Abstract
Background
The recent outbreaks of avian influenza (H5N1) have placed a renewed emphasis on preparing for an influenza pandemic in humans. Of particular concern in this planning is the allocation of resources, such as ventilators and antiviral medications, which will likely become scarce during a pandemic.Methods
We applied a collaborative process using best evidence, expert panels, stakeholder consultations and ethical principles to develop a triage protocol for prioritizing access to critical care resources, including mechanical ventilation, during a pandemic.Results
The triage protocol uses the Sequential Organ Failure Assessment score and has 4 main components: inclusion criteria, exclusion criteria, minimum qualifications for survival and a prioritization tool.Interpretation
This protocol is intended to provide guidance for making triage decisions during the initial days to weeks of an influenza pandemic if the critical care system becomes overwhelmed. Although we designed this protocol for use during an influenza pandemic, the triage protocol would apply to patients both with and without influenza, since all patients must share a single pool of critical care resources.Free full text

Development of a triage protocol for critical care during an influenza pandemic
Associated Data
Abstract
Background
The recent outbreaks of avian influenza (H5N1) have placed a renewed emphasis on preparing for an influenza pandemic in humans. Of particular concern in this planning is the allocation of resources, such as ventilators and antiviral medications, which will likely become scarce during a pandemic.
Methods
We applied a collaborative process using best evidence, expert panels, stakeholder consultations and ethical principles to develop a triage protocol for prioritizing access to critical care resources, including mechanical ventilation, during a pandemic.
Results
The triage protocol uses the Sequential Organ Failure Assessment score and has 4 main components: inclusion criteria, exclusion criteria, minimum qualifications for survival and a prioritization tool.
Interpretation
This protocol is intended to provide guidance for making triage decisions during the initial days to weeks of an influenza pandemic if the critical care system becomes overwhelmed. Although we designed this protocol for use during an influenza pandemic, the triage protocol would apply to patients both with and without influenza, since all patients must share a single pool of critical care resources.
The recent outbreaks of avian influenza (H5N1)1–4 have placed a renewed emphasis on preparing for an influenza pandemic in humans.5,6 Developing plans to deal with the allocation of critical care resources, including mechanical ventilators, which will likely become scarce during a pandemic,6–8 presents a significant challenge. Health care systems in the developed world have rarely encountered the type of resource scarcities envisaged during an influenza pandemic. Models of the potential impact of a pandemic on the Ontario population predict that hospital admissions for influenza will peak at 1823 per day over a 6-week period.9 This translates to 72% of the total hospital capacity being used by influenza patients. Similarly, the demand for intensive care unit (ICU) resources, solely for patients with influenza, would peak at 171% of current ICU bed capacity and 118% of the ventilator capacity. These figures do not take into account the current usage rate of critical care for patients without influenza, which is nearly at 100%. Nor does this model factor in the availability of human resources. Surge response strategies10 (e.g., scaling back elective procedures, opening additional critical care areas and implementing the use of “mass critical care”11,12) will partially mitigate the sudden demand for medical care during an influenza pandemic; however, these strategies will be inadequate to fully address the demands on the health care system.
When resource scarcities occur, the tenets of biomedical ethics and international law dictate that triage protocols be used to guide resource allocation.13–15 International law requires a triage plan that will equitably provide every person the “opportunity” to survive. However, such a law does not guarantee either treatment or survival.16 We have developed this triage protocol in an effort to ensure the equitable and efficient use of critical care resources if scarcities occur during an influenza pandemic.
Methods
In December 2004, at the request of the steering committee of the Ontario Health Plan for an Influenza Pandemic (OHPIP), a group of clinicians with expertise in critical care, infectious diseases, medical ethics, military medicine, triage and disaster management was convened to provide advice regarding critical care during an influenza pandemic. They specifically sought to address issues surrounding critical care resource allocation.
The working group undertook an in-depth review of the medical literature by searching MEDLINE for articles published from January 1966 to December 2004 using the terms “triage,” “intensive care,” “critical care,” “mechanical ventilation,” “influenza” and “pandemic.” The group also conducted an in-depth review of the disaster literature, military protocols and published pandemic plans as well as Internet searches and networking with experts in critical care medicine, military medicine and disaster medicine to identify any existing critical care triage protocols or to find information necessary to develop a protocol if none existed. Preliminary results of this work, including a prototype triage protocol, were incorporated into the June 2005 version of the OHPIP.7 The prototype protocol was then refined in January 2006 on the basis of input from leading experts in a wide variety of relevant medical disciplines across Ontario.
