Abstract
Objective
Systematic review of possible long-term effects of sports-related concussion in retired athletes.Data sources
Ten electronic databases.Study selection
Original research; incidence, risk factors or causation related to long-term mental health or neurological problems; individuals who have suffered a concussion; retired athletes as the subjects and possible long-term sequelae defined as >10 years after the injury.Data extraction
Study population, exposure/outcome measures, clinical data, neurological examination findings, cognitive assessment, neuroimaging findings and neuropathology results. Risk of bias and level of evidence were evaluated by two authors.Results
Following review of 3819 studies, 47 met inclusion criteria. Some former athletes have depression and cognitive deficits later in life, and there is an association between these deficits and multiple prior concussions. Former athletes are not at increased risk for death by suicide (two studies). Former high school American football players do not appear to be at increased risk for later life neurodegenerative diseases (two studies). Some retired professional American football players may be at increased risk for diminishment in cognitive functioning or mild cognitive impairment (several studies), and neurodegenerative diseases (one study). Neuroimaging studies show modest evidence of macrostructural, microstructural, functional and neurochemical changes in some athletes.Conclusion
Multiple concussions appear to be a risk factor for cognitive impairment and mental health problems in some individuals. More research is needed to better understand the prevalence of chronic traumatic encephalopathy and other neurological conditions and diseases, and the extent to which they are related to concussions and/or repetitive neurotrauma sustained in sports.Free full text
A systematic review of potential long-term effects of sport-related concussion
Associated Data
Abstract
Objective
Systematic review of possible long-term effects of sports-related concussion in retired athletes.
Data sources
Ten electronic databases.
Study selection
Original research; incidence, risk factors or causation related to long-term mental health or neurological problems; individuals who have suffered a concussion; retired athletes as the subjects and possible long-term sequelae defined as >10 years after the injury.
Data extraction
Study population, exposure/outcome measures, clinical data, neurological examination findings, cognitive assessment, neuroimaging findings and neuropathology results. Risk of bias and level of evidence were evaluated by two authors.
Results
Following review of 3819 studies, 47 met inclusion criteria. Some former athletes have depression and cognitive deficits later in life, and there is an association between these deficits and multiple prior concussions. Former athletes are not at increased risk for death by suicide (two studies). Former high school American football players do not appear to be at increased risk for later life neurodegenerative diseases (two studies). Some retired professional American football players may be at increased risk for diminishment in cognitive functioning or mild cognitive impairment (several studies), and neurodegenerative diseases (one study). Neuroimaging studies show modest evidence of macrostructural, microstructural, functional and neurochemical changes in some athletes.
Conclusion
Multiple concussions appear to be a risk factor for cognitive impairment and mental health problems in some individuals. More research is needed to better understand the prevalence of chronic traumatic encephalopathy and other neurological conditions and diseases, and the extent to which they are related to concussions and/or repetitive neurotrauma sustained in sports.
Introduction
There is tremendous interest in understanding the possible long-term effects of concussions sustained during a career in sports. It has been believed for decades that repetitive neurotrauma sustained in boxing is associated with chronic brain damage in some former athletes. In case descriptions dating back to the 1920s, some long-career boxers have been described as having a neurological syndrome referred to as ‘punch drunk syndrome’,1 traumatic encephalopathy2 dementia pugilistica,3 chronic traumatic encephalopathy (CTE)4 and chronic progressive traumatic encephalopathy.5 In recent years, a number of studies have been conducted with former NFL players. There is emerging evidence that some retired NFL players have mild cognitive impairment,6 7 neuroimaging abnormalities8 9 and differences in brain metabolism10 disproportionate to their age. Autopsy cases of former professional football players have revealed diverse forms of neuropathology, including immunoreactivity for hyperphosphorylated tau (p-tau) in a specific pattern (eg, irregularly distributed in depths of cortical sulci) in which p-tau is not expected to be present through normal ageing or in association with frontotemporal dementia or Alzheimer’s disease.11 This article represents a systematic review of the existing literature on possible long-term effects of sport-related concussions, including risk for Alzheimer’s disease and CTE.
Methods
A systematic review was performed to address the question of long-term effects of sport-related concussion for the 5th International Consensus Conference on Concussion in Sport: ‘What is the current state of the scientific evidence about the prevalence, risk factors, and causation of possible long-term sequelae like CTE and other neurodegenerative diseases, with respect to sports concussion?’ Additional questions addressed included (i) what are the definition, clinical features and underlying pathophysiology (if any) of ‘subconcussive blows’ (ie, subconcussive impacts) and (ii) what have we learnt from the retired athlete population?’
Search terms and databases
Keywords were selected by agreement of all authors and then submitted to a librarian with expertise in systematic reviews who developed a draft MEDLINE search strategy. This was reviewed by a second expert health sciences librarian using the CADTH Peer Review Checklist for Search Strategies according to the PRESS 2015 Guideline Statement. The draft search strategy was revised based on suggestions from the PRESS review, and then tested to be sure known key studies were retrieved. The MEDLINE search (see online supplementary table 1) was adapted and translated for all other databases. The following 10 databases were searched: MEDLINE (Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R)), CINAHL Plus with Fulltext, EMBASE, PsycInfo, Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Scopus, Web of Science, PsycARTICLES and SPORTDiscus. The search was limited to English-language and peer-reviewed publications, but had no date restriction. The search was conducted 10–11 September 2016.
Study selection criteria and data extraction
Studies were included if they (i) were original research; (ii) evaluated the incidence/prevalence, risk factors or causation related to neurodegenerative disease; (iii) included individuals who have suffered a sport-related concussion; (iv) evaluated athletes and/or retired athletes as the study subjects and (v) evaluated possible long-term sequelae defined as >10 years after sports-related injury. Studies were excluded from this review if they were published in a language other than English, animal studies, review articles, case reports, book chapters, conference abstracts, editorials/commentaries/expert opinion, theses or dissertations.
