Abstract
Importance
Clear guidelines on the health effects of dairy food are important given the high prevalence of obesity, cardiovascular disease and diabetes, and increasing global consumption of dairy food.Objective
To evaluate the effects of increased dairy food on cardio metabolic risk factors.Data sources
Searches were performed until April 2013 using MEDLINE, Science Direct, Google,Embase, the Cochrane Central Register of Controlled Trials, reference lists of articles, and proceedings of major meetings.Study selection
Randomized controlled studies with healthy adults randomized to increased dairy food for more than one month without additional interventions.Data extraction and synthesis
A standard list was used to extract descriptive, methodological and key variables from all eligible studies. If data was not included in the published report corresponding authors were contacted.Results
20 studies with 1677 participants with a median duration of dietary change of 26 (IQR 10-39) weeks and mean increase in dairy food intake of 3.6 (SD 0.92) serves/day were included. Increased dairy food intake was associated with a modest weight gain (+0.59, 95% confidence interval 0.34 to 0.84kg, p<0.0001) but no significant change in waist circumference (0.35 , -0.75 to 1.45 cm); insulin resistance (HOMA –IR -0.94 , -1.93 to 0.05 units); fasting glucose (0.87, -0.27 to 2.01 mg/dl); LDL-cholesterol (1.36 ,-2.38 to 5.09 mg/dl); HDL-cholesterol (0.45, -2.13 to 3.04 mg/dl); systolic (-0.13, -1.73 to 1.98 mmHg) and diastolic blood pressure (0.13, -1.73 to 1.98 mmHg) or C-reactive protein (-0.08, -0.63 to 0.48 mg/L). Results were similar for studies with low-fat and whole-fat dairy interventions.Limitations
Most clinical trials were small and of modest quality. .Conclusion
Increasing whole fat and low fat dairy food consumption increases weight but has minor effects on other cardio-metabolic risk factors.Trial registration actrn
Australian New Zealand Clinical Trials Registry ACTRN12613000401752, http://www.anzctr.org.au.Ethics approval number
NTX/10/11/115.Free full text

Effects of High and Low Fat Dairy Food on Cardio-Metabolic Risk Factors: A Meta-Analysis of Randomized Studies
Abstract
Importance
Clear guidelines on the health effects of dairy food are important given the high prevalence of obesity, cardiovascular disease and diabetes, and increasing global consumption of dairy food.
Objective
To evaluate the effects of increased dairy food on cardio metabolic risk factors.
Data Sources
Searches were performed until April 2013 using MEDLINE, Science Direct, Google,Embase, the Cochrane Central Register of Controlled Trials, reference lists of articles, and proceedings of major meetings.
Study Selection
Randomized controlled studies with healthy adults randomized to increased dairy food for more than one month without additional interventions.
Data Extraction and Synthesis
A standard list was used to extract descriptive, methodological and key variables from all eligible studies. If data was not included in the published report corresponding authors were contacted.
Results
20 studies with 1677 participants with a median duration of dietary change of 26 (IQR 10-39) weeks and mean increase in dairy food intake of 3.6 (SD 0.92) serves/day were included.
Increased dairy food intake was associated with a modest weight gain (+0.59, 95% confidence interval 0.34 to 0.84kg, p<0.0001) but no significant change in waist circumference (0.35 , -0.75 to 1.45 cm); insulin resistance (HOMA –IR -0.94 , -1.93 to 0.05 units); fasting glucose (0.87, -0.27 to 2.01 mg/dl); LDL-cholesterol (1.36 ,-2.38 to 5.09 mg/dl); HDL-cholesterol (0.45, -2.13 to 3.04 mg/dl); systolic (-0.13, -1.73 to 1.98 mmHg) and diastolic blood pressure (0.13, -1.73 to 1.98 mmHg) or C-reactive protein (-0.08, -0.63 to 0.48 mg/L). Results were similar for studies with low-fat and whole-fat dairy interventions.
Limitations
Most clinical trials were small and of modest quality. .
Conclusion
Increasing whole fat and low fat dairy food consumption increases weight but has minor effects on other cardio-metabolic risk factors.
Trial Registration ACTRN
Australian New Zealand Clinical Trials Registry ACTRN12613000401752, http://www.anzctr.org.au
Ethics Approval Number
NTX/10/11/115
Introduction
Clear guidelines on the health effects of dairy food are important given the high and increasing prevalence of obesity[1], cardiovascular disease [2] and diabetes[3] in most countries, and the increasing global consumption of dairy food[4]. Many current dietary guidelines promote low fat dairy as a healthy food[5,6]. This advice is supported by observational studies which report that increased dairy consumption is associated with lower blood pressure[7-11], weight reduction [12], improved insulin sensitivity[7,11,13,14], less inflammation [15,16] and a lower ratio of total to HDL cholesterol[17]. A modest inverse association between dairy consumption and cardiovascular disease has also been reported[18-20].
In contrast, whole fat dairy is not recommended in most food guidelines [21-23] because of the concern that saturated fat in dairy food may have an adverse effect on serum lipids which could increase the risk of cardiovascular disease. Despite these guidelines the effects of high fat dairy food on the risk of obesity, diabetes and cardiovascular disease are uncertain. A recent meta-analysis found no association of dietary saturated fat intake and the risk of cardiovascular disease[24]. Whole fat dairy foods contain many fatty acids, which may have favorable as well as unfavorable effects on lipids and other cardio-metabolic risk factors[25]. Also, effects of reducing saturated fat from one food are determined by other dietary changes, including carbohydrates, and mono-unsaturated and poly-unsaturated fatty acids[17].
