have been observed in humans undergoing IL-7 therapy (C. L. Mackall, personal communication).
In previous studies, we and others have described numerous B cell deficiencies that reflected aberrant activation associated with HIV viremia (3–7, 19). However, in a recent study involving a large cohort of HIV-infected individuals (11), we began accumulating preliminary data suggesting that other types of deficiencies occur in B cells, especially in individuals with advanced disease (4). Since the advent of effective antiretroviral therapy, these deficiencies have been more difficult to document, given the dramatic reductions in the numbers of profoundly lymphopenic individuals. In the present study, we describe a subpopulation of CD10+ B cells that is markedly increased in HIV-infected individuals, especially those who are profoundly lymphopenic and maintain a high viral burden. The frequency of these B cells is directly correlated with serum levels of IL-7, which in turn are directly and inversely correlated with levels of plasma viremia and CD4+ T cell count, respectively.
We also investigated the nature of the CD10+ B cells expanded in HIV-infected individuals with active disease. Although it was previously suggested that the expression of CD10 on human B cells was associated with germinal center founder B cells (20), recent findings suggest that CD10 also defines immature/transitional B cells (21). Our data suggest that both types of CD10+ B cells are present in peripheral blood, but that only the immature/transitional B cells are expanded in advancing HIV disease, consistent with the increased levels of IL-7 also observed in these individuals. We thus provide evidence for the existence of immature/transitional B cells in the human periphery that are expanded with advancing HIV disease.
Results
CD10 Defines a Population of Immature/Transitional B Cells Expanded in HIV Disease.
In a previous study (11), we reported a decrease in memory B cell function in HIV-infected individuals that was associated with active disease, as defined by CD4+ T cell counts <350 cells per μl and plasma viremia >10,000 copies of HIV RNA per ml (group 1 in Fig. 1). In humans, the memory B cell compartment is generally defined by the expression of CD27. However, we found that the decreases in memory B cell function were not correlated with decreases in CD27 expression (unpublished data); this observation was likely a reflection of the increased expression of CD27 on CD21lo B cells that arises as a result of HIV-induced hyperactivation (Fig. 1A and ref. 19). Although activated CD27+/CD21lo B cells are largely absent in HIV-infected individuals with controlled disease (CD4+ T cell count >500 cells per μl and undetectable HIV plasma viremia; group 2 in Fig. 1) and in HIV-negative individuals, they can represent 50% of B cells in HIV-infected individuals with active disease (Fig. 1A). Thus, CD27 may not represent an appropriate marker for the B cell memory phenotype in diseases such as HIV where high levels of immune activation occur and may confound the use of standard phenotypic markers of B cell memory. In searching for a phenotypic correlation for decreased memory B cell function, we observed that B cells of HIV-infected individuals with active disease expressed significantly higher levels of CD10 when compared with B cells of HIV-infected individuals with controlled disease and HIV-negative individuals (Fig. 1B). The median expression of CD10 on B cells in group 1 was 29%, compared with 10% in group 2 and 11% in HIV-negative individuals. Furthermore, and consistent with our findings regarding memory B cell function (11), the percentage of CD10 expression on B cells in HIV-infected individuals was inversely correlated with CD4+ T cell count (r = −0.619, P < 0.0001), and directly correlated with levels of HIV RNA in plasma (r = 0.629, P < 0.0001). Of note, the peripheral B cell compartment of one individual whose CD4+ T cells were almost completely depleted and who was expectedly unable to mount a memory B cell response (11) comprised 58% CD10+ B cells. Taken together, these data suggest that the expansion of CD10+ B cells in HIV-infected individuals is associated with disease progression.
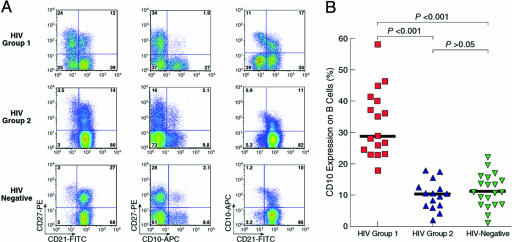
Analysis of CD10 expression on B cells from HIV-infected and HIV-negative individuals. (A) Profiles of expression for CD21, CD27, and CD10 are shown for one representative of each group: HIV-infected individuals with active disease (HIV group 1; CD4+ T cell counts <350 cells per μl and plasma viremia >10,000 copies of HIV RNA per ml); HIV-infected individuals with controlled disease (HIV-group 2; CD4+ T cell counts >500 cells per μl and undetectable HIV plasma viremia); and HIV-negative individuals. (B) Comparative analysis of levels of CD10 expression on B cells for the three groups of individuals defined in A.
