Abstract
Free full text

Conservative management of symptomatic knee osteoarthritis: a flawed strategy?
Abstract
Conservative management of medial compartment knee osteoarthritis (OA) is a misleading term used to describe the application of medical, orthotic, and/or rehabilitative therapies exclusive of surgical interventions. The implication of this nomenclature is that these therapies offer satisfactory symptom relief, alter disease progression, and have limited side effects. Unfortunately, conservative therapeutic options possesses few, if any, characteristics of an ideal treatment, namely one that significantly alleviates pain, improves knee function, and reduces medial compartmental loading without adverse side effects. As uncompensated mechanical loading is a primary culprit in the development and progression of knee OA, we propose that the therapeutic perspective of conservative treatment should shift from pharmacological treatments, which have no influence on joint loading, minimal potential to alter joint function, substantial associated risks, and significant financial costs, towards minimally invasive load absorbing therapeutic interventions. A safe and effective minimally invasive medical device specifically engineered for symptomatic relief of medial knee OA by limiting joint contact forces has the potential to reduce the clinical and economic knee OA burden. This review characterizes the current standard of care recommendations for conservative management of medial compartment knee OA with respect to treatment efficacy, risk profile, and economic burden.
Introduction
Osteoarthritis (OA) is a disease characterized by progressive articular cartilage destruction, ultimately leading to disabling pain and joint dysfunction. The knee is the most commonly affected joint and knee OA represents the leading cause of disability in the adult population.1–3 More than 1 in 3 Americans over 60 years of age have radiographic evidence of knee OA and 1 in 8 have symptomatic knee OA.4 With the continued aging of the population and the alarming obesity epidemic, the prevalence of OA is expected to increase by 40% by 2025.5 OA is also responsible for a substantial economic burden, accounting for $128 billion per year in direct and indirect costs in the United States alone.6–8 Overall, the clinical and economic burden of OA is anticipated to increase and will remain a major medical problem for decades to come.
A wide variety of treatment options are available to the patient with knee OA, categorized as non-pharmacological, pharmacological, and surgical. Commonly utilized non-pharmacological treatments include weight loss, lateral wedge insoles, bracing, and physical therapy. Pharmacological treatments include analgesics, nonsteroidal anti-inflammatory drugs (NSAIDS), opioids, hyaluronic acid or corticosteroid injections, and various drugs purported as disease-modifying osteoarthritis drugs (DMOADs). Surgical options include arthroscopic debridement and lavage, high tibial osteotomy, and unicompartmental and total knee arthroplasty. Despite the fact that all of the 12 existing guidelines for knee OA management dictate that optimal management of OA requires a combination of non-pharmacological and pharmacological modalities,9 these conservative therapies have major limitations. Perhaps the most notable shortcoming of non-pharmacological and pharmacological treatment is a failure to successfully correct the underlying pathology - namely, abnormal joint loading resulting in continued disease progression. The purpose of this paper is to summarize the clinical evidence on conservative care for knee OA treatment and to identify the attributes of the ideal treatment regimen in this patient population.
The typical knee osteoarthritis conservative care regimen
Conservative options for knee OA treatment can be classified as orthotic joint unloading therapies, analgesics, anti-inflammatories, opioids, DMOADs, and hyaluronic acid injections. In general, joint unloading therapies such as weight loss, lateral wedge insoles, and bracing, are the preferred first-line treatments for symptomatic knee OA. If symptom improvement is not realized after an extended period, generally 3 to 6 months of use, add-on therapy utilizing analgesics such as acetaminophen is recommended. Topical NSAIDs and capsaicin are also recommended as alternatives to oral analgesics or in combination with them. If acetaminophen does not provide sufficient analgesia, oral NSAIDs at their lowest effective dose are recommended, with the caution that long-term use should be avoided whenever possible because of their association with gastrointestinal side effects. In patients with elevated gastrointestinal risk, COX-2 inhibitors or nonselective NSAIDs in combination with a proton pump inhibitor are recommended. If acetaminophen, nonselective NSAIDs, and COX-2 inhibitors all prove insufficient (or intolerable), DMAODs such as glucosamine sulfate, chondroitin sulfate, or diacerein may be attempted. Opioids, with or without acetaminophen, may be used if other oral analgesics fail, although stronger opioids are discouraged except when very severe pain is present due to concerns of dependency and complications. Intra-articular injections of hyaluronic acid are considered if oral medications fail to provide symptomatic relief.
