Abstract
Background
Adolescents with type 1 diabetes experience stress related to treatment management, feeling different from peers, and deciding to tell others about their diabetes.Purpose
This study examined the relationship of stress reactivity and coping with self-management, quality of life, and metabolic control in an ethnically diverse sample of adolescents with type 1 diabetes.Methods
Adolescents (n = 327) completed measures of coping and stress reactivity, self-management, and quality of life. Glycosylated hemoglobin data were collected from medical records.Results
Low-income and minority status were related to lower levels of primary control coping (e.g., problem solving) and secondary control coping (e.g., acceptance), and higher levels of disengagement coping (e.g., avoidance). Self-management mediated the relationship between coping and stress reactivity with quality of life and metabolic control. Race/ethnicity and income moderated the relationship between coping and self-management goals.Conclusions
Results indicate differences in coping related to income and race/ethnicity and demonstrate the impact of coping on self-management and health outcomes in adolescents with type 1 diabetes.Free full text

Coping, Self-Management, and Adaptation in Adolescents with Type 1 Diabetes
Abstract
Background
Adolescents with type 1 diabetes experience stress related to treatment management, feeling different from peers, and deciding to tell others about their diabetes.
Purpose
This study examined the relationship of stress reactivity and coping with self-management, quality of life, and metabolic control in an ethnically diverse sample of adolescents with type 1 diabetes.
Methods
Adolescents (n = 327) completed measures of coping and stress reactivity, self-management, and quality of life. Glycosylated hemoglobin data were collected from medical records.
Results
Low-income and minority status were related to lower levels of primary control coping (e.g., problem solving) and secondary control coping (e.g., acceptance), and higher levels of disengagement coping (e.g., avoidance). Self-management mediated the relationship between coping and stress reactivity with quality of life and metabolic control. Race/ethnicity and income moderated the relationship between coping and self-management goals.
Conclusions
Results indicate differences in coping related to income and race/ethnicity and demonstrate the impact of coping on self-management and health outcomes in adolescents with type 1 diabetes.
Introduction
Type 1 diabetes is one of the most common chronic childhood illnesses, affecting as many as 1 in 400 youth, with a peak onset during adolescence [1]. Management of type 1 diabetes is complex and demanding, requiring the adolescent and family to frequently monitor blood glucose levels, food intake, and exercise, and adjust insulin accordingly [2]. For youth with type 1 diabetes, the transition into adolescence is often associated with poorer self-management and deteriorating metabolic control [3]. In addition to the stress of self-management, adolescents with type 1 diabetes report stress related to feeling different from peers, feeling guilty about “bad numbers,” and deciding how and when to tell others about diabetes [4]. These high levels of diabetes-related stress are likely to have a negative impact on adolescents’ quality of life (QOL) and metabolic control [5]. In addition, stress may affect adolescents’ motivation and ability to perform self-management tasks, resulting in poorer metabolic control [6]. Therefore, it is important to understand the strategies that adolescents use to cope with diabetes-related stress and the relationships among coping, self-management, QOL, and metabolic control in adolescents with type 1 diabetes. The purpose of this study was to test a model of coping and stress reactivity, self-management, and the diabetes-related outcomes of QOL and metabolic control in an ethnically diverse sample of early adolescents with type 1 diabetes.
Coping in Adolescents with Type 1 Diabetes
The broader literature on coping indicates that the ways in which children and adolescents cope with stress are important mediators and moderators of the emotional and behavioral outcomes of stressful situations [7]. Coping in youth with type 1 diabetes has been studied over the past 25 years, using a variety of measures and approaches. Findings from these studies consistently demonstrate relationships between coping and self-management, quality of life, and metabolic control. Greater use of avoidant (or emotion-focused) coping strategies, such as wishful thinking, has been shown to be related to poorer metabolic control [8–10] and poorer psychosocial outcomes, including lower QOL and more depressive symptoms [8, 11, 12]. In contrast, greater use of approach (or problem-focused) coping strategies has been related to better metabolic control and better psychosocial adjustment in youth with type 1 diabetes [11, 13, 14]. Similarly, greater use of avoidant coping and less use of approach coping has been related to poorer self-management [13, 15]. To our knowledge, however, no studies have examined self-management as a mediator of the relationship between coping and the outcomes of metabolic control and QOL. Coping may directly influence metabolic control and QOL by decreasing the negative impact of stress; however, coping may also indirectly influence metabolic control and QOL through improved self-management. Self-management in adolescents with type 1 diabetes has been associated with both metabolic control and QOL [16, 17]. Therefore, self-management may be an important mediating link between coping and metabolic control and QOL.