Subsequently 150 critical care leaders in the province were invited to comment on the final report of the working group, which included the triage protocol. Fifty-five of these leaders reviewed the report and provided feedback, which was used to improve the clarity of the protocol. In this article we present our proposed protocol for critical care triage during an influenza pandemic.
Results
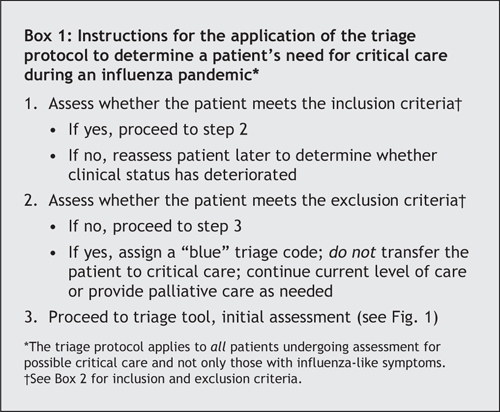
The literature search, Internet searches and consultations with experts failed to identify any general triage protocols for critical care. Therefore, the working group embarked on developing a critical care triage protocol. Although triage protocols were identified for trauma17–20 and chemical, biological, radiation and nuclear events,16 these were not felt to be generalizable to the population or situations in critical care. However, certain features of these protocols (e.g., a colour-coded triage tool,21 inclusion criteria, exclusion criteria and minimum qualifications for survival16) were deemed useful for a triage protocol for critical care. Illness severity scoring systems used to predict critical care outcomes were also assessed for potential inclusion in the protocol.22–27 The Sequential Organ Failure Assessment (SOFA) score was felt to be the most appropriate scoring system for use in a triage protocol given its basis on physiologic parameters, ease of calculation, requirement for simple laboratory tests and its validation for use in patients with a wide variety of conditions requiring critical care.22,28–31 (The scoring criteria for the SOFA score are provided in Appendix 1, available online at www.cmaj.ca/content/cgi/full/175/11/1377/DC1.) The final protocol developed by the working group is presented in part in Fig. 1 and in Box 1 and Box 2.
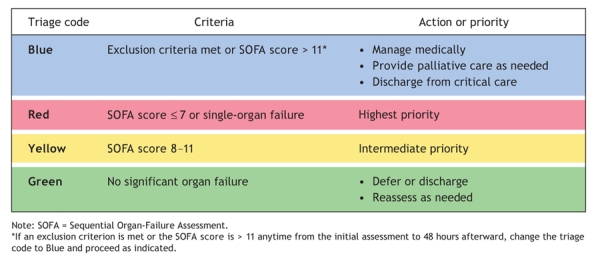
Fig. 1: Prioritization tool used in triage protocol for the initial assessment of patients' needs for critical care during an influenza pandemic. See online Appendix 1 for the SOFA scoring criteria and online Appendix 2 for the complete prioritization tool, which includes details on reassessing patients at 48 and 120 hours (appendices are available at www.cmaj.ca/cgi/content/full/175/11/1377/DC1). See Box 2 for exclusion criteria.
The protocol is designed to provide guidance for making triage decisions during the initial days to weeks of an influenza pandemic if the critical care system is overwhelmed. The impetus for this triage protocol was the potential for the critical care system to be flooded by patients with influenza during a pandemic. However, it must be noted that the triage protocol would apply to all patients who are being considered for critical care, not just those with influenza, since all patients must share a single pool of resources.
