Abstract
Background
A breast cancer diagnosis can entail numerous physical and psychosocial challenges. Yoga practice (YP) may contribute to improved well-being for these patients.Primary study objective
Investigate feasibility and impact of YP on quality of life (QoL), mood, fatigue, and perceived stress immediately after breast cancer diagnosis.Methods
Thirty women were randomly assigned to a yoga group (YG) or control group (CG) immediately after cancer diagnosis.Setting
Pilot study conducted at an academic medical center breast clinic.Participants
Females (N = 30) who received a biopsy-proven breast cancer diagnosis without metastatic disease.Intervention yg
One individual YP session at baseline, then 2 individual and 8 weekly group sessions followed by weekly gentle yoga at home (DVD). Questionnaires and saliva samples (ie, cortisol) completed at baseline and 12 weeks postdiagnosis.Results
Both groups reported significant improvements in QoL postintervention but with no significant difference between groups. Emotional well-being, mood-related tension-anxiety, depression-dejection, and confusion-bewilderment scores improved for both groups, and cortisol and cortisone levels decreased. Lumpectomies were prevalent with YG (67%) and CG (47%). YP was rated as "very effective," providing relaxation (85%), stress relief (69%), and reduced muscle tension/general feeling of wellness (each 62%).Conclusion
Feasibility of YP immediately after breast cancer diagnosis was good. Improvement in emotional well-being, anxiety, depression, and levels of confusion was found in both groups. To our knowledge, this is the first study examining the impact of YP immediately after breast cancer diagnosis. Further research in this area is warranted.Free full text

Language: English | Chinese | Spanish
A Randomized Controlled Pilot Study Assessing Feasibility and Impact of Yoga Practice on Quality of Life, Mood, and Perceived Stress in Women With Newly Diagnosed Breast Cancer
一项评估瑜伽练习对新诊断出患有乳腺癌的女性的生活质量、情绪和感知到的压力之 可行性和影响的随机对照试验研究
Estudio piloto controlado y aleatorizado para evaluar la viabilidad y el impacto de la práctica de yoga sobre la calidad de vida, el estado de ánimo y el estrés percibido en mujeres con cáncer de mama de reciente diagnóstico
Abstract
Background:
A breast cancer diagnosis can entail numerous physical and psychosocial challenges. Yoga practice (YP) may contribute to improved well-being for these patients.
Primary Study Objective:
Investigate feasibility and impact of YP on quality of life (QoL), mood, fatigue, and perceived stress immediately after breast cancer diagnosis.
Methods:
Thirty women were randomly assigned to a yoga group (YG) or control group (CG) immediately after cancer diagnosis.
Setting:
Pilot study conducted at an academic medical center breast clinic.
Participant(s):
Females (N = 30) who received a biopsy-proven breast cancer diagnosis without metastatic disease.
Intervention (YG):
One individual YP session at baseline, then 2 individual and 8 weekly group sessions followed by weekly gentle yoga at home (DVD). Questionnaires and saliva samples (ie, cortisol) completed at baseline and 12 weeks postdiagnosis.
Results:
Both groups reported significant improvements in QoL postintervention but with no significant difference between groups. Emotional well-being, mood-related tension-anxiety, depression-dejection, and confusion-bewilderment scores improved for both groups, and cortisol and cortisone levels decreased. Lumpectomies were prevalent with YG (67%) and CG (47%). YP was rated as “very effective,” providing relaxation (85%), stress relief (69%), and reduced muscle tension/general feeling of wellness (each 62%).
Conclusion:
Feasibility of YP immediately after breast cancer diagnosis was good. Improvement in emotional well-being, anxiety, depression, and levels of confusion was found in both groups. To our knowledge, this is the first study examining the impact of YP immediately after breast cancer diagnosis. Further research in this area is warranted.