Studies have consistently shown that lower income and minority youth with type 1 diabetes are at greater risk for poor metabolic control, hospitalizations for ketoacidosis, and long-term complications [18, 19]. Differences in coping styles may help to explain some of these demographic differences in diabetes-related outcomes. For example, the high levels of chronic stress experienced by adolescents from lower income families may interfere with their ability to use complex coping strategies, such as problem solving and cognitive restructuring [20]. Previous studies of coping in adolescents with type 1 diabetes have been limited by a lack of diversity. Thus, it is important to examine demographic differences in coping with diabetes, which may be affected by the higher levels of stress experienced by lower income and minority youth.
Research on coping in youth with other chronic conditions supports a developmentally appropriate model of stress and coping that differentiates between controlled/voluntary and automatic/involuntary responses to stressful events or circumstances [7, 21]. This model, supported by factor analysis, expands previous conceptualizations of coping to include three coping factors: primary control engagement coping, secondary control engagement coping, disengagement coping, as well as involuntary responses to stress, or stress reactivity (e.g., physiological arousal, rumination) [22]. Primary control engagement coping includes attempts to change the problem or one’s response to it (e.g., problem solving, emotional expression); secondary control engagement coping includes attempts to adapt to the stressor (e.g., acceptance, distraction); and disengagement coping includes avoidance, denial, and wishful thinking. This model extends previous conceptualizations of coping, in which some strategies do not clearly fit into the emotion-focused/problem-focused categories. A coping strategy such as forming a plan, for example, may help to solve a problem and also relieve negative emotions. Research with the current model has shown that higher levels of secondary control engagement coping and lower levels of disengagement coping were more effective for coping with pain in a pediatric population [22]. This model of automatic and voluntary responses to stress provides the conceptual framework for this analysis.
Purpose
The purpose of this study was to examine the relationship of stress reactivity and coping (primary, secondary, and disengagement) with self-management, QOL, and metabolic control (i.e., glycosylated hemoglobin—A1C). In addition, we explored associations between demographic variables (e.g., gender, race/ethnicity, SES) and adolescents’ responses to stress. We tested a structural model of self-management as a mediator of coping and stress reactivity and diabetes-related outcomes (i.e., QOL, A1C). We hypothesized that higher levels of primary and secondary control coping and lower levels of disengagement coping and stress reactivity would be associated with increased self-management, which, in turn, would be related to better outcomes. Finally, we explored race/ethnicity and income as potential moderators of the relationship between coping and self-management.
Methods
We report an analysis of baseline data from an ongoing randomized clinical trial. The purpose of the larger study is to determine the effect of an internet-based coping skills training intervention on physiologic adaptation (A1C), psychosocial adaptation (QOL), and family adaptation (conflict) compared to an internet-based education intervention for adolescents with type 1 diabetes.
Participants and Procedure
Adolescents with type 1 diabetes were eligible for the study if they were between the ages of 11 and 14, had no other serious health problems, and had been diagnosed for at least 6 months. A total of 541 adolescents with type 1 diabetes were identified as eligible from outpatient diabetes clinics at four sites across the USA, selected to provide an oversample of racial/ethnic minorities. Of these, 90 refused participation (most common reasons were time commitment, lack of interest), 22 asked to be contacted later, and another 79 failed to complete baseline data. After providing consent (assent) in line with university IRB requirements, 327 adolescents completed baseline questionnaires on a password-protected, study-specific website. At least 10 subjects (and ideally 20) for each parameter in the model are sufficient for structural equation modeling [23], and our models contain 25 parameters. Demographic information was provided by parents during the consent process. Sample characteristics are presented in Table 1.
