Abstract
Free full text

Case Report
Weston-Hurst syndrome: a rare fulminant form of acute disseminated encephalomyelitis (ADEM)
Abstract
A 25-year-old Pakistani woman presented to the emergency department with a 2-day history of rapidly progressive tetraplegia followed by sudden loss of consciousness. This was preceded by an upper respiratory tract infection. On examination, she was deeply comatose with a GCS of 3/15 and intact brainstem reflexes. She was in respiratory distress, and an endotracheal tube had been passed. She had flaccid quadriplegia with depressed deep tendon reflexes and upgoing plantar response. Her MRI brain with contrast showed extensive brainstem involvement with haemorrhagic foci along with signal changes in the corpus callosum. The patient was put on a respirator. She was given IV methyl prednisolone, and later on 5 sessions of plasmapheresis were performed. After 3 months, the patient gradually recovered and started communicating. Her motor power had improved to 2/5 in her arms and 1/5 in the lower extremities. She was then discharged for further rehabilitation at home.
Background
Acute haemorrhagic leucoencephalitis (AHLE), Weston-Hurst syndrome, or Hurst disease, is a rare fulminant and fatal demyelinating disease of the central nervous system. It is considered to be a rapidly progressive form of either acute disseminated encephalomyelitis (ADEM) or a variant of tumefactive multiple sclerosis. Like ADEM, it is thought to be a post-infectious disorder. From the first case described by Hurst in August 1941 to the last case in the medical literature published in February 2016, the total number of reported cases still remains under 100 in 75 years; with a dismal prognosis, very high reported mortality and little means of diagnosis before the patient eventually succumbs to the disease. This case is unique in a way that despite the hyper-acute onset and aggressive presentation, the patient still survived and is slowly recovering. We propose that although Hurst disease is usually fatal, prompt recognition and aggressive management can improve chances of survival.
Case presentation
A 25-year-old Pakistani woman presented to the emergency department with a 2-day history of rapidly progressive weakness of all four extremities. Within a few hours, the lady was in a bedfast state. This weakness was associated with dysesthesias. This ictus was preceded by an upper respiratory tract infection 2 weeks back. There was no history of sphincter involvement, headache, seizures or visual impairment. One day before presentation, she had sudden loss of consciousness. There was no past history of hypertension, cardiac disease, stroke or transient ischaemic attacks. She was a non-smoker with no history of substance abuse. The family history was non-contributory.
On physical examination, she was a young lady deeply comatose with a GCS of 3/15. The patient had a regular pulse of 110 bpm. Her blood pressure was 90/60 mm Hg, and oral temperature was 98.6°F. She was in respiratory distress, and an endotracheal tube had been passed in the emergency unit to secure her airway. She was immediately shifted to the intensive care unit for assisted ventilation. Her brainstem reflexes were intact. The cranial nerves were intact and symmetric. She had flaccid quadriplegia with depressed deep tendon reflexes and bilateral positive Babinski's sign. Signs of meningeal irritation were absent. Her abdomen was soft and non-tender. There was no clinical evidence of organomegaly or ascites. Bowel sounds were audible. The patient's precordial examination revealed normal heart sounds. Auscultation of the lung fields revealed equal air entry on both sides.
