Abstract
Free full text

PNAS Plus
Antigen expression level threshold tunes the fate of CD8 T cells during primary hepatic immune responses
Associated Data
Significance
The liver possesses unique immunological properties, with the capability of inducing tolerance upon transplantation, yet is also the target of immune-mediated damage in chronic viral hepatitis. To investigate the basis of these dichotomous outcomes, we manipulated several determinants capable of influencing outcomes of hepatic–immune interactions. Our findings reveal that a threshold of antigen expression within the liver is the dominant factor determining the fate of CD8 T cells recognizing intrahepatic antigen, irrespective of their affinity for antigen or the site of initial antigen encounter, with high-level antigen expression leading to exhaustion of T cell function. To our knowledge, for the first time, this study provides a unified model explaining the divergent consequences of hepatic–immune interactions.
Abstract
CD8 T-cell responses to liver-expressed antigens range from deletional tolerance to full effector differentiation resulting in overt hepatotoxicity. The reasons for these heterogeneous outcomes are not well understood. To identify factors that govern the fate of CD8 T cells activated by hepatocyte-expressed antigen, we exploited recombinant adenoassociated viral vectors that enabled us to vary potential parameters determining these outcomes in vivo. Our findings reveal a threshold of antigen expression within the liver as the dominant factor determining T-cell fate, irrespective of T-cell receptor affinity or antigen cross-presentation. Thus, when a low percentage of hepatocytes expressed cognate antigen, high-affinity T cells developed and maintained effector function, whereas, at a high percentage, they became functionally exhausted and silenced. Exhaustion was not irreversibly determined by initial activation, but was maintained by high intrahepatic antigen load during the early phase of the response; cytolytic function was restored when T cells primed under high antigen load conditions were transferred into an environment of low-level antigen expression. Our study reveals a hierarchy of factors dictating the fate of CD8 T cells during hepatic immune responses, and provides an explanation for the different immune outcomes observed in a variety of immune-mediated liver pathologic conditions.
The liver is acknowledged to possess unique tolerogenic properties, which have likely evolved to maintain immunological unresponsiveness toward food-derived and microbial antigens that enter the circulation via the gut (1, 2). This tolerogenic capability of the liver is demonstrated in animal models of liver transplantation, in which liver allografts are accepted across complete MHC mismatch barriers and are able to protect other donor tissues from rejection (reviewed in ref. 3). In humans, the tolerogenic hepatic environment is likely to contribute to impaired immune clearance of the hepatitis B virus (HBV) and hepatitis C virus (HCV), which result in persistent infection in a significant proportion of exposed individuals and are associated with major morbidity and mortality. In contrast, effective immune responses to hepatotropic pathogens leading to resolution of infection are observed in most hepatitis A and E virus infections, the majority of individuals infected with HBV during adulthood, and a minority of those infected by HCV (reviewed in refs. 4, 5). The liver is also susceptible to a variety of autoimmune-mediated conditions (6). Collectively, these observations indicate that effective immune responses can be initiated and/or sustained in the liver despite its apparent predisposition toward the generation of tolerance. Unfortunately, there is no small animal model in which to study the parameters that determine the balance between intrahepatic immunity and tolerance in viral hepatitis. Thus, the factors that shape immune outcome have not yet been identified.
By studying the fate of antigen-specific CD8 T cells transferred into mice expressing antigen in the liver, it has been shown that, despite being a nonlymphoid organ, the liver is able to support primary CD8 T-cell activation (7). However, depending on the choice of antigen expressed and mode of delivery, the outcome of intrahepatic CD8 T-cell activation has been varied, ranging from deletion and/or functional silencing (8–10) to cytotoxic T lymphocyte (CTL) development (11, 12). This observed diversity of T-cell fates parallels the heterogeneous outcomes of liver-immune interactions observed during hepatotropic viral infections in humans. Thus, reconciliation of these findings holds the potential to yield critical insights into the immunopathological basis of immune-mediated liver disease as well as liver-associated tolerance.
In this study, we developed an integrated system in which we manipulated parameters predicted to influence the generation of effector CD8 T cells encountering their cognate antigen on hepatocytes. By identifying three key determinants of the generation of functional effector cells in response to hepatocyte-expressed antigen, this study provides, for the first time to our knowledge, a unified model that explains and predicts the functional outcome of CD8 T-cell activation by liver-expressed antigen and reconciles findings from a number of previous studies that addressed this question.
Results
A Membrane Antigen Expressed by Hepatocytes Is Efficiently Cross-Presented in Lymphoid Tissues.
By studying the response of antigen-specific T cells adoptively transferred into transgenic mice that expressed the cognate antigen within the liver, we have previously demonstrated that the site of primary CD8 T-cell activation determines immune outcome. Our results indicated that primary activation in the liver committed T cells to develop into poor effectors and undergo premature death, whereas activation in the lymph nodes (LNs) promoted full effector differentiation (13). As antigen expressed by hepatocytes is likely to be presented to CD8 T cells within the liver via direct presentation by hepatocytes and within lymphoid tissues by cross-presenting antigen-presenting cells (APCs), we developed a model to determine the relative contribution of the direct and cross-presentation pathways to T-cell development following de novo expression of antigen by hepatocytes.
To restrict antigen expression to the liver, we generated recombinant adenoassociated virus (rAAV) vectors that express a membrane-anchored form of ovalbumin (mOVA) in hepatocytes. To increase specificity, rAAVs were pseudoserotyped to type-8 capsid and a hepatocyte-specific promoter/enhancer system was used. A standard dose of rAAV.mOVA [5 × 1010 vector genome copies (vgc)] administered i.v. induced OVA expression on 100% of hepatocytes but not on F4/80+ Kupffer cells or CD31+ liver endothelial cells (Fig S1 A and B). By using this rAAV vector, we have also shown that antigen was not detected at extrahepatic sites (14). Serum alanine aminotransferase levels were not increased after rAAV.mOVA treatment (Fig. S1C), indicating lack of associated liver damage. Liver sections confirmed normal tissue histology.
To determine whether a membrane-localized antigen expressed by hepatocytes could be cross-presented in lymphoid tissues, naive H-2Kb–restricted OVA-specific T-cell receptor (TCR) transgenic CD8 T cells specific for the OVA-derived peptide SIINFEKL (OT-I) were adoptively transferred into C57BL/6 (B6) recipients treated with rAAV.mOVA. Lymphocytes from the liver, spleen, LNs, and blood were harvested at 3 h after OT-I T-cell transfer and examined for expression of CD69, an early activation marker. CD69hi OT-I cells were found in the liver, spleen, and LNs, but not in the blood, indicating they were activated in situ in these various organs (Fig. 1A). To test whether the observed extrahepatic activation of OT-I was caused by cross-presentation, we sought to restrict initial antigen encounter to that mediated via direct presentation by hepatocytes. To achieve this, we used rAAV to deliver a transgene encoding H-2Kb (rAAV.Kb) to bm1 mice, which express the variant MHC class I molecule H-2Kbm1 (14) (Fig. S2). H-2Kbm1 forms a complex with the OVA-derived peptide SIINFEKL but does not mediate effective activation of OT-I T cells (15). We found that OT-I T cells transferred into bm1 mice coadministered rAAV.mOVA and rAAV.Kb were activated only in the livers and not in the LNs or spleens at 3 h after transfer (Fig. 1B). In an alternative approach, Alb-Kb mice expressing transgenic H-2Kb in hepatocytes under the control of the hepatocyte-specific albumin promoter (13, 16, 17) were bred onto the bm1 background to generate Alb-Kb.bm1 recipients. OT-I T cells that were transferred into Alb-Kb.bm1 recipients treated with rAAV.mOVA were also found to be activated only within the liver (Fig. 1C). Together, these results suggest that extrahepatic OT-I activation observed in the LNs and spleens of rAAV.mOVA-treated B6 mice was mediated by cross-presentation rather than by direct presentation of hepatocyte-expressed mOVA.
