Abstract
Objective
To examine the relationships among maternal and child depressive symptoms and child and family psychosocial factors.Method
Secondary analysis of baseline data for a coping skills intervention for school-age children (ages 8-12) with type 1 diabetes (T1D) and their mothers. Children and mothers completed measures of depressive symptoms, coping, quality of life, and family functioning.Results
There was a strong relationship between maternal and child depressive symptoms (r = .44, p < .001). Maternal depressive symptoms were negatively related to child quality of life, perceptions of coping, and family functioning. Impact of diabetes on quality of life, finding coping with diabetes upsetting, and family warmth mediated the relationship between maternal and child depressive symptoms.Conclusions
Maternal depression may negatively affect child adjustment through its influence on quality of life, coping, and family functioning. Implications for interventions to improve psychosocial adjustment in children with T1D are discussed.Free full text

Mediators of Depressive Symptoms in Children with Type 1 Diabetes and their Mothers
Abstract
Objective
To examine the relationships among maternal and child depressive symptoms and child and family psychosocial factors.
Method
Secondary analysis of baseline data for a coping skills intervention for school-age children (ages 8-12) with type 1 diabetes (T1D) and their mothers. Children and mothers completed measures of depressive symptoms, coping, quality of life, and family functioning.
Results
There was a strong relationship between maternal and child depressive symptoms (r = .44, p < .001). Maternal depressive symptoms were negatively related to child quality of life, perceptions of coping, and family functioning. Impact of diabetes on quality of life, upset related to coping, and family warmth mediated the relationship between maternal and child depressive symptoms.
Conclusions
Maternal depression may negatively affect child adjustment through its influence on quality of life, coping, and family functioning. Implications for interventions to improve psychosocial adjustment in children with T1D are discussed.
Type 1 diabetes (T1D) is one of the most common chronic childhood illnesses, affecting 1 in every 400 individuals under the age of 20 (National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), 2002). The recommended treatment regimen for T1D is complex and demanding, requiring frequent monitoring of blood glucose levels (at least 4/day), monitoring and controlling of carbohydrate intake, frequent insulin administration (3-4 injections/day or infusion from a pump), altering insulin dose to match diet and activity patterns, and checking urine for ketones when necessary (American Diabetes Association, 2007). A landmark study demonstrated that following this intensive regimen and maintaining glycemic control may delay or prevent medical complications in youth with T1D by 27% to 76% (DCCT Research Group, 1994). However, adherence to the demands of such intensive treatment may be burdensome and stressful for youth with T1D and their mothers, who are primarily responsible for treatment management (Anderson et al., 2002).
Children with T1D are at risk for psychological disorders, especially depression, with rates as high as 33% (Blanz, Rensch-Riemann, Fritz-Sigmund, & Schmidt, 1993). In a study that followed youth with T1D for 9 years, 42.4% of youth developed at least one episode of psychiatric disorder during the follow-up, with depressive disorders being the most common (27.5%) followed by anxiety disorders (19.6%) (Kovacs, Goldston, Obrosky, & Bonar, 1997). In addition, children and adolescents with diabetes experience longer episodes of depression than medically-well depressed youth (Kovacs, Obrosky, Goldston, & Drash, 1997). Further, there is some evidence that depression in children is related to poor metabolic control (Hassan, Loar, Anderson, & Heptulla, 2006), increased risk for retinopathy (Kovacs, Mukerji, Drash, & Iyengar, 1995), and increased risk for hospitalization (Garrison, Katon, & Richardson, 2005; Stewart, Rao, Emslie, Klein, & White, 2005). Evidence also suggests that ‘subthreshold depression’ or increased depressive symptoms in children and adolescents in the general population are associated with poor health outcomes (Lewinsohn, Solomon, Seeley, & Zeiss, 2000). As a result of these findings, the American Diabetes Association recently issued a statement calling for regular annual screening for depression in children ages 10 and older as part of children’s clinical care (Silverstein et al., 2005). However, the majority of research on psychological disorders in children with T1D has been conducted with adolescents, and less is known about depressive symptoms and family functioning in school-age children.
Not only does T1D increase the risk of psychological disorders in children, but evidence supports that parents, particularly mothers, of children with T1D also experience psychosocial distress (Kovacs, Goldston et al., 1997; Mullins et al., 2004). Parents of children with T1D report parenting stress associated with the responsibility required to manage T1D on a daily basis and fears of hypoglycemia (Streisand et al., 2005). Research also indicates that most parents are likely to experience significant distress (e.g., symptoms of anxiety and depression) after the initial diagnosis, and that mothers report more distress than fathers (Kokkonen, Taanila, & Kokkonen, 1997), but little is known about the effects of parents’ adjustment over time. One of the only longitudinal studies of depressive symptoms in mothers of children with T1D found that after a period of initial adjustment, mothers seem to experience an increase in depressive symptoms and overall psychological distress with duration of illness (Kovacs et al., 1985, 1990). In addition, a recent study of parents of children ages 8-12 with T1D found that 29% of parents scored above the clinical criterion for increased depressive symptoms (Whittemore, Urban, Tamborlane, & Grey, 2003). These findings suggest that a considerable number of children with T1D have parents who are experiencing significant emotional distress, which is likely to impact children’s psychosocial adjustment.
A review of parent and family functioning in parents of children with chronic illness found that greater maternal psychological adjustment problems (e.g., distress) were related to poorer psychosocial adjustment in children (Drotar, 1997). Increased maternal distress has been related to higher levels of distress in children with T1D, and maternal psychological distress and depressive symptoms have been shown to predict later child depressive symptoms (Chaney et al., 1997; Kovacs, Goldston et al., 1997). More specifically, one study found that children with T1D whose mothers were depressed developed depressive disorders at a rate 2.64 times than children with T1D whose mothers were not depressed (Kovacs, Goldston et al., 1997).
