Abstract
Background
The 7.5 kb cryptic plasmid of Chlamydia trachomatis has been shown to be a virulence factor in animal models, but its significance in humans still remains unknown. The aim of this study was to investigate the prevalence and potential involvement of the C. trachomatis cryptic plasmid in causing various clinical manifestations; including infertility, reproductive tract disintegrity, menstrual disorder, and polycystic ovarian syndrome (PCOS) among genital C. trachomatis-infected patients.Results
A total of 180 female patients of child bearing age (mean 30.9 years old, IQR:27-35) with gynecological complications and subfertility issues, who visited Obstetrics and Gynecology clinics in Kuala Lumpur, Malaysia were recruited for the study. Prevalence of genital chlamydial infection among these patients was alarmingly high at 51.1% (92/180). Of the 92 chlamydia-infected patients, 93.5% (86/92) were infected with plasmid-bearing (+) C. trachomatis while the remaining 6.5% (6/92) were caused by the plasmid-free (-) variant. Our data showed that genital C. trachomatis infection was associated with infertility issues, inflammation in the reproductive tract (mucopurulent cervicitis or endometriosis), irregular menstrual cycles and polycystic ovarian syndrome (PCOS). However, no statistical significance was detected among patients with plasmid (+) versus plasmid (-) C. trachomatis infection. Interestingly, plasmid (+) C. trachomatis was detected in all patients with PCOS, and the plasmid copy numbers were significantly higher among PCOS patients, relative to non-PCOS patients.Conclusion
Our findings show a high incidence of C. trachomatis infection among women with infertility or gynecological problems in Malaysia. However, due to the low number of plasmid (-) C. trachomatis cases, a significant role of the plasmid in causing virulence in human requires further investigation of a larger cohort.Free full text

Prevalence of plasmid-bearing and plasmid-free Chlamydia trachomatis infection among women who visited obstetrics and gynecology clinics in Malaysia
Abstract
Background
The 7.5 kb cryptic plasmid of Chlamydia trachomatis has been shown to be a virulence factor in animal models, but its significance in humans still remains unknown. The aim of this study was to investigate the prevalence and potential involvement of the C. trachomatis cryptic plasmid in causing various clinical manifestations; including infertility, reproductive tract disintegrity, menstrual disorder, and polycystic ovarian syndrome (PCOS) among genital C. trachomatis–infected patients.
Results
A total of 180 female patients of child bearing age (mean 30.9 years old, IQR:27–35) with gynecological complications and subfertility issues, who visited Obstetrics and Gynecology clinics in Kuala Lumpur, Malaysia were recruited for the study. Prevalence of genital chlamydial infection among these patients was alarmingly high at 51.1 % (92/180). Of the 92 chlamydia-infected patients, 93.5 % (86/92) were infected with plasmid-bearing (+) C. trachomatis while the remaining 6.5 % (6/92) were caused by the plasmid-free (−) variant. Our data showed that genital C. trachomatis infection was associated with infertility issues, inflammation in the reproductive tract (mucopurulent cervicitis or endometriosis), irregular menstrual cycles and polycystic ovarian syndrome (PCOS). However, no statistical significance was detected among patients with plasmid (+) versus plasmid (−) C. trachomatis infection. Interestingly, plasmid (+) C. trachomatis was detected in all patients with PCOS, and the plasmid copy numbers were significantly higher among PCOS patients, relative to non-PCOS patients.
Conclusion
Our findings show a high incidence of C. trachomatis infection among women with infertility or gynecological problems in Malaysia. However, due to the low number of plasmid (−) C. trachomatis cases, a significant role of the plasmid in causing virulence in human requires further investigation of a larger cohort.
Background
Chlamydia trachomatis is a common bacterial sexually transmitted disease (STD) worldwide. Chlamydial urogenital infection has increased at a fast rate, with more than 2.8 million new cases diagnosed each year [1]. In Malaysia, a high prevalence of chlamydial antibody was detected among urban citizens [2], particularly young females and sex workers [3]. Long term asymptomatic persistency of the pathogen among 50–70 % of individuals results in wide spread of the disease [4], and leads to delayed treatment, which in turn causes prostatitis and epididymitis in males or infertility in females [5]. In females, the pathogen can ascend the reproductive tract to the endometrial epithelium and fallopian tubes, leading to pelvic inflammatory disease (PID) in approximately 20–40 % of the infected patients; among which 11 % develop tubal factor infertility while 9 % show ectopic pregnancy [6]. C. trachomatis-mediated inflammation in the genital tract can result in cervicitis or endometriosis, causing lesions, abnormal mucopurulent discharge and thickening of the uterus inner layer [6]. Inflammation can also contribute to hormonal disorders, i.e., polycystic ovarian syndrome (PCOS) and irregular menses [7]. Additionally, newborn infants can be infected at birth when delivered through an infected birth canal, causing severe conjunctivitis or pneumonia [8].
