Abstract
Free full text

Genetic complexity of autoimmune myocarditis
Abstract
Autoimmune myocarditis, a chronic stage of myocardial inflammation, occurs in a small subset of patients after acute cardiotropic viral infection and can lead to dilated cardiomyopathy (DCM). This disease can be recapitulated in susceptible mouse strains by infection with coxsackievirus B3, or by immunization with cardiac myosin or cardiac troponin I. The etiologies of myocarditis are multifactorial and genetically complex. Genetic linkage between susceptibility to myocarditis/DCM and the major histocompatibility complex (MHC) genes have been reported in both humans and experimentally induced mouse models. However, unlike other autoimmune diseases, the non-MHC genes seem to have greater impact than MHC genes on disease susceptibility. Several myocarditis-related non-MHC loci have been identified by our laboratory and others in different models. Most of these loci overlap with other autoimmune disease susceptibility loci, suggesting common or shared genetic traits influencing general autoimmunity. For example, we have demonstrated that Eam1 and Eam 2 may influence disease susceptibility via regulating T cell apoptosis at different developmental stages. Blockade of signaling through specific genes, such as CTLA4, ICOS and PD-1, can either enhance or prevent the development of experimental autoimmune myocarditis, but it remains unclear whether functional polymorphisms in these genes are involved in predisposition to disease. In humans, mutations/deletions in immunologically important genes such as CD45, and genes encoding cardiac proteins, have been reported in patients with recurrent myocarditis or DCM. Identification of genetic polymorphisms controlling autoimmune myocarditis will help us understand the mechanisms underlying autoimmune diseases in general, thereby improving potential therapies in patients.
1. Autoimmune Myocarditis in Humans
Myocarditis, pathologic inflammation of the myocardium, is the leading cause of heart failure in patients less than 40 years of age [1]. About 10-20% of people with histological evidence of myocarditis, even in asymptomatic patients, will develop chronic disease eventually leading to dilated cardiomyopathy (DCM) [2]. Despite the well-established morbidity and mortality associated with myocarditis, its clinical etiologies and presentations are broad and difficult to evaluate. Cardiotropic viruses, such as coxsackievirus B3 (CVB3), are well known agents that can induce clinical myocarditis [3]. After the acute phase caused by direct cytopathic effects of the virus, a small proportion of patients subsequently develop autoimmune-mediated, chronic myocarditis [4], accompanied by circulating autoantibodies to cardiac myosin and other heart antigens, which can sometimes lead to heart failure and death associated with DCM.
2. Murine models of autoimmune myocarditis
Animal models resembling human myocarditis can be produced in susceptible mice by intraperitoneal inoculation of heart-passaged CVB3 [5] or immunization with purified cardiac myosin or cardiac α-myosin heavy chain peptide in complete Freund’s adjuvant [6]. After the acute phase of viral myocarditis has subsided, a few strains of mice, especially A/J and other strains sharing the A background, develop a second phase characterized by diffuse intra-heart infiltrates and large areas of myocyte necrosis and fibrosis. This phase occurs in the absence of infectious virus [7] and is believed to be mediated by cardiac-specific autoimmune responses, as suggested by the presence of IgG autoantibodies to cardiac myosin [8, 9]. Myocarditis induced by immunization with cardiac myosin or its peptide provides a virus-free mouse model, which simulates the second phase of the viral disease. Most important, cardiac myosin immunization produces pathology only in strains of mice that are susceptible to the second phase of CVB3-induced myocarditis, showing that the genetic predisposition to autoimmune myocarditis is similar in both models [10]. Furthermore, adoptive transfer of activated autoreactive T cells [11, 12] or autoantibodies [13] derived from cardiac myosin - immunized mice are able to induce disease in recipients of different strains, suggesting that myocarditis with similar phenotypic characteristics may develop via different mechanisms. In addition, immunization with another cardiac-specific autoantigen, troponin I, was also able to elicit severe autoimmune myocarditis in A/J mice followed by cardiomegaly, fibrosis, reduced fractional shortening, and reduced survival rate [14].