In the general literature on children of depressed parents, it is well established that maternal depression is a risk factor for child psychopathology, especially depression (Beardslee, Versage, & Gladstone, 1998). The effects of maternal depression on children are likely transmitted through multiple mechanisms, including exposure to negative maternal cognitions, behaviors, and affect, and the stressful context of the children’s lives (Goodman & Gotlib, 1999). Depressed mothers may model maladaptive ways of thinking and coping, thereby compromising children’s ability to cope successfully with stressful life events (Hammen, Shih, & Brennan, 2004). Maternal depression may also contribute to impaired parenting and marital conflict, creating a stressful environment which may negatively affect child development and child psychosocial health (Cummings & Davies, 1994).
Family functioning has been strongly linked to children’s adjustment to diabetes, including metabolic control and psychosocial functioning. In general, greater parental involvement, more diabetes-specific support, and less family conflict has been related to better childhood adjustment to diabetes (Grey, Boland, Yu, Sullivan-Bolyai, & Tamborlane, 1998; Hanson, De Guire, Schinkel, & Henggeler, 1992; Sayfer et al., 1993). However, little research has been undertaken to determine specific family factors associated with depression in children, especially those younger than adolescence, with T1D. In one such study, adolescents with clinically significant depressive symptoms were more likely to perceive their families as extreme (rigid and disengaged) and less likely to perceive their families as balanced (flexible and connected) than adolescents with fewer depressive symptoms. Moreover, higher levels of depressive symptoms were related to lower levels of cohesion and adaptability and less diabetes-specific warmth/support (Whittemore et al., 2002).
Thus, children with T1D and their mothers are at increased risk for depressive symptoms, and maternal depression may contribute to the development of depressive symptoms in children by creating a stressful family environment. Further research is needed on the prevalence and implications of maternal depression in mothers of children with T1D. While a significant number of youths with T1D suffer from psychological disorders (e.g., depression), many do not experience any serious adjustment problems (Grey, Boland, Yu et al., 1998) Thus, it is important to understand the risk factors that may result in poorer adjustment..
This study was a secondary analysis of baseline data from an intervention study on coping skills training for school-age children with T1D and their parents (see Grey, Boland, Davidson, Li, & Tamborlane, 2000 for a description of the intervention). The purpose was to determine the relationships among maternal and child depressive symptoms and child and family psychosocial factors. Following Goodman and Gotlib’s (1999) model for the transmission of maternal depression, we hypothesized that family factors and child factors would mediate the relationship between maternal and child depressive symptoms as the result of exposure to mothers’ negative and/or maladaptive cognitions, behaviors, and affect, and exposure to a stressful environment. Specific research questions included: 1) Do child factors affected by exposure to maternal negative and/or maladaptive cognitions, behaviors and affect (i.e., difficulty and upset related to coping with diabetes, impact of diabetes on quality of life) mediate the relationship between maternal and child depressive symptoms? 2) Do family functioning factors related to a stressful family environment (i.e., conflict related to diabetes, responsibility for treatment, warmth/support, guidance/control, and family cohesion and adaptability) mediate the relationship between maternal and child depressive symptoms?
Method
Participants
Participants were 108 school-aged children with T1D and their mothers who completed baseline data collected as part of a randomized, controlled trial of a coping skills intervention. Children in this study ranged in age from 8 to 12 years old (M = 9.94; SD = 1.46), and slightly more than half the sample was female (60%). The mean duration of diabetes was 3.6 years (SD = 2.8), and 75% of children were on pump therapy. The average glycosylated hemoglobin (HbA1c) was 7.0 % (SD = 1.2), indicating that most of the children in the sample were meeting treatment goals (American Diabetes Association, 2007). Mothers ranged in age from 28 to 52 years (M = 39.8; SD = 5.5). The majority of the sample was Caucasian (81.7%), 12% was Hispanic and 6.3% was African American. Socioeconomic status as measured by income was generally high with 61% above $80,000, 29% between $40-79,999 and 10% less than $40,000.
Procedure
The primary study was an efficacy study of a coping skills intervention compared to group education with school-aged children with T1D and their parents. Participants were recruited through regular clinic appointments at a large pediatric diabetes clinic. Children were eligible if they were: (1) between the ages of 8 and 12 years; (2) diagnosed with T1D and treated with insulin for at least 6 months; (3) free of other health problems and; (4) in school grade appropriate to within 1 year of age. A total of 190 children were assessed for eligibility, of which 58% agreed to participate, 19% expressed interest but did not attend scheduled appointments, 20% declined participation for various reasons (e.g., too busy or too far), and 3% were not eligible. For the sake of clarity, only mothers were included in the current analyses (97% of the total sample of 111).
Children and mothers interested in participating in the study completed the consent/assent process approved by the Human Subjects Research Review Committee at a separate appointment. Upon consent (assent), mothers and children completed the questionnaire data. All data reported here were collected prior to randomization for the intervention. Families were compensated for their time ($10). Clinical data (e.g., hemoglobin A1c) was collected at the clinic visit closest to the completion of questionnaire data.
Measures
Self-report data were collected from children and mothers. Child measures included child depressive symptoms, child coping, child quality of life, and child’s perception of family functioning. Parent measures included maternal depressive symptoms and perception of family functioning.