背景
背景:乳腺癌的诊断结果可能要使 患者承受诸多身体和心理挑战。瑜 伽练习 (YP) 或有助于改善这些患 者的身心健康。
主要研究目标:研究 YP 对紧接乳 腺癌诊断后的生活质量 (QoL)、情 绪、疲劳和感知到的压力之可行性 和影响。
方法: 三十名女性在癌症诊断后立 即被随机分配至一个瑜伽小组 (YG) 或对照小组 (CG)。
机构: 试验研究在一个学术医疗中 心的乳房诊所开展。
参与者: 已经活检确诊是乳腺癌而 癌症尚无转移的女性 (N=30)。
干预 (YG): 基线时安排一次个人 YP 课程,然后安排 2 次个人课程 和 8 次每周小组课程,最后每周在 家进行柔和瑜伽锻炼 (DVD)。于基 线时和诊断后 12 周展开问卷调查 并采集唾液样本(即皮质醇)。
效果: 干预后,两组均报告 QoL 显著改善,但两组无明显区别。两 组的情感健康、情绪相关紧张-紧 张-焦虑、抑郁-沮丧,及混乱- 困惑分数均有所提高,皮质醇和皮 质酮水平下降。两组中进行乳房肿 瘤切除术的比例较大, YG 组为67% ,对照组为47% 。YP 被评为“非常 有效”,让人放松 (85%)、缓解精 神压力 (69%) 及缓解肌肉紧张/大 体感觉健康(各为 62%)。
结论: 紧接乳腺癌诊断后 YP 可行 性良好。两组的情绪健康、焦虑、 抑郁和混乱程度有所改善。据我们 所知,这是首次紧接乳腺癌诊断后 验证 YP 之影响的研究。此领域的 进一步研究已获批准。
SINOPSIS
Fundamentación:
Un diagnóstico de cáncer de mama puede conllevar numerosos retos físicos y psicosociales. La práctica de yoga puede contribuir a la mejora del bienestar de estos pacientes.
Objetivo principal del estudio:
Investigar la viabilidad y el impacto de la práctica de yoga sobre la calidad de vida (CdV), el estado de ánimo, el cansancio y el estrés percibidos inmediatamente después del diagnóstico de cáncer de mama.
Métodos:
Se asignó un grupo de treinta mujeres a un grupo de yoga (GY) o de control (GC) inmediatamente después del diagnóstico de cáncer.
Participante(s):
Mujeres (N = 30) que recibieron un diagnóstico de cáncer de mama sin metástasis demostrado mediante biopsia.
Intervención (YG):
Una sesión individual de práctica de yoga al inicio; a continuación, 2 sesiones individuales y 8 sesiones semanales en grupo, seguidas de yoga suave semanal en su hogar (DVD). Se rellenaron cues-tionarios y se tomaron muestras de saliva (por ejemplo, para la determinación de cortisol) al inicio y 12 semanas después del diagnóstico.
Resultados:
Ambos grupos notificaron mejoras significativas en la CdV posintervención, sin diferencia significativa entre los grupos. En ambos grupos mejoraron las puntuaciones de bienestar emocional, tensión-tensión-ansiedad relacionadas con el estado de ánimo, las puntuaciones de depresión-abatimiento y confusióndesconcierto, y disminuyeron las concentraciones de cortisol y cortisona. Las mastectomías parciales fueron prevalentes, con un 67 % en el GY y un 47 % en GC. La práctica de yoga se calificó de “muy efectiva” en la relajación (85 %), el alivio del estrés (69 %) y la reducción de la tensión muscular o mejora de la sensación de bienestar general (62 % cada una).
Conclusiones:
La viabilidad de la práctica de yoga inmediatamente después del diagnóstico de cáncer fue buena. En ambos grupos se hallaron mejoras en el bienestar emocional, la ansiedad, la depresión y los niveles de confusión. Que sepamos, este es el primer estudio que explora el impacto de la práctica de yoga inmediatamente después del diagnóstico de cáncer de mama. Se aconseja continuar la investigación en este área.