Very recently, Tanejia V. et al. developed a spontaneous myocarditis model in NOD mice (Ag7-/-) carrying the human DQ8 molecule (NOD.DQ8.Aβo) [15]. In this model, a high mortality was observed in female NOD.DQ8.Aβo mice at 16 weeks or older, associated with severe systolic dysfunction, enlarged heart with mononuclear infiltrates, and autoreactive T and B cells. Yet, NOD.DR3.Aβo, the trangene negative littermates, NOD and B10. DQ8 mice had no sign of cardiac pathology. Interestingly, in the spontaneous model females were predominantly affected, in contrast to human cases and the induced models where males seem to have a somewhat greater incidence [1, 16]. These results may imply different roles of sex-related genes in pathogenesis of spontaneous versus induced myocarditis.
3. Genetic linage between MHC and autoimmune myocarditis
Autoimmune myocarditis is a disease of heterogeneous etiology, involving interplay between predisposing genes and triggering environmental factors. Polymorphisms in the major histocompability complex (MHC) are among the strongest predisposing genetic factors in autoimmune diseases in general [17]. Most genetic studies in humans have been performed in patients with DCM, in which only some cases may represent an end stage of autoimmune myocarditis. In these studies, both serologic analyses [18-21] and recent molecular analyses [22, 23] have suggested that a significant correlation of DCM with MHC class II antigens, particularly HLA-DR4. Yet, this association was not observed in a small populational study with 36 patients (32 DCM and 4 myocarditis) [24]. Other positive (DR12, DR15, DPB*0601) [22-24] and negative (DR11, DQB1*0301) [23] associations have also been reported, but are also inconsistent between populations. The discrepancy in MHC association with DCM between different groups may be relevant to the differencing influences of ethnic origin, sex, age and geographic parameters of the populations under study. In one of the above studies [24], 4 myocarditis patients had been analyzed separately. Although no conclusion with statistical significance could be drawn due to the limited number of cases, all 4 patients were DQ5 positive and 3 possessed the allele DQB1*0501. In addition, the development of spontaneous myocarditis in NOD mice (Ag7-/-) carrying DQ8 but not DR3 transgene suggests polymorphisms in MHC class II is important in predisposition to myocarditis and HLA-DQ8 may be a risk factor in humans [15].
In studies of mice, determination of the MHC contribution to susceptibility to myocarditis were made among the H-2 congenic mice on either A/J (A/J, H-2a; A.BY, H-2b; A.CA, H-2f and A.SW, H-2s) or C57BL/10J (B10.A, H-2a; B10.S, H-2s and B10.PL, H-2u) backgrounds [10, 25]. Interestingly, in both viral and myosin-induced models, the s, a and f haplotypes are associated with increased morbidity of autoimmune-based myocarditis, whereas the b haplotype is associated with a relatively low responsiveness. Notably, the MHC polymorphisms also influence the prevalence and titer of cardiac-specific autoantibodies. For example, the A.BY mice are poor producers of myocardial autoantibodies, whereas A.SW and A.CA are good producers after either viral infection or myosin immunization [10, 25].
The role of MHC class I in autoimmune myocarditis has not been well elucidated in either humans or animals. Lin A et al. have reported that a 14bp deletion in the 3’-untranslated region of human nonclassical MHC class I genes, HLA-G, is a risk factor for DCM in a Chinese Han population [26]. Strong linkage disequilibrium between HLA-G and, in particular HLA-DR and DQ alleles, was also observed [27], indicating that HLA-G alone or together with the linked HLA-DR or DQ allelic products could play a role in the development of autoimmune myocarditis.