Child Depressive Symptoms
The Children’s Depression Inventory (CDI, Kovacs, 1980) was developed as a self-report screening measure of depressive symptoms in school-aged children and adolescents, including disturbance in mood and hedonic capacity, self-evaluation, vegetative functions, and interpersonal behaviors. It contains 27 multiple choice items that yield total scores from 0 to 54. Higher scores reflect greater symptomatology. The CDI has been used extensively; concurrent and discriminant validity has been established with broad samples of children with known mental health problems and in studies of children and adolescents with T1D (Kovacs et al., 1990). Internal reliability for the present sample was α = .65. A score of 13 has been recommended as a criterion score for clinical depression when the CDI is not followed by a clinical evaluation (Smucker, Craighead, Craighead, & Green, 1986). In the current study, a score of 13 or higher and/or an indication of current suicidal thoughts (i.e., “I want to kill myself.”) required an immediate assessment for suicidal ideation by a licensed clinician (clinical psychologist or marriage and family therapist), who determined if the child needed a referral for treatment or if the child required hospitalization.
Child Coping
The Issues in Coping with IDDM - Child scale (ICC, Kovacs, Brent, Feinberg, Paulauskas, & Reid, 1986) was used as a self report measure of children and adolescents’ perceptions of 1) how hard or difficult to handle (14 items; total score 0-42, e.g., “testing my blood;”) and 2) how upsetting (12 items; total score 12-36, e.g., “being different from other kids”) issues are related to their T1D management. Higher scores indicate that children find it more difficult or upsetting to cope with diabetes. Internal reliability for the present sample was α = .66 for the How Hard scale and α = .58 for the How Upsetting scale.
Child Quality of Life
The Diabetes Quality of Life Scale for Youth (DQOLY, Ingersoll & Marrero, 1991), developed as a modification of the Diabetes Quality of Life Scale for adults (DCCT Research Group, 1996), was used to assess children’s and adolescents’ perceptions of the impact of intensive treatment regimens on their general satisfaction with life, and on diabetes-related concerns over social, school and peer relationships. There are three subscales: Diabetes Life Satisfaction scale (18 items; total score 18-72); Disease Impact Scale (21 items; total score 21-84) and Disease-related Worries scale (8 items; total score 8-32). Higher scores indicate greater negative impact and worry (poorer quality of life), but better life satisfaction. In the current analyses, only the Impact subscale was used due to the high correlation between subscales (r = .84 with Worries subscale, r = -.55 with Satisfaction subscale). Internal reliability for the present sample was α = .88 for the Impact scale.
Child perception of family functioning was measured with the Diabetes Family Behavior Scale (DFBS, McKelvey et al., 1993), a self-report measure of diabetes-specific family support behaviors thought to be important in helping or hindering a child or adolescent’s diabetes management. It consists of two subscales: guidance-control (15 items; total score 15-75) and warmth-caring (15 items; 15-75) as reported by the child. Higher scores indicate more support behaviors. Internal consistency for the present sample was α = .43 for the guidance/control scale and α = .70 for the warmth/caring scale.
Maternal Depressive Symptoms
The Center for Epidemiologic Depression Scale (CES-D) was used as a brief, self-report measure of depressive symptoms (Radloff, 1977). A total score is calculated from 20 items and ranges from 0-60. Higher scores indicate more depressive symptoms, and the authors recommend that a score of 16 serve as a criterion for which further evaluation is warranted. This measure is widely used with both clinical samples and community surveys. Internal consistency for the present sample was α = .88. A score of 16 or higher required an immediate assessment for suicidal ideation by a licensed clinician (clinical psychologist or marriage and family therapist) to determine if the mother needed a referral for treatment or if she required hospitalization.
Maternal perception of family functioning was measured with two instruments
The Diabetes Responsibility and Conflict Scale (DRCS, Rubin, Young-Hyman, & Peyrot, 1989) was completed by mothers to evaluate the distribution of diabetes-related responsibilities across parent and child (15 items; total score 15-75) and the degree of diabetes-related conflict encountered by parent and child (15 items; total score 15-75). Higher scores reflect greater parent responsibility and more parent-child conflict, respectively. Internal consistency for the present data was α = .80 for the responsibility scale and α = .88 for the conflict scale. The Family Adaptability and Cohesion Scale (FACES II, Olson et al., 1982) was completed by mothers to assess two aspects of family functioning: cohesion or emotional bonding within a family (16 items; total score 16-90) and adaptability or ability for the family to alter its role relationships and power structure in response to situational and developmental stress (14 items; total score 14-60). Higher scores indicate greater adaptability and cohesion in the family.
Metabolic control was assessed with hemoglobin A1c (HbA1c), a measure of the child’s average blood sugar over the past 3 months. Average HbA1c for populations without diabetes is <6%. The ADA recommendation for children ages 6-12 is <8% (American Diabetes Association, 2007).
Data Analyses
All data were double entered in a database and checked for accuracy. Analyses were performed using SPSS (v. 14.0, Chicago, IL) statistical packages. In keeping with Baron and Kenny’s (1986) statistical guidelines for assessing mediation, preliminary correlational analyses were conducted to test for multicollinearity among variables of interest. Subsequently, linear regression analyses were conducted to evaluate how child and family functioning factors influence the relationship between maternal and child depressive symptoms. According to Baron and Kenny (1986), three conditions must be met for a variable to be a potential mediator: (a) the independent variable (maternal depressive symptoms) must be associated with the mediator (e.g., child coping, impact on quality of life, family functioning); (b) the independent variable must be associated with the dependent variable (child depressive symptoms), and (c) the mediator must be associated with the dependent variable. Mediation is said to occur if the effect of the independent variable on the dependent variable is zero after controlling for the mediator. Any other decline is evidence of a partial mediation. A Sobel (1982) test was used to determine if these mechanisms of mediation were significant. Given that our data are cross-sectional, these analyses do not indicate a causal relationship between variables, and thus, the proposed mediational effects are considered exploratory.