The effects of a high dairy food diet on diabetes and cardiovascular disease have not been evaluated in randomized clinical outcome trials. The large long term randomized dietary intervention studies which evaluated the ‘Dietary Approaches to Stop Hypertension’ (DASH) [26] and ‘Mediterranean’ [27] diets on clinical outcomes, while including increased low fat dairy food in the intervention, do not allow an evaluation of the independent effects of changes in dairy food intake. Health effects of whole and low fat dairy food would be more reliably evaluated in clinical trials than in observational studies, and by assessing a number, rather than just one cardio-metabolic risk factor. We therefore undertook a meta-analysis of randomized clinical studies that evaluated effects of changing whole and low fat dairy food intake in healthy adults on a broad range of cardio-metabolic risk factors including weight, insulin resistance, lipids, blood pressure and c- reactive protein (CRP).
Methods
We followed the PRISMA (http://www.prisma-statement.Org ) guidelines throughout the design, implementation, analysis, and reporting of this meta-analysis. See Checklist S1 and File S1 for the PRISMA checklist and flow chart, respectively. A protocol for the study was designed and is available as File S2. The study was registered with the Australian New Zealand Clinical Trials Registry, with trial registration number ACTRN12613000401752.
Search Strategy
We searched for all trials that randomized adults to increased dairy for at least one month without additional interventions (e.g. caloric restriction, multiple dietary interventions), had an appropriate control group, and sufficient data to calculate estimates of effect with standard deviations on at least one of the following: weight, waist circumference, blood pressure, HDL and LDL cholesterol, fasting glucose, insulin resistance and C-reactive protein. Studies were excluded if they were observational or otherwise non-randomized; were commentaries, reviews, or duplicate publications from the same study. We restricted to studies of healthy adults who did not have diabetes, hypertension or vascular disease. Both feeding and dietary advice trials and studies with a crossover or parallel group study design were included.
Searches were performed of literature published through March 2013 using Medline, Science Direct, Google, Embase, the Cochrane Central Register of Controlled Trials, reference lists of articles, and proceedings of major meetings for relevant literature. The search terms were ‘dairy’ and each of the following; ‘cardio metabolic risk’, ‘weight’, ‘waist circumference’, ‘glucose’, ‘insulin’, ‘insulin resistance’, ‘inflammation’, ‘inflammatory markers’, ‘blood pressure’, ‘cholesterol’ and ‘lipids’.
Assessment of study eligibility and data extraction
One reviewer screened all abstracts and titles and, upon retrieval of candidate studies, two team members (JB, KS) reviewed the full text to determine eligibility. If the study was eligible, data were abstracted by JB. Through an iterative process, a standard list was used to extract descriptive, methodological and key variables from all eligible studies. Data extracted included years the study was performed and reported, the primary aim of the study, population characteristics, funding source, control and intervention diets, duration of follow-up, estimates of effect and standard deviations. If data was not included in the published report corresponding authors were contacted [28,29]. The quality of each study was rated using the Jadad score[30]. Questions arising during data abstraction were resolved by discussion with all team members.
Definitions
Dairy food with less 1% fat, such as trim or low fat milk was categorized as a low fat dairy food. Dairy food that included full fat milk (3-4% fat), cheese, butter, cream and ice cream, was categorized as whole fat dairy food..
The method used to quantify insulin resistance was the homeostatic model assessment- Insulin resistance (HOMA-IR)[31]. This estimates steady state insulin sensitivity as units. The equation that is used is HOMA-IR = glucose (mmol/L) x insulin (munits/L) ÷22.5.
Statistical analysis
Each cardio-metabolic risk factor when on a higher and lower dairy diet was compared between cases and controls from the same study. For those studies with 3 treatment groups, comparison was made between the control and the high dairy food group. Effects were measured at least 4 weeks after randomization, with the final results used for studies with more than one measurement during follow up. A negative effect size means that dairy has a favorable effect on the cardio metabolic risk factor. Because increase in HDL-cholesterol is considered beneficial, positive and negative exponents were switched to maintain consistency in presentation. In one study the standard deviation was not reported [32] but calculated from the 95% confidence intervals.
For each cardio-metabolic risk factor the weighted mean change from baseline to follow up was calculated across all included studies within each randomized group. The inverse-variance method, whereby study differences are weighted according to the reciprocal of their variance, was used to pool all standardized mean differences to yield an overall effect size with corresponding 95% confidence intervals.
When SD were not available, the mean weighted standard deviation of the group was used. For studies that used standard error of the mean (SEM) , this was converted to SD.
Each meta-analysis was assessed for heterogeneity by a Chi square test and I2 statistic. A fixed effects model was used when heterogeneity was not present (I2=0) and a random effects model was used when statistical heterogeneity (I2≥1%) was present. A p-value of <0.05 was considered statistically significant. Studies are presented in Forrest plots in order of statistical power. Stratified analyses was studied by low fat and whole fat dairy, duration of dietary intervention (less than or greater than 6 months), body weight of study participants, and industry or public source of funding. Studies where the intervention was skim, trim or <1% dairy food are low fat dairy studies. Sensitivity analyses were also conducted to evaluate the impact of selected studies on overall pooled estimates and heterogeneity. The Statistical analyses were performed using RevMan software version 5·2 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen).