Table 1
Sample demographics (n = 327)
| Mean (SD) | ||
|---|---|---|
| Age | 12.3 (1.1) | |
| Duration of diabetes (years) | 5.5 (3.5) | |
| N (%) | ||
| Gender | Male | 150 (45.9) |
| Female | 177 (54.1) | |
| Race/ethnicity | White/non-Hispanic | 201 (61.8) |
| Black/Hispanic/others | 124 (38.2) | |
| Income | <$40,000 | 68 (21.6) |
| $40,000–$79,999 | 87 (27.6) | |
| ≥$80,000 | 160 (50.8) | |
| Therapy | Pump | 193 (59.0) |
| Injection—basal | 81 (24.8) | |
| Injection—conventional | 53 (16.2) | |
Measures
The Responses to Stress Questionnaire assessed coping strategies used by adolescents in response to diabetes-related stressors. The first ten questions were designed to be developmentally specific to the concerns of adolescents with type 1 diabetes (e.g., feeling different from peers, dealing with diabetes care), and the total stress score ranges from 0 to 30 (mean in our sample = 10.28, SD = 4.77) [4]. The following 57 items ask adolescents how they respond to the diabetes-related stressors with a range of voluntary coping and involuntary responses to stress characteristic of adolescents [21]. The four factors included in the analyses are Primary Control Engagement Coping (9 items; problem solving, emotional expression, emotional regulation), Secondary Control Engagement Coping (12 items; distraction, acceptance, positive thinking, cognitive restructuring), Disengagement Coping (9 items; avoidance, denial, wishful thinking), and Stress Reactivity (12 items; e.g., physiological arousal, rumination). The Responses to Stress Questionnaire has demonstrated internal consistency and test–retest reliability ranging from adequate to excellent [21]. Mean ratio scores were calculated to account for differences in overall levels of coping [24]. For the current sample, Cronbach’s alpha was 0.77 for primary control engagement coping, 0.80 for secondary control engagement coping, 0.77 for disengagement coping, and 0.88 for stress reactivity.
The Self-Management in Adolescents with Diabetes questionnaire was used to assess adolescents’ self-management tasks and goals [25]. It is a 52-item self-report measure, consisting of five subscales: collaboration with parents, diabetes care activities, diabetes problem solving, diabetes communication, and goals. The stability of the measure ranged from 0.60 to 0.88 at 2 weeks to 0.59 to 0.85 at 3 months [25]. For the current study, we used the activities subscale (e.g., “I check my blood sugar before eating.”), (range = 0–45, Cronbach’s alpha = 0.74); the collaboration subscale (e.g., “My parents help me decide my insulin dose.”), (range = 0–39, Cronbach’s alpha = 0.80); and the goals subscale (e.g., “One of my goals is to take care of my diabetes more on my own.”), (range = 0–21, Cronbach’s alpha = 0.63) as indicators of self-management.
The Pediatric Quality of Life instrument was developed to evaluate QOL in children with chronic health conditions [26]. The 28-item diabetes-specific QOL measure consists of five discrete subscales: general diabetes QOL, general type 1 diabetes treatment QOL, specific type 1 diabetes treatment QOL, worry, and communication. Scores on each scale are transformed to a score of 0–100; higher scores reflect better QOL. High reliability and validity have been established in various clinical and community samples [26]. For the current study, we used the general diabetes QOL subscale (Cronbach’s alpha = 0.89).
Glycosylated Hemoglobin (A1C). The glycosylation of the hemoglobin molecule provides objective criteria of metabolic control over the most recent 8–12 weeks. A1C is routinely measured quarterly in patients with type 1 diabetes. In the majority of the sample (80%), analyses were performed using the Bayer Diagnostics DCA2000®, which provides results in 6 min on a fingerstick blood sample (normal range = 4.2–6.3%). The other methods used were Roche Tinaquant, immunoturbidimetry, and high-performance liquid chromatography. The American Diabetes Association recommends that adolescents maintain A1C at or below 8% [2].
Data Analyses
Data were coded and transferred from the online database to Access™ databases. Descriptive analyses were conducted using ANOVA to test for demographic differences in coping. Bivariate correlations were conducted to examine the relationship between stress reactivity and coping with self-management, QOL, and A1C. To test self-management as a mediator of coping and adaptation, we used structural equation modeling with the MPlus program. The maximum likelihood method was used to estimate the fit of the model, and standardized path coefficients are presented. We report several fit indices for the model, including the Comparative Fit Index (CFI), the Tucker Lewis Index (TLI), and the Root Mean Square Error of Approximation (RMSEA). Models with CFI and TLI indices greater than 0.9 are considered to have a relatively good fit, and a RMSEA of less than 0.10 indicates an adequate fit, and less than 0.05 indicates a good fit [27]. Finally, race/ethnicity and income were tested as potential moderators of the relationship between coping and self-management by examining the interaction of income/racial categories × responses to stress for self-management activities and goals with general linear regression models.
