Abstract
Context
Survival estimates help individualize goals of care for geriatric patients, but life tables fail to account for the great variability in survival. Physical performance measures, such as gait speed, might help account for variability, allowing clinicians to make more individualized estimates.Objective
To evaluate the relationship between gait speed and survival.Design, setting, and participants
Pooled analysis of 9 cohort studies (collected between 1986 and 2000), using individual data from 34,485 community-dwelling older adults aged 65 years or older with baseline gait speed data, followed up for 6 to 21 years. Participants were a mean (SD) age of 73.5 (5.9) years; 59.6%, women; and 79.8%, white; and had a mean (SD) gait speed of 0.92 (0.27) m/s.Main outcome measures
Survival rates and life expectancy.Results
There were 17,528 deaths; the overall 5-year survival rate was 84.8% (confidence interval [CI], 79.6%-88.8%) and 10-year survival rate was 59.7% (95% CI, 46.5%-70.6%). Gait speed was associated with survival in all studies (pooled hazard ratio per 0.1 m/s, 0.88; 95% CI, 0.87-0.90; P < .001). Survival increased across the full range of gait speeds, with significant increments per 0.1 m/s. At age 75, predicted 10-year survival across the range of gait speeds ranged from 19% to 87% in men and from 35% to 91% in women. Predicted survival based on age, sex, and gait speed was as accurate as predicted based on age, sex, use of mobility aids, and self-reported function or as age, sex, chronic conditions, smoking history, blood pressure, body mass index, and hospitalization.Conclusion
In this pooled analysis of individual data from 9 selected cohorts, gait speed was associated with survival in older adults.Free full text

Gait Speed and Survival in Older Adults
Abstract
Context
Survival estimates help individualize goals of care for geriatric patients, but life tables fail to account for the great variability in survival. Physical performance measures, such as gait speed, might help account for variability, allowing clinicians to make more individualized estimates.
Objective
To evaluate the relationship between gait speed and survival.
Design, Setting, and Participants
Pooled analysis of 9 cohort studies (collected between 1986 and 2000), using individual data from 34 485 community-dwelling older adults aged 65 years or older with baseline gait speed data, followed up for 6 to 21 years. Participants were a mean (SD) age of 73.5 (5.9) years; 59.6%, women; and 79.8%, white; and had a mean (SD) gait speed of 0.92 (0.27) m/s.
Main Outcome Measures
Survival rates and life expectancy.
Results
There were 17 528 deaths; the overall 5-year survival rate was 84.8% (confidence interval [CI], 79.6%–88.8%)and 10-year survival rate was 59.7% (95%CI, 46.5%–70.6%). Gait speed was associated with survival in all studies (pooled hazard ratio per 0.1 m/s, 0.88; 95% CI, 0.87–0.90; P<. 001). Survival increased across the full range of gait speeds, with significant increments per 0.1 m/s. At age 75, predicted 10-year survival across the range of gait speeds ranged from 19% to 87% in men and from 35% to 91% in women. Predicted survival based on age, sex, and gait speed was as accurate as predicted based on age, sex, use of mobility aids, and self-reported function or as age, sex, chronic conditions, smoking history, blood pressure, body mass index, and hospitalization.
Conclusion
In this pooled analysis of individual data from 9 selected cohorts, gait speed was associated with survival in older adults.
Remaining years of life vary widely in older adults, and physicians should consider life expectancy when assessing goals of care and treatment plans.1 However, life expectancy based on age and sex alone provides limited information because survival is also influenced by health and functional abilities.2 There are currently no well-established approaches to predicting life expectancy that incorporate health and function, although several models have been developed from individual data sources.3–5 Gait speed, also often termed walking speed, has been shown to be associated with survival among older adults in individual epidemiological cohort studies 6–12 and has been shown to reflect health and functional status.13 Gait speed has been recommended as a potentially useful clinical indicator of well-being among the older adults.14 The purpose of this study is to evaluate the association of gait speed with survival in older adults and to determine the degree to which gait speed explains variability in survival after accounting for age and sex.
METHODS
Overview
We used individual participant data from 9 cohort studies, baseline data for which were collected between 1986 and 2000 (Table 1).8,15,16,18–23 Each study, which included more than 400 older adults with gait speed data at baseline, monitored survival for at least 5 years. Analyses performed herein were conducted in 2009 and 2010. All studies required written informed consent and institutional review board approval.
Table 1
Characteristics of Participants in the 9 Cohort Studies
| Study | No. (%) of Participants by Study | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| CHS8 | EPESE15 | Health, ABC16,17 | Hispanic EPESE8 | Invecciare in Chianti18 | Osteoporotic Fractures in Men19 | NHANES III20 | PEP21 | Study of Osteoporotic Fractures22 | |
| Sample size, No. | 5801 | 2128 | 3048 | 1905 | 972 | 5833 | 3958 | 491 | 10 349 |
| Women | 3336 (57.51) | 1404 (65.98) | 1575 (51.67) | 1098 (57.64) | 541 (55.66) | 0 | 2044 (51.64) | 216 (43.99) | 10 349 (100) |
| Race/ethnicity | |||||||||
 White White | 4854 (83.68) | 2126 (99.91) | 1783 (58.50) | 0 | 972 (100) | 5223 (89.54) | 2535 (64.05) | 394 (80.24) | 9662 (93.36) |