Results
Search Results
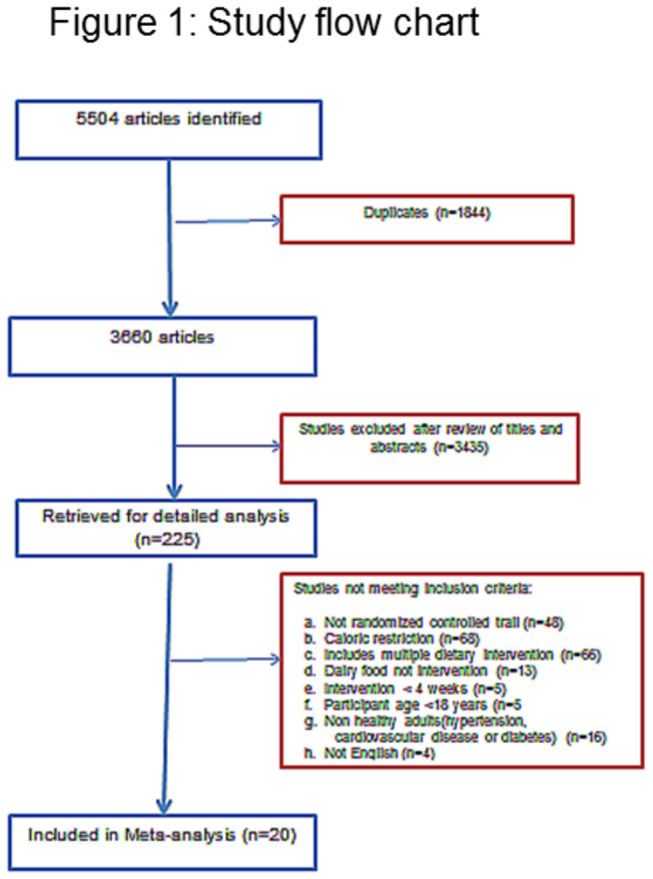
The literature search yielded 5504 citations (2495 on Pub Med and 2849 on Science Direct,160 on Google), of which included 1844 duplicates. After title and abstract screening, the full text of 225 articles were evaluated, with 205 excluded either because the intervention included caloric restriction or had multiple dietary changes, or the study was in a population with disease (Figure 1). Twenty studies were included in the meta-analysis.
Characteristics of studies
Characteristics of the 20 included trials which included 1677 participants are summarized in Table 1. The average age was 51 (SD 16) years and 78% of participants were female. The median duration of follow up was 26 (IQR 10-39) weeks. The average difference in dairy intake between groups was 3.12 (SD 0.62) standard serving sizes /day. Within studies there was no imbalance between randomized groups. One crossover study [28] had a higher dropout rate for subjects initially randomized to low compared to high dairy intake (49% vs. 22%).
Table 1
| Trial Year published | Country | Population | Mean BMI (kg/M2) | Funding source | Number of subjects (% female) | Mean Age years (SD) | Design | Length of intervention (Weeks) | Primary outcome | Low dairy | High Dairy (+ serves /day) | Jadad Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alonso[32] 2009 | Spain | Normotensive college students | 23.6 | Public | 45 (60%) | 19·9 (1·5) | Crossover | 8 | Blood pressure and weight | 1·5 serves/day | 3·5 whole-fat | 2 |
| Baran[46] 1990 | America | Healthy volunteers | 22.8 | Industry | 37 (100%) | 36.5 (3.4) | Parallel | 156 | Bone density | Usual diet | 2.5 whole-fat or low-fat dairy | 2 |
| Barr[29] 2000 | North America | Healthy volunteers | 25.8 | Industry | 198 (64%) | 65·2 (6·7) | Parallel | 12 | Weight, blood pressure, lipids | Usual diet | 3 low-fat dairy | 3 |
| Benatar[45] 2014 | New Zealand | Healthy volunteers | 24.6 | Public | 120 (75%) | 46·3 (12·0) | Parallel | 4 | Weight, blood pressure | Usual diet | 3·5 whole-fat or low-fat dairy | 3 |
| Chee[36] 2003 | Malaysia | Postmenopausal Chinese woman | 23.8 | Industry | 173 (100) | 59·0 (3·2) | Parallel | 104 | Bone loss | Usual diet | 2 low-fat dairy | 3 |
| Crichton[28] 2012 | Australia | Overweight and obese volunteers | 31.5 | Public | 36 (83) | 47·3 (15·1) | Crossover | 26 | Weight | ≤1 serves/day | 4 low-fat dairy | 2 |
| Eagan[37] 2006 | North America | Normal weight young women | 22.5 | Industry | 37 (100) | 20·0 (2·0) | Parallel | 26 | Fat mass | Usual diet | 3 whole-fat or low-fat dairy | 2 |
| Gardner[47] 2007 | North America | Healthy volunteers | 26.0 | Industry | 28 (79) | 52(9) | Crossover | 4 | Lipids | Usual diet | 2·5 low-fat dairy | 3 |