Results
Descriptive Statistics
Table 1 presents the descriptive statistics for child and mother reports of current depressive symptoms, coping with diabetes, quality of life, and family functioning variables. In general, children reported only moderate impact of diabetes on quality of life, they found coping with diabetes somewhat difficult and upsetting, and they reported that that their families were supportive of their diabetes. Mothers reported that families were relatively high in cohesion and adaptability, and relatively low in conflict related to diabetes management. In terms of depression, 12.3% (n = 13) of the children in the sample met the cutoff score for symptoms of depression (CDI score ≥ 13) and 22.2% (n = 24) of the mothers met the cutoff score for symptoms of depression (CES-D score ≥ 16).
Table 1
Descriptive Statistics and Correlations among Maternal and Child Depressive Symptoms and Key Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
1. CES-D
 M = 11.10 (7.73) M = 11.10 (7.73) | -- | |||||||||||
2. CDI
 M = 6.26 (5.48) M = 6.26 (5.48) | .44*** | -- | ||||||||||
3. ICC Coping Upset
 M = 17.82 (3.36) M = 17.82 (3.36) | .22* | .46*** | -- | |||||||||
4. ICC Coping Hard
 M = 18.19 (4.09) M = 18.19 (4.09) | .04 | .31*** | .30** | -- | ||||||||
5. YQoL Impact
 M = 36.18 (8.96) M = 36.18 (8.96) | .31*** | .58*** | .43*** | .24* | -- | |||||||
6. FACES Adaptability
 M = 48.64 (5.79) M = 48.64 (5.79) | -.32*** | -.15 | -.11 | -.16 | -.22* | -- | ||||||
7. FACES Cohesion
 M = 66.84 (7.66) M = 66.84 (7.66) | -.33*** | -.20* | -.16 | -.02 | -.14 | .57*** | -- | |||||
8. DRC Conflict
 M = 26.91 (11.75) M = 26.91 (11.75) | .25** | .19 | .25** | .15 | .24* | -.27** | -.24* | -- | ||||
9. DRC Responsibility
 M = 49.32 (8.95) M = 49.32 (8.95) | .07 | .21* | .13 | .13 | .21* | -.04 | .05 | .25** | -- | |||
10. DFBS Warmth/Caring
 M = 59.05 (7.27) M = 59.05 (7.27) | -.21* | -.51*** | -.43*** | -.31*** | -.65*** | .26** | .22* | -.27** | -.13 | -- | ||
11. DFBS Guidance/Control
 M = 47.17 (6.45) M = 47.17 (6.45) | -.07 | .04 | .14 | .08 | -.01 | .01 | .08 | .11 | .62*** | .12 | -- | |
12. HbA1c
 M = 7.03 (1.19) M = 7.03 (1.19) | .10 | .07 | .19* | .13 | .25** | -.27** | -.25** | .28** | .08 | -.13 | .12 | -- |
Preliminary Analyses
Preliminary analyses were conducted to determine if there was a relationship between child gender or age and other key variables. There were no significant group differences on any of the key variables for boys and girls. Child age was related to three of the six family factor variables: older children reported less maternal guidance/control (r = -.49, p < .001), and mothers of older children reported less difficulty handling diabetes management (r = -.50, p < .001) and less family cohesion (r = -.20, p = .047).
Correlational Analyses
Bivariate correlations were conducted with child and maternal depressive symptoms and other key variables to determine which variables met the criteria as possible mediators. As shown in Table 1, there was a significant association between maternal and child depressive symptoms (r = .44, p < .001), in that higher levels of maternal depressive symptoms were related to higher levels of child depressive symptoms.
Further, higher levels of maternal depressive symptoms were related to children finding it more upsetting to cope with diabetes (r = .22), greater negative impact of diabetes on child’s quality of life (r = .31), higher levels of family conflict (r = .25), and lower levels of family adaptability (r = -.32), cohesion (r = -.33), and child’s perception of family warmth/caring (r = -.21, all p < .05). Similarly, higher levels of child depressive symptoms were related to children finding it more upsetting (r = .46) and more difficult (r = .31) to cope with diabetes, greater negative impact of diabetes on child’s quality of life (r = .58), greater difficulty handling responsibility (r = .21), and lower levels of family cohesion (r = -.20) and child’s perception of family warmth/caring (r = -.51, all p < .05). Neither maternal nor child depressive symptoms were significantly related to child’s perceptions of family guidance/control related to diabetes.
Although child’s metabolic control (HbA1c) was not significantly related to maternal or child depressive symptoms, poorer metabolic control was associated with children finding it more upsetting to cope with diabetes (r = .19), greater negative impact of diabetes on child’s quality of life (r = .25), lower levels of family adaptability (r = -.27) and cohesion (r = -.25), and higher levels of family conflict (r = .28, all p < .05).
Tests for Mediation
As per Baron and Kenny’s (1986) statistical guidelines, the following variables met the first three conditions as possible mediators (see above): how upsetting it was for the child to cope with diabetes, impact on quality of life, family cohesion, and child’s perception of family warmth/caring. Using linear regression analyses, each of these variables was tested for mediation.
