Abstract
Background
Prognosis for women with abdominal aortic aneurysm might be worse than the prognosis for men. We aimed to systematically quantify the differences in outcomes between men and women being assessed for repair of intact abdominal aortic aneurysm using data from study periods after the year 2000.Methods
In these systematic reviews and meta-analysis, we identified studies (randomised, cohort, or cross-sectional) by searching MEDLINE, Embase, CENTRAL, and grey literature published between Jan 1, 2005, and Sept 2, 2016, for two systematic reviews and Jan 1, 2009, and Sept 2, 2016, for one systematic review. Studies were included if they were of both men and women, with data presented for each sex separately, with abdominal aortic aneurysms being assessed for aneurysm repair by either endovascular repair (EVAR) or open repair. We conducted three reviews based on whether studies reported the proportion morphologically suitable (within manufacturers' instructions for use) for EVAR (EVAR suitability review), non-intervention rates (non-intervention review), and 30-day mortality (operative mortality review) after intact aneurysm repair. Studies had to include at least 20 women (for the EVAR suitability review), 20 women (for the non-intervention review), and 50 women (for the operative mortality review). Studies were excluded if they were review articles, editorials, letters, or case reports. For the operative review, studies were also excluded if they only provided hazard ratios or only reported in-hospital mortality. We assessed the quality of the studies using the Newcastle-Ottawa scoring system, and contacted authors for the provision of additional data if needed. We combined results across studies by random-effects meta-analysis. This study is registered with PROSPERO, number CRD42016043227.Findings
Five studies assessed the morphological eligibility for EVAR (1507 men, 400 women). The overall pooled proportion of women eligible (34%) for EVAR was lower than it was in men (54%; odds ratio [OR] 0·44, 95% CI 0·32-0·62). Four single-centre studies reported non-intervention rates (1365 men, 247 women). The overall pooled non-intervention rates were higher in women (34%) than men (19%; OR 2·27, 95% CI 1·21-4·23). The review of 30-day mortality included nine studies (52 018 men, 11 076 women). The overall pooled estimate for EVAR was higher in women (2·3%) than in men (1·4%; OR 1·67, 95% CI 1·38-2·04). The overall estimate for open repair also was higher in women (5·4%) than in men (2·8%; OR 1·76, 95% CI 1·35-2·30).Interpretation
Compared with men, a smaller proportion of women are eligible for EVAR, a higher proportion of women are not offered intervention, and operative mortality is much higher in women for both EVAR and open repair. The management of abdominal aortic aneurysm in women needs improvement.Funding
National Institute for Health Research (UK).Free full text
Morphological suitability for endovascular repair, non-intervention rates, and operative mortality in women and men assessed for intact abdominal aortic aneurysm repair: systematic reviews with meta-analysis
Summary
Background
Prognosis for women with abdominal aortic aneurysm might be worse than the prognosis for men. We aimed to systematically quantify the differences in outcomes between men and women being assessed for repair of intact abdominal aortic aneurysm using data from study periods after the year 2000.
Methods
In these systematic reviews and meta-analysis, we identified studies (randomised, cohort, or cross-sectional) by searching MEDLINE, Embase, CENTRAL, and grey literature published between Jan 1, 2005, and Sept 2, 2016, for two systematic reviews and Jan 1, 2009, and Sept 2, 2016, for one systematic review. Studies were included if they were of both men and women, with data presented for each sex separately, with abdominal aortic aneurysms being assessed for aneurysm repair by either endovascular repair (EVAR) or open repair. We conducted three reviews based on whether studies reported the proportion morphologically suitable (within manufacturers' instructions for use) for EVAR (EVAR suitability review), non-intervention rates (non-intervention review), and 30-day mortality (operative mortality review) after intact aneurysm repair. Studies had to include at least 20 women (for the EVAR suitability review), 20 women (for the non-intervention review), and 50 women (for the operative mortality review). Studies were excluded if they were review articles, editorials, letters, or case reports. For the operative review, studies were also excluded if they only provided hazard ratios or only reported in-hospital mortality. We assessed the quality of the studies using the Newcastle–Ottawa scoring system, and contacted authors for the provision of additional data if needed. We combined results across studies by random-effects meta-analysis. This study is registered with PROSPERO, number CRD42016043227.
Findings
Five studies assessed the morphological eligibility for EVAR (1507 men, 400 women). The overall pooled proportion of women eligible (34%) for EVAR was lower than it was in men (54%; odds ratio [OR] 0·44, 95% CI 0·32–0·62). Four single-centre studies reported non-intervention rates (1365 men, 247 women). The overall pooled non-intervention rates were higher in women (34%) than men (19%; OR 2·27, 95% CI 1·21–4·23). The review of 30-day mortality included nine studies (52 018 men, 11 076 women). The overall pooled estimate for EVAR was higher in women (2·3%) than in men (1·4%; OR 1·67, 95% CI 1·38–2·04). The overall estimate for open repair also was higher in women (5·4%) than in men (2·8%; OR 1·76, 95% CI 1·35–2·30).
