Abstract
Purpose
The accurate diagnosis and classification of dry eye disease (DED) is challenging owing to wide variations in symptoms and lack of a single reliable clinical assessment. In addition, changes and severity of clinical signs often do not correspond to patient-reported symptoms. To better understand the inconsistencies observed between signs and symptoms, we conducted a systematic literature review to evaluate published studies reporting associations between patient-reported symptoms and clinical signs of DED.Methods
PubMed and Embase were searched for English-language articles on the association between clinical signs and symptoms of DED up to February 2014 (no lower limit was set).Results
Thirty-four articles were identified that assessed associations between signs and symptoms, among which 33 unique studies were reported. These included 175 individual sign-symptom association analyses. Statistical significance was reported for associations between sign and symptom measures in 21 of 33 (64%) studies, but for only 42 of 175 (24%) individual analyses. Of 175 individual analyses, 148 reported correlation coefficients, of which the majority (129/148; 87%) were between -0.4 and 0.4, indicating low-to-moderate correlation. Of all individual analyses that demonstrated a statistically significant association, one-half (56%) of reported correlation coefficients were in this range. No clear trends were observed in relation to the strength of associations relative to study size, statistical methods, or study region, although results from three studies did suggest that disease severity may be a factor.Conclusion
Associations between DED signs and symptoms are low and inconsistent, which may have implications for monitoring the response to treatment, both in the clinic and in clinical trials. Further studies to increase understanding of the etiopathogenesis of DED and to identify the most reliable and relevant measures of disease are needed to enhance clinical assessment of DED and the measurement of response to therapeutic interventions.Free full text
Associations between signs and symptoms of dry eye disease: a systematic review
Abstract
Purpose
The accurate diagnosis and classification of dry eye disease (DED) is challenging owing to wide variations in symptoms and lack of a single reliable clinical assessment. In addition, changes and severity of clinical signs often do not correspond to patient-reported symptoms. To better understand the inconsistencies observed between signs and symptoms, we conducted a systematic literature review to evaluate published studies reporting associations between patient-reported symptoms and clinical signs of DED.
Methods
PubMed and Embase were searched for English-language articles on the association between clinical signs and symptoms of DED up to February 2014 (no lower limit was set).
Results
Thirty-four articles were identified that assessed associations between signs and symptoms, among which 33 unique studies were reported. These included 175 individual sign–symptom association analyses. Statistical significance was reported for associations between sign and symptom measures in 21 of 33 (64%) studies, but for only 42 of 175 (24%) individual analyses. Of 175 individual analyses, 148 reported correlation coefficients, of which the majority (129/148; 87%) were between −0.4 and 0.4, indicating low-to-moderate correlation. Of all individual analyses that demonstrated a statistically significant association, one-half (56%) of reported correlation coefficients were in this range. No clear trends were observed in relation to the strength of associations relative to study size, statistical methods, or study region, although results from three studies did suggest that disease severity may be a factor.
Conclusion
Associations between DED signs and symptoms are low and inconsistent, which may have implications for monitoring the response to treatment, both in the clinic and in clinical trials. Further studies to increase understanding of the etiopathogenesis of DED and to identify the most reliable and relevant measures of disease are needed to enhance clinical assessment of DED and the measurement of response to therapeutic interventions.
Video abstract
Click here to view.(102M, avi)
Introduction
Dry eye disease (DED) is a complex, multifactorial condition characterized by inflammation of the ocular surface and lacrimal glands and reductions in the quality and/or quantity of tears.1 The prevalence of DED is high and ranges from 5% to 33% of the adult population worldwide.2 DED is considered to be a symptomatic disease,2 and many patients experience eye irritation, stinging, dryness, ocular fatigue, and fluctuating visual disturbances.3 These symptoms can lead to significant functional impairment in daily and social activities, quality of life, and productivity among affected patients.4 DED also poses a substantial economic burden to payers, patients, and society owing to associated health care costs and loss of productivity.5
The accurate diagnosis and classification of DED is complicated by the heterogeneous nature of the disease and wide variations in symptoms. A number of clinical tests assessing signs of DED are available that can broadly be divided into either those that evaluate tear production/quality or those that assess the integrity of the ocular surface. However, there is lack of a single test that can be used to accurately assess disease progression or response to treatment.3,6 The clinical picture of DED is further complicated by the observation that changes in and severity of clinical signs often do not correspond to patient-reported symptoms. This may impact both the diagnosis and management of DED in clinical practice and the design and interpretation of clinical trials with sign and symptom endpoints.
Our objective was to conduct a systematic literature review of the available evidence on associations between clinical signs and symptoms in DED in order to better understand the inconsistencies observed between these measures. To our knowledge, this is the first systematic review to address this issue, and therefore, it should provide new insights into the topic.
Methods
PubMed and Embase were searched for English-language articles published up to February 28, 2014 (no lower limit was set), reporting associations between signs and symptoms of DED, and the primary data supporting those findings were identified. The search terms used were (dry eye syndrome [Medical Subject Heading (MeSH)] or “dry eye disease”) AND ([test OR tests OR sign OR signs] AND [symptom OR symptoms]) AND (correlation OR association). The search was limited to humans and English language. The MeSH dry eye syndrome (PubMed) and dry eye (Embase) include keratoconjunctivitis sicca, Sjögren’s syndrome (SS), and xerophthalmia.