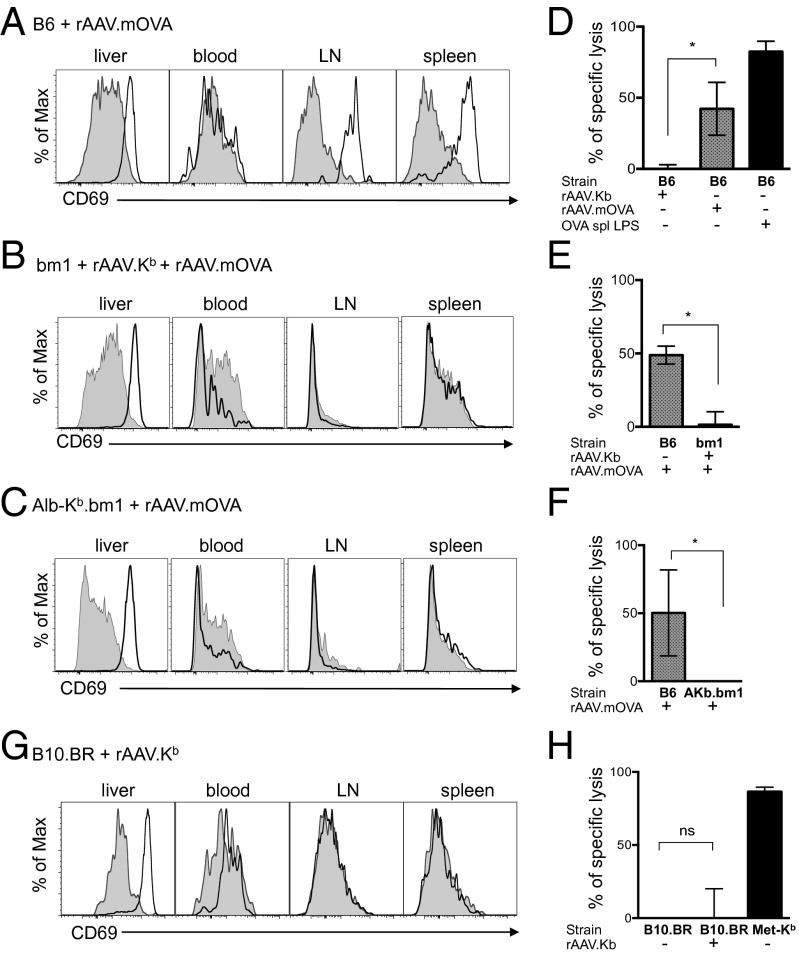
Extrahepatic OT-I T-cell activation and CTL activity in B6 mice treated with rAAV.mOVA is associated with cross-presentation. (A) Expression of CD69 on donor (CD45.1+) CD8+ OT-I T cells 3 h after transfer into B6 mice pretreated with rAAV.mOVA (5 × 1010 vgc, administered 7 d earlier). (B) CD69 expression on donor OT-I CD8+ T cells 3 h after transfer into bm1 mice treated with rAAV.mOVA and rAAV.Kb (5 × 1010 vgc each, administered 7 d earlier). (C) CD69 expression on donor CD8+ OT-I T cells 3 h after transfer into Alb-Kb.bm1 treated with rAAV.mOVA (5 × 1010 vgc, administered 7 d earlier). (D–F) In vivo cytotoxicity against SIINFEKL-coated splenocytes 1 wk after 106 OT-I LN cells were transferred into B6, bm1, or Alb-Kb.bm1 mice treated with rAAVmOVA and/or rAAV.Kb (5 × 1010 vgc) the following day. OVA spl LPS: i.v. transfer of 107 OVA-coated splenocytes and 1 μg LPS 1 wk earlier. (G) CD69 expression by donor CD8+ DesRAG−/− T cells at 3 h after transfer into B10.BR mice pretreated with rAAV.Kb (5 × 1010 vgc, administered 7 d earlier). (H) In vivo cytotoxicity against H-2Kb+ splenocytes 1 wk after transfer of 5 × 105 DesRAG−/− LN cells into B10.BR mice that were treated with rAAV.Kb (1011 vgc) the following day. Transgenic Met-Kb mice (expressing H-2Kb in the liver and lymphoid tissues) adoptively transferred with 106 DesRAG−/− LN T cells were used as positive controls. (A, B, C, and G) CD69 expression of OT-I or DesRAG−/− T cells transferred into untreated mice of each strain are shown as shaded plots. Overlays represent at least six mice per group from two or three independent experiments. Bar graphs show mean percent ± SD of specific killing measured in three mice per group, with at least three independent experiments performed. [*Significant at P < 0.05; ns, nonsignificant; differences tested by ANOVA and Bonferroni post hoc test (D and H) or Student t test (E and F).]
T-Cell Activation by Cross-Presentation in Lymphoid Tissues Influences CTL Activity.
To examine the contributions of the direct presentation and cross-presentation pathways to CTL development, we transferred OT-I T cells into B6, bm1, or Alb-Kb.bm1 mice, and treated them 1 d later with rAAV.mOVA, with coinjection of rAAV.Kb for bm1 mice. CTL function was assessed 1 wk after OT-I transfer by in vivo cytotoxicity assay using SIINFEKL-pulsed B6 splenocytes as targets. CTL activity was detected only in B6 mice, in which cross-presentation was present (Fig. 1 D–F). The lack of CTL activity in bm1 recipients treated with rAAV.Kb (Fig. 1E) and Alb-Kb.bm1 (Fig. 1F) was not caused by a failure of OT-I T cells to proliferate to the same extent as in B6 mice, as the number of OT-I T cells recovered from these strains after rAAV.mOVA treatment were similar to those detected in B6 mice (Fig. S3).
To investigate the response of CD8 T cells with different specificity, we tested the outcome of CD8 Des T-cell activation following adoptive transfer into rAAV.Kb-treated syngeneic B10.BR (H-2k) recipients. The Des TCR is specific for H-2Kb complexed with endogenous peptide. Hence, in rAAV.Kb-treated B10.BR recipients, Des T cells are predicted to recognize H-2Kb expressed by hepatocytes, but not epitopes derived from the H-2Kb protein presented in the context of recipient H-2k molecules. This model therefore essentially excludes the contribution of recipient cross-presentation to Des T-cell activation (13, 16, 17). Consistent with our previous findings in Alb-Kb transgenic mice that express H-2Kb only on hepatocytes (13, 16, 17), Des T-cell activation at 3 h after transfer into rAAV.Kb-treated mice was restricted to the liver (Fig. 1G). Despite efficient intrahepatic activation leading to proliferation of transferred Des T cells (Fig. S4), CTL function never developed in vivo (Fig. 1H). Consistent with our previous findings (13), these results also suggested a potential requirement for antigen presentation in secondary lymphoid organs for effective CTL formation.
CTLs Generated in the Presence of Extrahepatic Cross-Presentation Were Silenced by Persistent Intrahepatic Antigen Expression.
Although OVA-specific cytotoxicity was consistently detected in rAAV.mOVA-treated B6 mice at 1 wk after OT-I transfer, this response was not as effective as that seen after OT-I stimulation with OVA-coated splenocytes and LPS (Fig. 1D, black bar indicates positive control). Extension of in vivo cytotoxicity measurements to week 3 after OT-I transfer revealed no detectable residual OT-I CTL activity in rAAV.mOVA-treated B6 mice (Fig. 2A). This was not caused by T-cell deletion, as OT-I cells were still present and were sequestered in the livers of recipient mice (Fig. 2B), which continued to express high levels of OVA (Fig. 2C). Restimulation of these mice by i.v. transfer of OVA-coated splenocytes and LPS led to an increase in OT-I T cell numbers but did not restore cytotoxic function (Fig. 2B), suggesting that intrahepatic T cells retained their ability to recognize antigen and proliferate but were functionally silenced by extrinsic or intrinsic mechanisms. A second cohort of OT-I T cells transferred into these mice proliferated to the same extent as those transferred into rAAV.mOVA-treated controls that had not received the first cohort of OT-I T cells (Fig. 2D), confirming antigen availability at this time point. Together, these results indicate that, although CTLs were generated via cross-presentation in secondary lymphoid tissues, they were subsequently “silenced” at the functional level between 1 and 3 wk postactivation.