In recent years, several research groups suggest that the C. trachomatis without plasmid demonstrates a weaker degree of virulence. The plasmid-deficient strains show impaired ability to infect the female mouse genital tract [9, 10]. C. trachomatis infection damages the reproductive tract by activating TLR2 and initiates a Th1-dependent inflammatory response. In a study using plasmid-cured C. muridarum mutant infection in a murine model, TLR2-dependent cytokine was not detected and no sign of oviduct damage can be observed, suggesting that the plasmid-cured mutant has lost virulence [9]. Also, intra-vaginal immunization of the plasmid-deficient strains provide protection in the murine model of genitourinary tract infection [11]; as well as in trachoma infected macaques [12] due to the failure to trigger a Toll-like receptor 2-dependent immune response [13]. These findings have led to research on use of plasmid-deficient strains as a potential human vaccine. In fact, an intravaginal infection of attenuated plasmidless C. trachomatis L2 has been shown to provide protection to the host because it is nonpathogenic and raises systemic antibody in the C3H/HeJ mouse model [11].
Despite compelling evidence in animal models, there is no equivalent finding from human clinical study confirming the significance of plasmid in C. trachomatis infection. A recent study in human ocular C. trachomatis infection reveals that no direct association exists between plasmid copy numbers and disease severity [14]. Therefore, further work should be done to establish the plausible connection. In this study, we investigated the prevalence of plasmid-bearing (+) or plasmid-free (−) C. trachomatis infection and the plasmid copy numbers among obstetrics and gynecology patients in Kuala Lumpur, the capital city of Malaysia. By associating the data with the patients’ clinical presentations, we evaluated the prevalence and risk of plasmid (+) and plasmid (−) variants in affecting gynecological disorders.
Results
Demographics of the study population
The patient cohort from this study comprised 180 female patients of child-bearing age (mean: 30.95 years old; IQR: 27–35) who visited the Obstetrics and Gynecology clinic at the University of Malaya Medical Centerfrom 2010 to 2014 (Table 1). A total number of 124 patients were married, 13 were single or had divorced, and the remaining 43 patients did not reveal their marital status. Most of the patients were of Malay ethnicity (68.3 %), followed by Indians (13.3 %), Chinese (12.7 %), and others (5.5 %), reflecting the demographics of the multiethnic Malaysian population. A majority of the patients recruited to the study presented with gynecological complications or subfertility issues, and had a higher risk of STD infection. The main reason for patients’ visit to the clinic was due to infertility (37 %). Other reasons included abdominal pain, bleeding, menorrhagia, irregular menstrual cycles and others. Two patients had cystectomy whereas one had a history of resolved PID.
Table 1
Patient demographics. Numbers (percentages) of patients with or without C. trachomatis infection; and patients infected with plasmid (−) or plasmid (+) variants. n =
= 180. The P values for all variables were measured with Fisher’s exact test. For age, a t-test (a) was used. n.s.: non-significant
180. The P values for all variables were measured with Fisher’s exact test. For age, a t-test (a) was used. n.s.: non-significant
| Parameters | All patients (n  = = 180) 180) | No infection (n  = = 88) 88) |
C. trachomatis infection (n  = = 92) 92) | P value | OR (95 % CI) | Plasmid (−) C. trachomatis (n  = = 6) 6) | Plasmid (+) C. trachomatis (n  = = 86) 86) | P value | OR (95 % CI) |
|---|---|---|---|---|---|---|---|---|---|
| Age (years) | |||||||||
 Mean [IQR] Mean [IQR] | 30.9 [27–35] | 30.7 [27–34.25] | 31.29 [27–35] | 0.60 n.s. a | 30.2 [26.75–32.25] | 33.3 [27–35] | 0.59 n.s. a | ||
 Maximum Maximum | 45 | 44 | 45 | 36 | 45 | ||||
 Minimum Minimum | 20 | 20 | 20 | 26 | 20 | ||||
| Marital status | |||||||||
 Married Married | 124 (68.8 %) | 55 (44.4 %) | 69 (55.6 %) | 0.078 n.s. | 1.800 (0.94–3.41) | 3 (4.3 %) | 66 (95.6 %) | 0.16 n.s. | 0.303 (0.056–1.62) |
 Single Single | 12 (6.7 %) | 6 (50 %) | 6 (50 %) | 1.00 n.s. | 0.953 (0.29–3.07) | 0 (0 %) | 6 (100 %) | 1.00 n.s. | 0.952 (0.048–18.87) |
 Divorced Divorced | 1 (0.5 %) | 0 (0 %) | 1 (100 %) | 1.00 n.s. | 2.902 (0.11–72.24) | 0 (0 %) | 1 (100 %) | 1.00 n.s. | 4.385 (0.16–118.8) |
 unknown unknown | 43 (23.8 %) | 27 (62.7 %) | 16 (37.3 %) | 0.053 n.s. | 0.475 (0.23–0.96) | 3 (18.7 %) | 13 (81.2 %) | 0.60 n.s. | 5.615 (1.02–3.09) |
| Ethnicity | |||||||||