Interpretation
Compared with men, a smaller proportion of women are eligible for EVAR, a higher proportion of women are not offered intervention, and operative mortality is much higher in women for both EVAR and open repair. The management of abdominal aortic aneurysm in women needs improvement.
Funding
National Institute for Health Research (UK).
Introduction
Treatment guidelines recommend that an abdominal aortic aneurysm in men should be considered for elective repair once the aneurysm has reached a diameter of 5·5 cm, based on randomised trials that compared early elective repair with surveillance; these trials included only a small proportion of women.1 The decision to offer repair is made when the probable risk of rupture exceeds the risk of repair. Since the rate of rupture of small abdominal aortic aneurysm is four times higher in women than men at the same diameter,2 women are often considered for repair at diameters smaller than 5·5 cm. Several studies3, 4 have suggested that the prognosis of individuals with abdominal aortic aneurysm is worse for women than men, with the operative mortality following repair of intact aneurysm being higher in women than men.
To determine whether women, compared with men, are being offered adequate management of their intact aneurysms once they have reached the aneurysm diameter threshold for intervention, three pieces of crucial information are required: the proportion of each sex morphologically suitable for endovascular aneurysm repair (EVAR; often preferred to open repair because it is minimally invasive and has a lower operative mortality), the proportion of each sex not offered repair (for which the suitability for EVAR might be influential), and the 30-day mortality after elective aneurysm repair, either EVAR or open repair.
Randomised trials have reported that 30-day operative mortality for elective repair of abdominal aortic aneurysm is about three times higher after open repair than after EVAR,5 but again, women were poorly represented in these trials, perhaps partly because the early generation endografts were not suitable for most women.6, 7 However, data from the large Medicare database in the USA suggest that this relative difference in 30-day mortality between EVAR and open repair is observed for both men and women, even though the absolute mortality was higher in women than men.8 An earlier systematic review,9 including studies published by July, 2009, showed that for elective open repairs the operative mortality (30 day or in-hospital) was 7·6% for women versus 5·1% for men. For EVAR, the mortality for women was 2·9% versus 1·5% for men, but included only 1014 women undergoing EVAR.
The aim of this study was to quantify how the prognosis of women with abdominal aortic aneurysm compares with the prognosis in men. Therefore, we have systematically searched for contemporary evidence that describes the outcome of women with an intact abdominal aortic aneurysm of the size for which repair is considered in three sequential stages of the care pathway.
Methods
Search strategy and selection criteria
We identified relevant publications according to PRISMA guidelines, with the aim of systematically reviewing published data and grey literature published since 2005 or 2009. First, we obtained data for the proportion of men and women with abdominal aortic aneurysm being assessed for aneurysm repair who were morphologically suitable for EVAR (EVAR suitability review); second, we obtained data for the proportion of men and women not offered aneurysm repair (non-intervention review); and finally, we obtained data for the elective operative (30 day) mortality in men and women after either EVAR or open repair reported since an earlier review9 was published in 2010, (operative mortality review). A favourable ethical opinion for the systematic reviews done for the SWAN project was obtained from the West of Scotland REC 5 (15/WS/0136).
For our reviews, we searched MEDLINE and Embase using a combination of controlled vocabulary (MeSH or Emtree; panel) terms and free-text terms in ProQuest Dialog (ProQuest, Ann Arbor, MI, USA) and restricting the search to data published since Jan 1, 2005 (EVAR suitability and non-intervention reviews), and since Jan 1, 2009 (operative mortality review, and therefore were not included in the 2010 review)9 for articles in English, French, or German. We also searched CENTRAL, ClinicaTrials.gov, Current Controlled Trials, and the National Research Register (UK) for details of ongoing or unpublished studies. We complemented searches by scanning reference lists of relevant articles, by direct enquiries to the companies' marketing endografts for the EVAR suitability review, and by hand-searching the abstracts of the 2015 and 2016 annual meetings of the Society for Vascular Surgery (North America) and the European Society for Vascular Surgery for all reviews. The final search date for all reviews, including a PubMed search, was Sept 2, 2016.
