Abstract
Free full text

Getting Leukocytes to the Site of Inflammation
Abstract
There is no “response” in either the innate or adaptive immune response unless leukocytes cross blood vessels. They do this through the process of diapedesis, in which the leukocyte moves in ameboid fashion through tightly apposed endothelial borders (paracellular transmigration) and in some cases through the endothelial cell itself (transcellular migration). This review summarizes the steps leading up to diapedesis, then focuses on the molecules and mechanisms responsible for transendothelial migration. Surprisingly, many of the same molecules and mechanisms that regulate paracellular migration also control transcellular migration, including a major role for membrane from the recently described lateral border recycling compartment. A hypothesis that integrates the various known mechanisms of transmigration is proposed.
Getting leukocytes to the site of injury or infection is of prime importance, and an elaborate series of adhesion events between leukocytes and endothelium ensures that leukocytes leave the bloodstream only at the inflammatory site. In a sequence of adhesive steps, leukocytes attach to the vessel wall, locomote along the wall to the endothelial borders, traverse the endothelium and the subendothelial basement membrane, and migrate through the interstitial tissue.50,69 The inflammatory response is a double-edged sword. Most pathology involves inflammation that persists too long, is self-directed, and/or is in the wrong place at the wrong time. Therefore, careful regulation of the inflammatory response is critical for our wellbeing.
Transendothelial migration (TEM), the step in the inflammatory response in which leukocytes actually cross the endothelial cells lining the blood vessels at the site of inflammation, is a critical point in the regulation of this response. All of the benefit from the inflammatory response and almost all of the collateral damage take place once leukocytes leave the blood vessels. Most TEM takes place at endothelial borders (paracellular transmigration). Recently, there has been a flurry of interest in TEM through the endothelial cell body (transcellular migration). The mechanisms behind transcellular migration are less well established. This review first focuses on some general types of molecules and mechanisms that have been implicated in paracellular TEM and tries to show how these observations may be related. Then it reviews transcellular migration and makes a case that these 2 routes of transmigration may have more in common than originally thought. Some of this discussion has been borrowed from a recent review70 but updated here. Finally, in a brief section that I hope will be of special interest to veterinary pathologists, I discuss some problems with studying TEM in the most common experimental animal host: the laboratory mouse.
The Process of Leukocyte Extravasation
Circulating leukocytes move passively in the bloodstream swept along in the center of the channel by the laminar flow of blood. In postcapillary venules at sites of inflammation, local changes in hemodynamics result in greatly reduced blood flow rate. This increases the chances that leukocytes will make contact with the endothelial cells lining the vessel. Leukocyte adhesion molecules, whose expression on the surface of endothelial cells is induced by the inflammatory response, increase the chances that these contacts will lead to productive binding. Since the inflammatory response is capable of wreaking so much damage in the tissues, it is in the body’s best interest to have an elaborate series of checks in place before allowing leukocytes to enter tissue. Indeed, the series of adhesion events that are required for extravasation resemble a combination lock. The correct molecules must interact, and they must do so in the correct order within a short period of time (Fig. 1).
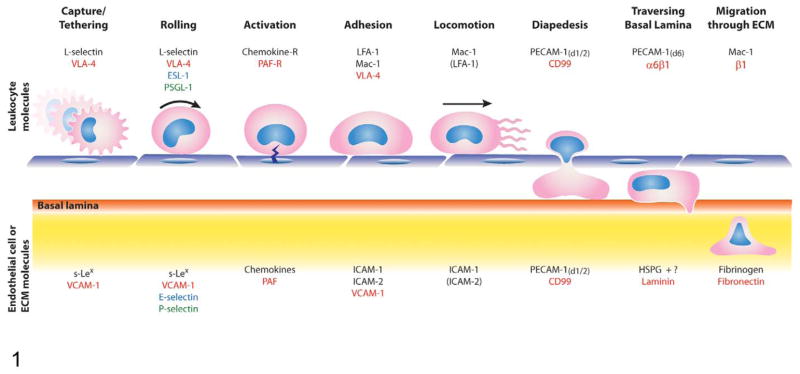
Sequential steps in leukocyte emigration are controlled by interactions between specific molecules on leukocytes and their counter-receptors on endothelial cells. The steps in leukocyte emigration described in the text are depicted schematically here. For each step, the molecules that interact between leukocyte and endothelial cell are printed in the same color. This diagram is not all-inclusive, and other molecules may mediate each of these events for distinct leukocyte types under different inflammatory conditions. Endothelial cells are depicted in blue and the leukocytes in pink with blue nuclei. Protrusions on the leukocyte surface in the capture/tethering step represent microvilli that bear L-selectin and very late antigen 4 (VLA-4). The lightning bolt at the activation step represents the triggering of inside-out activation of leukocyte integrins by signals from the endothelium and endothelial surface via G protein–coupled receptors. Parentheses around LFA-1 and ICAM-2 in the locomotion step indicate that these molecules have been shown to play a role in this step for monocytes in vitro but have not been verified in vivo. The basal lamina is depicted as the orange strip separating the underside of the endothelium from the remainder of the extracellular matrix (ECM). Many members of the β1 family of integrins are involved in migration through the ECM and are represented by “β1.” Most of the β1 ligands are not listed on the ECM side of this cartoon. ESL-1, E-selectin ligand 1; s-Lex sialyl-Lewis x antigen; VCAM-1, vascular cell adhesion molecule 1; PSGL-1, P-selectin glycoprotein ligand 1; LFA-1, lymphocyte function-associated antigen 1; Mac-1, macrophage-1 antigen; PAF, platelet activating factor; PAF-R, PAF receptor; ICAM, intercellular adhesion molecule; PECAM-1, platelet/endothelial cell adhesion molecule 1; PECAM-1 (d1/2), PECAM-1 domains 1 and 2 are responsible for this step; PECAM-1 (d6), PECAM-1 domain 6 is responsible for this step; α6β1, VLA-6, the integrin responsible for binding laminin; HSPG, heparan sulfate proteoglycan.
Histamine and other mediators of acute inflammation stimulate the translocation of preformed P-selectin from Weibel-Palade bodies to the luminal surface of endothelial cells. P-selectin interacts with selectin ligands on the leukocytes. Selectin ligands are sialylated fucosylated carbohydrate residues of the Lewis x blood group family (sialyl-Lewisx, sLex) attached to proteins. The best characterized of these selectin ligand carriers is P-selectin glycoprotein 1 expressed by leukocytes.63 However, any glycoprotein bearing the correct residue is a potential ligand for selectins. (For example, CD34 expressed by endothelial cells, when modified to bear selectin ligands, becomes an interacting partner for L-selectin on leukocytes.85) Binding interactions of selectins to their ligands have very fast on and off rates, which allow the rapidly moving leukocytes to be initially captured from the bloodstream and bind tentatively to the endothelium as they move along in a process aptly called rolling. Endothelium that has been activated by proinflammatory cytokines for several hours expresses an additional inducible selectin, E-selectin, which promotes “slow rolling” of leukocytes due to partial activation of integrins on the leukocyte.49,50
The purpose of rolling and slow rolling is to bring the leukocyte into contact with the endothelial cell so that the leukocyte can be further activated by chemokines and other proinflammatory agents presented on the surface of the endothelial cells. These chemokines, either made by the endothelium or by interstitial inflammatory cells and subsequently transported to the luminal side of the endothelium, bind to heparin sulfate glycosaminoglycans on the luminal surface.18,65 Contact of the chemokines with chemokine receptors (a subset of G protein–coupled receptors) on the leukocyte transduces signals within the leukocyte that lead to activation of leukocyte integrins. Integrins are a family of heterodimeric adhesion receptors that exist in the resting state in an inactive conformation.43 Activation of the integrins results in a conformational change that favors binding of their ligands.43,48 Since the integrins are activated by signals downstream of the chemokine receptors on the same cell, this is known as “inside-out” integrin activation.
