Abstract
Free full text

Brain and Spinal CordProtection duringAortic Surgery
Concurrent aneurysms of the aortic arch and the thoracic aorta (TA) or the thoracoabdominal aorta (TAA) are most often caused by degenerative processes and connective-tissue diseases. In addition, dissected aortas can dilate over time and develop combined aneurysms of the arch and TA/TAA. Finally, failed endovascular repair of the arch or descending aorta creates another group of patients who need combined arch and TA/TAA reconstruction—that is, conversion to open repair.
The traditional surgical treatment of these complex aortic aneurysms consists of a 2-stage approach using the elephant trunk technique,1,2 in which the first stage is performed via sternotomy and the second stage via left thoracotomy or thoracolaparotomy. Recently, the second step has often been completed by endovascular extension of the elephant trunk. However, not all patients can profit from this less invasive technique, due to anatomic restrictions. In addition, for the sake of long-term outcome, patients with connective-tissue disease are probably better treated with open repair.
Single-Step Repair of Complex Aortic Aneurysms. All of this means that a substantial group of patients with combined disease of the aortic arch and thoracic aorta must undergo open surgery. In recounting our experience, we have described our technique of single-step aortic arch and TA/TAA repair via a left thoracotomy (arch + TA) or thoracolaparotomy (arch + TAA).3 This procedure is possible only if the ascending aorta is not diseased or has not been replaced by a tube graft.
Extracorporeal Circulation. The technique of extracorporeal circulation depends on the extent of the disease. If arch involvement is restricted to the distal segment of the arch and if cross-clamping at the level of the brachiocephalic or left carotid artery is feasible, left-heart bypass is achieved with the installation of a left atrial-to-left femoral artery circuit using a Bio-Medicus pump (Medtronic Bio-Medicus Inc; Eden Prairie, Minn). In the event of entire arch replacement and open proximal anastomosis, total extracorporeal circulation is achieved by means of cannulating the left femoral artery and the left femoral vein for the right atrium, and arresting the heart. Cardioplegic solution is infused via a large (24F) Foley catheter, which is inflated in the ascending aorta or tube graft.
Distal Aortic and Antegrade Brain Perfusion. Before the aortic arch is opened, a cross-clamp is positioned on the descending aorta, thereby enabling perfusion of the distal body and spinal cord via the left femoral artery (Fig. 1). After aortotomy and the infusion of cardioplegic solution, the brachiocephalic and left carotid arteries are cannulated with 13F to 15F catheters, providing antegrade brain perfusion with a volume flow of 10 mL/kg/min and a mean pressure of approximately 60 mmHg. The aortic reconstruction is performed with the patient under moderate hypothermia (28–30 °C).
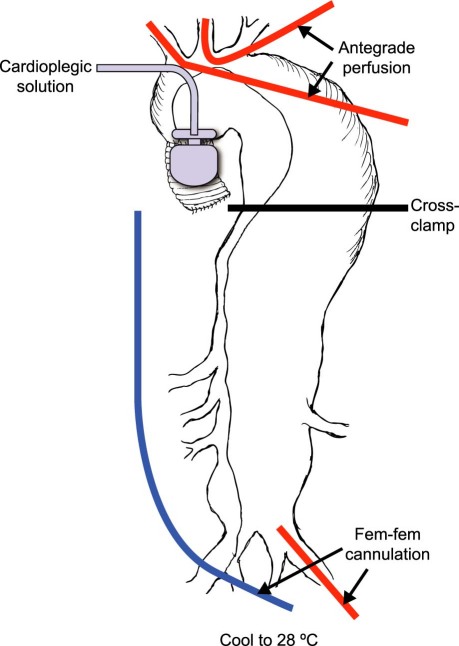
Fig. 1 Schematic drawing of extracorporeal circulation during repair of the aortic arch and thoracoabdominal aorta via a left-sided thoracolaparotomy. In the left groin, the femoral artery and vein are cannulated and a long venous cannula is positioned at the level of the right atrium. The patient is cooled to 28 °C, after which a cross-clamp is positioned at the mid descending thoracic aorta. The arch aneurysm is opened, and a large Foley catheter is inserted into the ascending aorta or into a previously implanted ascending tube graft, enabling the infusion of cardioplegic solution via a Bio-Medicus pump. Subsequently, the brachiocephalic and left carotid arteries are cannulated with selective perfusion catheters to enable antegrade brain perfusion. Fem-fem = femoral artery and femoral vein
Brain and Spinal Cord Protection. Neuromonitoring of the brain and spinal cord is performed by means of transcranial Doppler ultrasonography, electroencephalography, and monitoring of motor-evoked potentials. The distal aortic pressure is normally kept at a mean value of 60 mmHg; however, if amplitudes of the evoked potentials diminish, we increase the distal arterial pressure. This correction is especially necessary in patients with severe arterial hypertension, who need higher pressures for adequate spinal cord perfusion.
Results. During a 7-year period, we treated 40 patients with TA or TAA and concomitant aortic arch aneurysm, which represented approximately 15% of our overall TA/TAA procedures. There were no intraoperative deaths and the 30-day mortality rate was 7.5%. We encountered no early paraplegia, and 1 patient (2.5%) experienced a temporary, delayed neurologic deficit. One patient had a cerebral infarction, whereas another had postoperative cerebral edema, from which that patient recovered completely.
From a technical standpoint, we found simultaneous arch and TA/TAA repair to be feasible in all patients. In order to achieve adequate access to the proximal arch and supra-aortic vessels, we preferred to approach via a high (4th-intercostal-space) thoracotomy.
Summary. In our experience, single-stage open repair of descending thoracic or thoracoabdominal aortic aneurysms with concurrent aortic arch disease is technically feasible via a high left thoracotomy or a thoracolaparotomy. Distal aortic and antegrade brain perfusion, in combination with brain and spinal cord protection, seems to contribute to adequate surgical and neurological outcome.
Footnotes
Address for reprints: Michael J. Jacobs, MD, PhD, Maastricht University Medical Center, P. Debyelaan 25, Maastricht 6202 AZ, The Netherlands
E-mail: [email protected]
Presented at the Joint Session of the Denton A. Cooley Cardiovascular Surgical Society and the Michael E. DeBakey International Surgical Society; Austin, Texas, 10–13 June 2010
References
Articles from The Texas Heart Institute Journal are provided here courtesy of Texas Heart Institute
Citations & impact
Impact metrics
Article citations
Best strategy for cerebral protection in arch surgery - antegrade selective cerebral perfusion and adequate hypothermia.
Ann Cardiothorac Surg, 2(3):331-338, 01 May 2013
Cited by: 15 articles | PMID: 23977602 | PMCID: PMC3741862
Review Free full text in Europe PMC
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Brain and spinal cord protection during simultaneous aortic arch and thoracoabdominal aneurysm repair.
J Vasc Surg, 49(4):886-892, 01 Apr 2009
Cited by: 11 articles | PMID: 19341883
Regarding "Brain and spinal cord protection during simultaneous aortic arch and thoracoabdominal aneurysm repair".
J Vasc Surg, 50(3):705-6; author reply 706, 01 Sep 2009
Cited by: 0 articles | PMID: 19700105
Hypothermia for aortic surgery.
J Thorac Cardiovasc Surg, 145(3 suppl):S56-8, 01 Mar 2013
Cited by: 32 articles | PMID: 23410782
Review