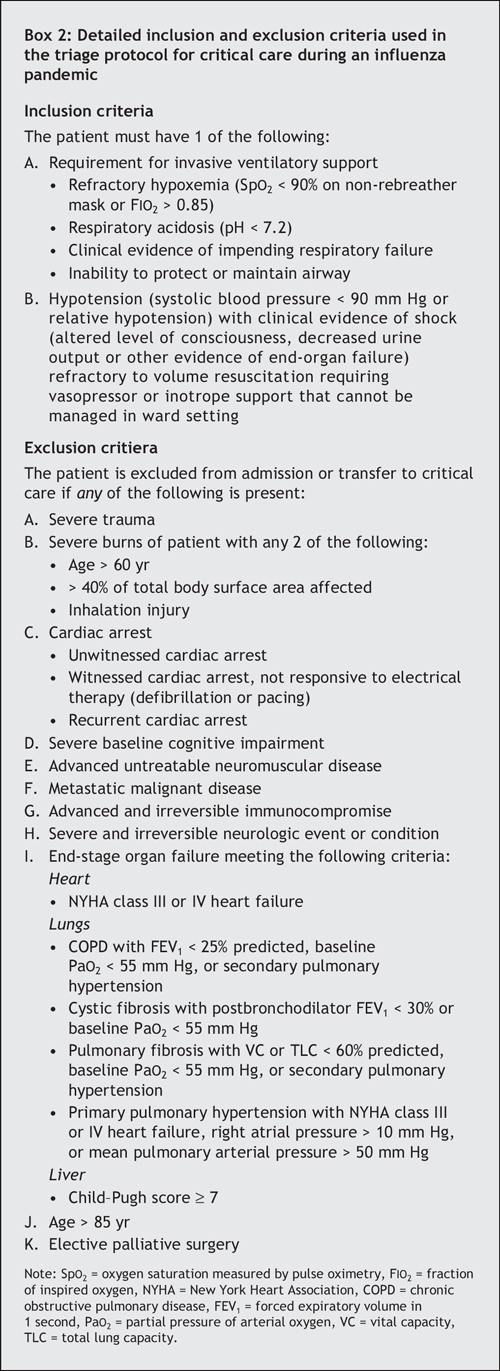
The triage protocol has 4 main components: inclusion criteria, exclusion criteria, minimum qualifications for survival and a prioritization tool. The inclusion criteria (Box 2) identify patients who may benefit from admission to critical care and primarily focus on respiratory failure, since the provision of ventilatory support is what fundamentally differentiates the ICU from other acute care areas (e.g., step-down units). It is anticipated that expanded care models will be developed as part of the surge capacity response and will permit hemodynamic support and other advanced care modalities to be provided in areas that have appropriate monitoring but do not typically provide this level of care. However, should hemodynamic support not be available elsewhere, it will qualify as an inclusion criterion for critical care admission.
The exclusion criteria (Box 2) can be broken down into 3 categories: patients who have a poor prognosis despite care in an ICU, patients who require resources that simply cannot be provided during a pandemic and patients with advanced medical illnesses whose underlying illness has a poor prognosis with a high likelihood of death, even without their current concomitant critical illness. The first category reflects the “hard” boundaries that many intensivists recognize from their day-to-day care of patients,32–35 such as end-stage cancer, severe burns,36 severe trauma,37,38 unwitnessed or recurrent cardiac arrests39 and patients with a baseline SOFA score greater than 11, who have more than a 90% mortality.22,28 Advanced age clearly contributes to higher death rates in specific disease subsets of critically ill patients,40,41 but it may not be a strong predictor of critical care outcomes in general and therefore was not included in the original draft protocol. However, we received strong and consistent feedback from both expert and stakeholder consultations that an age criterion should be included. This remains one of the areas requiring further research and community input.
The second category of exclusion criteria includes patients who may benefit from critical care but would require intense use of resources and prolonged care that cannot be justified during a pandemic, when the goal is to do the most for the most with the limited resources available. The third category of exclusion criteria includes patients who have high resource requirements and are likely to experience significant complications from influenza (e.g., patients with advanced cancer or immunosuppression). Others in this category are patients who have end-stage cardiac, hepatic or pulmonary failure. The cut-off marks selected here are adapted from the transplant literature42–45 and typically represent a baseline death rate higher than 50% within the next 1 to 2 years. Given that transplantation is unlikely during a pandemic, combined with the cumulative risk of death from their acute critical illness, these patients again fall into a category where considerable resources would have to be expended with a low probability of long-term survival. Many of the criteria in this third category require more detailed definitions in order to put it into practice. These were omitted for brevity but will be included in the training provided for triage officers.