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, titles and abstracts of all articles were reviewed, and articles for full-text review were further identified. Bibliographies of full-text publications and literature on file also were reviewed for additional evidence.
Results
Of the 288 titles/articles reviewed, 63 articles were selected for full-text review after excluding articles that did not assess the association of signs and symptoms. From reference lists of the 63 articles, an additional 14 relevant articles were identified. From the combined group of 77 articles, 43 were excluded as analysis of the full text indicated they did not assess association of signs and symptoms, yielding 34 articles for final inclusion (Figure 1).
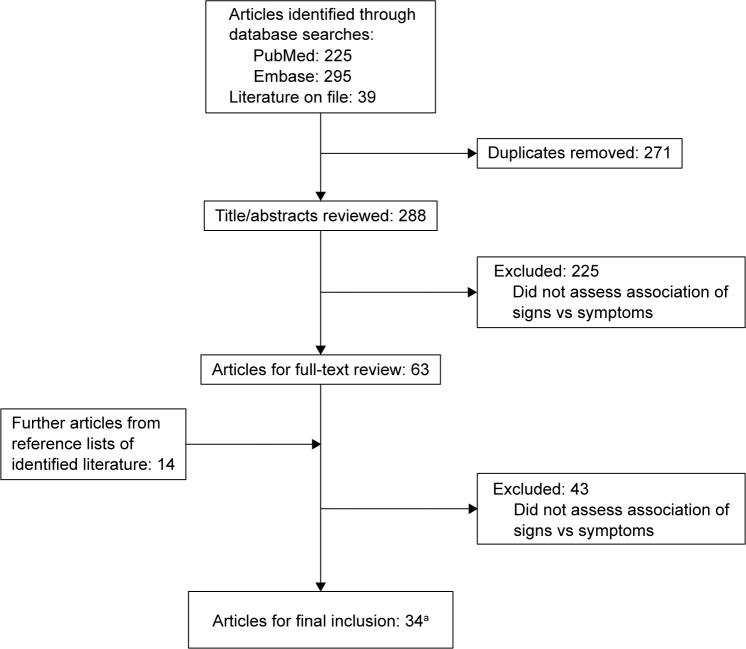
Preferred reporting items for systematic reviews and meta-analyses flow diagram.
Note: aOf which 33 articles reported unique studies.
Table 1 summarizes the literature identified as meeting the study criterion of reporting primary data on associations between signs and symptoms of DED. Articles were categorized according to the symptom measures used: 1) Ocular Surface Disease Index© (OSDI), 25-item National Eye Institute Visual Function Questionnaire (NEI VFQ-25), or visual analog scale (VAS); 2) frequency of symptom instruments; and 3) symptom severity or other symptom measures. For signs, we focused on clinical tests that are commonly used in clinical trials. These were tear breakup time (TBUT), Schirmer tear test, ocular surface dye staining, and tear osmolarity. Details on these sign and symptom measures are provided in Table 2. Other tests for which associations with symptoms were reported but are not described were tear meniscus height, phenol red thread test, lid margin telangiectasia, lid-parallel conjunctival folds, lid-wiper epitheliopathy, fluorescein clearance test, meibomian gland dysfunction assessment, closed chamber humidity difference, and infrared thermometry (each was reported in ≤5 articles).
Table 1
Studies reporting associations between symptoms and clinical signs/tests in DED
| Study | Country | Study design | Population, N | Age, mean (SD),a sex, % female | Method for symptom assessment | Clinical sign/test | Correlationcoefficientb | Significance | Statisticaltest used |
|---|---|---|---|---|---|---|---|---|---|
| Symptom measurement using OSDI, NEI VFQ-25, or VAS | |||||||||
| Schiffman et al22 | USA | Clinic-based validation study | Normal (N=30); DED (N=109) | Normal: 54.5 (13.4), 83; DED: 57.5 (13.9), 79 | OSDI | TBUT Schirmer tear test Total staining (LG) Total staining (F) | −0.14 −0.21 0.13 0.19 | NS S (P=0.01) NS S (P=0.02) | Spearman |
| Amparo et al24 | USA | Retrospective, clinic-based, cohort study | DED (N=186) | 54 (15), 66 | OSDI | Corneal staining (F) Tear osmolarity | 0.31 −0.091 | S (P<0.001) NS | Pearson or Spearman |
| Vitale et al35 | USA | Clinic-based study | Primary SS (N=42) | 54.9 (12.7), 95 | OSDI NEI VFQ-25 | TBUT Schirmer tear test Total staining (F + LG) TBUT Schirmer tear test Total staining (F + LG) | 0.06 0.04 0.19 0.24 −0.04 0.20 | All NS | Spearman |
| Sullivan et al37 | USA and EU | Retrospective, clinic-based cohort study | Normal (N=82); DED (N=262) | Normal and DED: 46.1 (16.4), 73 | OSDI | TBUT Schirmer tear test Corneal staining (F) Conjunctival staining (LG) | 0.09c 0.06c 0.15c 0.14c | NR | Pearson |
| Adatia et al42 | Canada | Clinic-based study | SS (N=18) | 54.3 (10.6),d 89 | OSDI SSD | Corneal staining (LG) Corneal staining (LG) | −0.2278 −0.2736 | All NS | Pearson |
| Tuisku et al54 | Finland | Clinic-based study | Normal (N=10); SS (N=20) | Normal: 49.8 (5.0), 90; SS: 54.5 (7.0), 90; SS: 54.5 (7.0), 95 | OSDI VAS | Corneal staining (F) Schirmer tear test TBUT Corneal staining (F) Schirmer tear test TBUT | 0.56 −0.47 −0.32 0.54 −0.51 −0.33 | S (P<0.01) S (P<0.01) NS S (P<0.01) S (P<0.01) NS | Spearman |