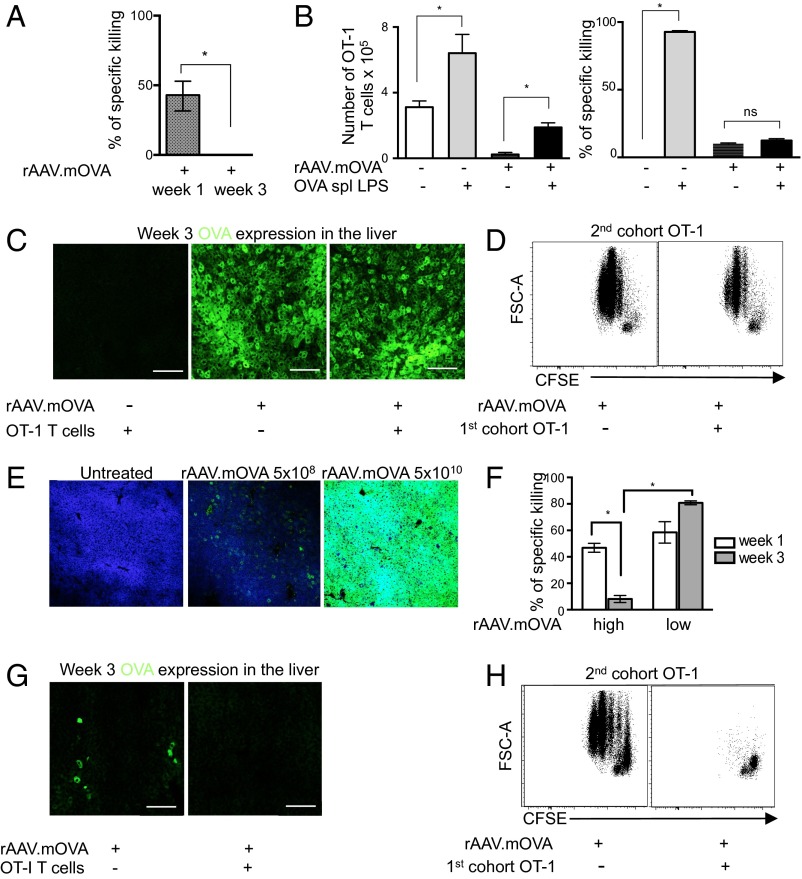
Cytotoxic OT-I T cells were silenced at 3 wk by high but not low levels of intrahepatic antigen. (A) In vivo cytotoxicity in the spleen at 1 wk and 3 wk after transferring 106 OT-I LN cells into B6 mice treated with rAAV.mOVA (5 × 1010 vgc) the following day. (B) Ability of 107 OVA-coated splenocytes and 1 µg LPS (OVA spl LPS) delivered i.v. to restore proliferation (Left) or cytotoxicity (Right) of OT-I T cells transferred into B6 mice and treated with rAAV.mOVA (5 × 1010 vgc) 6 wk earlier. Total T-cell numbers (in spleen, liver, LNs, and blood) and cytotoxicity in the spleen were measured 7 d after restimulation. Bars show mean ± SD measured in three mice per group. (C) OVA expression in liver 3 wk after transferring 106 OT-I LN cells into B6 mice treated with rAAV.mOVA (5 × 1010 vgc) the following day. Controls did not receive OT-I cells or were treated with rAAV.Kb (5 × 1010 vgc). Images are representative of livers from three mice per group. (D) OT-I T cells were not able to clear OVA-expressing hepatocytes in mice treated with a high dose of rAAV.mOVA. B6 mice were adoptively transferred with a first cohort of 106 CD45.2+ OT-I LN cells or PBS solution and then, 1 d later, treated with rAAV.mOVA (5 × 1010 vgc). After 3 wk, a second cohort of 2 × 106 CFSE-labeled CD45.1+ OT-I cells was adoptively transferred into the same recipient mice. Proliferation of the second cell cohort was assessed by gating on liver CD8+ CD45.1+ 2 d after transfer and assessing CFSE dilution. Flow plots are representative of five or seven mice per group from two independent experiments. (E) Expression of OVA in the liver 7 d after high- and low-dose rAAV.mOVA treatment of B6 mice. OVA expression was detected by immunofluorescence as per C. (F) OT-I cytotoxicity in the spleen at week 1 and week 3 after transfer of 106 OT-I LN cells into B6 mice treated with high- or low-dose rAAV.mOVA as indicated. (G) Efficient clearance of OVA-expressing hepatocytes in B6 mice by week 3 after transfer of 106 OT-I LN cells and low-dose inoculation with rAAV.mOVA (5 × 108 vgc) compared with mice that did not receive OT-I T cells. (H) OT-I T cells cleared detectable expression of OVA by hepatocytes in mice treated with a low dose of rAAV.mOVA. B6 mice were adoptively transferred with a first cohort of 106 CD45.2+ OT-I LN cells or PBS solution and then, 1 d later, treated with rAAV.mOVA (5 × 108 vgc). After 3 wk, a second cohort of 2 × 106 CFSE-labeled CD45.1+ OT-I cells was adoptively transferred into the same recipient mice. Proliferation of the second cell cohort was assessed in the liver by gating on CD8+ CD45.1+ lymphocytes 2 d after transfer and assessing CFSE dilution. Proliferation of the second OT-I cohort was only observed in controls that did not receive the first cohort of OT-I T cells. Flow plots are representative of at least seven mice per group in two independent experiments.
Lower Frequencies of Antigen-Expressing Hepatocytes Led to Development of CTLs That Persistently Maintained Function.
The induction of antigen expression on almost all hepatocytes after a standard dose of rAAV treatment is akin to that observed in transgenic mice in which antigen is continually expressed on hepatocytes, and to liver transplantation, in which all liver cells express donor antigen. However, it is unlikely that these levels of antigen expression are achieved early in infections by hepatotropic viruses or by current gene therapy protocols. To investigate the effects of lower levels of antigen expression, we reduced the dose of nonreplicative rAAV vector administered. B6 mice were treated with 1/100th of the standard dose of rAAV.mOVA (5 × 108 vgc), which resulted in OVA expression by a small proportion of hepatocytes (Fig. 2E). Following administration of low-dose rAAV.mOVA, OT-I also developed CTL function at week 1 in B6 mice (Fig. 2F). However, in contrast to the “silencing” of OT-I function observed after high-dose rAAV treatment, CTL activity in the low-dose–treated group persisted at week 3 (Fig. 2F). In these mice, no detectable OVA expression was found in the liver 3 wk following treatment (Fig. 2G). The complete clearance of residual OVA-expressing cells was confirmed by the failure of a second cohort of adoptively transferred OT-I cells to be activated and proliferate in these recipients (Fig. 2H). Thus, in B6 mice, low numbers of OVA-expressing hepatocytes were sufficient to trigger OT-I CTL that mediated clearance of antigen expression, and this was associated with persisting CTL activity at week 3.
A Threshold in the Number of Antigen-Expressing Hepatocytes Determines CD8 T-Cell Outcome.
These data indicated that, in B6 mice, the number of hepatocytes transduced was a key determinant of CD8 T-cell fate: high intrahepatic antigen load was associated with silencing of CTL. To determine the level of initial hepatocyte transduction required for CTL silencing and to explore the effects of antigen expression levels more akin to those occurring during hepatotropic viral infections (4), we assessed OT-I CTL activity in B6 mice treated with intermediate doses of rAAV 3 wk earlier. To facilitate quantification of antigen-expressing hepatocytes, we generated a new rAAV vector that expressed GFP bicistronically with mOVA (rAAV.GFP-mOVA). Administration of a standard dose of this new vector (5 × 1011 vgc) also led to 100% transduction of hepatocytes, indicating comparable efficacy of this vector with rAAV.mOVA (Fig. 3A). Similar to rAAV.mOVA-treated mice, CTL activity was not observed in mice treated with the standard (high) dose of rAAV.GFP-mOVA, but was detected in mice treated with lower doses of rAAV. CTL function was maintained only when less than 25% of hepatocytes were transduced, indicating that a threshold existed for initial transduction levels required for CTL silencing (Fig. 3B).

A threshold of intrahepatic antigen expression determines the functional outcome of CD8 T-cell responses. (A) GFP expression in B6 mice treated with PBS solution or 1011 vgc of rAAV.GFP-mOVA for 7 d. Deconvolution micrographs of fixed liver sections stained with DAPI (blue) and phalloidin-Alexa Fluor 594 (red) with GFP expression in green show 100% transduction efficiency. (B) In vivo cytotoxicity 3 wk after transfer of 106 OT-I LN cells into B6 mice treated with a range of rAAV.GFP-mOVA doses, plotted against proportion of GFP+ hepatocytes in mice not injected with T cells.
Low Frequencies of Antigen-Expressing Hepatocytes Could Promote CTL Development in the Absence of Cross-Presentation, Depending on T-Cell Specificity.
Based on our findings that cross-presentation was associated with CTL generation in B6 mice treated with high-dose rAAV.mOVA (Fig. 1), we hypothesized that exclusion of cross-presentation would also prevent CTL development after low-dose rAAV.mOVA treatment. To test this, OT-I T cells were transferred into Alb-Kb.bm1 mice treated with a low dose (5 × 108 vgc) of rAAV.mOVA, or into bm1 mice coadministered high-dose rAAV.Kb and low-dose rAAV.mOVA. Surprisingly, we found high levels of CTL activity at 1 and 3 wk after OT-I transfer in both recipient strains despite the exclusion of cross-presentation (Fig. 4). CTL development was not mediated by residual cross-presenting APCs cotransferred with OT-I T cells, as robust CTL responses were also found when donor cells from OT-I mice backcrossed to bm1 were used (Fig. S5). These results showed that, after low-dose rAAV treatment, direct activation of OT-I T cells exclusively by OVA-expressing hepatocytes was able to prime CTLs by week 1 and that these CTLs were not silenced at week 3.