Citations were independently screened by pairs of authors. A third reviewer adjudicated disagreements between authors. Following the initial abstract and title screening process, full-text articles were retrieved and data were extracted using a standardised method. Results were extracted by one author and reviewed by a second author to ensure accuracy and completeness.
Assessment of risk of bias and level of evidence
For each article that met inclusion criteria, risk of bias and strength of evidence were independently rated by two authors using the Downs and Black checklist.12 The level of evidence was assessed using the Oxford 2011 Level of Evidence13 criteria and rated by two authors.
Results
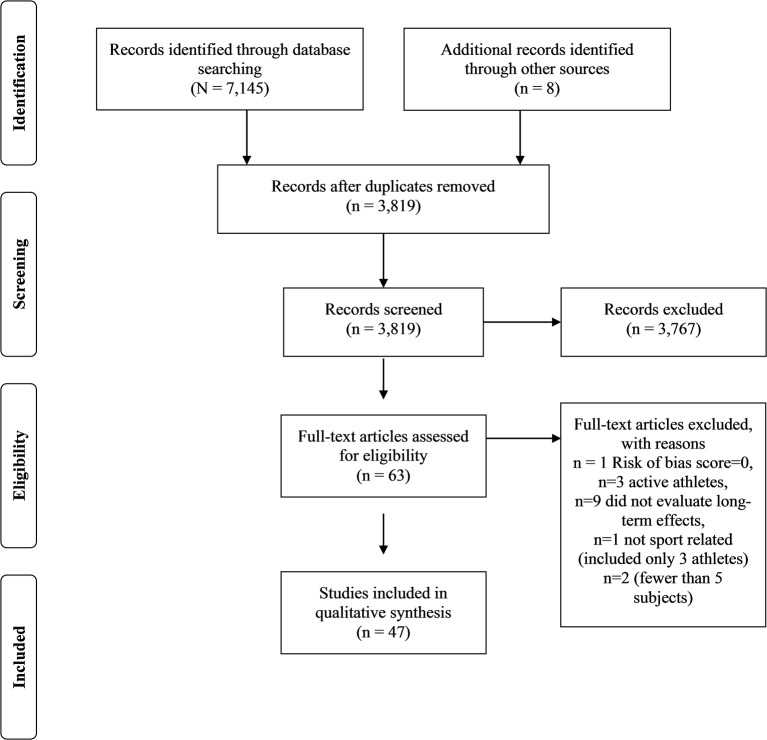
The database search identified 7145 articles (figure 1, note correction: in figure 1, the PRISMA diagram, Records excluded n = 3,756 PRISMA). After duplicates were removed, 3819 records were screened and a total of 47 were included in this review. Those articles are listed in table 1. Online supplementary table 2 presents a summary of the key findings from these studies. Online supplementary table 3 presents a review of the methodological quality and risk for bias of the 47 studies. The average methodological quality rating using the Downs and Black criteria for these 47 publications was 8.1.
Table 1
Studies identified through the search process
| Clinical studies | Imaging and combined imaging/clinical studies |
|---|---|
| Kelly et al74 | Hampshire et al32 |
| Lolekha et al38 | Small et al28 |
| Lehman et al41 | Koerte et al10 |
| Murelius et al34 | Lin et al17 |
| Kerr et al29 | Gardner et al22 |
| Didehbani et al35 | Multani et al27 |
| Seichepine et al75 | Wilde et al26 |
| Randolph et al7 | Strain et al24 |
| Vann Jones et al19 | Koerte, Huf et al21 |
| Kerr et al30 | Koerte et al18 |
| Kerr et al31 | Ford et al33 |
| Stamm et al36 | Hart et al8 |
| Hume et al37 | Goswami et al23 |
| Meehan et al20 | Casson et al62 |
| Montenigro et al16 | Pathology studies |
| Baron et al42 | Corsellis et al76 |
| Lehman et al43 | Roberts et al56 |
| Critchley 5 | McKee et al49 |
| Maudsley and Ferguson77 | Omalu et al50 |
| Savica et al44 | Hazrati et al51 |
| Roberts et al57 | McKee et al11 |
| Guskiewicz et al6 | Bieniek et al52 |
| Guskiewicz et al39 | Ling et al53 |
| Hinton et al70 | Koga et al55 |
Subconcussive head impacts
Interest has been expressed in the concept of ‘subconcussive blows’ (ie, subconcussive head impacts) as an indicator of repetitive neurotrauma. Subconcussive impacts are typically defined as involving the transfer of mechanical energy to the brain at enough force to injure axonal or neuronal integrity, but not be expressed in clinical symptoms.14 15 These impacts have been proposed as a separate variable from concussion history by some researchers. We reviewed five subconcussive impact studies that (i) defined the concept or (ii) quantified the criteria (ie, years of exposure, estimated number of impacts). These studies are discussed, in part, in the sections below. They either discussed the concept of subconcussive impacts or added the estimated number of subconcussive impacts to the athletes’ concussion history.16 The majority of subjects were American football athletes or soccer players. Most studies identified significant group-level differences between ‘high exposure’ and ‘low/no exposure’ athletes,10 17 18 although there were some studies that did not support the notion that repetitive subconcussive impacts have a measurable, detrimental effect.19 20 Some studies have drawn inferences about subconcussive impacts based solely on a person’s participation in certain contact or collision sports. For example, Meehan and colleagues20 surveyed >3702 college alumni between the ages of 40 and 70, 2121 of whom had no reported history of concussion. In those with no reported concussions (a proxy for studying subconcussive impacts), there were no differences in anxiety, depression, emotional dyscontrol, sleep disturbance or perceived cognitive functioning in those who participated in collision sports versus those who did not. There was greater use of alcohol in former collision sport athletes.