 Malay Malay | 123 (68.3 %) | 64 (52.1 %) | 59 (47.9 %) | 0.26 n.s. | 0.6705 (0.35–1.26) | 4 (6.7 %) | 55 (93.2 %) | 1.00 n.s. | 1.127 (0.19–6.51) |
 Indian Indian | 24 (13.3 %) | 11 (45.9 %) | 13 (54.1 %) | 0.82 n.s. | 1.152 (0.48–2.72) | 1 (7.6 %) | 12 (92.3 %) | 1.00 n.s. | 1.233 (0.13–11.50) |
 Chinese Chinese | 23 (12.7 %) | 10 (43.5 %) | 13 (56.5 %) | 0.65 n.s. | 1.284 (0.53–3.10) | 1 (7.6 %) | 12 (92.3 %) | 1.00 n.s. | 1.233 (0.13–11.50) |
 Others Others | 10 (5.5 %) | 3 (30 %) | 7 (70 %) | 0.33 n.s. | 2.333 (0.58 to 9.32) | 0 (0.0 %) | 7 (100.0 %) | 1.00 n.s. | 0.815 (0.13–11.50) |
C. trachomatis infection is associated with various gynecological disorders
Genital C. trachomatis infection in each patient was first diagnosed by detection of the C. trachomatis Momp (OmpA) gene. Total DNA was first isolated from the patients’ endocervical swabs and PCR amplified using a human β-globin control primer to ensure the successful extraction of DNA from the endocervical swabs (data not shown). The presence of C. trachomatis DNA was detected with Momp primer using a nested PCR amplification method (outer primers followed by inner primer amplification) [15]. The results were further confirmed using a quantitative real-time PCR method with inner primer alone. MOMP is expressed on the cell surface with a porin activity that is often used for diagnosis of C. trachomatis [16]. Over half of the patients, i.e., 51.1 % (92/180), were diagnosed with genital C. trachomatis infection, suggesting a high incidence of sexually transmitted chlamydial infection among the female patients recruited (Table 2). No significant difference was detected among patients by age, marital status or ethnic background. We then sequenced the Momp PCR product and performed a nucleotide BLAST to assess the diversity of C. trachomatis strains in the local population. Interestingly, our data revealed that all samples examined showed a D serotype (data not shown).
Table 2
Chlamydial infection in patients with different symptoms. Numbers (percentages) of patients with or without C. trachomatis infection. n =
= 180. The P values for all variables were measured with Fisher’s exact test. n.s.: non-significant
180. The P values for all variables were measured with Fisher’s exact test. n.s.: non-significant
| Parameters | All patients (n = = 180) 180) | Non-infected (n = = 88) 88) |
C. trachomatis
-infected (n  = = 92) 92) | P value | Odd Ratio (95 % CI) |
|---|---|---|---|---|---|
| Fertility | |||||
 Fertile Fertile | 112 | 76 (67.9 %) | 36 (32.1 %) | ||
 Infertile Infertile | 68 | 12 (17.6 %) | 56 (82.4 %) | <0.0001*** | 9.852 (4.70 to 20.63) |
  - 1° or 2° infertility - 1° or 2° infertility | 43 | 4 (9.3 %) | 39 (90.7 %) | < 0.0001*** | 20.580 (6.83 to 62.02) |
  - Miscarriage - Miscarriage | 25 | 8 (32.0 %) | 17 (68.0 %) | 0.0013** | 4.486 (1.77 to 11.36) |
| Reproductive tract | |||||
 Normal lining Normal lining | 143 | 79 (55.2 %) | 64 (44.8 %) | ||
 Inflammation Inflammation | 37 | 9 (24.3 %) | 28 (75.7 %) | 0.00088*** | 3.84 (1.69 to 8.72) |
  - Mucopurulent Cervicitis - Mucopurulent Cervicitis | 25 | 9 (36.0 %) | 16 (64.0 %) | 0.0876 n.s. | 2.167 (0.90 to 5.23) |
  - Endometriosis - Endometriosis | 12 | 0 (0.0 %) | 12 (100.0 %) | 0.0001*** | 30.43 (1.77 to 524.2) |
| Menstrual Cycle | |||||
 Regular Regular | 130 | 70 (53.8 %) | 60 (46.2 %) | ||
 Irregular Irregular | 50 | 18 (36.0 %) | 32 (64.0 %) | 0.0452* | 2.074 (1.05 to 4.06) |
| Hormonal Disorder | |||||
 Undiagnosed Undiagnosed | 170 | 87 (51.2 %) | 83 (48.8 %) | ||
 PCOS PCOS | 10 | 1 (10.0 %) | 9 (90.0 %) | 0.0184* | 9.434 (1.17 to 76.14) |
*P<0.05 **P<0.01 ***P<0.001
Overall, C. trachomatis infection showed an association with infertility (OR:9.85, 95 % CI:4.70–20.63, P <
< 0.0001***) (Table 2). Among patients who were fertile, only 32.1 % (36/112) were infected by C. trachomatis, whereas among infertile patients, 82.4 % (56/68) had C. trachomatis infection. Notably, a high C. trachomatis prevalence of 90.7 % (39/43,) was detected among patients who were diagnosed with primary (1°) or secondary (2°) infertility (OR:20.580, 95 % CI:6.83–62.02, P
0.0001***) (Table 2). Among patients who were fertile, only 32.1 % (36/112) were infected by C. trachomatis, whereas among infertile patients, 82.4 % (56/68) had C. trachomatis infection. Notably, a high C. trachomatis prevalence of 90.7 % (39/43,) was detected among patients who were diagnosed with primary (1°) or secondary (2°) infertility (OR:20.580, 95 % CI:6.83–62.02, P <
< 0.0001***). Meanwhile, 68 % (17/25) of patients who experienced miscarriage were infected by C. trachomatis (OR:4.486, 95 % CI:1.77–11.36, P
0.0001***). Meanwhile, 68 % (17/25) of patients who experienced miscarriage were infected by C. trachomatis (OR:4.486, 95 % CI:1.77–11.36, P =
= 0.0013**).