As seen in Table 2, how upsetting it was to cope with diabetes partially mediated the relationship between maternal and child depressive symptoms, accounting for an additional 14% of the variance. When child’s upset related to coping was added to the model, the beta value for maternal depressive symptoms decreased from .44 to .35 (see Figure 1). In addition, the Sobel test for mediation (Sobel, 1982) was significant (z = 2.09, p = .04). Figure 2 illustrates that the impact of diabetes on child’s quality of life also partially mediated the relationship between maternal and child depressive symptoms, accounting for an additional 22% of the variance, with the beta value for maternal depression decreasing from .44 to .28; the Sobel test was also significant (z = 2.95, p = .003). Finally, Figure 3 illustrates that child’s perception of family warmth/caring partially mediated the relationship between maternal and child depressive symptoms, accounting for an additional 19% of the variance, with the beta value for maternal depression decreasing from .44 to .34; the Sobel test was also significant (z = 2.05, p = .04). Family cohesion was not a significant mediator of the relationship between maternal and child depressive symptoms.1
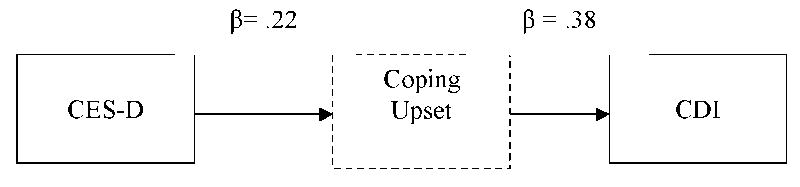
Child Perceptions of Coping as a Mediator of Maternal and Child Depressive Symptoms. Standardized coefficients are presented for each step in this pathway.
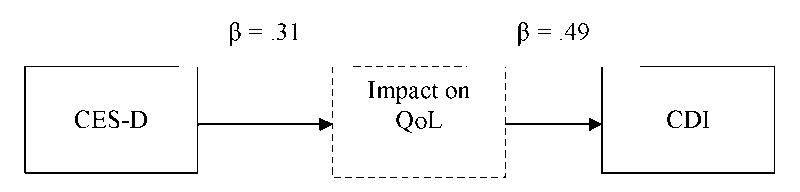
Impact of Diabetes on Quality of Life as a Mediator of Maternal and Child Depressive Symptoms. Standardized coefficients are presented for each step in this pathway.
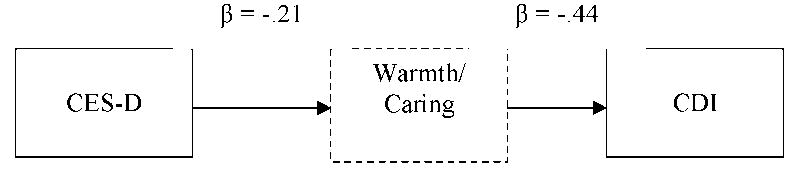
Family Warmth/Caring as a Mediator of Maternal and Child Depressive Symptoms. Standardized coefficients are presented for each step in this pathway.
Table 2
Multiple Regressions of Maternal Depressive Symptoms and Psychosocial Factors on Child Depressive Symptoms.
| Predictors | β | R2 | R2 change | F change |
|---|---|---|---|---|
| Step 1 | ||||
 CES-D CES-D | .44 | .19 | 24.35*** | |
| Step 2 | ||||
 Coping Upset Coping Upset | .38 | .32 | .14 | 21.39*** |
| Step 2 | ||||
 Impact on QoL Impact on QoL | .49 | .40 | .22 | 37.96*** |
| Step 2 | ||||
 Cohesion Cohesion | -.06 | .18 | .00 | .38 |
| Step 2 | ||||
 Warmth/Caring Warmth/Caring | -.44 | .36 | .19 | 30.84*** |
Note: β = standardized beta.
* <.05. ** < .01.
Discussion
The purpose of the current study was to examine the relationships among maternal and child depressive symptoms and child and family psychosocial factors in school-age children with T1D. Results indicate that there is a strong relationship between depressive symptoms in children with T1D and their mothers, similar to what has been reported by past research (Kovacs, Goldston et al., 1997). In addition, a substantial number of mothers and children (22.2% of mothers and 12.3% of children) in our sample reported clinically significant levels of depressive symptoms. As a point of comparison, the rates of major depressive disorder in the general population (based on diagnostic interviews) are estimated at 6.6% for adults (Kessler et al., 2003) and 2.2% for children (Costello, Mustillo, Erkanli, Keeler, & Angold, 2003). These findings highlight the importance of screening for depressive symptoms not only in children with T1D, but also in their mothers. Given that maternal distress is a major risk factor for depression in children with T1D (Kovacs, Goldston et al., 1997), additional attention to the psychosocial adjustment of mothers of children with T1D is warranted.
Findings from the current study also provide information regarding ways in which maternal depression may affect child psychosocial adjustment. Children’s perceptions that coping with diabetes was upsetting, impact of diabetes on child’s life, and child’s perception of family warmth/caring mediated the relationship between maternal and child depressive symptoms. Mothers with higher levels of depressive symptoms appear to contribute to increased depressive symptoms in children with T1D due to difficulty providing warm and caring support for children living with T1D, particularly support related to collaborating around diabetes treatment management. In the current study, children with T1D whose mothers reported higher depressive symptoms felt more upset in living with T1D and felt a greater impact of T1D on their lives, suggesting inadequate coping and a lower quality of life. Although there was no direct relationship between child’s metabolic control and maternal or child depressive symptoms in our sample, poorer metabolic control was linked to greater negative impact of diabetes on child’s quality of life, lower levels of family adaptability and cohesion, and higher levels of conflict related to diabetes management, all of which were also associated with maternal symptoms of depression. This suggests that the negative effects of maternal depression on children’s quality of life and family functioning may ultimately result in poorer metabolic control.