| Ghadirian [35] 1995 | Canada | Postmenopausal nuns | 23.0 | Industry | 158(100%) | 79 (9.5) | Parallel | 4 | Uric acid | 0 | 3.6 whole-fat or low-fat dairy | 2 |
| Gunther [38] 2005 | North America | Healthy woman | 22.2 | Industry | 99 (100) | 20·0 (2·1) | Parallel | 52 | Weight | Usual diet | 3 low-fat dairy | 2 |
| Kukuljan [34] 2009 | Australia | Older men (>50years) | 27.6 | Public | 89(0%) | 60.9 (7.5) | Parallel | 52 | Bone Density | Usual diet | 1.7 low-fat dairy | 2 |
| Lau[39] 2001 | China | Postmenopausal women | 22.2 | Industry | 185 (100) | 57·0 (1·8) | Parallel | 104 | Bone loss | Usual diet | 2 low-fat dairy | 3 |
| Manios[33] 2009 | Greece | Postmenopausal women | 30.4 | Industry | 62(100) | 61.2 (4.9) | Parallel | 52 | Weight | Usual diet | 3 low-fat dairy | 2 |
| Palacios[40] 2011 | Puerto Rico | Obese adults | 38.5 | Public | 16 (81) | 37·0 (2·2) | Parallel | 21 | Weight, lipids | Usual diet | 4 whole-fat or low-fat dairy | 1 |
| Stancliffe[41] 2011 | North America | Overweight and obese with metabolic syndrome | 30.7 | Industry | 40 (53) | 37·0 (9·9) | Parallel | 12 | Inflammatory markers | 0·5 serves /day | 3·5 whole-fat or low-fat dairy | 2 |
| Tardy[42] 2009 | France | Healthy women with abdominal obesity | 32.6 | Public | 39 (100) | 36·4 (7·7) | Parallel | 4 | HOMA | Usual diet + vegetable oils | 3 whole-fat | 2 |
| Van Meilj[49] 2010 | Holland | Overweight adults | 32.0 | Industry | 35 (71) | 49·5(13·2) | Crossover | 8 | Blood pressure, Lipids, inflammatory marker, glucose | Usual diet | 3 low-fat dairy | 2 |
| Wennersberg[43] 2009 | Scandinavia | Metabolic syndrome | 30.0 | Industry and Public | 105 (67) | 51·2 (8·0) | Parallel | 26 | Waist circumference | Usual diet | 3-5 whole-fat or low-fat dairy | 2 |
| Zemel[48] 2010 | North America | Obese and overweight adults | 30.0 | Industry | 20 (30) | 31·0 (10·3) | Crossover | 4 | Inflammatory markers | 0 | 3 low-fat dairy | 3 |
| Zemel (phase 1)[44] 2005 | North America | Obese adults | 34.9 | Industry | 34 (59) | 41·7 (2·8) | Parallel | 26 | Weight | Usual diet | 3 whole-fat or low-fat dairy | 1 |
Sixteen studies had a parallel group design and 4 were cross-over studies. In 10 studies increased dairy food included whole fat dairy, while 10 only low fat dairy food was advised. Fifteen of the studies were at least partly funded by the dairy or food industry.
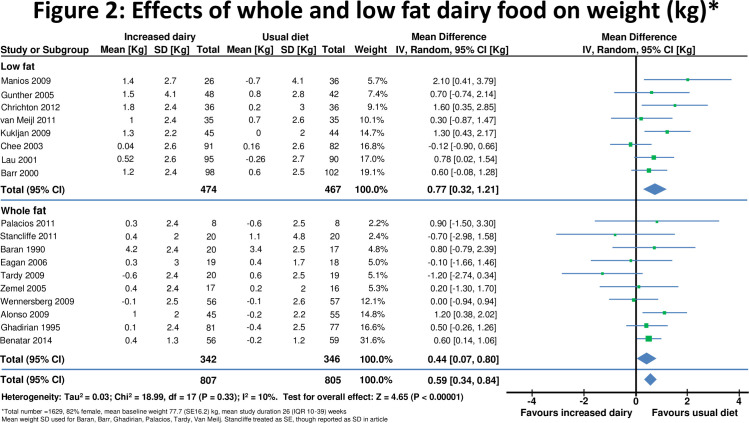
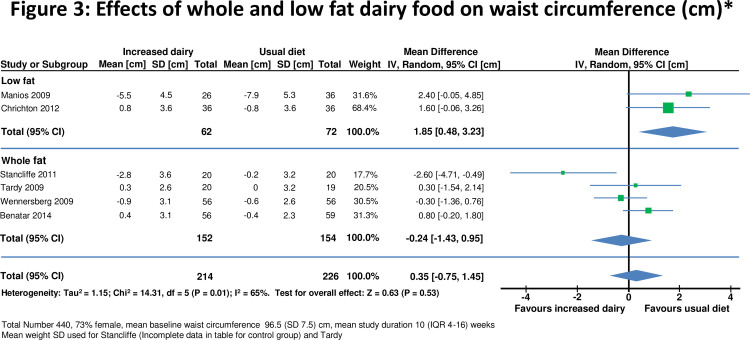
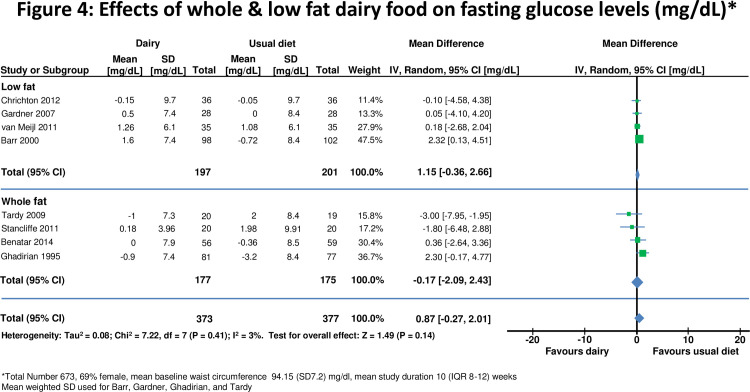
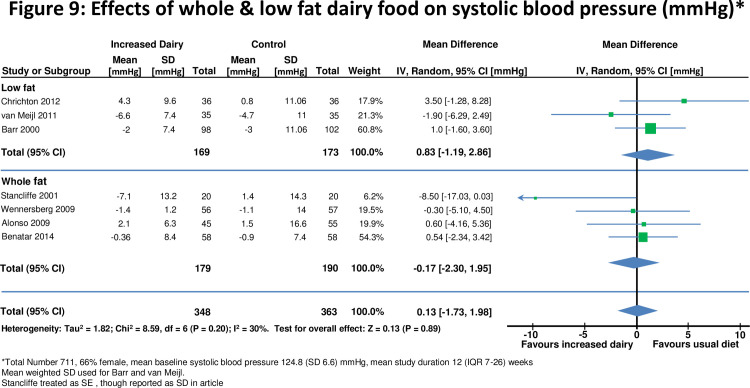
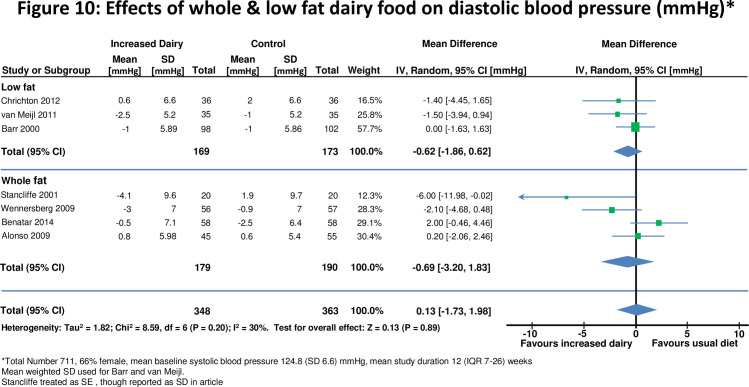
Change in risk factors on a high and a lower dairy diet in all studies combined are displayed in Figures 2-10. Results stratified by duration of intervention, participant body weight and by funding source are displayed in table 2.