The panel shows the MeSH headings and key information for the three reviews, which were informed by the review protocols. For the EVAR suitability review, studies were included if they had more than 20 women, all or nearly all of the patients were considered for abdominal aortic aneurysm repair, morphological criteria for suitability were clearly defined with measurements or device instructions for use, and had CT with 1 mm slices and 3D reconstruction. For the non-intervention review, studies were included if they had more than 20 women, all or nearly all of the patients were considered for abdominal aortic aneurysm repair, and if it was a team decision whether repair offered. For the operative review, studies were included if they had a study period after the year 2000, and had more than 50 women. Studies were excluded if they were review articles, editorials, letters, or case reports, and if they only provided hazard ratios or only reported in-hospital mortality.
The appendix has the full search strategies and PRISMA flow diagrams. For duplicated data, the most recent or most comprehensive paper was included. Studies must have included both men and women, and presented data for each separately. Initial screening was based on the study title, followed by reviewing abstracts, after which full-text versions of the selected shortlist of documents were obtained and assessed for eligibility by two reviewers (RSvA and JTP for the EVAR suitability review and PU and JTP for the non-intervention review and operative mortality review). We recorded study design and setting, demographic and technical details, and potential biases (eg, ascertainment of outcomes). A summary checklist was completed for each study. When necessary, we contacted authors for the provision of additional data. Differences of opinion about study inclusion were resolved by discussion or a third reviewer. Two reviewers independently undertook quality scoring using the Newcastle–Ottawa score for cohort or cross-sectional studies.10
Data analysis
We made an estimate of the suitability for EVAR in men and women from each study, calculated as the number of each sex whose abdominal aortic aneurysm was suitable for EVAR (according to the manufacturers' instructions for use) divided by the number who were assessed. We made an estimate of the non-intervention rate in men and women from each study, calculated as the number of each sex who were not offered repair divided by the number who were assessed.
95% CIs for percentages were calculated assuming normality on the log odds scale. Differences between women and men in each study were expressed as odds ratios (OR). For all reviews, we did random-effects meta-analyses on the log odds (or log OR) scale using the method of DerSimonian and Laird;11 estimates were then transformed back to the probability (or OR) scale. We assessed heterogeneity using the I2 statistic.12 Results are presented as forest plots. The reviews were registered in the PROSPERO database (CRD42016043227).
Role of the funding source
The funder of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
After our search and evaluation (appendix), five papers based on five studies13, 14, 15, 16, 17 were eligible for inclusion in the meta-analysis regarding suitability for endovascular repair. Another study18 also included suitability for endovascular sealing technology, but used a selected population. The characteristics of the included studies are summarised in the appendix. One of these studies included more than 100 women, most studies were small, and the quality of these studies was assessed as fair. The criteria of morphological suitability for EVAR were different in each study; three studies13, 15, 16 included all the aneurysms diagnosed (including those not offered intervention), one study17 did not specify which patients were being considered for EVAR, and one study14 only considered patients who had undergone elective repair. The largest study15 has published two further updates but neither provided sufficient information to merit inclusion in the review.19, 20 Threshold abdominal aortic aneurysm diameter for inclusion ranged from 4 cm to 5 cm. In total, information was available for 1507 men and 400 women in whom the suitability for EVAR ranged from 46% to 64% for men and from 25% to 47% for women. The overall pooled estimate of suitability for EVAR was 34% in women compared with 54% in men; both overall estimates had significant heterogeneity (figure 1A). For the proportion of women compared with men who were suitable for EVAR, the OR was 0·44 (95% CI 0·32–0·62), with moderate heterogeneity (figure 1B).
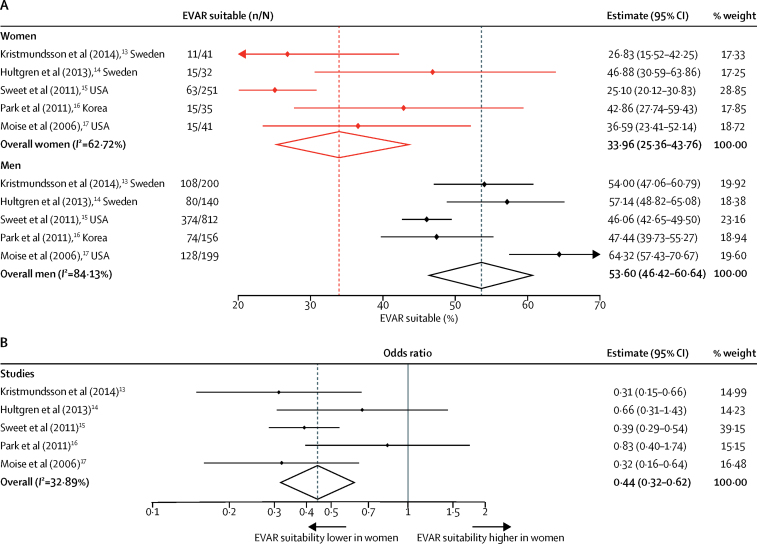
Forest plots of the proportion of aneurysm patients morphologically suitable for EVAR
(A) Women and men separately. (B) Women versus men. EVAR=endovascular repair.
