Abstract
Free full text

The Relationship of Waist Circumference and BMI to Visceral, Subcutaneous, and Total Body Fat: Sex and Race Differences
Abstract
The purpose of this study was to examine sex and race differences in the relationship between anthropometric measurements and adiposity in white and African-American (AA) adults. Visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT) areas were measured with computed tomography (CT). Fat mass (FM) was measured with dual-energy-X-ray absorptiometry (DXA). Correlation coefficients were used to assess the relationship of waist circumference (WC) and BMI to VAT, SAT, and FM within sex-by-race groups. General linear models were used to compare relationships between WC or BMI, and adiposity across sex and race, within age groups (18–39 and 40–64 years). The sample included 1,667 adults (men: 489 white; 120 AA; women: 666 white, 392 AA). WC and BMI correlations were highest for FM and SAT compared to VAT. Women had higher FM levels than men regardless of WC, but the sex difference in FM was attenuated in younger AA adults with a high BMI. For a given level of WC or BMI, women had higher levels of SAT than men; however, significant interactions indicated that the relationship was not consistent across all levels of BMI and WC. Sex and race differences in VAT varied significantly with WC and BMI. In general, white adults had higher levels of VAT than AA adults at higher levels of BMI and WC. Sex differences, and in some instances race differences, in the relationships between anthropometry and fat-specific depots demonstrate that these characteristics need to be considered when predicting adiposity from WC or BMI.
INTRODUCTION
Obesity is defined as an excess of body fat, which can be measured in laboratory settings using methods such as dual-energy X-ray absorptiometry (DXA), magnetic resonance imaging, or computed tomography (CT). DXA methods can provide measures of general adiposity such as total body fat (fat mass (FM)), whereas magnetic resonance imaging or CT can estimate regional adiposity such as visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT). Indirect indicators of body composition, such as BMI and waist circumference (WC), are commonly used as surrogate measures of adiposity in population studies. These anthropometric measures have been instrumental in monitoring the obesity epidemic (1), as well as linking obesity status with an increased risk for cardiovascular disease (2,3), type 2 diabetes (4), and mortality (5,6).
The utility of BMI and WC in describing obesity status depends on the assumption that anthropometric measures are correlated with more direct measures of adiposity such as FM, SAT, or VAT, or with markers of ectopic fat deposition in skeletal muscle, liver, and other organs. However, several studies have shown that for the same BMI, the amount of body fat, regardless of fat depot, is significantly influenced by sex (7–10) and race (11–13), although race differences have been somewhat inconsistent (14,15). In addition, the relationship between WC and depot-specific adiposity also shows differences according to sex (16–18) and race (11,19,20). These results suggest that simple anthropometric markers may not identify the same level of adiposity across different demographic groups. However, race and sex differences in the relationship between BMI or WC and adiposity have not necessarily been examined together in a large dataset, across varying levels of obesity, or with direct measures of body fat. We recently demonstrated significant differences between white and African-American (AA) men and women in measures of overall and depot-specific adiposity (21). This study extends this research by comparing the relationship between anthropometric indicators (WC or BMI) and directly measured adipose tissue (VAT, SAT, and FM) across sex and race in a large biracial group.
METHODS AND PROCEDURES
Sample
The Pennington Center Longitudinal Study (PCLS) is an ongoing investigation of the effects of obesity and lifestyle factors on the development of chronic diseases such as type 2 diabetes, cardiovascular disease, and cancer. The sample is composed of volunteers who have participated in nutrition, weight loss and other metabolic intervention and observational studies at the Pennington Biomedical Research Center in Baton Rouge, Louisiana since 1992. The current cross-sectional study is limited to adult participants who had DXA and abdominal CT scans between 1996 and 2008. All anthropometric data were collected within 60 days of the DXA (mean ± s.d.: 22.3 ± 12.8 days) and CT scans (mean ± s.d.: 25.8 ± 14.0 days). This sample comprised 1,667 total adults (489 white men, 120 AA men, 666 white women, and 392 AA women), between 18 and 64 years of age (mean ± s.d.: 43.4 ± 12.1 years). In this sample, self-reported hypertension was 7% and self-reported diabetes was 6%. Unfortunately, there is no information available on specific medication use. Each volunteer provided their written informed consent and all PCLS procedures, including this analysis were approved by the Pennington Biomedical Research Center institutional review board.