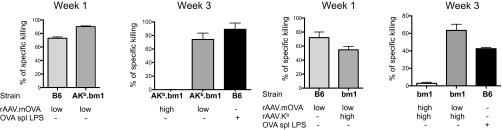
Exclusion of cross-presentation at low antigen doses did not prevent OT-I T cells developing into CTL after stimulation with high-affinity WT OVA. In vivo cytotoxicity at week 1 and week 3 following adoptive transfer of 106 OT-I T cells into B6, Alb-Kb.bm1, or bm1 mice treated with high-dose (5 × 1010 vgc) or low-dose (5 × 108 vgc) rAAV.mOVA and/or rAAV.Kb the following day, as indicated. OVA spl LPS, B6 mice injected with OVA-coated B6 splenocytes and 1 µg LPS 7 d earlier.
It was unexpected that hepatocytes could induce OT-I development into cytotoxic effectors by direct-presentation, as we have shown consistently in the past that naive CD8 Des T cells exclusively activated by hepatocytes developed poor CTL function and/or died prematurely, resulting in undetectable CTL activity in vivo (18). However, the outcome of intrahepatic Des T-cell activation had never been assessed in the setting of low H-2Kb antigen expression. We therefore measured Des CTL function in B10.BR mice treated with low-dose rAAV.Kb (5 × 108 vgc). Des T cells underwent activation and proliferation in these animals (14), but were unable to kill H-2Kb–expressing target cells in vivo (Fig. 5A). In these low-dose rAAV.Kb-treated mice that also received Des T cells, H-2Kb–expressing hepatocytes were still present at week 3, as demonstrated by immunofluorescent staining (Fig. 5B) and by their ability to stimulate proliferation of a second cohort of adoptively transferred naive Des T cells (Fig. 5C). These results suggest that, although Des T cells proliferated in response to low frequencies of H-2Kb-expressing hepatocytes, they failed to develop sufficient CTL function to clear antigen-expressed hepatocytes. Therefore, in contrast to OT-I T cells, Des T cells exclusively activated by hepatocytes did not develop into CTL at low antigen doses.
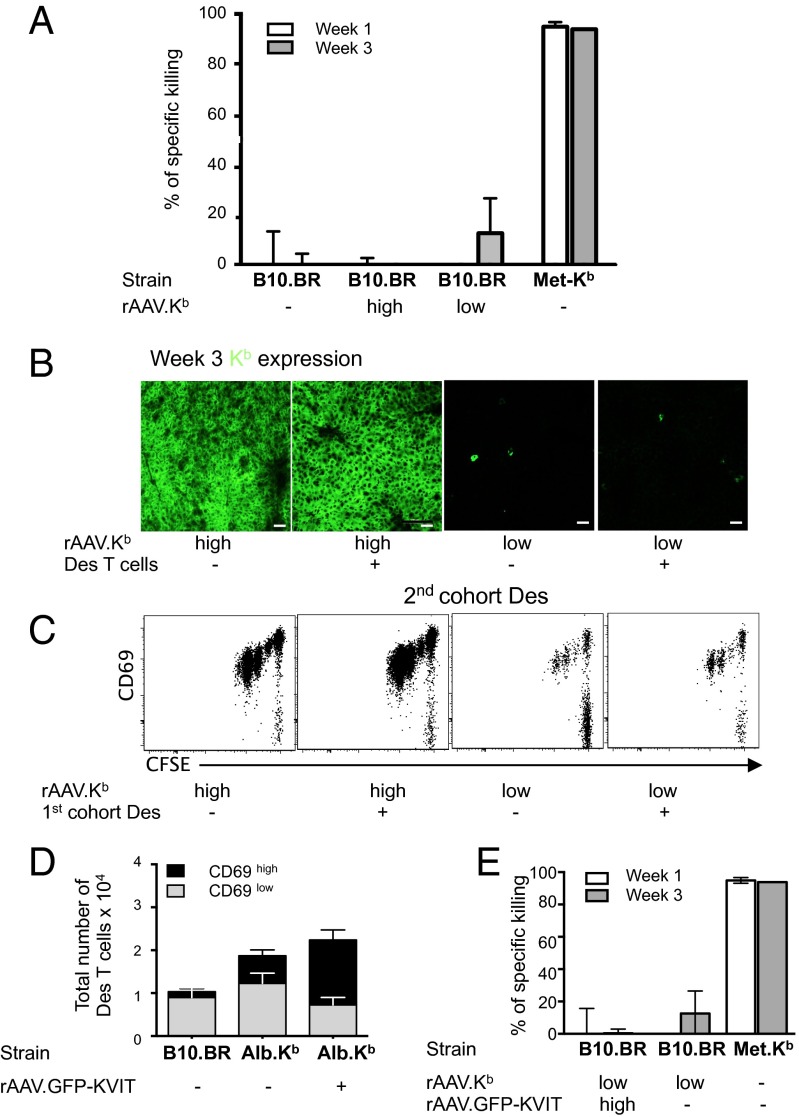
Lack of Des CTL development at low antigen dose was not a result of low pMHC occupancy. (A) In vivo cytotoxicity specific to H-2Kb+ target splenocytes at week 1 and week 3 after adoptive transfer of 1.5 × 106 DesRAG−/− LN cells into B10.BR mice treated with high- (5 × 1010 vgc) or low-dose (5 × 108 vgc) rAAV.Kb the following day. (B) Persisting H-2Kb expression in B10.BR mice treated with high- and low-dose rAAV.Kb, whether or not they received 106 DesRAG−/− LN cells the day before rAAV treatment. (C) Des T cells were unable to clear H-2Kb+ hepatocytes after 3 wk in mice treated with rAAV-Kb. B10.BR mice were adoptively transferred with a first cohort of 106 DesRAG−/− LN cells or PBS solution and then, 1 d later, treated with rAAV.Kb (5 × 1010 or 5 × 108 vgc). After 3 wk, a second cohort of 2 × 106 CFSE-labeled DesRAG−/− cells was adoptively transferred into the same recipient mice. Proliferation of the second cell cohort was assessed by gating on CD8+ CFSE+ cells 2 d after transfer and assessing CFSE dilution. (D) Total numbers of Des T cells and numbers of recently activated CD69hi Des T cells were quantified in the liver at 3 h after 106 DesRAG−/− LN cells were injected into B10.BR or Alb-Kb mice treated with rAAV.GFP-KVIT 7 d earlier. Bar graphs show mean ± SD of three mice. (E) In vivo cytotoxicity measured at weeks 1 and 3 after transfer of 106 DesRAG−/− LN cells into B10.BR mice treated with indicated doses of rAAV.Kb and/or rAAV.GFP-KVIT the following day. Met-Kb mice receiving 1.5 × 106 DesRAG−/− LN cells 5 d before cytotoxicity assay were used as positive controls. Bar graphs show mean percent ± SD of specific killing measured in three mice per group for two independent experiments.
Increasing Peptide:MHC Complex Occupancy Did Not Alter the Outcome of Des T-Cell Activation by Hepatocytes.
One potential explanation for the different functional outcomes observed after Des T-cell and OT-I T-cell stimulation in the liver was the amount of antigen expressed in each hepatocyte, as this would affect the number of peptide:MHC complexes (pMHC) available for TCR recognition and hence T-cell activation. It has been reported that the self-peptides recognized by the Des TCR in the context of H-2Kb are present only at low levels, estimated at 200 copies per cell, corresponding to ~0.3% H-2Kb occupancy (19). In contrast, H-2Kb occupancy by SIINFEKL can range from 10% to 80% (corresponding to 3,000–85,000 H-2Kb:SIINFEKL complexes per cell) depending on the form and amount of OVA expressed (20). To increase the number of H-2Kb:self-peptide complexes available to Des T cells, we replaced SIINFEKL in our expression construct with KVITFIDL, one of three epitopes that associate with H-2Kb for Des TCR recognition. Treatment of Alb-Kb mice with this vector (rAAV.GFP-KVIT) increased Des T-cell activation and retention in the liver compared with untreated controls (Fig. 5D), suggesting that treatment with rAAV.GFP-KVIT was effective in increasing the numbers of H-2Kb:KVITFIDL complexes. However, in contrast to the outcome of OT-I responses following administration of low-dose OVA, in which persisting CTL responses were observed, we did not detect Des CTL generation in B10.BR mice coadministered low-dose rAAV.Kb with high-dose rAAV.GFP-KVIT (Fig. 5E), suggesting that differences in MHC occupancy did not explain the different fates of OT-I and Des T cells.
TCR:pMHC Affinity Influences the Outcome of T-Cell Activation in Response to Liver-Expressed Antigen.