While the frequency of joint unloading modality use is unknown, the prevalence of analgesic use in symptomatic knee OA patients is staggering. Over 650,000 patients in the US chronically consume NSAIDS and over 350,000 have a chronic opioid prescription. Additionally almost 3 out of 4 knee OA patients, representing 3 million patients, have used analgesics in the last month.4
Limitations of conservative care for knee osteoarthritis treatment
Despite the liberal prescribing of conservative care for knee OA, three major therapeutic limitations warrant re-examining this treatment paradigm: unsatisfactory clinical efficacy for pain relief, potential for side effects with pharmacological options, and inability to delay disease progression.
Ineffectiveness of conservative care for symptomatic knee osteoarthritis
Conservative care for knee OA has unsatisfactory overall efficacy. The Osteoarthritis Research Society International (OARSI) Treatment Guidelines Committee estimated the effect sizes of common treatments for OA knee pain and collated the number of published knee OA treatment guidelines that voted for or against widespread use of the therapy (Figure 1).10 For reference, the term effect size refers to the standardized mean difference of effects between two therapies divided by the pooled standard deviation and can be interpreted as trivial (<0.2), small (0.2–0.49), moderate (0.5–0.79), or large (≥0.8) effects.11
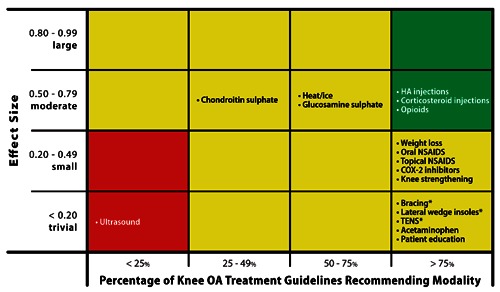
Relationship of effect size with degree of support from published guidelines for knee osteoarthritis (OA) treatments. Green shading represents characteristics of an ideal OA treatment, with moderate to large effect size and support from most (>75%) knee OA treatment guidelines. Red shading represents characteristics of an unsatisfactory OA treatment, with trivial to small effect size and support from few (<25%) knee OA treatment guidelines. Yellow shading represents characteristics of equivocal OA treatments, with effect size and knee OA treatment guideline support data not included in categories above. *Effect size not available.
Several noteworthy observations can be made from these data. First, many of the commonly prescribed knee OA treatments have poor efficacy. Second, of the five conservative treatments with moderate effect sizes, only HA injections and opioids are recommended by at least 75% of the knee OA treatment guidelines. Analgesics and NSAIDS are perhaps the most commonly utilized conservative care treatment with almost 3 out of 4 patients with symptomatic knee OA using them in the last month to manage pain.4 Unfortunately, the effect size of acetaminophen on knee OA pain is just 0.13, which implies a trivial clinical effect. The effectiveness of NSAIDS in pain amelioration is similarly poor with no statistical difference detected between subjects taking NSAIDS vs. placebo.12 The OARSI guidelines for viscosupplementation were guided by the results of a Cochrane review of 76 randomized trials published through 2006 that reported moderate effect sizes (range 0.54–0.61) at 1 to 4 weeks versus placebo for pain, function, and stiffness.13 However, clinical effectiveness diminished over time and, by 5 to 13 weeks, there was no evidence of benefit. Recently, a more comprehensive and timely analysis of the clinical effectiveness of viscosupplementation for knee OA has been published. Rutjes et al.14 identified 89 randomized controlled trials of viscosupplementation for knee OA published through January 2012. The authors concluded that viscosupplementation was associated with a short-term, clinically irrelevant benefit approximating a 0.9 cm improvement in pain severity on a 10-cm visual analogue scale. Additional observations with viscosupplementation for knee OA included even smaller effect sizes reported when outcome assessment was blinded and increased risks for serious adverse events (odds ratio 1.41).
The widespread adoption of these minimally effective conservative treatments should be a cause for concern. Although multimodal conservative therapy is widely advocated and unanimously supported by knee OA treatment position statements,15 this regimen is successful in less than 50% of patients after 12 weeks and,16 over 1 year, results in statistically significant, but practically minor improvements (effect size=0.3) in OA symptoms.17 Overall, there is a distinct mismatch between consensus knee OA treatment guidelines and best evidence data summaries derived from systematic reviews.