Some studies considered relaxation of the morphological criteria for EVAR, which increased the proportion of women suitable for EVAR. For instance, in the largest study including 251 women,15 relaxation of the neck length to longer than 7·5 mm (from >15 mm) increased the suitability for EVAR from 63 (25%) women to 113 (45%) women. In one study,13 relaxation of the minimum iliac diameter from 7·5 mm or 8 mm to 6 mm increased the proportion of 41 women eligible for EVAR from 11 (27%) to 16 (39%). The type of endograft considered also affects the proportion of women suitable for EVAR. For example, in one excluded study18 of 78 women that considered both conventional endografts and endovascular sealing, 32 (41%) women were suitable for the Gore Excluder graft (Gore Medical, Flagstaff, AZ, USA), but 61 (78%) would have been eligible for endovascular-sealing technology.18
The largest study15 investigated how suitability for EVAR declined with increasing aneurysm diameter, with almost no women being considered suitable for EVAR if their abdominal aortic aneurysm diameter cutoff exceeded 6·5 cm compared with 30% of men being suitable. The other four studies13, 14, 16, 17 provided few demographic or clinical details, so it was not possible to investigate how the suitability for EVAR in women might depend on age or other characteristics.
Our search and evaluation of non-intervention rates (appendix) yielded four publications, all from the UK, including two papers21, 22 and two abstracts23, 24 (both with additional information provided by the authors). All four studies were retrospective, with a total of 1365 men and 247 women; the studies were assessed as of fair quality (appendix). The overall results showed greater heterogeneity for men than for women and suggested that a third (34%) of potentially eligible women were either not offered or refused abdominal aortic aneurysm repair. The proportion was about double the non-intervention rate in men (19%; OR 2·27, 95% CI 1·21–4·23; figure 2). The difference in non-intervention rates between men and women was highest for the earliest study22 at a specialist tertiary referral centre.
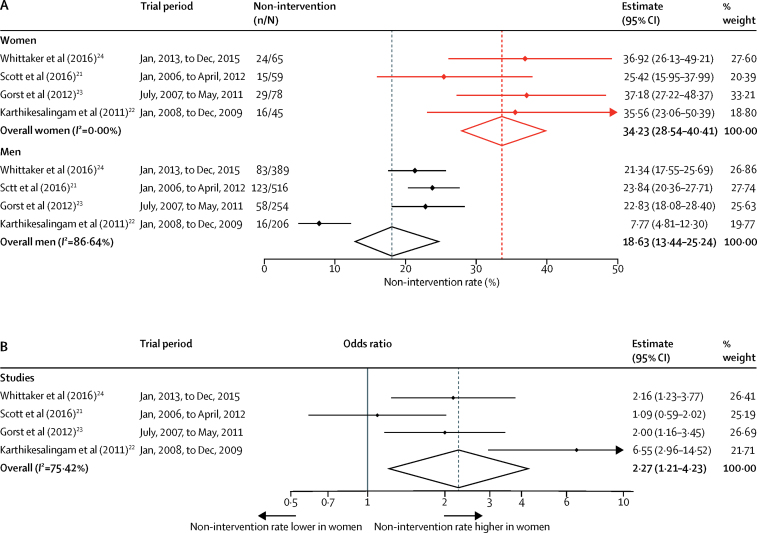
Forest plots of non-intervention rates in cohorts of patients assessed for intact abdominal aortic aneurysm repair
(A) Women and men separately. (B) Women versus men.
After our search and evaluation for studies on elective operative mortality (appendix), eight papers based on eight studies met the inclusion criteria.25, 26, 27, 28, 29, 30, 31, 32 For one study31 reporting from 1992 to 2012, the 30-day operative mortality data for the late era (2003–12) were obtained from the corresponding author. Similarly, the data for 30-day mortality for the time period 2006–10 in the Swedish study28 were supplied by the corresponding author. All studies included consecutive patients undergoing EVAR or open repair, or both, for infrarenal abdominal aortic aneurysm between January, 2000, and March, 2015. One further study5 was identified and we excluded the few patients with repairs before 2000. Therefore, nine studies were included in the meta-analysis. All nine studies provided data for intact infrarenal aneurysms only: two5, 31 studies excluded symptomatic abdominal aortic aneurysm. The English study32 was population-based, but for EVAR only. We excluded a similar study,33 including open repair but covering an earlier time period, because much of the 30-day mortality was not aneurysm-related.
