Abstract
Background
Current mitigation strategies for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) rely on the population-wide adoption of nonpharmaceutical interventions (NPIs). Monitoring the adoption of NPIs and their associations with SARS-CoV-2 infection history can provide key information for public health.Methods
We sampled 1030 individuals in Maryland from 17-28 June 2020 to capture sociodemographically and geographically resolved information about NPI adoption and access to SARS-CoV-2 testing, and examine associations with self-reported SARS-CoV-2 positivity.Results
Overall, 92% reported traveling for essential services and 66% visited friends/family. Use of public transport was reported by 18%. In total, 68% reported strict social distancing indoors and 53% reported strict masking indoors; indoor social distancing was significantly associated with age, and race/ethnicity and income were associated with masking. Overall, 55 participants (5.3%) self-reported ever testing positive for SARS-CoV-2, with strong dose-response relationships between several forms of movement frequency and SARS-CoV-2 positivity. In a multivariable analysis, a history of SARS-CoV-2 infection was negatively associated with strict social distancing (adjusted odds ratio [aOR] for outdoor social distancing, 0.10; 95% confidence interval, .03-.33). Only public transport use (aOR for >7 times vs never, 4.3) and visiting a place of worship (aOR for ≥3 times vs never, 16.0) remained significantly associated with SARS-CoV-2 infection after adjusting for strict social distancing and demographics.Conclusions
These results support public health messaging that strict social distancing during most activities can reduce SARS-CoV-2 transmission. Additional considerations are needed for indoor activities with large numbers of persons (places of worship and public transportation), where even NPIs may not be possible or sufficient.Free full text

Rapid Real-time Tracking of Nonpharmaceutical Interventions and Their Association With Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Positivity: The Coronavirus Disease 2019 (COVID-19) Pandemic Pulse Study
Abstract
Background
Current mitigation strategies for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) rely on the population-wide adoption of nonpharmaceutical interventions (NPIs). Monitoring the adoption of NPIs and their associations with SARS-CoV-2 infection history can provide key information for public health.
Methods
We sampled 1030 individuals in Maryland from 17–28 June 2020 to capture sociodemographically and geographically resolved information about NPI adoption and access to SARS-CoV-2 testing, and examine associations with self-reported SARS-CoV-2 positivity.
Results
Overall, 92% reported traveling for essential services and 66% visited friends/family. Use of public transport was reported by 18%. In total, 68% reported strict social distancing indoors and 53% reported strict masking indoors; indoor social distancing was significantly associated with age, and race/ethnicity and income were associated with masking. Overall, 55 participants (5.3%) self-reported ever testing positive for SARS-CoV-2, with strong dose-response relationships between several forms of movement frequency and SARS-CoV-2 positivity. In a multivariable analysis, a history of SARS-CoV-2 infection was negatively associated with strict social distancing (adjusted odds ratio [aOR] for outdoor social distancing, 0.10; 95% confidence interval, .03–.33). Only public transport use (aOR for >7 times vs never, 4.3) and visiting a place of worship (aOR for ≥3 times vs never, 16.0) remained significantly associated with SARS-CoV-2 infection after adjusting for strict social distancing and demographics.
Conclusions
These results support public health messaging that strict social distancing during most activities can reduce SARS-CoV-2 transmission. Additional considerations are needed for indoor activities with large numbers of persons (places of worship and public transportation), where even NPIs may not be possible or sufficient.
The severe acute respiratory syndrome coronavirus 2 (SARS CoV-2) and associated coronavirus disease 2019 (COVID-19) pandemic continues to evolve at a rapid pace, having affected more than 23 million persons globally and more than 5.7 million in the United States as of 25 August 2020 [1]. While there has been rapid progress in therapeutics [2, 3] and vaccine development [4, 5], nothing to date is a panacea. The primary means of curtailing transmission remain testing, contact tracing, and continued implementation of nonpharmaceutical interventions (NPIs), such as social distancing and masking [6, 7].
A growing number of reports have demonstrated the impact of social distancing on reducing SARS-CoV-2 transmission. Many of these reports have modeled these impacts using state- and/or county-level data on government-imposed interventions/restrictions or geolocation data from mobile phone users as a surrogate for social distancing and mobility [8–14]. While these analyses allow for an examination of trends across multiple geographies and large sample sizes, they are ecological in nature, and thus need to be supplemented by methods that can capture finer-scale changes in behavior, such as population-based surveys.