INTRODUCTION
Women with a new diagnosis of breast cancer frequently experience stress, emotional distress, anxiety, and fatigue before, during, and after treatment. Quality of life (QoL) in the first year after breast cancer diagnosis is significantly affected1 and correlates positively with survival.2 Alternative methods of exercise like yoga have shown promise in improving QoL in breast cancer survivors.3,4 Yoga is a complementary, mind-body exercise and relaxation strategy.5 The term yoga comes from a Sanskrit word that means yoke (harmony) or union, and yoga has been described as the union of mind, body, and spirit, consisting of skills, tools, or techniques such as pranayama (breath work); asana (physical postures, movement); and meditation (concentration, mental clarity, and awareness). According to Yoga Journal, 11 million people in the United States perform yoga occasionally, and approximately 6 million practice yoga on a regular basis. In small pilot studies, hatha yoga, the most commonly practiced form of yoga in the United States, has been found to decrease stress, anxiety, and fatigue.6–9
Studies designed using yoga to assess physical and psychological benefits, QoL, emotional outcomes, and fatigue in breast cancer survivors have primarily shown positive and beneficial effects.8 Studies of individuals participating in stress reduction programs such as yoga or other mindfulness-based exercises also have shown a reduction in salivary cortisol levels,10,11 which can be a surrogate marker for stress levels. Breast cancer malignancy has been associated with activation of the hypothalamic-pituitary-adrenal (HPA) axis, and the biopsychological aspects of a new cancer diagnosis can subsequently result in cortisol dysregulation.11 Salivary cortisol and cortisone were therefore also examined in this study.
Even though the effects of yoga have been studied in breast cancer survivors at different stages of treatment, there is limited data on the effects of yoga in the immediate postdiagnosis period. The pilot study sought to examine the feasibility of a yoga practice (YP) in the period immediately following a breast cancer diagnosis. We hypothesized that compared with the control group (CG) participants, participants in a yoga group (YG) would experience improvement in QoL, mood, stress, and fatigue, and we predicted a greater decrease in cortisol levels from pre- to posttreatment in the YG.
METHODS AND DESIGN
Thirty women with a new diagnosis of biopsy-proven breast cancer were enrolled between November 1, 2010, and August 30, 2011. Participants were recruited from the Breast Cancer Clinic at Mayo Clinic in Rochester, Minnesota, where they received preoperative education and counseling regarding potential breast cancer surgical options.
Participants
Participants were female, aged 21 years or older, with a recent biopsy-proven diagnosis of noninvasive or invasive breast cancer without evidence of meta-static disease, with plans to undergo the standard treatment of surgery for breast cancer, and residing within a 45-minute driving distance of the local yoga studio where classes were conducted.
Exclusion criteria included patients previously having participated in regular yoga classes (1 or more days per week), having maintained a regular personal practice of yoga in the past 3 months, or otherwise planning to start yoga while being enrolled in the study. In addition, those patients planning to receive neoadjuvant chemo-therapy, being pregnant, or not speaking English were excluded. The study was approved by the Mayo Clinic Institutional Review Board.
Intervention
Participants were randomly assigned to either the YG (n = 15) or the CG (n = 15). Information about demographics, breast cancer diagnosis, stage of disease, and prescribed treatment regimen (surgery, chemotherapy, radiation) were collected from medical charts. Both groups completed baseline surveys and provided a baseline salivary cortisol sample. After study completion, participants in the CG were offered 8 weekly, 60-minute yoga sessions, similar to the YG.
Measures
Participants completed the following surveys and evaluation pre- and postintervention.
Mayo Clinic Complementary and Alternative Therapy (CAM) Survey. This survey collects information about previous participation in other complementary and alternative therapy programs, as well as satisfaction and perceived effectiveness of the intervention.
Functional Assessment of Cancer Treatment—Breast Cancer (FACT-B). The FACT-B is a 44-item instrument measuring multidimensional QoL in patients with breast cancer.12
Perceived Stress Scale (PSS). The PSS is a widely used 10-item, self-report instrument measuring the perception of stress.13
The Profile of Mood States—Short Form (POMSSF). The POMS-SF is a 37-item short form of the Profile of Mood States measuring psychological distress.14
Brief Fatigue Inventory (BFI). The BFI is a 9-item scale asking patients to rate their current, usual, and worst level of fatigue in the last 24 hours.15
Salivary cortisol levels. All participants provided single salivary cortisol samples at baseline and at 12 weeks for assessment of cortisol levels. Samples were collected using Salivette devices (Sarstedt Salivette Supply T154, Nümbrecht, Germany).
Yoga Practice Intervention
The YG participants (n = 15) were instructed by a registered yoga instructor (ie, a minimum of 200 hours of yoga training and in good standing with the Yoga Alliance). Participants received three individual therapeutic yoga sessions (60 minutes). The first session was individualized at the time of consent, and participants were given information on YP assessment and the first component of yoga, pranayana (breath work). The second and third individual yoga sessions started 1 week after surgery at a local yoga studio. The yoga offered was a combination of gentle and hatha yoga, which included pranayama and gentle movements of the upper and lower body on a chair or mat. Those in the YG were asked to attend one weekly 60-minute gentle YG class for 8 weeks during the postoperative period (week 4 to week 12). All participants received a gentle yoga DVD to use at home at least once per week.