Previous research supports that depressed mothers expose children to maladaptive coping styles, are unable to meet children’s emotional needs, and provide inadequate parenting with respect to social and cognitive skills and styles (Goodman & Gotlib, 1999). In addition, depressed mothers have been shown to be less positive in their interactions with their children (Lovejoy, Graczyk, O’Hare, & Neuman, 2000). These deficits in parenting become particularly important for school-age children who developmentally have a great need for maternal social support and assistance in coping with life stressors (Lee & Gotlib, 1991). Research also indicates that children of depressed mothers are exposed to a greater number of stressors in their lives than children of non-depressed mothers (Adrian & Hammen, 1993). Thus, children with T1D face the chronic stress of disease management, which appears to be compounded by the additional stress of living with a mother who is depressed.
The transactional nature of maternal and child depression in T1D must also be recognized. In this study, higher levels of child depressive symptoms were related to higher levels of maternal perception of family conflict and difficulty handling responsibility, and lower levels of parent-reported family cohesion. Child depressive symptoms may contribute to increased maternal stress, impaired family functioning, and increased maternal depressive symptoms. However, none of these factors mediated the relationship between maternal and child depressive symptoms. It is possible that other factors, such as the genetic loading for depression, account for the lack of a significant mediating relationship. Given that the current data are cross-sectional, we are unable to draw conclusions about the directions of effects. It is possible that the relationship between variables is different from what we hypothesized (e.g., maternal depression could lead to child depression, which could impact child’s quality of life). Further longitudinal research is needed to improve our understanding of the impact of diabetes-specific child and family factors on the transactional relationship between maternal and child depression.
Interventions for children with T1D indicate that coping skills training (e.g., Grey, Boland, Davidson et al., 1998) and family-centered interventions (e.g. Wysocki, Greco, Harris, Bubb, & White, 2001) have demonstrated improvements in family communication and child physiological and psychosocial outcomes. However, little research has been undertaken on interventions that specifically address maternal and/or child depression in this population. Programs to prevent depression in children living with depressed parents in the general population have demonstrated short-term improvements in child depressive symptoms, behaviors, attitudes, and understanding (Beardslee, Gladstone, Wright, & Cooper, 2003). Despite these promising findings, however, the long-term effects of intervention programs to prevent depression in children are unknown (Merry, McDowell, Hetrick, Bir, & Muller, 2004).
Treatment or prevention of depression in children and adolescents with T1D and their mothers is even more challenging due to the additional psychosocial stressors of living with a complex and demanding chronic illness, as well as the need for parent-child collaboration in self-management. The ability of depressed mothers or depressed children with T1D to cope with daily self-management and social challenges may be compromised, and they are likely to have difficulty communicating in a warm and caring style to support ongoing adjustment. Research indicates that family involvement is important for management of T1D (Anderson et al., 2002), which may be negatively affected when a mother is depressed. Further research on mediators of child and maternal depression is indicated, and there is a need for interventions designed to prevent and treat depressive symptoms in children with T1D and their mothers.
Some limitations of the current study must be acknowledged. First, the cross-sectional nature of the study limits our ability to draw conclusions about the direction of effects. Further, the current sample was in good metabolic control and relatively wealthy, which may limit the generalizability of the findings. In addition, the time commitment required to participate in the treatment study may have biased the sample, as it may have been more difficult for lower income and lower functioning families to participate. Finally, the current study only included mothers, thereby limiting the conclusions that may be drawn regarding fathers of children with T1D, which may be important to consider (Phares, Lopez, Fields, Kamboukos, & Duhig, 2005).
Despite these limitations, the current findings suggest the need for family-based interventions to focus on preventing and treating maternal and child psychosocial distress in children with T1D. The goal of such interventions may be to recognize the burden that diabetes management places on mothers, to identify the risk for increased depressive symptoms in mothers and children, to identify effective coping strategies for mothers and children, and to support parenting that fosters child development and psychosocial adjustment. Such interventions could also focus on promoting self-care among mothers, including teaching relaxation techniques, and helping families to mobilize support networks. Results of this study suggest the need to screen for maternal psychosocial adjustment, particularly depressive symptoms, and to provide additional resources and support to mothers at risk, given that their distress may present a major risk factor for child psychosocial adjustment.
Acknowledgments
Funding for this study was provided by grant 1 R01 NR04009 from the National Institute of Nursing Research.
Footnotes
1To correct for skewness, log CDI and log CES-D were used in the regression analyses, with essentially the same results.
