Abstract
Objective
To determine mediators of 12-month outcomes of Internet interventions for youth with type 1 diabetes transitioning to adolescence.Methods
In this multisite clinical trial, 320 youth were randomized to one of two Internet-based interventions: Coping skills (TEENCOPE™) or diabetes education (Managing Diabetes). Mediators of the interventions' effects on glycosylated hemoglobin and quality of life were examined. Data were collected at baseline and at 3, 6, and 12 months.Results
Self-efficacy mediated treatment effects on quality of life in both interventions. For TEENCOPE™, stress reactivity, primary control coping, and secondary control coping mediated treatment effects, whereas for Managing Diabetes, social acceptance mediated treatment effects. There were no significant effects of either intervention on glycosylated hemoglobin.Conclusions
2 Internet interventions for youth with type 1 diabetes resulted in improved quality of life by different mechanisms, suggesting components of both diabetes education and coping skills may help to achieve better outcomes in youth with type 1 diabetes.Free full text

Mediators of 12-Month Outcomes of Two Internet Interventions for Youth With Type 1 Diabetes
Abstract
Objective To determine mediators of 12-month outcomes of Internet interventions for youth with type 1 diabetes transitioning to adolescence.
To determine mediators of 12-month outcomes of Internet interventions for youth with type 1 diabetes transitioning to adolescence. Methods
Methods In this multisite clinical trial, 320 youth were randomized to one of two Internet-based interventions: Coping skills (TEENCOPE™) or diabetes education (Managing Diabetes). Mediators of the interventions’ effects on glycosylated hemoglobin and quality of life were examined. Data were collected at baseline and at 3, 6, and 12 months.
In this multisite clinical trial, 320 youth were randomized to one of two Internet-based interventions: Coping skills (TEENCOPE™) or diabetes education (Managing Diabetes). Mediators of the interventions’ effects on glycosylated hemoglobin and quality of life were examined. Data were collected at baseline and at 3, 6, and 12 months. Results
Results Self-efficacy mediated treatment effects on quality of life in both interventions. For TEENCOPE™, stress reactivity, primary control coping, and secondary control coping mediated treatment effects, whereas for Managing Diabetes, social acceptance mediated treatment effects. There were no significant effects of either intervention on glycosylated hemoglobin.
Self-efficacy mediated treatment effects on quality of life in both interventions. For TEENCOPE™, stress reactivity, primary control coping, and secondary control coping mediated treatment effects, whereas for Managing Diabetes, social acceptance mediated treatment effects. There were no significant effects of either intervention on glycosylated hemoglobin. Conclusions
Conclusions 2 Internet interventions for youth with type 1 diabetes resulted in improved quality of life by different mechanisms, suggesting components of both diabetes education and coping skills may help to achieve better outcomes in youth with type 1 diabetes.
2 Internet interventions for youth with type 1 diabetes resulted in improved quality of life by different mechanisms, suggesting components of both diabetes education and coping skills may help to achieve better outcomes in youth with type 1 diabetes.
Type 1 diabetes is one of the most common and challenging chronic illnesses affecting youth in the United States, with projected estimates of the incidence increasing by 23%, from 166,018 in 2010 to 203,385 in 2050 (Imperatore et al., 2012). In adolescence, youth with type 1 diabetes face considerable challenges during this period of physiological, psychosocial, and cognitive development. Adolescents assume greater responsibility for their diabetes self-management, but carrying out a complex and demanding treatment regimen is difficult during a developmental phase when peer acceptance is a priority (Delamater, 2009). Adolescents with type 1 diabetes often exhibit poorer metabolic control and self-management along with increased psychosocial stress, distress, and lower quality of life (QOL) compared with younger children and adults with type 1 diabetes (Insabella, Grey, Knafl, & Tambolane, 2007).
Given the challenges faced by adolescents with type 1 diabetes, interventions are needed to improve self-management and protect them against deterioration of metabolic control and poor psychosocial outcomes. Standards of care for youth with type 1 diabetes identify the importance of self-management education (American Diabetes Association, 2013; Silverstein et al., 2005), and evidence supports that psychosocial interventions focused on self-management have the potential to improve metabolic control of type 1 diabetes as well as QOL in youth (Anderson, Brackett, Ho, & Laffel, 1999; Grey, Boland, Davidson, Li, & Tamborlane, 2000; Laffel et al., 2003; Nansel, Iannotti, & Liu, 2012; Wysocki et al., 2007). A recent pilot study of an Internet-based psychosocial intervention also had promising results on self-management and problem solving (Mulvaney, Rothman, Wallston, Lybarger, & Dietrich, 2010). Even in successful interventions, however, the mechanism of change is not always clear, nor which components of the intervention were effective.
While evaluating the main effects of interventions is critical to improving health outcomes, it is equally important to examine moderators and mediators of randomized clinical trials—even those that are unsuccessful—to determine how and for whom interventions may work (Kraemer, Wilson, Fairburn, & Agras, 2002). Examining mediators provides evidence for the mechanisms of change, which offers direction for program implementation and future research (Kazdin, 2007). Investigating mediators of interventions also allows for testing the theoretical basis and the effect of interventions on separate outcomes (La Greca, Silverman, & Lochman, 2009). Although Internet-based interventions have been successful in improving outcomes in pediatric populations, most have not explicitly tested mediators and moderators of the effects. For example, a family cognitive behavioral therapy delivered over the Internet was successful in reducing pain intensity and improving function in youth with chronic pain (Palermo, Wilson, Peters, Lewandowski, & Somheghi, 2009), but the researchers did not test for moderators of the effects. Similarly, an Internet-based educational program for youth with asthma resulted in reduced asthma-related emergencies and a decrease in the daily use of rescue medication (Runge, Lecheler, Horn, Tews, & Schaefer, 2006). However, the authors did not report on increased asthma knowledge as a mediator of these effects. As Ritterband et al. (2009) note, “testing which mechanisms of change within the model are responsible for bringing about behavior change … is critical to Internet intervention research” (p. 23). In type 1 diabetes, it is important to test for both mediators and moderators of interventions on psychosocial outcomes, such as QOL, as well as clinical outcomes, such as metabolic control.
