Abstract
Free full text

2019 Novel coronavirus: where we are and what we know
Abstract
There is a current worldwide outbreak of a new type of coronavirus (2019-nCoV), which originated from Wuhan in China and has now spread to 17 other countries. Governments are under increased pressure to stop the outbreak spiraling into a global health emergency. At this stage, preparedness, transparency, and sharing of information are crucial to risk assessments and beginning outbreak control activities. This information should include reports from outbreak sites and from laboratories supporting the investigation. This paper aggregates and consolidates the virology, epidemiology, clinical management strategies from both English and Chinese literature, official news channels, and other official government documents. In addition, by fitting the number of infections with a single-term exponential model, we report that the infection is spreading at an exponential rate, with a doubling period of 1.8 days.
Introduction
On 12th December 2019, Wuhan Municipal Health Commission (WMHC) reported 27 cases of viral pneumonia with seven of them being critically ill. Most patients had a recent history of exposure to wildlife animals at the Huanan Seafood Wholesale Market in Wuhan, China, where poultry, snake, bats, and other farm animals were also sold.
This was identified to be caused by a new type of coronavirus, tentatively named 2019-nCoV by the World Health Organization (WHO). The pandemic is escalating rapidly. We searched the associated literature in both Chinese and English to summarize virology, epidemiology information; to calculate the mean doubling time value; to compare two guidelines of 2019-nCoV management (the WHO guideline and the Chinese 4th edition guideline which is currently being used).
Virology
2019-nCoV is the seventh member of the family of coronaviruses that infect humans, after MERS-nCoV and SARS-nCoV. Through genome sequencing, the genetic sequence of the 2019-nCoV became available to the WHO, which enabled different laboratories to produce reverse-transcription diagnostic polymerase chain reaction (RT-PCR) test specifically for detection of viral RNA. The 2019-nCoV is a β CoV of group 2B with over 70% similarity in genetic sequence to SARS-nCoV [1].
The source of the new coronavirus infection has been determined as bats. With full-length genome sequences, Zhou and colleagues found that 2019-nCoV is 96% identical at the whole-genome level to a bat coronavirus [2]. Wu and colleagues performed phylogenetic analysis on the complete viral genome and deduced that the virus was most closely related to a group of SARS-like coronavirus previously sampled from bats in China [3]. Ji and colleagues performed comprehensive sequence analysis and comparison in conjunction with relative synonymous codon usage (RSCU) bias among different animal species based on the 2019-nCoV RNA genome sequence, and the results showed the virus to be a recombinant virus between the bat coronavirus and another coronavirus with unknown origin. They also suggested that snake is the most probable animal reservoir due to the virus’s RSCU bias being closest to snake [4]. Zhu and colleagues used deep learning algorithms to analyze the gene sequences of novel coronaviruses and other coronaviruses to predict potential viral hosts. Their results indicated that bats and minks may be the two potential hosts of the novel coronavirus, while minks may be the intermediate hosts of the virus [5]. The novel coronavirus showed a similar pattern of infection to other coronaviruses in humans, particularly severe acute respiratory syndrome coronavirus (SARS-nCoV), Bat SARS-like CoV, and Middle East respiratory syndrome coronavirus (MERS-nCoV). After comparing coronaviruses in other vertebrates, the study found that the bat coronaviruses had the most similar infection patterns to the novel coronaviruses. After comparing the infection patterns of other vertebrate coronavirus hosts, the infection patterns of minks were found to be most similar to those of the novel coronavirus.
By modelling the spike protein of the receptor for 2019-nCoV, Xu and colleagues reported that angiotensin-converting enzyme 2 (ACE2) could be the receptor for this virus [6]. Similarly, ACE2 is also the receptor for SARS-nCoV and NL63 [7–9]. According to their model, the binding strength between 2019-nCoV and ACE2 is higher than the threshold required for virus infection, albeit being weaker than that between SARS-nCoV and ACE2. Zhou and colleagues conducted virus infectivity studies and showed that ACE2 is essential for 2019-nCoV to enter HeLa cells [10]. These data indicated that ACE2 is likely to be the receptor for 2019-nCoV. Zhao and colleagues analyzed normal lung tissue cells of eight healthy individuals, and found that the only Asian donor has over five times as much ACE2 expressing cell ratio than white and African American donors [11]. These results point to a possible heightened susceptibility of Asian population, although more evidence is needed to draw such conclusion.