In humans, CD10 is expressed at high levels on B cell progenitors in the bone marrow and then progressively disappears with maturation, except on activated germinal center founder B cells, where it is coexpressed with CD27 (20). These activated mature CD10+ B cells are also detected in the peripheral blood (20), although a recent study suggests that the majority of CD10+ B cells in the peripheral blood represent immature/transitional B cells (21). To determine whether the increased expression of CD10 on B cells of HIV-infected individuals with active disease corresponded to either of these populations, we performed phenotypic analyses on the various B cell populations depicted in Fig. 1. In agreement with the profile of immature/transitional B cells recently described in humans (21), expression of CD10 on B cells of HIV-infected individuals with active disease was largely restricted to CD27− B cells, and levels of CD10 were higher (CD10hi) on a portion of CD21lo compared with CD21hi B cells (Fig. 1A). Also consistent with an immature/transitional B cell phenotype (21, 22), the least mature CD10hi/CD21lo B cells expressed the highest levels of IgM, CD38, and CD24 and lowest levels of IgD, CD44, CD22, CD95, and B cell activation factor (BAFF) receptor whereas the more intermediate (CD10int) CD21hi B cells displayed a pattern of expression for these markers that was closer to that of mature CD10−/CD21hi B cells (Fig. 2). Furthermore, the majority of CD10+ B cells of HIV-infected individuals did not express markers of B cell activation (data not shown), which is also consistent with an immature/transitional phenotype (21, 22). However, a small percentage of B cells coexpressing CD10 and CD27 that did not vary with HIV disease status could also be distinguished (Fig. 1A) and likely represented the more mature activated germinal center founder B cells that have also been associated with CD10 expression (20).

Patterns of expression of cell surface markers on B cells of HIV-infected individuals with active disease depicting their immature/translational phenotype. Profiles are shown for one representative individual in group 1 of Fig. 1. Histograms are color coded to reflect expression of each marker within the three gates shown in the Top Left plot: CD10hi/CD21lo least mature B cells (blue), CD10int/CD21hi intermediate B cells (green), and CD10−/CD21hi mature B cells (red).
Thus, CD10 expression defines two populations of B cells, a minor mature population that coexpresses CD27 and an immature CD27− population, within which lies a spectrum of transitional states from the more immature CD10hi/CD21lo to the least immature CD10int/CD21hi B cells that can be clearly identified in the HIV-infected individuals with active disease (Fig. 1A).
The maturation status of the CD10+ B cells described in Fig. 1 was further investigated by Ig diversity analysis by using a technique that measures diversification-induced loss of AluI restriction sites in the CDR regions of the VH3 family (23). VH3 diversity indices were determined on unfractionated B cells, as well as on B cells sorted into CD10+ and CD10− fractions. As shown in Fig. 3A for a representative HIV-infected individual with active disease, the CD10+ fraction, with an index of 0.05, was most closely related to germ-line VH3 sequences; in contrast, the CD10− fraction was most diversified, whereas the unfractionated B cells contained the predicted intermediate level of Ig diversification. Similar results were obtained with CD10+ and CD10− fractions derived from HIV-negative individuals, although in contrast to HIV-infected individuals with active disease, the differences between the two fractions were not as pronounced (Fig. 3B), and likely reflected a greater representation of mature germinal center founder B cells within the CD10+ B cell population of healthy individuals (Fig. 1A).

Ig diversity analysis confirms the immaturity of CD10+ B cells. Shown is AluI restriction analysis of RT-PCR products on unfractionated and sorted CD10− and CD10+ B cell fractions isolated from a representative HIV-infected individual with active disease (A) and an HIV-negative individual (B). The Ig VH3 diversity index is defined as the ratio of intensities of uncut PCR product (331 bp) in the presence (+) to uncut PCR product in the absence (−) of AluI. Bands of 45 and 57 bp represent AluI sites in CDR1, and the band of 71 bp represents an AluI site present in the framework region of certain members of the VH3 family.