Full details of the included studies are summarised in the appendix. Three population-based studies28, 30, 32 were done in Sweden (765 women), the USA (5421 women), and the UK (2304 women). Other, mostly smaller, studies,25, 26, 27, 29, 31 based on either single centre or voluntary registries, were all from the USA and included 2438 women. Individual patient data meta-analysis5 of four prospective randomised controlled trials contributed data for 148 women. These data gave a total of 11 076 women operated on in nine separate studies, with an overall 30-day mortality of 2·31% (95% CI 1·99–2·68) after EVAR with no heterogeneity (figure 3A) and 5·37% (95% CI 4·18–6·88) after open repair with slight heterogeneity (figure 4A). These data contrast with the more heterogeneous results for a much larger cohort of 52 018 men operated on in these same studies with an overall 30-day mortality of 1·37% (95% CI 1·12–1·68) after EVAR and 2·82% (95% CI 1·88–4·22) after open repair (Figure 3, Figure 4). The Medicare study30 provided the most data for the results of open repair. When this study was removed from the meta-analysis, the change in 30-day mortality was little: 4·72% for women (95% CI 3·83–5·82) and 2·50% for men (1·76–3·55). Similarly for EVAR, after exclusion of the two largest studies,30, 32 the change in 30-day mortality was little: 2·55% for women (95% CI 1·83–3·55) and 1·24% for men (0·81–1·89).
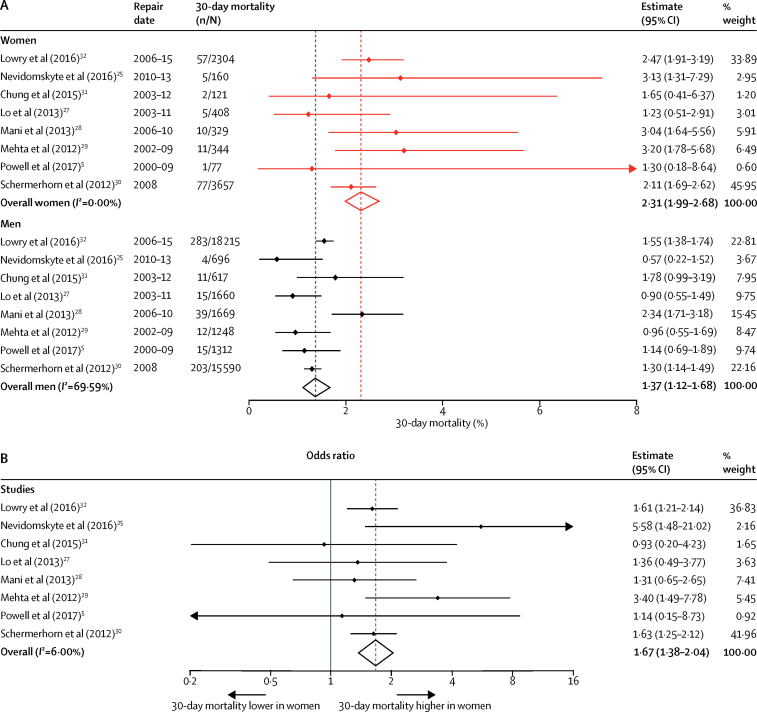
Forest plots of 30-day mortality after EVAR for intact abdominal aortic aneurysm
(A) Women and men separately. (B) Women versus men. EVAR=endovascular repair.
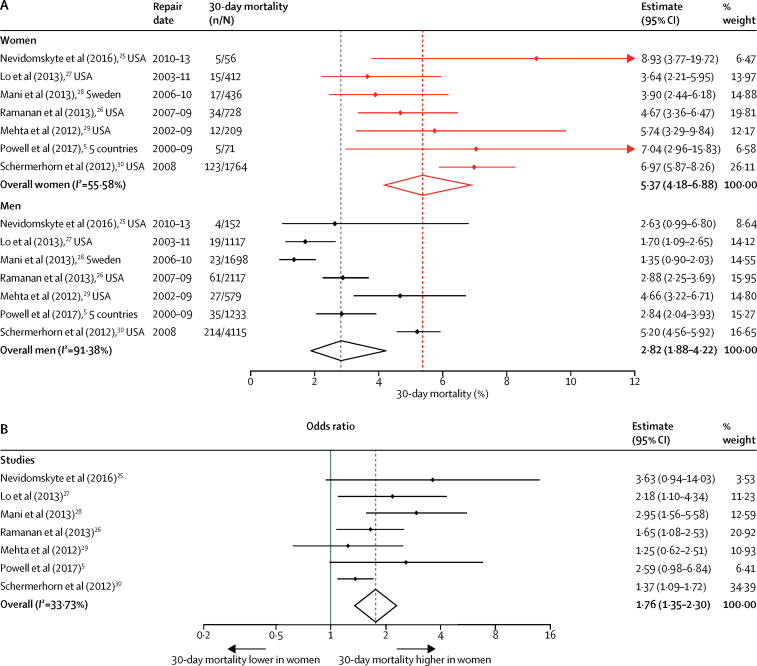
Forest plots of 30-day mortality after open repair for intact abdominal aortic aneurysm
(A) Women and men separately. (B) Women versus men.