0.0013**).
The inflammation (cervicitis with mucopurulent discharge or endometriosis) of patients’ reproductive tract was recorded by clinicians during examination. C. trachomatis infection showed a close connection with the inflammation in the reproductive system (OR:3.84, 95 % CI:1.69–8.72, P =
= 0.0008***) (Table 2). Our data showed that approximately 64 % (16/25) of patients who were diagnosed with mucopurulent cervicitis (OR:2.167, 95 % CI:0.90–5.23, P
0.0008***) (Table 2). Our data showed that approximately 64 % (16/25) of patients who were diagnosed with mucopurulent cervicitis (OR:2.167, 95 % CI:0.90–5.23, P =
= 0.087) and 100 % (12/12) of patients with endometriosis (OR:30.43, 95 % CI:1.77–524.2, P
0.087) and 100 % (12/12) of patients with endometriosis (OR:30.43, 95 % CI:1.77–524.2, P <
< 0.0001***) had C. trachomatis infection.
0.0001***) had C. trachomatis infection.
In addition, we showed that C. trachomatis infection exhibited significant association with irregular menstrual cycles (OR:2.07, 95 % CI:1.05–4.06, P =
= 0.045*) as well as PCOS (OR:9.43, 95 % CI:1.17–76.14, P
0.045*) as well as PCOS (OR:9.43, 95 % CI:1.17–76.14, P =
= 0.018*), when compared to the uninfected controls.
0.018*), when compared to the uninfected controls.
Higher incidence of plasmid-bearing C. trachomatis infection among patients with infertility, inflammation and PCOS
Next, we investigated if the patients enrolled were infected by plasmid (+) or (−) C. trachomatis variants. Total DNA extracted from the vaginal swabs of the C. trachomatis-infected patients were amplified with two sets of cryptic plasmid primers (which target Pgp1 and Pgp8 respectively) using quantitative real-time PCR analysis. Of the 92 C. trachomatis-infected patients, we detected that 93.5 % (86/92) were caused by plasmid (+) C. trachomatis whereas only 6.5 % (6/92) were caused by plasmid (−) C. trachomatis (Table 1).
When comparing the clinical parameters of the patients, we noted no significant correlation between the plasmid and the tendency for the patients to exhibit infertility (OR:0.76, 95 % CI:0.13–4.40, P =
= 0.562), inflammation (OR:5.26, 95 % CI:0.28–98.68, P
0.562), inflammation (OR:5.26, 95 % CI:0.28–98.68, P =
= 0.155), irregular menses (OR:2.81, 95 % CI:0.31–25.24, P
0.155), irregular menses (OR:2.81, 95 % CI:0.31–25.24, P =
= 0.315) and PCOS (OR:1.59, 95 % CI:0.08–30.6, P
0.315) and PCOS (OR:1.59, 95 % CI:0.08–30.6, P =
= 0.529) (Table 3). Among the patients with infertility, 92.8 % (52/56) cases were diagnosed with plasmid (+) C. trachomatis, compared to only 7.14 % (4/56) cases with plasmid (−) C. trachomatis. Similarly, the majority of the patients who had inflammation in the reproductive tract (96.4 %, 27/28) and PCOS (100 %, 9/9) were caused by plasmid (+) C. trachomatis. Among the 6 patients infected by plasmid (−) C. trachomatis, 2 were fertile while 4 had infertility. However, 5 among the 6 showed no sign of inflammation and had regular menstrual cycles.
0.529) (Table 3). Among the patients with infertility, 92.8 % (52/56) cases were diagnosed with plasmid (+) C. trachomatis, compared to only 7.14 % (4/56) cases with plasmid (−) C. trachomatis. Similarly, the majority of the patients who had inflammation in the reproductive tract (96.4 %, 27/28) and PCOS (100 %, 9/9) were caused by plasmid (+) C. trachomatis. Among the 6 patients infected by plasmid (−) C. trachomatis, 2 were fertile while 4 had infertility. However, 5 among the 6 showed no sign of inflammation and had regular menstrual cycles.