Epidemiology
A total of 515 environment samples were collected from businesses related to the patients and their neighborhood on 1st January 2020 and transported to Institute of Viral Disease, Chinese Center for Disease Control and Prevention (CCDC) for testing. On 12th January 2020, 70 more samples from wildlife shops in the seafood market were collected for testing. PCR testing results showed that out of the 585 samples, 33 were tested positive to contain 2019-nCoV, and the virus was successfully isolated from positive samples, suggesting that the virus originated from wildlife animals sold in the seafood market in southern China [12]. However, this idea was challenged by a Lancet report detailing the first 41 infected patients who were hospitalized between 16th December 2019 and 2nd January 2020 [13], which stated “No epidemiological link was found between the first patient and later cases”. Their data also showed that, in total, 13 of the 41 cases had no link to the marketplace. Speaking to Science, Daniel Lucey from Georgetown University noted that since the virus seems to have an incubation period of up to 14 days and the first reported case emerged on 1st December 2019, it is possible that the initial human infection took place in November if not earlier. If so, the virus possibly spread silently between people in Wuhan before the cluster of cases from Huanan Seafood Wholesale Market was discovered in late December [14, 15]. Tracing the source of the virus, controlling the source and clarifying the intermediate host of the virus are the key links to control the continuous transmission of the virus from animals to people. Work is currently underway to determine possible virus reservoirs.
Person-to-person transmission of the coronavirus was confirmed by Chan and colleagues, who reported a case of five patients in a family cluster [16]. The estimates for reproduction number R0 differ between different research teams and are constantly updated as more information comes to light. WHO has published their estimation of R0 to be 1.4–2.5 using early information. Jonathan Read and colleagues from Lancaster University fitted a deterministic Susceptible-Exposed-Infected-Recovered (SEIR) metapopulation transmission model of infection within and between major Chinese cities to the daily number of confirmed cases of 2019-nCoV in Chinese cities and cases reported in other countries/regions, using an assumption of Poisson-distributed daily time increments. They determined the R0 to be around 3.1 [17]. Majumder and colleagues at Boston Children’s Hospital used Incidence Decay and Exponential Adjustment (IDEA) model to estimate R0 to be between 2.0 and 3.3 [18]. A large group of researchers from multiple institutes led by Jianhong Wu from York University proposed a more general deterministic SEIR compartmental model using more parameters, and arrived at a much higher R0 number of 6.47 [19]. Li and colleagues analyzed data on the first 425 confirm cases in Wuhan and found that R0 to be 2.2, without specifying their modelling method [15]. Table Table11 compares the R0 values from studies conducted by different groups.
Table 1
R0 Estimations from different groups
According to National Health Commission in China [24], 9692 confirmed cases, 15,238 suspected cases, 213 deaths and 171 cures have been announced as on 31st January 2020. The number of confirmed cases has surpassed SARS in 2003. The actual number of cases is likely to be much higher as the confirmation is severely limited by the number of PCR test kits as well as staff available in each hospital. Figure 1a traces the number of confirmed cases, suspected cases and deaths and cured in China over time, with data taken from the past daily statements of National Health Commission [24]. Figure 1b shows that the virus is spreading at an exponential speed after 16th January 2020, evident from the number of confirmed cases increases linearly with log scale. Using a single-term exponential model, we yielded a high R2 value of 0.95. The exponent is 0.38, meaning that the infected population doubles in size around every 1.8 days. A divergence from the exponential fit is observed at the data point on the 31st January 2020, and we expect further divergence in the future, due to the effect of the new quarantine measures starting to take place.
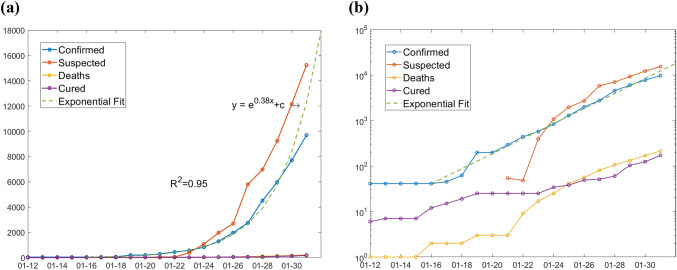
Number of confirmed cases, suspected cases, deaths, and cure in China over time. a Normal y-axis. b log-scale y-axis
Currently (31st January 2020), the virus has been spread to 17 other countries [25], with number of confirmed cases: Thailand (14), Japan (11), Singapore (10), Australia (9), Malaysia (8), USA (6), France (5), Germany (5), Korea (4), United Emirates (4), Canada (3), Vietnam (2), Nepal (1), Finland (1), Sri Lanka (1), India (1), and Cambodia (1). Using back-calculation method, Nishiura has estimated the cumulative incidence in China in real time, allowing us to update and discuss the extent of transmission at the source [26].