Control Group
The CG (n = 15) continued with usual care before and after the surgical procedure. Following the study completion, the CG participants were offered eight free yoga classes and provided with a yoga DVD.
Main Outcome Measures
Participant characteristics and outcomes were summarized with frequencies and percentages for categorical data and with mean and range (or median and interquartile range [IQR] where appropriate) for continuous data. Cortisol, cortisone, QoL, mood, fatigue, and perceived stress levels within each treatment group were compared between baseline and 12 weeks postintervention with Wilcoxon signed-rank tests, and the pre- and post-differences were compared between treatment groups with Wilcoxon rank-sum tests. Although this was designed as a pilot study and thus underpowered to detect small differences, P values < .05 were considered statistically significant. All analyses were performed using SAS version 9 (Cary, North Carolina).
RESULTS
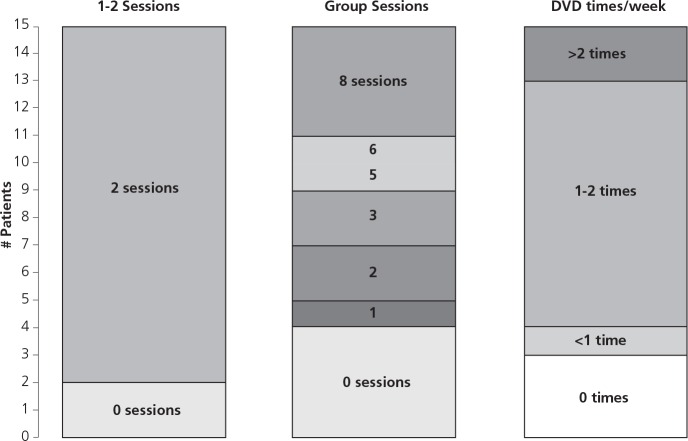
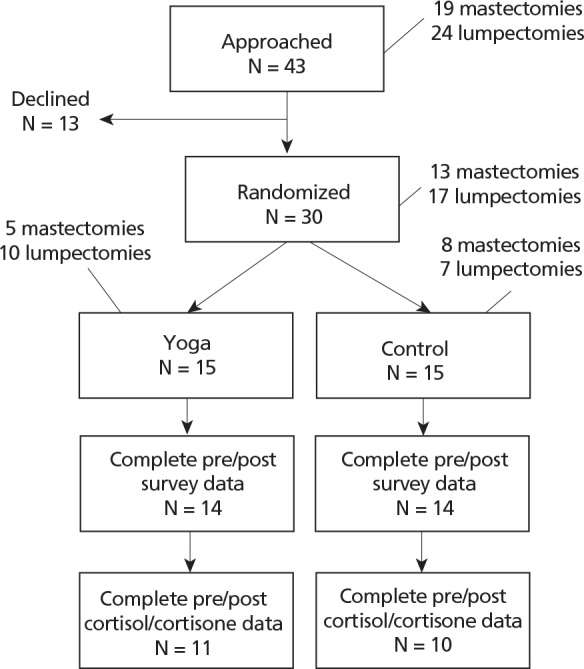
For recruitment, 43 patients were approached over the course of 9 months (recruitment rate, 70%). Feasibility of the intervention was good, and adherence to protocol high, with 15 participants (100%) in the YG attending the first individual session and 13 (87%) attending all three individual yoga sessions (Figure 1). Six patients (40%) attended five or more of the recommended eight group sessions (median 3 classes), and 11 (73%) reported performing the home-based, DVD-guided exercises at least once weekly. One participant (7%) in each group dropped out of the study (Figure 2).
The groups were similar in baseline characteristics (Table 1) with the YG having a higher rate of lumpectomy vs mastectomy. Radiation was more common in the YG, but this is to be expected given the higher lumpectomy rate.