Table 3
C. trachomatis plasmid in patients with different symptoms. Numbers (percentages) of patients infected with plasmid (−) or plasmid (+) C. trachomatis variants. n =
= 92. The P values for all variables were measured with Fisher’s exact test. n.s.: non-significant
92. The P values for all variables were measured with Fisher’s exact test. n.s.: non-significant
| Parameters |
C. trachomatis-infected patients (n = = 92) 92) | Plasmid (−) C. trachomatis (n = = 6) 6) | Plasmid (+) C. trachomatis (n = = 86) 86) | P value | Odd Ratio (95 % CI) |
|---|---|---|---|---|---|
| Fertility | |||||
 Fertile Fertile | 36 | 2 (5.55 %) | 34 (94.4 %) | ||
 Infertile Infertile | 56 | 4 (7.14 %) | 52 (92.8 %) | 0.5629 n.s. | 0.764 (0.13 to 4.40) |
  - 1° or 2° infertility - 1° or 2° infertility | 39 | 3 (7.6 %) | 36 (92.3 %) | 0.5295 n.s. | 0.755 (0.14 to 3.95) |
  - Miscarriage - Miscarriage | 17 | 1 (5.8 %) | 16 (88.2 %) | 0.6939 n.s. | 0.875 (0.09 to 8.01) |
| Reproductive tract | |||||
 Normal lining Normal lining | 64 | 5 (7.8 %) | 59 (92.1 %) | ||
 Inflammation Inflammation | 28 | 1 (3.5 %) | 27 (96.4 %) | 0.4045 n.s. | 2.288 (0.25 to 20.55) |
  - Mucopurulent Cervicitis - Mucopurulent Cervicitis | 16 | 0 (0.0 %) | 16 (100 %) | 0.1550 n.s. | 5.269 (0.28 to 98.68) |
  - Endometriosis - Endometriosis | 12 | 1 (8.3 %) | 11 (91.6 %) | 0.5786 n.s. | 0.733 (0.078 to 6.88) |
| Menstrual Cycle | |||||
 Regular Regular | 60 | 5 (8.3 %) | 55 (91.6 %) | ||
 Irregular Irregular | 32 | 1 (3.1 %) | 31 (96.8 %) | 0.3153 n.s. | 2.818 (0.31 to 25.24) |
| Hormonal Disorder | |||||
 Undiagnosed Undiagnosed | 83 | 6 (72.2 %) | 77 (92.7 %) | ||
 PCOS PCOS | 9 | 0 (0 %) | 9 (100 %) | 0.5293 n.s. | 1.59 (0.083 to 30.6) |
Higher relative plasmid copy numbers associated with PCOS
To examine if the abundance of plasmid in C. trachomatis is associated with the presence of the clinical symptoms, we quantified the plasmid copy numbers in each patient (Figure 1). The average CT value from two cryptic plasmid primers (Pgp1 and Pgp8) for each patient was obtained. Relative plasmid copy numbers per bacterium (ratio for plasmid:Momp) for all 92 C. trachomatis-infected patients were calculated. In general, we noticed no direct connection between fertility, the reproductive tract lining and menstrual cycle, consistent with the previous studies in human ocular infection and in vitro tissue tropism [14, 17]. Notably, PCOS patients showed a higher plasmid copy number (2.386 ±
± 0.284 versus 1.734
0.284 versus 1.734 ±
± 0.096, P
0.096, P =
= 0.0472), relative to the non-PCOS patients. Although endometriosis patients also demonstrated a comparatively higher plasmid copy number, (2.193
0.0472), relative to the non-PCOS patients. Although endometriosis patients also demonstrated a comparatively higher plasmid copy number, (2.193 ±
± 0.308 versus 1.714
0.308 versus 1.714 ±
± 0.110, P
0.110, P =
= 0.114), no statistical significance was noted.
0.114), no statistical significance was noted.
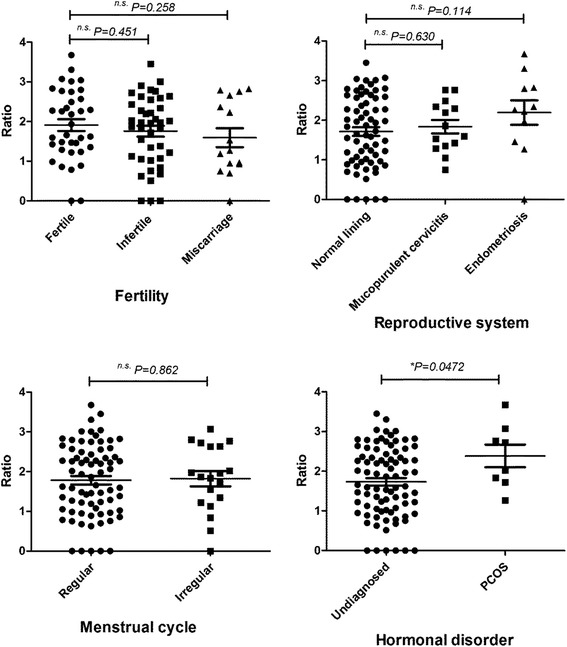
Plasmid copy numbers among C. trachomatis-infected patients with different clinical parameters. Dot plot graphs show the ratio of plasmid:Momp as determined by quantitative real-time PCR assay. Each dot represents data from a single patient in each group (n =
= 92). The P values were measured with unpaired Student’s t-test. Data was considered significant when *P
92). The P values were measured with unpaired Student’s t-test. Data was considered significant when *P <
< 0.05. n.s.: non-significant
0.05. n.s.: non-significant
Discussion
In this study, we reported a high prevalence (51.1 %) of C. trachomatis infection among female adults of child bearing age, with subfertility or gynecological problems who visited Obstetrics and Gynecology clinics in Malaysia. This indicates that there is a pressing need for wider population screening to increase awareness and prevent the spread of the disease among the community. Most of the patients who demonstrated symptoms were diagnosed with genital C. trachomatis infection, including infertility (82.4 %), reproductive system lesions (75.7 %), irregular menses (64 %) and PCOS (90 %), suggesting the C. trachomatis is a leading factor for female reproductive system disorders.
