Abstract
Background
Long-term care facilities are high-risk settings for severe outcomes from outbreaks of Covid-19, owing to both the advanced age and frequent chronic underlying health conditions of the residents and the movement of health care personnel among facilities in a region.Methods
After identification on February 28, 2020, of a confirmed case of Covid-19 in a skilled nursing facility in King County, Washington, Public Health-Seattle and King County, aided by the Centers for Disease Control and Prevention, launched a case investigation, contact tracing, quarantine of exposed persons, isolation of confirmed and suspected cases, and on-site enhancement of infection prevention and control.Results
As of March 18, a total of 167 confirmed cases of Covid-19 affecting 101 residents, 50 health care personnel, and 16 visitors were found to be epidemiologically linked to the facility. Most cases among residents included respiratory illness consistent with Covid-19; however, in 7 residents no symptoms were documented. Hospitalization rates for facility residents, visitors, and staff were 54.5%, 50.0%, and 6.0%, respectively. The case fatality rate for residents was 33.7% (34 of 101). As of March 18, a total of 30 long-term care facilities with at least one confirmed case of Covid-19 had been identified in King County.Conclusions
In the context of rapidly escalating Covid-19 outbreaks, proactive steps by long-term care facilities to identify and exclude potentially infected staff and visitors, actively monitor for potentially infected patients, and implement appropriate infection prevention and control measures are needed to prevent the introduction of Covid-19.Free full text

Epidemiology of Covid-19 in a Long-Term Care Facility in King County, Washington
Abstract
Background
Long-term care facilities are high-risk settings for severe outcomes from outbreaks of Covid-19, owing to both the advanced age and frequent chronic underlying health conditions of the residents and the movement of health care personnel among facilities in a region.
Methods
After identification on February 28, 2020, of a confirmed case of Covid-19 in a skilled nursing facility in King County, Washington, Public Health–Seattle and King County, aided by the Centers for Disease Control and Prevention, launched a case investigation, contact tracing, quarantine of exposed persons, isolation of confirmed and suspected cases, and on-site enhancement of infection prevention and control.
Results
As of March 18, a total of 167 confirmed cases of Covid-19 affecting 101 residents, 50 health care personnel, and 16 visitors were found to be epidemiologically linked to the facility. Most cases among residents included respiratory illness consistent with Covid-19; however, in 7 residents no symptoms were documented. Hospitalization rates for facility residents, visitors, and staff were 54.5%, 50.0%, and 6.0%, respectively. The case fatality rate for residents was 33.7% (34 of 101). As of March 18, a total of 30 long-term care facilities with at least one confirmed case of Covid-19 had been identified in King County.
Conclusions
In the context of rapidly escalating Covid-19 outbreaks, proactive steps by long-term care facilities to identify and exclude potentially infected staff and visitors, actively monitor for potentially infected patients, and implement appropriate infection prevention and control measures are needed to prevent the introduction of Covid-19.