Neuroimaging
We reviewed 14 neuroimaging articles relating to the possible long-term sequelae of sports-related concussion. These included structural imaging, diffusion tensor imaging (DTI), magnetic resonance spectroscopy (MRS) and positron emission tomography (PET). The majority of subjects were American football athletes and soccer players. Most studies identified significant group-level differences in these imaging modalities; however, lack of standardisation in imaging acquisition and analysis limits the generalisability of the findings. The average methodological quality rating using the Downs and Black criteria for these publications was 7.4, and the average level of evidence was 4.0.
Structural imaging
A structural 3 T MRI study of 72 former American professional football players with cognitive and mental health symptoms revealed a higher rate of cavum septum pellucidum (CSP), greater length and greater ratio of CSP to septum length compared with 14 former non-contact athlete controls.21 The greater length of the CSP was also associated with decreased performance on a memory test and a test of word pronunciation. Gardner and colleagues measured CSP (1.5 and 3 T MRI) in 17 retired American professional football players presenting to a memory clinic with cognitive and mental health symptoms.22 Compared with matched controls from the memory clinic with no history of traumatic brain injury (TBI), CSP was more common in retired football players (94% vs 18%) and the length was also significantly greater.
Goswami and colleagues reported that football athletes with a history of concussion (n=19) had significant cortical thinning of the anterior temporal lobe and orbitofrontal cortex compared with controls (n=17).23 Koerte and colleagues identified decreased cortical thickness in former professional soccer players (n=15).10 (NOTE: Koerte citation 10 should be Koerte citation 18)Group-level analyses of cortical thickness revealed greater cortical thinning with increasing age in right inferolateral-parietal, temporal and occipital cortex, and this was associated with lower cognitive performance. Strain and colleagues found that older retired athletes with at least one remote history of concussion with loss of consciousness had significantly smaller bilateral hippocampal volumes and decreased memory performance.24
Diffusion tensor imaging
In a study of 37 amateur soccer players, a lifetime concussion history was not associated with changes in fractional anisotropy (FA) or cognitive performance.25 However, high-frequency soccer heading (>885 per year) was associated with lower memory scores and lower FA in three regions of interest in the temporo-occipital white matter. In a study of 10 boxers (8 retired, 2 active), there were no group differences in FA between the boxers and non-contact sport controls, although DTI metrics were associated with declarative memory and reaction time.26 Using whole-brain tract-based spatial statistics analysis, 18 retired professional football players were compared with 17 healthy controls.27 They found no differences in FA but did find increased axial diffusivity in the right hemisphere of retired players in the superior longitudinal fasciculus, corticospinal tract and anterior thalamic radiations, suggesting possible axonal degeneration in these tracts.
Magnetic resonance spectroscopy
Koerte and colleagues studied 11 former professional soccer players without a history of concussion compared with 14 age-matched controls.10 In the soccer players, a significant increase was observed in both choline, a membrane marker, and myo-inositol (ml), a marker of glial activation. There were no significant differences in neurocognitive testing between groups. Increased levels of choline and glutamate/glutamine were also found in five former professional male athletes with history of multiple concussions and multiple symptoms compared with control athletes with no history of brain trauma.17
Positron emission tomography
A PET study explored the use of 2-(1-{6-[(2-[F-18]fluoroethyl) (methyl)amino]−2 naphthyl} ethylidene) malononitrile (FDDNP) for measuring both tau and amyloid in living brains.28 Five former professional American football players with mood and cognitive problems were compared with five age, education and body mass-matched controls. FDDNP binding signals were higher in players versus controls in subcortical regions and amygdala. The authors noted that the study was limited by the small sample size and lack of pathological confirmation.
Cognitive functioning and mental health
We reviewed 24 articles relating to possible long-term cognitive and mental health problems associated with concussion. The average methodological quality rating using the Downs and Black criteria for these publications was 9.7, and the average level of evidence was 3.8. Some of these studies are cross-sectional surveys.7 20 29–31 Some in-person clinical assessment studies have been conducted with8 10 17 18 21–24 26–28 32 33 and without7 19 34–37 neuroimaging. There are also studies that begin with a survey and then have a follow-up in-person assessment.38 A number of cross-sectional studies have identified decrements on objective neuropsychological testing7 8 24 37 and subjectively experienced cognitive difficulties on self-report measures6 20 in former athletes. Some studies report a frequency–response relationship, with greater cognitive impairments in those with greater levels of exposure to head impacts or concussions.16 36 However, other studies have not found a frequency–response relationship when examining cognitive function.8 31 33 Guskiewicz and colleagures surveyed 2552 retired NFL players and found that 1.3% (n=33) reported a physician diagnosis of Alzheimer’s disease. Of the 758 who were aged ≥50, 2.9% (n=22) reported a physician diagnosis of mild cognitive impairment. Of the 641 former players who had a spouse or close relative complete a questionnaire, 12.0% (n=77) were identified as having significant memory problems. Former players with 3+ concussions during their playing career had a fivefold greater risk of mild cognitive impairment (MCI) diagnosis after age 50 compared with those with no prior concussions.6 Randolph and colleagues surveyed 513 retired NFL players aged ≥50 for whom their wives completed a questionnaire regarding memory. In this sample, 35.1% had a score on a scale completed by their spouses (AD8) that was suggestive of possible cognitive impairment.7 This is much higher than the 12.0% rate reported in the previous study,6 for unclear reasons. The rate of clinical diagnoses of MCI (vs survey screening) is unknown.