Results
Descriptive Analyses
There were no significant differences in coping related to age, gender, or treatment type, but there were differences related to income and race/ethnicity (see Table 2). Compared to adolescents from the highest income families (annual income≥$80,000), those from the lowest income families (annual income<$40,000) had significantly lower levels of primary control coping (p<0.001) and secondary control coping (p<0.01), and significantly higher levels of disengagement coping (p<0.01), representing a medium-sized effect for income. There was not a significant difference in income level for stress reactivity. In addition, there were small to medium-sized effects of race/ethnicity on coping; minority youth reported significantly lower levels of primary control coping (p<0.001) and secondary control coping (p<0.05), and higher levels of disengagement coping (p<0.05) than white, non-Hispanic youth. There was not a significant difference in stress reactivity for race/ethnicity.
Table 2
Demographic differences in responses to stress
| Demographics | N | Coping and responses to stress
| ||||
|---|---|---|---|---|---|---|
| Primary control mean (SD) | Second control mean (SD) | Disengagement mean (SD) | Stress reactivity mean (SD) | |||
| Age | 11–12 | 188 | 0.19 (0.04) | 0.26 (0.06) | 0.15 (0.03) | 0.19 (0.04) |
| 13–14 | 139 | 0.19 (0.04) | 0.26 (0.05) | 0.15 (0.03) | 0.19 (0.04) | |
| p value | 0.361 | 0.445 | 0.531 | 0.412 | ||
| Gender | Male | 150 | 0.19 (0.04) | 0.26 (0.06) | 0.15 (0.03) | 0.19 (0.04) |
| Female | 177 | 0.19 (0.04) | 0.26 (0.05) | 0.15 (0.03) | 0.19 (0.03) | |
| p value | 0.154 | 0.916 | 0.568 | 0.433 | ||
| Income | Less than $40,000 | 68 | 0.18 (0.04) | 0.25 (0.06) | 0.15 (0.03) | 0.19 (0.04) |
| $40,000–$79,000 | 87 | 0.19 (0.04) | 0.26 (0.06) | 0.15 (0.03) | 0.19 (0.03) | |
| $80,000+ | 160 | 0.20 (0.04) | 0.27 (0.05) | 0.14 (0.03) | 0.19 (0.03) | |
| p value | 0.001 | 0.045 | 0.005 | 0.077 | ||
| Race | White | 201 | 0.20 (0.04) | 0.27 (0.05) | 0.14 (0.03) | 0.19 (0.04) |
| Non-White | 124 | 0.18 (0.04) | 0.25 (0.05) | 0.15 (0.03) | 0.19 (0.03) | |
| p value | 0.001 | 0.049 | 0.012 | 0.126 | ||
| Therapy | Injection | 134 | 0.19 (0.04) | 0.27 (0.06) | 0.15 (0.03) | 0.19 (0.03) |
| Pump | 193 | 0.19 (0.04) | 0.26 (0.05) | 0.15 (0.03) | 0.19 (0.04) | |
| p value | 0.976 | 0.087 | 0.691 | 0.298 | ||
Correlational Analyses
Bivariate correlations indicate the associations between coping and stress reactivity with self-management, QOL, and metabolic control (i.e., A1C) (see Table 3).
Table 3
Correlations between coping, self-management, quality of life, and metabolic control
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Primary Control | – | ||||||||
 M = 0.24 (0.04) M = 0.24 (0.04) | |||||||||
| Secondary Control | 0.52*** | – | |||||||
 M = 0.33 (0.06) M = 0.33 (0.06) | |||||||||
| Disengagement | −0.59*** | −0.50*** | – | ||||||
 M = 0.19 (0.04) M = 0.19 (0.04) | |||||||||
| Stress Reactivity | −0.57*** | −0.77*** | 0.27*** | – | |||||
 M = 0.24 (0.05) M = 0.24 (0.05) | |||||||||
| SMOD Activities | 0.37*** | 0.30*** | −0.28*** | −0.29*** | – | ||||
 M = 32.1 (5.9) M = 32.1 (5.9) | |||||||||
| SMOD Collaboration | 0.08 | 0.06 | −0.11 | 0.00 | 0.22*** | – | |||
 M = 21.8 (6.7) M = 21.8 (6.7) | |||||||||
| SMOD Goals | 0.32*** | 0.24*** | −0.19*** | −0.28*** | 0.35*** | −0.06 | – | ||
 M = 15.6 (2.8) M = 15.6 (2.8) | |||||||||
| PedsQL | 0.43*** | 0.53*** | −0.31*** | −0.50*** | 0.37*** | −0.01 | 0.30*** | – | |
 M = 80.3 (12.3) M = 80.3 (12.3) | |||||||||
| A1C | −0.14** | −0.19*** | 0.06 | 0.16* | −0.24*** | −0.02 | −0.21*** | −0.07 | – |
 M = 8.3 (1.5) M = 8.3 (1.5) |
SMOD self-management of diabetes, PedsQL pediatric quality of life
Mediation Analyses
The original structural model based on the hypothesized relationships between coping and stress reactivity, self-management, QOL, and A1C was a good fit for the data (CFI = 1.00, TLI = 1.044, RMSEA<0.001). As seen in Fig. 1, greater use of primary control engagement coping was related to higher levels of self-management, while greater stress reactivity was related to lower levels of self-management. Furthermore, the self-management factor, made up of the activities and goals subscales, was positively related to QOL. Support for mediation was found; there was a significant indirect effect of primary control engagement coping on QOL through self-management (β = 0.51±0.17, p = 0.002). There was also a significant indirect effect of stress reactivity on QOL through self-management (β = −0.25±0.11, p = 0.018). There was not a significant direct effect for any responses to stress on QOL.