Table 2
| Metabolic risk factors | Diet Change <6 months duration | Diet change ≥ 6 months duration | Normal weight (BMI <25 kg/m2) | Overweight or obese (BMI > 25kg/m2) | Industry funded studies | Public funded studies |
|---|---|---|---|---|---|---|
| Total number of studies | 10 | 10 | 8 | 12 | 14 | 6 |
| Total number of subjects | 738 | 982 | 854 | 823 | 1246 | 431 |
| Weight (kg) | +0.64* (0.35 to 0.92) | +0.58* (0.10 to 1.07) | +0.57* (0.29 to 0.85) | +0.67* (0.22 to 1.13) | +0.41* (0.09 to 0.72) | +0.79* (0.47 to 1.11) |
| N | 738 | 891 | 895 | 534 | 1198 | 431 |
| Waist circumference (cm) | -0.34 (-2.23 to 1.55) | +1.01 (-0.66 to 0.85) | +0.80 (-0.25 to 1.85) | -0.24 (-1.20 to 1.68) | -0.24 (-2.56 to 2.07) | +0.89 (-0.09 to 1.69) |
| N | 194 | 246 | 115 | 325 | 214 | 226 |
| HOMA- IR (units) | -1.32 (-2.84 to 0.20) | 0.00 (-0.45 to 0.45) | -0.12 (-0.4 to 0.24) | -1.29 (-2.90 to 0.32) | -1.59 (-4.77 to 1.59) | -0.39* (-1.02 to 0.24) |
| N | 195 | 75 | 116 | 154 | 115 | 155 |
| Fasting Glucose (mg/dl) | +0.05 (-0.01 to 0.12) | -0.01 (-0.18 to 0.17) | +0.09 (-0.01 to 0.19) | +0.02 (-0.06 to 1.10) | +0.07 (0.00 to 0.14) | +0.01 (-0.13 to 0.10) |
| N | 601 | 72 | 196 | 477 | 524 | 226 |
| LDL-cholesterol (mg/dl) | +0.94 (-2.97 to 4.85) | +2.67 (-8.49 to 13.83) | +7.3* (2.34 to 12.26) | 1.13 (-3.85 to 1.59) | -1.65 (-3.98 to 7.27) | +1.14 (-4.66 to 6.94) |
| N | 480 | 222 | 115 | 587 | 460 | 242 |
| HDL-cholesterol (mg/dl) | -1.33 (-3.52 to 6.19) | +0.64 (-2.71 to 1.43) | 4.63 (-2.34 to 11.60) | -0.95 (-2.72 to 0.81) | -0.86 (-3.01 to 1.29) | 2.37 (-3.19 to 7.94) |
| N | 443 | 221 | 155 | 509 | 419 | 245 |
| C- reactive protein (mg/L) | -0.55 (-1.26 to 0.16) | +0.11 (-0.77 to 0.98) | +1.18 (-0.68 to 3.04) | -0.43 (-1.01 to 0.14) | -0.41 (-1.00 to 0.17) | 0.62 (-0.99 to 2.23) |
| N | 268 | 183 | 116 | 335 | 265 | 186 |
| Systolic blood pressure (mmHg) | +0.48 (-1.39 to 2.36) | +1.76 (-1.95 to 5.47) | +0.57 (-1.37 to 2.51) | -1.05 (-2.62 to 0.52) | -1.44 (-3.15 to 0.28) | +0.64 (-1.10 to 2.37) |
| N | 526 | 185 | 216 | 495 | 423 | 288 |
| Diastolic blood pressure (mmHg) | +0.56 (-1.91 to 3.02) | +0.74 (-1.78 to 3.25) | +0.56 (-1.91 to 3.02) | +0.74 (-1.78 to 3.25) | -0.01 (-2.87 to 2.85) | +1.29 (-0.85 to 3.42) |
| N | 526 | 185 | 216 | 495 | 423 | 423 |
Effects on body weight
Eighteen [10,28,29,32-46] studies reported effects on weight in 1629 individuals (Figure 2). The mean body mass index (BMI) at baseline was 25.6(SD 6.2) kg/m2 and weight 77.7(SD 16.2) kg. Increased dairy intake was associated with a modest weight gain (+0.59, 95% confidence interval 0.34 to 0.84kg, p<0.0001). In six studies[28,33,41-43,45] in 440 individuals waist circumference did not change significantly(0.35 , -0.75 to 1.45cm) (Figure 3).