CD40L but Not BAFF Can Rescue the Poor Proliferative Responses of CD10+ B Cells to B Cell Receptor (BCR) Stimulation.
Responsiveness to BCR triggering by means of anti-IgM and costimulation effects of CD40 ligand (CD40L) and BAFF have been shown to discriminate between immature and mature B cells in mice (22, 24). We thus used responsiveness to anti-IgM as a means of further evaluating the maturational stage of the CD10+ B cells. As shown in Fig. 4A, the proliferation of CD10+ B cells in response to anti-IgM was very weak, marginally enhanced by BAFF, yet robustly enhanced by CD40L. In contrast to CD10+ B cells, the proliferation of CD10− B cells in response to anti-IgM was moderate, clearly enhanced by BAFF and enhanced even more so by CD40L. The differences in proliferation between CD10+ and CD10− B cells were even more pronounced when the CD10−/CD21lo activated B cells (see Fig. 1A), which express reduced levels of surface IgM and display a reduced proliferative potential (data not shown and ref. 7), were fractionated from the CD10− B cells. As predicted, the CD10−/CD21lo B cells proliferated weakly in response to all three B cell stimuli whereas the CD10−/CD21hi B cells displayed the highest proliferation (Fig. 4A).

Proliferative responses of CD10+ B cells are consistent with an immature status. Unfractionated and CD10/CD21-fractionated B cells were incubated for 72 h at 37°C in the absence or presence of various stimuli followed by measurement of proliferation. (A) Proliferation of unfractionated and CD10/CD21-fractionated B cells for one representative HIV-infected individual with active disease. (B) Combined analyses of proliferation for six HIV-infected individuals with active disease, depicted by fold enhancement of proliferation of the CD10−/CD21hi over CD10+ B cell fractions.
To more fully characterize the proliferative properties of CD10+ B cells, data on several donors were collected and analyzed by fold enhancement of proliferation in response to anti-IgM, anti-IgM plus BAFF, or anti-IgM plus CD40L relative to the CD10−/CD21hi B cell fraction (Fig. 4B). For each of the three treatments, the fold enhancement of proliferation of CD10−/CD21hi over CD10+ B cells was significant (P < 0.05), indicating that the immature/transitional CD10+ B cells were significantly less responsive to stimulation than the mature CD10−/CD21hi B cells. Furthermore, comparisons across treatments revealed that the fold enhancement of proliferation to anti-IgM + BAFF did not significantly differ from that to anti-IgM alone, whereas the fold enhancement of proliferation to anti-IgM plus CD40L was significantly lower than that to the other two stimuli (Fig. 4B). These data indicate that, when compared with the robust proliferative responses of mature CD10−/CD21hi B cells, the weak proliferative response of immature/transitional CD10+ B cells to anti-IgM could be overcome by CD40L but not by BAFF.
CD10 Expression on B Cells of HIV-Infected Individuals Correlates with Serum Levels of IL-7.
Given the strong evidence that the majority of CD10+ B cells in the peripheral blood represented immature/transitional B cells, we considered possible explanations for the expansion of these cells in HIV-infected individuals with active disease. In light of the observation that levels of CD10 on B cells were directly correlated with HIV plasma viremia and inversely correlated with CD4+ T cell count, and that similar correlation patterns have been described with levels of IL-7 (12, 13), we postulated that the expansion of CD10+ immature B cells in HIV-viremic and lymphopenic individuals may be associated with increased levels of IL-7. Accordingly, we analyzed these parameters in a group of patients representing a wide spectrum of HIV disease status. Consistent with our hypothesis and the published data, serum levels of IL-7 were directly correlated with the percentage of B cells expressing CD10 and with HIV plasma viremia, and inversely correlated with CD4+ T cell count (Fig. 5). Individuals with very advanced HIV disease, as defined by low CD4+ T cell count and high HIV plasma viremia, had the highest serum levels of IL-7 and the highest percentage of CD10+ B cells. The increased levels of IL-7 were unlikely to be causing a direct effect on CD10+ B cells in the periphery because we found minimal expression of the IL-7 receptor CD127 on B cells, and no clear segregation of IL-7 receptor by CD10 expression (data not shown). Nonetheless, these correlations with levels of IL-7 provide a plausible, although indirect, mechanistic explanation for why HIV-infected individuals with advanced disease would expand their immature/transitional B cells in vivo.