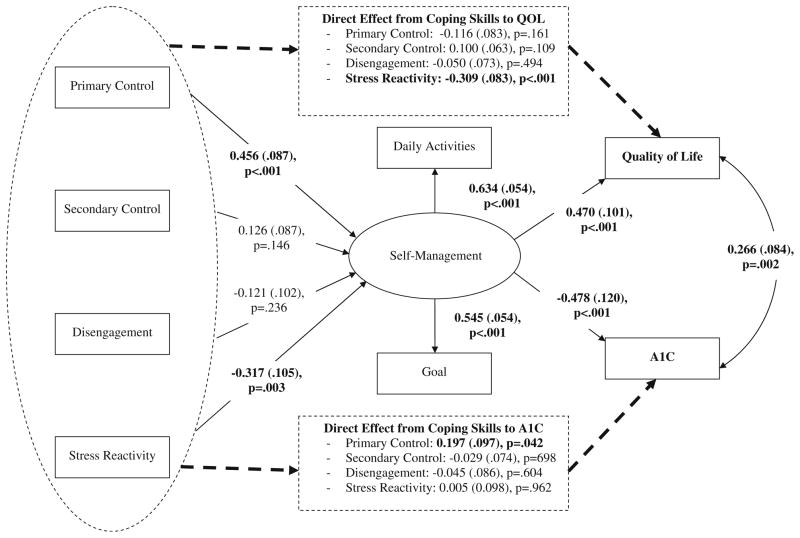
Mediation model for the effect of self-management on the relationships between coping and stress reactivity on A1C and Quality of Life (QOL). The numbers provided for each path are standardized coefficients and error terms. Solid lines indicate indirect effects; dashed lines indicate direct effects
Greater self-management was also related to lower A1C. Support for mediation from responses to stress to A1C through self-management was also found; there was a significant indirect effect of primary control engagement coping on A1C through self-management (β = −0.62±0.02, p = 0.004). There was also a significant indirect effect of stress reactivity on A1C through self-management (β = 0.03±0.01, p = 0.024). Finally, there was a significant direct effect of primary control coping on A1C.
Moderation Analyses
In our sample, there was considerable overlap between race and income; 67% of White/non-Latino youth had relatively high income (≥$80 K/year) while only 23% of non-white youth had high income. In this sample, it would be difficult to examine race and income effect separately. Therefore, we created four groups: White and high income (≥$80 K/year, n = 134), White and lower income (<$80 K/year, n = 67), minority and high income (≥$80 K/year, n = 26), and minority and lower income (<$80 K/year, n = 87). These categories were used to examine race/income as potential moderators of the relationship between coping and self-management.
There was no significant effect of race/income on the associations between responses to stress and the daily activities of self-management (see Table 4). Race/income did moderate the association between stress reactivity and self-management goals (p = 0.022). There was a significant effect of stress reactivity on goals for White/high income youth (β = −0.14, p<0.001), but this effect was not significant for White/lower income youth or minority youth. Finally, there was a trend toward significance for the moderating effect of race/income on the association between disengagement coping and self-management goals (p = 0.071). The effect of disengagement coping on goals was only significant for White/high income youth (β = −0.15, p = 0.002).