Another potential explanation for the different functional outcomes observed after Des and OT-I T-cell stimulation by hepatocytes was the differing TCR affinities for their respective ligands. Low-affinity TCR:pMHC interactions have been reported to be less effective at activating CD8 T cells and supporting effector expansion (21, 22). It is possible that the Des TCR affinity to H-2Kb complexed to one or all of the three defined self-peptides was lower than the OT-I TCR affinity to H-2Kb:SIINFEKL. As Des and OT-I TCR affinities for their ligands have not been compared, we expressed a lower-affinity ligand for OT-I and tested if its expression in hepatocytes would result in failure to elicit CTL function. We replaced the fourth asparagine residue of the WT SIINFEKL (OVA) with a threonine to generate SIITFEKL (OVA-T4) to create the rAAV.GFP-mOVA-T4 vector. OVA and OVA-T4 are reported to demonstrate similar binding efficiencies to H-2Kb, but the H-2Kb:OVA-T4 complex binds with lower affinity to the OT-I TCR compared with H-2Kb:OVA (22). To assess the effect of varying pMHC:TCR affinity on CD8 T-cell priming by hepatocytes, we cocultured naive OT-I T cells with hepatocytes isolated from B6 mice that had been transduced in vivo to express OVA or OVA-T4. Low numbers of hepatocytes expressing WT OVA acted as efficient APCs to induce activation and proliferation of most OT-I T cells (Fig. S6). A significant proportion of OT-I T cells stimulated by WT OVA-expressing hepatocytes also expressed IFN-γ, suggesting that they were functional. In contrast, hepatocytes expressing the low-affinity OVA-T4 variant induced poor OT-I activation, proliferation, and IFN-γ production (Fig. S6), akin to that previously described for Des T-cell responses (13). The suboptimal OT-I response to OVA-T4-expressing hepatocytes was reversed by addition of exogenous IL-2, suggesting that presentation of a high-affinity antigen by hepatocytes could remove the requirement for additional cosignals to mediate effective priming, which was required during presentation of lower-affinity antigen.
To test the ability of hepatocytes expressing low- or high-affinity antigen to induce CTLs in vivo, OT-I T cells were transferred into B6 mice treated with rAAV.GFP-mOVA or rAAV.GFP-mOVA-T4 vectors. Both vectors had comparable transduction efficacies (Fig. 6A and Fig. S7), and their administration to mice led to activation and proliferation of most transferred OT-I T cells in the liver and lymphoid organs (Fig. 6B). However, when CTL activity was measured at week 3, only expression of the high-affinity WT OVA, but not the lower-affinity OVA-T4 variant, led to CTL generation after low-dose rAAV vector treatment (Figs. 4 and and6C).6C). Higher rAAV doses did not elicit CTL activity at 3 wk for either variant (Fig. 6C).

A low-affinity OVA variant expressed in hepatocytes following rAAV transduction did not lead to detectable CTL function at 3 wk despite promoting efficient OT-I recruitment and proliferation. (A) GFP expression in B6 mice treated 7 d prior with PBS solution or 1 × 1011 vgc of rAAV.GFP-mOVA or rAAV.GFP-mOVA-T4. Deconvolution micrographs of fixed liver sections stained with DAPI (blue) and phalloidin-Alexa Fluor 594 (red) with GFP expression in green. (B) Expression of CD69 on CD45.1+CD8+ OT-I T cells at 3 h after transfer of 5 × 106 CD45.1+ OT-I LN cells into B6 mice pretreated with 1 × 1011 vgc rAAV.GFP-mOVA or rAAV.mOVA-T4 (black lines) compared with untreated B6 controls (shaded; histograms; Upper), and proliferation of CD45.1+ donor cells 36 h after transfer (dot plots; Lower). (C) In vivo cytotoxicity assay at week 3 after transfer of 107 CD45.1+ OT-I LN cells into B6 mice treated with indicated doses of rAAV.GFP-mOVA or rAAV.GFP-mOVA-T4 1 d after T-cell transfer.
Together, these results suggest that, when a low percentage of hepatocytes expressed antigen, CD8 T cells activated by higher-affinity TCR:pMHC interactions could develop effector function whereas lower affinity interactions, although still able to stimulate proliferation, were insufficient to induce full functional differentiation in the absence of cosignals that are not provided by hepatocytes.
High Levels of Antigen Expression in the Liver Promote T-Cell Exhaustion.
To characterize the mechanisms involved in CTL silencing at high antigen dose, we phenotyped intrahepatic OT-I T cells isolated from mice treated with high or low doses of rAAV.mOVA at week 3 after adoptive transfer. OT-I T cells from the liver of mice treated with a high dose of rAAV.mOVA expressed very high levels of the PD-1 inhibitory receptor, a hallmark of exhausted T cells (Fig. 7 A and B). A significant proportion of OT-I T cells from liver also expressed Tim-3, but there were no significant differences in Tim-3 expression between OT-I T cells from the high- and low-dose treatment groups (Fig. 7 A and B). T-cell exhaustion was confirmed at the functional level. OT-I T cells from the livers of mice treated with high-dose rAAV.mOVA did not exhibit degranulation of cytotoxic granules or express IFN-γ upon ex vivo restimulation (Fig. 7 C and D). In contrast, most OT-I T cells isolated from the low-dose treatment group expressed low to intermediate levels of PD-1 (Fig. 7 A and B), degranulated efficiently, and coexpressed IFN-γ upon ex vivo restimulation (Fig. 7 C and D). There were significantly higher numbers of intrahepatic OT-I T cells that degranulated and expressed IFN-γ in mice treated with low-dose rAAV compared with mice treated with high-dose rAAV (Fig. 7D). These findings were consistent with the results of in vivo CTL assays. In OT-I T cells isolated from the livers of mice treated with a low rAAV.mOVA dose, but not mice treated with a high dose of rAAV.mOVA, quantitative real-time–PCR confirmed expression of mRNA for IFN-γ and also demonstrated expression of TNF-α mRNA upon peptide restimulation (Fig. S8). However, no IL-2, IL-4, IL-17, or IL-10 mRNA expression was detected in OT-I T cells from either group of mice, suggesting that OT-I T cells did not differentiate into Tc2-, Tc17-, or IL-10–producing regulatory CD8 T cells.
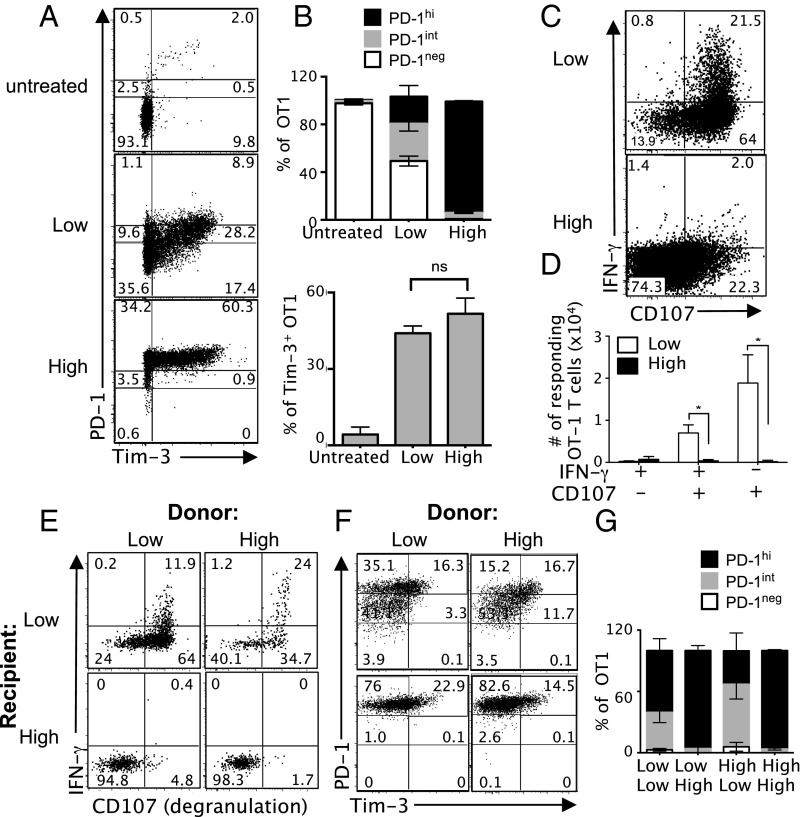
High-dose rAAV treatment promoted and maintained a functionally exhausted phenotype. (A and B) B6 mice adoptively transferred with 3 × 106 CD45.1+ OT-I LN cells were treated 1 d later with a low dose (5 × 108 vgc) or high dose (5 × 1010 vgc) of rAAV.mOVA. Liver leukocytes were harvested 3 wk later to assess cell surface expression of PD-1 and Tim-3. Flow plots were gated on CD8+ CD45.1+ cells and are representative of seven mice per group in two independent experiments. (B) Histograms represent mean ± SEM of four mice per group. Data representative of two separate experiments. (C and D) Cytotoxic degranulation (CD107 binding) and expression of IFN-γ upon ex vivo peptide restimulation following the experimental protocol outlined for A and B. Flow plots are representative of seven mice per group in two independent experiments. (D) Histograms represent mean ± SEM of four mice per group. This experiment was repeated once (n = 3 mice per group). (E–G) B6 mice adoptively transferred with 3 × 106 CD45.1+ OT-I LN cells were treated 1 d later with a low dose (5 × 108 vgc) or high dose (5 × 1010 vgc) of rAAV.mOVA. Liver leukocytes were harvested 1 wk later and transferred into secondary B6 recipients that had been injected 1 wk earlier with a low dose (5 × 108 vgc) or high dose (5 × 1010 vgc) of rAAV.mOVA. Three weeks after secondary T-cell transfer, livers were harvested to assess (F and G) expression of PD-1 and Tim-3 and (E) cytolytic function (CD107 binding) and IFN-γ production of intrahepatic OT-I T cells. Dot plots were gated on CD8+ CD45.1+ cells and are representative of three mice per group. (E) Histograms represent mean ± SEM of three mice per group. Data are representative of two independent experiments.