On December 31, 2019, China reported a cluster of pneumonia cases of unknown cause that would later be identified as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1-3 Patients with the illness, called coronavirus disease 2019 (Covid-19), frequently present with fever, cough, and shortness of breath within 2 to 14 days after exposure.4 As of March 23, 2020, there had been 332,930 confirmed cases of Covid-19 reported globally, and 14,510 deaths had been reported.5 In recognition of the widespread global transmission of Covid-19, the World Health Organization declared Covid-19 to be a pandemic on March 11, 2020.6 The first case of Covid-19 in the United States was diagnosed on January 20, 2020, in Snohomish County, Washington, in a person who had recently traveled to Wuhan, China.7
On February 28, Public Health–Seattle and King County (PHSKC) was notified of a positive Covid-19 test result from a patient who had been admitted to a local hospital and tested on the basis of newly revised testing criteria from the Centers for Disease Control and Prevention (CDC).8 The patient resided in Facility A, a skilled nursing facility with approximately 130 facility residents and 170 staff. When the initial case was confirmed on February 28, 2020, PHSKC and the CDC immediately began case investigation, contact tracing, quarantine of exposed persons, isolation of persons with confirmed or suspected Covid-19, and on-site enhancement of infection prevention and control. Some of the information obtained through the investigation was rapidly reported through a Morbidity and Mortality Weekly Report.9
Case Report
On February 27, 2020, PHSKC was notified of a 73-year-old woman with cough, fever, and shortness of breath who resided in Facility A, in which a cluster of unexplained febrile respiratory illness was occurring. The index patient had symptom onset on February 19 and worsening respiratory status requiring supplemental oxygen for 5 days before she was transferred to a local hospital on February 24, 2020. At the hospital, she was found to be febrile (temperature as high as 39.6°C), with tachycardia, tachypnea, and hypoxemia (oxygen saturation, 83% while she was breathing ambient air). She became more hypoxemic over the next 24 hours, despite bilevel positive airway pressure (BiPAP), and was intubated on February 25, 2020, because of respiratory failure. A computed tomographic (CT) scan of the chest revealed diffuse bilateral pulmonary infiltrates. Her medical history included insulin-dependent type II diabetes mellitus, obesity, chronic kidney disease, hypertension, coronary artery disease, and congestive heart failure. She had no known travel or contact with persons known to have Covid-19.
Multiplex viral respiratory panel and bacterial cultures (sputum and bronchoalveolar lavage) were unrevealing. The CDC testing criteria for Covid-19 had been recently revised to include severely ill persons for whom no cause had been identified.10 On February 27, an astute clinician requested Covid-19 testing on the basis of the new CDC criteria allowing testing in cases of severe, unexplained pneumonia despite the lack of an epidemiologic link and obtained nasopharyngeal and oropharyngeal swabs and a sputum specimen to test for SARS-CoV-2 by real-time reverse-transcriptase polymerase chain reaction (rRT-PCR). On February 28, 2020, results were positive, 9 days after symptom onset and 4 days after hospital admission. The patient died on March 2, 2020.
Methods
In response to the travel-associated case of Covid-19 in neighboring Snohomish County, PHSKC activated its emergency response on January 20, 2020, and began active surveillance for Covid-19, focused on identifying cases of suspected and confirmed Covid-19 and tracing contacts. PHSKC collects data on demographics, clinical status, and results of laboratory testing gathered from Covid-19 case investigations into its local surveillance database and analyzes these data in combination with laboratory records and case reports obtained from the Washington Disease Reporting System.
On receiving notification on February 28 of the Covid-19 diagnosis for the index patient, who was a resident of Facility A, PHSKC immediately began an investigation of the cluster of Covid-19–like illness that was occurring in this facility. A CDC field team arrived on March 1, at the request of PHSKC, to assist with the investigation. Facility residents, visitors, and health care personnel with confirmed Covid-19 were interviewed by telephone to collect information on symptoms, severity, coexisting conditions, travel history, and close contacts with known Covid-19. Guidance related to self-isolation, self-quarantine, and testing for symptomatic close contacts was provided during interviews, as appropriate. If a case patient was unable to be interviewed (e.g., because the patient had been intubated), a proxy was asked to provide as many details as possible. Medical chart abstractions were performed to confirm information about underlying health conditions among facility residents with Covid-19.
