Abstract
Free full text

Antibody-based depletion of Foxp3+ T cells potentiates antitumor immune memory stimulated by mTOR inhibition
Abstract
Inhibition of mTOR signaling enhances antitumor memory T lymphocytes while increasing the frequency of immunosuppressive regulatory T cells (Tregs). We report here a strategy to further improve immunologic memory by controlling CD4+ T cells with CD4-depleting monoclonal antibody therapy thereby improving CD8+ memory T cell quality and function. We report that removal of Tregs is the mechanism underlying immunological memory formation in response to this combination immunotherapy.
The key immune signals needed for a primary adaptive immune response has long been well understood. However, the trigger for converting a CD8+ effector cell to a memory cell has only recently been elucidated.1,2 Inhibition of the mTOR pathway modulates cellular metabolism and enhances CD8+ memory T cell formation. Previously, we applied this concept to cancer immunology in preclinical models using multiple syngeneic murine tumors.3 mTOR inhibition produced a multitude of immune effects culminating in the suppression of tumor growth. Although in our system, mTOR inhibition enhanced the quality of the antitumor memory cells, we also observed immunosuppressive effects as well. This was not surprising since the canonical mTOR inhibitor, rapamycin, is routinely used to suppress the immune system following solid organ transplantation. In our preclinical models, mTOR inhibition decreased the proliferation of activated CD4+ and CD8+ T cell in vitro and in vivo, and increased the relative abundance of regulatory T cells (Tregs). Therefore, we asked if a strategy to control Tregs could potentially further enhance the formation of memory T cells in response to mTOR inhibition.
Tregs are arguably the most important negative regulator of cellular immunity. However, there is no translatable strategy to specifically remove or inhibit Tregs. Therefore, we tested an approach to deplete all CD4-expressing T cells using an anti-CD4 monoclonal IgG2b antibody. CD4 depletion was timed to allow the presence of CD4+ T helper cells during primary immune activation. We observed that CD8+ T cells primed in the absence of CD4+ cell failed to express eomesodermin (Eomes) an early memory cell marker. Others have also reported that CD4+ T cells are needed for effective CD8+ memory cell formation.4,5 For example, CD8+ memory cells formed in the absence of CD4+ cells exhibited an exhausted phenotype and increased expression of programmed cell death 1 (PD-1).4,5 However, once CD8+ T effector cells have activated and expanded, CD4+ T cell help is dispensible. Subsequent tumor control is dependent upon CD8+ memory cells that possess the hallmark ability to activate by simply engaging the T-cell receptor with soluble antigens. In other words, antigen presenting cells and CD4+ T helper cells are no longer required. In fact, after the initial stages of immune priming, CD4+ T cell activity is dominated by regulatory function. We, and others, have shown that CD4+ T cell depletion specifically at this point in the immunological cascade leads to enhanced formation of both central and effector CD8+ memory cells and enhanced control of tumor growth.
Prior studies examining CD4+ T-cell depletion as a means to control tumor growth have assumed that the effects of ablating CD4+ immune cells were a direct consequence of diminished Treg levels. However, to firmly establish this as the mechanism-of-action we performed 2 separate experiments. We used a transgenic mouse that carries a transgene for the diphtheria toxin receptor under the control of the forkhead box P3 (Foxp3) promoter. Instead of depleting all CD4 cells, the Foxp3-expressing subset was specifically depleted by virtue of the diphtheria toxin transgene. Similar to CD4 depletion, Foxp3 depletion enhanced CD8 memory formation in the presence of mTOR inhibition. In a reciprocal experiment, activated and GFP-tagged Tregs were replaced following CD4+ T-cell depletion. If Treg depletion is the primary causal factor, we anticipated that replacing Tregs should neutralize any benefits derived from CD4 depletion and this is precisely what we observed. Together, these experiments empirically identified Treg depletion as the cellular mechanism underlying the enhanced immunity following CD4+ T-cell depletion. Interestingly, intratumoral Treg depletion has been identified at the primary mode of action for ipilimumab.6 Based on a positive Phase III trial, ipilimumab was FDA approved for the treatment of advanced melanoma. Therefore, it is intriguing to consider the possibility that targeted CD4+ T-cell depletion may produce a similar immune effect in patients but with a different, potentially less risky, safety profile.