Regarding mental health, depression has been most frequently studied. Five studies report a frequency–response relationship between concussions or head impact exposure and depression symptom reporting.16 30 35 39 40 Didehbani and colleagues studied cognitively intact former NFL athletes and found greater depression symptoms compared with age and intelligence quotient (IQ)-matched subjects.35 In a sample of 797 former collegiate athletes (all sports), approximately 39% of whom reported one or more prior concussions, their rates of self-reported mental health and cognitive problems were as follows: depression=10.4%, anxiety=16.2%, alcohol dependence=5.8%, substance use=2.9% and cognitive problems=3.8%.30 This sample also completed the Patient Health Questionnaire-9 (PHQ-9) to screen for depression. The rate of screening positively for depression (ie, PHQ-9≥10) stratified by concussion history was as follows: 0=2.8%, 1=5.6%, 2=10.4% and 3+=8.9%.31 The rate of self-reported depression in retired NFL players (n=1044), stratified by concussion history, was as follows: 0=3.0%, 1–2=8.2%, 3–4=13.7%, 5–9=19.3% and 10+=26.8%.29
The link between soccer heading, cognitive functioning and psychological health is unclear. No association between cognitive function and length of career or position played was found in older (mean age=67 years) retired professional soccer players.19 Similarly, former professional soccer players who still play recreationally were found to have largely similar performance on a variety of cognitive assessments compared with matched non-contact sport athlete controls.18 In this study, however, the soccer players had a greater decrease in cortical thickness with age—and cortical thickness in parietal and occipital areas of the brain were negatively correlated with lifetime estimates of heading.
Five long-term effects cohort studies using medical record linkage or death certificates41–45 have been published, one after the cut-off date for this systematic review.45 The results of these studies are summarised in online supplementary table 1. Three studies of causes of death in former NFL players have been published.41–43 Two of these studies examined the death certificates of those who died between 1960 and 2007 (334 deaths from a cohort of 3439 former players). All cause and specific mortality rates (eg, cancer, cardiovascular disease, pulmonary disease and other health problems) were lower in former players than in men from the general population.42 43 Baron and colleagues reported that the rates of psychiatric illness and suicide were significantly lower in the former athletes than in men from the general population.42 They also reported that diseases of the nervous system and sense organs were somewhat higher than men in the general population, but the difference was not statistically significant. Of the 334 former players who had died, 12 (3.6%) had one of these latter diseases listed on his death certificate when it would have been expected, from population estimates, that the number should be 9.7 people (ie, 2.9%). There was no autopsy confirmation of the diseases listed on the death certificate and no analysis of genetic susceptibility (eg, apolipoprotein E). In a reanalysis of the same data set, Lehman and colleagues43 reported that the rates of Alzheimer’s disease and amyotrophic lateral sclerosis (ALS) were higher in former NFL football players compared with men in the general population. Of the 334 death certificates reviewed, the number of times neurodegenerative diseases were listed as an underlying or contributing cause of death was as follows: Alzheimer’s disease/dementia=7 (2.1%), Parkinson’s disease=3 (0.9%) and ALS=7 (2.1%). In two medical record linkage studies of former high school football players,44 45 the rates of dementia, mild cognitive impairment and parkinsonism did not differ in comparison to control subjects (see table 2).
Table 2
Cohort studies of former American football players using medical record linkage or death certificates
| Psychiatric illness | Suicide | Alzheimer’s disease or dementia | Mild cognitive impairment | Parkinson’s disease/ parkinsonism | ALS | Any neurodegenerative disease | ||||
| First author/ref | Sample | Sample size | Years played | % (n) | % (n) | % (n) | % (n) | % (n) | % (n) | % (n) |
| Janssen 45 | Former American varsity high school football | 296 | 1956–1970 | NR | NR | 0.7 (2) | 1.7 (5) | 1.0 (3) | 0 (0) | 3 (10) |
| Former high school athlete controls* | 190 | 1956–1970 | NR | NR | 0.5 (1) | 2.1 (4) | 1.6 (3) | 0 (0) | 4 (8) | |
| Savica 44 | High school football | 438 | 1946–1956 | NR | NR | 3.0 (13) | NR | 2.3 (10) | 0.5 (2) | 5.7 (25) |
| Non-athlete controls† | 140 | – | NR | NR | 1.4 (2) | NR | 3.6 (5) | 0.7 (1) | 5.7 (8) | |
| Baron 42 | Deceased former NFL players | 334 | 1959–1988 | 1.2 (4) | 2.7 (9) | NR | NR | NR | NR | 3.6 (12)‡ |
| Men in general population | – | – | 3.5 (11.7) | 6.5 (21.8) | NR | NR | NR | NR | 2.9 (9.7) | |
| Lehman 43 | Deceased former NFL players | 334 | 1959–1988 | NR | NR | 2.1 (7) | NR | 0.9 (3) | 2.1 (7) | 5.1 (17) |
| Men in general population | – | – | NR | NR | NR | NR | NR | NR | NR | |
| Lehman 41 | Deceased former NFL players | 537 | 1959–1988 | NR | 2.2 (12) | NR | NR | NR | NR | NR |
| Men in general population | – | – | NR | 4.8 (25.6) | NR | NR | NR | NR | NR |
The two studies of high school football players are medical record linkage studies and illustrate the rates of diagnoses present in those records. The three studies of former NFL players are based on reviewing death certificates and address underlying or contributing causes of death. There were 3439 former NFL players, of whom 334 died between 1960 and 200742 43, and 537 died between 1960 and 2013.41 The differing methodologies do not allow a direct comparison between high school and former NFL athletes. *Controls were non-football-playing male varsity athletes, such as swimmers, wrestlers and basketball players.
†Controls were non-football-playing male students in the glee club, band or choir.
‡Defined by Baron et al as any disease of nervous system and sense organs. From Baron et al
42: mental, psychoneurotic and personality disorders=4 (expected=11.7; standardised mortality ratio (SMR)=0.34, 95% CI 0.09 to 0.87). Intentional self-harm=9 (expected=21.8, SMR=0.41, 95% CI 0.19 to 0.78). Diseases of the nervous system and sense organs=12 (expected=9.7; SMR=1.24, 95%
CI 0.19 to 0.78). Diseases of the nervous system and sense organs=12 (expected=9.7; SMR=1.24, 95% CI 0.64 to 2.16). For Lehman et al
43, the number of times neurodegenerative diseases were listed as an underlying or contributing cause of death is reported. From Lehman et al
41 : suicide=12 (expected=25.6, SMR=0.47, 95%
CI 0.64 to 2.16). For Lehman et al
43, the number of times neurodegenerative diseases were listed as an underlying or contributing cause of death is reported. From Lehman et al
41 : suicide=12 (expected=25.6, SMR=0.47, 95% CI 0.24 to 0.82).