We also observed similar outcomes in terms of IFN-γ production and cytotoxic degranulation when low numbers (n = 500) of CD8 OT-I T cells were transferred (Fig. S9), suggesting that the influence of rAAV dose on CD8 T-cell outcome was not caused by the high precursor frequency of OT-I T cells used in this study, but is likely to affect outcomes at more physiological precursor frequencies of antigen-specific T cells.
The Exhausted T-Cell Phenotype Is Maintained by High Intrahepatic Antigen Load.
The exhausted phenotype and functional impairment of intrahepatic T cells could be irreversibly imprinted by the presence of high antigen levels during primary activation, or maintained by persistence of high levels of hepatic antigen. To address the role of intrahepatic antigen level after T-cell priming, we isolated intrahepatic OT-I that had been activated for 1 wk in mice treated with low or high doses of rAAV.mOVA, and retransferred these into second cohorts of mice treated with a high or low dose of rAAV.mOVA. Three weeks later, the phenotype and function of these T cells was assessed. OT-I T cells that were initially activated in mice treated with a low dose of rAAV.mOVA and transferred into mice treated with a high rAAV dose failed to degranulate and express IFN-γ upon ex vivo restimulation (Fig. 7E). In addition, these cells expressed high levels of PD-1 (Fig. 7F). In contrast, T cells activated in mice treated with a high dose of rAAV.mOVA and subsequently transferred into mice treated with a low rAAV dose expressed lower levels of PD-1 and acquired CTL function (Fig. 7 E–G). Thus, although T cells activated with a high antigen load were functionally impaired early after activation, they were not irreversibly compromised. These results demonstrate that, although the exhausted phenotype and functional silencing observed in the presence of high levels of intrahepatic antigen were determined by the amount of intrahepatic antigen, this was not irreversibly imprinted during initial T-cell activation. Instead, the maintenance of the exhausted phenotype and function required ongoing antigen exposure at least during the early phase of the immune response.
Collectively, these results indicate that, in the absence of intrahepatic inflammation, antigen expression in hepatocytes promotes the development of functional CTLs via extrahepatic cross-presentation and direct hepatocyte-mediated presentation of high-affinity antigen. However, the level of hepatocyte-expressed antigen is a dominant parameter in determining long-term CD8 T-cell functional outcome.
Discussion
By manipulating individual parameters that influence the response of naive CD8 T cells recognizing hepatocyte-expressed antigen, we have identified three key factors that determine the development and maintenance of functional effector responses to antigen within the liver: antigen cross-presentation, TCR affinity, and threshold of antigen expression. Although cross-presentation in lymphoid tissues contributed to effector cell generation, direct presentation of high-affinity antigen by hepatocytes alone could also elicit CTL. However, regardless of CD8 T-cell activation by the direct presentation or cross-presentation pathway, persisting high-level antigen expression by hepatocytes eventually silenced CTL function, including that of high-affinity CTLs. Thus, this study reveals a hierarchical contribution of three factors—amount of hepatic antigen, TCR:pMHC affinity, and cross-presentation—that dictate functional outcome following activation of naive CD8 T cells by hepatocyte-expressed antigen in vivo.
As would be expected from previous studies showing that a pancreatic self-antigen can be cross-presented in the draining LN (23), this study demonstrates that a hepatocyte membrane-expressed antigen was efficiently cross-presented in lymphoid tissues. As the liver is unique among solid organs in being able to support primary activation of CD8 T cells (7), we investigated the relative contribution of extrahepatic cross-presentation and intrahepatic presentation to the immune response to de novo expressed hepatocyte-expressed antigen. Unexpectedly, cross-presentation of liver-expressed antigen promoted the generation of CTLs (“cross-priming”) and not deletional tolerance (“cross-tolerance”) as reported for pancreatic self-antigen (23). It is possible that low-level immunogenicity of rAAV vectors altered the quality of cross-presenting APCs in our model; however, this is unlikely to be the explanation, as OT-I T cells transferred into mice expressing transgenic OVA in a noninflammatory setting have also been reported to develop into CTL (24). Rather, we favor the possibility that efficient cross-priming was promoted by the high amount of antigen expressed by hepatocytes. Regardless, CTLs generated by cross-presentation were effectively silenced between 1 and 3 wk in the presence of high-level antigen expression by hepatocytes, despite the initial development of effector function.
We recently described two mechanisms involved in impairing effector responses after intrahepatic activation: nonapoptotic degradation of T cells in hepatocyte lysosomes within the first day of activation [“suicidal emperipolesis” (25)] and Bim-dependent apoptosis of T cells surviving suicidal emperipolesis (17). Although donor OT-I cells initially retained in the liver were efficiently deleted in mice treated with high-dose rAAV.mOVA within the first 18 h, a minority of OT-I T cells survived early deletion, which subsequently expanded and accumulated within the liver. These T cells and those activated in lymphoid tissues by cross-presentation failed to develop sustained in vivo CTL function. Restimulating recipient mice with OVA-coated splenocytes and LPS increased the number of liver-sequestered T cells, but failed to restore their function. Thus, these functionally defective T cells were able to recognize liver-expressed antigen and were not in a “proliferative block” (8). This result is consistent with reports from Chisari and coworkers showing that anti-HBV effector CD8 T cells adoptively transferred into HBV transgenic mice cycled and expanded rapidly in this organ, but progressively lost cytotoxic function and their ability to secrete IFN-γ (26, 27). It is unclear whether, in our model, intrahepatic OT-I T cells cycled continuously in the presence of persisting antigen or whether they were quiescent; ongoing work will clarify this issue.
Minor variability in the phenotype of effector-like cells observed in this study highlights the programming plasticity of T cells bearing the same TCR. Although all OT-I T cells expressed the same TCR, they did not all express exactly the same phenotype. This result is consistent with the findings of a recent study (28) that showed that general expansion and contraction of antigen-specific CD8 T lymphocyte responses associated with robust outcomes is achieved through population averaging of discordant individual naive T-cell fates, rather than by uniform behavior of individual cells. Unbiased mathematical modeling (29) also fits the experimental data and supports the concept that complex T-cell responses are driven by stochastic processes and variability in individual cells. Thus, despite variability in individual cell phenotype, overall consistent functional outcomes were observed in vivo in our experimental system.
The observation that persisting CTL function was associated with antigen clearance in the low-dose rAAV treatment groups suggests that continued exposure to antigen in the liver incapacitated effector CD8 T cells. T cells activated in the presence of high antigen load bear the signature of exhausted T cells (30) at 3 wk postactivation as they failed to degranulate, were poor IFN-γ producers, and expressed high levels of PD-1. Exhaustion in the presence of high numbers of antigen-expressing hepatocytes was not immediately and irreversibly determined in the initial phase of activation; the ongoing presence of intrahepatic antigen determined T-cell fate. OT-I T cells activated in the presence of high-level antigen expression by hepatocytes subsequently transferred into recipients expressing low levels of antigen exhibited cytotoxic degranulation and the capacity to express IFN-γ, and expressed lower levels of PD-1. In contrast, similarly activated cells transferred into a high liver antigen environment exhibited an exhausted phenotype and impaired function.