Discussion
In the present study, we identify a population of immature/transitional B cells, defined by the expression of CD10, that is expanded in the peripheral blood of HIV-infected individuals with active disease. In individuals with markedly advanced disease (CD4+ T cell counts <50 cells per μl), immature/transitional B cells can account for >60% of total B cells. Phenotypic analyses clearly revealed the transitional nature of these immature B cells, with the most immature CD10hi/CD21lo population resembling transitional 1 (T1) B cells and the least immature CD10int/CD21hi population being more akin to transitional 2 (T2) B cells described in mice (22, 25). When characterized functionally, these cells were indeed found to be unresponsive to BCR-mediated proliferation as compared with their more mature CD10− counterparts. That CD10+ B cells were unresponsive to BCR triggering by means of IgM, despite expressing the highest levels of surface IgM, is consistent with the functional immaturity of transitional B cells described in humans and mice (21, 26, 27). Although CD40L enhanced proliferation of CD10+ B cells, BAFF had little effect, a finding that is also consistent with the functional properties of immature/transitional B cells described in mice (22, 27). Whereas the lower levels of BAFF receptor on CD10+ B cells may explain their unresponsiveness to BAFF, it is unlikely to be the sole factor, considering the total lack of responsiveness of these cells to both anti-IgM and BAFF, despite appreciable expression of each respective receptor. Nonetheless, our findings suggest that an increasing percentage of B cells in the peripheral blood of HIV-infected individuals with advancing disease are unresponsive to several B cell stimuli.
The CD10+ B cells identified in HIV-infected individuals with active disease were also present in the peripheral blood of HIV-negative and HIV-infected individuals with controlled disease, although at significantly lower levels. The phenotypic and functional characterization, as well as Ig diversification of CD10+ B cells of healthy individuals, would suggest that a high proportion of these cells are also immature/transitional B cells, as proposed in recent studies (21, 28). However, ≈20% of CD10+ B cells of HIV-negative individuals and HIV-infected individuals with controlled disease coexpressed CD27, compared with 6–8% coexpression of CD27 in HIV-infected individuals with active disease (Fig. 1A). The expression of CD27 on CD10+ B cells is more consistent with mature activated germinal center founder B cells (20) and would explain at least in part why the differences between CD10+ and CD10− B cells of healthy individuals were not as striking as in HIV-infected individuals with active disease.
Comparison of CD10+ B cells and other B cell populations present in the peripheral blood of HIV-infected individuals with active disease also provides insight into the pathogenesis of HIV disease. Numerous B cell abnormalities have been associated with HIV disease, with the vast majority being ascribed to HIV-induced hyperactivation (3–7, 19). In previous studies, aberrantly activated CD21lo B cells were described in HIV-viremic patients and thought to arise as a result of HIV-induced terminal differentiation, as evidenced by decreased proliferative responses to B cell stimuli, increased secretion of immunoglobulins, and the appearance of plasmacytoid features (7). The data presented here extend the previous findings by further defining the activated CD21lo B cells as constituting a very distinct CD10− subset that expresses CD27. In patients with advancing disease, immature/transitional CD10+ B cells, of which a proportion also express low levels of CD21, account for an increasing proportion of the total B cell population. HIV disease progression has also been associated with increased levels of autoantibodies (29, 30), and recent studies indicate that CD10-expressing recently emigrated B cells display increased autoreactivity compared with their more mature counterparts (31). It remains to be determined whether the increases in immature/transitional CD10+ B cells in HIV-infected individuals with advancing disease contribute to increased levels of autoantibodies.