Most members of the integrin family bind to extracellular matrix proteins. Leukocytes bear integrins of the β2 (CD18) family, whose ligands are expressed by endothelial cells. In particular, they bind to members of the immunoglobulin gene superfamily, intercellular adhesion molecules 1 and 2 (ICAM-1 and ICAM-2).31,43,122 Lymphocytes and monocytes bear an integrin of the β1 family (very late antigen 4 [VLA-4], CD49d/CD29, α4β1 integrin) that binds to vascular cell adhesion molecule 1 (VCAM-1).32,39,64 Once activated, leukocyte integrins bind tightly to their ligands on endothelial cells, allowing leukocytes to arrest on the endothelial surface. Experimentally, antibodies that block the function of selectins or their ligands or genetic deletion of the same prevents leukocyte rolling. Antibodies that block integrin function or genetic deletion of leukocyte integrins does not inhibit rolling but prevents firm adhesion of leukocytes to endothelium.
Adherent leukocytes crawl to nearby endothelial borders in preparation for extravasation. Interestingly enough, when observed directly by intravital microscopy, some leukocytes migrate upstream against the blood flow. Intraluminal crawling, or “locomotion,” is mediated by a subset of leukocyte integrins and endothelial cell adhesion molecules—namely, Mac-1 (CD11b/CD18) interacting with ICAM-1.79,92 For monocytes in vitro, at least, LFA-1 (CD11a/CD18) and ICAM-2 can support locomotion.92
TEM, or diapedesis, is the process whereby the leukocyte squeezes in ameboid fashion across the endothelial cells. This almost always happens at endothelial cell borders101,117 (a small fraction of transmigration occurs through the endothelial cell body; this will be discussed later). TEM is arguably the point of no return in the inflammatory response. The preceding steps of leukocyte rolling, activation, adhesion, and locomotion are all reversible, and most leukocytes that attach to the postcapillary venule at the site of inflammation reenter the circulation. However, once the leukocyte commits to diapedesis, it does not go back—at least not as the same cell type.72 (Recently, an exception to this rule has been demonstrated in vivo: In the setting of ischemia-reperfusion injury, almost 10% of neutrophils that crossed the endothelium soon migrated back into the circulation.117)
During TEM, the paradigms of leukocyte extravasation switch: Capturing, rolling, tight adhesion, and locomotion are all processes that involve interaction in 2 dimensions at the plane of leukocyte–endothelial cell interaction. Transmigration and the steps that follow involve interactions of the leukocyte in 3 dimensions as it moves across the endothelial cell, subendothelial basement membrane, pericytes, and interstitial tissue. The preceding adhesive events involve heterophilic adhesion (one molecule on the leukocyte binding to a different molecule on the endothelial cell), whereas transmigration largely requires homophilic adhesion of one molecule on the leukocyte interacting with the same molecule expressed by the endothelial cell. Platelet/endothelial cell adhesion molecule 1 (PECAM-1, PECAM, CD31) was the first molecule shown to play an exclusive role in mediating transmigration in vitro74 and in vivo.17,108 PECAM is expressed diffusely on the surfaces of most leukocytes and is concentrated at the borders of endothelial cells. CD99 has a similar distribution on endothelial cells and leukocytes, and homophilic interaction of CD99 on these cells has been shown to be required for TEM as well, both in vitro91 and in vivo.13,14,28 As expected, blockade of these molecules selectively blocks transmigration, without affecting the processes of rolling, tight adhesion, or locomotion. A more complete discussion of the molecular regulation of TEM is presented in the next section.
Postcapillary venules are surrounded by their own basal lamina and loosely invested by a discontinuous layer of pericytes—modified vascular smooth muscle cells. Once across the endothelial cell border, the leukocyte must still traverse these as well as the surrounding interstitial tissue to get to the site of inflammation. Relatively little is known about the molecular interactions involved in these processes. However, Nourshargh and colleagues demonstrated that following TEM, neutrophils111 and monocytes109 migrate through areas in the basement membrane where collagen IV and laminin 10 are expressed at relatively low density. This may be the path of least resistance, but the advantage of this could be to minimize the amount of proteolysis necessary to get these leukocytes to the site of injury. During this process, CD11a on the neutrophils interacting with ICAM-1 expressed by pericytes guides them as they seek out these low-density portals.80 Elongation of leukocyte tails as they exit the bloodstream has been noted by several observers. Recently, the molecular basis of this was identified. Adhesion of neutrophil LFA-1 (CD11a/CD18) to ICAM-1 (which could be on the endothelial cell or pericyte) keeps the trailing edge of the leukocyte relatively immobile, while the leading edge keeps moving forward using the integrin VLA-3 to bind to components of the extracellular matrix.44
Molecules Regulating TEM
Several endothelial molecules have been implicated in the control of diapedesis, including ICAM-1,120 VCAM-1,64 junctional adhesion molecules A77 and C77 (JAM-A and JAM-C), endothelial cell-selective adhesion molecule,113 PECAM,72 CD99,55,91 and CD99L2.15,90 Of these, PECAM and CD99 have been the most extensively studied for their role in transmigration and are known to have no role in the preceding step of firm adhesion, whereas several of the other molecules, notably ICAM-1, VCAM-1, and the JAM family, are known to be involved in the tight adhesion step that is a prerequisite for TEM, making their function in transmigration somewhat unclear. Since the focus of this review is on the diapedesis step, I now review the role of these molecules in TEM more extensively. Readers who are not interested in this level of detail may skip to the next section.
ICAM-1 is involved in firm adhesion of leukocytes to the apical surface of endothelial cells through interactions with leukocyte CD11a/CD18 and/or CD11b/CD18. Dimers of ICAM-1 on the endothelial surface (ie, in cis) are the preferential ligands for CD11/18.68,81 Once adherent, ICAM-1 becomes enriched under the leukocyte as it migrates to the endothelial cell border and continues to surround it during transmigration.95 The actin cytoskeleton is involved in this process; specifically, the Src-dependent phosphorylation of the actin-binding molecule cortactin is required for ICAM-1 clustering.120,121 VCAM-1 is involved in the firm adhesion of monocytes and lymphocytes bearing very late antigen 4 (VLA-4, CD49d/CD29).
VCAM-1 clustering has been observed in the steps leading up to diapedesis. Both ICAM-1 and VCAM-1 are enriched over actin-rich “docking structures” that form prior to TEM.10,22 Engagement of VCAM-1 activates intracellular calcium release and the small GTPase Rac-1. This in turn activates the endothelial NADPH oxidase Nox2.26 Reactions downstream of this have effects on the adherens junctions (see below).