 Black Black | 909 (15.67) | 2 (0.09) | 1265 (41.50) | 0 | 0 | 235 (4.03) | 699 (17.66) | 89 (18.13) | 654 (6.32) |
 Hispanic Hispanic | 0 | 0 | 0 | 1905 (100) | 0 | 122 (2.09) | 623 (15.74) | 0 | 0 |
 Other Other | 38 (0.66) | 0 | 0 | 0 | 0 | 253 (4.34) | 101 (2.55) | 8 (1.63) | 33 (0.32) |
| Age mean (SD), y | 72.81 (5.58) | 78.85 (5.52) | 73.62 (2.87) | 74.74 (5.96) | 74.58 (7.08) | 73.61 (5.84) | 75.17 (6.93) | 74.08 (5.74) | 71.81 (5.21) |
| Age group, y | |||||||||
 65–74 65–74 | 3852 (66.40) | 559 (26.27) | 1912 (62.73) | 1083 (56.85) | 555 (57.10) | 3401 (58.31) | 2033 (51.36) | 279 (56.82) | 7486 (72.34) |
 75–84 75–84 | 1732 (29.86) | 1204 (56.58) | 1136 (37.27) | 668 (35.07) | 302 (31.07) | 2183 (37.42) | 1484 (37.49) | 188 (38.39) | 2596 (25.08) |
 ≥85 ≥85 | 217 (3.74) | 365 (17.15) | 0 | 154 (8.08) | 115 (11.83) | 249 (4.27) | 441 (11.14) | 24 (4.89) | 200 (1.93) |
 Missing Missing | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 67 (0.65) |
| Gait speed, mean (SD), m/s | 0.86 (0.22) | 0.83 (0.13) | 1.12 (0.23) | 0.56 (0.23) | 1.00 (0.28) | 1.19 (0.23) | 0.68 (0.23) | 0.88 (0.24) | 0.95 (0.22) |
| Gait speed class, m/s | |||||||||
 <0.4 <0.4 | 149 (2.57) | 0 | 4 (0.13) | 515 (27.03) | 35 (3.60) | 11 (0.19) | 480 (12.13) | 20 (4.07) | 33 (1.19) |
 ≥0.4 to <0.6 ≥0.4 to <0.6 | 526 (9.07) | 78 (3.67) | 20 (0.66) | 621 (32.60) | 59 (6.07) | 54 (0.93) | 897 (22.66) | 40 (8.15) | 466 (4.50) |
 ≥0.6 to <0.8 ≥0.6 to <0.8 | 1887 (32.53) | 791 (37.17) | 189 (6.20) | 467 (24.51) | 110 (11.32) | 206 (3.53) | 1368 (34.56) | 110 (22.40) | 1752 (16.93) |
 ≥0.8 to <1.0 ≥0.8 to <1.0 | 2076 (35.79) | 1105 (51.93) | 705 (23.13) | 220 (11.55) | 246 (25.31) | 875 (15.00) | 887 (22.41) | 166 (33.81) | 3768 (36.41) |
 ≥1.0 to <1.2 ≥1.0 to <1.2 | 1077 (18.57) | 135 (6.34) | 1093 (35.86) | 77 (4.04) | 305 (31.38) | 1774 (30.41) | 294 (7.43) | 116 (22.63) | 3054 (29.51) |
 ≥1.2 to <1.4 ≥1.2 to <1.4 | 0 | 17 (0.80) | 684 (22.44) | 4 (0.21) | 170 (17.49) | 1911 (32.76) | 32 (0.81) | 36 (7.33) | 970 (9.37) |
 ≥1.4 ≥1.4 | 86 (1.48) | 2 (0.09) | 353 (11.58) | 1 (0.05) | 47 (4.84) | 1002 (17.18) | 0 | 3 (0.61) | 217 (2.10) |
| Mobility aid use | |||||||||
 None None | NA | 1962 (92.20) | 3048 (100) | 1817 (95.38) | 881 (90.64) | 5792 (99.30) | 3664 (92.57) | 463 (94.11) | 10 165 (98.22) |
 Cane Cane | NA | 87 (4.09) | 0 | 49 (2.57) | 8 (0.82) | 38 (0.65) | 201 (5.08) | 21 (4.27) | All aids |
 Walker Walker | NA | 67 (3.15) | 0 | 23 (1.21) | 3 (0.31) | 0 | 74 (1.87) | 5 (1.01) | Combined |
 Other/missing Other/missing | NA | 12 (0.56) | 0 | 16 (0.84) | 80 (8.23) | 3 (0.05) | 19 (0.48) | 3 (0.61) | 184 (1.78) |
| BMI, mean (SD) | 26.68 (4.71) | 26.63 (4.64) | 27.40 (4.82) | 27.91 (5.13) | 27.51 (4.11) | 27.39 (3.83) | 26.66 (5.11) | 27.53 (5.12) | 26.61 (4.57) |
| BMI category | |||||||||
 <25 <25 | 2237 (38.65) | 803 (38.24) | 983 (32.25) | 555 (29.13) | 276 (28.40) | 1593 (27.31) | 1544 (39.01) | 156 (31.77) | 4352 (42.05) |
 25–30 25–30 | 2407 (41.49) | 886 (42.64) | 1288 (42.26) | 758 (39.79) | 437 (46.96) | 2991 (51.28) | 1559 (39.39) | 211 (42.97) | 3842 (37.12) |
 >30 >30 | 1144 (19.72) | 411 (19.31) | 777 (25.49) | 577 (30.29) | 243 (25.00) | 1247 (21.38) | 852 (21.53) | 123 (25.05) | 2155 (20.82) |
 Missing Missing | 13 (0.22) | 28 (1.32) | 0 | 15 (0.79) | 16 (1.65) | 2 (0.03) | 3 (0.08) | 1 (0.20) | 0 |
| Hospitalized past year | NA | 395 (18.57) | 456 (14.98) | 304 (15.96) | 129 (13.27) | NA | 775 (19.58) | 97 (19.76) | 1116 (11.51) |
| Diseases | |||||||||
 Cancer Cancer | 830 (14.33) | 486 (22.84) | 575 (18.91) | 115 (6.04) | 95 (9.77) | 1697 (29.09) | 387 (9.78) | 113 (23.01) | NA |
 Arthritis Arthritis | 2977 (51.94) | 2055 (96.57) | 1706 (56.72) | 812 (42.62) | 304 (31.31) | 2764 (47.39) | 1827 (46.16) | 286 (58.25) | 6003 (63.10) |
 Diabetes Diabetes | 690 (11.90) | 335 (15.74) | 453 (14.88) | 455 (23.88) | 106 (10.91) | 624 (10.70) | 607 (15.34) | 84 (17.11) | 681 (7.04) |
 Heart disease Heart disease | 1230 (21.20) | 312 (14.66) | 652 (22.03) | 155 (8.14) | 49 (5.05) | 1379 (23.64) | 484 (12.23) | 89 (18.13) | NA |
| Self-reported health excellent/very good | 2177 (37.61) | 542 (74.48) | 1343 (44.12) | 870 (45.67) | 591 (62.61) | 5012 (85.95) | 1204 (30.47) | 229 (46.64) | 8537 (82.49) |
| Total deaths during follow-up | 3851 (66.39) | 1955 (91.87) | 848 (27.82) | 972 (51.02) | 187 (19.24) | 1073 (18.40) | 2837 (71.68) | 293 (59.55) | 5512 (53.26) |
| Median survival years (95% CI) | 13.25 (13.00–13.56) | 9.57 (9.17–9.92) | NE | 11.70 (11.11-NE) | NE | NE | 9.86 (9.53–10.19) | 11.15 (9.82–11.92) | 17.23 (16.97–17.47) |
| Follow-up period, median (range), y | 13.25 (0.01–18.06) | 9.57 (0.10–20.65) | 9.00 (0.02–9.00) | 11.54 (0.07–12.29) | 6.00 (0.18–6.00) | 6.84 (0.04–8.26) | 9.86 (0.08–17.75) | 11.15 (0.12–13.76) | 15.03 (0.02–21.00) |
| Length of walk | 15 feet | 8 feet | 6 m | 8 feet | 4 m | 6 m | 4 m | 4 m | 6 m |
| Year of baseline data collection | 1989–90, 1992–93 | 1987–1989 | 1997–1998 | 1995–1996 | 1998–2000 | 2000–2002 | 1988–1994 | 1996 | 1986–1988, 1997 |
| Year of most recent mortality follow-up | 2007 | 2008 | 2007 | 2007 | 2006 | 2008 | 2006 | 2010 | 2008 |
Abbreviations: ABC, Aging and Body Composition; BMI, body mass index, calculated as weight in kilograms divided by height in meters squared; CHS, Cardiovascular Health Study; CI, confidence interval; EPESE, Established Populations for the Epidemiological Study of the Elderly; NA, not applicable; NE, not estimable due to insufficiently long follow-up and resulting in low mortality rate less than or close to 50%; NHANES III, Third National Health and Nutrition Examination Survey; PEP, Predicting Elderly Performance.