Weight gain was observed both in studies which increased low fat (+0.77, 0.32 to 1.21 kg, p<0.001) and whole fat dairy food (+0.44, 0.07 to 0.80kg, p=0.04). Modest weight gain was also observed in 10 studies (n= 692) which included overweight and obese subjects (+0.66, 0.04 to 1.29kg, p=0.04) and in 8 studies (n= 937) of normal weight participants (+0.60, 0.35 to 0.85kg, p<0.001).
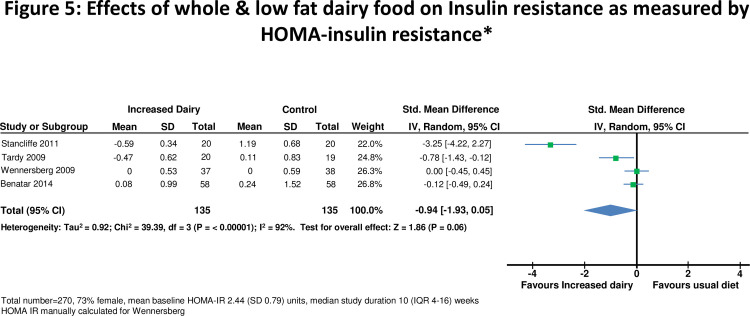
Effects on insulin resistance
In 8 studies [10,28,29,35,41,42,45,47], there was no significant change in fasting glucose on higher compared to lower dairy diet (Figure 4). Four studies [41-43,45] assessed effects on HOMA-IR in 270 subjects (Figure 5). One [42] did not report standard deviation so a weighted mean standard deviation from the other studies was used. HOMA-IR was recalculated in one study which used incorrect units [43]. For all studies combined HOMA-IR was slightly improved on the high dairy diet (-0.94, -1.93 to 0.05 units, p=0.06). However there was heterogeneity between studies (I2 =92%), accounted for by the two smallest studies [41,42] which reported reduced insulin resistance on the high dairy diet (-1.37, -1.64 to -1.10 units). HOMA-IR was similar on high and low dairy diets in the two larger studies[43,45] (-0.05, -0.26 to 0.17 units). HOMA-IR did not change significantly for studies stratified by body weight, duration of intervention or high versus low fat dairy (Table 2).
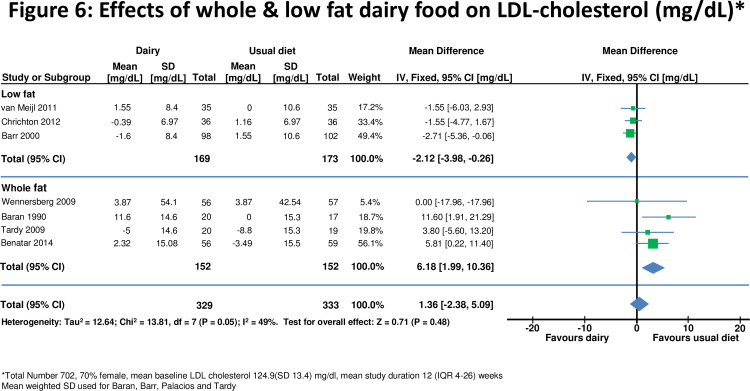
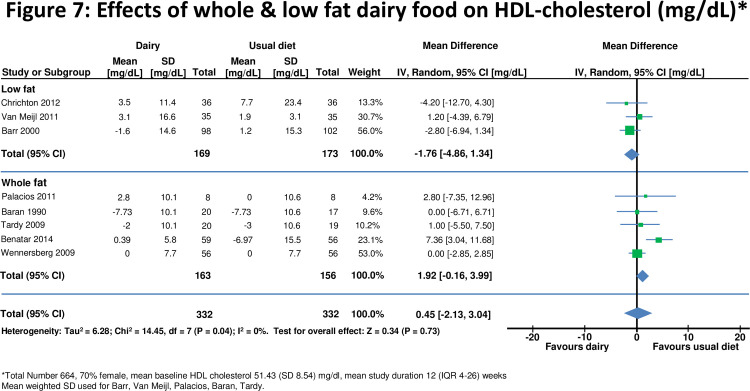
Effects on LDL and HDL cholesterol
Eight studies [10,28,29,40, 42, 43,45,46] assessed effects on LDL- and/or HDL-cholesterol (n=664 for HDL, n=662 for LDL). For all studies combined there was no significant change in either LDL or HDL-cholesterol after increasing dairy food (Figures 6 and and7).7). Effects of HDL-cholesterol were consistent (I2=0%) across studies, but there was heterogeneity for LDL-cholesterol (I2=49%). There was no change in LDL cholesterol when whole fat dairy (+6.18, 1.99 to 10.36 mg/dl) or low fat dairy (-2.12, -3.98 to -0.26 mg/dl) food was increased (Figure 6). Results were similar for shorter and longer periods of dietary intervention and for studies which included normal and overweight or obese participants.