4. Genetic linage between non-MHC loci and autoimmune myocarditis
Progress in delineating the role of non-MHC genes in autoimmune diseases has been more problematic, probably because of the overriding influence of MHC in most instances [18]. In humans, several DCM-related non MHC loci have been defined on chromosomes 1q32, 2q11-22, 2q31, 9q13-22 and 10q21-23 [28], but it is unclear whether they are associated with autoimmune myocarditis.
The murine model of autoimmune myocarditis has unique advantages in mapping non-MHC loci because the major determinants of disease susceptibility seem to reside outside the MHC. We previously reported that most A congenic mouse strains, such as A/J, A.CA and A.SW differing only at the MHC locus (H-2 a, f, s, respectively), are susceptible to chronic autoimmune myocarditis after infection with CBV3. In contrast, mouse strains with a B10 background such as C57BL/10J, B10.A, B10.S and B10.PL (H-2 b, a, s, u, respectively) are largely resistant [25]. The similar pattern was confirmed in myosin-induced myocarditis model [10]. These results highlight the importance of genes that are not closely linked to MHC in the susceptibility to autoimmune myocarditis. To focus on the role of non-MHC genes on susceptibility to myosin-induced myocarditis, we used two prototypic mouse strains – A.SW and B10.S - that share the same MHC genes but have either A or B background. A.SW is susceptible and B10.S is resistant to autoimmune myocarditis, respectively. Utilizing polymorphic SSLP markers throughout the murine genome, linkage analysis of F1 × F1 (F2) mice revealed two non-MHC loci – the Eam1 on proximal chromosome l and Eam2 on distal region of chromosomes 6 – that are either significant or highly suggestive linkage to autoimmune myocarditis [16]. Both loci or their human counterparts have been previously identified in other autoimmune diseases such as lupus, diabetes, autoimmune encephalomyelitis and autoimmune orchitis in mouse [29-32], as well as diabetes and autoimmune thyroid disease in humans [33-35] (Fig.1). This observation suggests that although autoimmune diseases display a large variety of clinical manifestations, there are likely controlled by a number of shared inherited genetic abnormalities and pathogenic mechanisms. It also highlights the importance of understanding the genetic mechanisms leading to autoimmunity in any model system, including myocarditis, since knowledge gained will likely have wider applicability. Interestingly, we have found that both Eam1 and Eam2 influence the apoptosis of T cells at different stages of development [16] (Fig.1). It remains to be demonstrated that the genetic elements controlling sensitivity to apoptosis maps to the same location as those controlling disease susceptibility, and how these two phenomena are related.
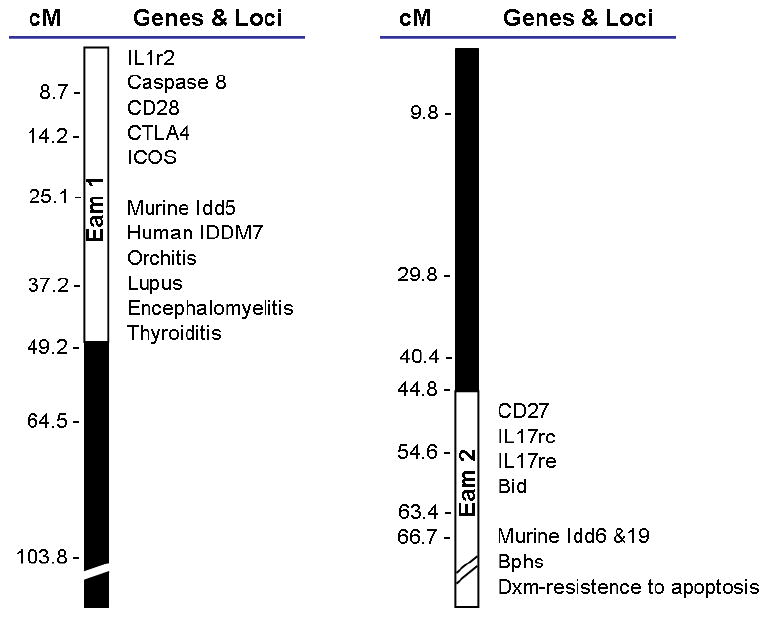
Genetic mapping data suggest that loci on Chrs. 1 and 6 play a role in susceptibility to experimental autoimmune myocarditis. These loci have been tentatively named Eam1 and Eam2. Eam1 overlaps with loci found to be important in human diabetes (IDDM7), and autoimmune thyroid disease, and murine diabetes (Idd5). This locus harbors important immune genes like IL1r2, caspases 8, CD28, CTLA4 and ICOS. Eam2 harbors genes like CD27, IL17rc, IL17re and Bid, as well as overlaps with other loci important for murine diabetes (idd6 and idd19), Bphs (Bordetella pertussis-induced histamine sensitization) and Dxm-resistance to apoptosis.