Investigations
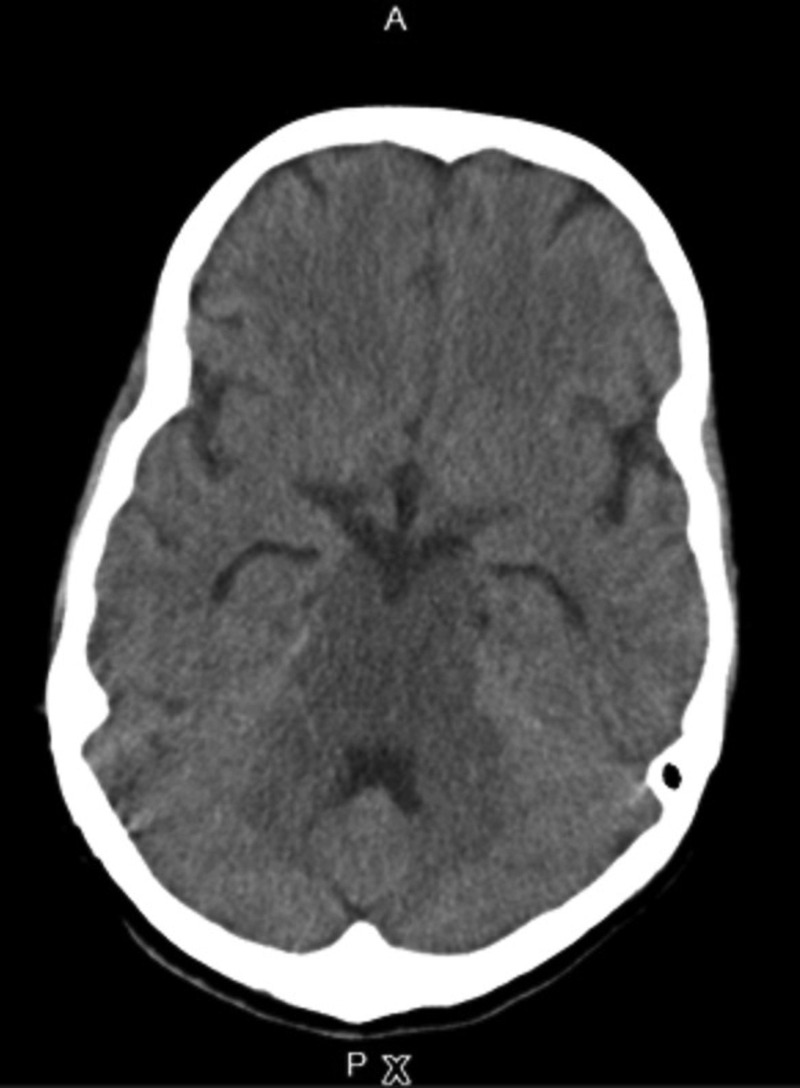
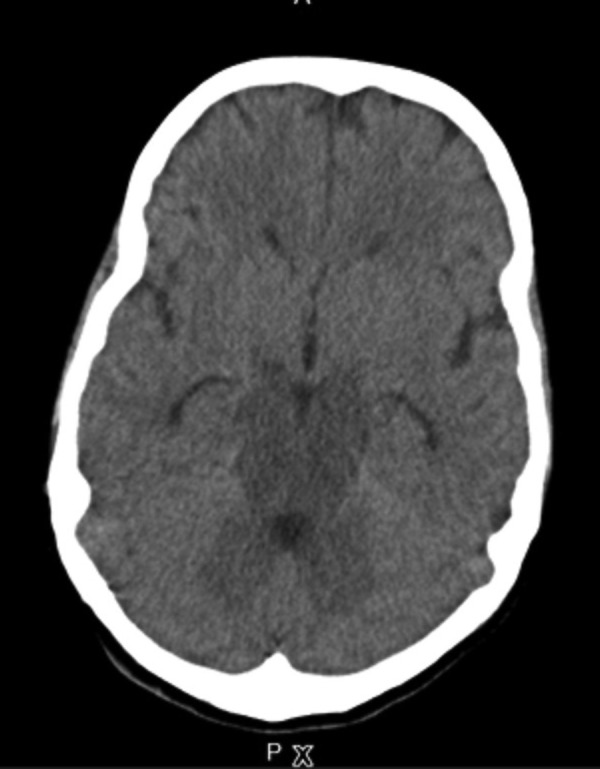
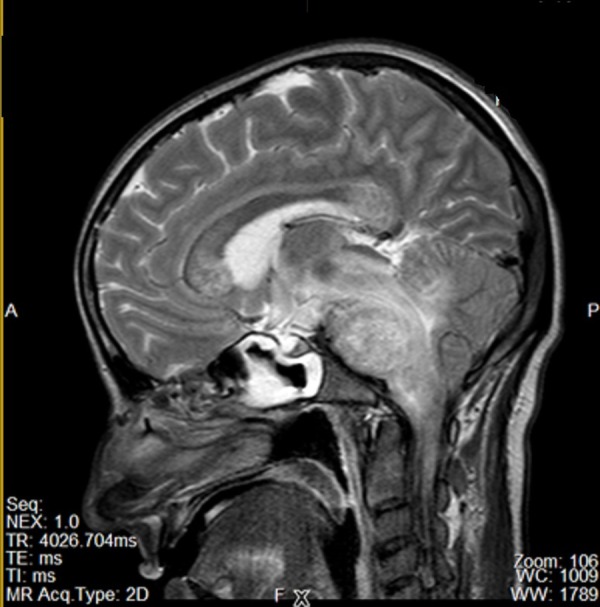
The laboratory analysis demonstrated a normal complete blood cell count and erythrocyte sedimentation rate. Her liver function tests, renal function tests, blood sugar and electrolytes were normal. Her chest X-ray, ECG and echocardiography were unrevealing. The lipid profile was also normal. Antinuclear antibody (ANA) was negative, and hepatitis B and C serology were nonreactive. Non-contrast-enhanced CT brain revealed hypodense signals throughout the brainstem (figures 1 and and2).2). Her MRI brain with contrast showed extensive brainstem involvement along with signal changes in the corpus callosum (figures 33–5). Haemorrhagic foci were also noted. There was no significant post-contrast enhancement. Cerebrospinal fluid (CSF) analysis showed mildly raised proteins (65 mg/dL) with normal glucose and cell count. CSF oligoclonal bands and herpes simplex virus PCR were negative. Her EEG consisted of a low voltage record with no discernable wave form and no epileptic discharges, suggestive of diffuse cortical dysfunction. Viral serologies for HSV and EBV were negative, whereas influenza serology did not indicate recent infection.
Differential diagnosis
The patient's presentation led to differential considerations of stroke in young, cerebral abscess, viral encephalitis, acute pyogenic meningitis or acute disseminated encephalomyelitis (ADEM). Her MRI brain was consistent with Weston-Hurst syndrome, a rapidly progressive and fulminant form of ADEM. Cerebral abscess was not confirmed. Her laboratory work-up also did not support the other differentials. ECG, ECHO, ANA and lipid profile did not identify any possible risk factors for stroke in young. CSF R/E was not consistent with meningitis. CSF herpes PCR was also negative, almost ruling out HSV encephalitis. She was then managed accordingly.