Monitoring trends in the adoption of NPIs via surveys may provide insight into the trajectory of local SARS-CoV-2 epidemics, and can guide public health practice and policy [8]. Declining or poor levels of NPI adoption could signal an impending upsurge in cases, indicating a need to mobilize resources to medical facilities and expand testing to facilitate early diagnosis and isolation. In contrast, high levels of NPI adoption could support decisions related to reopening businesses. Such approaches can also help to identify subgroups (eg, race, income, age) who are differentially practicing social distancing or other preventive behaviors, and can directly collect data to help distinguish between travel for essential services/employment versus leisure, both of which will be important for eventual public health messaging. While some data collected via mobile phone applications may also be able to provide information on the type of location visited (eg, a restaurant vs residence), there may still exist nuances in the reasons for travel (eg, an employee vs guest at a restaurant) that would be unavailable; further, information about the differences in travel by sociodemographic subgroups may not be always available. While surveys could capture this type of granular information at frequent intervals, to date most surveys have focused on symptoms, COVID-19 impacts, and attitudes towards NPIs [15–17].
We used an online panel to rapidly sample persons in Maryland to capture granular information on NPI adoption, travel, access to SARS-CoV-2 testing, and associations with self-reported SARS-CoV-2 positivity.
METHODS
Study Setting
As of 30 June 2020, Maryland had nearly 68 000 confirmed COVID-19 cases and more than 3200 deaths; the current positive test proportion is 4.56% [18]. Community transmission has been sustained since 12 March 2020 [18], and statewide stay-at-home orders were implemented from 30 March to 15 May 2020. As of 18 April 2020, Maryland required face coverings on public transit and within retail outlets for employees and customers. Stage 2 of phased reopening began on 12 June 2020, allowing indoor restaurant dining to resume at 50% capacity; on 19 June 2020, gyms, retail stores, salons, barbershops, nail salons, amusement parks, outdoor pools, and indoor worship services were permitted to open with capacity restrictions [19].
Study Sample
Participants were recruited from across Maryland from 17–28 June 2020 using Dynata (https://www.dynata.com), which is among the largest first-party global data platforms. Dynata maintains a database of potential participants who are randomized to specific surveys if they meet the specified demographic targets of the survey; participants receive modest compensation for participation. Security checks and quality verifications are used to verify identity and prevent duplication before participants begin surveys. These include digital fingerprinting to prevent duplication, spot checking via third-party verification to prove identity, and a dedicated panelist quality team. Dynata staff are active in multiple online research quality initiatives, including the European Society for Opinion and Marketing Research.
We provided Dynata with quotas for age, gender, race, and income based on the population composition of Maryland. Quotas were monitored through the Dynata internal router system and self-reported survey data. Dynata distributed survey invitations to 2322 persons. Of these, 1466 visited the survey site and responded to at least 1 question: 109 started but did not complete the survey, and 310 responses were excluded for noneligibility (age <18 years or residence outside Maryland). We further excluded 17 participants who did not provide a response to ever being tested for SARS-CoV-2, for a final sample size of 1030 (target = 1000).
Survey
The electronic survey was based on a combination of existing COVID-19 surveys and new questions on sociodemographic characteristics, adoption of NPIs (including social distancing and mask wearing), and access to SARS-CoV-2 testing. All questions were asked with respect to the prior 2 weeks. To understand social distancing practices, participants were asked about the types of places/locations they visited in the prior 2 weeks and the frequency of those visits, including to indoor locations, such as large gatherings, homes of friends and family members, gyms, salons, grocery stores, pharmacies, restaurants, and places of worship, and to outdoor locations, such as beaches and pools. Participants were also asked about social distancing practices and mask wearing at these locations.
Statistical Analysis
Chi-square tests and Mann-Whitney tests were used to compare categorical and continuous variables, respectively. Logistic regression was used to identify the variables associated with ever testing positive for SARS-CoV-2 infection. Variables of interest included demographics; mobility patterns, including types of outdoor and indoor locations visited in the prior 2 weeks; and adoption of masking and social distancing. Variables were considered for inclusion in multivariable models if they held biological significance, were statistically significant in univariable models (P < .05), and/or had significant variable importance scores, as determined by machine-learning feature selection using random forest with a Boruta wrapper algorithm [20]. As a sensitivity analyses, we restricted the outcome to a self-report of a recent (prior 2 weeks) positive SARS-CoV-2 test.
Ethical Clearance
The study was approved by the Institutional Review Board of the Johns Hopkins Bloomberg School of Public Health (IRB00012413), and all participants consented to participate.