| Pult et al28 | Germany | Clinic-based study | Normal non-contact lens wearers (N=47) | Median age, 35 (range 19–70), 64 | OSDI | NIBUT Corneal staining (F + LG) Conjunctival staining (F + LG) | −0.591 0.012 0.060 | S (P<0.001) NS NS | Pearson or Spearman |
| Kastelan et al55 | Croatia | Clinic-based study | Contact lens wearers (N=16) | 32 (6.3), 38 | OSDI | Schirmer tear test | −0.50 | NR | Pearson |
| Ozcura et al29 | Turkey | Prospective clinic-based study | Normal and DED (N=68) | 44.25 (11.13), 79 | OSDI | Schirmer tear test TBUT | −0.182 −0.296 | NS S (P=0.01) | Pearson |
| Yoon et al56 | South Korea | Clinic-based study | DED (N=50) | 51 (12.1), 82 | OSDI | Corneal staining (F + LG) | 0.297 | NS | Spearman |
| Versura et al23 | Italy | Clinic-based study | Normal (N=25); DED (N=105) | Normal: 44.5 (12.5), 72; DED: 54.8 (15), 76 | OSDI | Tear osmolarity | 0.223 | S (P-value NR) | Pearson |
| de A F Gomes et al57 | Brazil | Clinic-based study | Systemic sclerosis (N=45), of whom DED (N=22) | Normal: 48.7 (10.1), 91.3; DED: 53.5 (14.7), 86.4 | OSDI | TBUT Schirmer tear test Conjunctival staining (RB) | −0.22 −0.11 0.07 | NS | Spearman |
| Bunya et al16 | USA | Cross-sectional study | SS (N=49) | 53.7 (15.9), 92 | OSDI | Schirmer tear test Tear osmolarity | 0.20 −0.39 | NS S (P<0.01) | Spearman |
| Machado et al58 | Brazil | Prospective, randomized, comparative, crossover study | DED (N=30) | Group Ae: 42 (15.96), 87; group Be: 47.67 (10.23), 73 | OSDI | Corneal staining (RB, group A)e Corneal staining (RB, group B)e Corneal staining (LG, group A)e Corneal staining (LG, group B)e | 0.341 0.521 0.328 0.453 | NS S (P<0.05) NS NS | Pearson |
| Frequency of symptom instruments | |||||||||
| Schein et al7,8 | USA | Population-based prevalence study | N=2,420 elderly participants | 73.5 (5.1), 58 | Dry eye symptoms (six-item questionnaire) | Schirmer tear test RB | NR NR | NS NS | Chi-squared test for proportions |
| Macri et al59 | USA and Italy | Case-controlled study | Normal (N=32); MGD (N=54); ATD (N=39) | Normal: 59.79 (14.60); MGD: 60.15 (13.95); ATD: 60.38 (14.23), % female NR for this study. | Frequency of symptoms, eleven-item questionnaire | Corneal staining (F) Schirmer tear test | 0.504 −0.437 | All S (P<0.0001) | Spearman Pearson |
| Macri and Pflugfelder60 | USA | Case-controlled study | Normal (N=19); MGD (N=37); ATD (N=43) | Normal: 59.4 (15.4); MGD: 59.7 (17.5); ATD: 66.3 (16.2), % female NR for this study. | Frequency of symptoms, eleven-item questionnaire | Corneal staining (F) Schirmer tear test | 0.47 −0.34 | All S (P<0.001) | Spearman |
| Gulati et al61 | USA | Clinical validation study | Normal and DED (N=53) | 56 (14), 83 | Frequency of symptoms, two-item instrument | Corneal staining (F) TBUT Schirmer tear test Conjunctival staining (RB) | 0.24 −0.38 −0.34 −0.0002 | NS S (P<0.01) S (P=0.01) NS | Spearman |
| Nichols et al38 | USA | Clinic-based study | DED (N=75) | Median 46.2 (range 21.4–81), 70 | Dryness Grittiness Soreness Redness Fatigue | Total staining (F)/total staining (RB)/Schirmer tear test/TBUT | −0.09 to 0.18 −0.02 to 0.27− 0.13 to 0.12 −0.04 to 0.14 −0.10 to 0.15 | All NS | Spearman |
| Guo et al19 | People’s Republic of China | Population-based study | Normal and DED (N=1,816) | 54.86 (11.72), 44 | Six-item frequency of symptom questionnaire | TBUT ≤10 seconds Corneal staining (F) score ≥1 Schirmer tear test score ≤5 mm | 0.41 0.361 0.164 | All S (P<0.001) | Pearson |
| Lu et al20 | People’s Republic of China | Population-based study | Normal and DED (N=1,840) | 56.25 (12.26), 44 | Six-item frequency of symptom questionnaire | TBUT ≤10 seconds Corneal staining (F) score ≥1 Schirmer tear test score ≤5 mm | 0.302 0.339 0.195 | All S (P<0.001) | Pearson |
| Severity of symptom or other symptom measures | |||||||||
| Begley et al36 | USA | Cross-sectional multicenter study | Normal (N=28); non-SS DED (N=73); SS (N=21) | Normal: 47 (NR), 68; non-SS DED: 52 (NR), 87; SS: 53 (NR), 100 | Clinician grade | Schirmer tear test TBUT Corneal staining (F) Conjunctival staining (LG) | −0.394 −0.482 0.447 0.453 | All S (P≤0.01) | Spearman |