Progress has been made in determining moderators of the effects of interventions for youth with type 1 diabetes, such as age (Graue, Wentzel-Larsen, Hanestad, & Søvik, 2005), gender (Whittemore et al., 2012), and family structure (Ellis et al., 2007), but few studies have examined mediators of intervention effects. In one of the only studies to do so, the authors found that the positive effects of multisystemic therapy on metabolic control were mediated by increased blood glucose testing (Ellis et al., 2007). Another study found that improvements in parent–child communication and problem solving mediated the effects of behavioral family systems therapy on metabolic control, adherence, and family conflict (Wysocki et al., 2008). To our knowledge, no other research on mediators of intervention effects in youth with type 1 diabetes has been conducted.
The Current Study
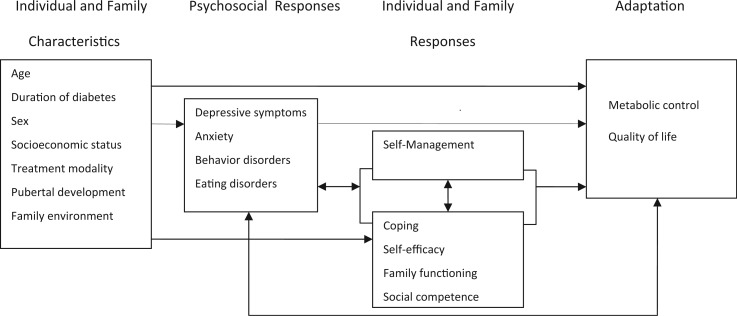
The conceptual framework for this study was based on a stress-adaptation model (Pollock, 1986) that describes the process of adaptation specific to youth with type 1 diabetes (Whittemore, Jaser, Guo, & Grey, 2010) (Figure 1). How youth adapt to the stress of diabetes is impacted, or mediated, by the ways in which they cope with the stress of diabetes (Jaser et al., 2012), their self-efficacy for diabetes management (Johnston-Brooks, Lewis, & Garg, 2002), their social competence (Edgar & Skinner, 2003), and family functioning (Anderson et al., 2002; Cohen, Lumley, Naar-King, Partridge, & Cakan, 2004; Wysocki et al., 2009). Thus, improvements in QOL and metabolic control are proposed to occur through changes in coping, self-efficacy, social competence, self-management, and family conflict. Our research team designed two Internet -based psycho-educational interventions—TEENCOPETM and Managing Diabetes—to impact these mediating factors. We demonstrated that both the education (Managing Diabetes) and coping skills training (TEENCOPETM) interventions improved QOL in adolescents with type 1 diabetes over 12 months, but metabolic control did not improve in either intervention group (Grey et al., 2013). The purpose of the current study was to examine the proposed mediators (coping, self-efficacy, social competence, self-management, and family conflict) of the effects of two Internet -based interventions on the primary outcomes of metabolic control and QOL.
Method
The current study was a multisite clinical trial aimed at comparing the efficacy of two Internet psycho-educational interventions for youth with type 1 diabetes transitioning to adolescence (TEENCOPE™ and Managing Diabetes) (Whittemore et al., 2012). The coping skills training intervention, TEENCOPETM, developed a cast of ethnically diverse adolescent characters who had type 1 diabetes to model coping skills. A graphic novel format demonstrated each of the following skills: Assertive communication, social problem-solving, stress management, positive self-talk, and conflict resolution (Grey et al., 2000). Further, a monitored online discussion board allowed TEENCOPE™ participants to communicate with other youth enrolled in the study. The educational intervention, Managing Diabetes, used a visually appealing and highly interactive interface to present diabetes education (American Diabetes Association, 2013; Silverstein et al., 2005). This program included tailored problem-solving exercises on healthy eating, physical activity, glucose control, sick days, and diabetes technology. The programs were developed with feedback from adolescents with type 1 diabetes and input from diabetes educators (Whittemore, Grey, Lindemann, Ambrosino, & Jaser, 2010). Each program had five sessions that were released weekly, and each session took approximately 30 min to complete. Participation was high, with 77% of TEENCOPETM and 79% of Managing Diabetes participants completing at least 4 of 5 sessions, and 52% of TEENCOPETM participants contributing to the online discussion board. Satisfaction was also high (mean score = 3.9 of 5).
Participants
Youth with type 1 diabetes (n = 320) participated in this study. A convenience sample was recruited from four clinical sites: Children’s Hospital of Pennsylvania, University of Arizona, University of Miami, and Yale University. Youth were eligible if they were diagnosed with type 1 diabetes for at least 6 months, aged 11–14, had no other significant medical problems, were able to speak and write English, and had access to high-speed Internet at home, school, or in the community. The mean age was 12.3 ± .1 years, diabetes duration was 6.1 ± 3.5 years, and the mean glycosylated hemoglobin (HbA1c) level was 8.3 ± 1.5%. Nearly 59% used pump therapy, 55% were female, and 65% were White, non-Hispanic, 19% Hispanic, 8% Black, and 8% Other. About 50% of the families reported annual income ≥$80,000.
Procedure
Institutional review boards at all clinical sites approved the study. Youth and parents were recruited from outpatient diabetes clinics, and trained research personnel obtained informed consent/assent. Parents provided demographic data at the time of enrollment, and youth were provided instructions for secure, online collection of psychosocial data at baseline and at 3, 6, 12, and 18 months. Only data up to 12 months were used in the current analysis, as participants were invited to crossover to the other intervention after 12 months. If online data collection was not completed within 3 months of enrollment, youth were considered as passively refusing study participation. Routine clinic-acquired HbA1c values were obtained by chart review. See Figure 2 for CONSORT (Schulz, Altman, & Moher, 2010) flow diagram.