Anthropometry
Standardized anthropometric measures were obtained on all participants. Height was measured using standard methods with a stadiometer. Participants were required to remove shoes and asked to hold an inhaled breath, while a nurse lightly applied traction to the patient’s head in order to maintain alignment with the Frankfort Plane. A second nurse then lowered the slide until it reached the vertex of the skull and recorded the reading from the indicator. This process was repeated, and the average of the two heights is used in analysis (a third measurement is obtained if the first two measurements are >0.5 cm apart). Weight was measured in duplicate using a digital scale after all outer clothing, heavy pocket items, and shoes were removed. Weight was recorded to the nearest 0.1 kg. A third measurement was obtained if the first two measurements were >0.5 kg different. BMI was calculated as the weight in kilograms divided by the height in meters squared (kg/m2). WC was measured, in duplicate, at the midpoint between the inferior border of the ribcage and the superior aspect of the iliac crest using an inelastic measuring tape. WC measures were averaged, however, a third measure was taken if measures differed by >0.5 cm.
Body composition
FM (kg) was measured by a whole body DXA scanner. FM was calculated as percent body fat × scale weight, where percent body fat was derived from DXA, and scale weight was the digital scale weight. Two Hologic models (Bedford, MA) were used for imaging: the QDR2000 (n = 869) was phased out in 2006, and replaced with the QDR4500 (n = 798) which has been in service since 2001. Concordance between the two DXA machines was determined with same-day scans on a subsample of participants (n = 32), resulting in measurements with a high degree of agreement (R2 = 0.987). An equation was used to convert the QDR2000 data to QDR4500 data: Y = 0.8015X + 2.3903. Each DXA used a phantom prior to data collection for calibration and to document stability of measures over time. Manufacturer calibrations were performed twice a year as recommended. Each participant’s scan was analyzed with the latest software QDR for Windows V11.2.
Abdominal VAT and SAT areas (cm2) were measured with CT at the Baton Rouge General Medical Center, Baton Rouge, Louisiana. Participants lay in a supine position with arms overhead to obtain a cross-sectional image at the L4–L5 intervertebral space. Three different CT scanners were utilized for PCLS: GE High Speed Advantage (1996–2000; n = 805); GE LightSpeed Plus (2000–2007; n = 827); and GE LightSpeed VCT (2007–2008; n = 35). CT scanners were calibrated daily to air. CT imaging was transferred to Pennington Biomedical Research Center for analysis with commercially available software (Analyze; Analyze Direct, Rochester, MN). Abdominal VAT and SAT procedures for measuring cross-sectional area (cm2) have been previously described (22).
Covariates
Participant age was computed from birth and observation dates. Smoking status was self-reported during the screening process, and participants were classified as “non smokers,” “current smokers,” or “former smokers.” Menopausal status (premenopausal/postmenopausal) was determined in women from their age and responses to questions regarding their reproductive history. Women aged 55+ years of age or those who indicated that they can no longer have children because of achieving menopause were considered to be postmenopausal.
Statistical analysis
As an initial analytical step, Pearson correlation coefficients were calculated to assess pair-wise associations between anthropometric and adipose tissue measurements. General linear statistical models were used to investigate differences in relationships of WC or BMI to FM, SAT, and VAT, across sex and race groups in the total sample and within young and old age categories. We also considered the impact of smoking status and menopause status on these relationships. Extreme outliers were identified for each model with WC or BMI as a predictor separately for FM, SAT, and VAT outcomes. Any participant, in any of the models whose studentized residual was greater than 3, was removed from the analysis (total for all models: n = 50; 2.8%; resulting in final sample size of n = 1,667).
Covariates in each model for the overall sample included age group (18–39 years; 40–64 years), smoking, menopause (as appropriate), anthropometric measure (BMI or WC), and terms were also included for the interactions between anthropometric measure by age group, anthropometric measure by sex by race, and age group by race by sex. Smoking was not significant in the majority of the models, and was removed as a covariate in the final models. Due to significant age group interactions in the overall models, we further stratified the analyses by age group (18–39 years and 40–64 years).
