Abstract
Background and aim
Diabetes in often associated with an increased severity and mortality in patients with COVID-19. We aimed to find out whether the severity and mortality in patients with diabetes with COVID-19 has any correlation to the level of glycemic control.Methods
A Boolean search was made in PubMed database using the specific keywords related to our objectives up till May 14, 2020 and full text of article retrieved with the supplements published in English language.Results
Two studies available so far have studied the outcomes of severity and mortality in patients with diabetes stratified on glycemic control. Both the studies have unequivocally found that patients with poorly-controlled hyperglycemia (blood glucose >180 mg/dl) have significantly higher level of poor prognostic markers biochemically, compared to the well-controlled arms (blood glucose <180 mg/dl). Moreover, significant increase in severity and mortality was observed in cohorts with poorly-controlled blood glucose due to any cause (diabetes or stress hyperglycemia), compared to the well-controlled cohorts with COVID-19, even after the adjustment of multiple confounders.Conclusions
Poorly-controlled hyperglycemia increases the severity and mortality in patients with COVID-19. All treating physician must strive for a good glycemic control (blood glucose <180 mg/dl) in patients with or without diabetes.Free full text

Does poor glucose control increase the severity and mortality in patients with diabetes and COVID-19?
Abstract
Background and aim
Diabetes in often associated with an increased severity and mortality in patients with COVID-19. We aimed to find out whether the severity and mortality in patients with diabetes with COVID-19 has any correlation to the level of glycemic control.
Methods
A Boolean search was made in PubMed database using the specific keywords related to our objectives up till May 14, 2020 and full text of article retrieved with the supplements published in English language.
Results
Two studies available so far have studied the outcomes of severity and mortality in patients with diabetes stratified on glycemic control. Both the studies have unequivocally found that patients with poorly-controlled hyperglycemia (blood glucose >180 mg/dl) have significantly higher level of poor prognostic markers biochemically, compared to the well-controlled arms (blood glucose <180 mg/dl). Moreover, significant increase in severity and mortality was observed in cohorts with poorly-controlled blood glucose due to any cause (diabetes or stress hyperglycemia), compared to the well-controlled cohorts with COVID-19, even after the adjustment of multiple confounders.
Conclusions
Poorly-controlled hyperglycemia increases the severity and mortality in patients with COVID-19. All treating physician must strive for a good glycemic control (blood glucose <180 mg/dl) in patients with or without diabetes.
1. Introduction
Poor glycemic control was associated with a significant increased risk of complications and death during the past pandemics of Middle East Respiratory Syndrome Coronavirus (MERS-CoV), H1N1 influenza and Severe Acute Respiratory Syndrome Coronavirus-1 (SARS-CoV-1) [[1], [2], [3]].
Although various studies and their meta-analysis have recently shown that the patients with diabetes have a significantly higher risk of severe COVID-19 and increased mortality, no studies were available until recently, that analyzed the relation of glycemic control to the severity and mortality in COVID-19. Thus, we sought to find the relation of glycemic control to the severity and mortality with COVID-19, in patients with diabetes or uncontrolled hyperglycemia.
2. Methods
A Boolean search in PubMed database up till May 14, 2020 using the specific key words “SARS-CoV-2” or, “COVID-19” or, “Diabetes” or, “Stress hyperglycemia” or, “Glycemic control” or, “Outcome” or, “Severity” or, “Mortality” with the interposition of “AND” was made, and the full text of all articles with their supplement published in English language were retrieved.