| Self-assessed severity | Schirmer tear test TBUT Corneal staining (F) Conjunctival staining (LG) | −0.323 −0.353 0.273 0.336 | All S (P≤0.01) | Spearman | |||||
| Afonso et al62 | USA | Case-control study | Normal (N=40); DED (N=40) | Normal: 53 (22), NR; DED: 56 (17), NR | 12-item symptom severity questionnaire | Schirmer tear test | −0.39 | S (P<0.001) | Spearman |
| Nguyen et al27 | USA | Prospective, nonrandomized, observational case series | DED (N=18) | 56.6 (15), 72 | Six-page Indiana University Dry Eye Questionnaire 2002 | Schirmer tear test Conjunctival staining (RB) TBUT | −0.357 0.168 −0.229 | All NS | Spearman |
| Yolton et al63 | USA | Clinic-based study | Normal and DED (N=49) | 41.3 (18.6), 57 | Four-item severity of discomfort questionnaire | Total staining (RB) TBUT | 0.24 −0.27 | NS S (P<0.05) | Spearman Pearson |
| Nichols et al64 | USA | Clinical validation study | DED (N=75) | Median 46.2 (range 21.4–81.0), 70 | McMonnies questionnaire | Total staining (F) Total staining (RB) Schirmer tear test TBUT | 0.09 0.09 −0.13 −0.19 | All NS | Spearman |
| Cennamo et al65 | Italy | Clinic-based study | Normal (N=15); DED (N=45) | Normal: 29 (NR), 47; DED: 34 (NR), 49 | Dry eye sensation defined by itching, burning, irritation, and watering | Degree of alteration detected by Schirmer tear test Degree of alteration detected by TBUT | 0.705 0.483 | All S (P<0.01) | Spearman |
| Labbe et al21 | People’s Republic of China | Population-based cross-sectional study | N=1,456; without DED (N=1,215); DED (N=241) | Without DED: 64.33 (9.38), 57.8; DED: 67.26 (9.60), 68.5 | Three-item symptom questionnaire (eye dryness, grittiness, burning) | Schirmer tear test TBUT Corneal staining (F) | −0.04 −0.04 −0.001 | NS NS NS | Pearson |
| Hay et al9 | UK | Population-based cross-sectional study | Ocular and/or dry mouth symptoms (N=341) | Median 46 (male), median 49 (female), 55 | Presence of ocular symptoms | Schirmer tear test | NR | Weak association (positive predictive value = 0.25) | Predictive value analysis |
| Cardona et al15 | Spain | Prospective longitudinal study | Symptoms associated with tear deficiency (N=26) | 37.73 (12.39), 62 | Severity of scratchiness 18 other correlations for total staining (F), TBUT, total staining (LG) versus irritation, dryness, grittiness, soreness, vision changes, light sensitivity | Total staining (F) TBUT Total staining (LG) | 0.47 −0.41 NR NR | S (P<0.05) S (P<0.05) NS NS | Spearman |
| Lin et al10 | Taiwan | Population-based study | DED (N=459) | 72.2 (5.1), 46 | Eight-item interviewer-administered questionnaire | TBUT ≤10 seconds Schirmer tear test score ≤5 mm Corneal staining (F) score ≥1 | NR NR NR | NS S (P<0.05) NS | Comparison of proportions by chi-squared test |
| Mizuno et al17 | Japan | Multicenter study | DED (N=158) | 62.5 (12.6), 91 | General vision Eleven other NEI VFQ-25 subscales (Japanese version) | Total staining (F) Total staining (RB)/TBUT/Schirmer tear test Total staining (RB)/total staining (F)/TBUT/Schirmer tear test | −0.176 −0.019 to 0.111 −0.155 to 0.173 | S (P<0.05) NS NS | Pearson |
| Singh Bhinder and Singh Bhinder11 | India | Clinic-based study | DED (N=16) | 48.56 (16.68), 44 | Reflex epiphora | Total staining (LG) TBUT | NR NR | S (P<0.001) S (P=0.001) | Wilcoxon matched-pairs test |
Notes:
Abbreviations: ATD, aqueous tear deficiency; DED, dry eye disease; EU, European Union; F, fluorescein; LG, lissamine green; MGD, meibomian gland disease; NEI VFQ-25, 25-item National Eye Institute Visual Function Questionnaire; NIBUT, noninvasive breakup time; NR, not reported; NS, not significant; OSDI, Ocular Surface Disease Index©; S, significant; SD, standard deviation; SS, Sjögren’s syndrome; SSD, Symptom Severity of Discomfort scale; RB, rose bengal; TBUT, tear breakup time; VAS, visual analog scale.