Specimen collection and diagnostic testing were conducted in accordance with CDC guidelines.11 In brief, upper respiratory specimens (nasopharyngeal and oropharyngeal swabs) were collected with synthetic fiber swabs. Each swab was stored in a sterile tube with viral transport media between 2°C and 8°C before being transported to the Washington Department of Health Public Health Laboratory for diagnostic testing. Sputum was collected only when the person had a productive cough or when clinically indicated. Diagnostic testing was done in accordance with the CDC’s SARS-CoV-2 rRT-PCR panel for detection of SARS-CoV-2.12-14
As part of the intensive response, at least 100 long-term care facilities in King County were contacted by email on March 6, 2020, through a REDCap survey that was used to obtain information on residents or staff known to have Covid-19 or on clusters of influenza-like illness among residents and staff. Nonresponders were sent up to five reminders to complete the survey.15 In addition, countywide databases that capture all emergency medical service transfers from long-term care facilities to acute care facilities were reviewed on a daily basis for evidence of cases or clusters of influenza-like illness. Finally, routine passive surveillance for influenza-like illness clusters in long-term care facilities was used to identify possible Covid-19; reporting is mandated for a confirmed case of influenza or for two or more cases of influenza-like illness in a 72-hour period. All long-term care facilities with evidence of a cluster of respiratory illness were contacted by telephone for additional information, including information on infection-control strategies that were in place and on personal protective equipment (PPE) supplies. On the basis of this information, the long-term care facilities were prioritized according to risk of Covid-19 introduction, and the highest-priority facilities were visited by response personnel to perform diagnostic testing of those with influenza-like illness and to implement infection-control assessment, training, and support.
Results
On February 28, 2020, four cases of Covid-19 were confirmed among residents of King County; 1 person had presumed travel-related exposure, and 3 were identified by testing hospitalized patients who had severe respiratory illness (e.g., pneumonia) and who had tested negative for influenza and other respiratory pathogens. One of these was the index patient from Facility A; one was a Facility A staff member. When the index case was identified on February 28, at least 45 residents and staff dispersed across Facility A had symptoms of respiratory illness; PHSKC was notified of this increase by the facility on February 27.
As of March 18, a total of 167 persons with Covid-19 that was epidemiologically linked to Facility A had been identified (Figure 1); 144 were residents of King County and 23 were residents of Snohomish County. Cases of Covid-19 occurred among facility residents (101 persons), health care personnel (50), and visitors (16) (Table 1). Among facility residents, 118 were tested; 101 results were positive and 17 negative. Most affected persons had respiratory illness consistent with Covid-19; however, chart review of facility residents found that in 7 cases no symptoms had been documented. Clinical presentation ranged from mild (no hospitalization) to severe, including 35 deaths by March 18. Reported dates of symptom onset ranged from February 15 to March 13. The median age of the patients was 83 years (range, 51 to 100) among facility residents, 62.5 years (range, 52 to 88) among visitors, and 43.5 years (range, 21 to 79) among facility personnel; 112 patients (67.1%) were women (Table 1). The hospitalization rates for residents, visitors, and staff were 54.5%, 50.0%, and 6.0%, respectively. As of March 18, the preliminary case fatality rate was 33.7% for residents and 6.2% for visitors; no staff members had died. Most (94.1% of 101) facility residents had chronic underlying health conditions, with hypertension (67.3%), cardiac disease (60.4%), renal disease (40.6%), diabetes mellitus (31.7%), pulmonary disease (31.7%), and obesity (30.7%) being most common. Of the coexisting conditions evaluated, hypertension was the only underlying condition present in 7 facility residents with Covid-19. The 50 health care personnel with confirmed Covid-19 worked in the following occupational categories: physical therapist, occupational therapist assistant, speech pathologist, environmental care (housekeeping, maintenance), nurse, certified nursing assistant, health information officer, physician, and case manager.

Shown are cases of Covid-19 in Washington that had been epidemiologically linked to Facility A as of March 18, 2020.