Table 4
Moderation effects of race and income on self-management
| White and high income N = 134 β ± SE (p value) | White and low income N = 67 β ± SE (p value) | Minority and high income N = 26 β ± SE (p value) | Minority and low income N = 87 β ± SE (p value) | Interaction effect (p value) | |
|---|---|---|---|---|---|
| Effect on daily activities of self-management | |||||
| Primary control | 0.352±0.097 (<0.001) | 0.332±0.130 (0.012) | 0.236±0.256 (0.357) | 0.197±0.114 (0.086) | 0.750 |
| Secondary control | 0.319±0.076 (<0.001) | 0.129±0.094 (0.171) | 0.174±0.177 (0.328) | 0.179±0.096 (0.062) | 0.418 |
| Disengagement | −0.364±0.104 (<0.001) | −0.220±0.128 (0.088) | 0.010±0.217 (0.963) | −0.120±0.106 (0.258) | 0.270 |
| Stress reactivity | −0.247±0.074 (0.001) | −0.165±0.095 (0.084) | −0.077±0.182 (0.671) | −0.096±0.073 (0.189) | 0.506 |
| Effect on self-management goals | |||||
| Primary control | 0.170±0.046 (<0.001) | 0.182±0.062 (0.003) | 0.134±0.121 (0.269) | 0.033±0.054 (0.546) | 0.198 |
| Secondary control | 0.137±0.036 (<0.001) | 0.100±0.045 (0.027) | 0.134±0.084 (0.113) | 0.021±0.045 (0.646) | 0.241 |
| Disengagement | −0.154±0.050 (0.002) | 0.023±0.062 (0.715) | 0.022±0.104 (0.832) | −0.001±0.051 (0.985) | 0.071 |
| Stress reactivity | −0.140±0.035 (<0.001) | −0.009±0.045 (0.841) | −0.101±0.086 (0.240) | 0.000±0.035 (0.999) | 0.022 |
Discussion
The current study examined coping in a large, diverse sample of adolescents with type 1 diabetes. We found that the use of secondary control engagement coping strategies, such as acceptance and distraction, and primary control engagement coping strategies, such as problem solving, to cope with diabetes-related stress were linked with better self-management and better adaptation. Perhaps most importantly, we found support for self-management as a mediator of the relationship between coping and metabolic control, as well as coping and QOL.
Two important demographic differences emerged in the coping strategies reported by youth in our sample: race/ethnicity and income. There was a medium-sized effect of family income on coping, with adolescents from the lowest income category reporting less primary and secondary control engagement coping and more disengagement coping strategies than adolescents in the highest income category. Similarly, there was a small effect for race/ethnicity, with minority youth reporting lower rates of primary and secondary control engagement coping and higher rates of disengagement coping than non-Hispanic White youth. These differences in coping may help to explain the findings from other studies that Hispanic and Black adolescents tend to have poorer metabolic control than White adolescents [19, 28]. In these studies, as in our sample, family income is often highly associated with race/ethnicity; therefore, more work is needed to tease apart the effects of race/ethnicity and income on coping and metabolic control. It is possible that adolescents from lower income families experience higher levels of stress, interfering with the cognitive abilities required to use primary and secondary control coping strategies, such as problem solving and cognitive restructuring [20]. It is notable that in our sample, there were no significant differences in coping strategies related to age, gender, or treatment type. Our age range was somewhat limited, however, to early adolescents (ages 11–14), and it is possible that differences exist between younger and older adolescents [29].
Results from the current study support that the effect of coping on metabolic control and QOL is mediated by adolescents’ self-management activities and goals. Specifically, higher levels of primary control engagement coping were related to higher levels of self-management, which, in turn, were related to better QOL and lower A1C. In contrast, higher levels of stress reactivity were related to lower levels of self-management, which, in turn, were related to poorer QOL and higher A1C. Self-management did not mediate the relationship between secondary control or disengagement coping on QOL and A1C. In addition, primary control coping had a direct effect on A1C. This may be explained by the items on the primary control coping scale that assesses emotion regulation, which has been linked with better metabolic control [28]. Furthermore, stress reactivity had a direct effect on quality of life, suggesting that intrusive thoughts and physiological arousal related to diabetes stress have a negative impact on adolescents’ QOL. Collectively, these findings expand the previous work of Grey and colleagues [30], by providing greater specificity as to the coping strategies and stress responses that promote better or worse adaptation to type 1 diabetes. Promoting problem solving and stress management appears particularly important.