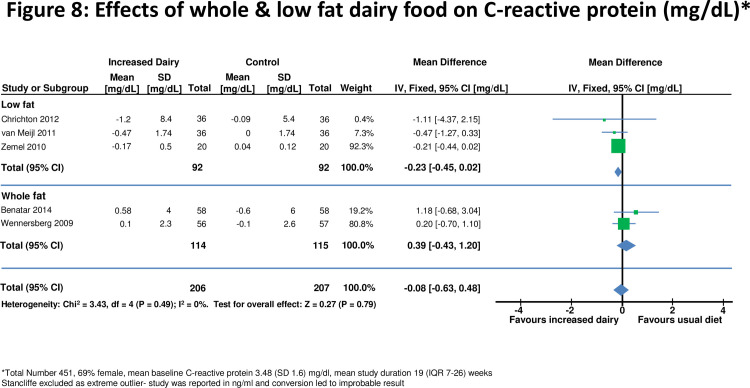
Effects on C-reactive protein
Five studies[28,43,45,48,49] assessed effects on C-reactive protein in 400 individuals (Figure 8). For all studies combined there was no significant change in C-reactive protein on a high dairy diet (-0.08, -0.63 to 0.48 mg/dL). However two smaller studies [41,48] reported significant reductions in C-reactive protein with increased dairy intake. There was no evidence for effects on C-reactive protein when studies were stratified by duration of dietary intervention, high and low fat dairy, or normal or overweight subjects (Table 2).
Effects on blood pressure
Seven studies [10,28,29,32,41,43,45,49] assessed effects on blood pressure in 711 participants (Figures 9 and and10).10). For all studies there was no significant change in either systolic blood pressure or diastolic blood pressure. There was also no evidence for effects on blood pressure when studies were stratified by duration of dietary intervention, high and low fat dairy or normal or overweight subjects.
Evaluation of heterogeneity and sensitivity analysis
Industry sponsored studies were more likely to report favorable effects on risk factors than non-industry sponsor studies (Table 2). Results were also similar when analysis was repeated excluding the 4 cross-over studies. Funnel plots identified that the study by Stancliffe [41] reported decreases in LDL cholesterol, HOMA-IR, C-reactive protein and waist circumference on the increased dairy diet beyond the 95% confidence range for all studies combined (see S2 File in the accompanying notice [67]). This study also reported the greatest decrease in blood pressure and weight of all studies. Excluding this study in a sensitivity analysis substantially decreased heterogeneity, but overall effects were similar, and there was no other consistent difference between smaller and larger studies. The study by Manios[33] was the only study that fell outside the 95% confidence interval for weight, though excluding the study had no overall effect on results. This study had an imbalance in randomization with fewer people randomized to high dairy food (n=30) compared to the control group (n=40). The study by Ghadirian[35] was outside the 95% confidence interval for fasting plasma glucose. In this study, the control group had a statistically significant reduction in fasting plasma glucose, with little change for the high dairy group. Analysis repeated excluding this study showed no overall effect (+0.02,-0.05 to 0.09mmol/L, p=0.56) and a reduction in heterogeneity (25→0%).
On the basis of a funnel plot and Begg’s test, no significant publication bias was shown in the meta-analysis of body weight, waist circumference, insulin resistance, blood pressure, lipids and C-reactive protein.
Discussion
This systematic analysis of randomized dietary intervention trials suggests that a moderate increase in dairy food consumption has no or small effects on the major cardiovascular and metabolic risk factors [50]. This conclusion contrasts with results from several large epidemiological studies, which concluded that dairy food may have favorable effects on insulin resistance and decrease the risk of type 2 diabetes[7,51]. However, in these observational studies[32,52-54] dairy food intake was associated with an overall healthier eating pattern, healthier lifestyle, higher socio economic status and educational attainment, which are each associated with more favorable cardio metabolic profiles[55]. Evaluating effects of dairy in randomized intervention trials is likely to be more reliable than from observational studies, where associations may not be causal.
Several observational studies have suggested that dairy food may facilitate weight loss, particularly in obese and overweight individuals [12]. Also in randomized trials where the intervention included both increased dairy food and caloric restriction, weight loss has been reported [56]. However, in the current meta-analysis, which included studies which gave no advice on calorie restriction, increasing dairy food resulted in a modest weight gain. Results were similar in studies which included overweight and obese participants. Whilst no direct comparison is possible, mean weight gain on low fat dairy food is double that of whole fat dairy food. This is counterintuitive but is in keeping with a recent viewpoint in JAMA pediatrics[57] which suggest that trim milk is associated with increased weight in children. It is likely the weight gain was the result of increased total calories in studies which encouraged greater dairy intake without other changes in diet. It is uncertain whether weight gain also occurs when dairy food is taken as part of, rather than in addition to a balanced diet.