Measures
All measures have been used previously in studies of adolescents with type 1 diabetes. Psychometric information on each measure is provided in Table I.
Table I.
Psychometric Properties of the Major Study Variables
| Variable | N | M | SD | Α | Range | |
|---|---|---|---|---|---|---|
| Potential | Actual | |||||
| HbA1c | 314 | 8.3 | 1.5 | 5.4–14.4 | ||
| PedsQL | 320 | 80.8 | 11.8 | 0.87 | 0–100 | 43.5–100.0 |
| Primary control coping | 320 | .19 | .04 | 0.77 | ||
| Secondary control coping | 320 | .26 | .06 | 0.80 | ||
| Disengagement coping | 320 | .15 | .03 | 0.77 | ||
| Stress reactivity | 320 | .19 | .04 | 0.87 | ||
| Diabetes self-efficacy | 320 | 45.1 | 11.7 | 0.88 | 24–120 | 24–81 |
| Self-management of diabetes | ||||||
    Collaboration Collaboration | 320 | 21.8 | 6.7 | 0.68 | 0–39 | 4–38 |
    Activities Activities | 320 | 32.3 | 5.7 | 0.74 | 0–45 | 12–44 |
    Problem solving Problem solving | 320 | 14.5 | 3.9 | 0.80 | 0–21 | 2–21 |
| Social competence | 319 | 16.4 | 3.2 | 0.75 | 5–20 | 5–20 |
| Diabetes family conflict | 320 | 26.3 | 5.9 | 0.87 | 19–57 | 19–57 |
Note. The Primary Control Coping, Secondary Control Coping, Disengagement Coping, and Stress Reactivity variables do not have a range, as they are proportion scores, calculated by dividing the total score for each variable by the total score for the entire measure.
Metabolic control was measured by HbA1c, an indicator of the metabolic control over the past 8–12 weeks, using the DCA2000 (Bayer, Tarrytown, NY) in the majority of participants. Very few (3%) results were done by outside laboratories, and these results were not significantly different from those from the DCA2000.
QOL was evaluated with the Pediatric Quality of Life Inventory (PedsQL) (teen version)–Core (Varni, Seid, & Kurtin, 1999). This instrument consists of 23 items that measure health-related QOL, with higher scores reflective of better QOL.
Coping was assessed with the Responses to Stress Questionnaire (Connor-Smith, Compas, Wadsworth, Thomsen, & Saltzman, 2000), in which adolescents reported on how they responded to diabetes-specific stressors with 57 items. The four factors included in the current study were primary control coping (problem solving, emotional modulation, emotional expression), secondary control coping (positive thinking, cognitive restructuring, acceptance, distraction), disengagement coping (avoidance, denial, wishful thinking), and stress reactivity (physiological arousal, rumination). Proportion scores were used to control for response bias, and higher scores indicate that adolescents reported greater use of that type of coping in relation to their total coping. Cronbach’s alpha ranged from 0.77 to 0.88 in our sample.
The Self-Efficacy for Diabetes Scale measures youth perceptions about their personal competence and resourcefulness for successfully managing their diabetes (Grossman, Brink, & Hauser, 1987). The diabetes-specific self-efficacy subscale (24 items) was used in this study, with lower scores indicative of higher self-efficacy.
The Self-Management of Diabetes–Adolescents (Schilling et al., 2009), a 52-item self-report measure, was used to evaluate adolescents’ self-management. The subscales Collaboration with Parents, Diabetes Care Activities, and Diabetes Problem Solving were used in this analysis. Higher scores indicate better self-management.
Social competence was measured with the social acceptance subscale (five items) of the Self-Perception Profile for Adolescents scale (Harter, 1988). Higher scores reflect greater perceived social competence, such as satisfaction with number of friends.
The Diabetes Family Conflict Scale was used to evaluate diabetes-related treatment conflict (Hood, Anderson, Butler, & Laffel, 2007). This 19-item scale measures conflict between family members on diabetes management activities, and higher scores on this scale are indicative of greater diabetes-related conflict.
Data Analyses
The sample and each of the variables were described using frequency distributions and appropriate summary statistics. Group differences at baseline were tested with t-tests or chi-square. In this article, we focused on the theoretical mediators of the intervention effects, or the factors expected to change as a result of the interventions. To test this, we examined the association between changes in the proposed mediators with changes in outcomes. Because participants were randomized to the two different interventions, each targeting different theoretical constructs, the change in outcomes may be attributed to the interventions. Mediation effects were examined in each intervention group (TEENCOPETM or Managing Diabetes) separately using a mediation analysis approach proposed for within-subject designs (Judd, Kenny, & McClelland, 2001), to show the specificity of mediators by condition. The advantage of this approach is that it can detect the association between a changed mediator and changed outcome after removing effects from the variability of cross-sectional correlations. All potential mediators were standardized with the means and standard deviations from the total sample. The mediation analysis was performed with the following steps: (1) the change in mediator from baseline at 12 months was estimated from a mixed-effects model controlling for demographics (i.e., gender, child age, race, duration of diabetes, household income, therapy type, and study site); (2) the effect of the change in mediator on the improvement of outcome (HbA1c/QOL) within subjects was tested after controlling for the variability of cross-sectional correlations between the mediator and outcome over time as well as the demographic covariates; and (3) the final multivariate model was a mixed-effects model developed to determine whether the mediators that showed a significant change over 12 months were associated with a significant change in outcomes at 12 months.
Results
Preliminary Analyses
The two groups were comparable at baseline, with the exception of years of parental education, with those in Managing Diabetes having 0.7 years more education (Table II). There were, however, significant differences across the four sites in race/ethnicity, income, therapy type (pump or injections), parent education, and HbA1c, and these were controlled in the analyses.
Table II.