In the nine included studies, 30-day mortality was significantly higher in women than in men for both types of repair: the overall OR for EVAR was 1·67 (95% CI 1·38–2·04) and for open repair 1·76 (1·35–2·30; Figure 3, Figure 4). Confounding factors such as age, abdominal aortic aneurysm diameter, number of symptomatic abdominal aortic aneurysms included, and comorbidities were reported inconsistently, but the adjusted OR continued to show a higher mortality in women of almost double (table); only three studies reported separately for EVAR and open repair.
Table
Adjusted odds ratios for 30-day mortality for women versus men undergoing repair of intact abdominal aortic aneurysms
| Main adjustment factors | Type of repair | Adjusted odds ratio (95% CI) | p value | |
|---|---|---|---|---|
| Powell et al (2017)5 | Age, abdominal aortic aneurysm diameter, creatinine | EVAR and open | 2·01 (0·82–4·94) | 0·13 |
| Ramanan et al (2013)26 | Age, comorbidities | Open | 1·69 (1·06–2·69) | 0·03 |
| Lo et al (2013)27 | Age, comorbidities, type of repair | EVAR and open | 1·7 (1·0–2·8) | 0·063 |
| Mani et al (2013)28 | Age, comorbidities, type of repair | EVAR and open | 1·44 (1·01–2·04) | 0·008 |
| Mehta et al (2012)29 | Age, abdominal aortic aneurysm diameter | EVAR | 3·36 (1·44–7·85) | 0·01 |
| Lowry et al (2016)32 | Age, comorbidities, ethnicity | EVAR | 1·54 (1·15–2·07) | 0·004 |
Comorbidities were defined differently in each study.
Discussion
Prognosis of abdominal aortic aneurysm is often regarded as worse in women than men,3, 4 with adverse factors likely to include the older age of women, and higher morbidity and mortality after elective aneurysm repair. The data from our systematic review do not suggest that the proportion of women morphologically suitable for EVAR has improved since earlier this century.6, 7 However, the operative mortality in both men and women has fallen substantially since a 2010 systematic review,9 particularly for open repair; although 30-day operative mortality remains almost twice as high in women as in men. Some of the reduction in operative mortality in women might have come at the expense of the high proportion of women (a third) who are assigned to a non-intervention policy; although, the literature on non-intervention policy remains sparse.
Surgical registries and national databases do not record or report the numbers of patients with abdominal aortic aneurysm who either are morphologically suitable for EVAR or denied elective repair. The only non-intervention data identified came from four single centres in the UK, with decisions about repair being made at a multidisciplinary team meeting: presumably the women not offered repair had extensive comorbidities and had a high risk of early postoperative death. Only one of these series21 has provided detailed follow-up data for those initially assigned to a non-intervention policy. The study showed that after 3 years, only about a third of these patients remained alive and that 37% had died of rupture. Similarly, in the other full paper,22 only 35% of non-intervention patients were alive at 2 years.
Since EVAR is a less invasive procedure than open repair and is associated with a third to half of the 30-day mortality, the rate of morphological eligibility for EVAR is likely to effect the non-intervention rates for elective abdominal aortic aneurysm surgery. In 2001, using early-generation endografts, one study7 reported that only 39% of women versus 60% of men were morphologically eligible for EVAR. Our systematic review shows no improvement, with an overall estimate of 34% of women being morphologically suitable for EVAR, based on the manufacturers' instructions for use. The principal morphological criteria rendering women unsuitable for EVAR include both short and angulated proximal aneurysm necks and the dimensions of the access iliac arteries. Many endovascular specialists are willing to relax the strict requirements of the instructions for use,34 and adjunct techniques do exist, such as iliac conduits, to use EVAR in narrow or heavily calcified iliac arteries. Nowadays, lower profile devices suitable for smaller access vessels and devices that can adapt to shorter and more angulated necks are available. Potentially, this availability should allow more women to be treated by EVAR. However, summary information from the Characterization of Human Aortic Anatomy Project20 for 2012–13 lower profile devices (including Aorfix [Lombard Medical, Didcot, UK], Endurant II [Medtronic, Minneapolis, MN, USA], and Ovation [Endologix, Irvine, CA, USA]) suggests that only 40% of women remain suitable for EVAR based on the instructions for use. Other information from this project indicates that in women older than 80 years, EVAR eligibility is particularly low (29%).19 No endografts have been designed specifically for women, but preliminary data suggest that the endovascular-sealing technology is the approach most likely to increase the proportion of women suitable for endovascular repair.18
A comprehensive systematic review and meta-analysis9 showing the sex-specific differences in mortality after either EVAR or open repair of abdominal aortic aneurysm was published in 2010. This review included publications from 1995 to July, 2009, for operative mortality (either 30-day or in-hospital mortality; in-hospital mortality is usually lower than 30-day mortality). Operative mortality was higher in women than in men (overall OR for EVAR 2·51, 95% CI 1·72–3·69 vs OR for open repair 1·50, 1·33–1·69). The results were dominated by a 20-year review (1980–2000) from the USA with 81 384 women35 and contained few data for patients who underwent EVAR. By contrast, we focused on 30-day mortality only in studies published since Jan 1, 2009, which included more data for EVAR. Again the mortality for both EVAR and open repair was almost twice as high in women as in men, with mortality for EVAR being much lower than for open repair. Overall 30-day mortality for EVAR was 2·3% and for open repair was 5·4% for women versus 1·4% for EVAR and 2·8% for open repair in men. Although the overall mortality has decreased since the 2010 systematic review, the OR for women versus men has changed little. The mortality following open repair in women appears to be unacceptably high.