All age groups can be infected. According to Bin Cao, the Executive vice President at the Institute of Respiratory Medicine, Chinese Academy of Medical Sciences, 72% confirmed infection cases are aged 40 and above, 64% are male. 40% patients also have other underlying diseases such as diabetes and high blood pressure [27].
Modeling the spread
Lauren Gardner from Johns Hopkins University led a team of researchers to model the real-time spread of the coronavirus. The team's new analysis was based on a model, the outbreak boundary control decision support framework, released last December, which integrates the dynamics of the outbreak and outbreak control of the new coronavirus pneumonia into a decision support tool to facilitate border control in the early stages of an outbreak to mitigate further spread. The team used a random set of population epidemic simulation tools to simulate the dynamics of the epidemic, and considered the border protection mechanism (immigration inspection) in the modeling process, which is mainly used to identify infected people or high-risk groups [23]. The aggregation population model is mainly constructed based on the population network, which is divided into urban and intercity parts, and the edge of the network is the air line between different cities. At each node of the network, the researchers used a discrete-time Susceptible-Exposed-Infected-Recovered (SEIR) model to simulate the dynamics of an outbreak.
The researchers were able to observe a lot of interesting information from the model, which ran from the start of the outbreak until 25th January. Specifically, the researchers estimated that as of 25th January, 40 cases of 2019-NCoV had been exported from China. At the same time, the team estimated that the number of 2019-nCoV cases in China may have been much higher than reported for the whole of January, up to about 20,000 cases of 2019-nCoV in the country as of 25th January 25 (the number reported at the time was nearly 2000). Researchers also estimated that hundreds of people in Wuhan were infected in early December. The model is, however, limited by many factors, as explained by the team on their blog post. They are primarily due to the numbers being used are conservative estimates, the transmission of 2019-nCoV, such as the R0 value and incubation period, being uncertain, asymptomatic infections are not covered and only air travel was included [23].
Clinical guidelines
Severity definitions
We compare the severity definitions between the WHO [28] and Chinese 4th edition guidelines [29]. The categories of the severity of 2019-nCoV infection are very different in two guidelines. The WHO guideline shows five levels of severity: mild, severe, acute respiratory distress, sepsis, and septic shock. It covers both the adult and child age groups. The children one is from < 2 months to 5 years old. From mild to acute respiratory distress levels, the respiratory rate and SpO2 are two important parameters for judging patients’ clinical condition. For sepsis in adults, the patients’ mental, circulating, and respiratory parameters are recommended to rank the severity; while in children, the definition of the systemic inflammatory response syndrome (SIRS) are used. In the septic shock adult patients, hypotension in adults is a substantial sign or vasopressor maintenance for mean atrial pressure ≥
2 months to 5 years old. From mild to acute respiratory distress levels, the respiratory rate and SpO2 are two important parameters for judging patients’ clinical condition. For sepsis in adults, the patients’ mental, circulating, and respiratory parameters are recommended to rank the severity; while in children, the definition of the systemic inflammatory response syndrome (SIRS) are used. In the septic shock adult patients, hypotension in adults is a substantial sign or vasopressor maintenance for mean atrial pressure ≥ 65 mmHg with lactate level >
65 mmHg with lactate level > 2 mmol/L. In the septic shock for children, the criteria are based on the guideline of hemodynamic support of paediatric and neonatal Septic Shock from the American College of Critical Care Medicine [30].
2 mmol/L. In the septic shock for children, the criteria are based on the guideline of hemodynamic support of paediatric and neonatal Septic Shock from the American College of Critical Care Medicine [30].
The Chinese 4th edition defined three levels of severity: mild, severe, and life-threatening. The parameters are simpler than those of the WHO. Mild category is without any particular parameters; respiratory rate and SpO2 are recommended for severe-level evaluation, and it is similar to the parameters for mild-to-acute respiratory distress levels in the WHO guideline. Life-threatening level is considered when patients need mechanical ventilation, or presents as shock or multiple organ dysfunction syndrome, or requires intensive-care unit admission (Table (Table22).