Comparison of Demographic and Clinical Characteristics by Group
| TEENCOPETM n = 167 | Managing Diabetes n = 153 | ||
|---|---|---|---|
| n (%) | n (%) | p-value | |
| Gender | |||
    Male Male | 74 (44.3) | 69 (45.1) | .89 |
    Female Female | 93 (55.7) | 84 (54.9) | |
| Race | |||
    White, non-Hispanic/ non-Latino White, non-Hispanic/ non-Latino | 109 (65.7) | 95 (62.5) | .56 |
    Non-White Non-White | 57 (34.3) | 57 (37.5) | |
| Annual income | |||
    <$40,000 <$40,000 | 35 (22.2) | 30 (19.9) | .89 |
    $40,000–$79,999 $40,000–$79,999 | 44 (27.8) | 43 (28.5) | |
    $80,000+ $80,000+ | 79 (50.0) | 78 (51.6) | |
| Therapy type | |||
    Pump Pump | 99 (59.3) | 91 (59.5) | .97 |
    Injection Injection | 68 (40.7) | 62 (40.5) | |
| Mean (SD) | Mean (SD) | ||
| Age | 12.3 (1.1) | 12.3 (1.1) | .89 |
| Parent guardian education (years) | 14.3 (2.7) | 15.0 (2.9) | .03 |
| Duration (months) | 365 (230) | 342 (208) | .35 |
| HbA1c at baseline (%) | 8.4 (1.6) | 8.2 (1.3) | .14 |
Direct Effects of Interventions on Outcomes
In the intent-to-treat analysis, both intervention groups had slight increases in HbA1c levels: Mean HbA1c of adolescents in the TEENCOPETM group increased from 8.29 to 8.43, and mean HbA1c for adolescents in the Managing Diabetes group increased from 8.15 to 8.25, over 12 months (F = 3.91, p = .05). Both groups also showed significant improvements in QOL over time; mean PedsQL score in the TEENCOPETM group increased from 79.95 to 82.03 and mean PedsQL score in the Managing Diabetes group increased from 82.91 to 85.65 over 12 months (F = 31.92, p < .001). However, there were no significant differences between the two interventions on primary outcomes over 12 months of follow-up (Grey et al., 2013).
Effects of Intervention on Mediators
In the TEENCOPETM group, there were significant changes in self-efficacy, primary control coping, secondary control coping, stress reactivity, and collaboration with parents, after controlling for demographic variables (Table III). In the Managing Diabetes group, there were significant changes in self-efficacy, collaboration with parents, problem solving, and social acceptance (Table II).
Table III.
Mediation Effects on HbA1c Level and Quality of Life
| Variable (standardized) | Changed mediator at 12 months | Mediation effect on HbA1c level | Mediation effect on quality of life |
|---|---|---|---|
| Δ ± StdErr (p-value) | Coeff ± StdErr (p-value) | Coeff ± StdErr (p-value) | |
| TEENCOPE | |||
    Self-efficacy Self-efficacy | −0.651 ± 0.120 (<.0001) | 0.123 ± 0.085 (.1494) | −2.100 ± 0.676 (.0022) |
    Primary control coping Primary control coping | 0.272 ± 0.117 (.0219) | −0.105 ± 0.081 (.1992) | 3.032 ± 0.625 (<.0001) |
    Secondary control coping Secondary control coping | 0.284 ± 0.104 (.0074) | −0.096 ± 0.095 (.3178) | 3.226 ± 0.737 (<.0001) |
    Disengagement coping Disengagement coping | −0.233 ± 0.124 (.0627) | 0.081 ± 0.076 (.2934) | −0.942 ± 0.617 (.1286) |
    Stress reactivity Stress reactivity | −0.324 ± 0.114 (.0054) | 0.034 ± 0.084 (.6820) | −2.959 ± 0.655(<.0001) |
    Collaboration with parents Collaboration with parents | −0.360 ± 0.090 (.0001) | −0.040 ± 0.088 (.6491) | 0.785 ± 0.716 (.2750) |
    Diabetes care activity Diabetes care activity | −0.090 ± 0.089 (.3098) | −0.125 ± 0.086 (.1500) | 2.536 ± 0.695 (.0003) |
    Diabetes problem solving Diabetes problem solving | 0.189 ± 0.104 (.0711) | −0.036 ± 0.084 (.6689) | 1.136 ± 0.664 (.0886) |
    Social acceptance Social acceptance | 0.080 ± 0.094 (.4008) | −0.041 ± 0.093 (.6582) | 2.648 ± 0.778 (.0008) |
    Family conflict Family conflict | 0.109 ± 0.102 (.2856) | 0.186 ± 0.084 (.0290) | −2.790 ± 0.617(<.0001) |
| Managing Diabetes | |||
    Self-efficacy Self-efficacy | −0.242 ± 0.114 (.0352) | −0.022 ± 0.065 (.7299) | −2.565 ± 0.490 (<.0001) |
    Primary control coping Primary control coping | 0.087 ± 0.099 (.3833) | 0.012 ± 0.080 (.8820) | 1.112 ± 0.602 (.0662) |
    Secondary control coping Secondary control coping | 0.026 ± 0.103 (.8007) | 0.029 ± 0.071 (.6835) | 1.415 ± 0.567 (.0135) |
    Disengagement coping Disengagement coping | 0.013 ± 0.115 (.9118) | −0.031 ± 0.064 (.6320) | −0.774 ± 0.518 (.1368) |
    Stress reactivity Stress reactivity | −0.146 ± 0.086 (.0940) | 0.061 ± 0.082 (.4571) | −0.953 ± 0.662 (.1514) |
    Collaboration with parents Collaboration with parents | −0.375 ± 0.085 (<.0001) | −0.021 ± 0.076 (.7851) | −0.162 ± 0.639 (.8002) |
    Diabetes care activity Diabetes care activity | −0.097 ± 0.081 (.2350) | −0.014 ± 0.078 (.8599) | 1.181 ± 0.638 (.0656) |
    Diabetes problem solving Diabetes problem solving | 0.278 ± 0.086 (.0017) | 0.039 ± 0.071 (.5855) | −0.458 ± 0.620 (.4606) |
    Social acceptance Social acceptance | 0.216 ± 0.095 (.0244) | −0.024 ± 0.080 (.7655) | 2.210 ± 0.609 (.0004) |
    Family conflict Family conflict | −0.205 ± 0.114 (.0754) | 0.032 ± 0.058 (.5782) | −1.703 ± 0.492 (.0007) |
Note. The change in mediators at 12 months was estimated after controlling for demographic variables (gender, age, race/ethnicity, duration of diabetes, household income, therapy type, and study site). The mediation effect was estimated considering the variability of the cross-sectional correlation between mediator and outcome over time, controlling for demographic variables.