Very similar to our approach, a Canadian group recently reported three loci in A/J --H2a mice that control susceptibility to CVB3-induced myocarditis in comparison to B10.A-H2a mouse strain [36]. These three loci include one locus (Vms1) on chromosome 1 centered on D1Mit200 (80 cM), a second locus (Vms2) on chromosome 4 centered on D4Mit81 (38 cM) and a third locus (Vms3) on chromosome 3 centered on D3Mit19 (87.6 cM). Vms1 was linked to both myocardial infiltration and sarcolemmal damage in females, whereas Vms 2 and Vms3 were segregated only with sarcolemmal damage in males. None of them overlap with our loci, but Vms1 region was previously identified as heart failure modifier locus and Vms2 was defined for initial spontaneous loss of immunologic tolerance [36].
Other strains of mouse, such as BALB/c and DBA/2, also demonstrate susceptibility to autoimmune myocarditis induced by CBV3 infection or cardiac myosin immunization. However, the pathogenic mechanisms may be different. Myocarditis in A/J and Balb/c mice is transferable only with activated lymphocytes, whereas disease can be induced in DBA/2 mice by passive transfer of myosin-specific autoantibodies [13]. Analysis of DBA/2xCByD1F1 backcross mice has suggested that a locus on chromosome 12 is strongly linked with autoantibody-induced myocarditis and a second region on chromosome 1 that contributes to disease susceptibility only in male mice [13].
5. Specific genes that relate to autoimmune myocarditis
Despite the progress in identification of potential myocarditis-related loci in both human and mouse, disease-causing mutations are rarely defined. A case report on a 31-year-old female suggested that myocarditis may be associated with C77G polymorphism of CD45 exon 4, which alters the splicing and CD45RA/CD45RO phenotype of lymphocytes [37]. Mutations/deletions in genes encoding cardiac proteins, including cardiac actin [38], cardiac β-myosin heavy chain and cardiac troponin T [28], have also been found in patients with DCM; again their significance in autoimmune myocarditis in particular is not specified.
Polymorphisms in costimulatory molecule CTLA-4 have been reported to influence the development of autoimmune diseases in general [17]. Blocking of CTLA-4 function exacerbated autoimmune myocarditis in both A/J and C57BL/6 mice, but no polymorphisms in CTLA-4 have been found between the two strains (Ligons D. and Cihakova D., unpublished data). Similarly, manipulation of other immunologically important regulatory genes, such as ICOS [39] and PD-1 [40], is able to influence the development of autoimmune myocarditis in animal models. For example, administration of anti-ICOS blocking antibodies attenuates the incidence and severity of the disease [39], whereas blocking of PD-1/PD-1 ligands pathway increased the myocardial inflammation [40]. However, it remains unclear whether genetic polymorphisms distinguish susceptible and resistant human subjects or mouse strains.