Table 1
Baseline Characteristics and the Subsequent Treatment Modalities
| Control (n = 15) | Yoga (n = 15) | |
|---|---|---|
| Age (y), mean (range) | 55 (40-73) | 58 (48-75) |
| Type of surgery, n (%) | ||
    Mastectomy Mastectomy | 8 (53) | 5 (33) |
    Lumpectomy Lumpectomy | 7 (47) | 10 (67) |
| Adjuvant therapy, n (%) | ||
    None None | 5 (33) | 1 (7) |
    Hormonal therapy only (Arimidex, Tamoxifen) Hormonal therapy only (Arimidex, Tamoxifen) | 2 (13) | 3 (20) |
    Radiation (± hormonal therapy) Radiation (± hormonal therapy) | 4 (27) | 7 (47) |
    Chemotherapy (± radiation or hormonal therapy) Chemotherapy (± radiation or hormonal therapy) | 4 (27) | 4 (27) |
Quality of Life and Mood
Certain aspects of QoL and mood improved significantly within both groups. The emotional well-being (FACT-B) QoL score increased by a median 2.5 points in the YG (P = .02) and by 4.5 points in the CG (P = .007). Tension-anxiety, depression-dejection, and confusion-bewilderment mood scores (POMS) also significantly improved within both groups (median improvements ranged from 0.4 to 0.9). There was no significant difference between the YG and CG with respect to preand postintervention, with the exception of social/family well-being (P = .045) where improvement was slightly higher for the CG (median improvement, 2.5) than the YG (median improvement, 0; Table 2).
Table 2
Changes in the Quality of Life (QoL), Mood, Fatigue, Stress, and Cortisol Levels
| Yoga | Control | Yoga vs Control | ||||
|---|---|---|---|---|---|---|
| Post-Pre median (IQR) | Pa | Post-Pre median (IQR) | Pa | Pb | ||
| QoL (FACT-B)c | ||||||
    Physical well-being Physical well-being | −1.5 (−7.0, 0.0) | .03d | −0.8 (−9.0, 1.0) | .14 | .69 | |
    Social/family well-being Social/family well-being | 0.0 (−2.0, 1.0) | .40 | 2.5 (0.0, 3.7) | .03d | .045d | |
    Emotional well-being Emotional well-being | 2.5 (0.0, 5.0) | .02d | 4.5 (1.0, 6.0) | .007d | .45 | |
    Functional well-being Functional well-being | 1.0 (−3.0, 3.0) | .98 | −0.5 (−1.0, 4.0) | .79 | .85 | |
    FACT-G: Total FACT-G: Total | 2.4 (−11.0, 7.0) | .92 | 3.5 (−2.0, 11.0) | .35 | .43 | |
    FACT-B: Additional concerns FACT-B: Additional concerns | 2.0 (0.0, 4.0) | .13 | 1.5 (−1.0, 5.0) | .08 | .91 | |
    FACT-B: Total FACT-B: Total | 3.9 (−11.0, 10.0) | .70 | 6.5 (−2.5, 12.0) | .12 | .49 | |
    FACT-B: Trial outcome index FACT-B: Trial outcome index | 2.5 (−8.0, 6.0) | .80 | −0.3 (−6.0, 4.0) | .74 | .85 | |
| Mood (POMS) | ||||||
    Tension-anxiety Tension-anxiety | −0.9 (−1.2, −0.3) | <.001d | −0.6 (−1.0, −0.3) | .007d | .43 | |
    Vigor-activity Vigor-activity | −0.3 (−1.0, 0.3) | .30 | −0.1 (−1.0, 0.3) | .53 | .65 | |
    Fatigue-inertia Fatigue-inertia | −0.4 (−1.0, 0.4) | .39 | −0.3 (−0.6, 0.0) | .38 | .87 | |
    Depression-dejection Depression-dejection | −0.4 (−0.6, 0.0) | .008d | −0.4 (−1.3, 0.0) | .03d | .98 | |
    Confusion-bewilderment Confusion-bewilderment | −0.8 (−1.6, −0.2) | <.001d | −0.8 (−1.2, −0.4) | .001d | .84 | |
    Anger-hostility Anger-hostility | −0.2 (−0.6, 0.0) | .04d | 0.1 (−0.7, 0.4) | .58 | .46 | |
    Overall Overall | −0.5 (−0.7, −0.1) | .002d | −0.4 (−0.8, 0.0) | .048d | .73 | |
| Fatigue (BFI)e | −0.1 (−0.8, 0.8) | .99 | −0.3 (−2.7, 0.7) | .45 | .49 | |
| Perceived Stress (PSS)e | −1.5 (−6.0, 0.0) | .03d | −1.5 (−7.0, 0.0) | .06 | .94 | |
| Cortisol, ng/dL | −10.0 (−39.0, 2.1) | .32 | −12.1 (−40.9, −4.2) | .02d | .55 | |
| Cortisone, ng/dL | −86.0 (−191.0, 63.0) | .32 | −74.5 (−323.0, 19.0) | .09 | .92 | |
Abbreviations: POMS, Profile of Mood States; Post, postintervention; Pre, preintervention.