CI 0.24 to 0.82).
ALS, amyotrophic lateral sclerosis; n, frequency; NR, not report.
Neuropathology
Autopsy studies have revealed multiple forms of neuropathology, both macroscopic and microscopic, in former contact and collision sport athletes. Macroscopic findings include (i) frontal and temporal atrophy, thinning of the hypothalamic floor, shrinkage of the mammillary bodies, pallor of the substantia nigra, hippocampal sclerosis and reduction in brain mass; (ii) enlarged ventricles and (iii) CSP with or without septal fenestrations.46–48 Microscopic features include (i) localised neuronal and glial accumulations of p-tau with varying microscopic morphologies, involving perivascular areas of the cerebral cortex and sulcal depths, and with a preference for neurons within superficial cortical laminae; (ii) multifocal axonal varicosities involving deep cortex and subcortical white matter; (iii) variable and often absent Aβ deposits and (iv) TDP-43-positive inclusions and neurites.46–48
We reviewed nine neuropathology studies that included five or more subjects. These reports focused on the pathology associated with CTE. The average methodological quality rating using the Downs and Black criteria for these publications was 5.2, and the average level of evidence was 4.2. In 2010, McKee et al described the neuropathology of 12 former athletes (7 football players, 3 boxers and 1 hockey player) whose brains and spinal cords had been donated to the Center for the Study of Traumatic Encephalopathy at Boston University School of Medicine.49 Subjects ranged in age from 42 to 85 years (average age 65) and all had a history of cognitive and behavioural changes associated with CTE. Three of the athletes also had signs and symptoms of motor neuron disease (MND). P-tau immunoreactivity in neurons and astroglia in the depth of sulci was noted in all subjects. Seven of the nine cases without MND also had TDP-43 immunoreactive inclusions.
In 2011, Omalu et al reported autopsy findings in 17 athletes (14 professional, 3 high school).50 Selected brain samples or whole-brain specimens were examined by routine histopathology, special stains and immunohistochemistry. CTE pathology was based on the presence of topographically distributed neurofibrillary tangles and neuritic threads, with or without amyloid plaques, and the absence of features indicative of another tauopathy. The authors found CTE changes in 10 of the 14 professional athletes and 1 of 3 high school athletes (71% overall). The authors noted four histological phenotypes, based on relative abundance of p-tau in cerebral cortex, subcortical structures and brainstem, and presence or absence of diffuse β-amyloid plaques.
In 2013, McKee et al described the neuropathology in 85 subjects with a history of mild TBI, 64 of which were former athletes.11 The brains of 18 cognitively intact controls with no history of repetitive mild TBI were also examined. The diagnosis of CTE was based on p-tau immunoreactivity around small blood vessels at the depths of cortical sulci, clusters of p-tau-positive subpial and periventricular astrocytes, and neurofibrillary tangles in the superficial layers of the cerebral cortex—this pathology was identified in 80% of the cases and none of the control subjects. Other abnormalities included TDP-43 immunoreactivity (85% of cases) and comorbid neurodegenerative disease including MND (12%), Parkinson’s or Lewy body disease (16%), Alzheimer’s disease (11%) and frontotemporal lobar degeneration (6%). A neuropathological staging system for CTE (stages I–IV) was also proposed.
In 2013, Hazrati described a series of six retired professional Canadian football players whose ages ranged from 61 to 87 years.51 The subjects had a history of multiple concussions and medically or family member documented cognitive, behavioural and/or motor symptoms. Three of the six subjects had neuropathological findings consistent with CTE. The other three subjects were diagnosed with Alzheimer’s disease, Parkinson’s disease and MND. In addition, the CTE cases showed comorbid pathology of Alzheimer’s disease, vascular disease and cancer.
Bieniek and colleagues studied a range of neurodegenerative disease cases along with a small number of normal controls.52 Review of available medical records from 1721 men identified 66 cases with a history of contacts sports. The authors found that 21 of the 66 cases (32%) had cortical p-tau staining consistent with CTE. None of the 162 control brains, and none of the 33 cases with a history of a single TBI, had CTE pathology. This study was conducted using a neurodegenerative disease brain bank, so there were comorbid neurodegenerative conditions (Alzheimer’s disease, Lewy body disease, frontotemporal lobar degeneration) in 20 of the 21 cases with CTE.
Ling and colleagues53 conducted a large-scale postmortem study of CTE in the UK using the McKee et al11 criteria. They screened 268 cases and found histological evidence of CTE in 32 (11.9%), including cases of women with this pathology. The mean age at death was 81 years. The majority of the positive cases met neuropathological criteria for other neurodegenerative diseases and had prior exposure to at least one TBI.
Until 2015, there was no consensus regarding the neuropathological criteria for the diagnosis of CTE. The National Institutes of Neurological Disease and Stroke and National Institute of Biomedical Imaging and Bioengineering (NINDS/NIBIB) funded a panel of neuropathologists to establish criteria. The consensus panel defined the pathognomonic lesion of CTE as an accumulation of p-tau in neurons and astroglia distributed around small blood vessels at the depths of cortical sulci and in an irregular pattern.54 In addition to p-tau-related supportive criteria, TDP-43 immunoreactive inclusions and macroscopic features (ventricular enlargement and CSP) were identified as supportive of CTE.