Treatment
The patient was put on a respirator. Her vitals were constantly monitored. She was given IV methyl prednisolone 1 g per day for 5 days, fluids, mannitol and antibiotics. Physiotherapy and nursing care were continued. Her GCS improved to 5/15. On account of persistent respiratory failure, poor GCS and failure to wean off, tracheostomy was done on the 7th day of ICU admission, and plasmapheresis was initiated. Five sessions were performed on alternate day with 2 L plasma removed per session. The patient's GCS improved to 11/15 after 1 month. Her tracheostomy was downsized, and she was successfully weaned off ventilatory support after another 15 days. She was still quadriplegic and was shifted to the high dependency unit for further care. Her tracheosotomy tube was removed after 2 weeks. Aggressive rehabilitation continued.
Outcome and follow-up
After 3 months of hospitalisation, the patient recovered to the extent that she started communicating with eye gestures and verbal sounds. She was tolerating small semisolid oral feeds and was breathing on her own. Her motor power had improved to 2/5 in her arms and 1/5 in the lower extremities. She was then discharged for home nursing care and rehabilitation.
Discussion
Acute haemorrhagic leucoencephalitis (AHLE), Weston-Hurst syndrome, or Hurst disease, is a rare fulminant and fatal demyelinating disease of the central nervous system.1 2 It is considered as a rapidly progressive form of ADEM by some while others label it as a variant of tumefactive multiple sclerosis.1 Like ADEM, it is thought to be a post-infectious disorder with an underlying immune aetiology. Infections like viruses and even mycoplasma pneumoniae have been implicated in various case reports.3–5 However, the true aetiopathogenesis is still unknown and elusive, and almost half cases have no such prior history.