Populations
All studies recruited community-dwelling older adults. Although some sought representative samples,8,15,20,23 others focused on healthier participants,16,17 single sex,19,22 or older adults from primary care practices.21 Only participants 65 years and older with baseline gait speed data were included in this study. Individual study goals, recruitment methods, and target populations have been published.8,15–23
Measures
Gait speed was calculated for each participant using distance in meters and time in seconds. All studies used instructions to walk at usual pace and from a standing start. The walk distance varied from 8 ft to 6 m. For 8 ft, we converted to 4-m gait speed by formula.24 For 6 m, we created a conversion formula (4-m speed=−0.0341 + (6-mspeed)×0.9816 withR2=0.93, based on a cohort of 61 individuals with concurrent 4- and 6-m walks). For 15 feet (4.57 m),23 speed was simply meters divided by time. Where available, data on fast gait speed (walk as fast as comfortably able25) and the Short Physical Performance Battery were obtained.26 Survival for each individual used study monitoring methods, including the National Death Index and individual study follow-up. Time from gait speed baseline to death was calculated in days. Five-year survival status was confirmed for more than 99% of participants.
Additional variables include sex, age, race/ethnicity (white, black, Hispanic, other, defined by participant), height(centimeters), weight(kilograms), body mass index (BMI), calculated as weight in kilograms divided by height in meters squared (<25, 25–30, and >30), smoking (never, past, current), use of mobility aids (none, cane, walker), systolic blood pressure, self-reports of health (excellent or very good vs good, fair, or poor), hospitalization in the past year (yes/no), and physician-diagnosed medical conditions (cancer, arthritis, diabetes, and heart disease, all yes/no). Measures of self-reported functional status were not collected in all studies and varied in content and form. We created a dichotomous variable reflecting dependence in basic activities of daily living (ADLs) based on report of being unable or needing help from another person to perform any basic activity, including eating, toileting, hygiene, transfer, bathing, and dressing. For individuals independent in ADLs, we created a dichotomous variable reflecting difficulty in instrumental ADLs based on report of difficulty or dependence with shopping, meal preparation, or heavy housework due to a health or physical problem. Participants were then classified into 1 of 3 groups; dependent in ADLs, difficulty with instrumental ADLs, or independent. Physical activity data were collected in 6 studies, but time frames and items varied widely. Two studies used the Physical Activity Scale for the Elderly (PASE).27 We dichotomized the PASEs core at 100.28 We created operational definitions of other covariates that were reasonably consistent across studies. Covariates were identical for height, weight, BMI, and systolic blood pressure. Hospitalization within the prior year was determined largely by self-report, and chronic conditions were by self-report of physician diagnosis, with heart disease encompassing angina, coronary artery disease, heart attack, and heart failure.
Statistical Analysis
Descriptive statistics summarized participant characteristics, follow-up period, and median survival from baseline. A study-wide a priori P value of .002 provides a conservative Bonferroni correction accounting for atleast 25 individual statistical comparisons. Kaplan-Meier product-limit survival curves graphically summarize lifetimes for each gait speed category.29 For graphical purposes, gait speed was categorized into 0.2-m/s increments with lower and upper extremes being grouped as less than 0.4 m/s and higher than 1.4 m/s.
Cox proportional hazards regression models were used to assess associations between gait speed and survival, adjusting for age at baseline, for which hazard ratios (HRs) correspond to a 0.1-m/s difference in gait speed. The analyses were repeated adjusting for height, sex, race, BMI, smoking history systolic blood pressure, diseases, prior hospitalization, and self-reported heath. Proportionality of hazards was verified by examining Schoenfeld residual plots.30 Appropriateness of using gait speed as a continuous predictor was confirmed by observing linearity in Cox models with ordered 0.2-m/s gait speed categories. To examine the influence of early deaths, we repeated analyses excluding deaths within 1 year of gait speed measurement and moved up the 0 time for survival assessment (results were similar; eTable 1 available at http://www.jama.com). Subgroup analyses were repeated in strata by age (65–74, 75–84, or ≥85 years), sex, race, self-reported health status, smoking history, BMI, functional status, use of mobility aids, and hospitalization and by report of cancer, arthritis, diabetes, and heart disease.29 Results were pooled across sex because no substantial sex differences existed in HRs within subgroup strata.
To obtain simple and clinically usable estimates of survival probability based on sex, age, and gait speed, we fit logistic regression models separately for each sex with dichotomized 5- and 10-year survival as the response variable and age, gait speed, and their interaction as continuous predictors. To obtain estimates of median survival (further life expectancy), we fit Weibull accelerated failure–time models separately for each with time to death as the response variable, and age, gait speed, and their interaction as continuous predictors. To compare ability to predict survival among candidate variables and to determine whether gait speed improves predictive accuracy beyond other clinical measures, we fit logistic regression models with dichotomized 5-year or 10-year survival as the response variable and various combinations of predictors as independent variables with both linear and squared terms for BMI. The area under the receiver operating characteristic (ROC) curve or C statistic was used as a measure predictive of accuracy for mortality. All study-specific statistical analyses were performed using SAS version 9.2 (SAS Institute Inc, Cary, North Carolina).