Koga et al55 examined 139 cases of multiple system atrophy (MSA) using NINDS/NIBIB CTE criteria. CTE pathology was found in 8 (6%) of the 139 MSA cases, all of which were male, and 4 with a history of contact sports. The authors also noted that 7.2% were identified as having ageing-related tau astrogliopathy (ARTAG), a pathology that should be differentiated from CTE pathology. The authors speculated that falls secondary to the movement disorder may cause CTE pathology.
Neurological and mental health features of CTE
Prior to 2005, slurred and dysarthric speech, gait problems, parkinsonism and cognitive impairment (including dementia) were considered common clinical features of CTE.56–58 Although historical case descriptions sometimes included histories of mental health problems and severe substance abuse, these were not considered core features of the condition. The largest study examining the clinical features of chronic brain damage in living subjects was published as a monograph by Roberts in 1969.57 From a list of 16 781 retired boxers, Roberts selected an age-stratified random sample of 250; he was able to locate and clinically examine 224 of these men.57 He concluded that 17% had the syndrome (11% had a mild form of the syndrome and 6% had severe problems). For boxers over the age of 50 who had ≥150 fights, 50% had the syndrome compared with 7% with <50 fights. In recent years, the clinical features of CTE have been greatly expanded to include many psychosocial problems, depression, anxiety, anger and other health problems.11 46 48 50 More research is needed to determine the extent to which those problems are associated with the neuropathology of CTE. Proposed criteria for diagnosing CTE have been published by Jordan,59 Victoroff60 and Montenigro and colleagues.61 At present, however, there are no agreed upon or validated clinical criteria for CTE, thus there is no accepted method for diagnosing CTE in a living person.
781 retired boxers, Roberts selected an age-stratified random sample of 250; he was able to locate and clinically examine 224 of these men.57 He concluded that 17% had the syndrome (11% had a mild form of the syndrome and 6% had severe problems). For boxers over the age of 50 who had ≥150 fights, 50% had the syndrome compared with 7% with <50 fights. In recent years, the clinical features of CTE have been greatly expanded to include many psychosocial problems, depression, anxiety, anger and other health problems.11 46 48 50 More research is needed to determine the extent to which those problems are associated with the neuropathology of CTE. Proposed criteria for diagnosing CTE have been published by Jordan,59 Victoroff60 and Montenigro and colleagues.61 At present, however, there are no agreed upon or validated clinical criteria for CTE, thus there is no accepted method for diagnosing CTE in a living person.
Discussion
This systematic review identified 47 studies relating to possible long-term problems with brain health associated with sport-related concussion (see table 1 and online supplementary tables 2 and 3). The methods used included clinical assessments, cross-sectional surveys, neuroimaging and autopsies. Several cohort studies using medical record linkages or death certificates have also been published.41–45 The majority of studies included were a lower level of evidence (mainly level 4 or 5 with only 9 studies having level 3 evidence). All but one study included in this review had risk of bias scores
< 13, highlighting the potential of threats to the internal and external validity of these studies.
Subconcussive impacts
A small number of studies examined the possible long-term effects of subconcussive head impacts. There are significant methodological challenges associated with the study of subconcussive impacts.15 The challenge researchers face at this time is that (i) there is no established definition of a subconcussive impact or a subconcussive injury, (ii) a impact may or may not cause an injury, and it is difficult to determine if an injury has occurred, and (iii) the biomechanical features and thresholds for quantifying a impact and identifying an injury have not been agreed upon. Therefore, the hypothesis that subconcussive impacts cause long-term neurological injury requires more research before conclusions can be drawn.
Neuroimaging
Imaging studies have been conducted mostly with former American professional football players,8 21–24 27 28 32 33 but also with former soccer players10 18 21 and boxers.26 Imaging studies of retired professional football players reveal structural changes in the brain such as cortical thinning18 23 and CSP,21 22 62 functional changes in brain metabolism,32 as measured by functional MRI, microstructural differences in white matter,8 9 as measured by DTI, and accumulations of tau on PET imaging28 in some former athletes. The literature to date has significant methodological limitations that lower the overall level of evidence and temper confidence in conclusions that can be drawn. The imaging literature includes studies that likely are not representative of the broader population of former athletes. In reviewing the methodology and results of some imaging studies, it is sometimes unclear the extent to which positive findings were based on a priori hypotheses, exploratory post hoc analyses or both. A significant methodological weaknesses in the literature is lack of replication. Although positive findings have been reported in studies within an imaging modality, such as DTI or MRS, the specific findings within those studies differ.
Clinical studies
In total, 18 of the 24 studies relating to possible cognitive and mental health problems associated with exposure to collision sports and concussions have been published in the past five years, reflecting the interest in this topic and rapid growth of the knowledge base. These cross-sectional clinical studies and survey studies reveal that some of the former athletes have cognitive deficits or decrements6 7 36 37 and psychological health problems.16 29 35 Survey studies have revealed that a substantial minority of former NFL players have mental health problems,63–65 and current depression is more likely in those with a history of concussions.29 It is also important to appreciate that chronic pain and opioid use is relatively common in former NFL players,66 and those with depression and chronic pain also have greater life stress and financial difficulties.64 There are at least three unanswered questions relating to these studies. First, the contribution of repetitive subconcussive head impacts to these clinical features is poorly characterised and understood. Second, a frequency–response relationship between concussions, head impact exposures and the severity of future clinical symptoms is unknown. Finally, modifying factors for the development of clinical symptoms and problems in association with repetitive neurotrauma are largely unknown.