Although a high rate of genital C. trachomatis prevalance was detected in our study, the patients recruited were suspected to be at risk of the bacterial infection based on the clinical examination. The rates of C. trachomatis infection vary in different studies depending on the group of patients recruited and the study region. For example, a study using 50 infertile female patients showed a 40 % infection rate by C. trachomatis [18] whereas other studies reported only a 8 % [19] or 15 % C. trachomatis infection rate. Among patients with tubal infertility, the prevalence of C. trachomatis was reported to be 38.3 % among 120 patients [20]. Consistent to the previous study, the presence of plasmid (+) C. trachomatis was high (93.5 %). However, the prevalence using real-time PCR amplification depends highly on the assay sensitivity. For data validation, a glycogen-positive test for bacterial isolates can be used to confirm the presence of plasmid in the bacteria [21].
Various research groups have established that the plasmid (+) C. trachomatis demonstrated a higher virulence in animal models of ocular or genital infections [9–14]. Consistent with these findings, our results showed that high percentages of those who had infertility (92.8 %), inflammation in the reproductive tract (96.4 %), irregular menses (96.8 %) and PCOS (100 %) were diagnosed with plasmid (+) but not plasmid (−) variants of C. trachomatis. Although these observations provide support for previous work which suggests the usage of plasmidless C. trachomatis as a potential human vaccine [11], caution must be taken as some of the patients who showed symptoms were infected by the plasmid (−) strains. Also note that the genetic diversity of human populations may contribute to results contradicting experiments performed using inbred animals. Therefore, additional surveys which involve a larger human cohort should be conducted to ensure the over-all safety of the plasmidless strains among individuals from diverse backgrounds.
Plasmid (+) or (−) C. trachomatis strains demonstrated no difference with regards to growth kinetics, plaquing efficiency and size but showed a defect in glycogen granule accumulation and intrainclusion movement [10]. A recent study showed that C. trachomatis is capable of inducing alteration to global host histone modifications and double strand break repair, thus generating an environment favorable for malignant transformation [22]. In fact, C. trachomatis infection poses risk for infected individuals to develop cervix intraepithelial neoplasia [23, 24], in a similar way to other tumor-inducing pathogens. Extra-chromosomal plasmid DNA may play a role in integrating with the host genome which leads to this pathological damage. The conserved 7.5 kb cryptic plasmid is a small, non-conjugative and non-integrative extrachromosomal DNA that contains genes encoding 8 proteins [25]. The plasmid Pgp3 encodes for immunogenic trimers which trigger specific antibody production in infected individuals [26, 27]; and is secreted into the cytosol of infected cells during chlamydial infection [28, 29]. Meanwhile, Pgp4 encodes for a protein which comprises a putative helix-loop-helix domain which functions as transcriptional regulator for virulence-associated genes [10, 30]. Therefore, expression of plasmid genes may be crucial in leading to clinical symptoms. To support this notion, a quantitative protein analysis could be carried out in the future to measure the amount of plasmid-derived proteins in the patient sample.
Conclusion
In conclusion, we suggest that plasmids maybe a potential risk factor for reproductive system disorders including infertility, inflammation in the reproductive tract, irregular menses and PCOS in genital chlamydial infection. However, continued work is required to substantiate plasmids as a virulence factor in future studies with a larger human cohort.
Methods
Study design
A total number of 180 female patients of child-bearing age who visited the Obstetrics and Gynecology Outpatient Clinics at the University of Malaya Medical Centre voluntarily participated in the study from 2010 to 2014. Detailed clinical information on reasons for referral, gynecological history including menstruation, symptoms of genital and urinary tract infection, obstetric and medical histories were documented. The subjects’ vulva and cervix were examined for the presence of lesions, warts, ulcers, ectopy, erythma and discharge. Patients with a positive urine pregnancy test, recent antibiotic therapy, yeast infection and genital tuberculosis were excluded from the study. The participants were briefed that their blood and vaginal swab samples will be used for research purposes, and written consent was obtained. This study has been approved by the University of Malaya Medical Centre Medical Ethics Committee.
DNA extraction
Endocervical swabs were collected by using a Floqswab (Copan, Brescia, Italy) and transferred to a laboratory in a UTM-RT universal transport medium tube (Copan). The samples were vortex mixed and the cells were centrifuged at 400× g for 10 min. The cells recovered were lysed and separated with phenol chloroform. The DNA was precipitated using 1:10 volume of 3 M sodium acetate and isopropanol at −20 °C overnight incubation. The samples were washed and eluted with TE buffer.