Table 2
Summary of severity
| Summary of the definitions for severity of 2019-CoV in two guidelines | ||||
|---|---|---|---|---|
| Severity category in WHO guideline | Definition for adults in WHO guideline | WHO definition for children | Severity category in the Chinese 4th edition guideline | Definition in the Chinese 4th edition guideline |
| Mild | Patient with pneumonia and no signs of severe pneumonia | Child with non-severe pneumonia has cough or difficulty breathing + fast breathing: fast breathing (in breaths/min): < 2 months, ≥ 2 months, ≥ 60; 2–11 months, ≥ 60; 2–11 months, ≥ 50; 1–5 years, ≥ 50; 1–5 years, ≥ 40 and no signs of severe pneumonia 40 and no signs of severe pneumonia | Mild | Patient can present as common symptoms: fever, dry cough, fatigue, headache, sore throat |
| Severe | Adolescent or adult: fever or suspected respiratory infection, plus one of respiratory rate > 30 breaths/min, severe respiratory distress, or SpO2 < 30 breaths/min, severe respiratory distress, or SpO2 < 90% on room air 90% on room air | Child with cough or difficulty in breathing, plus at least one of the following: 1. Central cyanosis or SpO2 < 2. Severe respiratory distress 3. Signs of pneumonia with a general danger sign: inability to breastfeed or drink, lethargy or unconsciousness, or convulsions 4. Other signs of pneumonia may be present: chest in-drawing, fast breathing (in breaths/min): < 2–11 months, ≥ 1–5 years, ≥ | Severe | Patient who fits any one of the following condition: 1. Respiratory rate ≥ 2. SpO2 ≤ 3. PaO2/FiO2 ≤ |
| Acute respiratory distress | 1. Onset: new or worsening respiratory symptoms within one week of known clinical insult 2. Chest imaging (radiograph, CT scan, or lung ultrasound): bilateral opacities, not fully explained by effusions, lobar or lung collapse, or nodules 3. Origin of oedema: respiratory failure not fully explained by cardiac failure or fluid overload. Need objective assessment (e.g. echocardiography) to exclude hydrostatic cause of oedema if no risk factor present 4. Oxygenation Mild ARDS: 200 mmHg Moderate ARDS: 100 mmHg Severe ARDS: PaO2/FiO2 When PaO2 is not available, SpO2/FiO2 ≤ | 1. Child has the same symptoms as adults’ (left 1–3) 2. Bilevel NIV or CPAP ≥ Mild ARDS (invasively ventilated): 4 Moderate ARDS (invasively ventilated): 8 Severe ARDS (invasively ventilated): OI | Life-threatening | Patient fits any of the following conditions: 1. Patient presents respiratory distress and needs mechanical ventilation support 2. Patient presents shock 3. Patient presents MODS and needs ICU admission |
| Sepsis | Life-threatening organ dysfunction caused by a dysregulated host response to suspected or proven infection, with organ dysfunction Signs of organ dysfunction include: 1. Altered mental status 2. Difficult or fast breathing 3. Low oxygen saturation, reducedurine output 4. Fast heart rate, weak pulse 5. Cold extremities or low blood pressure, skin mottling 6. Or laboratory evidence of coagulopathy, thrombocytopenia, acidosis, high lactate or hyperbilirubinemia | Children: suspected or proven infection and ≥ 2 SIRS criteria, of which one must be abnormal temperature or white blood cell count 2 SIRS criteria, of which one must be abnormal temperature or white blood cell count | ||
| Septic shock | Patient persists hypotension despite volume resuscitation, requires vasopressors to maintain MAP ≥ 65 mmHg and serum lactate level > 65 mmHg and serum lactate level > 2 mmol/L 2 mmol/L | Patients presents any hypotension (SBP < 1. Altered mental state 2. Tachycardia or bradycardia (HR < 3. Prolonged capillary refill (> 4. Mottled skin or petechial or purpuric rash; increased lactate 5. Oliguria; hyperthermia or hypothermia | ||
ARI acute respiratory infection, BP blood pressure, bpm beats/minute, CPAP continuous positive airway pressure, FiO2 fraction of inspired oxygen, MAP mean arterial pressure, NIV non-invasive ventilation, SBP systolic blood pressure, SD standard deviation, SIRS systemic inflammatory response syndrome, SpO2 oxygen saturation, ARDS acute respiratory distress syndrome, HR heart rate, PaO2 partial press of oxygen, SBP systolic blood pressure, ICU intensive-care unit, MODS multiple organ dysfunction syndrome, OI Oxygenation Index, OSI Oxygenation Index
Management guidelines
In the WHO guideline, the oxygen and intravenous fluid treatments are recommended to mild and severe cases. The targets are SpO2 ≥
≥ 90% in non-pregnant adult or child, and SpO2
90% in non-pregnant adult or child, and SpO2 ≥
≥ 92–95% in pregnant patients. Mechanical ventilation is recommended in the both adults and children with acute respiratory distress syndrome. The tide volume is recommended from 6 ml/kg. Hypercapnia is acceptable and longer than 12 h ventilation per day is suggested to use in severe ARDS cases. The treatments of sepsis and septic shock are following the 2016 international guideline of sepsis and septic shock [31].