Mediation Analyses of Intervention Effects on Outcomes
There were differences in significant mediators across the two programs. For youth in TEENCOPETM, improvements in self-efficacy (p = .002), primary control coping (p < .001), secondary control coping (p < .001), and stress reactivity (p < .001) were associated with improvement in QOL (Table III). For youth in Managing Diabetes, improvements in self-efficacy (p < .001) and social acceptance (p < .001) were associated with improvements in QOL (Table II). Self-management and family conflict were not significant mediators of the effects of either program on QOL. There were no significant mediators for HbA1c in either of the programs.
Discussion
This study examined the theoretically proposed mediators of two Internet psycho-educational programs for young adolescents with type 1 diabetes, both of which had a positive effect on QOL. Youth who received the TEENCOPETM intervention reported increased use of adaptive coping strategies (i.e., greater primary control and secondary control coping) and a decrease in stress reactivity, which mediated the effects of the intervention on QOL. Youth who received an educational intervention reported increased social competence, which mediated the positive effects of the intervention on QOL. In addition, self-efficacy improved in both groups, which also mediated the positive effects of the interventions on QOL. Results of the mediation analysis support several hypothesized relationships of the theoretical framework that guided the study (Whittemore, Jaser, et al., 2010), and suggest that components of both diabetes education and coping skills may help to achieve better QOL outcomes in youth with type 1 diabetes.
Self-efficacy is recognized as a central factor contributing to behavioral change and adherence to treatment regimens in youth with type 1 diabetes (Johnston-Brooks et al., 2002). Many psycho-educational interventions for youth with type 1 diabetes are based on Bandura’s social learning theory, which posits that behavior change occurs when self-efficacy for the behavior increases (Bandura, 1986). As such, the proposed mechanism of change for these interventions is increased self-efficacy; however, few researchers have explicitly tested this. By examining self-efficacy as a mediator of treatment effects, we were able to determine whether the interventions worked as intended. In fact, in both the TEENCOPETM and Managing Diabetes groups, improved self-efficacy mediated intervention effects on QOL. Self-efficacy is enhanced through role modeling and skill mastery, which were objectives of both Internet interventions. The TEENCOPETM intervention focused on modeling coping skills using role models (e.g., how to effectively communicate with a teacher about diabetes), whereas the Managing Diabetes intervention included practice in specific diabetes management skills (e.g., calculating insulin adjustments). Thus, the two interventions may have improved self-efficacy in different aspects of diabetes management, both of which resulted in improved QOL.
As expected, the TEENCOPE™ intervention improved coping skills by encouraging adolescents to use more primary control coping (e.g., problem solving) and secondary control coping (e.g., positive thinking) strategies. TEENCOPE™ also reduced adolescents’ reports of stress reactivity, which may reflect the use of strategies learned in the stress reduction module. Results of the mediator analyses of the Internet TEENCOPE™ program replicates outcomes from previous in-person group coping skills training groups, which also resulted in improved QOL (Grey et al., 2000), and provide further support for the proposed model of adaptation. In an intervention for children of depressed parents, increased use of secondary control coping skills also mediated the effect of the intervention on psychosocial outcomes (e.g., depressive symptoms) (Compas et al., 2010). Taken together, these results support the importance of teaching adaptive coping skills to youth with type 1 diabetes (Jaser et al., 2012).
For adolescents who received the Managing Diabetes intervention, increased social competence mediated the effects of the intervention on QOL. This was somewhat surprising, given that the Managing Diabetes intervention did not target social skills. Perhaps by teaching diabetes-related skills in the context of healthy, positive images of teens with diabetes, youth who received this program had improved self-concept. This result, however, is in line with previous findings that social competence and positive self-concept were associated with better emotional well-being in youth with type 1 diabetes (Edgar & Skinner, 2003).
Although diabetes-specific family conflict has a strong association with QOL (Laffel et al., 2003) and poorer metabolic control (Ingerski et al., 2010), we did not find a decrease in family conflict to be a significant mediator of the effects of the interventions on either of these primary outcomes. There may have not been enough variation in the level of family conflict reported in our sample of early adolescents, who possibly had greater parental engagement in diabetes management than would be evident in an older group of adolescents.
Unlike in the original in-person Coping Skills Training groups (Grey et al., 2000), we did not find a significant effect of the Internet intervention on metabolic control. There are several possible reasons for this discrepancy. First, the original intervention was conducted with older adolescents (ages 12–20, mean age = 14), whereas the current study focused on early adolescents (ages 11–14, mean age = 12). The decision to target a younger age-group was made to prevent the deterioration in adherence and metabolic control often seen in older adolescents before it occurs (Hegelson, Siminerio, Escobar, & Becker, 2009). Thus, results from the current study are more in line with the Coping Skills Training groups conducted in-person with school-age children (ages 8–12, mean age = 10), in which we found no effect on metabolic control, but did show improvements in QOL, self-efficacy, and coping over 12 months for both the coping skills training and education interventions (Grey et al., 2009). Low rates of participation in the school-age groups (24% of those consented could not be scheduled for groups) were a driving factor for moving to online interventions. Although our effects may be smaller than in the original study, our potential reach is greater. Another difference was that the original coping skills training intervention included 6 weekly sessions, followed by monthly visits for 12 months. This is a significantly larger “dose” than what was included in the TEENCOPETM and Managing Diabetes interventions, which consisted of 5 weekly sessions. It is possible that a greater number of sessions or more booster sessions are needed to have an effect on metabolic control. Thus, although we did not find an improvement in metabolic control, the minimal increase in HbA1c over 12 months during this critical stage of adolescence may be seen as a positive outcome in this age-group. Contrary to other studies demonstrating that self-efficacy enhanced glucose control (e.g., Johnston-Brooks et al., 2002), self-efficacy did not mediate intervention effects on HbA1c in our sample. This may be due to the relatively small changes in HbA1c over time.