Age-adjusted HRs were pooled from all studies using standard meta-analytic statistical methodology. Heterogeneity of HRs across studies was assessed using the Q and I2 statistics.31,32 We used a random-effects model to appropriately pool the HRs on the log scale while incorporating any heterogeneity among study estimates and then transform back to obtain an overall HR, along with a 95% confidence interval(CI)and P value.33 Sensitivity of the results was assessed by fitting a shared frailty34 (unrelated to the geriatric syndrome frailty) model to individual participant data with a γ-distributed frailty parameter to account for study effect (results similar; not shown).34,35 Five-and 10-year pointwise survival rates from the Kaplan-Meier curves for each sex, age-group, and gait speed category combination were pooled across studies using a random-effects model on the complementary log-log scale36 and then appropriately inverted to obtain overall estimates of survival, as presented in the tables. We further used the standard random effects meta-analytic model to combine sex-specific regression coefficients for age, gait speed, and their interaction from logistic regression models for 5- and 10-year survival and used the overall estimates to construct clinically usable survival probability nomograms; combine sex-specific regression coefficients for age, gait speed, and their interaction from accelerated failure time models for time to death and used the overall estimates to construct clinically usable life-expectancy nomograms; and combine areas under ROC curves obtained from 9 studies. An increase of 0.025 in overall area under ROC curve was interpreted as clinically relevant better accuracy.37 To appropriately combine entire survival curves across the 9 studies, we used the generalized least squares method for joint analysis of survival curves.38 We used a random-effects model with weights obtained by inverse of the variance of the survival function at the median life times to pool the median survival times for each sex, age group, and gait speed category. We used Comprehensive Meta Analysis version 2.2 (Biostat Inc, Englewood, New Jersey) for all meta-analytic methods and Stata SE 8 (StataCorp, College Station, Texas) for fitting shared frailty models.
RESULTS
The 9 participating studies contributed a total of 34 485 participants (Table 1). Although most studies included men and women, 2 were sex specific.19,22 Of the total, 59.6% were women. There were substantial numbers of African American (n=3852) and Hispanic (n=2650) participants. The studies had a wide age range, including 1765 persons older than 85 years. Similarly, there was a wide range of gait speeds, from less than 0.4 m/s (n=1247) to more than 1.4 m/s (n=1491). Study follow-up time ranged from 6.0 to 21.0 years, with participants followed up for a mean of 12.2 and a median of 13.8 years. There were 17 528 total deaths across all studies, with rates varying from 18.40% to 91.87% in individual studies. Mortality rates appear to be related to length of follow-up (Table 1).
To assess consistency across studies, risk of death was estimated per 0.1-m/s higher gait speed. Age-adjusted HRs by study ranged from 0.83 to 0.94 and all were significant (P<.001; Figure 1). We also examined the survival HRs for gait speed by study in subgroups, including age, sex, race/ethnicity, BMI, smoking history, use of mobility aids, prior hospitalization, self-reported health, functional status, and selected chronic diseases. There were consistent associations across studies, although given the large sample sizes, Q statistics were often statistically significant (details available in eFigure 1A–M available at http://www.jama.com). For the 3 levels of functional status (independent, difficulty with instrumental ADLs, and dependent in ADLs), the pooled HR per 0.1-m/s increase in gait speed for those who were independent was 0.92 (P= .005), for those with difficulty in instrumental activities was also 0.92 (P<.001) but was 0.94 (P=.02) among those dependent in ADLs. Because physical activity measures were not sufficiently consistent across studies, effects could not be pooled. The Osteoporotic Fractures in Men (MrOS)19 and Hispanic Established Populations for Epidemiologic Studies of the Elderly (EPESE)8 used the Physical Activity Scale for the Elderly (PASE). When dichotomized at a score of 100 into low and high activity, MrOS had consistent and statistically significant HRs for low (HR, 0.85; 95% CI, 0.81–0.88) and high (HR, 0.87; 95% CI, 0.84–0.90) physical activity. In the Hispanic EPESE, the HR for low physical activity was significant (0.92; 95% CI, 0.88–0.96) but the HR for higher physical activity was not (0.99; 95% CI, 0.95–1.04). Pooled HRs for all subgroups except functional status were consistently in the range of 0.81 to 0.92 and all were significant (P<.002).
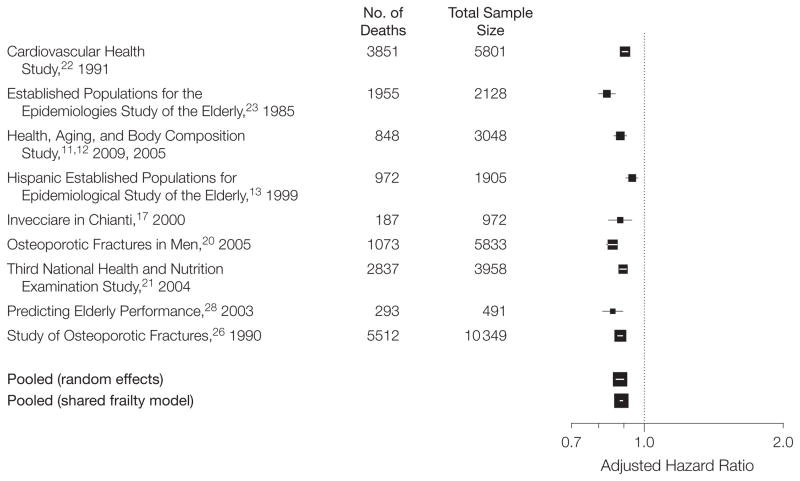
Age-Adjusted Hazard Ratio for Death per 0.1-m/s Higher Gait Speed
The size of the data markers is proportional to the square root of the number of participants. The error bars indicate 95% confidence intervals. The Q statistic for heterogeneity is 45.2 (P<.001; I2, 82.3). Pooled using random effects and shared frailty models.