Table 2
Summary of signs and symptom measures
| Description | |
|---|---|
| Clinical signs/tests | |
| Schirmer tear test | Assesses tear fluid availability. Severity grading: >10 mm, normal; 6–10 mm, mild-to-moderate; 0–5 mm, severe22 |
| Ocular surface staining | Assesses damage of the ocular surface through staining of the cornea and/or conjunctiva with fluorescein dye, rose bengal, or lissamine green. Grading is on a scale ranging from absent to severe (increases with severity) |
| TBUT | Assesses tear film stability. After fluorescein instillation, the time interval between a complete blink and the first appearance of a dry spot in the precorneal tear film is measured; <10 seconds commonly associated with DED2 |
| Tear osmolarity | Reflects the concentration of solutes in the tear film; an increase of tear osmolarity is a marker of DED1 |
| Patient-reported symptom measures | |
| OSDI | 12-item questionnaire used to assess dry eye symptoms within the past week. 5-point Likert-type response format yielding scores ranging from 0 (least severe) to 100 (most severe)22 |
| NEI VFQ-25 | 25-item vision-related quality of life measurement tool consisting of 12 subscales rated on a 0 (worst) to 100 (best) scale66 |
| VAS | Psychometric response scale used for describing subjective characteristics or attitudes. Respondents mark the location on a 100 mm line that corresponds to the amount of pain, ocular comfort, or symptoms of dryness that they experience |
| Symptom severity and frequency assessments | Assessments of patient-reported severity (eg, absent, mild, moderate, severe) and frequency (eg, none, rarely, sometimes, often, all of the time) of common symptoms (eg, burning, stinging, grittiness, foreign body sensation, tearing, ocular fatigue, dryness) |
Abbreviations: DED, dry eye disease; NEI VFQ-25, 25-item National Eye Institute Visual Function Questionnaire; OSDI, Ocular Surface Disease Index©; TBUT, tear breakup time; VAS, visual analog scale.
For the majority (29/34) of articles identified, the strength of association was measured by the Pearson or Spearman’s correlation coefficients; five articles used other statistical tests (eg, the chi-squared test).7–11 Among the 34 articles, 33 unique studies were reported (Schein et al7,8 reported data from the same study). Of these, 14 studies were conducted in USA/Canada, two in South America, eight in Europe, seven in Asia, and two jointly in USA/Europe. From the 33 unique studies, 175 individual sign–symptom association analyses were reported. Statistical significance was reported for associations between sign and symptom measures in 21 of 33 (64%) studies, but for only 42 of 175 (24%) individual analyses. Of the 175 individual analyses, 148 reported correlation coefficients; the majority of coefficients (129/148; 87%) were between −0.4 and 0.4, indicating low-to-moderate correlation.12–14 For the individual analyses that demonstrated a statistically significant correlation coefficient, one-half (56%) of reported coefficients were in this range. For 27 individual analyses, correlation coefficients were either not reported15 or other statistical tests were used.7–11
For the majority (79%) of individual analyses reporting correlation coefficients, the correlations were in the direction that would be expected for a correlation between increasing severity of signs and increasing severity of symptoms; increases in the severity of symptoms/OSDI score would be expected to be positively correlated with increases in ocular surface dye staining/tear osmolarity and negatively correlated with increases in TBUT/Schirmer tear test results. For most analyses, where correlation was in the opposite direction of that expected, statistical significance was not reached, and the coefficient value was close to zero. Only one significant correlation reported by Bunya et al16 went against the direction expected (negative correlation between OSDI and tear osmolarity).