ICAM-2, another LFA-1 ligand, is constitutively expressed on endothelial cells, where it is concentrated at cell borders but retains considerable surface expression. Antibodies against ICAM-2 do not seem to have a major effect on TEM in vitro, and compared to ICAM-1, ICAM-2 seems to play a lesser role.82 However, in some inflammatory models in vivo, blocking antibodies or genetic deletion of ICAM-2 inhibit transmigration of neutrophils.42,118
JAM-A is concentrated at endothelial cell borders. While it normally engages in homophilic adhesion, during inflammation it can bind to LFA-1 on the leukocyte.77 Blocking JAM-A on human endothelial cells using a polyclonal antibody in vitro has been shown to reduce TEM77; however, other investigators using polyclonal or monoclonal antibodies have seen no effect.52,92,95 Yet, in vivo studies show decreased inflammation61 and TEM118 when JAM-A is blocked. JAM-C is likewise concentrated at endothelial cell borders. It can engage in homophilic adhesion with JAM-C or heterophilic adhesion with JAM-B or CD11b/CD18. The latter interaction is implicated in TEM in vitro47 and in vivo.24 For an extensive review of the roles of JAM family members in the inflammatory response, the reader is referred to a recent review.112
Endothelial cell–selective adhesion molecule is molecularly related to the JAMs but has a long cytoplasmic domain. As its name implies, its distribution is mostly limited to endothelial junctions, but it is expressed on activated platelets.75 It binds homophilically, but a ligand on leukocytes has not been described. ESAM-deficient mice have no defect in lymphocyte extravasation, but had a transient decrease in neutrophil emigration (marked decrease at 2 hours that had recovered by 4 hours).113
PECAM-1 (CD31) is an Ig superfamily member concentrated at the borders of endothelial cells as well as expressed diffusely on platelets and leukocytes. Homophilic interaction of leukocyte PECAM with endothelial PECAM is required for TEM.57,74 Blockade with monoclonal antibody against the amino-terminal homophilic interaction domain, soluble PECAM-Fc chimeras, and genetic deletion of PECAM inhibit TEM in vitro and in vivo (reviewed in Muller72). When PECAM is transfected into cells that normally lack it, expression of PECAM imparts on them the ability to support TEM.27 This gain of function has not been demonstrated with other adhesion molecules. When PECAM–PECAM interactions are blocked, leukocytes are arrested tightly adherent to the apical surface of the cell51 and actively migrate along the junctions as if searching for a place to transmigrate.92 In vivo, at sites of inflammation, leukocytes are able to get to the postcapillary venules at the site of inflammation but are unable to transmigrate efficiently. They are seen in vastly increased numbers apparently adherent to the endothelial cell luminal surface,17,89 reminiscent of the block to TEM seen in vitro.51,74
CD99 is a relatively unique molecule unrelated to any other molecule in the human genome except the closely related paralog CD99-like 2 (CD99L2), which may have arisen from a common ancestral gene.100 The gene encoding CD99 is in the pseudoautosomal region of the human X chromosome.98 In mice, the region of the genome syntenic to the pseudoautosomal region of the human X chromosome is on chromosome 4,78 and this is where mouse CD99 is encoded. Similar to PECAM, homophilic interaction between CD99 at the endothelial cell border and CD99 on monocytes91 and neutrophils55 is required for transmigration. However, CD99 regulates a later step in transmigration than PECAM. Leukocytes in which PECAM has been blocked can still be prevented from transmigrating if anti-CD99 is added after the anti-PECAM block has been removed. Conversely, when CD99 interaction is first blocked, leukocytes can no longer be inhibited from transmigrating by anti-PECAM antibody when the anti-CD99 block is removed.91 In support of this, confocal images of leukocytes blocked in the act of transmigration by anti-CD99 show their leading edge under the endothelial cytoplasm, their cell body lodged at the border between endothelial cells, and the trailing uropod on the apical surface.55,91 As long as the block continues, they migrate along the junctions over the surface of the endothelium in this manner, unable to finish transmigration.55 There is indirect evidence that CD99 in fact cannot function unless PECAM acts first.27 Blocking antibodies against mouse CD99 inhibit inflammation in several animal models. Migration of T lymphocytes into skin13 and neutrophils and monocytes into the peritoneal cavity28 are blocked by interfering with CD99 function.
CD99L2 is a molecule ancestrally related to CD99. It is encoded by a gene on the X chromosome, as is CD99, but unlike CD99, the gene encoding CD99L2 is not in the pseudoautosomal region.78 CD99L2 expression in mice seems similar to that of CD99. That is, it is expressed on vascular endothelium of all tissues examined15,90 and is expressed at the borders of endothelial cells. It is expressed to varying degrees on all circulating blood cells. Only polyclonal antibodies against murine CD99L2 have been tested in vivo. They block neutrophil and monocyte influx in the thioglycollate peritonitis model.15,90 It is tempting to speculate that the incomplete blockade of inflammation seen when interfering with either CD99 or CD99L2 is due to partial redundancy of the function of these molecules.
VE-cadherin is the major adhesion molecule of the endothelial adherens junction. It negatively regulates transmigration. Antibodies against VE-cadherin enhance early migration into a site of inflammation in vivo.38 In vitro studies show that VE-cadherin is transiently removed from the site of transmigration at the cell junction.4,94 Mutation of the cytoplasmic tail of VE-cadherin so that it cannot interact with p120 or β-catenin or overexpression of p120 to outcompete the kinases that would phosphorylate it (see below) prevents clearance of VE-cadherin from the cell border and blocks transmigration.2,3
Mechanistic Considerations
Targeted Trafficking of the Lateral Border Recycling Compartment
Other endothelial molecules that have been shown to play a role in TEM by virtue of the inhibition of TEM by blocking antibodies include poliovirus receptor (CD155),83 MUC18 (CD146),9 activated leukocyte cell adhesion molecule (ALCAM/CD166),62 integrin associated protein (IAP/CD47),7,99 and nepmucin/CLM-9.46 When added to the well-characterized molecules discussed in the previous section, this raises the question of why so many molecules are required for TEM. Is this just an artifact of clogging up the junction with antibody or turning the cell junctions into immune complexes? This is unlikely, as most of these studies used control antibody, Fab or F(ab′)2 fragments, soluble recombinant adhesion mole- cules, siRNA knockdown, or genetic deletion to buttress their claims.
What if most of the endothelial molecules reported to control transmigration were part of a large multimolecular “transmigration complex” that combined to make a platform to support transmigration analogous to the way that multiple transcription factors and coactivators combine to make DNA accessible to transcription? Loss of or interference with any one of the molecules in that case could make the complex less efficient at supporting diapedesis and could account for the published results. The lateral border recycling compartment (LBRC) may be such a complex.