The overall HR for survival per each 0.1 m/s faster gait speed was 0.88 (95% CI, 0.87–0.90; P<.001) when pooled across all studies using a random-effects meta-analytic statistical approach (Figure 1 and eFigure 1 available at http://www.jama.com). Further adjustment for sex, BMI, smoking status, systolic blood pressure, diseases, prior hospitalization, and self-reported health did not change the results (overall HR, 0.90; 95% CI, 0.89–0.91; P<.001). Using data from all studies, we created for each sex, 5- and 10-year survival tables (Table 2, data derived from pooled Kaplan-Meier estimates evaluated at 5 and 10 years, presented in 3 age groups) and graphs (eFigure 3 and eFigure 4 predicted survival based on pooled logistic regression coefficients, data presented with age as a continuous variable). Gait speed was associated with differences in the probability of survival at all ages in both sexes, but was especially informative after age 75 years. In men, the probability of 5-year survival at age 85 ranged from 0.3 to 0.88 (eFigure 3A) and the probability of 10-year survival at age 75 years ranged from 0.18 to 0.86 (eFigure 4A). In women, the probability of 5-year survival remained greater than 0.5 until advanced age (eFigure 3B), but 10-year survival at age 75 years ranged from 0.34 to 0.92 and at age 80 years from 0.22 to 0.86 (eFigure 4B). Stratification by sex-specific median height failed to show systematic differences in survival rates between short and tall participants, so results presented are not stratified by height. Stratification by race/ethnicity (non-Hispanic white, black, Hispanic) suggested generally similar survival rates by gait speed among age and sex groups. Confidence intervals were often wide. In some subsets of slow walkers of Hispanic descent, survival rates were 10% to 20% higher than in other groups (eTable 2).
Table 2
Five- and 10-Year Survival in Men and Women by Age and Gait Speed Group
| Gait Speed, m/s | 5-Year Survival (95% CI), %a | 10-Year Survival (95% CI), % | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | |||||||||
| Age 65–74 | Age 75–84 | Age ≥85 | Age 65–74 | Age 75–84 | Age ≥85 | Age 65–74 | Age 75–84 | Age ≥85 | Age 65–74 | Age 75–84 | Age ≥85 | |
| Speed <0.4 | 68 (47–82) | 60 (38–76) | 25 (15–36) | 80 (71–86) | 69 (58–78) | 47 (40–54) | 56 (23–80) | 15 (4–33) | 8 (3–18) | 58 (46–69) | 35 (24–47) | 11 (5–19) |
| ≥0.4 to <0.6 | 77 (72–81) | 57 (49–64) | 31 (24–39) | 88 (85–90) | 75 (68–80) | 61 (50–70) | 53 (41–64) | 23 (15–31) | 6 (3–11) | 67 (61–72) | 42 (36–48) | 18 (9–30) |
| ≥0.6 to <0.8 | 79 (74–83) | 65 (57–71) | 49 (35–61) | 91 (89–93) | 82 (78–86) | 74 (69–78) | 57 (52–62) | 31 (24–38) | 11 (3–28) | 74 (71–77) | 52 (46–57) | 23 (18–28) |
| ≥0.8 to <1.0 | 85 (82–88) | 75 (69–79) | 54 (43–64) | 93 (91–95) | 89 (86–91) | 73 (59–83) | 67 (62–71) | 43 (36–50) | 14 (7–25) | 80 (75–83) | 62 (56–68) | 39 (22–56) |
| ≥1.0 to <1.2 | 90 (85–93) | 83 (76–87) | 68 (57–77) | 96 (94–98) | 91 (87–94) | 61 (35–79) | 69 (63–74) | 53 (46–59) | 50 (6–84) | 86 (82–89) | 73 (70–77) | 33 (13–54) |
| ≥1.2 to <1.4 | 93 (86–96) | 85 (79–89) | 62 (46–74) | 96 (94–97) | 93 (87–96) | 67 (5–95) | 75 (40–91) | 51 (16–78) | NE | 83 (38–96) | 80 (72–86) | NE |
| Speed ≥1.4 | 95 (89–97) | 93 (86–96) | 91 (51–99) | 97 (94–99) | 95 (72–99) | NE | 93 (81–98) | 50 (6–84) | NE | 87 (71–95) | 92 (71–98) | NE |
| All gait speeds | 87 (82–91) | 74 (65–81) | 46 (39–53) | 93 (91–94) | 84 (80–87) | 64 (58–70) | 62 (58–66) | 36 (30–42) | 10 (8–13) | 77 (71–82) | 54 (46–60) | 22 (15–29) |
Abbreviations: CI, confidence interval; NE, not estimable due to small number of participants in categories.
We also used our analyses to estimate median years of remaining life based on sex, age, and gait speed. (Figure 2, predicted survival data are based on an accelerated failure time model with Weibull distribution, with age as a continuous variable, and eTable 3, data are derived from pooled Kaplan-Meier estimates evaluated at 5 and 10 years in 3 age groups.) In the pooled sample, median survival in years for the age groups 65 through 74 years was 12.6 for men and 16.8 for women; for 75 through 84 years, 7.9 for men and 10.5 for women; and for 85 years or older, 4.6 for men and 6.4 years for women (eTable 3 available at http://www.jama.com). Predicted years of remaining life for each sex and age increased as gait speed increased, with a gait speed of about 0.8 m/s at the median life expectancy at most ages for both sexes (Figure 2; a PDF of enlarged graphs is available at http://www.jama.com). Gait speeds of 1.0 m/s or higher consistently demonstrated survival that was longer than expected by age and sex alone. In this older adult population, the relationship of gait speed with remaining years of life was consistent across age groups, but the absolute number of expected remaining years of life was larger at younger ages. For 70-year-old men, life expectancy ranged from 7 to 23 years and for women, from 10 to 30 years.
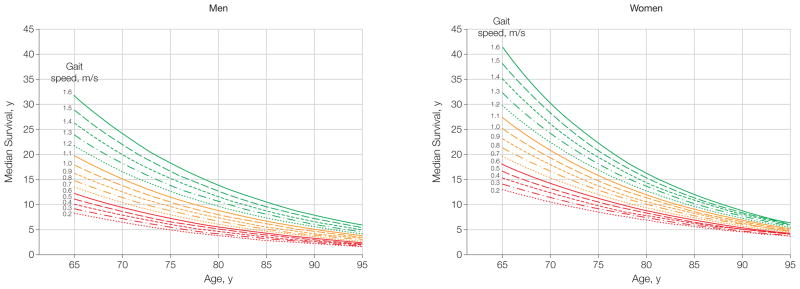
Predicted Median Life Expectancy by Age and Gait Speed
A PDF of enlarged graphs is available at http://www.jama.com.