3. Results
To date, only two studies have analyzed the outcomes of severity and mortality in patients with diabetes with COVID-19, based on the level of glycemic control. A large retrospective study conducted by Zhu et al. [4] has studied 7336 patients with COVID-19 and analyzed the data of 810 type 2 diabetic patients, stratified on the basis of level of glycemic control, in a 28-days follow-up. This study compared 528 poorly-controlled diabetes (defined as blood glucose >180 mg/dl), to 282 well-controlled diabetes (defined as blood glucose between 70 and 180 mg/dl). Notably, a significant difference in hematological and biochemical profile that are suggestive of poor prognostic markers, were significantly higher in poorly-controlled (mean HbA1c 8.1%) diabetic cohorts, compared to the well-controlled (mean HbA1c 7.3%) group. There was a significantly lower lymphocyte count (49.6% vs. 30.5%) and a significantly higher neutrophil count (19.4% vs. 10.7%), white blood cell count (12.2% vs. 6.3%), C-reactive protein (CRP, 59.5% vs. 47.5%), procalcitonin (35% vs 24.2%), aspartate transaminase (AST, 20.4% vs. 11.3%) and D-dimer (55.4% vs. 35.6%) in poorly-controlled group, compared to the well-controlled group, respectively. In addition, a significantly higher percentage of patients in poorly-controlled group had oxygen saturation (SpO2) of <95%, compared to the well-controlled group (22.7% vs. 12.6%, respectively). With regards to the severity, a significant increase in Acute Respiratory Syndrome (ARDS, 21.4% vs. 7.1%, p < 0.001), acute heart injury (9.9% vs. 1.4%, p < 0.001) acute kidney injury (3.8% vs. 0.7%, p = 0.019) and septic shock (4.7% vs. 0.0%, p = 0.004) were observed in patients having poorly-controlled diabetes, compared to the well-controlled group. These findings suggest that patients with poorly-controlled diabetes have clearly poor prognosis, compared to the patients with well-controlled diabetes. Indeed, the adjusted hazard ratio (HR) for all-cause mortality was 0.13 (95% CI, 0.04–0.44, p < 0.001) in well-controlled vs. poorly-controlled diabetic group which suggest an 87% relative lesser mortality rate in patients with well-controlled diabetes. However, this finding may not be conclusive, in the absence of adjustment for other confounding factors that can also increase mortality.
Interestingly, this study by Zhu et al. [4] also sub-analyzed the data of 500 patients of diabetes with COVID-19, after conducting a 1:1 propensity score-matching (matched for other comorbidities that include hypertension, cardio- and cerebro-vascular disease and chronic kidney disease) and compared the outcomes of 250 patients with diabetes in each group. Notably, a significant increase in ARDS (14.8% vs. 7.2%, p = 0.01) acute kidney injury (3.2% vs. 0.4%, p = 0.04) and acute heart injury (6.8% vs. 1.6%, p = 0.01) was still observed in poorly-controlled arm (n = 250) compared to the well-controlled arm (n = 250), despite the adjustment of multiple confounding factors. Moreover, the adjusted HR for all-cause mortality was 0.14 (95% CI, 0.03–0.60, p = 0.008) in the well-controlled arm, compared to the poorly-controlled arm, thereby suggesting an 86% relative decrease in mortality in the former group, compared to the latter. Fig. 1 depicts the diagrammatic representation of findings from the propensity-matched arms.
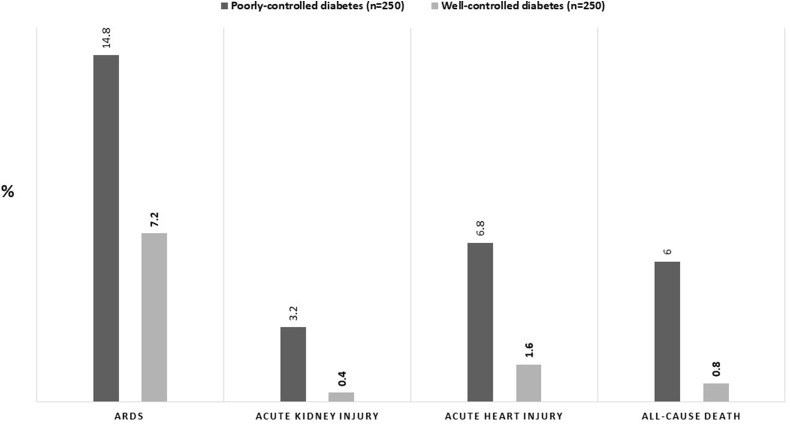
Severity and mortality in patients with COVID-19 in a propensity-matched cohort of poorly-controlled vs. well-controlled diabetes (n = 500).