Even under steady state conditions, there is a considerable amount of membrane movement taking place at the endothelial cell borders. Membrane is internalized into and recycled from an interconnected reticulum of tubulovesicular structures that resides just beneath the plasma membrane of the endothelial cell borders.57 This compartment, which has come to be called the LBRC,58 is distinct from caveolae, typical recycling endosomes, and vesiculo-vacuolar organelles.57 By electron microscopy, most of the components appear to be 50-nm vesicles. About 30% of the cell’s PECAM resides in this compartment and recycles with a half time of about 10 minutes.57 This compartment also contains CD99 and JAM-A but not VE-cad-herin.59 In high endothelial venule endothelium, the Ig superfamily molecule nepmucin (CLM-9), which promotes lymphocyte TEM is in the LBRC.46
The purpose of the constitutive recycling is not known. However, when a leukocyte transmigrates, membrane from the LBRC is redirected (Fig. 2). It is targeted to and exteriorized at the cell border at the position where the leukocyte is transmigrating.57,58 Blocking homophilic PECAM-PECAM interactions between leukocyte and endothelial cell blocks targeted recycling from the LBRC and blocks transmigration. Moreover, there is accumulating evidence that targeted recycling from the LBRC is an essential step in TEM: LBRC membrane is trafficked to the site of transmigration by kinesin molecular motors along microtubules.58 Disrupting or bundling microtubules or inhibiting the motor domain of kinesin blocks targeted recycling and blocks TEM. Lymphocytes and activated lymphoblasts transmigrate in a manner that cannot be blocked by anti-PECAM antibodies.12,71 Nevertheless, transmigration of lymphoblasts can be efficiently blocked by disrupting targeted recycling of the LBRC.58 A tyrosine → phenylalanine mutation at residue 663 on the cytoplasmic tail of PECAM blocks the ability of PECAM to support TEM. This mutation interferes with the ability of PECAM to enter and leave the LBRC and markedly diminishes its ability to participate in targeted recycling.27
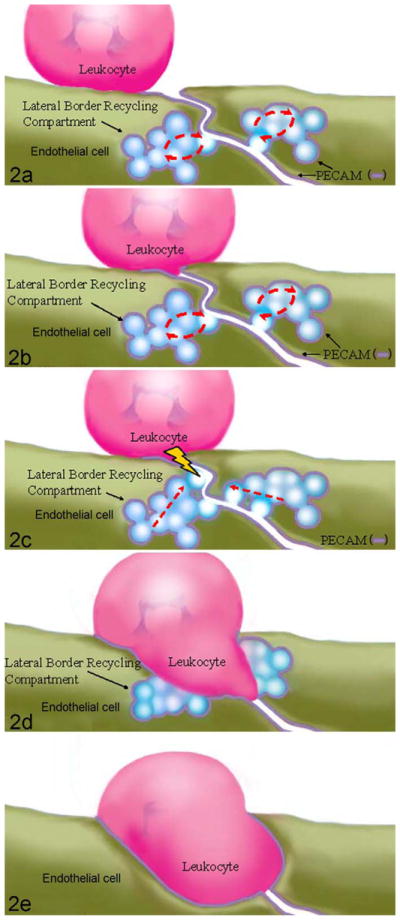
Schematic view of the movement of the lateral border recycling compartment (LBRC) during paracellular transmigration. Note: For Figures 2–4, the drawing is not to scale. Endothelial cell thickness is exaggerated to allow depiction of the LBRC and various signaling molecules. In reality the endothelial cell is ≤ 0.5 μm thick, while the leukocyte is ~7 – 10 μm in diameter. (a) Constitutive recycling of the LBRC is ongoing as the leukocyte locomotes toward the intercellular border. (b) Upon reaching the apical side of the endothelial border, leukocyte platelet/endothelial cell adhesion molecule (PECAM) engages endothelial cell PECAM, which is enriched in plasma membrane at the cell borders (and in the LBRC). (c) In cases of PECAM-dependent transmigration, leukocyte PECAM-endothelial cell PECAM interaction triggers a signal(s) (lightning bolt) that redirect recycling of the LBRC to the site of leukocyte engagement. In cases of PECAM-independent transmigration, some other interaction triggers this signal. (d) Membrane from the interconnected vesicles of the LBRC move to surround the leukocyte. (e) Recruitment of the LBRC continues as the leukocyte passes across the endothelial cell border. Modified from Wedlich D, ed. Cell Migration in Development and Disease. Fig. 13.2, page 246. Published 2005. Copyright Wiley-VCH Verlag GmbH & Co. KGaA. Reproduced with permission.
Targeted recycling of LBRC membrane during TEM potentially solves many of the “problems” inherent in the process. Rather than having to “unzip” high-density homophilic adhesions of VE-cadherin, PECAM, JAM-A, CD99, and so on, these molecules (and other structural components of the junction) may be pushed aside by membrane from the LBRC. This then presents unligated molecules that the leukocyte must interact with (eg, PECAM, JAM-A, CD99, nepmucin) on its path across the endothelial cell while removing structural barriers to transmigration (eg, the adherens junction complex of VE-cadherin and associated catenins). In fact, the absence of VE-cadherin from the LBRC could explain the observation that when a leukocyte crosses the endothelial border, VE-cadherin at the border appears to move out of the way.4,94 As the transmigrating leukocyte is surrounded by membrane coming from the LBRC, VE-cadherin at the cell border may be either diluted or pushed out of the way. Hypothetically, once the leukocyte has moved across the junction, the LBRC may be pulled back into the cell, allowing the other components to diffuse back into place, reestablishing the endothelial junction without having to reform all of the complex 3-dimensional interactions. VE-cadherin has been shown to undergo endocytosis via a clathrin-dependent pathway119; it is apparently not internalized into the LBRC.
Several other nonmutually exclusive events have been proposed to be critical for leukocyte transmigration.
Clustering Surface ICAM-1 and VCAM-1
The adhesion step immediately upstream of diapedesis is an obvious prerequisite for diapedesis, and there is reason to think that some of the events that occur during this step signal the events that regulate transmigration. Clustering of ICAM-1 and VCAM-1 on the endothelial cell has been observed as the leukocyte approaches the endothelial cell border.10,22 The initial leukocyte-facilitated clustering of ICAM-1 requires RhoA activation115 as well as Src-dependent phosphorylation of the actin-binding protein cortactin, which is also associated with actin filament remodeling that takes place during transmigration.121 In turn, ICAM-1 engagement or clustering induces Src-dependent phosphorylation of cortactin.30 This may be a self-amplification cycle: The initial recruitment of ICAM-1 and VCAM-1 may be due to adhesion to their leukocyte ligands. This clustering induces phosphorylation of cortactin, which leads to the actin polymerization and the recruitment of more ICAM-1 to the site of leukocyte adhesion, which induces more cortactin phosphorylation. Mice rendered genetically deficient for cortactin by homologous recombination display decreased leukocyte extravasation at sites of inflammation.93 Clustering of ICAM-1 and VCAM-1 stimulates signaling in the endothelial cells that promote diapedesis in ways that are discussed later.
Clustering of ICAM-1 and VCAM-1 is seen on “docking structures” or “transmigratory cups,” fingerlike projections of endothelial apical surface membrane reported to surround the lower portion of adherent leukocytes. The membrane is enriched in ICAM-1 and VCAM-1 and overlies cytoplasm enriched in f-actin and actin-binding proteins. Sanchez-Madrid and coworkers first used the term “docking structures” to describe these finger-like projections that engaged polyclonally activated lymphocytes and lymphoblasts adherent to cytokine-activated human umbilical vein endothelial cells (HUVEC).10 Subsequently, Carman et al19 demonstrated similar projections of ICAM-1 that seemed to rise up off the endothelial surface and surround at least the lower part and sides of leukocytes engaging cytokine-activated endothelial cells or ICAM-1-transfected CHO cells. Disruption of the cytoskeleton abolished these structures but had no effect on leukocyte adhesion. The authors commented that this might belie a role in transmigration. They referred to these structures, associated with both paracellular and transcellular migration, as “transmigratory cups.”22
However, not everyone who reports rings of ICAM-1 enrichment around transmigrating leukocytes has seen docking structures or transmigratory cups. For example, Ridley’s group, using a similar system, showed distinct ICAM-1 enrichment around transmigrating lymphoblasts but no docking structures.67 Luscinskas’s group also demonstrated local enrichment of ICAM-1 around transmigrating neutrophils undergoing transmigration95 and commented that they did not see such actin-rich microvilli.