The “minimum qualifications for survival” form the third component of the triage protocol. These qualifications represent a ceiling on the amount of resources that can be expended on any one person. This is a concept foreign to many medical systems in developed countries but one that has been used in war zones and refugee camps.16 The minimum qualifications for survival dictate reassessment at 48 and 120 hours, as well as an ongoing cut-off ceiling if a patient ever has a SOFA score of 11 or higher or any other exclusion criteria. The key component of the minimum qualifications for survival is the attempt to identify at an early stage patients who are not improving and who are likely to have a poor outcome. In day-to-day practice, it may take days or weeks of intensive care before this poor outcome occurs. During a pandemic, several other patients could have had their lives saved during this time.
The final component of the triage protocol is a tool for the prioritization of patients for admission to the ICU and access to ventilation (Fig. 1; see the complete prioritization tool in Appendix 2, available online at www.cmaj.ca/cgi/content/full/175/11/1377/DC1). For ease of use, the familiar colour scheme (blue or black, red, yellow, green) commonly used in civilian and military disaster triage protocols was adopted. Patients in the blue (or black) category are those who fall into the expectant category and should not receive critical care. Depending on their condition and medical issues, patients may either continue to have curative medical care on a ward or palliative care. Patients in the red category have the highest priority for ICU admission and mechanical ventilation, if required. In selecting the patients for this category, the aim is to find those who are sick enough to require the resource and whose outcome will be poor if they do not receive it but are not so sick that they will not recover even if they do receive ICU care. Patients with single organ failure, particularly those with respiratory failure due to influenza who otherwise have a low SOFA score, are included in the red category assuming they have no exclusion criteria. These patients will derive the maximum benefit from ICU care and mechanical ventilation. The goal is to optimize the effectiveness of the triage protocol so that every patient who receives resources will survive. Although this is unlikely to be completely successful, it can be used as a target to guide modification of the triage protocol based on patient outcomes during a pandemic. Patients in the yellow category are those who, at baseline, are very sick and may or may not benefit from critical care. They should receive care if the resources are available but not at the expense of denying care to someone in the red category. At the reassessment points, patients who are improving are given high priority (red) for continued care, while those who are not showing signs of improvement are classified as yellow. Patients in the green category are those who should be considered for transfer out of the ICU because they are well enough to be cared for without mechanical ventilation or other ICU-specific interventions.
Interpretation
This triage protocol is a tool aimed at maximizing benefits for the largest number of patients presenting to an overwhelmed critical care system. The ethical values that inform this protocol were derived from the work of the Joint Centre for Bioethics, in the document Stand on Guard for Thee.46 The authors identify 10 substantive values (individual liberty, protection of the public from harm, proportionality, privacy, duty to provide care, reciprocity, equity, trust, solidarity and stewardship) and 5 procedural values (reasonable, open and transparent, inclusive, responsive and accountable).
Under normal circumstances, all patients should have an equal claim to receive the health care they need. Unfortunately, during a pandemic it will not be possible for all patients to receive intensive care due to finite resources. A triage protocol will assist in distributing the available resources fairly by triaging patients who will not benefit from treatment to noncritical care management, thereby conserving critical care resources for patients who are more likely to benefit. Although it may be unfortunate that some patients do not receive all that they could possibly “use,” this does not by default make it unfair. Any restrictions placed on treatment must, however, adhere to the value of proportionality, which requires that restrictions to individual liberties not exceed what is necessary to address the essential needs of the community.
The protocol was developed by experts in advance of a pandemic, to allow time for thoughtful contemplation and community input before ever employing the protocol. When the protocol is implemented, it must be used in an open and transparent manner. Its limitations must be acknowledged, with plans to revise it as information becomes available regarding prognostic factors, specifics of the influenza virus causing the pandemic and resource availability. Processes for ongoing re-evaluation and for consideration of exceptions must be developed in addition to an appeals mechanism. Aside from being an ethical imperative, a process to evaluate and refine the triage protocol prevents undertriage or overtriage, both of which increase overall deaths in disasters.47 This process will require a central triage committee as well as appropriate infrastructure to collect and review the information for analysis and to disseminate revisions to the protocol. This committee may serve many different and distant critical care centres. The central triage committee must assure a population-based approach with equitable resource allocation. Advanced training will be required for triage officers to effectively implement the triage protocol. This is not unique to our protocol, since most military and disaster triage guidelines also require extensive training for effective use.