Limitations
Although one of the strengths of the current study is the inclusion of a diverse group of youth from multiple sites, we did have relatively less enrollment of youth with low income (Whittemore et al., 2013). Further, results must be interpreted in light of moderate attrition (28%). Our use of intent-to-treat analysis, however, is a conservative approach to manage missing data. In addition, the use of multiple DCA2000s rather than a central laboratory assay for HbA1C may have limited our ability to detect changes in metabolic control. Alternatively, it is possible that the lack of change in metabolic control was due to limitations of the Internet programs. Finally, generalizability of findings is limited because our sample targeted younger adolescents from 11 to 14 years of age, specifically due to our focus on preventing the emergence of poorer outcomes that tend to occur later in adolescence, and many of the youth in our study were already in good metabolic control.
Clinical and Research Implications
Evidence from the current study supports that elements of both the educational and coping skills programs may be needed to improve some outcomes in youth with type 1 diabetes. The improvements in QOL resulting from the educational program (Managing Diabetes) suggest that developmentally appropriate education may be needed for early adolescents. Often, when youth are diagnosed at a younger age, diabetes education is directed at caregivers, and our results suggest that adolescents may benefit from further education and tailored problem-solving exercises during early adolescence. Similarly, the positive effects of the TEENCOPETM intervention on QOL indicate that coping skills training can improve QOL in adolescents by increasing their use of adaptive coping strategies, such as problem solving and positive thinking. While these programs did not have a positive impact on metabolic control, we should not overlook the importance of QOL as an important measure of the impact of chronic illness on well-being (Ingerski et al., 2010).
Research on mediators is necessary to explore causal mechanisms, helping to develop and test theory and identify specific targets for interventions (Shrout & Bolger, 2002). In the current sample, self-efficacy, coping, and social competence mediated the effects of the programs on QOL, suggesting that future preventive interventions should target these factors to see similar improvements. These results also lend support to our model of adaptation that hypothesized these mediators (Whittemore, Jaser, et al., 2010). To design the most effective and efficient interventions, more work is needed testing mediators of promising interventions and identifying which factors may be important to target. The current study is an important step in this work.
Funding
This work was supported by the National Institute of Nursing Research (grant number R01-NR04009); the Jonas Centers for Nursing Excellence and National Institute of Nursing Research award to A.C. (grant number T32-NR-008346-10); and the National Institute of Diabetes and Digestive and Kidney Diseases award to S.J. (grant number K23-DK088454;). Clinical Trials Registry Number: NCT00684658.
Conflicts of interest: None declared.
References
- American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care. 2013;35:S11–S66. [Europe PMC free article] [Abstract] [Google Scholar]
- Anderson BJ, Brackett J, Ho J, Laffel L. An office-based intervention to maintain parent-adolescent teamwork in diabetes management. Diabetes Care. 1999;22:713–722. [Abstract] [Google Scholar]
- Anderson BJ, Vangsness L, Connell A, Butler D, Goebel-Fabbri A, Laffel L. Family conflict, adherence, and glycaemic control in youth with short duration Type 1 diabetes. Diabetic Medicine. 2002;19:635–642. [Abstract] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W. H. Freeman; 1986. [Google Scholar]
- Cohen DM, Lumley MA, Naar-King S, Partridge T, Cakan N. Child behavior problems and family functioning as predictors of adherence and glycemic control in economically disadvantaged children with Type I diabetes: A prospective study. Journal of Pediatric Psychology. 2004;29:171–184. [Abstract] [Google Scholar]
- Compas BE, Champion JE, Forehand R, Cole DA, Reeslund KL, Fear J, Hardcastle EJ, Keller G, Rakow A, Garai E, Merchant MJ, Roberts L. Coping and parenting: Mediators of 12-month outcomes of a family group cognitive-behavioral preventive intervention with families of depressed parents. Journal of Consulting and Clinical Psychology. 2010;78:623–634. [Europe PMC free article] [Abstract] [Google Scholar]
- Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology. 2000;68:976–992. [Abstract] [Google Scholar]
- Delamater AM. Psychological care of children and adolescents with type 1 diabetes. Pediatric Diabetes. 2009;10:175–184. [Abstract] [Google Scholar]
- Edgar KA, Skinner TC. Illness representations and coping as predictors of emotional well-being in adolescents with type 1 diabetes. Journal of Pediatric Psychology. 2003;28:485–493. [Abstract] [Google Scholar]
- Ellis DA, Yopp J, Templin T, Naar-King S, Frey MA, Cunningham PB, Idalski A, Niec LN. Family mediators and moderators of treatment outcomes among youths with poorly controlled type 1 Diabetes: Results from a randomized controlled trial. Journal of Pediatric Psychology. 2007;32:194–205. 10.1093/jpepsy/jsj116. [Abstract] [Google Scholar]