Table 1
| Characteristic | Residents (N=101) | Health Care Personnel (N=50) | Visitors (N=16) | Total (N=167) |
|---|---|---|---|---|
| Median age (range) — yr | 83 (51–100) | 43.5 (21–79) | 62.5 (52–88) | 72 (21–100) |
| Sex — no. (%) | ||||
| Male | 32 (31.7) | 12 (24.0) | 11 (68.8) | 55 (32.9) |
| Female | 69 (68.3) | 38 (76.0) | 5 (31.2) | 112 (67.1) |
| Hospitalized — no. (%) | ||||
| Yes | 55 (54.5) | 3 (6.0) | 8 (50.0) | 66 (39.5) |
| No | 9 (8.9) | 44 (88.0) | 8 (50.0) | 61 (36.5) |
| Unknown | 37 (36.6) | 3 (6.0) | 0 | 40 (24.0) |
| Died — no. (%) | ||||
| Yes | 34 (33.7) | 0 | 1 (6.2) | 35 (21.0) |
| No | 67 (66.3) | 50 (100.0) | 15 (93.8) | 132 (79.0) |
| Chronic underlying conditions — no. (%)† | ||||
| Hypertension‡ | 68 (67.3) | 4 (8.0) | 2 (12.5) | 74 (44.3) |
| Cardiac disease | 61 (60.4) | 4 (8.0) | 3 (18.8) | 68 (40.7) |
| Renal disease | 41 (40.6) | 0 | 2 (12.5) | 43 (25.7) |
| Diabetes mellitus | 32 (31.7) | 5 (10.0) | 1 (6.2) | 38 (22.8) |
| Obesity | 31 (30.7) | 3 (6.0) | 3 (18.8) | 37 (22.2) |
| Pulmonary disease | 32 (31.7) | 2 (4.0) | 2 (12.5) | 36 (21.6) |
| Cancer | 15 (14.9) | 0 | 0 | 15 (9.0) |
| Compromised immune system | 9 (8.9) | 0 | 0 | 9 (5.4) |
| Liver disease | 6 (5.9) | 0 | 0 | 6 (3.6) |
Through ongoing surveillance and outreach to provide technical assistance with infection prevention and control to long-term care facilities (e.g., nursing homes, assisted living), a total of 30 King County facilities with at least one confirmed Covid-19 case, including Facility A, were identified by March 18. Of the first 8 facilities affected after Facility A, at least 3 had clear epidemiologic links to Facility A (Figure 2). Two of the facilities with definitive epidemiologic links had staff working both at that facility and at Facility A; the third facility had received two patient transfers from Facility A. Information received from surveys of long-term care facilities and on-site visits identified factors that were likely to have contributed to the vulnerability of these facilities, including staff who had worked while symptomatic; staff who worked in more than one facility; inadequate familiarity with and adherence to PPE recommendations; challenges to implementing proper infection control practices, including inadequate supplies of PPE and other items (e.g., alcohol-based hand sanitizer); delayed recognition of cases because of a low index of suspicion; limited availability of testing; and difficulty identifying persons with Covid-19 on the basis of signs and symptoms alone. Examples of specific PPE challenges included an initial lack of available eye protection, frequent changes in PPE types because supply chains were disrupted and PPE was being obtained through various donations or suppliers, and a need for a designated staff member to observe PPE use to ensure that staff were consistent with safe PPE handling (e.g., not touching or adjusting face protection, primarily face masks, during extended use). Working collaboratively, state and local health departments and CDC staff provided five focused PPE trainings for facility staff, including donning and doffing demonstrations and practice, and three additional basic infection control visits, including hand hygiene assessments, audits of PPE use, and reviews of environmental cleaning and disinfection practices.
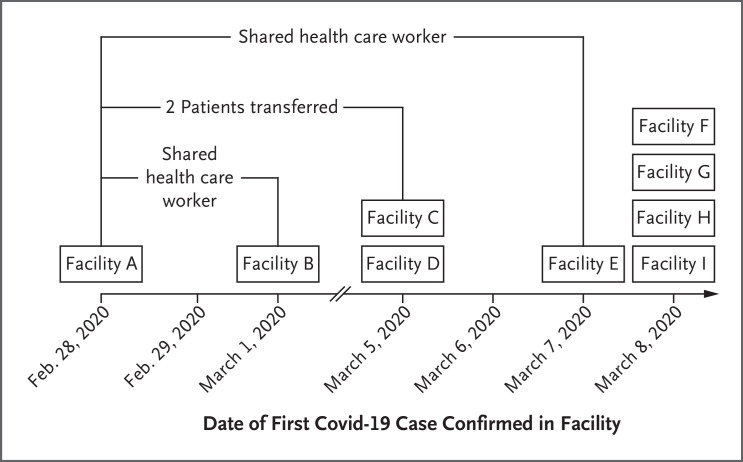
The first nine long-term care facilities (e.g., nursing homes or assisted living facilities) in King County with one or more confirmed cases of Covid-19 are shown according to the date of the first confirmed case. Facilities are those identified as of March 9, 2020. The direction of potential introduction of Covid-19 from one facility to another is unknown.