The expansion of CD10+ B cells that are immature, resting, and relatively resistant to activation and proliferation stimuli in HIV-infected individuals who otherwise demonstrate classic signs of HIV-induced immune activation was thus paradoxical. Given that HIV disease progression ultimately leads to severe lymphopenia and mechanisms of homeostatic compensation, as evidenced by increased levels of IL-7 (12, 13), we considered the possibility that the increases in the percentage of B cells expressing CD10 with advancing disease was also associated with increased levels of IL-7 in serum. Although we were not able to distinguish the effects of HIV viremia and CD4+ T cell count on the association between CD10 expression on B cells and serum levels of IL-7, a similar link between IL-7 and lymphopenia in non-HIV diseases has led to the suggestion that, in HIV disease, it is the loss of CD4+ T cells and not HIV viremia that is the major driving force behind elevated levels of IL-7 (12, 32). If such is the case, it remains to be determined whether the expansion of immature B cells is a direct response to the increased levels of IL-7 or an indirect effect that emanates from loss of CD4+ T cells. Nonetheless, these findings offer two very provocative possibilities: either the levels of CD4+ T cells have a direct effect on early B cell maturation, for which there is currently no evidence (33), or IL-7 has a direct and perhaps homeostatic effect on B cells. Although the CD10+ B cells that we identified did not express the IL-7-specific receptor CD127, it is possible that IL-7 causes an expansion of IL-7-responsive B cells in the bone marrow, which then reach a bottleneck in their maturation process in the periphery. In an ongoing clinical trial involving administration of IL-7 to oncology patients, increases in immature B cells in the bone marrow have been observed in several patients who maintained relatively normal total lymphocyte counts (C. L. Mackall, personal communication). It will be fruitful to compare the expanded immature B cells observed in the lymphopenic setting of HIV disease, where levels of IL-7 are chronically elevated, with the expansion of immature B cells observed in the lymphocyte-repleting setting of oncology patients receiving short courses of IL-7.
In conclusion, our findings describing CD10+ B cells in HIV-infected individuals illustrate yet another facet of B cell perturbation and dysfunction associated with HIV disease. In addition, we provide insight into human B cell development by further characterizing immature/transitional CD10+ B cells. Finally, in seeking to explain the expansion of a relatively inert CD10-expressing B cell population in the setting of HIV-mediated immune activation, we provide evidence that immature/transitional B cells may arise from IL-7-mediated homeostatic compensation in lymphopenic individuals.
Materials and Methods
Subjects, Cells, and Clinical Assays.
Peripheral blood mononuclear cells were isolated from density gradient-separated leukapheresis products obtained from HIV-infected individuals. Serum levels of IL-7 were measured by ELISA (R & D Systems), and HIV plasma viremia was measured by standard bDNA assay (Bayer, Elkhart, IN). All subjects provided informed consent, in accordance with the Institutional Review Board of the National Institute of Allergy and Infectious Diseases, National Institutes of Health.
Separation of B Cells.
B cells were isolated from peripheral blood mononuclear cells by magnetic bead-based negative selection (StemCell Technologies, Vancouver). The B cells were then fractionated into CD10− and CD10+ subsets by using biotinylated anti-human CD10 (Serotec), followed by incubation with anti-biotin beads (Miltenyi Biotec, Auburn, CA). CD10− B cells were further fractionated into CD10−/CD21hi and CD10−/CD21lo B cells by using FITC-conjugated anti-human CD21 (Beckman Coulter), followed by incubation with anti-FITC beads (Miltenyi Biotec). Control experiments were performed to confirm that the presence of anti-human CD21 and CD10 mAbs and magnetic beads in the positively enriched fractions did not affect cellular proliferation. The purity of B cells, as determined by flow cytometry, was >95% whereas the purity of subsequent CD10+, CD10−, CD10−/CD21hi, and CD10−/CD21lo B cell fractions ranged from 75–95%.
Immunofluorescence Staining.
Surface stains were performed as described (19), with the use of additional mAbs, including mouse anti-human CD10-allophycocyanin, CD24-PE, CD44-PE, CD127-PE, and CD19-PE-Cy7 (BD Biosciences).
Proliferation Assay.
The proliferation of bulk B cells and various fractions of B cells was measured as described (7). Reagent concentrations were as follows: anti-IgM (10 μg/ml), CD40L (1 μg/ml), and BAFF (1 μg/ml).
Ig Diversity Assay.