PCR amplification
Diagnosis of C. trachomatis was performed as described [15]. Nested PCR was performed to amplify the genes that encode for Major Outer Membrane Protein (MOMP) and plasmid using outer and inner primers (Table 4). PCR samples were run in a Veriti Thermal Cycler (Applied Biosystems, Essex, UK) at the following conditions: 95 °C for 3 min, 30 cycles of 95 °C for 30 s, 50 °C for 1 min, and 72 °C for 1 min, followed by a final extension at 72 °C for 7 min using HelixAmp Taq DNA polymerase (Nanohelix, Daejeon, South Korea). The first round PCR was amplified using 50 ng of DNA isolated from endocervical swabs with outer primer pairs. Then, 1 μl of first round PCR product was used as the template in the second round PCR and amplified with inner primer pairs. The amplicons were run on gel electrophoresis using 1.5 % agarose gel and viewed under a UV transilluminator. Human β-globin gene was used as a positive control to confirm successful DNA retrieval from patient swabs. PCR amplification for human β-globin primer was run separately in PCR master mix containing a total volume 50 μl as follows: 1 μl template DNA, 200 mM of each of dNTP, 25 pmol of each primer, 4 mM Tune Up solution, 5 μl of PCR buffer and 2.5 units of HelixAmp Taq DNA polymerase recombinant (Nanohelix, Daejeon, South Korea). PCR samples were run at the following conditions: 95 °C for 3 min, 30 cycles amplification consisted of 95 °C for 30 s, 50 °C for 1 min, and extension at 72 °C for 1 min, followed by final extension at 72 °C for 7 min.
Table 4
PCR primers used in C. trachomatis conventional PCR and real-time PCR diagnosis. For nested PCR amplification of Momp and plasmid, outer primer pairs were used at first round PCR, while inner primer pairs were used at second round PCR amplification. For real-time PCR diagnosis, Momp inner primer pairs, plasmid Pgp8 inner primer pairs and plasmid Pgp1 primer pairs were used
| Target genes | Primer | Sequence (5′-3′) | Amplicon size |
|---|---|---|---|
| Momp | Outer forward | TTGTTTTCGACCGTGTTTTG | 455 bp |
| Outer reverse | AGCRTATTGGAAAGAAGCBCCTAA | ||
| Inner forward | AAACWGATGTGAATAAAGARTT | 395 bp | |
| Inner reverse | TCCCASARAGCTGCDCGAGC | ||
| Plasmid Pgp8 | Outer forward | TTGGCYGCTAGAAAAGGCGATT | 212 bp |
| Outer reverse | TCCGGAACAYATGATGCGAAGT | ||
| Inner forward | AACCAAGGTCGATGTGATAG | 150 bp | |
| Inner reverse | TCAGATAATTGGCGATTCTT | ||
| Plasmid Pgp1 | Forward | TTCTTTGATGGCTTCCCAAC | 456 bp |
| Reverse | ACGATTTTCTCCAACCGATG | ||
| β-globin | Forward | GAAGAGCCAAGGACAGGTAC | 268 bp |
| Reverse | CAACTTCATCCACGTTCACC |
Quantitative real-time PCR amplification
A quantitative real-time PCR assay was used to confirm the diagnosis and to determine the plasmid copy numbers in patient samples. DNA samples isolated from the vaginal swabs of C. trachomatis-infected patients were prepared. Mastermix containing 1 μl template DNA, 1× SsoAdvanced Universal SYBR Green Supermix (Biorad, Hercules, CA), 10 pmol primers were run using a Mx3000 Stratagene thermacycler (Agilent Technologies, Santa Clara, CA). Primers used were inner primers for Momp, inner primer for plasmid Pgp8, and plasmid Pgp1 primers. Plasmid copy number for each patient was calculated as below:
Sequencing
Amplification of an approximately 871 bp fragment of OmpA was performed by nested PCR. The first PCR step was carried out with outer primer pair (Table 1) using 10 μl of DNA extracted from swabs. Amplification was performed in a final reaction volume of 50 μl containing 0.3 μM of each primer, 0.2 mM of dNTPs, 3 μl of TuneUp solution (Nanohelix, Korea) and 5U of HelixAmp™Taq DNA polymerase (Nanohelix, Korea). The first amplification conditions consisted of initial polymerase activation at 94 °C for 2 min; 40 cycles of 94 °C for 45 s, 60 °C for 45 s and 72 °C for 90 s and a final elongation step at 72 °C for 5 min. In the second round PCR, 3 μl of product from the first PCR step was amplified using inner primer pairs (Table 1). Nested PCR conditions consisted of 95 °C for 5 min; 40 cycles of 94 °C for 1 min, 60 °C for 1 min and 72 °C for 2 min and a final elongation step at 72 °C for 10 min. The amplified products were visualized by electrophoresis on 1.5 % agarose gel stained with GelRed solution (Biotium).