RESULTS
Descriptive characteristics of the sample are presented in Table 1. AA men were younger (P < 0.0001) and had lower WC (P = 0.0002) than white men. AA women were younger (P < 0.0001) and had a smaller percentage who were postmenopausal, but had higher weight (P < 0.0001), BMI (P < 0.0001), and WC (P = 0.0005) than white women. White men were younger (P < 0.0001) and had greater weight (P < 0.0001), height (P < 0.0001), and WC (P < 0.0001) than white women. AA men were younger (P = 0.01), and had greater weight (P < 0.0001), height (P < 0.0001) and WC (P = 0.02), but smaller BMI (P = 0.0005), than AA women. Postmenopausal status in the 40–64 year age group was 43% in white women and 18% in AA women.
Table 1
Descriptive characteristics of white and African-American men and women in the Pennington Center Longitudinal Study (PCLS)
| Men
| Women
| |||
|---|---|---|---|---|
| White | African American | White | African American | |
| n | 489 | 120 | 666 | 392 |
| Age (years) | 42.6 ± 13.1a,b | 36.9 ± 13.2b | 47.3 ± 10.4a | 39.9 ± 10.8 |
| Weight (kg) | 93.6 ± 15.7b | 92.1 ± 16.9b | 78.1 ± 14.6a | 82.9 ± 14.7 |
| Height (cm) | 177.2 ± 6.6b | 177.4 ± 6.6a | 163.3 ± 5.8 | 163.5 ± 5.9 |
| BMI (kg/m2) | 29.8 ± 4.8 | 29.2 ± 4.8b | 29.3 ± 5.1a | 31.0 ± 5.2 |
| WC (cm) | 100.7 ± 13.0a,b | 95.3 ± 14.1b | 88.8 ± 13.3a | 91.9 ± 12.7 |
| Smoking status (%) | ||||
 Never Never | 74 | 76 | 74 | 88 |
 Former Former | 24 | 13 | 20 | 7 |
 Current Current | 2 | 11 | 6 | 5 |
| Postmenopausal (%) | NA | NA | 35 | 10 |
Data are presented as mean ± standard deviation.
WC, waist circumference.
Correlations between anthropometric measures and body fat
Correlations with WC were lowest for abdominal VAT (range: 0.73–0.77) compared to abdominal SAT (range: r = 0.82–0.92) and FM (range: r = 0.85–0.93). Similarly, the correlations with BMI were lowest for abdominal VAT (range: 0.61 – 0.69) compared to abdominal SAT (range: r = 0.86–0.93) and FM (range: r = 0.91–0.94). The correlation coefficients were all statistically significant (P < 0.0001) and similar across sex-by-race groups.
General linear models
In the general linear models for the total sample, significant interactions were observed between anthropometric measures and age group (age group by anthropometric measure was significant in five of six models; age group by race by sex was significant in two of the six models). Due to these significant age interactions, we stratified the analyses by age group, and we summarized the main and interaction effects for race and sex in the figures. We were not able to present the anthropometry-adjusted mean FM, SAT, and VAT values due to several significant interactions.
Figures 1–3 present the scatter plots for FM, SAT, and VAT with WC or BMI, respectively, by age group. Within the figures, we present statistical significance (P values) corresponding to the overall main effects for sex and race as well as significant interaction effects.
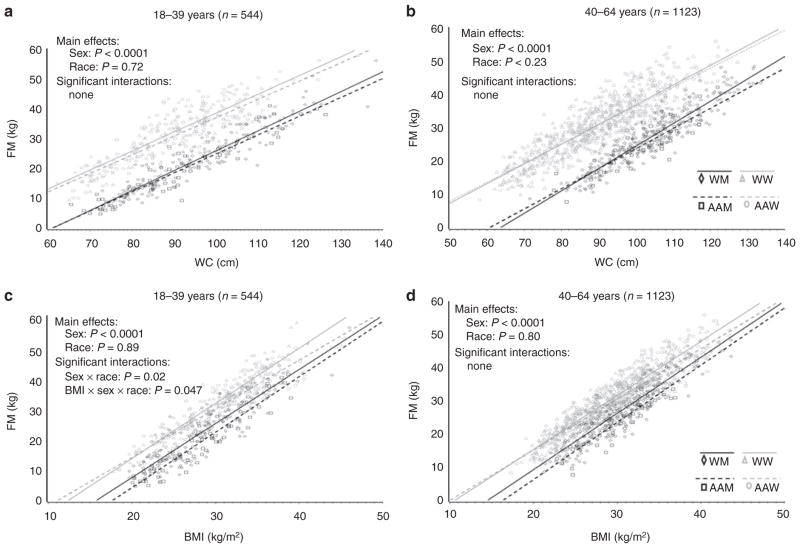
Relationship between FM and (a) WC in 18–39 years, (b) WC in 40–64 years, (c) BMI in 18–39 years, and (d) BMI in 40–64 years within sex-by-race groups. All correlations are significant at P < 0.0001. AAM, African-American men; AAW, African-American women; FM, total body fat; WC, waist circumference; WM, white men; WW, white women.