In addition, race/ethnicity and income moderated on the relationship between coping and self-management. For White youth from high income families, coping was significantly associated with self-management, such that higher levels of stress reactivity and greater use of disengagement coping were related to fewer self-management goals. For minority and lower income youth, however, coping efforts did not seem to impact self-management to the same extent. It is likely that, for lower income families, economic stress is more salient than diabetes-related stress reported on by this sample [31]. Thus, for lower income youth, the coping strategies used to deal with economic stress may be better predictors of their adaptation. Furthermore, the high levels of chronic stress experienced by lower income and minority youth may interfere with the cognitive abilities required to use primary and secondary control coping strategies, such as problem solving and cognitive restructuring [20]. Note that the small number of high-income/minority youth in our sample limits the conclusions that can be made about the moderating effects.
Limitations
This study is limited by the cross-sectional design, which does not allow us to test for direction of effects. As such, the mediation analyses must be considered exploratory, since tests of mediation may be biased in cross-sectional samples. In addition, the current study used baseline data from an intervention study, which required participants to commit to a study lasting 18 months. Therefore, our sample may be biased by self-selection, as the demands of the intervention study may have excluded adolescents from more stressed families. Finally, our sample was in relatively good metabolic control; the mean A1C was 8.0%, which is the target for this age group [2]. It is possible that adolescents who have poorer metabolic control use different coping strategies.
Implications
Findings from this study highlight the youth who may be at higher risk for poor adaptation. Previous studies have shown that lower socioeconomic status and minority race/ethnicity have been correlated with poorer metabolic control, more hospitalizations for ketoacidosis, higher rates of long-term complications, and increased age-adjusted mortality rates [18, 19]. Our findings may help to explain how coping contributes to poorer outcomes in these populations. In our sample, minority and lower income youth were less likely to use adaptive coping strategies (i.e., primary and secondary control coping), and their coping efforts had less of an impact on self-management. This suggests that low income and minority youth may need additional support in developing and using coping skills to deal with diabetes-related stress, and that the ways they cope with stress related to poverty and discrimination may also be important to assess.
Furthermore, results from this study highlight the potential importance of coping to self-management, QOL, and metabolic control, warranting further attention to assessment of stress and coping in adolescents and interventions to promote adaptive coping. Specifically, these results suggest that interventions that promote or teach primary control coping strategies (e.g., problem solving, emotional expression), and secondary control coping strategies (e.g., acceptance, positive thinking), may help adolescents deal with diabetes-related stress in adolescents, particularly in minority groups. Finally, our results suggest that adolescents with type 1 diabetes may benefit from learning strategies to manage stress (e.g., relaxation), reducing stress reactivity.
Directions for Future Research
Further studies are needed in diverse populations to tease apart the effects of income and race/ethnicity, as well as the moderating effects of family functioning, on adolescents’ coping with diabetes-related stress. Longitudinal studies are also needed to determine the direction of effects. A recent study, for example, examined the relationships among coping and metabolic control in adolescents with type 1 diabetes over 4 years using a cross-lagged design and found that coping, psychological symptoms, and metabolic control were inter-related over time [32]. Finally, further studies are needed to determine the best setting, and optimal age for interventions aimed at improving coping in adolescents with type 1 diabetes.
Measurement of coping has varied widely in studies of youth with type 1 diabetes, limiting interpretation and generalizability. First, previous studies of coping in youth with type 1 diabetes have been limited by relatively small sample sizes and little diversity in samples. In many studies, broad categories of coping (e.g., approach/avoidance) [13] were used, while others measured specific coping strategies (e.g., daydreaming, use of humor) [11]. Coping researchers have questioned the utility of broad coping categories (e.g., emotion-focused/problem-focused), noting that they are neither exclusive nor exhaustive [33]. A strategy such as social support seeking, for example, does not easily fit within one category. Furthermore, a recent review of coping measures in adolescents highlights the need for consistent use of measures that have been developed for adolescents [34]. Results from the current study suggest that the Responses to Stress Questionnaire may be an effective way to measure diabetes-related coping in adolescents, given the strong associations with self-management and adaptation.
In conclusion, adolescents with type 1 diabetes experience chronic stress related to the burden of intensive treatment management, and it is important that we determine the most effective coping strategies for dealing with diabetes-related stress. Taken together, our results demonstrate the impact of coping on self-management and health outcomes in adolescents with type 1 diabetes, supporting the need for interventions that promote adaptive coping, with a focus on primary control coping and stress management strategies.