Perceived Stress and Fatigue
Perceived stress level improved similarly in the YG (median improvement, 1.5; P = .03) and CG (median improvement, 1.5; P = .06). Fatigue level did not significantly change from pre- to postintervention (Table 2).
Cortisol and Cortisone
Cortisol and cortisone levels decreased from pre- to postintervention. Cortisol and cortisone levels changed by a median of 10.0 ng/dL (P = .32) and 86.0 ng/dL (P = .32), respectively, within the YG and by a median of 12.1 ng/dL (P = .02) and 74.5 ng/dL (P = .09), respectively, within the CG. There was no difference in the level of decrease between groups (P = .55 and P = .92, respectively; Table 2).
Yoga Ratings, Sessions, and Rated Effectiveness
There was no correlation between the total number of exercise sessions performed and outcome measures (data not shown). Feasibility and adherence was high, however, and the YP was rated as “very effective,” providing relaxation (85%), stress relief (69%), and reduction of muscle tension or general feeling of wellness (each 62%).
Limitations
Because this was a pilot study, our sample size was small, and it is possible that one might have seen different or more significant results with a larger sample. Given that the patients were recently diagnosed and all were undergoing treatment, the nonactive CG could potentially also have benefited from more rest. Asymptomatic patients possibly being enrolled could also have contributed to the somewhat unclear trends seen in these primary investigations. With regard to salivary cortisol, additional measures collected at specific times during the day and more than twice during the study could potentially provide clearer evidence of cortisol changes throughout the study. The YG had more patients with lumpectomy than the CG, which had more patients who underwent mastectomy. This may have minimized the potential benefit from yoga as patients with mastectomy had prolonged recovery and may have more potential benefit from YP.
DISCUSSION
This study sought to examine the feasibility of YP started at the time of breast cancer diagnosis and potential impact on QoL, mood, stress, fatigue, and cortisol levels. Recruitment for the study was fairly quick with patients' interest in yoga relatively high (70%). Adherence with the study protocol was good, with a majority of participants attending all three individual yoga sessions (87%) as well as performing the home-based exercises (73%). Attendance at studio group-sessions was somewhat lower (40%), supporting previous research indicating that studio attendance may be much lower than home practice frequency.16 Overall recruitment and attendance records do, however, suggest feasibility of YP immediately after diagnosis.
Contrary to prediction, overall QoL did not significantly change from pre- to postintervention for either of the groups in this study. The emotional well-being sub-scale significantly improved within both groups but with no significant difference between groups. Other significant findings suggest that the CG improved in social well-being, and the YG worsened in physical well-being.
These results contradict findings from other studies of yoga vs waitlist groups in breast cancer survivors where improved QoL16 or a protective effect for social well-being8,17,18 have been found in the YG. Patients not receiving chemotherapy have also demonstrated significant improvement in emotional, social, spiritual, and overall QoL, and adherence has been positively associated with physical well-being and negatively associated with fatigue and distressed mood.8 One small, randomized controlled study with a yoga intervention in 18 patients with more advanced breast cancer (stages II-IV) nevertheless found no improvement in QoL.19
Our study differs significantly from the above studies in that recruitment was started at the time of breast cancer diagnosis. This is a particularly challenging time for patients, with significant emotional turmoil and impaired QoL.20 The improved emotional well-being seen across groups could potentially be a reflection of returning to baseline following the initial turmoil of diagnosis. The decrease in the physical well-being observed in our study might be secondary to treatments received including breast irradiation, but it remains unclear why this negative change was seen only in the YG, especially given the minimal side effects reported by the participants and high satisfaction reported with the intervention.