In reviewing the 33 studies identified, we did not find any consistent trends in relation to the strength/significance of associations between specific measures of signs and symptoms. Table 1 shows associations of composite symptom scores with clinical signs in 30 studies. The remaining three studies15,17,18 reported associations for individual symptoms rather than composite symptom scores. Of these, Nichols and Smith found no significant correlation of individual symptoms with signs.18 Cardona et al reported significant correlations of scratchiness with staining and TBUT, but no other significant correlations.15 The third study by Mizuno et al reported a significant correlation of general vision with fluorescein staining but no other significant correlations.17
We also considered factors of the study design that may have influenced the statistical significance of results, including study size, statistical methods, and study region. With regard to study size, two of the largest population-based surveys (conducted in the People’s Republic of China, N>1,800) reported significant correlations between more frequent symptoms (≥1 symptom reported often or all the time) and lower Schirmer tear test scores (≤5 mm), lower TBUT (≤10 seconds), and higher fluorescein staining (≥1; P<0.001 for all).19,20 However, correlation estimates were modest (r ranging from 0.164 to 0.41), and statistical significance may have been reached owing to the large sample size, rather than clinical significance. Two other large population-based studies (N=2,420;7,8 N=1,45621) did not show a significant correlation between signs and symptoms, while in a large study conducted in Taiwan (N=459), only the Schirmer tear test showed a significant association with symptoms.10 We also considered whether the statistical test that was used to evaluate significance influenced the results, as the Spearman’s test is thought to be less prone to producing misleading findings.3 However, no trend was observed between the test used and the significance levels reported. In addition, the geographic setting did not appear to have an effect on correlation results; statistically significant correlations were reported for 29% and 31% of individual analyses from USA/Canada and the rest of the world, respectively.
Results from three studies provided data on the potential impact of patients’ DED severity on the significance of correlation. In an OSDI validation study, low nonsignificant correlations (ranging from −0.21 to 0.19) were observed between OSDI score and DED clinical tests (Schirmer tear test, TBUT, fluorescein staining, lissamine green staining) in a sample of 109 patients with DED and 30 controls.22 In contrast, statistically significant correlations ranging from −0.38 to 0.31 (P-value ranging from <0.001 to <0.05) were observed when the analysis included only patients with Schirmer tear test scores <10 mm. A second study of 105 patients with DED and 25 controls reported an increase in correlation strength between tear osmolarity and OSDI score as DED severity (based on a severity score system from the Dry Eye WorkShop [DEWS] report)1 increased from mild (r=0.313) to moderate (r=0.462).23 The third study included 186 patients receiving treatment for DED.24 Analyses assessing all patients found a low, albeit statistically significant (r=0.31; P<0.001) correlation between corneal fluorescein staining and symptoms, but no correlation between tear osmolarity and OSDI. The analysis was then repeated after patients were grouped according to previously reported cutoffs for the identification of patients with DED.25,26 These subgroups were 1) OSDI >12 (ie, with ocular surface disease), 2) a change of >4.5 OSDI units, and 3) tear osmolarity value >314 mOsm/L at baseline. Results of OSDI score >12 and tear osmolarity subsets were consistent with those of the broader population. However, the correlation between corneal fluorescein staining and OSDI was higher in the >4.5 OSDI subset compared with that in the total cohort (r=0.46 versus r=0.31, respectively; both P<0.001).
An important consideration for the statistical significance of association is the treatment that subjects may be receiving for DED, since treatment could potentially improve symptoms without an equal effect on signs, or might improve signs while having less effect on symptoms. The influence of patients’ treatment across the studies we reviewed is difficult to judge, as most studies did not provide this information. Of those that did, in the study by Nguyen et al that reported nonsignificant correlations between signs and symptoms, all patients were using artificial tears, and two thirds were using topical cyclosporine.27 In the study by Amparo et al a significant correlation between corneal fluorescein staining and OSDI was reported for the overall study population. The correlation remained significant for patients receiving topical cyclosporine, topical corticosteroids, topical anakinra, and oral tetracycline, but not for patients receiving topical autologous serum.24 In studies by Pult et al28 and Ozcura et al29 in which patients using topical ophthalmic treatment were excluded, OSDI was significantly correlated with TBUT, but not with staining or the Schirmer tear test. From these studies, it does not appear that patients’ treatment had a prominent effect on the significance of correlation.
Discussion
The results of this systematic review indicate that associations between clinical signs of DED and patient-reported symptoms are low and inconsistent. These results may be in part due to the low correlations that have been observed between different objective tests. For example, one study of 635 patients with DED reported very low intratest agreement between the Schirmer tear test, rose bengal, fluorescein staining, and TBUT tests.30 Objective tests assess various disease processes that may have no inherent correlation with each other, which may explain some of this lack of correlation, and individual tests also have been shown to have low repeatability. The Schirmer tear test, in particular, has been suggested to have low reproducibility, with wide variations occurring between subjects and on different days/visits, and the reliability of the test can be affected by environmental conditions, eg, temperature and humidity.6,31 In a prospective clinical study, tear osmolarity was shown to be the most reliable test across normal, mild/moderate, and severe DED (correlation [r2] of 0.55 with disease severity as measured on an objective composite index), while TBUT, corneal staining, conjunctival staining, and Schirmer tear test scores were more informative for the severe forms of disease.32
With regard to symptoms, significant variations have been reported in patients with DED at different times of the day and in different environments, which also may contribute to the low association between signs and symptoms. For example, the proportion of patients with non-SS DED with moderate-to-severe symptoms was found to increase from 32% in the morning to 60% in the evening.33 Despite this, the repeatability of symptom measures may be better than for objective tests. The reliability of the OSDI, in particular, has been shown to be high, with one study reporting an intraclass correlation coefficient between test and retest scores of 0.8222 (values >0.7 are usually considered indicative of adequate test–retest reliability).34
Correlations between different symptom measures may be greater than between different clinical tests. For example, significant correlations between symptoms measured by OSDI and NEI VFQ-25 scores have been observed,35 and high significant correlations between OSDI and the McMonnies questionnaire and the NEI VFQ-25 (r=0.67 and −0.77, respectively) have been reported in patients with and without DED.22 Data from a study by Begley et al36 demonstrated that clinicians’ global grading of severity correlated more highly with patient symptoms (r value ranging from 0.749 to 0.856; P≤0.01) than with clinical signs, suggesting that clinicians may take greater account of patient symptoms in a dry eye evaluation than results of clinical tests.