Another retrospective observational study (n = 1122) by Bode et al. [5] from 88 hospitals in USA has also studied the outcome of 481 patients with diabetes (HbA1c ≥ 6.5%) and/or uncontrolled hyperglycemia (defined as ≥2 blood glucose value >180 mg/dl within any 24-h period) with COVID-19, over a follow-up of 37-days. Among the 53 patient who died, there was a significantly higher percentage of death (41.7 vs. 14.8%, p < 0.001) in patients with uncontrolled hyperglycemia who were not previously diagnosed as diabetes (HbA1c <6.5%), compared to the patients with diabetes. This suggest that stress hyperglycemia (defined by the American Diabetes Association [6] as a transient elevation in blood glucose in the setting of acute illness or after surgery in a patient with an A1C < 6.5%), may have a worser outcome in acute illness, compared to a previously diagnosed diabetes. This finding is not unexpected, given that the similar worser outcome was observed with stress hyperglycemia in previous meta-analyses [7,8]. Interestingly, stress hypoglycemia was one of the poor prognostic factors and had been associated with a significant increase in respiratory failure and death during the SARS-CoV-1 outbreak in 2003–2004, along with the diabetes [9]. Intuitively, this may also hint to a possible direct involvement of pancreas in COVID-19, especially in the light of positive Angiotensin Converting Enzyme 2 (ACE2) immunostaining of cadaveric pancreatic islet cells, similar to the lung alveolar epithelium and myocardium [10]. Interestingly, in a retrospective study of 52 COVID-19 patient, Wang et al. [11] found an evidence of acute pancreatic injury (diagnosed by raised amylase and lipase) in 17% of the patients, in the absence of any known risk factor that may cause acute pancreatitis. Whether this acute pancreatitis is related to a direct viral involvement of the pancreas by the SARS-CoV-2 or due to the enzymatic abnormalities related to critical illness, needs to be proven through a further larger studies.
4. Conclusions
Uncontrolled or poorly-controlled hyperglycemia due to any cause including diabetes or stress hyperglycemia is associated with a poor outcome (increases in severity and mortality) in patients with COVID-19. Data from both the studies unequivocally points that every clinician should strive to achieve a blood-glucose targets <180 mg/dL for most patients with diabetes with COVID-19, without provoking hypoglycemia, in the absence of evidence to the contrary. More studies will further strengthen our knowledge with regards to the relationship of glycemic control to the severity and mortality in patients with diabetes and COVID-19.
Funding
No funding
Declaration of competing interest
We hereby declare that we have no conflict of interest, related to this article.
References
Citations & impact
Impact metrics
Article citations
The effect of SARS-COV-2 variant on non-respiratory features and mortality among vaccinated and non-fully vaccinated patients.
Vaccine, 42(10):2655-2660, 14 Mar 2024
Cited by: 0 articles | PMID: 38490824 | PMCID: PMC11182488
Predictive Value of Nutrition and Inflammation-Related Indices on Prognosis in Type 2 Diabetes Mellitus Patients with Coronavirus Disease-2019.
Sisli Etfal Hastan Tip Bul, 58(1):55-61, 05 Apr 2024
Cited by: 0 articles | PMID: 38808055 | PMCID: PMC11128691
PMI-controlled mannose metabolism and glycosylation determines tissue tolerance and virus fitness.
Nat Commun, 15(1):2144, 08 Mar 2024
Cited by: 0 articles | PMID: 38459021 | PMCID: PMC10923791
Impact of COVID-19 on diabetes care: mixed methods study in an Indigenous area of Guatemala.
BMJ Open, 14(1):e079130, 02 Jan 2024
Cited by: 0 articles | PMID: 38167279 | PMCID: PMC10773399
Linking the Extended Autonomic System with the Homeostat Theory: New Perspectives about Dysautonomias.
J Pers Med, 14(1):123, 22 Jan 2024
Cited by: 0 articles | PMID: 38276245 | PMCID: PMC10817591
Go to all (41) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Impaired Fasting Glucose and Diabetes Are Related to Higher Risks of Complications and Mortality Among Patients With Coronavirus Disease 2019.
Front Endocrinol (Lausanne), 11:525, 10 Jul 2020
Cited by: 50 articles | PMID: 32754119 | PMCID: PMC7365851
Assessment of risk, severity, mortality, glycemic control and antidiabetic agents in patients with diabetes and COVID-19: A narrative review.
Diabetes Res Clin Pract, 165:108266, 11 Jun 2020
Cited by: 53 articles | PMID: 32533989 | PMCID: PMC7286824
Review Free full text in Europe PMC
J-shaped association between fasting blood glucose levels and COVID-19 severity in patients without diabetes.
Diabetes Res Clin Pract, 168:108381, 25 Aug 2020
Cited by: 19 articles | PMID: 32853687 | PMCID: PMC7445136
Newly-diagnosed diabetes and admission hyperglycemia predict COVID-19 severity by aggravating respiratory deterioration.
Diabetes Res Clin Pract, 168:108374, 15 Aug 2020
Cited by: 120 articles | PMID: 32805345 | PMCID: PMC7428425

 and
and 