To compare the 5-year survival predictive ability between demographics and gait speed vs other combinations of variables, we used areas under the ROC curve (C statistics) in logistic regression models for individual studies and pooled across studies (Table 3). Gait speed added substantially37 to age and sex in 7 of the 9 studies and in the pooled analysis. C statistics for age, sex, and gait speed were greater than those for age, sex, and chronic diseases in 4 of 9 studies, approximately equivalent in 5 studies and inferior in no studies. C statistics for age, sex, and gait speed were approximately equivalent to those for age, sex, chronic diseases, BMI, systolic blood pressure, and prior hospitalization in all 9 studies and in the pooled analysis. There were 4 studies that had sufficiently consistent data on functional status to create 3 categories: dependent in ADLs, difficulty with instrumental ADLs, and independent. For these studies, gait speed, age, and sex yielded a C statistic (0.741) that was not significantly different (P=.78) from age, sex, mobility aids, and functional status (P=.75; Table 3).
Table 3
Predictive Accuracy for 5- and 10-Year Survival by Individual Study and Pooled Data Presented as Area Under the Receiver Operating Characteristic Curves
| Outcome and Predictors | C Statistic (95% Confidence Interval) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| CHS8 | EPESE15 | Health, ABC16,17 | Hispanic EPESE8 | Invecciare in Chianti18 | Osteoporotic Fractures in Men19 | NHANES III20 | PEP21 | Study of Osteoporotic Fractures22 | Pooled | |
| 5-Year Mortality | ||||||||||
| Age, sex | 0.705 (0.685–0.725) | 0.685 (0.658–0.712) | 0.606 (0.575–0.637) | 0.694 (0.662–0.725) | 0.797 (0.754–0.841) | 0.700 (0.677–0.723) | 0.710 (0.691–0.729) | 0.674 (0.616–0.732) | 0.646 (0.625–0.667) | 0.690 (0.662–0.717) |
| Age, sex, diseases | 0.711 (0.692–0.731) | 0.692 (0.665–0.719) | 0.616 (0.586–0.647) | 0.703 (0.671–0.725) | 0.793 (0.747–0.838) | 0.704 (0.681–0.727) | 0.719 (0.700–0.737) | 0.694 (0.737–0.750) | 0.662 (0.639–0.684) | 0.698 (0.673–0.723) |
| Age, sex, diseases, BMI, systolic BP, prior hospitalization | 0.736 (0.717–0.755)b,c | 0.702 (0.676–0.728) | 0.650 (0.620–0.680)b,c | 0.728 (0.698–0.755)b,c | 0.808 (0.765–0.850) | 0.728 (0.706–0.749)b | 0.744 (0.727–0.762)b,c | 0.728 (0.674–0.781)b,c | 0.665 (0.643–0.686) | 0.719 (0.693–0.745)b |
| Age, sex, use of mobility aid, functional statusa | NA | NA | NA | 0.735 (0.705–0.765) | 0.803 (0.756–0.851) | NA | 0.738 (0.720–0.757) | 0.720 (0.663–0.776) | NA | 0.747 (0.720–0.774) |
| Age, sex, gait speed | 0.734 (0.716–0.753)c | 0.711 (0.685–0.737)c | 0.642 (0.612–0.673)b,c | 0.710 (0.679–0.741) | 0.803 (0.760–0.846) | 0.729 (0.707–0.751)b,c | 0.737 (0.719–0.755)b | 0.718 (0.664–0.771)c | 0.682 (0.662–0.703)b,c | 0.717 (0.694–0.740) 0.741 (0.706–0.775)d |
| 10-Year Mortality | ||||||||||
| Age, sex | 0.721 (0.707–0.734) | 0.725 (0.704–0.746) | NA | 0.700 (0.677–0.724) | NA | NA | 0.741 (0.726–0.757) | 0.674 (0.627–0.721) | 0.689 (0.676–0.703) | 0.712 (0.692–0.731) |
| Age, sex, diseases | 0.728 (0.715–0.742) | 0.738 (0.716–0.759) | NA | 0.709 (0.685–0.733) | NA | NA | 0.749 (0.734–0.764) | 0.698 (0.652–0.744) | 0.706 (0.692–0.719) | 0.724 (0.707–0.740) |
| Age, sex, diseases, BMI, systolic BP, prior hospitalization | 0.745 (0.732–0.759) | 0.749 (0.729–0.770) | NA | 0.733 (0.710–0.756)b | NA | NA | 0.768 (0.754–0.783)b | 0.723 (0.678–0.727)b,c | 0.709 (0.696–0.722) | 0.739 (0.719–0.759)b |
| Age, sex, functional status, walking aid usea | NA | NA | NA | 0.722 (0.699–0.746) | NA | NA | 0.761 (0.746–0.776) | 0.702 (0.655–0.748) | NA | 0.732 (0.698–0.767) |
| Age, sex, gait speed | 0.740 (0.727–0.754) | 0.753 (0.733–0.774)b | NA | 0.709 (0.685–0.732) | NA | NA | 0.766 (0.751–0.780)b | 0.723 (0.679–0.768)b,c | 0.719 (0.706–0.731)b | 0.737 (0.718–0.755)b,c 0.734 (0.692–0.777)d |
Abbreviations: ABC, Aging and Body Composition; BMI, body mass index, calculated as weight in kilograms divided by height in meters squared; BP, blood pressure; CHS, Cardiovascular Health Study; CI, confidence interval; EPESE, Established Populations for the Epidemiological Study of the Elderly; NA, not applicable; NHANES III, Third National Health and Nutrition Examination Survey; PEP, Predicting Elderly Performance.
For 10-year survival, 6 studies had sufficient follow-up time to perform many of the analyses (Table 3). Gait speed added predictive ability to age and sex in 4 of 6 studies and in the pooled analysis. C statistics for age, sex, and gait speed were not significantly different from C statistics with all the other factors for any study nor for the pooled analysis. Three studies had sufficiently consistent data on functional status at baseline to allow pooling. Gait speed, age, and sex yielded a C statistic (0.734) that was not significantly different from age, sex, mobility aids, and functional status (0.732; (P=.95; Table 3).