Another explanation for the low association between ocular signs and symptoms is that they can present independently of each other. Some symptomatic patients have only minimal ocular surface damage, while others demonstrate signs of DED in the absence of specific symptoms or with no symptoms at all. For example, in a study of 344 participants, only 57% of patients with evidence of DED by clinical signs reported an OSDI score >15 (considered indicative of DED).37 Similarly, in a clinic-based sample of 74 patients with an International Classification of Diseases, Ninth Revision code for DED, up to one-third of patients reported never having symptoms of eye fatigue, grittiness, redness, and/or soreness.38
The poor association between signs and symptoms could also be explained in part by the fact that symptom measures may assess particular properties of the disease (eg, grittiness or fatigue), which may not be related to measurable signs. A number of researchers also have suggested that sensory changes on the ocular surface may be an important factor. One theory is that in early/mild DED, corneal hyperalgesia may cause ocular discomfort before any clinical signs are evident.39,40 As corneal damage increases with disease progression, corneal sensation is expected to decrease, which could result in fewer patient-reported symptoms.39 In addition, reduced ocular sensitivity is expected to occur as a result of the normal aging process.41 This hypothesis is supported by the findings of a small study (N=18) that examined the correlation between corneal staining and corneal sensitivity and symptom severity.42 The authors demonstrated significant negative correlations between central corneal sensation and both fluorescein and lissamine green staining of the cornea, indicating that corneal sensation is reduced as ocular surface disease increases. In the same study, negative correlations were demonstrated between symptom severity and corneal staining, suggesting a reduction in symptoms paralleling the observed reduction in corneal sensitivity with increased disease. Bunya et al, who reported significant negative correlations between OSDI and tear osmolarity, also hypothesized that decreased corneal sensation with DED progression could explain their findings.16
The low association between signs and symptoms and the low repeatability of clinical tests have important implications for DED assessment and monitoring the response to treatment, both in the clinic and in clinical trials, in which it may be more difficult to demonstrate significant differences in treatment outcomes owing to the variability of the measurements. Given the discordance between measures, investigations to identify which tests, or combinations of tests, are most predictive of disease progression and long-term ocular surface damage may be valuable in order to inform assessments of DED and the interpretation of results. Efforts also are underway to identify biomarkers of DED progression that more reliably correlate with disease severity and provide a reliable metric of treatment response. Research to achieve a better understanding of the cellular changes that take place in DED also may provide a basis for reclassifying the disease and offer a rationale for subgroups in which signs and symptoms are better correlated.
New concepts are evolving that should further elucidate the pathogenic mechanisms of DED, which may lead to more precise diagnostic classifications, better correlations between signs and symptoms within each subclass, and the design of new therapeutic targets.43,44 Tear cytokines, chemokines, and soluble receptors show particular promise as biomarkers in DED.45–47 In one study, patients with DED were shown to have higher levels of inflammatory mediators in their tears compared with controls. In addition, tear cytokine/chemokine profiles differed between patients with DED with and without meibomian gland dysfunction,47 suggesting that patients with varying forms of DED may have distinctly different underlying pathogeneses, resulting in signs or symptoms that are uniquely expressed. In addition, evidence indicates that neuromediators are altered in the tear film of patients with DED, suggesting that they also could be used as biomarkers in DED. In a small study (N=19), various neuromediators were shown to be correlated with certain signs, but not others, in patients with SS, non-SS DED, and ocular cicatricial pemphigoid.48 For example, subgroup analyses showed that calcitonin gene-related peptide and neuropeptide Y, but not nerve growth factor, were changed in autoimmune (SS and ocular cicatricial pemphigoid) DED. These findings suggest that alterations in tear neuromediators could subclassify patients with DED, potentially improving correlations between signs and symptoms. Other biomarkers that have shown good correlation with DED are gene expression levels of ocular mucins in the conjunctival epithelium49,50 and lipid components in the tear fluid.51
The consistency between signs and symptoms also may be improved by newer tests that circumvent problems encountered with tear assays, such as variability owing to low sample volume or reflex tearing in some patients.52 As an alternative, a brush or membrane can be used to remove conjunctival cells from the conjunctival surface, and proteins assayed by immunostaining/flow cytometry or gene expression levels can be measured with polymerase chain reaction-based techniques.52
The majority of articles we identified used Pearson or Spearman’s correlation coefficients to report the association between signs and symptoms. Correlation coefficients provide an indication of the strength and direction of the linear relationship between two continuous variables; however, care is needed in their interpretation.12,53 One important issue is that statistical significance can be influenced by sample size. For example, two of the largest studies identified in this review (N>1,800)19,20 reported statistically significant correlations with values of r as low as 0.164 (up to 0.41), which may not be clinically meaningful. Another consideration is that since correlation coefficients are only valid for linear associations, a low correlation coefficient value may not imply a lack of association between two variables if the relationship is nonlinear.12,53
In evaluating the studies identified in this review, we did not observe any consistent trends in relation to the strength or significance of associations between specific measures of signs and symptoms, or regarding the influence of methodological factors on association results. However, our assessment was limited by the wide variation in study designs, clinical practices, and assessments used across the studies, making comparisons difficult. Another inherent limitation of the dataset was the small sample size in many of the studies, which may have reduced the ability to detect associations. An additional limitation of the literature search itself was that it did not include the terms “ocular surface disease” or “dysfunctional tear syndrome,” raising the possibility that we may not have captured some references. It is worth noting that most of the studies we reviewed were cross-sectional in design. The use of longitudinal studies in future research would allow for a more definitive understanding of the relationship between signs and symptoms, as an assessment can be made of the degree to which signs and symptoms increase or decrease synchronously over time.