Risk of pharmacological treatments for symptomatic knee osteoarthritis
In addition to clinical ineffectiveness, use of pharmacological treatments is associated with an elevated risk of complications. The safety profile of acetaminophen is inconclusive,15 although some RCTs have reported associations with gastrointestinal bleeding,18 gastrointestinal-related hospitalization,19 and renal failure.20 Oral NSAIDS are associated with elevated risk of gastrointestinal side effects,21 gastrointestinal-related hospitalization,19 and myocardial infarction in comparison to placebo or no treatment.22 Opioids are strongly associated with deleterious effects including constipation, nausea, vomiting, dizziness, somnolence, dependence and risk of any complication,23,24 and, therefore, are generally reserved for patients with severe pain who do not respond to NSAIDS. Although COX-2 inhibitors result in fewer serious gastrointestinal side effects compared to NSAIDS,25 the risk of cardiovascular events is greater.22,26–28 Intra-articular HA injections have no known systemic risks although local adverse events such as pain and swelling are common.13,29 The risks associated with pharmacological treatment are particularly concerning in the elderly OA patient with several comorbidities who may be vulnerable to side effects from drug interactions.
Inability of conservative care to delay disease progression
The so-called joint-offloading therapies that are mainstays of symptomatic OA treatment paradoxically have the poorest clinical benefit (all effect sizes £0.2). In theory, weight loss, lateral wedge insoles, and bracing would be hypothesized to improve knee OA symptoms by reducing overall knee joint loading forces or by correcting joint malalignment. In practice, however, these modalities have limited usefulness. Intensive weight loss regimens in obese knee OA patients have resulted in lower peak knee forces on the order of 2 kg for every 1 kg body weight lost.30 However, weight loss is exceedingly difficult to maintain over the long-term with only 12% of participants maintaining at least 75% of lost weight and 40% actually gaining more weight than was lost 3 years following an intensive weight loss intervention.31 A 12-week study of multimodal therapy that encouraged knee OA patients with a body mass index >28 kg/m2 to lose at least 5% of body weight reported that only 14% of patients achieved this goal.16 Similarly, lateral wedge insoles and knee bracing provide no demonstrable clinical benefit on knee pain or disease progression, which may be partially attributable to poor compliance and patient discomfort.32–38
Pain amelioration accomplished with analgesics or anti-inflammatories has been shown to have no benefit on delaying OA progression and, paradoxically, some studies have reported that these therapies may actually encourage OA progression since presumably patients may be more active with higher resulting forces across the knee joint.39–42 This phenomenon, termed analgesic arthropathy, may be associated with any pain-relieving modality and is caused because pain is a protective mechanism that causes compensatory changes in gait patterns in order to reduce mechanical loading at the knee joint. Similar to findings with acetaminophen and NSAIDS, HA injections may actually increase medial compartment loading and accelerate joint deterioration.39 Corticosteroid injections are associated with reductions in knee pain, but no change in knee function, over 2 weeks; however, these clinical improvements disappear by 4 weeks.10 Considering their short therapeutic window and that corticosteroids can be safety injected up to just 4 times per year, intra-articular corticosteroids are not a viable treatment for reliable knee OA symptom relief.
Disease-modifying osteoarthritis drugs are those purported to modify joint structure, not just to alleviate pain. However, the results of DMOAD clinical trials are inconclusive, demonstrating the full range of positive and negative results.43 To date, no DMOAD has been approved by the FDA for the treatment of OA, which requires a demonstration of a structural and clinical benefit. Since articular cartilage is aneural and avascular, the symptoms of OA are generated by structures other than cartilage and, therefore, the primary target of DMAOD therapy appears to be misdirected.44 Even if DMOAD were to demonstrate successful reversal of cartilage degradation, the clinical meaningfulness of this finding is questionable given that OA affects all joint tissues including meniscus, synovium, and subchondral bone, not just articular cartilage.
Long-term consequences of chronic conservative care
Clinical implications of long-term conservative care
Long-term conservative care of knee OA results in little, if any, meaningful improvement in pain relief. Furthermore, no conservative care modality reliably retards OA progression. Regardless of which conservative measures are utilized, knee OA patients will variably, but predictably, experience disease progression, enter into a protracted treatment gap,45 and undergo TKA with the same frequency and at the same rate as if these measures were not employed.