- Graue M, Wentzel-Larsen T, Hanestad BR, Søvik O. Evaluation of a programme of group visits and computer-assisted consultations in the treatment of adolescents with Type 1 diabetes. Diabetic Medicine. 2005;22:1522–1529. 10.1111/j.1464-5491.2005.01689.x. [Abstract] [Google Scholar]
- Grey M, Boland EA, Davidson M, Li J, Tamborlane WV. Coping skills training for youth with diabetes mellitus has long-lasting effects on metabolic control and quality of life. Journal of Pediatrics. 2000;137:107–113. [Abstract] [Google Scholar]
- Grey M, Whittemore R, Jaser SS, Ambrosino J, Lindemann E, Liberti L, Northrup V. Effects of coping skills training in school-age children with type 1 diabetes. Research in Nursing and Health. 2009;32:405–418. [Europe PMC free article] [Abstract] [Google Scholar]
- Grey M, Whittemore R, Jeon S, Murphy K, Faulkner MS, Delamater A, TeenCope Research G. Internet psycho-education programs improve outcomes in youth with type 1 Diabetes. Diabetes Care. 2013;36:2475–2482. 10.2337/dc12-2199. [Europe PMC free article] [Abstract] [Google Scholar]
- Grossman HY, Brink S, Hauser ST. Self-efficacy in adolescent girls and boys with insulin-dependent diabetes mellitus. Diabetes Care. 1987;10:324–329. [Abstract] [Google Scholar]
- Harter S. Manual for the Adolescent Self-Perception Profile. Denver, CO: University of Denver; 1988. [Google Scholar]
- Hegelson VS, Siminerio L, Escobar O, Becker D. Predictors of metabolic control among adolescents with diabetes: A 4-year longitudinal study. Journal of Pediatric Psychology. 2009;34:254–270. [Europe PMC free article] [Abstract] [Google Scholar]
- Hood KK, Anderson BJ, Butler D, Laffel L. Updated and revised diabetes family conflict scale. Diabetes Care. 2007;30:1764–1769. [Europe PMC free article] [Abstract] [Google Scholar]
- Imperatore G, Boyle JP, Thompson TJ, Case D, Dabelea D, Hamman RF, Lawrence JM, Liese AD, Liu LL, Mayer-Davis EJ, Rodriguez BL, Standiford D. Projections of Type 1 and Type 2 diabetes burden in the U.S. population aged <20 years through 2050: Dynamic modeling of incidence, mortality, and population growth. Diabetes Care. 2012;35:2515–2520. 10.2337/dc12-0669. [Europe PMC free article] [Abstract] [Google Scholar]
- Ingerski LM, Modi AC, Hood KK, Pai AL, Zeller M, Piazza-Waggoner C, Driscoll, KA, Rothenberg, ME, Franciosi, J, Hommel KA. Health-related quality of life across pediatric chronic conditions. Journal of Pediatrics. 2010;156:639–644. [Europe PMC free article] [Abstract] [Google Scholar]
- Insabella G, Grey M, Knafl KA, Tambolane WV. The transition to young adulthood in youth with type 1 diabetes on intensive treatment. Pediatric Diabetes. 2007;8:228–234. [Abstract] [Google Scholar]
- Jaser SS, Faulkner MS, Whittemore R, Jeon S, Murphy K, Delamater A, Grey M. Coping, self-management, and adaptation in adolescents with type 1 diabetes. Annals of Behavioral Medicine. 2012;43:311–319. [Europe PMC free article] [Abstract] [Google Scholar]
- Johnston-Brooks CH, Lewis MA, Garg S. Self-efficacy impacts self-care and HbA1c in young adults with type 1 diabetes. Psychosomatic Medicine. 2002;64:43–51. [Abstract] [Google Scholar]
- Judd CM, Kenny DA, McClelland GH. Estimating and testing mediation and moderation in within-subject designs. Psychological Methods. 2001;6:115–134. [Abstract] [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. [Abstract] [Google Scholar]
- Kraemer HC, Wilson T, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. [Abstract] [Google Scholar]
- La Greca AM, Silverman WK, Lochman JE. Moving beyond efficacy and effectiveness in child and adolescent intervention research. Journal of Consulting and Clinical Psychology. 2009;77:373–382. 10.1037/0003-066x.61.1.27. [Abstract] [Google Scholar]
- Laffel L, Vangsness L, Connell A, Goebel-Fabbri A, Butler D, Anderson BJ. Impact of ambulatory, family-focused teamwork intervention on glycemic control in youth with type 1 diabetes. Journal of Pediatrics. 2003;142:409–416. [Abstract] [Google Scholar]
- Mulvaney SA, Rothman RL, Wallston KA, Lybarger C, Dietrich MS. An internet-based program to improve self-management in adolescents with type 1 diabetes. Diabetes Care. 2010;33:602–604. [Europe PMC free article] [Abstract] [Google Scholar]
- Nansel TR, Iannotti RJ, Liu A. Clinic-integrated behavioral intervention for families of youth with type 1 diabetes: Randomized clinical trial. Pediatrics. 2012;129:e866–e873. 10.1542/peds.2011-2858. [Europe PMC free article] [Abstract] [Google Scholar]
- Palermo TM, Wilson AC, Peters M, Lewandowski A, Somheghi H. Randomized controlled trial of an Internet-delivered family cognitive-behavioral therapy intervention for children and adolescents with chronic pain. Pain. 2009;146:205–213. [Europe PMC free article] [Abstract] [Google Scholar]
- Pollock SE. Human responses to chronic illness: Physiologic and psychosocial adaptation. Nursing Research. 1986;35:90–95. [Abstract] [Google Scholar]
- Ritterband LM, Thorndike FP, Cox DJ, Kovatchev BP, Gonder-Frederick LA. A behavior change model for internet interventions. Annals of Behavioral Medicine. 2009;38:18–27. [Europe PMC free article] [Abstract] [Google Scholar]
- Runge C, Lecheler J, Horn M, Tews JT, Schaefer M. Outcomes of a web-based patient education program for asthmatic children and adolescents. Chest. 2006;129:581–593. [Abstract] [Google Scholar]
- Schilling LS, Dixon JK, Knafl KA, Lynn MR, Murphy K, Dumser S, Grey M. A new self-report measure of self-management of type 1 diabetes for adolescents. Nursing Research. 2009;58:228–236. [Europe PMC free article] [Abstract] [Google Scholar]
- Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomized trials. Annals of Internal Medicine. 2010;152:1–11. [Abstract] [Google Scholar]
- Shrout PE, Bolger AK. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–445. [Abstract] [Google Scholar]
- Silverstein JH, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel LM B, Deeb L, Grey M, Anderson B, Holzmeister LA, Clark N. Care of children and adolescents with type 1 diabetes. Diabetes Care. 2005;28:184–212. [Abstract] [Google Scholar]
- Varni JW, Seid M, Kurtin PS. Pediatric health-related quality of life measurement technology: A guide for health care decision makers. Journal of Clinical Outcomes Management. 1999;6:33–40. [Google Scholar]
- Whittemore R, Grey M, Lindemann E, Ambrosino J, Jaser SS. Development of an Internet coping skills training program for teenagers with type 1 diabetes. CIN: Computers, Informatics, Nursing. 2010;28:103–111. 10.1097/NCN.0b013e3181cd8199. [Europe PMC free article] [Abstract] [Google Scholar]
- Whittemore R, Jaser SS, Faulkner MS, Murphy K, Delamater A, Grey M, Group TR. Type 1 diabetes eHealth psychoeducation: Youth recruitment, participation, and satisfaction. Journal of Medical Internet Research. 2013;15:e15. [Europe PMC free article] [Abstract] [Google Scholar]
- Whittemore R, Jaser SS, Guo J, Grey M. A conceptual model of childhood adaptation to type 1 diabetes. Nursing Outlook. 2010;58:242–251. [Europe PMC free article] [Abstract] [Google Scholar]
- Whittemore R, Jaser SS, Jeon S, Liberti L, Delamater A, Murphy K, Faulkner, MS, Grey M. An internet coping skills training program for youth with type 1 diabetes. Nursing Research. 2012;61:395–404. [Europe PMC free article] [Abstract] [Google Scholar]
- Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Mauras N, White NH. Randomized trial of behavioral family systems therapy for diabetes: Maintenance of effects on diabetes outcomes in adolescents. Diabetes Care. 2007;30:555–560. 10.2337/dc06-1613. [Abstract] [Google Scholar]
- Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Taylor A, Sadler M, White NH. Randomized, controlled trial of behavioral family systems therapy for diabetes: Maintenance and generalization of effects on parent-adolescent communication. Behavior Therapy. 2008;39:33–46. [Abstract] [Google Scholar]
- Wysocki T, Nansel TR, Holmbeck GN, Chen R, Laffel L, Anderson BJ, Weissberg-Benchell J. Collaborative involvement of primary and secondary caregivers: Associations with youths diabetes outcomes. Journal of Pediatric Psychology. 2009;34:869–881. [Europe PMC free article] [Abstract] [Google Scholar]
Articles from Journal of Pediatric Psychology are provided here courtesy of Oxford University Press
Full text links
Read article at publisher's site: https://doi.org/10.1093/jpepsy/jst081
Read article for free, from open access legal sources, via Unpaywall:
https://academic.oup.com/jpepsy/article-pdf/39/3/306/3410890/jst081.pdf
Citations & impact
Impact metrics
Article citations
Psychoeducational Messaging to Reduce Alcohol Use for College Students With Type 1 Diabetes: Internet-Delivered Pilot Trial.
J Med Internet Res, 23(9):e26418, 30 Sep 2021
Cited by: 6 articles | PMID: 34591022 | PMCID: PMC8517820
Clinical Utility of Psychoeducational Interventions for Youth with Type 1 Diabetes: A Scoping Review.
Contin Educ, 2(1):76-108, 15 Jul 2021
Cited by: 0 articles | PMID: 38774890 | PMCID: PMC11104390
Review Free full text in Europe PMC
Monetary reinforcement for self-monitoring of blood glucose among young people with type 1 diabetes: evaluating effects on psychosocial functioning.
Diabet Med, 37(4):665-673, 19 Nov 2019
Cited by: 0 articles | PMID: 31701566 | PMCID: PMC7332232
Measuring Self-Efficacy in the Context of Pediatric Diabetes Management: Psychometric Properties of the Self-Efficacy for Diabetes Scale.
J Pediatr Psychol, 43(2):143-151, 01 Mar 2018
Cited by: 7 articles | PMID: 29106615 | PMCID: PMC5896602
A Danish version of self-efficacy in diabetes self-management: A valid and reliable questionnaire affected by age and sex.
Pediatr Diabetes, 19(3):544-552, 02 Nov 2017
Cited by: 2 articles | PMID: 29094452
Go to all (10) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Clinical Trials
- (1 citation) ClinicalTrials.gov - NCT00684658
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
An internet coping skills training program for youth with type 1 diabetes: six-month outcomes.
Nurs Res, 61(6):395-404, 01 Nov 2012
Cited by: 45 articles | PMID: 22960587 | PMCID: PMC3623558
Internet psycho-education programs improve outcomes in youth with type 1 diabetes.
Diabetes Care, 36(9):2475-2482, 11 Apr 2013
Cited by: 76 articles | PMID: 23579179 | PMCID: PMC3747907
School-aged children with type 1 diabetes benefit more from a coping skills training program than adolescents in China: 12-month outcomes of a randomized clinical trial.
Pediatr Diabetes, 21(3):524-532, 23 Feb 2020
Cited by: 7 articles | PMID: 31885120
Interventions to improve patients' compliance with therapies aimed at lowering glycated hemoglobin (HbA1c) in type 1 diabetes: systematic review and meta-analyses of randomized controlled clinical trials of psychological, telecare, and educational interventions.
Trials, 17:94, 17 Feb 2016
Cited by: 27 articles | PMID: 26888087 | PMCID: PMC4758163
Review Free full text in Europe PMC
Funding
Funders who supported this work.
NIDDK NIH HHS (2)
Grant ID: P30 DK092986
Grant ID: K23-DK088454
NINR NIH HHS (2)
Grant ID: R01-NR04009
Grant ID: T32-NR-008346-10
 1
1