The 871 bp OmpA fragments obtained were purified using a QIAquick Gel Extraction kit (Qiagen) and processed using a BigDye® Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems, Foster City, CA). The reaction mixtures were loaded onto a 3730xL DNA Analyzers (Applied Biosystems). The primers used for sequencing were inner primer pairs. Nucleotide sequence data were assembled by Bioedit and residues corresponding to flanking primers were excluded from analysis. Sequences were submitted to the standard nucleotide BLAST search engine at the National Center for Biotechnology Information (blast.ncbi.nlm.nih.gov/Blast.cgi) to determine the genotype.
Statistical analysis
Statistical analysis was done using GraphPad PRISM version 5. For normally distributed data, an unpaired t-test was used. For categorical data (clinical symptoms), Fisher’s exact test was used, with a no-symptom group as control. Odd ratio (OR) and 95 % confidence interval (CI) were calculated. Statistical significance was determined at P <
< 0.05*, P
0.05*, P <
< 0.01** and P
0.01** and P <
< 0.001***.
0.001***.
Acknowledgements
The authors would like to thank the volunteers and nurses at the University of Malaya Medical Center Obstetrics and Gynecology clinics for their assistance in sample collection. This study was supported by grants from Malaysia Ministry of Higher Education (HIR-MOHE E000013-20001) to WFW and Fundamental Research Grant Scheme (FRGS) FP027-2010B to NSS.
Abbreviations
| MOMP | Major outer membrane protein |
| OD | optical density |
| PCOS | polycystic ovary syndrome |
| PID | pelvic inflammatory disease |
| STD | sexually transmitted disease |
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
NSS, EMS, BPA, RG and SAB designed and supervised the study. TCY, FS, GMYT, and EM performed the experiments. SS and JH collected the samples and recorded clinical parameters of all patients. WFW and CYL performed statistical analysis of the study. TCY and WFW wrote the manuscript. All authors read and approved the final manuscript.
Contributor Information
Won Fen Wong, Phone: +603 79676672, Email: ym.ude.mu@nefnow.
Negar Shafiei Sabet, Email: ym.ude.iges@ragen.
References
Articles from BMC Microbiology are provided here courtesy of BMC
Full text links
Read article at publisher's site: https://doi.org/10.1186/s12866-016-0671-1
Read article for free, from open access legal sources, via Unpaywall:
https://bmcmicrobiol.biomedcentral.com/track/pdf/10.1186/s12866-016-0671-1
Citations & impact
Impact metrics
Article citations
Antibody responses to Chlamydia trachomatis vaccine candidate antigens in Chlamydia-infected women and correlation with antibody-mediated phagocytosis of elementary bodies.
Front Cell Infect Microbiol, 14:1342621, 02 Feb 2024
Cited by: 0 articles | PMID: 38371301 | PMCID: PMC10869445
The serodiagnositic value of Chlamydia trachomatis antigens in antibody detection using luciferase immunosorbent assay.
Front Public Health, 12:1333559, 27 Feb 2024
Cited by: 0 articles | PMID: 38476494 | PMCID: PMC10927828
Chlamydia Infection Remodels Host Cell Mitochondria to Alter Energy Metabolism and Subvert Apoptosis.
Microorganisms, 11(6):1382, 24 May 2023
Cited by: 1 article | PMID: 37374883 | PMCID: PMC10301204
Review Free full text in Europe PMC
Association between Chlamydial Infection with Ectopic and Full-Term Pregnancies: A Case-Control Study.
Trop Med Infect Dis, 7(10):285, 06 Oct 2022
Cited by: 3 articles | PMID: 36288026 | PMCID: PMC9609621
The role of tryptophan in Chlamydia trachomatis persistence.
Front Cell Infect Microbiol, 12:931653, 02 Aug 2022
Cited by: 6 articles | PMID: 35982780 | PMCID: PMC9378776
Review Free full text in Europe PMC
Go to all (18) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Diversity of endocervical microbiota associated with genital Chlamydia trachomatis infection and infertility among women visiting obstetrics and gynecology clinics in Malaysia.
PLoS One, 14(11):e0224658, 18 Nov 2019
Cited by: 14 articles | PMID: 31738795 | PMCID: PMC6860443
Activation of neutrophils by Chlamydia trachomatis-infected epithelial cells is modulated by the chlamydial plasmid.
Microbes Infect, 20(5):284-292, 02 Mar 2018
Cited by: 15 articles | PMID: 29499390
[Chlamydia trachomatis infection in women and the use of oral contraceptives].
Ned Tijdschr Geneeskd, 135(8):323-327, 01 Feb 1991
Cited by: 0 articles | PMID: 2008220
Vaccines for Chlamydia infections of the female genital tract.
Future Microbiol, 3(1):67-77, 01 Feb 2008
Cited by: 19 articles | PMID: 18230035
Review
Funding
Funders who supported this work.
Fundamental Research Grant Scheme (FRGS) (1)
Grant ID: FP027-2010B
High Impact Research (HIR) Grant (1)
Grant ID: HIR-MOHE E000013-20001