What do these docking structures represent, and why are they not universally seen? One possibility is that they represent a response of the endothelial cell to leukocytes that are either highly activated or tightly adherent. The structures were seen under conditions where the leukocytes were adherent but could not transmigrate, allowing time for recruitment of additional ICAM-1 and/or VCAM-1 molecules10,104 or under which the leukocytes were additionally activated by the exogenous application of platelet activating factor or chemokines on the apical surface of the endothelial cells.19,22 One could easily imagine that under these conditions, enhanced leukocyte integrin activation could result in greater recruitment of counterreceptors from the endothelial surface. In contrast, under conditions where the transmigrating neutrophils95 or lymphoblasts67 were activated by interactions with the cytokine-activated endothelium without additional apical chemokine provided, ICAM-1 enrichment was not accompanied by formation of transmigratory cups.
Loosening the Junctions
Several lines of evidence show that loosening the endothelial cell junctions is important for efficient transmigration. Clustering of ICAM-1 and VCAM-1 on endothelial cells transmits a number of signals into the endothelial cell (reviewed in van Buul et al105), some of which appear to be relevant to diapedesis. Cross-linking VCAM-153 and ICAM-1105 on the endothelial cell stimulates an increase in cytosolic free calcium ions, which has long been known to be a requirement for diapedesis.41 The increase in cytosolic free calcium ion has been shown to activate myosin light chain kinase (MLCK), leading to actin-myosin fiber contraction. This is believed to help endothelial cells separate.40
Stimulation of ICAM-1 leads to phosphorylation of VE-cadherin, which is a prerequisite for adherens junction disassembly.103 In HUVEC the kinases Src and Pyk2 phos-phorylate VE-cadherin on the p120 and β-catenin binding sites, tyrosine residues 658 and 731, respectively.3 This inhibits the binding of p120 and β-catenin to VE-cadherin. Since the interaction of these proteins with VE-cadherin is critical for retaining VE-cadherin at the adherens junction, this destabilizes the junctions. Alternatively, if p120 is overexpressed, VE-cadherin levels at the cell border remain high, and transmigration is inhibited.2 The authors of that paper hypothesized that overexpression of p120 interferes with or outcompetes the kinases that would normally phosphorylate VE-cadherin on Y658 and inhibit p120 binding.
Cross-linking VCAM-1 also activates Rac1106 and stimulates an increase in reactive oxygen species in endothelial cells26 that leads to loosening of adherens junctions. In other systems Rac1 activation leads to phosphorylation of VE-cadherin on serine 665, which signals its clathrin-dependent internalization.36 The net result is “loosening” of junctional structures.
Under resting conditions the vascular endothelial protein tyrosine phosphatase (VE-PTP) associates with VE-cadherin via plakoglobin (γ-catenin), maintaining VE-cadherin in a hypophosphorylated state at the junction. Interaction of leukocytes with cytokine-activated endothelial cells triggers rapid dissociation of VE-PTP from VE-cadherin, allowing it to be phosphorylated on tyrosine, increasing junctional permeability and facilitating TEM.76 A role for another VE-cadherin accessory molecule, p120 catenin, has been demonstrated recently.2 Overexpression of p120 prevented VE-cadherin phosphorylation and the formation of “gaps” in VE-cadherin staining along the endothelial junction during engagement of leukocytes. (These gaps were not spaces between cells but disruption of the staining pattern of VE-cadherin.) This was associated with a significant decrease in transmigration. Interestingly, the authors did not find evidence for VE-cadherin internalization during gap formation.2
In a similar manner, clustering of ICAM-1 activates RhoA, which activates Rho kinase (ROCK) (reviewed in Cernuda-Morollon et al23). This in turn phosphorylates and inactivates protein phosphatase 1c (PP1c), the major phosphatase inactivating MLCK. The end result is potentiation of actin-myosin contraction. It is important to point out that although intercellular gaps that are visible in the light microscope can be produced on endothelial cells cultured on glass coverslips, in vivo the gaps produced between endothelial cells by even the strongest inducers of vascular permeability (eg, histamine and serotonin) are in the order of hundreds of angstroms,56 and these are resealed by the time most leukocytes are recruited. This does not mean that these gaps are not important, but it means that in vivo, leukocytes must still crawl through closely adherent endothelial cells; they do not fall into holes between endothelial cells.
While inflammation involves both increases in vascular permeability and leukocyte extravasation and these 2 phenomena both involve the same postcapillary venules, there is abundant molecular evidence that they are quite distinct phenomena and can be mechanistically (as well as temporally—see above) separated. Mice deficient in cortactin have leakier postcapillary venules and an exaggerated response to histamine, but their leukocytes extravasate less efficiently than wild-type mice.93 Vascular permeability was shown to be due to reduced levels of Rap1, while reduced leukocyte adhesion and transmigration were due at least partially to inability of ICAM-1 to efficiently form clusters in the plane of the membrane.93
A Unifying Model of Paracellular Transmigration
ICAM-1 and VCAM-1 signaling, cytosolic free calcium flux, RhoA and Rac1 activation, VE-cadherin removal from the junction, MLCK activation, and targeted recycling of the LBRC have all been shown to be necessary for efficient transmigration. How are these diverse phenomena related? Are they sequential links in a chain or events occurring in parallel with all required for TEM to occur? Considering that many second messenger signaling systems interact with each other and feedback loops exist, this may be a question of semantics. However, the following undoubtedly oversimplified scheme seems to be consistent with all of the published data and at least provides a testable hypothesis (Fig. 3).
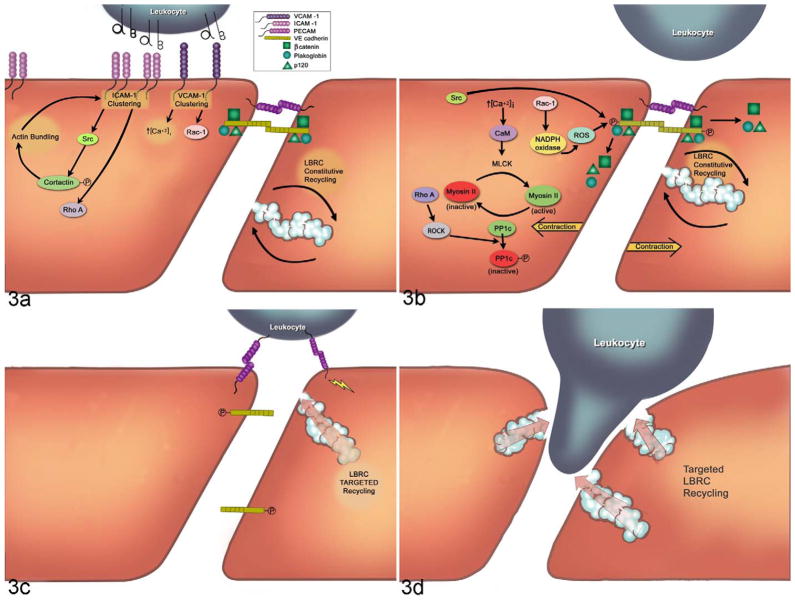
A unified schematic view of paracellular transendothelial migration. (See text for details and Figure 2 legend for note on the scale.) (a) Clustering of interecellular adhesion molecule 1 (ICAM-1) and vascular cell adhesion molecule 1 (VCAM-1) through engagement of their leukocyte integrin counterreceptors (αβ in diagram) initiates activation of Src, Rho A, and Rac-1, as well as increased cytosolic free calcium ion (↑[Ca+2]i). Phosphorylation of cortactin by Src stimulates f-actin rearrangements in the cortical cytoplasm, which facilitates more ICAM-1 clustering. (b) These signals lead to activation of myosin light chain kinase (MLCK), inactivation of protein phosphatase 1c (PP1c) through Rho kinase (ROCK), and phosphorylation of vascular endothelial specific cadherin (VE-cadherin), inducing release of the associated catenins (β-catenin, plakoglobin, p120). (c) Leukocyte PECAM engagement of endothelial cell PECAM and/or other leukocyte–endothelial cell interactions at the apical surface of the endothelial border activate kinesin molecular motors in the endothelial cell and stimulate targeted trafficking of lateral border recycling compartment (LBRC) membrane to the vicinity of the leukocyte. (d) Targeted trafficking of LBRC membrane continues as the leukocyte moves into the border between endothelial cells, now enlarged by the contribution of membrane from the LBRC. This process continues until transmigration is complete. CaM, calmodulin; ROS, reactive oxygen species; circled P, phosphorylated state. Reprinted by permission.70
LFA-1 preferentially binds to ICAM-1 dimers,68,81 which initiates clustering of ICAM-1. This stimulates phosphorylation of cortactin, enhancing the further actin-induced clustering of ICAM-1. This self-enhancing cycle leads to the enrichment of ICAM-1 around tightly adherent leukocytes. ICAM-1 multi-merization leads to increases in cytosolic free calcium and activation of RhoA (Fig. 3A).