Conclusion
The available evidence suggests that associations between commonly used assessments of signs and symptoms of DED are low and inconsistent. Further studies to increase understanding of the etiopathogenesis of DED and to identify the most reliable and relevant measures of disease are needed to enhance clinical assessment of DED and the measurement of response to therapeutic interventions.
Acknowledgments
This study was funded by Shire. The authors thank Nasser Malik, PhD, of Excel Scientific Solutions, who provided medical writing support funded by Shire.
Footnotes
Disclosure
MSK was an employee of Shire at the time this research was conducted and owns stock in Shire. SJS is an employee of Pharmerit International, who was a paid consultant to Shire in relation to this study. LS was an employee of Pharmerit International at the time this research was conducted and was a paid consultant to Shire in relation to this study. JDB has no financial interest in Shire and has received honoraria and research support from Alcon, Allergan, Bausch and Lomb, and Pfizer. The authors report no other conflicts of interest in this work.
References
Articles from Clinical Ophthalmology (Auckland, N.Z.) are provided here courtesy of Dove Press
Full text links
Read article at publisher's site: https://doi.org/10.2147/opth.s89700
Read article for free, from open access legal sources, via Unpaywall:
https://www.dovepress.com/getfile.php?fileID=27083
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.2147/opth.s89700
Article citations
Effectiveness of cyclosporine nanoemulsion eye drops in patients with mild-to-moderate dry eyes: objective and subjective evaluation.
BMC Ophthalmol, 24(1):401, 09 Sep 2024
Cited by: 0 articles | PMID: 39251947 | PMCID: PMC11385844
Efficacy and Safety of Perfluorohexyloctane in Evaporative Dry Eye Disease Associated With Meibomian Gland Dysfunction: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.
Cureus, 16(8):e67920, 27 Aug 2024
Cited by: 0 articles | PMID: 39206330 | PMCID: PMC11357713
Review Free full text in Europe PMC
Bridging the gap in managing dry eye disease: a consensus report by the Taiwan society of cataract and refractive surgeons.
BMC Ophthalmol, 24(1):314, 29 Jul 2024
Cited by: 0 articles | PMID: 39075430 | PMCID: PMC11285138
Predicting Risks of Dry Eye Disease Development Using a Genome-Wide Polygenic Risk Score Model.
Transl Vis Sci Technol, 13(5):13, 01 May 2024
Cited by: 1 article | PMID: 38767906 | PMCID: PMC11114613
A Phase IIa Multicenter, Randomized, Vehicle-Controlled, Dose Escalating Study to Evaluate the Safety, Efficacy, and Pharmacokinetics of CBT-001 Ophthalmic Solution in Patients With Primary or Recurrent Pterygium.
Ophthalmol Sci, 4(4):100502, 04 Mar 2024
Cited by: 0 articles | PMID: 38883924 | PMCID: PMC11179250
Go to all (109) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Depressive symptoms, resilience, and personality traits in dry eye disease.
Graefes Arch Clin Exp Ophthalmol, 257(3):591-599, 15 Jan 2019
Cited by: 16 articles | PMID: 30648207
Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: clinical implications.
Acta Ophthalmol, 92(2):161-166, 28 Dec 2012
Cited by: 184 articles | PMID: 23279964
Classifying signs and symptoms of dry eye disease according to underlying mechanism via the Delphi method: the DIDACTIC study.
Br J Ophthalmol, 103(10):1475-1480, 12 Jan 2019
Cited by: 3 articles | PMID: 30636211
Rethinking dry eye disease: a perspective on clinical implications.
Ocul Surf, 12(2 suppl):S1-31, 13 Feb 2014
Cited by: 105 articles | PMID: 24725379
Review