Significant improvements were seen in overall mood and multiple mood domains (tension-anxiety, depression-dejection, confusion-bewilderment, and anger hostility) across both groups with no significant between-group difference. Again, these findings are in contrast with other studies assessing similar outcomes and showing significant improvements in mood following yoga intervention.18,21 A possible explanation for these contradicting findings could be the fact that our participants were recruited immediately following diagnosis when patients are still attempting to adjust to the emotional turmoil of a new cancer diagnosis. It is possible that the passage of time and reassurance that the cancer is being treated could have led to significant improvement in QoL and mood well beyond a potential positive effect from a yoga intervention in this study.
Cancer diagnoses and subsequent treatments generally involve significant stressor exposure and persistent levels of fatigue. As with QoL and mood, our findings showed significant improvements in perceived stress levels for both groups, and again, these findings are contrary to existing research showing yoga interventions to be associated with improved stress levels compared with control groups. One of the most common symptoms reported by breast cancer survivors is fatigue, and it has been estimated that as many as 33% of these patients experience persistent fatigue.6 Even though a few well-conducted randomized studies have shown yoga to be associated with decreased levels of fatigue following breast cancer treatments,7 fatigue levels did not change for either group in the current study.
Cortisol level decreased from the initial measure to postintervention in both groups, although more significantly in the CG. Previous studies show contradicting findings in this area following yoga intervention, either not finding any change in cortisol slope,19 or finding significant improvement in cortisol levels for the postintervention YG.18
Studies examining the impact of yoga interventions in breast cancer survivors have examined a number of psychosocial factors, mainly through random recruitment. Studies targeting patients with specific symptoms, or at a very early stage in the course of illness, are rare, however. This could potentially explain how conflicting results may occur.
Results from this pilot study did not indicate clear benefits for patients undergoing YP immediately postdiagnosis. It is possible that during this period patients may be feeling overwhelmed, and the shock of the new breast cancer diagnosis may prevent them from truly benefiting from interventions. Improvements were found in emotional well-being, anxiety, depression, and levels of confusion in both groups, however, and breast cancer patients could potentially experience improvement in QoL, mood, and levels of perceived stress following treatment completion regardless of the interventions implemented. Study results show that the feasibility of YP immediately after breast cancer diagnosis was good, and adherence to individual sessions was very high. Participants pointed to relaxation as the most effective aspect of the intervention as well, indicating that YP immediately postdiagnosis may be most beneficial if individualized and if it included relaxation (eg, breathing) components. Given the novelty of this study, as well as the sample size and pilot study factors, further research is clearly warranted.
When developing future studies, in addition to increasing the sample size, we would consider offering more flexibility for participation in yoga programs immediately postdiagnosis, potentially through home-based interventions such as DVD or interactive ehealth-type practice rather than mandatory classes. Targeting patients with higher levels of symptoms such as stress, distress, or fatigue prior to the intervention may also increase the likelihood of detecting more substantial intervention benefit.
Acknowledgment
We sincerely thank Lace Up Against Breast Cancer (LUABC) and the Ralph Stump and Raedene Stump Foundation for providing the funding support for this study. We thank Ms Gladdie Hebl from Mayo Clinic Grant and Publication Support Services for her editorial assistance and Ms Hilary E. Blair in the Immunochemical Core Laboratory for assistance with the cortisol assays. We appreciate the data entry support by Mr David Hafferty.
Contributor Information
Sandhya Pruthi, Sandhya Pruthi, MD, and Daniela L. Stan, MD, are consultants, Division of General Internal Medicine, United States.
Daniela L Stan, Sandhya Pruthi, MD, and Daniela L. Stan, MD, are consultants, Division of General Internal Medicine, United States.
Sarah M Jenkins, Sarah M. Jenkins is a statistician and Marianne Huebner, PhD, is a research consultant, Division of Biomedical Statistics and Informatics, United States.
Marianne Huebner, Sarah M. Jenkins is a statistician and Marianne Huebner, PhD, is a research consultant, Division of Biomedical Statistics and Informatics, United States.
Beth A Borg, Beth A. Borg, RN, MHA, is an administrator and Barbara S. Thomley is a complementary and integrative medicine coordinator, Division of General Internal Medicine, United States.