In the meantime, if the leukocytes express VLA-4 and the endothelial cells are expressing VCAM-1, clustering of VCAM-1 also stimulates an increase in cytosolic free calcium, activation of Rac-1, and production of reactive oxygen species in endothelial cells.25,107 The latter activates protein kinase Cα (PKCα).1 The net result is loosening of endothelial cell junctions (Fig. 3A, 3B).
ICAM-1 and VCAM-1 signaling simultaneously result in weakening of the endothelial junctions due to effects on phos-phorylation of VE-cadherin. This dissociates VE-cadherin from its links to the actin cytoskeleton, and it potentially (but not necessarily) becomes subject to endocytosis in a clathrin-dependent manner (Fig. 3B).
The increase in cysolic free calcium activates MLCK to induce tension in the endothelial cells. The activation of MLCK is augmented by the inactivation of PP1 phosphatase mediated by the RhoA activation stimulated by signals originated through ICAM-1 clustering. The net result of contraction of the endothelial cell body against weakened junctions would be to allow easier passage of leukocytes (Fig. 3B).
With leukocytes poised over weakened adherens junctions, the other homophilic junctional adhesion molecules still hold the endothelial borders apposed. PECAM-PECAM interactions between leukocyte and endothelial cell57 or other signals58 stimulate targeted trafficking of LBRC membrane to surround the leukocyte (Fig. 3C). Targeted recycling of the LBRC may displace components of the adherens junction laterally, providing increased surface area and unligated molecules that the leukocytes want to interact with (Fig. 3D). It is possible, and even likely, that some of the many junctional molecules discussed earlier are also part of the LBRC or function to recruit it. That is, the LBRC may be one of the hypothetical multimolecular complexes controlling transmigration while other multimolecular complexes may function to recruit it to the site of TEM and reinternalize it after TEM.
The signals that trigger targeted recycling are not known, nor is it clear how the membrane is directed to the site of transmigration. However, weakening of the endothelial cell adherens junctions by brief calcium chelation leads to diffuse exteriorization of the LBRC along the endothelial cell border (unpublished data). It is possible that local weakening of the adherens junctions at the site of leukocyte engagement may allow for localized exteriorization of the LBRC.
Transcellular Migration
It is well accepted that leukocytes cross the endothelium at the cell borders (paracellular route), and direct in vivo observations show that in the cremaster muscle circulation, at least 90% of the transmigration events are clearly paracellular.101,117 However, there is increasing evidence that leukocytes can also pass directly through endothelial cells (transcellular route). This route may actually be favored at sights of tight endothelial junctions, such as at the blood-brain barrier. This section reviews what is known about transcellular migration, not because of its demonstrated physiologic importance, but because paracellular and transcellular migration have a great deal in common, and we may learn what is essential for transmigration by comparing the two.
Much of the original evidence for transcellular migration was indirect, based on single transmission electron micrographs that appeared to show leukocytes deeply indenting endothelial cells and/or passing across endothelial cells through a membrane-lined channel next to an intact junction.8,60,114 However, endothelial junctions are serpentine, and it was possible that the leukocyte was passing through a less structured junction.71 For a nice historical review of transcellular migration, the reader is referred to reference Sage and Carman.86 Transcellular migration was viewed with skepticism despite (or perhaps because of) the large amount of circumstantial evidence that supported it. The skeptics were to a great extent appeased by a paper published by the Dvorak lab in 1998.33 This provided arguably the first indisputable evidence of neutrophil transcellular migration in vivo. In these studies neutrophil emigration was stimulated by direct injection of formyl-methionyl leucyl phenylalanine (fMLP), a neutrophil chemoattractant and β2 integrin activator, into the skin of guinea pigs.33 The authors presented a collection of electron microscope serial sections in which neutrophils were shown to pass entirely across an endothelial cell without ever contacting a recognizable junction.33 Although the absolute frequency of transcellular migration was not addressed in this study, it demonstrated that transcellular migration was possible in vivo.
Recently, several in vitro models were established that produced reliable transcellular migration.22,59,67,120 These provided data on the molecules and mechanisms involved in this process. Perhaps surprisingly, many of the same molecules important for paracellular migration turn out to have a role in transcellular migration.
During transcellular TEM, ICAM-1 that is uniformly expressed on the luminal surface of HUVEC redistributes and is concentrated at the site of diapedesis. Furthermore, it is enriched in the membrane channel that surrounds the crossing leukocyte as it goes through the endothelial cell body.20,22,59,67,120 However, for transcellular migration, as for paracellular migration, some investigators58,95,120 do not observe the “docking structures” or “transmigratory cups” formed by projections of ICAM-1 above the plane of the endothelial cell membrane reported by others.10,22
In addition to ICAM-1, other molecules normally thought of to be restricted to the cell borders, including PECAM, JAM-A, and CD99 are seen around the leukocyte migrating transcellularly.20,22,59,67,120 In all cases, VE-cadherin is absent. These molecules are not only present but appear to be functional. Transcellular migration was found to be dependent on the “junctional molecules” PECAM and CD99. Blocking antibodies arrested transcellular migration.59 The reason for this may be explained by the mechanism, discussed below.
What Determines the Site of Transmigration?