A patient with knee OA and mild radiographic evidence of joint space narrowing will experience disease progression to a severity indicative of the need of TKA over a mean of 12 years, with over 75% of these patients advancing to this stage after 18 years.46 With an average age of OA symptom onset of approximately 60 years and a mean U.S. life expectancy of 78 years,47–50 over 75% of knee OA patients will eventually meet the radiographic criteria to warrant TKA. These patients will be forced to choose between undergoing TKA or, more commonly, refusing TKA at the expense of mobility and pain-free ambulation.51–53
In patients who elect to undergo arthroplasty for end-stage knee OA, the procedure reliably restores joint function and improves health-related quality of life.9 However, the procedure suffers from limitations. First, use of arthroplasty in elderly (>70 years) is associated with greater risk for perioperative complications versus their younger counterparts.54 Second, the lifespan of a TKA implant is poor in relation to the typical age of a TKA patient. From 1980 to 2006, the incidence of TKA has exponentially increased in patients aged 50 to 59 years.55 In fact, over 4.5 million Americans currently have an intact total knee prosthesis, including 5% of those 50 years and older.56 Given the earlier onset of knee OA and performance of TKA, the typical 10–15 year survival of a TKA implant, the continued aging of the population, the soaring rates of obesity, and the greater levels of residual pain after TKA in younger patients,57 it can be anticipated that many younger TKA patients will ultimately require revision surgery, a procedure with greater complication rates and lower treatment success rates compared to first-time TKA. Clearly, employing therapeutic strategies that delay or obviate the need for TKA would result in enormous clinical, economic, and societal benefits.
Economic implications of long-term conservative care
The economic burden of long-term conservative care is enormous. The estimated cost effectiveness of typical conservative modalities for knee OA treatment is listed in Table 1.58–62 Overall, knee OA treatments must be particularly cost effective in order for the typical patient to consider utilizing the therapy. Unfortunately, no known conservative treatment for knee OA has a cost per quality adjusted life year (QALY) below the commonly cited willingness to pay threshold of $1200 to $5700 per QALY in knee OA patients.58 This conclusion is confirmed by a systematic review reporting only limited evidence of cost effectiveness for conservative treatment of knee OA.63
Table 1
| Conservative modality | Cost effectiveness (Cost/QALY) |
| Maximum willingness to pay for knee osteoarthritis patients | $ 1200-570058 |
| Knee bracing | $ 600059 |
| Primary care weight loss program | $ 11,00059 |
| Intra-articular hyaluronic acid | $ 14,00060 |
| Nonsteroidal anti-inflammatory drugs | $ 15,00059 |
| COX-2 inhibitors | $ 71,00061 |
| Oxycodone | $ 76,00062 |
Unavailable cost-effectiveness data for acetaminophen, intra-articular corticosteroids, opioids, DMAOD, and lateral wedge insoles.
Direct costs attributable to conservative care modalities are considerable. OA patients spend $173 per year on medications and average 3.3 office visits per year.64 Viscosupplementation treatments cost $1700 to $3700 annually.65 As OA progresses, the cost of treatments concomitantly rises. The 3.6 million patients in the United States with end-stage knee OA spend almost $4000 per year on associated conservative treatments,45–58,63–66 resulting in $14.4 billion in annual costs. Despite the considerable costs of conservative care, these therapies arguably result in mediocre pain amelioration with no demonstrable change in disease progression. An ideal knee OA treatment would utilize the principle of reducing knee joint loading forces and would be initiated when early signs of radiographically confirmed knee OA are first identified. If such a therapy were developed, disease progression could be slowed, the need for joint arthroplasty could be delayed or obviated, and billions of dollars in annual costs for conservative therapies with limited clinical usefulness could be avoided.
Characteristics of the ideal knee osteoarthritis treatment
Unfortunately, no therapeutic option is available that possesses the characteristics of an ideal knee OA treatment, namely one that alleviates knee pain, improves knee function, reduces affected joint compartment loading without load transfer to adjacent joint surfaces, enjoys high patient acceptance, and is cost effective.67 A widely held position is that abnormal mechanical loading is the main culprit in the development of OA and, therefore, no drug can feasibly encourage healing until the underlying aberrant biomechanical malalignment issues are addressed.68–70 The fact that knee joint malalignment is an independent risk factor for knee OA in numerous studies is supportive of this hypothesis.71 Minimally invasive medical devices are widely used across many therapeutic areas and could potentially serve to fill this therapeutic void.70
OA onset and progression is largely influenced by excessive loading forces across the knee joint.72,73 Furthermore, unloading the knee of these forces may heal damaged cartilage.74 Therefore, it is intriguing to envision a minimally invasive implant that would improve patient symptoms, slow disease progression, and, ultimately, delay or obviate the need for TKA. Some have argued that adequate joint unloading may even renew or restore damaged tissue to normal.70,74 Such a therapy could reduce the reliance on TKA, with concomitant reductions in the associated clinical and economic burden of end-stage OA. A primary advantage of a minimally invasive implant over conservative unloading therapies is that the limitation of poor patient compliance is obviated.