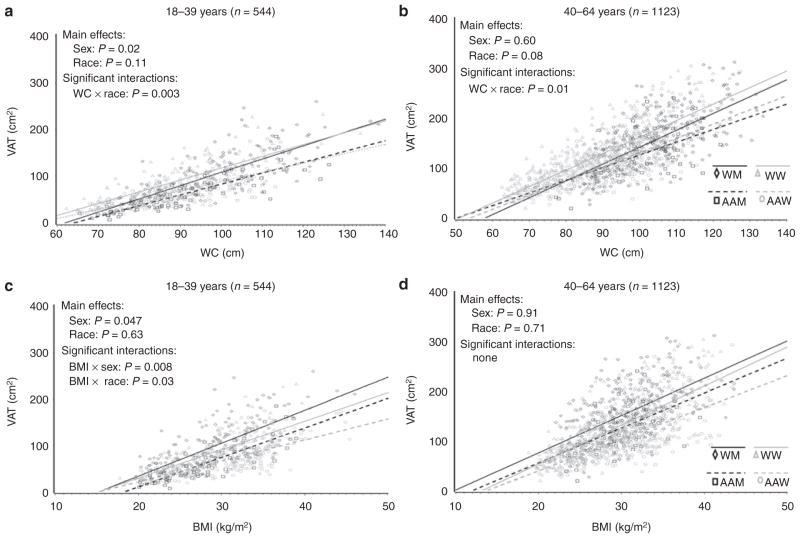
Relationship between VAT and (a) WC in 18–39 years, (b) WC in 40–64 years, (c) BMI in 18–39 years, and (d) BMI in 40–64 years within sex-by-race groups. All correlations are significant at P < 0.0001. AAM, African-American men; AAW, African-American women; VAT, visceral adipose tissue; WC, waist circumference; WM, white men; WW, white women.
Fat mass
Significant sex effects were observed for FM (Figure 1): across levels of WC and BMI, FM was significantly higher in women than in men. These sex effects were consistent across the younger and older age groups. Significant interactions were observed in the model for BMI in the younger age group. At higher levels of BMI the difference in FM between AA men and women becomes less, whereas the difference between white men and women appears to be consistent across the range of BMI (Figure 1c).
Subcutaneous adipose tissue
Significant main effects for sex were also observed for SAT (Figure 2): across levels of WC and BMI, SAT was significantly higher in women than in men. In the younger age group (Figure 2a), the difference between AA women and white women becomes less pronounced at higher levels of WC, but the opposite holds true for men. In older adults, the sex difference appears to become attenuated at higher levels of WC (Figure 2b). In the younger group, the difference in SAT between AA men and women is less pronounced at higher levels of BMI (Figure 2c) but the race difference was not significant in the older women or men regardless of BMI (Figure 2d).
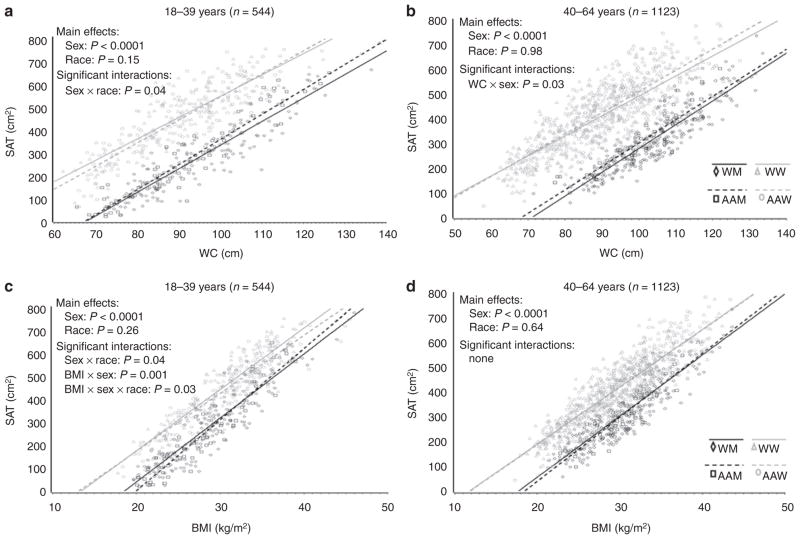
Relationship between SAT and (a) WC in 18–39 years, (b) WC in 40–64 years, (c) BMI in 18–39 years, and (d) BMI in 40–64 years BMI within sex-by-race groups. All correlations are significant at P < 0.0001. AAM, African-American men; AAW, African-American women; SAT, subcutaneous abdominal adipose tissue; WC, waist circumference; WM, white men; WW, white women.