Since our analysis of 30-day mortality, we have become aware of two sources of recent data, covering the period 2011–14. A retrospective cohort study36 of 6661 patients from the American College of Surgeons National Surgical Quality Improvement Program has shown that, for either EVAR or open repair of intact abdominal aortic aneurysm, 30-day mortality in women is double that of men and women have a 30% increase in complication rate, even after adjustment for age and aneurysm diameter: mortality in women was 2·9% for EVAR and 8·2% for open repair versus 1·1% for EVAR and 4·0% for open repair in men. Analysis of the similar size English administrative dataset (Hospital Episode Statistics) showed that 30-day mortality for elective admissions was 2·3% for EVAR and 7·0% for open repair in women versus 1·4% for EVAR and 4·1% for open repair in men (Michaels J A, University of Sheffield, personal communication). The apparent recent increase in mortality for open repairs might be explained by the decreasing proportion of operations undertaken as open repairs, which diminishes expertise at a time when the remaining open repairs are likely to be the most technically challenging cases.
These studies have several limitations. First and foremost, factors that might confound the comparison of men and women, such as age, aneurysm diameter, and comorbidities, were inconsistently reported. Operative mortality is known to increase with age, and women appear to develop clinically relevant aneurysms at an older age than men.37, 38 Since prevalence increases rapidly with age, especially in women,39 this factor is an important consideration. Nevertheless, when adjusted data were available, the much higher 30-day mortality in women remained. Second, there was a varying amount of heterogeneity in the meta-analyses, but the results for all outcomes consistently showed sex-specific differences. Third, it can take several years for publications to appear in print, which might cover several generations of endografts and experience for EVAR, so obtaining contemporary data is challenging. Fourth, the patients selected for EVAR and open repair in the various studies are likely to be different, including differences in aortic morphology, which might affect mortality from both EVAR and open repair. Particularly when used outside the instructions for use, the complication, re-intervention, and mortality for EVAR could all increase.34, 40 Finally, a relative paucity of data is available about the number of women versus men either eligible for EVAR or not considered for any intervention, which underscores the importance of reporting primary data by sex.41
Moreover, our review has several strengths. All the studies included in this series had to include both men and women and present the data for each separately, so that men and women from the same population and the same time period are compared in each study. Furthermore, we presented results as OR and compared women with men in each study (and overall), since these OR should be less susceptible to heterogeneity than the results for men and women separately.
In summary, the results of these reviews indicate that the prognosis of women with abdominal aortic aneurysm is worse than that of men; although, we have not considered the management of cardiovascular risk (often worse in women),42, 43 complications after repair, and longer term quality or length of life. Women have smaller aortas than men,44 and perhaps if a smaller threshold for both diagnosis and intervention were introduced, compared with those recommended for men, women might have a better chance of being offered and surviving intervention at a younger age. Given the relatively high mortality following open abdominal aortic aneurysm repair in women, it would seem to be crucial either to design an endograft for women or to accept that most women need to be referred to centres that either offer endovascular sealing technology or are specialists in open repair. Such measures might see an improved prognosis for women.
Acknowledgments
This project was funded by the UK National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme (project number 14/179/01). Work done at the University of Cambridge was additionally funded by the Medical Research Council (MR/L003120/1), the British Heart Foundation (RG/13/13/30194), and the National Institute for Health Research; Cambridge Biomedical Research Centre). The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the HTA programme, NIHR, National Health Service, or the Department of Health. We would like to thank the authors of studies included in these reviews who provided additional data to complete these reviews and other members of the SWAN collaborative group.