Neuropathology
Nine neuropathology studies were included in this review, seven of which were published between 2010 and 2016. Autopsy studies have revealed diverse forms of macroscopic and microscopic neuropathology in former athletes.11 48 50 51 Prior to 2015, there were no agreed upon neuropathological criteria for identifying CTE. The new consensus criteria provide a preliminary standardised approach to describe the neuropathology of CTE.54 The new consensus criteria differ from the criteria for CTE used in past studies, particularly by excluding tau pathology that is associated with ageing: primary age-related tauopathy67 and ARTAG.68 Importantly, tau pathology and the accumulation of other altered proteins such as Aβ, α-synuclein and TDP-43-positive immunoreactivity occurs with human ageing and several neurodegenerative diseases, and can also be found in people who are cognitively normal69; thus, it would be incorrect to assume that all such pathology is unique to, or caused by, CTE. To date, a cause and effect relationship between CTE and concussions or exposure to contact sports has not been established. More research on CTE is needed to better understand the incidence and prevalence of CTE pathology, the extent to which the neuropathological findings cause specific clinical symptoms, the extent to which the neuropathology is progressive, the clinical diagnostic criteria and other risk or protective factors. Well-designed case–control and cohort studies can begin to answer these important questions. Longitudinal studies are needed.
Limitations
A major limitation in the clinical assessment, survey, neuroimaging, cohort and autopsies studies published to date is that most do not consider relevant third variables when examining the association between prior concussions and long-term brain health problems. When evaluating the association between an ‘exposure’ (ie, concussion or repetitive head impacts) and ‘outcome’ (eg, long-term brain health problems), the possible roles of a relevant third variable are (i) effect modifier (eg, host susceptibility factors), (ii) intermediary and (iii) confounder. There are many candidate third variables that might be associated with the long-term cognitive and mental health of former athletes, from the psychiatric and neuroscience literature, including genetics, childhood adversity, personality factors, resilience, family history of mental health and neurological problems, steroid use, drug and alcohol use, opiate misuse, chronic pain, depression, anxiety, life stress, marital and family problems, diet and nutrition, exercise, obesity, diabetes, heart disease, other general medical problems, small vessel ischaemic disease and a diverse range of neurological conditions and diseases. In a survey study of former Division I collegiate athletes, for example, socioeconomic (ie, income) and nutritional factors (ie, greater fat and cholesterol and overall lower diet quality) were associated with perceived cognitive difficulties in older adults.70
Our systematic review has several methodological limitations. First, studies with negative findings are less likely to be published, and we only reviewed published studies, so there is a potential for publication bias in our conclusions. Second, we only included English-language articles, so there is potential for language bias influencing our conclusions. Third, we could not pool data across studies and meta-analyse risk associations or effect-modifying factors. Finally, the literature has major methodological limitations overall, and organising the review specifically as a best evidence synthesis might have resulted in more tempered conclusions about associations between multiple concussions and specific long-term outcomes.
Conclusion
In conclusion, there is evidence that some former athletes in contact, collision and combat sports suffer from depression39 and cognitive deficits6 7 later in life, and there is an association between these deficits and a history of multiple concussions.6 Former athletes are not at increased risk for death by suicide.41 71–73 Former high school American football players do not appear to be at increased risk for later life neurodegenerative diseases according to two studies.44 45 Retired professional American football players may be at increased risk for mild cognitive impairment.6 7 An increased risk for neurodegenerative diseases in retired American football players is suggested in one study examining death certificates,43 but more research is needed. Neuroimaging studies show modest evidence of macrostructural,21 22 24 microstructural,27 functional23 32 33 and neurochemical10 17 changes in some athletes. It is important to appreciate, however, that survey studies of former collegiate20 30 31 and professional29 athletes indicate that the majority of people rate their functioning as normal and consistent with the general population.
There is much more to learn about the potential cause and effect relationships of repetitive head impact exposure, concussions and long-term brain health. The potential for developing CTE must be a consideration; this condition appears to represent a distinct tauopathy with an unknown prevalence in former athletic populations. More research on the long-term sequelae is needed to better understand the incidence and prevalence of CTE and other neurological conditions among former athletes. The causes of mental health and cognitive problems in former athletes, like the general population, are broad and diverse including genetics, life stress, general medical problems (eg, hypertension, diabetes and heart disease), chronic bodily pain, substance abuse, neurological conditions and disease (eg, cerebrovascular disease) and neurodegenerative diseases (eg, Alzheimer’s disease, Parkinson’s disease and ALS). The extent to which repetitive neurotrauma causes static or progressive changes in brain microstructure and physiology, and contributes to later life mental health and cognitive problems, is poorly understood and requires further study.
Footnotes
Competing interests: GTM has been reimbursed by the government, professional scientific bodies and commercial organisations for discussing orpresenting research relating to mild TBI at meetings, scientific conferencesand symposiums. He serves as an Unaffiliated Neurotrauma Consultant for theNational Football League. He has received funding from General ElectricCompany, acting through its GE Healthymagination unit. He is also a subcontractPI on The NCAA-DOD Grand Alliance-Concussion Assessment, Research and Education(CARE Consortium). AG has a clinical practice in neuropsychology involvingindividuals who have sustained sport-related concussion (including current andformer athletes). He has operated as a contracted concussion consultant to theAustralian Rugby Union(ARU) from July 2016. He has received travel funding fromthe Australian Football League (AFL) to present at the Concussion in FootballConference in 2013. Previous grant funding includes the NSW Sporting InjuriesCommittee, the Brain Foundation (Australia), and the Hunter Medical ResearchInstitute (HMRI), supported by Jennie Thomas. He is currently funded