From the first case described by Hurst in August 1941 to the last case in the medical literature published in February 2016, the total number of reported cases still remains under 100 in 75 years.5 6 Though it is more common in young adults, like ADEM, cases have been reported in the elderly as well.7 Both genders are equally affected. The hallmark features are rapid progression, dismal prognosis and high mortality with most patients dying within 2–4 days of disease onset.5 7 The presentation is variable with fever, altered mentation, headache, nausea, vomiting, seizures and coma. Sometimes, the patient can present with status epilepticus.8
Autopsy findings have revealed haemorrhages in the white matter, brain oedema and myelin destruction grossly. There is only one case in the literature as yet that denotes involvement of the spinal cord.9 On microscopy, it is characterised by fibrinoid venous necrosis, neutrophilic debris, haemorrhages and demyelination.7 Neuroimaging with MRI brain is the gold-standard diagnostic modality. Although histopathology is definitive, some call its diagnosis a ‘neuropathological’ one. MRI brain demonstrates large patches of white matter involvement with oedema, mass effect and haemorrhages. Sometimes, changes are seen in the basal ganglia and thalami as well.9–11
Hurst disease is associated with a very poor prognosis. The disease has an abrupt natural course.12 In 1973, Gozytoni reported three cases of AHLE. One of these patients expired within 30 hours of hospitalisation. The disease usually results in mortality within 2–4 days.2 The treatment involves early diagnosis, aggressive supportive measures, such as management of cerebral oedema and immunomodulatory therapy like corticosteroids and plasmapheresis.13 If medical therapy fails in resolving raised intracranial pressure, craniotomy may be considered.
Some patients, after an initial favourable response to steroids, have been seen to develop new deficits with more lesions appearing on subsequent scans, eventually leading to brain herniation and death.7 Aggressive and prompt treatment is warranted in all cases to slow down the course of the disease. This case is one such example where aggressive and early management led to the eventual survival of the patient. She is still in a partially dependent state, but she is recovering slowly and steadily.
Footnotes
Contributors: All the authors contributed equally to this work. All the authors meet the criteria for authorship as established by ICMJE. Conception or design of the work- SN, MB, SA, AZN. Data collection- SN, MB, SA, AZN. Drafting the article- SN, MB, SA, AZN. Critical revision of the article- SN, MB, SA, AZN. Final approval of the version to be published-SN, MB, SA, AZN.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
Articles from BMJ Case Reports are provided here courtesy of BMJ Publishing Group
Full text links
Read article at publisher's site: https://doi.org/10.1136/bcr-2016-217215
Read article for free, from open access legal sources, via Unpaywall:
https://europepmc.org/articles/pmc5073582?pdf=render
Citations & impact
Impact metrics
Article citations
Acute Hemorrhagic Leukoencephalitis in a Patient With Hepatitis B.
Cureus, 16(8):e67587, 23 Aug 2024
Cited by: 0 articles | PMID: 39310623 | PMCID: PMC11416751
CASE REPORT: Fulminant acute hemorrhagic Leukoencephalitis (AHLE): A rare and ruinous outcome with cerebral herniation (COVID-19).
eNeurologicalSci, 35:100499, 06 Apr 2024
Cited by: 0 articles | PMID: 38628435 | PMCID: PMC11019095
[Weston-Hurst syndrome. A case report and literature review].
Rev Med Inst Mex Seguro Soc, 61(5):695-701, 04 Sep 2023
Cited by: 0 articles | PMID: 37773190 | PMCID: PMC10599785
Review Free full text in Europe PMC
[Acute hemorrhagic leukoencephalopathy. Case report].
Rev Med Inst Mex Seguro Soc, 61(2):239-244, 01 Mar 2023
Cited by: 0 articles | PMID: 37205605 | PMCID: PMC10395982
Review Free full text in Europe PMC
Spectrum of Hemorrhagic Encephalitis in COVID-19 Patients: A Case Series and Review.
Diagnostics (Basel), 12(4):924, 07 Apr 2022
Cited by: 5 articles | PMID: 35453972 | PMCID: PMC9032293
Go to all (10) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Pseudotumoral lesion as a manifestation of acute hemorrhagic leukoencephalitis (Weston-Hurst syndrome).
Mult Scler Relat Disord, 46:102583, 13 Oct 2020
Cited by: 4 articles | PMID: 33296979
Weston-Hurst syndrome with acute hemorrhagic cerebellitis.
Clin Neurol Neurosurg, 173:118-119, 11 Aug 2018
Cited by: 8 articles | PMID: 30121019
Acute hemorrhagic leukoencephalitis with severe brainstem and spinal cord involvement: MRI features with neuropathological confirmation.
J Magn Reson Imaging, 33(4):957-961, 01 Apr 2011
Cited by: 18 articles | PMID: 21448963
[Acute Weston Hurst necrotizing hemorrhagic leukoencephalitis].
Rev Neurol (Paris), 152(12):748-751, 01 Dec 1996
Cited by: 6 articles | PMID: 9205699
Review