SWAN (Screening Women for Aortic aNeurysm) collaborators
P Ulug, M J Sweeting, S G Thompson, J T Powell, and the following non-author collaborators: E Jones (University of Cambridge, Cambridge, UK); M J Bown, (University of Leicester, Leicester, UK); M J Glover (Brunel University, Uxbridge, UK); J Michaels (University of Sheffield, Sheffield, UK).
Contributors
PU did the searches, reviewed published works and organised extracted information in databases, created tables, drafted the manuscript, and prepared the supplementary material. MJS was the third reviewer, did analysis and statistics, and created the figures. RSvA translated studies and reviewed the published work. SGT obtained funding, and had input on analysis and presentation. JTP designed the study, reviewed the published works, created tables, and drafted the manuscript. All authors critically reviewed the manuscript.
References
Full text links
Read article at publisher's site: https://doi.org/10.1016/s0140-6736(17)30639-6
Read article for free, from open access legal sources, via Unpaywall:
http://www.thelancet.com/article/S0140673617306396/pdf
Citations & impact
Impact metrics
Article citations
Cost-effectiveness analysis of endovascular versus open repair in patients with abdominal aortic aneurysm in Iran: a cross-sectional study.
Int J Surg, 110(6):3338-3345, 01 Jun 2024
Cited by: 0 articles | PMID: 38502855
A prospective longitudinal study of risk factors for abdominal aortic aneurysm.
Physiol Rep, 12(13):e16130, 01 Jul 2024
Cited by: 1 article | PMID: 38946069 | PMCID: PMC11214915
Age-specific sex-differences in cerebral blood flow velocity in relation to haemoglobin levels.
Eur Stroke J, 9(3):772-780, 18 Apr 2024
Cited by: 1 article | PMID: 38634499 | PMCID: PMC11343687
Aortic aneurysms in patients with atherosclerotic coronary artery disease in the southwestern region of Romania - clinical and histopathological study.
Rom J Morphol Embryol, 65(2):251-256, 01 Apr 2024
Cited by: 0 articles | PMID: 39020539 | PMCID: PMC11384034
Effect of EVAR on International Ruptured AAA Mortality-Sex and Geographic Disparities.
J Clin Med, 13(9):2464, 23 Apr 2024
Cited by: 0 articles | PMID: 38730993 | PMCID: PMC11084331
Go to all (62) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Editor's Choice - Systematic Review and Meta-Analysis of Sex Specific Differences in Adverse Events After Open and Endovascular Intact Abdominal Aortic Aneurysm Repair: Consistently Worse Outcomes for Women.
Eur J Vasc Endovasc Surg, 62(3):367-378, 28 Jul 2021
Cited by: 17 articles | PMID: 34332836
Review
Laparoscopic surgery for elective abdominal aortic aneurysm repair.
Cochrane Database Syst Rev, 5:CD012302, 04 May 2017
Cited by: 6 articles | PMID: 28471523 | PMCID: PMC6481464
Review Free full text in Europe PMC
Endovascular versus open repair of abdominal aortic aneurysm in 15-years' follow-up of the UK endovascular aneurysm repair trial 1 (EVAR trial 1): a randomised controlled trial.
Lancet, 388(10058):2366-2374, 12 Oct 2016
Cited by: 268 articles | PMID: 27743617
Funding
Funders who supported this work.
British Heart Foundation (2)
Large-scale integrative studies of risk factors in coronary heart disease: from discovery to application. (renewal) (Joint funding with MRC)
John Danesh, Cambridge, University Of
Grant ID: RG/13/13/30194
Systematic approaches to the evaluation of emerging coronary risk markers. Large-scale epidemiological analyses of existing data and stored biological samples (renewal)
John Danesh, University of Cambridge
Grant ID: RG/08/014/24067
Medical Research Council (2)
Study of the interplay of genetic, biochemical, and lifestyle factors on coronary heart disease incidence
John Danesh, University of Cambridge
Grant ID: G0800270
Large-scale integrative studies of risk factors in coronary heart disease: from discovery to application
John Danesh, University of Cambridge
Grant ID: MR/L003120/1
National Institute for Health Research (NIHR) (3)
Screening women age 65 or over for abdominal aortic aneurysm: a modelling study and health economic evaluation
Professor Simon Thompson, University of Cambridge
Grant ID: 14/179/01
Grant ID: NF-SI-0512-10165
Screening women age 65 or over for abdominal aortic aneurysm: a modelling study and health economic evaluation
Professor Simon Thompson, University of Cambridge
Grant ID: HTA/14/179/01
UK National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme (1)
Grant ID: project number 14/179/01