Discussion
The vulnerability of long-term care facilities to respiratory disease outbreaks, including influenza and other commonly circulating human coronaviruses such as the common cold, is well recognized.16,17 As this report shows, the spread of Covid-19 reflected the same vulnerability in at least one long-term care facility. In total, 167 confirmed cases of Covid-19 had been identified among residents, personnel, and visitors as of March 18, and 30 skilled nursing and assisted living facilities in King County had identified at least one confirmed case of Covid-19. Staff working in multiple facilities while ill and transfers of patients from one facility to another potentially introduced Covid-19 into some of these facilities. The transmission within Facility A and to other facilities in the area posed a serious threat to the medically vulnerable population residing within long-term care facilities and strained the local acute care hospitals. Although the use of vaccine and antiviral medications can be effective in reducing the spread of influenza in long-term care facilities, such interventions are not currently available for Covid-19.18 Residents and health care personnel at long-term care facilities are at risk for Covid-19 transmission and severe outcomes, particularly for residents who are predominantly at advanced ages and have underlying medical conditions. Publicly available information on staffing and quality measures shows no indication that baseline practices at Facility A placed residents at greater risk than residents at other similar facilities.
This investigation had a number of limitations. Not all residents and staff were interviewed and tested for SARS-CoV-2, which might have led to under-ascertainment of infections, particularly for those who were presymptomatic or asymptomatic. For example, at another facility (Facility B) that had a subsequent Covid-19 outbreak epidemiologically linked to Facility A, swabbing of all residents revealed that infections with low cycle threshold values (indicating a large quantity of viral RNA) occurred among some residents who did not have symptoms.19 There was not a complete roster of visitors to Facility A, and it is possible that some infections among visitors were also missed by these surveillance and investigation efforts. Because symptom onset dates were not available in many cases, the epidemic curve is presented by date of report; however, this does not adequately represent the timing of disease onset in the facility, given that the median time from symptom onset to diagnosis in this cohort was 8 days but had considerable variability. Finally, case ascertainment and testing ramped up after the outbreak was recognized at Facility A, but there could have been infections and transmission at other facilities in the area earlier.
On March 10, 2020, the governor of Washington implemented mandatory screening of health care workers and visitor restrictions for all licensed nursing homes and assisted living facilities.20 These strategies are coordinated and supported by public health authorities, partnering health care systems, regulatory agencies, and their respective governing bodies.20-23 Local and state authorities strengthened prevention and mitigation strategies targeting transmission of Covid-19 and other respiratory viruses in long-term care facilities that include screening and restricted access policies for visitors and nonessential personnel; screening of health care personnel, including measurement of body temperature and interviewing for presence of respiratory symptoms, to identify and exclude symptomatic workers; strategies for close clinical monitoring of residents; social distancing, including restricting resident movement and group activities; staff training on infection prevention and control and PPE use; and establishment of plans for county and state coordination of needs and contingency plans for acquiring PPE in anticipation of delays or interruptions in supply.20,22,24,25 In addition to education, hands-on training, and maintaining adequate supplies, facilities need to reinforce staff adherence to infection prevention and control practices with regular auditing and feedback from observation of staff workflow. Substantial disruptions, such as staff absenteeism and increased workload, may affect the consistency with which these practices are implemented and monitored. The impact of these policies in protecting long-term care facilities should continue to be evaluated, along with the role of serial testing strategies to identify infected staff or patients as testing reagents and supplies become more available.