References
- Adrian C, Hammen C. Stress exposure and stress generation in children of depressed mothers. Journal of Consulting and Clinical Psychology. 1993;61:354–359. [Abstract] [Google Scholar]
- American Diabetes Association. Standards of medical care in diabetes - 2007. Diabetes Care. 2007;30:S4–S41. [Abstract] [Google Scholar]
- Anderson BJ, Vangsness L, Connell A, Butler D, Goebel-Fabbri A, Laffel LMB. Family conflict, adherence, and glycaemic control in youth with short duration Type 1 diabetes. Diabetic Medicine. 2002;19:635–642. [Abstract] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. [Abstract] [Google Scholar]
- Beardslee WR, Gladstone T, Wright EJ, Cooper AB. A family-based approach to the prevention of depressive symptoms in chidlren at risk: Evidence of parental and child change. Pediatrics. 2003;112:119–131. [Abstract] [Google Scholar]
- Beardslee WR, Versage EM, Gladstone T. Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1134–1141. [Abstract] [Google Scholar]
- Blanz BJ, Rensch-Riemann BS, Fritz-Sigmund DI, Schmidt MH. IDDM is a risk factor for adolescent psychiatric disorders. Diabetes Care. 1993;16:1579–1587. [Abstract] [Google Scholar]
- Chaney JM, Mullins LL, Frank RG, Peterson L, Mace LD, Kashani JH, et al. Transactional patterns of child, mother, and father adjustment in insulin-dependent diabetes mellitus: A prospective study. Journal of Pediatric Psychology. 1997;22:229–244. [Abstract] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. [Abstract] [Google Scholar]
- Cummings ME, Davies PT. Maternal depression and child development. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1994;35:73–112. [Abstract] [Google Scholar]
- DCCT Research Group. Effect of intensive insulin treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. Journal of Pediatrics. 1994;125:177–188. [Abstract] [Google Scholar]
- DCCT Research Group. Influence of intensive diabetes treatment on quality of life outcomes in the Diabetes Control and Complications Trial. Diabetes Care. 1996;19:195–203. [Abstract] [Google Scholar]
- Drotar D. Relating parent and family functioning to the psychological adjustment of children and with chronic health conditions: What have we learned? What do we need to know? Journal of Pediatric Psychology. 1997;22:149–165. [Abstract] [Google Scholar]
- Garrison MM, Katon WJ, Richardson LP. The impact of psychiatric comorbidities on readmissions for diabetes in youth. Diabetes Care. 2005;28:2150–2154. [Abstract] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychology Review. 1999;106:458–490. [Abstract] [Google Scholar]
- Grey M, Boland EA, Davidson M, Li J, Tamborlane WV. Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. Journal of Pediatrics. 2000;137:107–113. [Abstract] [Google Scholar]
- Grey M, Boland EA, Davidson M, Yu C, Sullivan-Bolyai S, Tambolane WV. Short-term effects of coping skills training as an adjunct to intensive therapy in adolescents. Diabetes Care. 1998;21:902–908. [Abstract] [Google Scholar]
- Grey M, Boland EA, Yu C, Sullivan-Bolyai S, Tamborlane WV. Personal and family factors associated with quality of life in adolescents with diabetes. Diabetes Care. 1998;21:909–914. [Abstract] [Google Scholar]
- Hammen C, Shih JH, Brennan PA. Intergenerational transmission of depression: Test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology. 2004;72:511–522. [Abstract] [Google Scholar]
- Hanson CL, De Guire MJ, Schinkel AM, Henggeler SW. Comparing social learning and family systems correlates of adaptation in youths with IDDM. Journal of Pediatric Psychology. 1992;17:555–572. [Abstract] [Google Scholar]
- Hassan K, Loar R, Anderson BJ, Heptulla RA. The role of socioeconomic status, depression, quality of life, and glycemic control in type 1 diabetes mellitus. The Journal of Pediatrics. 2006;149:526–531. [Abstract] [Google Scholar]
- Ingersoll GM, Marrero DG. A modified quality of life measure for youths: Psychometric properties. Diabetes Educator. 1991;17:114–118. [Abstract] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depression. JAMA. 2003;289:3095–3105. [Abstract] [Google Scholar]
- Kokkonen J, Taanila A, Kokkonen E-R. Diabetes in adolescence: The effect of family and psychologic factors on metabolic control. Nordic Journal of Psychiatry. 1997;51:165–172. [Google Scholar]
- Kovacs M. Rating scales used to assess depression in school-aged children. Acta Paediatrica. 1980;46:305–315. [Abstract] [Google Scholar]
- Kovacs M, Brent D, Feinberg TF, Paulauskas S, Reid J. Children’s self-reports of psychologic adjustment and coping strategies during the first year of insulin-dependent diabetes mellitus. Diabetes Care. 1986;9:472–479. [Abstract] [Google Scholar]
- Kovacs M, Goldston D, Obrosky DS, Bonar LK. Psychiatric disorders in youth with IDDM: Rates and risk factors. Diabetes Care. 1997;20:36–44. [Abstract] [Google Scholar]
- Kovacs M, Iyengar S, Goldston D, Stewart J, Obrosky DS, Marsh J. Psychological functioning of children with insulin-dependent diabetes mellitus: a longitudinal study. Journal of Pediatric Psychology. 1990;15:619–632. [Abstract] [Google Scholar]
- Kovacs M, Mukerji P, Drash A, Iyengar S. Biomedical and psychiatric risk factors for retinopathy. Diabetes Care. 1995;18:1592–1599. [Abstract] [Google Scholar]
- Kovacs M, Obrosky DS, Goldston D, Drash A. Major depressive disorder in youths with IDDM: A controlled prospective study of course and outcome. Diabetes Care. 1997;20:45–51. [Abstract] [Google Scholar]
- Lee CM, Gotlib IH. Family disruption, parental availability, and child adjustment: An integrative review. In: Prinz RJ, editor. Advances in the behavioral assessment of children and families. Vol. 5. London: Jessica Kingsley; 1991. pp. 166–199. [Google Scholar]
- Lewinsohn PM, Solomon A, Seeley JR, Zeiss A. Clinical implications of “subthreshold” depressive symptoms. Journal of Abnormal Psychology. 2000;109:345–351. [Abstract] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. [Abstract] [Google Scholar]