6. Concluding Remarks
Genetic mapping of complex disease traits and, in particular, those associated with autoimmune disease, is complicated, since most of them have a polygenic basis. Susceptibility to autoimmune myocarditis varies among populations and strains of mice, and possibly is controlled by different genetic factors associated with distinct etiology. Among multiple autoimmune diseases including diabetes, lupus, myocarditis and thyroiditis, several defined non-MHC susceptibility loci overlap or are shared, suggesting common genetic predisposition. Further identification of disease-causing mutations will not only facilitate the discovery of populations in risk, but also help in establishment of therapeutic strategies through unraveling the pathogenic mechanisms of autoimmune diseases.
Acknowledgments
The authors’ research is supported by NIH research grants R01 HL-077611 and R01 HL067290.
Footnotes
Take-home messages
Chronic myocarditis in humans after acute viral infection invloves autoimmune-mediated cardiac impairment.
Autoimmune myocarditis can be induced by viral infection or cardiac antigen immunization in susceptible mouse strains, or spontaneous develop in NOD.DQ8 transgenic mouse.
Susceptibility to experimental autoimmune myocarditis varies among different strains of mice. It is mainly controlled by non-MHC genes, but MHC class II genes modify the severity of the disease
Loci controlling autoimmune myocarditis overlap with other autoimmune disease loci, suggesting common or shared genetic traits.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
Full text links
Read article at publisher's site: https://doi.org/10.1016/j.autrev.2007.11.010
Read article for free, from open access legal sources, via Unpaywall:
https://europepmc.org/articles/pmc2233796?pdf=render
Citations & impact
Impact metrics
Article citations
T-Cell Receptor Sequences Identify Combined Coxsackievirus-Streptococci Infections as Triggers for Autoimmune Myocarditis and Coxsackievirus-Clostridia Infections for Type 1 Diabetes.
Int J Mol Sci, 25(3):1797, 01 Feb 2024
Cited by: 0 articles | PMID: 38339075 | PMCID: PMC10855694
Myocarditis in Athletes: Risk Factors and Relationship with Strenuous Exercise.
Sports Med, 54(3):607-621, 11 Dec 2023
Cited by: 1 article | PMID: 38079080
Review
Immunomodulatory Therapy for Giant Cell Myocarditis: A Narrative Review.
Cureus, 15(6):e40439, 14 Jun 2023
Cited by: 1 article | PMID: 37456487
Review
Clostridia and Enteroviruses as Synergistic Triggers of Type 1 Diabetes Mellitus.
Int J Mol Sci, 24(9):8336, 06 May 2023
Cited by: 1 article | PMID: 37176044 | PMCID: PMC10179352
Immunopathogenesis and immunomodulatory therapy for myocarditis.
Sci China Life Sci, 66(9):2112-2137, 29 Mar 2023
Cited by: 4 articles | PMID: 37002488 | PMCID: PMC10066028
Review Free full text in Europe PMC
Go to all (50) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Inflammatory dilated cardiomyopathy (DCMI).
Herz, 30(6):535-544, 01 Sep 2005
Cited by: 78 articles | PMID: 16170686
Review
Animal models for autoimmune myocarditis and autoimmune thyroiditis.
Methods Mol Med, 102:175-193, 01 Jan 2004
Cited by: 61 articles | PMID: 15286386
Novel nonmajor histocompatibility complex-linked loci from mouse chromosome 17 confer susceptibility to viral-mediated chronic autoimmune myocarditis.
Circ Cardiovasc Genet, 3(5):399-408, 21 Aug 2010
Cited by: 3 articles | PMID: 20729557
Genetically determined myocarditis: clinical presentation and immunological characteristics.
Curr Opin Cardiol, 23(3):219-226, 01 May 2008
Cited by: 16 articles | PMID: 18382209
Review
Funding
Funders who supported this work.
NHLBI NIH HHS (6)
Grant ID: R01 HL067290
Grant ID: R01 HL077611-03S1
Grant ID: R01 HL-077611
Grant ID: R01 HL077611-04
Grant ID: R01 HL067290-06
Grant ID: R01 HL077611