The experience described here indicates that outbreaks of Covid-19 in long-term care facilities can have a considerable impact on vulnerable older adults and local health care systems. The findings also suggest that once Covid-19 has been introduced into a long-term care facility, it has the potential to spread rapidly and widely. This can cause serious adverse outcomes among facility residents and staff, which underscores the importance of proactive steps to identify and exclude potentially infected staff and visitors, early recognition of potentially infected patients, and implementation of appropriate infection prevention and control measures.21-24,26 Lessons learned from this initial cluster can provide valuable guidance for long-term care facilities in other parts of the United States.
Acknowledgments
We thank the facility residents; the staff of Facility A for their ongoing efforts to provide care in the face of these challenges; staff at the local and state health departments responding to this public health emergency; staff at the Washington State Department of Health Public Health Laboratories and at the CDC Laboratories for their dedication; the acute care hospitals and their staff who have provided and continue to provide care for those affected by COVID-19; CDC staff at the Emergency Operations Center; and members of the Covid-19 response teams at the local, state, and national levels for their unwavering commitment in the face of this global public health emergency.
Notes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
This article was published on March 27, 2020, at NEJM.org.
A data sharing statement provided by the authors is available with the full text of this article at NEJM.org.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
Full text links
Read article at publisher's site: https://doi.org/10.1056/nejmoa2005412
Read article for free, from open access legal sources, via Unpaywall:
https://www.nejm.org/doi/pdf/10.1056/NEJMoa2005412
Citations & impact
Impact metrics
Article citations
Spatiotemporal Cluster Detection for COVID-19 Outbreak Surveillance: Descriptive Analysis Study.
JMIR Public Health Surveill, 10:e49871, 16 Oct 2024
Cited by: 0 articles | PMID: 39412839 | PMCID: PMC11525083
Clinical characteristics, treatment, and outcomes for elderly patients in a dedicated Covid-19 ward at a primary health care facility in western Norway: a retrospective observational study.
BMC Health Serv Res, 24(1):1098, 19 Sep 2024
Cited by: 0 articles | PMID: 39300524 | PMCID: PMC11414310
SARS-CoV-2 Seropositivity in Nursing Home Staff and Residents during the First SARS-CoV-2 Wave in Flanders, Belgium.
Viruses, 16(9):1461, 14 Sep 2024
Cited by: 0 articles | PMID: 39339937 | PMCID: PMC11437469
A comparison of COVID-19 and post-COVID-19 syndrome among symptomatic and asymptomatic patients in Bangladesh: A retrospective cohort study.
Heliyon, 10(16):e36202, 15 Aug 2024
Cited by: 0 articles | PMID: 39258212 | PMCID: PMC11386022
COVID-19 in nursing homes: Geographic diffusion and regional risk factors from January 1 to July 26, 2020 of the pandemic.
PLoS One, 19(8):e0308339, 15 Aug 2024
Cited by: 0 articles | PMID: 39146332 | PMCID: PMC11326555
Go to all (727) article citations
Other citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Asymptomatic and Presymptomatic SARS-CoV-2 Infections in Residents of a Long-Term Care Skilled Nursing Facility - King County, Washington, March 2020.
MMWR Morb Mortal Wkly Rep, 69(13):377-381, 03 Apr 2020
Cited by: 629 articles | PMID: 32240128 | PMCID: PMC7119514
COVID-19 in a Long-Term Care Facility - King County, Washington, February 27-March 9, 2020.
MMWR Morb Mortal Wkly Rep, 69(12):339-342, 27 Mar 2020
Cited by: 216 articles | PMID: 32214083 | PMCID: PMC7725515
Universal and Serial Laboratory Testing for SARS-CoV-2 at a Long-Term Care Skilled Nursing Facility for Veterans - Los Angeles, California, 2020.
MMWR Morb Mortal Wkly Rep, 69(21):651-655, 29 May 2020
Cited by: 80 articles | PMID: 32463809 | PMCID: PMC7269604
Surgical Infection Society Guidance for Operative and Peri-Operative Care of Adult Patients Infected by the Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2).
Surg Infect (Larchmt), 21(4):301-308, 20 Apr 2020
Cited by: 29 articles | PMID: 32310715
Review