92–95% in pregnant patients. Mechanical ventilation is recommended in the both adults and children with acute respiratory distress syndrome. The tide volume is recommended from 6 ml/kg. Hypercapnia is acceptable and longer than 12 h ventilation per day is suggested to use in severe ARDS cases. The treatments of sepsis and septic shock are following the 2016 international guideline of sepsis and septic shock [31].
In the Chinese 4th edition, anti-virus medicine is recommended to use in the patient with 2019-nCoV infection. Mechanical ventilation is recommended to use in severe and life-threatening cases. Extracorporeal membrane oxygenation (ECMO) can be used to reduce pulmonary impairment during the treatment period (Table (Table33).
Table 3
Summary of managements
| Summary of the managements in two guidelines | ||||
|---|---|---|---|---|
| Adults (WHO) | Children (WHO) | Chinese 4th edition | ||
| Mild | 1. Oxygen therapy at 5 l/min and titrate flow rates to reach target SpO2 ≥ 2. Patients with 2019-nCoV infection should be treated cautiously with intravenous fluids | 1. Oxygen therapy at 5 l/min and the target SpO2 is ≥ 2. Patients with 2019-nCoV infection should be treated cautiously with intravenous fluids | Mild | 1. Rest and oxygen treatment 2. Anti-virus regimes: interferon nebuliser therapy and oral anti-virus medicine 3. Antibiotics can be used when bacteria infection is proved |
| Severe | 1. Oxygen therapy at 5 l/min and titrate flow rates to reach target SpO2 ≥ 2. Patients with 2019-nCoV infection should be treated cautiously with intravenous fluids | 1. Oxygen therapy at 5 l/min and the target SpO2 is ≥ 2. Patients with 2019-nCoV infection should be treated cautiously with intravenous fluids | Severe | Use the strategies above plus: 1. Non-invasive ventilation 2. Intubation if patients’ condition cannot improve after 2 h NIV or patient cannot tolerate NIV 3. Mechanical ventilation starts with low tide volume. ECOM can be used in necessity 4. Corticosteroid can be used in short term. The dosage of methylprednisolone is recommended no more than 2 mg/kg per day (or other corticosteroid equal to this) |
| Acute respiratory distress | Use the strategies above plus: 1. Patients with ARDS, especially young children or those who are obese or pregnant, need intubation. Pre-oxygenate with 100% FiO2 for 5 min, via a face mask with reservoir bag, bag-valve mask, HFNO, or NIV. Rapid sequence intubation is appropriate after an airway assessment that identifies no signs of difficult intubation 2. The initial tidal volume is 6 ml/kg PBW; tidal volume up to 8 ml/kg PBW is allowed if undesirable side effects occur (e.g. dyssynchrony, pH < 3. Ventilation for > | User the strategies above plus: 1. Oxygen therapy at 5 l/min and children with emergency signs (obstructed or absent breathing, severe respiratory distress, central cyanosis, shock, coma or convulsions) should receive oxygen therapy during resuscitation to target SpO2 ≥ 2. Patients who continue to have increased work of breathing or hypoxemia even when oxygen is delivered via a face mask with reservoir bag (flow rates of 10–15 l/min, which is typically the minimum flow required to maintain bag inflation; FiO2 0.60–0.95) usually requires intubation 3. The initial tidal volume of mechanical ventilation is 6 ml/kg PBW; tidal volume up to 8 ml/kg PBW is allowed if undesirable side effects occur (e.g. dyssynchrony, pH < 4. Ventilation for > | Life-threatening | Use the strategies above plus: 1. Non-invasive ventilation 2. Intubation if patients’ condition cannot improve after 2 h NIV or patient cannot tolerate NIV 3. Mechanical ventilation starts with low tide volume. ECOM can be used in necessity 4. Corticosteroid can be used in short term. The dosage of methylprednisolone is recommended no more than 2 mg/kg per day (or other corticosteroid equal to this) |
| Sepsis | Use the strategies above plus: 1. Administer appropriate empiric antimicrobials within 1 h of identification of sepsis 2. Patients with sepsis-induced respiratory failure without matching ARDS criteria still need mechanical ventilation | The same as left | ||