B cells were sorted into CD10+ and CD10− fractions by using a FACS (FACSAria, BD Biosciences). The Ig VH3 diversity assay used was based on a modification of a previously described procedure (23). Total cellular RNA was isolated by using the RNeasy procedure (Qiagen, Valencia, CA) and reverse transcribed with a JH consensus reverse primer, 5′-TGAGGATCCGGTGACCAGGGTGCCTTGGCCCCAG. The cDNA was amplified with a VH3 consensus forward primer, 5′-GTCCCTGAGACTCTCCTGTG, labeled at the 5′ end with Cy5 (Operon), and the JH consensus reverse primer using the following conditions: 1 cycle of 2 min at 94°C followed by 35 cycles of 30 s at 94°C, 45 s at 58°C, and 30 s at 72°C. The PCR products were digested with AluI and separated on a 10% polyacrylamide nondenaturing gel, and band intensities were measured by using a PhosphorImager (Molecular Dynamics).
Statistics.
The Spearman rank method was used to test for correlations with adjustment of P values performed with the Bonferroni method. Differences in proliferation were compared by the two-tailed Wilcoxon signed-rank test on log-transformed ratios.
Acknowledgments
We thank Drs. James Arthos, Crystal Mackall, Terry Fry, Claude Kasten-Sportes, Dean Follman, and Misrak Gezmu for helpful discussions. We are indebted to the patients for their willingness to participate in our research efforts. This research was supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases, National Institutes of Health.
References
Articles from Proceedings of the National Academy of Sciences of the United States of America are provided here courtesy of National Academy of Sciences
Full text links
Read article at publisher's site: https://doi.org/10.1073/pnas.0511094103
Read article for free, from open access legal sources, via Unpaywall:
https://europepmc.org/articles/pmc1413756?pdf=render
Citations & impact
Impact metrics
Citations of article over time
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1073/pnas.0511094103
Article citations
Vaccine responses and hybrid immunity in people living with HIV after SARS-CoV-2 breakthrough infections.
NPJ Vaccines, 9(1):185, 09 Oct 2024
Cited by: 0 articles | PMID: 39384763 | PMCID: PMC11464709
B cells and atherosclerosis: A HIV perspective.
J Cell Physiol, 239(6):e31270, 23 Apr 2024
Cited by: 1 article | PMID: 38651687
Review
Humoral and cell-mediated immune responses in HIV-vertically infected young patients after three doses of the BNT162b2 mRNA SARS-CoV-2 vaccine.
Front Immunol, 14:1301766, 04 Jan 2024
Cited by: 0 articles | PMID: 38250079 | PMCID: PMC10797701
IL-7 receptor signaling drives human B-cell progenitor differentiation and expansion.
Blood, 142(13):1113-1130, 01 Sep 2023
Cited by: 7 articles | PMID: 37369082 | PMCID: PMC10644098
Utility of Polymerase Chain Reaction Versus Serology-Based Testing in Immunocompromised Patients With Bartonella henselae Infection.
Open Forum Infect Dis, 10(6):ofad130, 18 Mar 2023
Cited by: 1 article | PMID: 37305840 | PMCID: PMC10249265
Go to all (154) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Impairment of B-lymphocyte differentiation induced by dual triggering of the B-cell antigen receptor and CD40 in advanced HIV-1-disease.
AIDS, 12(12):1437-1449, 01 Aug 1998
Cited by: 36 articles | PMID: 9727564
Relationship between serum IL-7 concentrations and lymphopenia upon different levels of HIV immune control.
AIDS, 21(8):1048-1050, 01 May 2007
Cited by: 9 articles | PMID: 17457102
Idiopathic CD4+ T lymphocytopenia is associated with increases in immature/transitional B cells and serum levels of IL-7.
Blood, 109(5):2086-2088, 19 Oct 2006
Cited by: 75 articles | PMID: 17053062 | PMCID: PMC1801046
Regulation of CD40 ligand expression and use of recombinant CD40 ligand for studying B cell growth and differentiation.
Semin Immunol, 6(5):287-294, 01 Oct 1994
Cited by: 42 articles | PMID: 7865800
Review
Funding
Funders who supported this work.





