Abstract
Free full text

COVID-19 and intracerebral haemorrhage: causative or coincidental?
Abstract
Pneumonia appears to be the most common manifestation of coronavirus disease 2019 (COVID-19), but some extrapulmonary involvement, such as gastrointestinal, cardiac and renal, has been reported. The limited clinical data about the virus's behavior to date, especially extrapulmonary symptoms, suggest that we should be aware of the possibility of initial cerebrovascular manifestations of COVID-19.
Pneumonia appears to be the most common manifestation of the novel coronavirus disease 2019 (COVID-19), but some extrapulmonary involvement, such as gastrointestinal, cardiac and renal, has been reported [[1], [2], [3]]. The most common symptoms described to date include fever, cough, myalgia, fatigue and shortness of breath; in addition diarrhoea, chest pain, confusion, nausea and vomiting, headache, haemoptysis and hyposmia have been observed [4].
We present the case of a 79-year-old man with a history of fever and cough of 3 days' duration referred to the emergency department with acute loss of consciousness. At admission he was febrile (temperature 38.6°C), with a fast heart rate (115 beats per minute) and rapid breathing (respiratory rate, 22 breaths per minute). Blood pressure was 140/65 mm Hg. Partial pressure of oxygen was 51.8 mm Hg; partial pressure of carbon dioxide was 27.9 mm Hg; and saturated oxygen was 86.6%. There was no history of hypertension or anticoagulation therapy. In addition to loss of consciousness (Glasgow Coma Scale score = 7) and bilateral extensor plantar reflexes, physical examination revealed coarse rales in the left lower lobe of the lungs. Paraclinical findings revealed lymphopenia (590 cells/mm2), erythrocyte sedimentation rate of 85 mm/h, C-reactive protein of 10 mg/L, creatinine of 1.4 mg/dL, platelets of 210 × 109/L, prothrombin time of 12 seconds, international normalized ratio of 1 and partial thromboplastin time of 64 seconds, as well as normal liver function and other routine laboratory tests. Lung computed tomography revealed a ground-glass opacity in the left lower lobe, and brain computed tomography revealed a massive intracerebral haemorrhage (ICH) in the right hemisphere, accompanied by intraventricular and subarachnoid haemorrhage (Fig. 1). Real-time PCR of oropharyngeal swab confirmed COVID-19 infection.
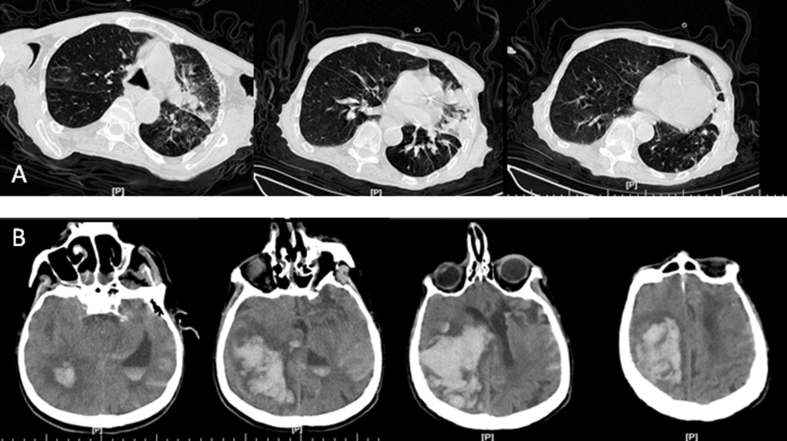
(A) Spiral lung CT scan revealing ground-glass opacity in lateral and anteromedial segment of left inferior lobe. (B) Brain CT scan revealing massive intracerebral haemorrhage in right hemisphere accompanied by intraventricular and subarachnoid haemorrhage. CT, computed tomographic.
The question that thus arises is whether, according to the recent epidemic in our region (the Mazandaran province of Iran), COVID-19 infection causes ICH or whether it is a coincidental event with ICH. COVID-19 has been shown to use the angiotensin-converting enzyme (ACE) II receptor for cell entry [4]. ACE II is highly expressed in lung alveolar type 2 cells and epithelial cells of gastrointestinal system [1,4]. Angiotensin II receptors are also expressed in circumventricular organs and in cerebrovascular endothelial cells, which play a role in the regulation of multiple functions in the brain, including regulation of hormone formation and sympathoadrenal system, water and sodium intake, vascular autoregulation and cerebral blood flow [5]. Angiotensin II is a vasoconstrictor which has a proinflammatory effect [6]. Thus, it is reasonable to hypothesize that brain ACE II could be involved in COVID-19 infection and its dysfunction, leading to disruption of autoregulation as well as blood pressure spikes due to arterial wall rupture.
Another question that arises is how the virus invades the central nervous system. Anecdotal reports from specialists in Iran consistently report hyposmia or anosmia to be common, particularly in the early stage of infection. It is possible that COVID-19 directly invades the central nervous system via the olfactory receptors of cranial nerve I in the nasal cavity cell membrane. Although this is just a theory, in order to explain the limited clinical data regarding the virus's behavior up to now, especially extrapulmonary symptoms, we should be aware of the possibility of initial cerebrovascular manifestations of COVID-19.
References
Articles from New Microbes and New Infections are provided here courtesy of Elsevier
Citations & impact
Impact metrics
Article citations
Atypical Complications during the Course of COVID-19: A Comprehensive Review.
Medicina (Kaunas), 60(1):164, 15 Jan 2024
Cited by: 2 articles | PMID: 38256424 | PMCID: PMC10819426
Review Free full text in Europe PMC
Auto-detection of the coronavirus disease by using deep convolutional neural networks and X-ray photographs.
Sci Rep, 14(1):534, 04 Jan 2024
Cited by: 1 article | PMID: 38177156 | PMCID: PMC10766625
SARS-CoV-2 and Brain Health: New Challenges in the Era of the Pandemic.
Microorganisms, 11(10):2511, 08 Oct 2023
Cited by: 0 articles | PMID: 37894169 | PMCID: PMC10609574
Review Free full text in Europe PMC
Hemorrhagic Coagulation Disorders and Ischemic Stroke: How to Reconcile Both?
Neurol Int, 15(4):1443-1458, 30 Nov 2023
Cited by: 1 article | PMID: 38132972 | PMCID: PMC10745771
Review Free full text in Europe PMC
COVID-19: An Overview of SARS-CoV-2 Variants-The Current Vaccines and Drug Development.
Biomed Res Int, 2023:1879554, 29 Aug 2023
Cited by: 4 articles | PMID: 37674935 | PMCID: PMC10480030
Review Free full text in Europe PMC
Go to all (174) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Gastrointestinal and Liver Manifestations of COVID-19.
J Clin Exp Hepatol, 10(3):263-265, 01 Apr 2020
Cited by: 54 articles | PMID: 32405183 | PMCID: PMC7212283
Review Free full text in Europe PMC
Case of COVID-19 presenting with gastrointestinal symptoms.
World J Virol, 9(1):1-4, 01 May 2020
Cited by: 3 articles | PMID: 32547932 | PMCID: PMC7280948
A Clinical Analysis of Extrapulmonary Complications in Novel Coronavirus Pneumonia Patients.
Int J Gen Med, 14:381-385, 09 Feb 2021
Cited by: 1 article | PMID: 33603443 | PMCID: PMC7881799
APOE genotype, hypertension severity and outcomes after intracerebral haemorrhage.
Brain Commun, 1(1):fcz018, 14 Sep 2019
Cited by: 9 articles | PMID: 32954261 | PMCID: PMC7425529