Several diabetes guidelines [5,58,59] recommend regular intake of low fat dairy because of its low glycemic index[60]. In observational studies[51,61] persons in the highest quartile of dairy consumption have less insulin resistance, and this association is strongest in those who are overweight or obese. In this analysis insulin sensitivity improved in two small studies[41,42] with no effect in the larger trials[43,45]. In stratified analyses there was no effect in overweight and obese participants, or with whole or low fat dairy interventions. Based on these observations, it is uncertain whether increasing dairy food improves insulin sensitivity, and further well designed studies are needed to resolve this question. A recent review by the American Diabetes Association[62] concluded that ‘none of the components of dairy appear to have an effect on glycemic control or cardiovascular disease risk reduction’, consistent with this analysis.
Many food guidelines encourage low fat dairy food, but advise avoiding whole fat dairy [22,63]. In the current analysis LDL cholesterol did not change significantly when whole fat dairy consumption was increased. Whilst the risk of cardiovascular disease is reduced when saturated fats are replaced by unsaturated fats [64], the reasons for this may be multifactorial. This study suggests that effects on LDL-cholesterol may not the primary reason.
Dairy intake was associated with lower blood pressure in observational studies [8,13] and in the large randomized DASH study [26]. In the DASH study the intervention included increased low fat dairy food, reduced total and saturated fat, and increased fruit and vegetables. In a secondary analysis it was estimated that low fat dairy could account for about half of the observed 5.5mmHg decrease in systolic blood pressure. However it is not possible to reliably estimate the effects of each dietary component when the intervention includes multiple dietary changes. For this reason the DASH study and studies of the Mediterranean diet [27] were not included in this meta-analysis. In this meta-analysis, the confidence intervals exclude significant effects (>1.6mmHg) of increasing dairy food on systolic and diastolic blood pressure.
Limitations of meta-analysis
The majority of subjects included in the meta-analysis were women, but there is currently no evidence for different effects of diet by gender. The diverse population and age range of subjects included makes the results relevant to improving lifestyle risk factors for diabetes and cardiovascular disease in the general population. Studying healthy populations also avoids possible treatment and disease effects on the outcomes of interest. Further research is needed to confirm similar neutral effects of dairy in patients with established diabetes and cardiovascular disease.
It is possible the duration of the dietary intervention was not long enough to identify effects on risk factors, but stratified analyses suggest similar results for longer and shorter periods of dietary intervention. The increase of 3.6 servings each day is a substantial dietary change, and previous studies suggest dietary interventions influence risk factors within one month[26,65].
Most studies included were relatively small. It is difficult to blind diet studies and the level of compliance with the dietary interventions was often uncertain. Several studies reported significant adverse or favorable effects of increasing dairy food on one or more risk factors, but sensitivity analyses suggested these studies had only a small effect on overall estimates. It is also possible that smaller studies which found no effects have not been published. Three quarters of the studies were funded by the dairy or food industry, and results were more favorable for industry compared to non-industry funded studies. This meta-analysis stratified studies by ‘low fat’ and ‘whole fat’ interventions, but a direct comparison of these studies may not be reliable, and no trials which directly compare ‘low’ with ‘whole’ fat dairy diets have been reported. Because studies were small, and some may be unreliable, the analysis can not exclude a small increase in LDL cholesterol with increase in whole fat dairy consumption. Studies are also needed to evaluate effects of other components of dairy food.
To provide a better estimate of health effects the meta-analysis evaluated associations with multiple rather than just one or two risk factors. However dairy food could influence the risk of cardiovascular disease or diabetes by pathways other than the risk factors measured[66]. The influence of dairy food on clinical outcomes rather than risk factors is most important for dietary guidelines. However, currently, no completed randomized trials allow independent assessment of the effects of changing dairy food on diabetic complications or cardiovascular events.
Conclusion
Increase in both whole and low fat dairy food, without other dietary interventions, is associated with a modest weight gain, with no or minor effects on other cardio-metabolic risk factors. These observations suggest that for most healthy individuals it is reasonable to include both low and whole fat dairy food as part of a healthy diet.
References
Articles from PLOS ONE are provided here courtesy of PLOS
Full text links
Read article at publisher's site: https://doi.org/10.1371/journal.pone.0076480
Read article for free, from open access legal sources, via Unpaywall:
https://journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0076480&type=printable
Citations & impact
Impact metrics
Citations of article over time
Article citations
Data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas.
Cochrane Database Syst Rev, 2(2022), 01 Feb 2022
Cited by: 12 articles | PMID: 36321557 | PMCID: PMC8805585
Review Free full text in Europe PMC
A randomized trial evaluating the effects of change in dairy food consumption on cardio-metabolic risk factors.
Eur J Prev Cardiol, 21(11):1376-1386, 17 Jun 2013
Cited by: 21 articles | PMID: 23774272
Effects of total fat intake on body fatness in adults.
Cochrane Database Syst Rev, 6:CD013636, 01 Jun 2020
Cited by: 17 articles | PMID: 32476140 | PMCID: PMC7262429
Review Free full text in Europe PMC
Behavioral Counseling to Promote a Healthful Diet and Physical Activity for Cardiovascular Disease Prevention in Adults Without Known Cardiovascular Disease Risk Factors: Updated Systematic Review for the U.S. Preventive Services Task Force
Agency for Healthcare Research and Quality (US), Rockville (MD), 25 Jan 2018
Cited by: 1 article | PMID: 29364620
ReviewBooks & documents Free full text in Europe PMC