Visceral adipose tissue
For VAT there were significant main effects for sex in the younger age group, but not in the older age group (Figure 3). However, as is evident from significant WC-by-race interactions, the effect of race becomes more pronounced at higher levels of WC, such that white men and women have higher levels of VAT than AA men and women (Figure 3a,b). There was a significant main effect for sex in the BMI model in the younger age group, and the interaction effects indicate that race and sex differences increased at higher levels of BMI (Figure 3c) but there were no significant effects in the older age group (Figure 3d).
DISCUSSION
The results revealed higher correlations for WC or BMI with FM and SAT than for VAT in each sex-by-race group. In addition, there were significant sex differences for all fat depots for a given level of BMI or WC. Regardless of WC or BMI, women had higher levels of SAT and FM than men. For both WC and BMI, sex effects for VAT were also significant in the younger age group; and the differences by sex and race increased across levels of WC and BMI.
Both WC and BMI were more highly correlated with FM and SAT than with VAT in all sex-by-race groups, which supports the results of other studies that have found that WC and BMI have higher correlations with FM and/or SAT than with VAT (18,23–26). The higher correlations between WC and SAT and FM than with VAT were expected, as WC is an assessment of both abdominal SAT and VAT (24). Furthermore, regardless of WC, there is about 3.5 times more SAT than VAT in our study, as well as in other studies (27) which may explain the higher correlations of WC to FM.
In general, whether adjusting SAT for WC or BMI, similar sex differences were observed. For the same BMI, other studies were consistent with our findings for sex differences: men have lower FM (7,8,14) and lower SAT (7,9,10), when compared to women. We also observed consistent sex differences across the age groups for SAT and FM in adults. While the sex effect was significant for VAT, there was not a consistent relationship for men and women across the continuum of either WC or BMI. Previous research has shown either similar levels of VAT in men and women (18), or found racial differences at the same BMI: white men and women have higher VAT than AA men and women (8,11,12,20,27,28), which may demonstrate a race and sex interaction. The interaction in the current analysis between anthropometric measure and race was significant for VAT, and this may explain the variation of sex effects across the range of WC and BMI. Finally, sex differences for WC- and BMI-adjusted VAT were only significant in the younger age group (18–39 years). A possible explanation for our discrepant findings between the two age groups for VAT may be due to the significantly older age of women in this sample when compared to men. Aging is associated with increases in VAT (16,29–31) and WC shows greater increases with age in women compared to men of the same race and similar age (30). These results suggest that sex effects of VAT diminish with aging. Thus not only are gender-specific cut points needed to delineate sex differences at the same WC and BMI for VAT, SAT, and FM, but also, age specific cut points for WC may be necessary for representing VAT.
Some previous studies have found no race differences in WC- or BMI-adjusted VAT (14,32), SAT (12,32), and FM (14). Our results found no significant main effects of race in either age group; however, a number of interactions involving race were observed indicating that race differences do exist at certain levels or WC or BMI. For VAT, the race effects were more pronounced at higher levels of adiposity, such that white men and women tended to have higher levels of VAT for a given BMI or WC.
A major strength of this study is the large sample of white and AA men and women with precise measures of adiposity from CT and DXA. Further, the sample spans a wide range of ages (18–64 years), BMI (17–49 kg/m2) and WC (58–147 cm) enabling robust comparisons and generalizability. However, the PCLS is not a population-based sample, rather the subjects are volunteers who have participated in clinical research studies. Another limitation of the current study is the lack of data in this particular sample for medication use, chronic disease status, and lifestyle behaviors such as nutritional intake, physical activity, and/or cardiorespiratory fitness. These characteristics have known influences on adipose tissue accumulation; however, we were able to control for other behavioral and physiological modifiers such as age, sex, race, smoking status, and menopause. Finally, this is a cross-sectional study, and the age analyses do not reflect actual changes over time.