Barbara S Thomley, Beth A. Borg, RN, MHA, is an administrator and Barbara S. Thomley is a complementary and integrative medicine coordinator, Division of General Internal Medicine, United States.
Susanne M Cutshall, Susanne M. Cutshall, MS, RN, CNS, is an integrative health specialist, Department of Surgery, United States.
Ravinder Singh, Ravinder Singh, PhD, is a consultant, Department of Laboratory Medicine and Pathology, United States.
Sadhna Kohli, Sadhna Kohli, PhD, is an associate consultant, Oncology Research, United States.
Judy C Boughey, Judy C. Boughey, MD, is a consultant, Division of General Surgery, and Valerie Lemaine, MD, MPH, is a senior associate consultant, Division of Plastic Surgery, Department of Surgery, all at Mayo Clinic, Rochester, Minnesota, United States.
Valerie Lemaine, Judy C. Boughey, MD, is a consultant, Division of General Surgery, and Valerie Lemaine, MD, MPH, is a senior associate consultant, Division of Plastic Surgery, Department of Surgery, all at Mayo Clinic, Rochester, Minnesota, United States.
Lise Solberg Nes, Lise Solberg Nes, PhD, is a psychologist in the Department of Medicine, University of Minnesota, Minneapolis, United States.
REFERENCES
Articles from Global Advances in Health and Medicine are provided here courtesy of SAGE Publications
Full text links
Read article at publisher's site: https://doi.org/10.7453/gahmj.2012.1.5.010
Read article for free, from open access legal sources, via Unpaywall:
https://europepmc.org/articles/pmc4890104?pdf=render
Citations & impact
Impact metrics
Citations of article over time
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.7453/gahmj.2012.1.5.010
Article citations
Exercise interventions for adults with cancer receiving radiation therapy alone.
Cochrane Database Syst Rev, 3:CD013448, 13 Mar 2023
Cited by: 8 articles | PMID: 36912791 | PMCID: PMC10010758
Review Free full text in Europe PMC
Physical Activity and Health-Related Quality of Life in Women With Breast Cancer: A Meta-Analysis.
JNCI Cancer Spectr, 6(6):pkac072, 01 Nov 2022
Cited by: 18 articles | PMID: 36474321 | PMCID: PMC9727071
Review Free full text in Europe PMC
A systematic review and meta-analysis of the effects of muscle relaxation training vs. conventional nursing on the depression, anxiety and life quality of patients with breast cancer.
Transl Cancer Res, 11(3):548-558, 01 Mar 2022
Cited by: 1 article | PMID: 35402172 | PMCID: PMC8990220
Meta-Analysis of Randomized Controlled Trials on Yoga, Psychosocial, and Mindfulness-Based Interventions for Cancer-Related Fatigue: What Intervention Characteristics Are Related to Higher Efficacy?
Cancers (Basel), 14(8):2016, 15 Apr 2022
Cited by: 13 articles | PMID: 35454922 | PMCID: PMC9032769
Review Free full text in Europe PMC
Yoga Therapy During Chemotherapy for Early-Stage and Locally Advanced Breast Cancer.
Integr Cancer Ther, 21:15347354221137285, 01 Jan 2022
Cited by: 5 articles | PMID: 36412916 | PMCID: PMC9706042
Go to all (13) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Randomized, controlled trial of yoga in women with breast cancer undergoing radiotherapy.
J Clin Oncol, 32(10):1058-1065, 03 Mar 2014
Cited by: 105 articles | PMID: 24590636 | PMCID: PMC3965260
Effects of a tailor-made yoga program on upper limb function and sleep quality in women with breast cancer: A pilot randomized controlled trial.
Heliyon, 10(16):e35883, 09 Aug 2024
Cited by: 0 articles | PMID: 39253212 | PMCID: PMC11382167
2013 SYR Accepted Poster Abstracts.
Int J Yoga Therap, 23 Suppl:32-53, 01 Jan 2013
Cited by: 1 article | PMID: 24176784
Review
Home-based multidimensional survivorship programmes for breast cancer survivors.
Cochrane Database Syst Rev, 8:CD011152, 24 Aug 2017
Cited by: 40 articles | PMID: 28836379 | PMCID: PMC6483678
Review Free full text in Europe PMC