Another key finding of this study was that exclusive activation of OT-I T cells by hepatocytes could lead to CTL generation, albeit only when a high-affinity ligand was expressed. This result was unexpected, as hepatocytes do not express the known costimulatory molecules CD80 and CD86 (31) and were shown to be poor promoters of effector responses in studies that used Des T cells (13). By simulating comparable conditions and modes of antigen presentation to Des and OT-I T cells, we confirmed that, regardless of expression levels and frequency of transduction, H-2Kb expression did not promote Des T-cell effector function, whereas OVA expression induced OT-I CTL differentiation. Our results suggest that these differing outcomes might be a result of different strengths of TCR:pMHC interactions, a factor known to be critical to the outcome of T-cell responses in the periphery (22, 32). Although the relative affinities of the Des and OT-I TCRs for their respective ligands are not known, Des T cells are less efficiently retained and require a longer time before undergoing first division after antigen encounter compared with OT-I cells, suggesting that Des TCR affinity for H-2Kb:KVITFIDL is lower than OT-I TCR affinity for H-2Kb:SIINFEKL. Indeed, we also found that expression of OVA-T4, a lower-affinity ligand for the OT-I T cells compared with WT OVA, did not elicit CTL function despite triggering activation and proliferation. Poor priming of OT-I T cells by this low-affinity variant could be reversed in vitro by addition of exogenous IL-2 during activation, suggesting that effective T-cell priming elicited by hepatocyte presentation of high-affinity ligands may be facilitated by the induction of sufficient strength to bypass the requirement for costimulation. In contrast, the failure of hepatocytes expressing lower-affinity ligands to elicit effective activation would be consistent with lack of expression of costimulatory molecules by this nonprofessional APC.
By identifying the relative importance of antigen level, TCR:pMHC affinity, and cross-presentation to CTL generation following activation by hepatocyte-expressed antigen, our model reconciles apparently discordant findings from several groups investigating the outcome of intrahepatic CD8 T-cell activation. First, this study ends an ongoing debate over whether T-cell tolerance observed in transgenic models is primarily a result of central tolerance or other regulatory mechanisms caused by constitutive transgene expression (11, 12). Regardless of de novo (rAAV.Kb treatment in this study) or transgenic [Alb-Kb mice (8, 13, 17, 25)] expression, Des T cells activated by hepatocytes never developed into CTL, a finding similarly observed for OT-I T cells activated intrahepatically by de novo-expressed lower-affinity ligands. Overall, a wide variety of outcomes have been reported after intrahepatic CD8 T-cell activation in mice expressing transgenic liver antigens, including ignorance (33), deletional tolerance (8, 13, 17, 25), and partial or full effector differentiation (11, 12, 24, 34). These variable outcomes are likely caused by the different TCR:pMHC affinity and/or levels of antigen expression in these models. Second, the finding that extrahepatic cross-presentation influences the generation of CTLs at high antigen dose is consistent with our previous studies showing that the site of activation can be an important determinant for CTL generation (13). However, the effects of this factor can be altered by TCR affinity and frequency of antigen-expressing hepatocytes. CD8 T cells activated via high affinity interactions differentiated into CTLs and maintained effector function following activation in the presence of antigen expression by less than 25% of hepatocytes, whereas T cells activated in lymphoid tissues via low-/intermediate-affinity interactions did not develop into CTLs when all hepatocytes expressed antigen. This does not mean that low-/intermediate-affinity T cells cannot mediate tissue damage. Development of Des CTLs able to cause hepatitis was observed in Met-Kb mice when H-2Kb was expressed by transgenesis on the right type of LN APCs (13). CTLs arising from lower-affinity interactions were also detected when inflammation triggered TLRs and costimulatory molecules that change the nature of the signals delivered by APCs to T cells (33). Third, this study explains why previous studies expressing OVA in hepatocytes have shown that OT-I T cells developed into CTLs (11, 12, 24). In all these studies, OT-I CTL activity was detected at week 1, before the onset of silencing observed in the present study, which was mediated by persisting liver antigen at week 3. We predict that the maintenance or loss of CTL activity will largely be dependent on whether hepatic antigen expression persists. Research by Crispe and coworkers has shown that OT-I CTL activity is detected at week 1 in recipients of mouse liver transplants (11) and in mice treated with rAAV vectors (12). In the liver transplant model, OVA peptide was injected into recipients of H-2Kb+ donor livers, which likely resulted in transient availability of H-2Kb:SIINFEKL complexes, whereas, in the rAAV study, type 2 capsid vectors were used to deliver OVA expressed under the control of the CMV promoter, resulting in low-level (1–2%) transduction of hepatocytes in bm8→B6 bone marrow chimeric mice. We predict that, in both models, the transient expression of antigen, or expression of antigen at low enough levels to be cleared by nascent CTLs, will result in persisting CTL activity. On the contrary, we would predict that, in a model in which OVA is transgenically expressed within hepatocytes, CTL activity reported to be present at 1 wk after transfer (24) will likely be silenced by week 3.
Our central finding that the frequency of antigen-expressing hepatocytes was the critical determinant of CTL function suggests that the proportion of infected hepatocytes plays an important role in influencing the development and outcome of virus-specific immune responses in HBV and HCV infection. The rapid targeting of a significant proportion of hepatocytes might be a strategy used by these viruses to silence most virus-specific T-cell clones and impair effective antiviral immune responses. This phenomenon might occur early in infection, especially at high viral loads, and compromise the T-cell repertoire, potentiating the development of chronic infection. Certainly, the threshold level observed in these present experiments would be well within those reported in infections with hepatotropic infections (4, 35). These results would also be consistent with those of Chisari and coworkers, who found ineffective activation of HBV core-specific CD8 T cells in HBV-transgenic mice with universal expression of cognate antigen by hepatocytes, but effector differentiation in association with intrahepatic activation in mice inoculated with recombinant vaccinia virus expressing HBV core, in which the levels of hepatocyte antigen expression are likely to be very low (27). Interestingly, our findings do contrast with studies of HBV in chimpanzees, in which a high-dose inoculum was observed to be associated with universal infection of hepatocytes yet effective clearance of infection, whereas intermediate doses were associated with limited infection and more rapid clearance, and a low-dose inoculum was able to lead to universal hepatocyte infection with delayed viral clearance or even viral persistence (36). Factors such as the kinetics of antigen expression and the influence of innate and CD4 T responses, which are critical to HBV clearance (36, 37), may at least in part explain the differences observed between the present work and the chimpanzee HBV model.
Our finding of an antigen expression threshold as a determinant of the outcome of immune responses to hepatocyte-expressed antigen also has direct implications for gene therapy protocols targeting the liver. Much progress has been made in establishing improved liver-targeting rAAV vectors to induce prolonged transgene expression. We now show that transducing ~25% of murine hepatocytes could tolerize the naive CD8 T-cell repertoire. In man, in which clearance of transgene-expressing hepatocytes and/or hepatocytes presenting viral proteins is thought to be mediated by effector/memory CD8 T cells, this threshold might be higher. Inducing tolerance of effector/memory CD8 T cells is nonetheless possible. By using the rAAV8 system used in clinical studies, we have recently provided proof of principle that overexpressing a single MHC molecule could lead to silencing of a primed, memory alloreactive response, leading to protection of a skin graft from rejection (14). Similar technology is already approved by the European Commission and European Medicines Agency for Glybera (rAAV1) and could potentially be extended for the induction of tolerance in autoimmune pathologic conditions (38).
In conclusion, these data suggest a number of key parameters contributing to the initial outcomes of CD8 T-cell responses to hepatocyte expressed antigen, and indicate a hierarchy in the influence of these factors on effector function. Further challenges in this area of research include increasing our understanding of the mechanisms that program or maintain CTL in a silent state, and identifying triggers that allow them to regain function.
Methods
rAAV Vectors for Liver-Targeted Gene Delivery.
Coding sequences for the antigens in this study were designed in-house and part-synthesized by GeneArt Gene Synthesis (Invitrogen), except for mOVA, which was donated by Frank Carbone (University of Melbourne, Melbourne). Sequences were subcloned into the pAM2AA expression vector that incorporates a liver-specific human α-1-anti-trypsin promoter and two ApoE hepatic control regions, flanked by AAV2 inverted terminal repeats (39). rAAV packaging was performed in HEK293D cells using pAM2AA, pXX6 helper plasmid (courtesy of Jude Samulski, University of North Carolina, Chapel Hill, NC) and pseudoserotyped to type 8 capsid (plasmid courtesy of James Wilson, University of Pennsylvania, Philadelphia) and purified by cesium chloride ultracentrifugation (40). The vgc counts were determined by quantitative PCR (14), and rAAV vectors were administered i.v. via the lateral tail vein.
Animals.