| Septic shock | Use the strategies above plus: 1. In resuscitation from septic shock in adults, give at least 30 ml/kg of isotonic crystalloid in adults in the first 3 h 2. Administer vasopressors when shock persists during or after fluid resuscitation. The initial blood pressure target is MAP ≥ | Use the strategies above plus: 1. In resuscitation from septic shock in children in well-resourced settings, give 20 ml/kg as a rapid bolus and up to 40–60 ml/kg in the first 1 h 2. Administer vasopressors when shock persists during or after fluid resuscitation. The initial blood pressure target is MAP ≥ | ||
ARI acute respiratory infection, BP blood pressure, bpm beats/minute, CPAP continuous positive airway pressure, FiO2 fraction of inspired oxygen, MAP mean arterial pressure, NIV non-invasive ventilation, SBP systolic blood pressure, SD standard deviation, SIRS systemic inflammatory response syndrome, SpO2 oxygen saturation, ARDS acute respiratory distress syndrome, HR heart rate, PaO2 partial press of oxygen, SBP systolic blood pressure, ICU intensive-care unit, MODS multiple organ dysfunction syndrome, ECOM extracorporeal membrane oxygenation, PBW predicted body weight
Discussion
How easily does 2019-nCoV spread, and how deadly is the virus? At the moment, we only have informed guesses, which are likely to solidify in the coming weeks and months. But what we know so far can shed some light on the characteristics of the virus, and offer some instructions on dealing with the rapidly growing pandemic. China’s health authorities and the government have been moving quickly. In response to the spreading virus, isolation strategy has been used. Many cities including Wuhan have been put on quarantine since 23rd January, 2020, when millions of Chinese traditionally travel due to Lunar New Year. Planes, trains, ferries, subways, and buses cease operation, and roads in and out of the cities were closed. Residents were encouraged to wear masks in public. Many places that usually attract a large crowd, such as cafes, bars, and cinemas in many cities, Disneyland in both Shanghai and Hongkong, Forbidden City in Beijing, are now closed until further notice. We will not know for some time the consequences of the quarantine measures.
Multiple research groups studying the disease around the world are providing different values on R0, using results obtained from their respective models. Morbidity varies in different environments, depending on factors like temperature, population density, and susceptibility to a disease in a population, so R0 would change accordingly over time. More reliable and accurate R0 value should appear as more information comes to light. We calculated that the number of confirmed infections after 16th January 2020 grows at an exponential rate, with a doubling time of 1.8 days. This result is significantly different from the doubling time of 7.4 days found in Li’s group, which was obtained from analyzing the cases before 4th January 2020. This might be due to several factors: at early stages, the lack of awareness for the disease and lack of detection methods would have hindered the disease detection and confirmation. Low number of confirmed cases would result in high uncertainty of the calculation. At later stages, the increase in availability of PCR test kits and other clinical resources would result in higher confirmation rate than the true value.
Virology results indicate that some Asian populations may potentially be more susceptible to 2019-nCoV than other races [6, 10, 11], which is consistent with the observation that disproportionally higher number of Asian populations is infected, even in an international metropolitan like Shanghai, although more evidence is needed to draw such conclusion. Chen and colleagues found a greater number of men than women in the 99 cases of 2019-nCoV which they reported. In previous SARS and MERS outbreaks, men were also more likely to be infected than women [32]. This may have to do with the important role that both woman's X chromosomes and sex hormones play in the body's immune system [33]. Their study also suggests that older men with chronic diseases are more likely to be infected with the new coronavirus because of their weakened immune system.