Early interpositional devices utilized free-floating technology with anteroposterior motion of the implant and rotation during flexion and extension. However, the lack of appropriate fixation resulted in an unacceptably high number of device dislocations and revision surgeries.75–77 Extra-capsular (non-articular) medial compartment knee load absorber implants are currently under evaluation in clinical trials that require only a subcutaneous incision and provide device fixation at the medial distal femoral cortex and the medial proximal tibial cortex to achieve significant offloading of the medical compartment.78,79 Continued advancements in minimally invasive, joint offloading medical devices for knee OA treatment are intriguing, especially given the overall failure of conservative management to improve symptoms or halt disease progression.
Conclusions
Conservative care for knee OA is neither clinically effective for pain or disease progression nor cost effective within the constraints of the typical patient's willingness to pay. The decade-long search for a safe and efficacious DMOAD continues with disappointing results and does not address the fundamental causative factor of abnormal joint loading. New treatment modalities for knee OA should be pursued given the stagnation in new efficacious offerings. The minimally invasive medical device market is an ideal arena to explore the concept of a joint unloading device that meets all of the characteristics of an ideal knee OA treatment.
References
Articles from Orthopedic Reviews are provided here courtesy of Open Medical Publishing
Citations & impact
Impact metrics
Article citations
Effectiveness of Internet-Based Telehealth Programs in Patients With Hip or Knee Osteoarthritis: Systematic Review and Meta-Analysis.
J Med Internet Res, 26:e55576, 30 Sep 2024
Cited by: 0 articles | PMID: 39348685 | PMCID: PMC11474128
Review Free full text in Europe PMC
Case report: Equine metacarpophalangeal joint partial and full thickness defects treated with allogenic equine synovial membrane mesenchymal stem/stromal cell combined with umbilical cord mesenchymal stem/stromal cell conditioned medium.
Front Vet Sci, 11:1403174, 22 May 2024
Cited by: 0 articles | PMID: 38840629
Equine Musculoskeletal Pathologies: Clinical Approaches and Therapeutical Perspectives-A Review.
Vet Sci, 11(5):190, 26 Apr 2024
Cited by: 1 article | PMID: 38787162 | PMCID: PMC11126110
Review Free full text in Europe PMC
A Finite Element Model to Investigate the Stability of Osteochondral Grafts Within a Human Tibiofemoral Joint.
Ann Biomed Eng, 52(5):1393-1402, 06 Mar 2024
Cited by: 0 articles | PMID: 38446329 | PMCID: PMC10995060
Effectiveness of Ultrasound-guided versus Anatomical Landmark-guided Genicular Nerve Block to Treat Chronic Knee Osteoarthritis: A Retrospective Cohort Study.
Oman Med J, 38(5):e550, 28 Sep 2023
Cited by: 0 articles | PMID: 38225997 | PMCID: PMC10788927
Go to all (43) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Intra-articular viscosupplementation with hylan g-f 20 to treat osteoarthritis of the knee: an evidence-based analysis.
Ont Health Technol Assess Ser, 5(10):1-66, 01 Jun 2005
Cited by: 3 articles | PMID: 23074461 | PMCID: PMC3382385
Arthroscopic lavage and debridement for osteoarthritis of the knee: an evidence-based analysis.
Ont Health Technol Assess Ser, 5(12):1-37, 01 Sep 2005
Cited by: 6 articles | PMID: 23074463 | PMCID: PMC3382413
The KineSpring(®) Knee Implant System: an implantable joint-unloading prosthesis for treatment of medial knee osteoarthritis.
Med Devices (Auckl), 6:69-76, 17 May 2013
Cited by: 12 articles | PMID: 23717052 | PMCID: PMC3663478
Review Free full text in Europe PMC
The pathophysiology of osteoarthritis: a mechanical perspective on the knee joint.
PM R, 4(5 suppl):S3-9, 01 May 2012
Cited by: 59 articles | PMID: 22632700 | PMCID: PMC3635670
Review Free full text in Europe PMC