In addition, we used C statistics to assess the ability of usual gait speed to predict survival compared with other physical performance measures, such as fast gait speed and the Short Physical Performance Battery (SPPB), a brief measure that includes walk speed, chair rise ability, and balance. We assessed usual vs fast gait speed in the single study with both measures (Invecciare in Chianti18 study: usual, 0.727 [95% CI, 0.678–0.776]; fast, 0.684 [95% CI, 0.630–0.739]), suggesting that fast walks did not have an advantage in survival prediction over usual-paced walks. Gait speed was superior to the SPPB in the Hispanic Established Populations for the Epidemiological Study of the Elderly8 (gait speed, 0.617; 95% CI, 0.585–0.649; SPPB, 0.574; 95% CI, 0.539–0.649); was equivalent in the following 3 studies: Health, Aging, and Body Composition (ABC) study and ABC16 (gait speed, 0.579; 95% CI, 0.548–0.610; SPPB, 0.560; 95% CI, 0.528–0.592); Invecciare in Chianti (gait speed, 0.727; 95% CI, 0.678–0.776; SPPB, 0.738; 95% CI, 0.690–0.735); Predicting Elderly Performance study18 (gait speed, 0.667; 95% CI, 0.610–0.724; SPPB, 0.691; 95% CI, 0.637–0.744); and worse than SPPB in the Established Populations for the Epidemiological Study of the Elderly15 (gait speed, 0.638; 95% CI, 0.610–0.777; SPPB, 0.663; 95% CI, 0.636–0.691).
COMMENT
Gait speed, age, and sex may offer the clinician tools for assessing expected survival to contribute to tailoring goals of care in older adults. The accuracy of predictions based on these 3 factors appears to be approximately similar to more complex models involving multiple other health-related factors, or for age, sex, use of mobility aids, and functional status. Gait speed might help refine survival estimates in clinical practice or research because it is simple and informative.
Why would gait speed predict survival? Walking requires energy, movement control, and support and places demands on multiple organ systems, including the heart, lungs, circulatory, nervous, and musculoskeletal systems. Slowing gait may reflect both damaged systems and a high-energy cost of walking.13,39–54 Gait speed could be considered a simple and accessible summary indicator of vitality because it integrates known and unrecognized disturbances in multiple organ systems, many of which affect survival. In addition, decreasing mobility may induce a vicious cycle of reduced physical activity and de-conditioning that has a direct effect on health and survival.6
The association between gait speed and survival is known.6,7,9–12,55,56 Prior analyses used single cohorts and presented results as relative rather than absolute risk, as done herein. Similarly, mortality prediction models have been developed.3–5,57–60 Some models use self-reported information but others also include physiological or performance data, for a total of 4 to more than 10 predictive factors. Only a few models assess overall predictive capacity using C statistics; the reported values are in the range found in the present study (published area under the curve range, 0.66–0.8261 vs this study, 0.717 and 0.737).
The strengths of this study are the very large sample of individual participant data from multiple diverse populations of community-dwelling elders who were followed up for many years and use of consistent measures of performance and outcome. We provide survival estimates for a broad range of gait speeds and calculate absolute rates and median years of survival. Compared with prior studies that were too small to assess potential effect modification by age, sex, race/ethnicity, and other subgroups, we were able to assess multiple subgroup effects with substantial power. This study has the limitations of observational research; it cannot establish causal relationships and is vulnerable to various forms of healthy volunteer bias. The participating study cohorts, while large and diverse, do not represent the universe of possible data. Our survival estimates should be validated in additional data sets. Only 1 of the 9 studies was based in clinical practice,21 and advanced dementia is rare in populations who are competent to consent for research. However, median years of survival in this study resemble estimates for US adults across the sex and age range assessed.62 We were unable to assess the association of physical activity with survival in pooled analyses because measures of activity were highly variable across studies. Also, participants in these studies had no prior knowledge about the meaning of walking speed. In clinical use, participants might walk differently if they are aware of the implications of the results. Although this study provides information on survival, further work is needed to examine associations of other important pooled outcomes such as disability and health care use and to examine effects in populations more completely based in clinical practice.
Because gait speed can be assessed by nonprofessional staff using a 4-m walkway and a stopwatch,21 it is relatively simple to measure compared with many medical assessments. Nevertheless, methodological issues such as distance and verbal instructions remain.63,64 Self-report is an alternative to gait speed for reflecting function. However, significant challenges remain in the use of self-report as well, such as choice of items and reliability, some of which can be addressed by emerging techniques such as computer adaptive testing based on item-response theory.65 The results found herein suggest that gait speed appears to be especially informative in older persons who report either no function all imitations or only difficulty with instrumental ADLs and may be less helpful for older adults who already report dependence in basic ADLs. The research studies analyzed herein used trained staff to measure gait speed. Staffin clinical settings would need initial training and may produce more variable results. Long-distance walks have become accepted in some medical fields and may contribute information beyond short walks.66–68 However, the longer distance and time to perform the test may limit feasibility in many clinical settings. Although the sample size of very slow walkers was small, our data suggest that there may be a subpopulation who walk very slowly but survive for long periods. It would be valuable to further characterize this subgroup.
Although the gait speed–survival relationship seems continuous across the entire range, cut points may help interpretation. Several authors have proposed that gait speeds faster than 1.0 m/s suggest healthier aging while gait speeds slower than 0.6 m/s increase the likelihood of poor health and function.7,21 Others propose one cutoff around 0.8 m/s.13 In our data, predicted life expectancy at the median for age and sex occurs at about 0.8 m/s; faster gait speeds predict life expectancy beyond the median. Perhaps a gait speed faster than 1.0 m/s suggests better than average life expectancy and above 1.2 m/s suggests exceptional life expectancy, but additional research will be necessary to determine this relationship.
How might gait speed be used clinically? First, gait speed might help identify older adults with a high probability of living for 5 or 10 more years, who may be appropriate targets for preventive interventions that require years for benefit. Second, gait speed might be used to identify older adults with increased risk of early mortality, perhaps those with gait speeds slower than 0.6 m/s. In these patients, further examination is targeted at potentially modifiable risks to health and survival. A recommended evaluation and management of slow walking includes cardiopulmonary, neurological and musculoskeletal systems.6,18 Third, gait speed might promote communication. Primary clinicians might characterize an older adult as likely to be in poor health and function because the gait speed is 0.5 m/s. In research manuscripts, baseline gait speed might help to characterize the overall health of older research participants. Fourth, gait speed might be monitored overtime, with a decline indicating a new health problem that requires evaluation. Fifth, gait speed might be used to stratify risks from surgery or chemotherapy. Finally, medical and behavioral interventions might be assessed for their effect on gait speed in clinical trials. Such true experiments could then evaluate causal pathways to determine whether interventions that improve gait speed lead to improvements in function, health, and longevity.