Acknowledgments
This research was supported by grant number R01-NR04009 from the National Institute of Nursing Research (PIs: Grey and Whittemore). Author Sarah S. Jaser was supported by awards from the National Institute of Diabetes and Digestive and Kidney Diseases (K23 NK088454) and the National Center for Research Resources (UL1 RR024139). The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official view of NIH. Clinical Trial Registry number: NCT00684658
Footnotes
Conflict of Interest Statement The authors have no conflict of interest to disclose.
Contributor Information
Sarah S. Jaser, Yale University School of Nursing, 100 Church Street South, PO Box 9740, New Haven, CT 06532, USA.
Melissa S. Faulkner, University of Arizona, Tucson, AZ, USA.
Robin Whittemore, Yale University School of Nursing, 100 Church Street South, PO Box 9740, New Haven, CT 06532, USA.
Sangchoon Jeon, Yale University School of Nursing, 100 Church Street South, PO Box 9740, New Haven, CT 06532, USA.
Kathryn Murphy, The Children’s Hospital of Philadelphia, Philadelphia, PA, USA.
Alan Delamater, University of Miami, Coral Gables, FL, USA.
Margaret Grey, Yale University School of Nursing, 100 Church Street South, PO Box 9740, New Haven, CT 06532, USA.
References
Full text links
Read article at publisher's site: https://doi.org/10.1007/s12160-012-9343-z
Read article for free, from open access legal sources, via Unpaywall:
https://academic.oup.com/abm/article-pdf/43/3/311/21991556/12160_2012_article_9343.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1007/s12160-012-9343-z
Article citations
A qualitative study on inner experience of self-management behavior among elderly patients with type 2 diabetes in rural areas.
BMC Public Health, 24(1):1456, 31 May 2024
Cited by: 1 article | PMID: 38822296 | PMCID: PMC11140989
Coping Styles and Cognitive Function in Older Non-Hispanic Black and White Adults.
J Gerontol B Psychol Sci Soc Sci, 78(5):789-798, 01 May 2023
Cited by: 0 articles | PMID: 36630289 | PMCID: PMC10174202
ISPAD Clinical Practice Consensus Guidelines 2022: Psychological care of children, adolescents and young adults with diabetes.
Pediatr Diabetes, 23(8):1373-1389, 05 Dec 2022
Cited by: 28 articles | PMID: 36464988 | PMCID: PMC10107478
Equity in Psychosocial Outcomes and Care for Racial and Ethnic Minorities and Socioeconomically Disadvantaged People With Diabetes.
Diabetes Spectr, 35(3):276-283, 15 Aug 2022
Cited by: 0 articles | PMID: 36082019 | PMCID: PMC9396713
Addressing the transition to a chronic condition: exploring independent adoption of self-management by patients with ANCA-associated vasculitis.
Rheumatol Adv Pract, 5(3):rkab075, 04 Nov 2021
Cited by: 1 article | PMID: 34778700 | PMCID: PMC8578693
Go to all (45) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Clinical Trials
- (1 citation) ClinicalTrials.gov - NCT00684658
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Associations of Coping Strategies With Glycemic and Psychosocial Outcomes Among Adolescents With Type 1 Diabetes Experiencing Diabetes Distress.
Ann Behav Med, 58(9):628-633, 01 Aug 2024
Cited by: 0 articles | PMID: 39014980 | PMCID: PMC11305127
Short-term effects of coping skills training as adjunct to intensive therapy in adolescents.
Diabetes Care, 21(6):902-908, 01 Jun 1998
Cited by: 105 articles | PMID: 9614605
Coping and psychological distress in mothers of adolescents with type 1 diabetes.
Matern Child Health J, 18(1):101-108, 01 Jan 2014
Cited by: 32 articles | PMID: 23420308 | PMCID: PMC3746006
Facilitating healthy coping in patients with diabetes: a systematic review.
Diabetes Educ, 39(1):33-52, 16 Oct 2012
Cited by: 58 articles | PMID: 23073967 | PMCID: PMC3549032
Review Free full text in Europe PMC
Funding
Funders who supported this work.
NCRR NIH HHS (1)
Grant ID: UL1 RR024139
NIDDK NIH HHS (2)
Grant ID: K23 DK088454
Grant ID: P30 DK092986
NINR NIH HHS (3)
Grant ID: R01-NR04009
Grant ID: R01 NR004009
Grant ID: R01 NR004009-16
PHS HHS (1)
Grant ID: K23 NK088454