C57BL/6 (H-2b) mice were purchased from the Animal Resources Centre (ARC). B10.BR (H-2k, CD45.1), Des, Des backcrossed into the recombinase activating gene-deficient background (DesRAG−/−) Alb-Kb, and Met-Kb mice have been described (13, 17). OT-I (41) and H-2Kbm1 (15) mice were kindly provided by William Heath (University of Melbourne, Melbourne). Alb-Kb and OT-I mice were backcrossed to H-2Kbm1. OT-I mice were also backcrossed to B6.SJL-Ptprca Pep3b/BoyJ mice (ARC). Mice were maintained under specific pathogen-free conditions in the Centenary Institute (Sydney). Experimental protocols were approved by the Sydney University Animal Care and Ethics Committee and Sydney Local Health District Animal Ethics Committee.
Quantifying Hepatocyte Antigen Expression by Flow Cytometry.
Hepatocytes were isolated as previously described (42). Hepatocytes were stained with biotinylated anti–H-2Kb (AF6-88.5; BD Pharmingen), anti–H-2Kk (36-7-5; BD), and streptavidin-phycoerythrin (PE) (Invitrogen); or with rabbit anti-OVA (clone 1670; provided by Andrew Lew, Walter and Eliza Hall Institute of Medical Research, Melbourne) and Alexa Fluor 488-conjugated anti-rabbit IgG (Invitrogen). Cells were stained with propidium iodide (3 μg/mL) before acquisition on a BD LSR II flow cytometer (BS Biosciences), and were analyzed in FlowJo 9.4.11 (Tree Star).
Confocal and Epifluorescence Analysis of Liver Sections.
Livers were perfused in situ with PBS solution followed by 10% (vol/vol) neutral buffered formalin and transferred to 10% (wt/vol) sucrose followed by 30% (wt/vol) sucrose solutions before embedding in optimal cutting temperature (OCT) compound (TissueTek). Sections (12 μm) were stained with rabbit anti-OVA (clone 1670), rat-anti-F4/80 (CI:A3-1; hybridoma) or rat anti-CD31 (MEC 13.3; BD Pharmingen) and Alexa Fluor 488 or Alexa Fluor 594-conjugated secondary antibodies (Invitrogen) before image acquisition on a DeltaVision microscopy imaging system with a 10× objective and Photometrics CoolSnap HQ2 camera or a Leica SP5 Confocal microscope (Leica Microsystems).
Purification, Adoptive Transfer, and Analysis of Donor Cells by Flow Cytometry.
Single-cell suspensions of peripheral LN cells from donor OT-I, Des, or DesRAG−/− mice were isolated as previously described (17, 25) and labeled with 5 μM carboxyfluorescein succinimidyl ester (CFSE) where indicated. One million to eight million LN cells were injected i.v. 7 d after rAAV treatment (for assays to determine primary site of activation) or 1 d before rAAV treatment (for in vivo cytotoxicity assays). Liver, spleen, LNs, and blood were harvested and stained as described previously (7). Antibodies were from BD Pharmingen unless otherwise stated, and included CD45.1 Horizon V450 (A20); CD8-Pacific Blue or CD8-allophycocyanin (53-6.7); CD69-PE, CD69-allophycocyanin, or CD69-PerCP-Cy5.5(H1.2F3); and CD44-allophycocyanin-Cy7 (IM7; Biolegend). Cells were stained with 0.1 μg/mL DAPI (Invitrogen) before acquisition on a BD LSR Fortessa flow cytometer (BD Biosciences), and were analyzed in FlowJo 9.4.11 (Tree Star).
In Vivo Cytotoxicity Assay.
Cytotoxicity of transferred Des T cells toward H-2Kb+ target splenocytes from 178.3 mice relative to control B10.BR splenocytes was measured as described previously (17). OT-I cytotoxicity was determined by their ability to kill SIINFEKL (2 μg/mL)-pulsed B6 splenocytes relative to unpulsed splenocytes. Target and control splenocytes were labeled with 5 μM or 0.5 μM CFSE and mixed 1:1, and 2 × 107 total cells were injected 16 h before harvesting; the percentage of specific killing was calculated as described previously (17).
Ex Vivo Degranulation Assay with Intracellular IFN-γ Staining.
Ex vivo degranulation assay and intracellular IFN-γ staining were performed as described previously (43) with some modifications. A maximum of 4 × 106 LN cells, splenocytes, or liver leukocytes were resuspended in Fc block (BD Pharmingen). After 20 min incubation at 4 °C, cells were centrifuged and resuspended in RPMI medium with 10% FCS in the presence of 0.1 μM synthetic SIINFEKL peptides, 0.5 μM Golgi-Stop (BD Biosciences), anti–CD107a-Alexa Fluor 647 (Biolegend), and anti–CD107b-AlexaFluor 647 (Biolegend). Cells were then incubated at 37 °C and 5% CO2 for 4 h, then centrifuged and stained with anti–CD8α-Horizon V500, anti–CD45.1-Pacific Blue, anti–CD4-FITC (BD Pharmingen), anti–CD11b-FITC (BD Pharmingen), anti–CD19-FITC (BD Pharmingen), anti–NK1.1-FITC (BD Pharmingen), and Live/Dead fixable blue dead cell stain (Life Technologies) for 30 min at 4 °C. Cell were then washed and fixed with 1% paraformaldehyde in PBS solution and stained with anti–IFN-γ-PE (Biolegend) in 0.25% saponin (Sigma-Aldrich) overnight. Cells were washed twice before flow cytometric analysis. Backgrounds were determined from controls without peptide stimulation and were subtracted from the values presented for test samples.
Acknowledgments
The authors thank the Centenary Institute Animal Facility and Advanced Cytometry Facility for their technical support, Dr. Frank Carbone for the mOVA cDNA, and Dr. Andrew Lew for the anti-OVA antibody used in this study. This work was supported by the National Health and Medical Research Council (NHMRC) Australia Program Grant 571408 and NHMRC Senior Research Fellowship 511903 (to P.B.). J.R.G. holds the Wenkart Chair of the Endothelium.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/10.1073/pnas.1406674111/-/DCSupplemental.
References
Articles from Proceedings of the National Academy of Sciences of the United States of America are provided here courtesy of National Academy of Sciences
Full text links
Read article at publisher's site: https://doi.org/10.1073/pnas.1406674111
Read article for free, from open access legal sources, via Unpaywall:
https://www.pnas.org/content/pnas/111/25/E2540.full.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1073/pnas.1406674111
Article citations
Optimized RNA interference therapeutics combined with interleukin-2 mRNA for treating hepatitis B virus infection.
Signal Transduct Target Ther, 9(1):150, 21 Jun 2024
Cited by: 0 articles | PMID: 38902241 | PMCID: PMC11189933
Retreatment with HBV siRNA Results in Additional Reduction in HBV Antigenemia and Immune Stimulation in the AAV-HBV Mouse Model.
Viruses, 16(3):347, 23 Feb 2024
Cited by: 1 article | PMID: 38543713 | PMCID: PMC10975807
Preclinical evaluation of therapeutic vaccines for chronic hepatitis B that stimulate antiviral activities of T cells and NKT cells.
JHEP Rep, 6(5):101038, 12 Feb 2024
Cited by: 2 articles | PMID: 38694959 | PMCID: PMC11061331
A hepatic network of dendritic cells mediates CD4 T cell help outside lymphoid organs.
Nat Commun, 15(1):1261, 10 Feb 2024
Cited by: 3 articles | PMID: 38341416 | PMCID: PMC10858872
IL-2 produced by HBV-specific T cells as a biomarker of viral control and predictor of response to PD-1 therapy across clinical phases of chronic hepatitis B.
Hepatol Commun, 7(12):e0337, 07 Dec 2023
Cited by: 3 articles | PMID: 38055623 | PMCID: PMC10984660
Go to all (62) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Effective intrahepatic CD8+ T-cell immune responses are induced by low but not high numbers of antigen-expressing hepatocytes.
Cell Mol Immunol, 13(6):805-815, 12 Oct 2015
Cited by: 20 articles | PMID: 26412123 | PMCID: PMC5101449
Intrahepatic Cross-Presentation and Hepatocellular Antigen Presentation Play Distinct Roles in the Induction of Hepatitis B Virus-Specific CD8+ T Cell Responses.
J Virol, 92(21):e00920-18, 12 Oct 2018
Cited by: 10 articles | PMID: 30089700 | PMCID: PMC6189498
CD40 activation rescues antiviral CD8⁺ T cells from PD-1-mediated exhaustion.
PLoS Pathog, 9(7):e1003490, 11 Jul 2013
Cited by: 89 articles | PMID: 23853599 | PMCID: PMC3708877
Immune outcomes in the liver: Is CD8 T cell fate determined by the environment?
J Hepatol, 63(4):1005-1014, 20 Jun 2015
Cited by: 33 articles | PMID: 26103545
Review