- McKelvey J, Waller DA, North AJ, Marks JF, Schreiner BJ, Travis LB, et al. Reliability and validity of the diabetes family behavior scale. Diabetes Educator. 1993;19:125–132. [Abstract] [Google Scholar]
- Merry S, McDowell H, Hetrick S, Bir J, Muller N. Psychological and/or educational interventions for the prevention of depression in children and adolescents. Chochrane Database of Systematic Reviews. 2004;2:1–10. [Abstract] [Google Scholar]
- Mullins LL, Fuemmeler BF, Hoff A, Chaney JM, Van Pelt J, Ewing CA. The relationship of parental overprotection and perceived child vulnerability to depressive symptomotology in children with type 1 diabetes mellitus: The moderating influence of parenting stress. Children’s Health Care. 2004;33:21–34. [Google Scholar]
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Diabetes in America. Bethesda, MD: NIH; 2002. publication No. 02-3892. [Abstract] [Google Scholar]
- Olson DH, McCubbin HI, Barnes H, Larsen A, Muzen M, Wilson M. Family adaptability and cohesion evaluation scales. In: Olson DH, McCubbin HI, Barnes H, Larsen A, Muzen M, Wilson M, editors. Family inventories: Inventories used in a national survey of families across the life cycle. St. Paul, MN: Family Social Science; 1982. pp. 5–24. [Google Scholar]
- Phares V, Lopez E, Fields S, Kamboukos D, Duhig AM. Are fathers involved in pediatric psychology research and treatment? Journal of Pediatric Psychology. 2005;30:631–643. [Abstract] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rubin RR, Young-Hyman D, Peyrot M. Parent-child responsibility and conflict in diabetes care. Diabetes. 1989;38(Supplement 2):28A. [Google Scholar]
- Sayfer AW, Hauser ST, Jacobson AM, Bliss R, Herskowitz RD, Wolfsdorf JI, et al. The impact of the family on diabetes adjustment: A developmental perspective. Child and Adolescent Social Work Journal. 1993;10:123–140. [Google Scholar]
- Silverstein JH, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel LMB, et al. Care of children and adolescents with type 1 diabetes. Diabetes Care. 2005;28:184–212. [Abstract] [Google Scholar]
- Smucker MR, Craighead WE, Craighead LW, Green BJ. Normative and reliability data for the Children’s Depression Inventory. Journal of Abnormal Child Psychology. 1986;14:25–39. [Abstract] [Google Scholar]
- Sobel ME. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological Methodology. San Francisco: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- Stewart SM, Rao U, Emslie GJ, Klein D, White PC. Depressive symptoms predict hospitalization for adolescents with type 1 diabetes mellitus. Pediatrics. 2005;115:1315–1319. [Abstract] [Google Scholar]
- Whittemore R, Kanner S, Singleton S, Hamrin V, Chiu J, Grey M. Correlates of depressive symptoms in adolescents with type 1 diabetes. Pediatric Diabetes. 2002;3:135–143. [Abstract] [Google Scholar]
- Whittemore R, Urban AD, Tamborlane WV, Grey M. Quality of life in school-age children with type 1 diabetes on intensive treatment and their parents. The Diabetes Educator. 2003;29:847–854. [Abstract] [Google Scholar]
- Wysocki T, Greco P, Harris MA, Bubb J, White NH. Behavior therapy for families of adolescents with diabetes: Maintenance of treatment effects. Diabetes Care. 2001;24:441–446. [Abstract] [Google Scholar]
Full text links
Read article at publisher's site: https://doi.org/10.1093/jpepsy/jsm104
Read article for free, from open access legal sources, via Unpaywall:
http://jpepsy.oxfordjournals.org/content/early/2007/11/08/jpepsy.jsm104.full.pdf
Citations & impact
Impact metrics
Citations of article over time
Article citations
Psychological variables and lifestyle in children with type1 diabetes and their parents: A systematic review.
Clin Child Psychol Psychiatry, 29(3):1174-1194, 30 May 2023
Cited by: 3 articles | PMID: 37249210 | PMCID: PMC11188552
Review Free full text in Europe PMC
The prevalence of depression among parents of children/adolescents with type 1 diabetes: A systematic review and meta-analysis.
Front Endocrinol (Lausanne), 14:1095729, 01 Mar 2023
Cited by: 7 articles | PMID: 36936139 | PMCID: PMC10014558
Review Free full text in Europe PMC
Prevalence of Depression in Patients with Type 1 Diabetes between 10 and 17 Years of Age in Jordan.
J Diabetes Res, 2023:3542780, 22 Feb 2023
Cited by: 2 articles | PMID: 36873812 | PMCID: PMC9977551
Evaluation of quality of life and depression in family caregivers of patients with type 1 diabetes in Iran: A case-control study.
SAGE Open Med, 11:20503121221146055, 10 Jan 2023
Cited by: 0 articles | PMID: 36643205 | PMCID: PMC9834789
Parental marital relationship satisfaction is associated with glycemic outcomes in children with type 1 diabetes.
J Diabetes Metab Disord, 21(2):1479-1489, 29 Jul 2022
Cited by: 1 article | PMID: 36404837 | PMCID: PMC9672269
Go to all (59) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Coping and psychological distress in mothers of adolescents with type 1 diabetes.
Matern Child Health J, 18(1):101-108, 01 Jan 2014
Cited by: 32 articles | PMID: 23420308 | PMCID: PMC3746006
A pilot study of observed parenting and adjustment in adolescents with type 1 diabetes and their mothers.
J Pediatr Psychol, 35(7):738-747, 04 Nov 2009
Cited by: 55 articles | PMID: 19889719 | PMCID: PMC2915622
Family functioning and maternal distress in adolescent girls with anorexia nervosa.
Int J Eat Disord, 42(6):531-539, 01 Sep 2009
Cited by: 22 articles | PMID: 19189407
Maternal depression and developmental disability: research critique.
Ment Retard Dev Disabil Res Rev, 13(4):321-329, 01 Jan 2007
Cited by: 67 articles | PMID: 17979207
Review
Funding
Funders who supported this work.
NINR NIH HHS (8)
Grant ID: 1 R01 NR04009
Grant ID: R01 NR004009-08
Grant ID: R01 NR004009
Grant ID: R01 NR004009-06
Grant ID: R01 NR004009-07
Grant ID: R01 NR004009-11
Grant ID: R01 NR004009-09
Grant ID: R01 NR004009-10