There have been other strategies for targeting Tregs for depletion in cancer patients. Another potential Treg marker is CD25, which is expressed by a majority of Tregs. CD25 is the α chain component of the IL-2 receptor and IL2 signaling is critical for CD4+ and CD8+ T cell stimulation. Therefore, strategies to target CD25 will affect a broad range of immune cells, thereby inducing non-desirable effects on other subsets of immune cells. For example, an anti-CD25 depleting antibody will deplete activated CD8+ lymphocytes also expressing CD25. Another limitation of this strategy is that some Tregs are actually CD25 negative, meaning that they would escape. In murine models, CD25 antibody-targeted cell depletion has been found to effectively prevent tumor initiation, but was ineffective in treating established tumors7 and has been shown to restrict adoptive immunotherapy.8 Another strategy uses an engineered protein chimeric of interleukin-2 and diphtheria toxin (denileukin diftitox, trade name Ontax) to target CD25 expressing cells. The approach has been tested in renal cell carcinoma (RCC) and melanoma patients,9,10 however clinical effectiveness was limited, possibly due to depletion of CD8+ T effector cells. Although our antibody-based method of CD4+ T-cell depletion is not exclusive to Tregs, it leaves the critical population of CD8 cells intact. Another potential, and yet untested benefit is that anti-CD4 antibody targeted depletion removes the pool of CD4+Foxp3- cells that can go on to express Foxp3 and become future Tregs.
We propose combining mTOR inhibition and CD4+ T-cell depletion to enhance antitumor immunity (Fig. 1). CD4 depletion removes regulatory T cells and the combination enhances the quality and function of antitumor CD8+ memory T cells even when the tumor itself is the only source of antigen and a separate cancer vaccine is not administered. A clearer understanding of the mechanism-of-action of the anti-CD4 antibody immunotherapy described here bolsters the rationale for future clinical investigation.
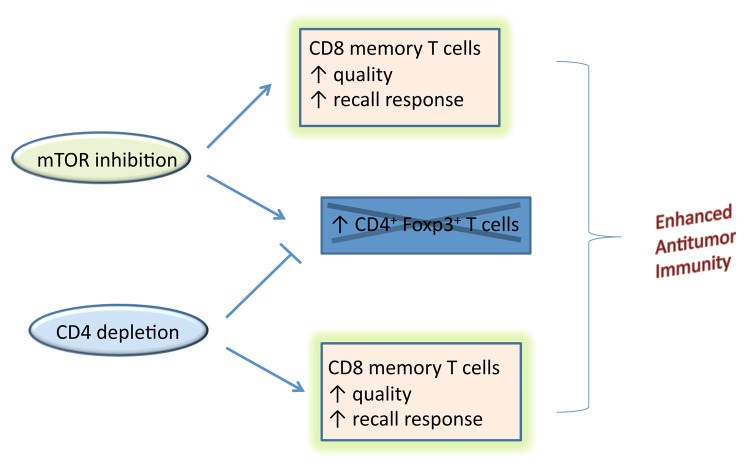
Figure 1. Enhanced antitumor immunity arises from combining mTOR inhibition with CD4+ T cell depletion. Co-administering both mTOR inhibitors and anti-CD4 antibodies to deplete CD4 lymphocytes enhance the formation of CD8+ memory T lymphocytes. The combination is rational because CD4+ T-cell depletion counters the potentially negative impact of mTOR inhibitors that can enhance immunosuppressive Foxp3-expressing regulatory T cells.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
Articles from Oncoimmunology are provided here courtesy of Taylor & Francis
Full text links
Read article at publisher's site: https://doi.org/10.4161/onci.29081
Read article for free, from open access legal sources, via Unpaywall:
https://www.tandfonline.com/doi/pdf/10.4161/onci.29081?needAccess=true
Citations & impact
Impact metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.4161/onci.29081
Article citations
Akt1 and -2 inhibition diminishes terminal differentiation and enhances central memory CD8+ T-cell proliferation and survival.
Oncoimmunology, 4(5):e1005448, 03 Feb 2015
Cited by: 31 articles | PMID: 26155399 | PMCID: PMC4485779
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Foxp3+ T cells inhibit antitumor immune memory modulated by mTOR inhibition.
Cancer Res, 74(8):2217-2228, 26 Feb 2014
Cited by: 25 articles | PMID: 24574514
OX40 costimulation can abrogate Foxp3+ regulatory T cell-mediated suppression of antitumor immunity.
Int J Cancer, 125(3):630-638, 01 Aug 2009
Cited by: 52 articles | PMID: 19455675 | PMCID: PMC3018329
A New Immunosuppressive Molecule Emodin Induces both CD4+FoxP3+ and CD8+CD122+ Regulatory T Cells and Suppresses Murine Allograft Rejection.
Front Immunol, 8:1519, 08 Nov 2017
Cited by: 16 articles | PMID: 29167674 | PMCID: PMC5682309
Regulatory T cells in tumor immunity.
Int J Cancer, 127(4):759-767, 01 Aug 2010
Cited by: 581 articles | PMID: 20518016
Review