In conclusion, the current research demonstrated sex and race differences in the relationship between WC, BMI and VAT, SAT, and FM. In some cases these differences were simple main effects, and in other cases they involved complex interactions. The importance of these findings implies that specific WC and BMI cut points may not reflect the same level of FM or abdominal obesity between white and AA men and women. Further, significant interactions indicated that the level of depot-specific adiposity differed across levels of the anthropometric indicator. In most cases, the race or sex differences increased at higher levels of adiposity. Future research needs to identify sensitive and specific BMI and WC thresholds which better delineate obesity-related cardiometabolic risk among different sex and age groups.
Acknowledgments
We gratefully acknowledge the contributions of Emily Mire and Connie Murla for data management and to the many clinical scientists and staff of the Pennington Biomedical Research Center who have contributed data to the development of the Pennington Center Longitudinal Study, in particular Drs William Cefalu, Nikhil Dhurandhar, Lilian Levitan, Timothy Church, Paula Geiselman, Alok Gupta, Corby Martin and Thomas Gettys. We also acknowledge Julia St Amant for her expert supervision of the CT acquisition and for the analysis of the majority of the CT scans reported herein.
Footnotes
DISCLOSURE
P.T.K. is partially funded by the Louisiana Public Facilities Authority Endowed Chair in Nutrition, C.B. is partially funded by the John W. Barton, Sr. Endowed Chair in Genetics and Nutrition, and E.R. is partially supported by the Douglas L. Gordon Chair in Diabetes and Metabolism.
References
Full text links
Read article at publisher's site: https://doi.org/10.1038/oby.2010.248
Read article for free, from open access legal sources, via Unpaywall:
https://onlinelibrary.wiley.com/doi/pdfdirect/10.1038/oby.2010.248
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/102501976
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1038/oby.2010.248
Article citations
Obesity-related renal dysfunction: gender-specific influence of visceral adiposity and early impact of metabolic and bariatric surgery.
Front Endocrinol (Lausanne), 15:1440250, 14 Oct 2024
Cited by: 0 articles | PMID: 39469576 | PMCID: PMC11513314
Interaction between non-alcoholic fatty liver disease and obesity on the risk of developing cardiovascular diseases.
Sci Rep, 14(1):24024, 14 Oct 2024
Cited by: 0 articles | PMID: 39402185 | PMCID: PMC11473819
Agreement between equation-derived body fat estimator and bioelectrical impedance analysis for body fat measurement in middle-aged southern Indians.
Physiol Rep, 12(20):e70095, 01 Oct 2024
Cited by: 1 article | PMID: 39431546 | PMCID: PMC11492144
Association of diabetic retinopathy with plasma atherosclerotic index, visceral obesity index, and lipid accumulation products: NHANES 2005-2008.
Lipids Health Dis, 23(1):331, 10 Oct 2024
Cited by: 0 articles | PMID: 39390607 | PMCID: PMC11465674
Development and cross-validation of prediction equations for body composition in adult cancer survivors from the Korean National Health and Nutrition Examination Survey (KNHANES).
PLoS One, 19(10):e0309061, 04 Oct 2024
Cited by: 0 articles | PMID: 39365800 | PMCID: PMC11451997
Go to all (326) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Visceral fat, waist circumference, and BMI: impact of race/ethnicity.
Obesity (Silver Spring), 16(3):600-607, 17 Jan 2008
Cited by: 200 articles | PMID: 18239557
Relationship of anthropometric indices to abdominal and total body fat in youth: sex and race differences.
Obesity (Silver Spring), 22(5):1345-1350, 19 Feb 2014
Cited by: 24 articles | PMID: 24493150 | PMCID: PMC4008658
Clinical utility of visceral adipose tissue for the identification of cardiometabolic risk in white and African American adults.
Am J Clin Nutr, 97(3):480-486, 30 Jan 2013
Cited by: 51 articles | PMID: 23364010 | PMCID: PMC3578400
Crossvalidation of anthropometry against magnetic resonance imaging for the assessment of visceral and subcutaneous adipose tissue in children.
Int J Obes (Lond), 30(1):23-30, 01 Jan 2006
Cited by: 235 articles | PMID: 16344845
Review