The primary limitation of the current protocol is that it has never been used. Future efforts to test and refine the protocol through modeling and disaster exercises are underway. Such activities will offer the first insight into the true utility of our protocol. A recently published conceptual framework for developing triage guidelines for use in a pandemic includes exclusion criteria similar to those developed by our working group.48
This triage protocol for critical care during an influenza pandemic was developed through a collaborative process using best evidence and applying ethical principles. It has been designed to be practical, user-friendly and flexible, but it requires testing in advance of a pandemic. It must be modified as information accrues during a pandemic. A significant lesson learned during this exercise is that development of a triage protocol is a complex process that cannot be undertaken during a pandemic. Similarly, the resource infrastructure required to support effective triage management must also be planned, established and tested before a pandemic. Whether jurisdictions adopt this triage protocol or work to develop alternatives, the time to begin the process is now.
@ See related article page 1393
Acknowledgments
The Emergency Management Unit of the Ontario Ministry of Health and Long-Term Care provided financial and logistical support for an expert panel retreat to refine the prototype and Internet resources for the stakeholder consultation. The Ontario Ministry of Health and Long-Term Care provided staff support for the working group.
Footnotes
This article has been peer reviewed.
Contributors: All of the authors contributed to the design of the triage protocol and provided intellectual content to the article. All of the authors approved the final version for publication.
Competing interests: None declared.
Correspondence to: Dr. Michael D. Christian, Rm. 2U, McMaster University Medical Centre, 1200 Main St. W., Hamilton ON L8N 3Z5; fax 905 523-1224; [email protected]
REFERENCES
Articles from CMAJ : Canadian Medical Association Journal are provided here courtesy of Canadian Medical Association
Full text links
Read article at publisher's site: https://doi.org/10.1503/cmaj.060911
Read article for free, from open access legal sources, via Unpaywall:
http://www.cmaj.ca/content/175/11/1377.full.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1503/cmaj.060911
Article citations
COVID-19 critical care triage across Canada: a narrative synthesis and ethical analysis of early provincial triage protocols.
Can J Anaesth, 71(8):1126-1136, 08 Apr 2024
Cited by: 0 articles | PMID: 38589739 | PMCID: PMC11269410
Predictors of outcomes of patients ≥ 80 years old admitted to intensive care units in Poland - a post-hoc analysis of the VIP2 prospective observational study.
Anaesthesiol Intensive Ther, 56(1):61-69, 01 Jan 2024
Cited by: 0 articles | PMID: 38741445 | PMCID: PMC11022638
A Nursing Care Model for Surge Capacity Management in Intensive Care Units During the COVID-19 Pandemic: Experience From Qatif Central Hospital, Saudi Arabia.
Cureus, 15(11):e48193, 02 Nov 2023
Cited by: 1 article | PMID: 38050496 | PMCID: PMC10693669
Dialysis resource allocation in critical care: the impact of the COVID-19 pandemic and the promise of big data analytics.
Front Nephrol, 3:1266967, 26 Oct 2023
Cited by: 0 articles | PMID: 37965069 | PMCID: PMC10641281
Review Free full text in Europe PMC
Exploring the clinical benefit of ventilation therapy across various patient groups with COVID-19 using real-world data.
Sci Rep, 13(1):10747, 03 Jul 2023
Cited by: 3 articles | PMID: 37400560 | PMCID: PMC10318022
Go to all (176) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Ethics of triage in the event of an influenza pandemic.
Disaster Med Public Health Prep, 2(2):114-118, 01 Jun 2008
Cited by: 19 articles | PMID: 18525374
Simple triage scoring system predicting death and the need for critical care resources for use during epidemics.
Crit Care Med, 35(5):1251-1256, 01 May 2007
Cited by: 51 articles | PMID: 17417099
An assessment of the validity of SOFA score based triage in H1N1 critically ill patients during an influenza pandemic.
Anaesthesia, 64(12):1283-1288, 23 Oct 2009
Cited by: 44 articles | PMID: 19860754
Triage of mechanical ventilation for pediatric patients during a pandemic.
Disaster Med Public Health Prep, 6(2):131-137, 01 Jun 2012
Cited by: 7 articles | PMID: 22700021
Review