Whether the leukocyte migrates paracellularly or transcellularly may depend on the relative tightness of the endothelial junctions and the ability of the leukocyte to breach them. Carman and Springer21 speculated that the leukocytes take the “path of least resistance” across the endothelium. If junctions are very tight, as for example, in the blood-brain barrier, migrating across the cell at a thin point may be easier, as seen in cerebral inflammation.54,116 However, that cannot be the only explanation since postcapillary venules, which are the sites of most inflammatory diapedesis (including transcellular migration33), have very leaky junctions. In fact, they are specialized for permeability, since this is the site of fluid reuptake from the interstitium.97 Endothelial cells in culture, where transcellular migration has been best demonstrated, form a monolayer of low electrical resistance even under the most optimal culture conditions.34
Transcellular migration may also occur if the leukocyte has difficulty reaching the junction, such as cells in which CD11b is nonfunctional92 or deficient.79 Phillipson et al79 reported that neutrophils deficient in CD11b/CD18 adhered to the endothelium at a site of inflammation but transmigrated poorly due to their inability to locomote along the endothelial surface. However, those that transmigrated tended to go transcellularly, perhaps because they achieved sufficient activation to transmigrate before they reached the cell border. Similarly, T cells deficient in the Rac activator Tiam1 are deficient in polarization and locomotion on endothelium and tend to migrate transcellularly.37
The Role of Leukocyte Activation
For low-resistance endothelia at least, transcellular migration may occur when leukocytes are highly and/or directly activated. The first indisputable evidence of neutrophil transcellular migration in vivo came from studies in which emigration was stimulated by direct injection of fMLP, a neutrophil chemoattractant and β2 integrin activator, into the skin of guinea pigs.33 The published in vitro studies of transcellular migration used monocyte chemotactic protein 1 (MCP-1), platelet activating factor, or stromal derived factor 1 (SDF-1) to stimulate migration of monocytes, neutrophils, and T cells, respectively,22 or employed mitogen-activated T lympho-blasts.21,67 Furthermore, these agents were added to the apical side of the endothelium where they would activate leukocytes but not provide a chemotactic gradient. In the standard TEM assay system in our lab,73 paracellular migration predominates and transcellular migration is almost never seen across cyto-kine activated HUVEC. However, when we applied chemokine or chemoattractant to the apical side of endothelial monolayers, 10% to 30% of leukocytes migrated transcellularly.59
Leukocyte activation would promote polymerization of actin in their lamellipodia, which has been associated with transcellular migration in vivo33 and shown to be necessary for transcellular migration in vitro.20 Leukocytes probe the apical surface of endothelial cells with “invasive podosomes” that contain polymerized actin. Podosomes deeply invaginated the surface in the areas of eventual transcellular migration.20
The Role of the LBRC
Membrane vesicles were seen accumulating in the region of transcellular migration.20 Millan et al reported that caveolin-1 accumulated in the regions of transcellular migration implying that these might be caveolae.67 However, other groups did not see any enrichment in caveolin-1 at the site of diapedesis.20,22,59
Mamdouh et al recently reported that the LBRC was critical for transcellular migration of leukocytes,59 similar to its involvement in paracellular migration. The LBRC membrane components PECAM, CD99, and JAM-A moved in concert to surround neutrophil and monocytes migrating transcellularly. The source of the membrane was demonstrated to be the LBRC and, similar to paracellular migration,58 was dependent on functioning microtubules.59 Microtubule depolymerizing agents blocked targeted recycling and blocked transcellular as well as paracellular migration.59
Using transfected cell lines, Yang et al showed that overexpression of ICAM-1 promoted transcellular migration,120 implicating a role for ICAM-1 in this process. However, when LBRC recycling was inhibited, there was no effect on ICAM-1 enrichment around adherent leukocytes, even though both paracellular and transcellular migration were blocked.59 Therefore, while enrichment of ICAM-1 may help promote transcellular migration and may even be a necessary prerequisite, it is not sufficient to promote transmigration in the absence of a functional LBRC.
The role of the LBRC in transcellular migration explains a number of observations made by several groups of investigators. The appearance in electron micrographs of membrane vesicles clustered around the leukocyte as it transmigrates20 is consistent with recruitment of the LBRC. Many of the studies that provide evidence for transcellular migration in vivo often show electron micrographs of leukocytes passing through the cell within a micron or two of an intact endothelial junction.54,116 This is exactly where the LBRC is situated and would put it in a prime location for its role in promoting transcellular as well as paracellular migration. Transcellular migration is also dependent on PECAM and CD99.59 Since expression of PECAM and CD99 on the cell surface is essentially restricted to the cell borders, this was unexpected. However, once the LBRC is recruited and becomes part of the membrane forming the transmigration pore, interaction of leukocyte and endothelial cell PECAM and CD99 is required for transcellular passage.
A Unifying Model of Transmigration
Paracellular migration involves an elaborate series of rolling, adhesion, and locomotion events designed to bring the leukocyte close to the endothelial border. Transcellular migration appears to use the same initial steps. However, for some reason the leukocytes migrate through the cell rather than at the border. A unifying mechanism may involve clustering of ICAM-1 and recruitment of the LBRC.
We speculate that a signal from the leukocyte may trigger recruitment of the LBRC to the sites of both paracellular and transcellular migration. It could be the same signal in both cases. If the leukocyte were so activated that it transmitted the signal prematurely before reaching the lateral border, the signaling cascade that sets the recruitment of the LBRC in motion might be directed to the apical surface of the cell where the leukocyte makes contact (Fig. 4). The fact that transcellular migration is more common among highly and directly activated leukocytes is consistent with this hypothesis. The mechanism by which the LBRC is redirected from the lateral border to the apical surface is not known. However, the clustering of ICAM-1 that precedes LBRC recruitment suggests that it might be involved in transmitting this signal through interactions with the leukocyte. Transcellular migration may also occur if the leukocyte has difficulty reaching the junction, such as cells in which CD11b is nonfunctional92 or deficient,79 cells that are unable to polarize,37 or vasculature in which the junction is particularly tight, such as the blood-brain barrier.54,116 A mechanism in which homophilic adhesion molecules such as PECAM, CD99, and JAM-A tightly engage leukocytes as they pass through the endothelial cell could allow leukocyte passage without plasma leakage. The LBRC could provide such a route.
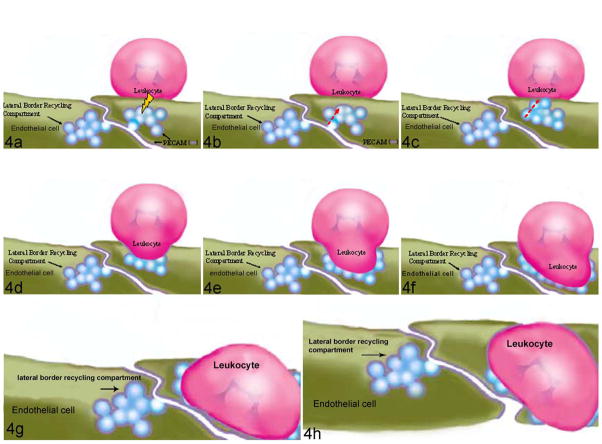
Schematic view of the movement of the lateral border recycling compartment (LBRC) during transcellular transmigration. (See Figure 2 legend for note on the scale.) (a) The signal that recruits targeted recycling to the vicinity of the leukocyte (lightning bolt) is given while the leukocyte is on the apical surface of the endothelial cell. (b) This causes targeting of the LBRC membrane along cortical microtubules toward the leukocyte. (c) A single fusion event may be sufficient to allow the entire interconnected LBRC to come into contact with the leukocyte. (d–f) As the leukocyte passes through the endothelial cell, additional LBRC membrane is recruited to surround the leukocyte. The transmigration pore is thus essentially a para-junctional junction lined by molecules the leukocyte needs to interact with (eg, PECAM, CD99, JAM-A) and lacking those it needs to bypass (eg, VE-cadherin and associated proteins). (g) At the basal surface a second fusion event may be necessary to allow the leukocyte to complete its migration (h) across the endothelial cell. Reprinted by permission.70
Carman et al20 showed leukocytes appearing to probe the endothelial surface with lamellipodia (podosomes), often deeply invaginating the surface of the endothelial cell. They were highly enriched for actin filaments,20,33 which were required for their function.20 Actin polymerization and lamellapodia formation are events triggered in leukocytes by integrin activation, so prominent podosomes in cells migrating transcellularly could be manifestations of high levels of leukocyte activation. The podosomes were hypothesized to initiate the formation of the transcellular channel. In previous reports such podosomes were observed invaginating the endothelial surface away from the junctions even under conditions where leukocytes crossed at the cell borders35,66 as well as under conditions where leukocytes were blocked in their attempts to cross at the junctions (Fig. 4a in Liao et al51). These lamellapodia may be a general mechanism for leukocytes to crawl across the endothelial surface. However, if they have a role in promoting transmigration, it is conceivable that they signal the recruitment of LBRC membrane to the leukocytes when they are at the cell borders as well as when they are not. In this case, the mechanisms of paracellular and transcellular migration would have even more in common.