The data provided herein are intended to aid clinicians, investigators, and health system planners who seek simple indicators of health and survival in older adults. Gait speed has potential to be implemented in practice, using a stop watch and a 4-m course. From a standing start, individuals are instructed to walk at their usual pace, as if they were walking down the street, and given no further encouragement or instructions. The data in this article can be used to help interpret the results. Gait speed may be a simple and accessible indicator of the health of the older person.
Acknowledgments
Funding/Support: Additional support for the pooled analyses was provided by grants AG023641, AG024827 and the Intramural Research Program, National Institute on Aging, NIH NIA Professional Services Contract Health and Human Services number 11200800292P. Dr Studenski received grant support from Merck to perform this work.
Role of the Sponsor: The role of Merck and Co in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript is as follows: Merck and Co reviewed and approved an initial proposal to conduct the study, which included gathering existing data and pooled statistical analyses. Representatives from Merck reviewed the initial manuscript draft.
Footnotes
Online-Only Material: A PDF of enlarged Figure 2 graphs; eTables 1–3, and eFigures 1A-M, 2, 3, and 4 are available at http://www.jama.com.
Author Contributions: Dr Studenski had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Studenski, Faulkner, Chandler, Nevitt, Kritchevsky, Ferrucci, Guralnik.Acquisition of data: Studenski, Faulkner, Nevitt, Visser, Kritchevsky, Badinelli, Harris, Newman, Cauley, Ferrucci, Guralnik.
Analysis and interpretation of data: Studenski, Perera, Patel, Rosano, Faulkner, Inzitari, Brach, Chandler, Cawthon, Barrett-Connor, Nevitt, Visser, Harris, Newman, Cauley, Guralnik.
Drafting of the manuscript: Studenski, Perera, Inzitari, Badinelli.
Critical revision of the manuscript for important intellectual content: Studenski, Perera, Patel, Rosano, Faulkner, Brach, Chandler, Cawthon, Barrett-Connor, Nevitt, Visser, Kritchevsky, Harris, Newman, Cauley, Ferrucci, Guralnik.
Statistical analysis: Studenski, Perera, Patel, Inzitari, Chandler, Guralnik.
Obtained funding: Studenski, Chandler, Nevitt, Kritchevsky, Badinelli, Harris, Newman, Ferrucci, Guralnik.
Administrative, technical, or material support: Studenski, Patel, Rosano, Faulkner, Cawthon, Nevitt, Visser, Badinelli, Harris, Newman, Cauley
Study supervision: Perera, Nevitt, Newman.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr Studenski reported receiving institutional grant support, travel expenses, and consultancy fees from Merck; consultlancy fees from Novartis and GTX; and royalties from Hazzart Text McGraw Hill. Dr Perera reported receiving institutional grant support from Merck Research Lab. Dr Inzitari reported receiving insitutional grant support from Merck. Dr Brach reported receiving institutional grant support from Merck. Dr Cawthon reported receiving consultancy fees from Amgen and Merck. Dr Cauley reported receiving consultancy fees and institutional grant support from Novartis. Drs Patel, Faulkner, Barett-Connor, Nevitt, Visser, Bandellini, Harris, Newman, Ferrucci, and Gurlanik reported no disclosures.
References
Full text links
Read article at publisher's site: https://doi.org/10.1001/jama.2010.1923
Read article for free, from open access legal sources, via Unpaywall:
https://jamanetwork.com/journals/jama/articlepdf/644554/joc05171_50_58.pdf
Subscription required at jama.ama-assn.org
http://jama.ama-assn.org/cgi/reprint/305/1/50.pdf
Free to read at jama.ama-assn.org
http://jama.ama-assn.org/cgi/content/abstract/305/1/50
Subscription required at jama.ama-assn.org
http://jama.ama-assn.org/cgi/content/full/305/1/50
Citations & impact
Impact metrics
Citations of article over time
Article citations
White matter integrity and motor function: a link between cerebral myelination and longitudinal changes in gait speed in aging.
Geroscience, 30 Oct 2024
Cited by: 0 articles | PMID: 39476324
Impact of community-based precision functional training on older adults' walking and cognitive abilities in rural Taiwan: a pre-posttest study.
BMC Geriatr, 24(1):819, 11 Oct 2024
Cited by: 0 articles | PMID: 39394100 | PMCID: PMC11468099
Wild capuchin monkeys as a model system for investigating the social and ecological determinants of ageing.
Philos Trans R Soc Lond B Biol Sci, 379(1916):20230482, 28 Oct 2024
Cited by: 3 articles | PMID: 39463253
Review
Effect of a Physical Exercise Intervention on Physical Function Parameters and Blood Analytical Changes in Lung Cancer Survivors: A Feasibility Study.
Clin Pract, 14(5):2202-2216, 18 Oct 2024
Cited by: 0 articles | PMID: 39451888 | PMCID: PMC11506576
Complexities and challenges of translating intervention success to real world gait in people with Parkinson's disease.
Front Neurol, 15:1455692, 09 Oct 2024
Cited by: 0 articles | PMID: 39445193 | PMCID: PMC11496290
Review Free full text in Europe PMC
Go to all (2,121) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Gait Speed Predicts Incident Disability: A Pooled Analysis.
J Gerontol A Biol Sci Med Sci, 71(1):63-71, 22 Aug 2015
Cited by: 212 articles | PMID: 26297942 | PMCID: PMC4715231
Hospitalization-Associated Change in Gait Speed and Risk of Functional Limitations for Older Adults.
J Gerontol A Biol Sci Med Sci, 74(10):1657-1663, 01 Sep 2019
Cited by: 22 articles | PMID: 30715162 | PMCID: PMC6748735
Improvement in usual gait speed predicts better survival in older adults.
J Am Geriatr Soc, 55(11):1727-1734, 03 Oct 2007
Cited by: 320 articles | PMID: 17916121
Gait speed as a measure in geriatric assessment in clinical settings: a systematic review.
J Gerontol A Biol Sci Med Sci, 68(1):39-46, 24 Aug 2012
Cited by: 229 articles | PMID: 22923430
Review
Funding
Funders who supported this work.
Intramural NIH HHS
NCATS NIH HHS (1)
Grant ID: UL1 TR000005
NIA NIH HHS (7)
Grant ID: K07 AG023641-05
Grant ID: AG023641
Grant ID: AG024827
Grant ID: P30 AG024827
Grant ID: K07 AG023641
Grant ID: P30 AG024827-08
Grant ID: P30 AG021332