throughthe HMRI, supported by Anne Greaves, and the University of Newcastle’s PriorityResearch Centre for Stroke and Brain Injury. KS is a physiotherapy consultantat Evidence Sport and Spinal Therapy in Calgary, Alberta, Canada. She hasreceived research grant support through the University of Calgary from theAlberta Children’s Hospital Research Institute, Hotchkiss Brain Institute andthe Canada Foundation for Innovation (including matching funds through theProvince of Alberta). She is a faculty member at the Sport Injury PreventionResearch Centre, which is one of the International Research Centres forPrevention of Injury and Protection of Athlete Health supported by theInternational Olympic Committee (IOC). KMG serves on the NCAA ConcussionProtocol Subcommittee as the Atlantic Coast Conference representative. He isalso a member of the USA Soccer Concussion Committee. JB supervises a TBIresearch laboratory which has received grant funding from pharmaceutical andindustry sponsors and the National Institutes of Health. He has receivedconsulting fees from industry and royalties from intracranial surgeryinstrumentation and has been a consultant for AIBA, NCAA, as well as providingexpert witness testimony for legal cases and the NCAA, and received speaker’shonoraria. He is the chairman of the Medical Advisory Board of Pop WarnerFootball, which is a non-compensated position. RCC serves as aconsultant/advisor to the National Football League Head, Neck and SpineCommittee and National Operating Committee on Standards for Athletic Equipment. He is Medical Director of Concussion Legacy Foundation and receives royaltiesfrom Houghton Mifflin. RC has a clinical and consulting practice in forensicneuropathology, including postmortem neuropathological interpretation ofindividuals who have sustained various types of traumatic brain injury. Hereceives salary support from the Lieber Institute for Brain Development, andsubcontracts with the NIH Neurobiobank at the University of Maryland forneuropathology interpretation. MT has been reimbursed for his travel andaccommodation expenses by conference and seminar organisers internationallywhen invited to speak on concussion and concussion-related topics. In situationswhere the organisers have been unable to provide financial support, theInternational Concussion and Head Injury Research Foundation (ICHIRF) hasreimbursed the cost of his travel and accommodation for attendance at theseevents. He is Medical Director of ICHIRF which receives research funding fromGodolphin Racing, the Injured Jockeys Fund, the NFL and private sponsors. Hedoes not receive any salary from ICHIRF, apart from the expenses mentionedabove. BDJ acts as an Unaffiliated Neurotrauma Consultant for theNational Football League, serves on the NFL Players Association Health andSafety Committee and is a Medical Advisory Physician for NFL Player Benefits. CRhas been reimbursed by professional scientific organisations and commercialentities for presenting research findings on sport-related concussion and mildtraumatic brain injury. He has had a clinical and consulting practice inneuropsychology including forensic neuropsychology, closed to new cases in July2016. He has received no salary support, or any other type of support, for hisresearch on sport-related concussion or brain injury in general. GI has beenreimbursed by the government, professional scientific bodies and commercialorganisations for discussing or presenting research relating to mild TBI andsport-related concussion at meetings, scientific conferences and symposiums. Hehas a clinical and consulting practice in forensic neuropsychology involvingindividuals who have sustained mild TBIs (including professional athletes). Hehas been a principal investigator and co-investigator on federal and industrygrants on topics relating to mild traumatic brain injury, neuropsychologicalassessment and depression. He has received consulting fees from pharmaceuticalcompanies. He receives royalties for books and one neuropsychological test. Hehas received research funding from several test publishing companies, includingImPACT Applications, CNS Vital Signs and Psychological Assessment Resources (PAR). He acknowledges unrestricted philanthropic support from the Mooney-ReedCharitable Foundation and ImPACT Applications. He previously served as acontractor in the area of TBI research through General Dynamics for the Defenseand Veterans Brain Injury Center within the US Department of Defense. Hereceives salary support for chairing the Brain and Behavior committee for theHarvard Integrated Program to Protect and Improve the Health of NFLPA Members.
Provenance and peer review: Not commissioned; externally peer reviewed.
Author note: The authors thank Amy J Markowitz, JD and Brian Fabian, MPA for editorial support.
References
Full text links
Read article at publisher's site: https://doi.org/10.1136/bjsports-2017-097791
Read article for free, from open access legal sources, via Unpaywall:
https://bjsm.bmj.com/content/bjsports/51/12/969.full.pdf
Citations & impact
Impact metrics
Article citations
Mental health symptom burden in elite ice hockey players and its association with self-reported concussive events.
BMC Sports Sci Med Rehabil, 16(1):197, 23 Sep 2024
Cited by: 0 articles | PMID: 39313839 | PMCID: PMC11421113
Longevity of Polish top-class athletes compared to other social elites and well-known people in the years 2001-2021.
Int J Occup Med Environ Health, 37(3):335-350, 21 Aug 2024
Cited by: 0 articles | PMID: 39221497 | PMCID: PMC11424149
The Influence of Induced Head Acceleration on Lower-Extremity Biomechanics during a Cutting Task.
Sensors (Basel), 24(15):5032, 03 Aug 2024
Cited by: 0 articles | PMID: 39124078 | PMCID: PMC11315045
Assessment of Sports Concussion in Female Athletes: A Role for Neuroinformatics?
Neuroinformatics, 30 Jul 2024
Cited by: 0 articles | PMID: 39078562
Review
Anisotropy component of DTI reveals long-term neuroinflammation following repetitive mild traumatic brain injury in rats.
Eur Radiol Exp, 8(1):82, 24 Jul 2024
Cited by: 0 articles | PMID: 39046630 | PMCID: PMC11269550
Go to all (232) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
History of Sport-Related Concussion and Long-Term Clinical Cognitive Health Outcomes in Retired Athletes: A Systematic Review.
J Athl Train, 55(2):132-158, 14 Jan 2020
Cited by: 21 articles | PMID: 31935139 | PMCID: PMC7017894
Review Free full text in Europe PMC
Association Between History of Multiple Concussions and Health Outcomes Among Former College Football Players: 15-Year Follow-up From the NCAA Concussion Study (1999-2001).
Am J Sports Med, 46(7):1733-1741, 05 Apr 2018
Cited by: 33 articles | PMID: 29620911
The association between white-matter tract abnormalities, and neuropsychiatric and cognitive symptoms in retired professional football players with multiple concussions.
J Neurol, 263(7):1332-1341, 03 May 2016
Cited by: 38 articles | PMID: 27142715
Systematic review of prognosis and return to play after sport concussion: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis.
Arch Phys Med Rehabil, 95(3 suppl):S210-29, 01 Mar 2014
Cited by: 54 articles | PMID: 24581907
Review