At least one potential mechanistic difference between para-cellular and transcellular migration remains. Since the LBRC is connected to the lateral endothelial cell surface at the cell borders, fusion of the LBRC membrane with the plasma membrane is not necessarily required to bring the LBRC in contact with the leukocyte for paracellular TEM. Yet, to bring this membrane compartment in contact with the leukocyte on the apical surface for transcellular migration would require membrane fusion. In fact, Carman et al20 provide evidence that membrane fusion is required for transcellular migration. However, since the LBRC vesicles are connected to each other,57 rather than multiple fusion events involving dozens or hundreds of vesicles, the entire surface area of the LBRC could be brought to surround the leukocyte with perhaps only two fusion events necessary: One at the apical surface and one at the basal surface of the endothelial cell.
Epilogue: Of Mice and Mice
So much of what we think we know about the human immune system comes from studies on mice. The vast majority of those studies are performed on a single strain of inbred mice, C57Bl/6. What is more worrisome is that the immune response of this strain of mice is not even representative of mice, let alone humans.5,6,11,16,84,96 Their response is skewed toward the development of proinflammatory cytokines and Th1 type responses.45,87,102 They are handy for studies of inflammatory and immune diseases because they develop these readily. For example, deletion of the gene for low density lipoprotein receptor or apolipoprotein E will lead to atherosclerosis in mice fed a high fat diet, but the lesions are substantial only in C57Bl/6.
Blocking PECAM function using monoclonal antibodies, soluble PECAM-Fc chimeras, or genetic deletion leads to an arrest of TEM in every mouse strain tested except C57Bl/6.89,96 This mouse strain seems to be unique in that genetic deletion of PECAM or administration of blocking antibody or mouse PECAM-Fc to these mice has no effect in a variety of inflammatory models.29,88,89 Even the closely related C57BL/10 strain responds to anti-PECAM therapy.96 The ability to circumvent the need for PECAM in the thioglycollate peritonitis model of inflammation has been linked to a small locus at the proximal end of chromosome 2.96 Therefore, earlier studies carried out in C57BL/6 mice that found no role or only a minor role for PECAM in inflammation need to be re-evaluated. See Muller72 for a detailed discussion of the role of PECAM in various in vivo models, including species other than mice.
In response to some stimuli, blockade or genetic deletion of PECAM will arrest leukocytes in C57Bl/6 mice between the abluminal surface of the endothelium and the subendothelial basement membrane.14,29,118 There is a role for leukocyte PECAM via heterophilic interactions with basement membrane components in traversing the basal lamina.51,110
Likewise, it seems that CD99, the blockade of which arrests leukocytes partway through the endothelial junction in vitro and apparently on the surface of endothelium in vivo in the FVB/n strain,28 only exhibits a blockade at the level of the basement membrane in the C57Bl/6 strain.13,14 We speculate that this may be due to the fact that both PECAM and CD99 are major components of the LBRC, and the C57Bl/6 mice, due to their high proinflammatory state, have a way to bypass the requirement for PECAM and CD99 engagement to recruit the LBRC to the site of transmigration.
Acknowledgments
I wish to thank Dr David Sullivan and Ms Begum Kutay for preparing Figure 1.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: Supported by grants from the National Institutes of Health (R01HL046849 and R37HL064774).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Reprints and permission: sagepub.com/journalsPermissions.nav
References
Full text links
Read article at publisher's site: https://doi.org/10.1177/0300985812469883
Read article for free, from open access legal sources, via Unpaywall:
https://europepmc.org/articles/pmc3628536?pdf=render
Citations & impact
Impact metrics
Article citations
Impact of obesity‑associated myeloid‑derived suppressor cells on cancer risk and progression (Review).
Int J Oncol, 65(2):79, 28 Jun 2024
Cited by: 1 article | PMID: 38940351 | PMCID: PMC11251741
Review Free full text in Europe PMC
Effect of GLP-1RA Treatment on Adhesion Molecules and Monocyte Chemoattractant Protein-1 in Diabetic Patients with Atherosclerosis.
Life (Basel), 14(6):690, 28 May 2024
Cited by: 1 article | PMID: 38929672
Application and advances of biomimetic membrane materials in central nervous system disorders.
J Nanobiotechnology, 22(1):280, 23 May 2024
Cited by: 0 articles | PMID: 38783302 | PMCID: PMC11112845
Review Free full text in Europe PMC
Participation of Hepcidins in the Inflammatory Response Triggered by λ-Carrageenin in Gilthead Seabream (Sparus aurata).
Mar Biotechnol (NY), 26(2):261-275, 14 Feb 2024
Cited by: 0 articles | PMID: 38353762 | PMCID: PMC11043163
TIPE proteins control directed migration of human T cells by directing GPCR and lipid second messenger signaling.
J Leukoc Biol, 115(3):511-524, 01 Feb 2024
Cited by: 0 articles | PMID: 37952106 | PMCID: PMC10890839
Go to all (176) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Mechanisms of leukocyte transendothelial migration.
Annu Rev Pathol, 6:323-344, 01 Jan 2011
Cited by: 335 articles | PMID: 21073340 | PMCID: PMC3628537
Review Free full text in Europe PMC
The regulation of transendothelial migration: new knowledge and new questions.
Cardiovasc Res, 107(3):310-320, 17 May 2015
Cited by: 48 articles | PMID: 25987544 | PMCID: PMC4592322
Review Free full text in Europe PMC
Crossing the Vascular Wall: Common and Unique Mechanisms Exploited by Different Leukocyte Subsets during Extravasation.
Mediators Inflamm, 2015:946509, 19 Oct 2015
Cited by: 82 articles | PMID: 26568666 | PMCID: PMC4629053
Review Free full text in Europe PMC
Mechanisms of transendothelial migration of leukocytes.
Circ Res, 105(3):223-230, 01 Jul 2009
Cited by: 178 articles | PMID: 19644057 | PMCID: PMC2739407
Review Free full text in Europe PMC
Funding
Funders who supported this work.
NHLBI NIH HHS (4)
Grant ID: R37HL064774
Grant ID: R01HL046849
Grant ID: R01 HL046849
Grant ID: R37 HL064774