The major difference between the WHO [28] and Chinese 4th edition guideline [29] is the standard in treating children with 2019-nCOV infection. Until now, a few cases of children infected have been reported with the youngest one is 10 years old. ARDS is a common symptom in the 2019-nCoV infection cases. SpO2 and respiration rate check became very important in the clinical practice. Mechanical ventilation is a major treatment of it, and it has been recommended in both guidelines. The low tidal volume, plateau pressure limitation, no oscillatory ventilation, and prone position have been evidenced as high proof [34]. The anti-virus medicine is recommended in the Chinese 4th edition. A recent publication reported 99 cases in Jinyin-Tan hospital were given anti-virus medicine such as oseltamivir (75 mg every 12 h, orally), ganciclovir (0.25 g every 12 h, intravenously), and lopinavir and ritonavir tablets (500 mg twice daily, orally), and the influence of the outcome has been mentioned in detail [32]. Short-term corticosteroids use is recommended in the Chinese 4th edition, the aim of which is to reduce the self-damage by over-reactive immune response. Antibiotic use is recommended when the patient has evidence of bacterial infection. Some patients in the 99 cases presented a rapid progress to ARDS, and the benefits of short-term use of methylprednisolone 1–2 mg/kg per day and intravenous immunoglobulin were observed in these patients [32]. These two guidelines are currently being used; however, some of the contents are still controversial, especially the benefits of steroids and antibiotic. Further study should be continued in the clinical practice. Our summary of WHO guidelines just included recommended contents. The controversial contents are excluded.
Compliance with ethical standards
On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
Full text links
Read article at publisher's site: https://doi.org/10.1007/s15010-020-01401-y
Read article for free, from open access legal sources, via Unpaywall:
https://link.springer.com/content/pdf/10.1007/s15010-020-01401-y.pdf
Citations & impact
Impact metrics
Article citations
Exploring Prehospital Data for Pandemic Preparedness: A Western Brazilian Amazon Case Study on COVID-19.
Int J Environ Res Public Health, 21(9):1229, 18 Sep 2024
Cited by: 0 articles | PMID: 39338112 | PMCID: PMC11431530
COVID-19 burden in Iran: disability-adjusted life years analysis from hospital data, 2020-2021.
Arch Public Health, 82(1):135, 26 Aug 2024
Cited by: 0 articles | PMID: 39187892 | PMCID: PMC11346186
Lessons from the COVID-19 pandemic: the unequal burden of COVID-19 on vulnerable populations in the Brazilian Central-West.
Cad Saude Publica, 40(8):e00199623, 19 Aug 2024
Cited by: 0 articles | PMID: 39166560 | PMCID: PMC11338597
Intimate partner violence and associated factors among women during the COVID-19 pandemic in Ethiopia: a systematic review and meta-analysis.
Front Glob Womens Health, 5:1425176, 23 Aug 2024
Cited by: 0 articles | PMID: 39246731 | PMCID: PMC11377230
Review Free full text in Europe PMC
Characteristics and Outcomes of Coronavirus Disease- 2019 Among Pregnant Women in Saudi Arabia; a Retrospective Study.
Int J Womens Health, 16:475-490, 14 Mar 2024
Cited by: 1 article | PMID: 38501054 | PMCID: PMC10946403
Go to all (251) article citations
Other citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
The SARS-CoV-2 outbreak: What we know.
Int J Infect Dis, 94:44-48, 12 Mar 2020
Cited by: 538 articles | PMID: 32171952 | PMCID: PMC7102543
Review Free full text in Europe PMC
COVID-19: a conundrum to decipher.
Eur Rev Med Pharmacol Sci, 24(10):5830-5841, 01 May 2020
Cited by: 8 articles | PMID: 32495923
A Practical Approach to the Management of Cancer Patients During the Novel Coronavirus Disease 2019 (COVID-19) Pandemic: An International Collaborative Group.
Oncologist, 25(6):e936-e945, 27 Apr 2020
Cited by: 372 articles | PMID: 32243668 | PMCID: PMC7288661
Review Free full text in Europe PMC
The First 75 Days of Novel Coronavirus (SARS-CoV-2) Outbreak: Recent Advances, Prevention, and Treatment.
Int J Environ Res Public Health, 17(7):E2323, 30 Mar 2020
Cited by: 104 articles | PMID: 32235575 | PMCID: PMC7177691
Review Free full text in Europe PMC

 1,2,3 and
1,2,3 and 