RESULTS
Characteristics of Study Population
The median age of participants was 43 years, and 55% were women. The majority (n = 618, 60%) were White, and 239 (23%) and 74 (7%) self-identified as Black/African American and Hispanic/Latino, respectively (Table 1). About 69% of the participants reported attending college or possessing a graduate degree, and the majority (55%) reported a household income less than $70 000. There were 303 (29%) respondents who reported working outside of their home. Participants were sampled from all 24 counties in Maryland, with the largest proportion from the most populous counties. In general, the sociodemographic characteristics of the study sample were reflective of the Maryland state population (Supplementary Figure S1).
Table 1.
Characteristics of Study Sample
| Overall | Never tested positive for SARS-CoV-2 | Ever tested positive for SARS-CoV-2 | |
|---|---|---|---|
| n = 1030 | n = 975 | n = 55 | |
| Median age (IQR) | 43 (32–57) | 44 (34–57) | 28 (22–35) |
| Median household size (IQR) | 2 (2–4) | 2 (2–4) | 2 (1–4) |
| Gender, n (%) | |||
 Female Female | 563 (55%) | 542 (95%) | 21 (4%) |
 Male Male | 461 (45%) | 428 (92%) | 33 (7%) |
 Other Other | 5 (.6%) | 4 (80%) | 1 (20%) |
| Race/ethnicity, n (%) | |||
 White/Caucasian White/Caucasian | 618 (60%) | 598 (97%) | 20 (3%) |
 Black/African American Black/African American | 239 (23%) | 217 (91%) | 22 (9%) |
 Hispanic/Latino Hispanic/Latino | 74 (7%) | 65 (88%) | 9 (12%) |
 Asian/Pacific Islander Asian/Pacific Islander | 52 (5%) | 50 (96%) | 2 (4%) |
 American Indian/Alaska Native American Indian/Alaska Native | 12 (1%) | 10 (83%) | 2 (17%) |
 Mixed/Other Mixed/Other | 35 (4%) | 35 (100%) | 0 (0%) |
| Educational attainment, n (%) | |||
 High school degree or less High school degree or less | 212 (21%) | 201 (95%) | 11 (5%) |
 Associate degree Associate degree | 104 (10%) | 99 (95%) | 5 (5%) |
 Some college, no degree Some college, no degree | 192 (19%) | 188 (97%) | 4 (2%) |
 Bachelor’s degree Bachelor’s degree | 283 (27%) | 263 (92%) | 20 (7%) |
 Graduate degree Graduate degree | 236 (23%) | 221 (93%) | 15 (6%) |
| Annual household income, n (%) | |||
 <$20 000 <$20 000 | 113 (11%) | 104 (92%) | 9 (8%) |
 $20 000–$39 000 $20 000–$39 000 | 162 (16%) | 150 (93%) | 12 (7%) |
 $40 000–$49 000 $40 000–$49 000 | 96 (9%) | 90 (94%) | 6 (6%) |
 $50 000–$69 000 $50 000–$69 000 | 200 (19%) | 192 (96%) | 8 (4%) |
 $70 000+ $70 000+ | 429 (42%) | 409 (95%) | 20 (5%) |
| Employment status, n (%) | |||
 Employed, working outside the home Employed, working outside the home | 303 (29%) | 271 (89%) | 32 (10%) |
 Employed, working from home Employed, working from home | 337 (33%) | 324 (95%) | 13 (4%) |
 Unemployed Unemployed | 191 (19%) | 186 (96%) | 5 (3%) |
 Retired Retired | 188 (18%) | 184 (97%) | 4 (2%) |
Data are shown by self-reported SARS-CoV-2 infection status. In the column representing the overall description, we have listed the column percentage to reflect the overall population characteristics; in the columns stratified by self-reported SARS-CoV-2 positivity status, we have listed the row percentage to allow for comparison of self-reported positivity by various subgroups. Overall column percentages may not sum to 100 if some participants elected not to answer a given question.
Abbreviations: IQR, interquartile range; SARS-C0V-2, severe acute respiratory syndrome coronavirus 2.
Recent Movement
Overall, 990 (96%) participants reported leaving their home at least once during the prior 2 weeks. Of these, almost all (92%) reported traveling for essential services (eg, grocery store or pharmacy) at least once, and 40% reported going 3 or more times in the prior 2 weeks. Following travel for essential services, the next most frequented places were visiting friends/family (66%); indoor venues such as bars, salons, or restaurants (49%); and outdoor venues such as beaches or pools (25%; Figure 1; Supplementary Figure S2). Among those who reported travel, 18% and 15% reported using public transport and visiting a place of worship, respectively. Activities were positively correlated with each another (Supplementary Figure S3). There were 5% who reported engaging in all activities. About a quarter (26%) reported attending at least 1 gathering of 10 or more people in the prior 2 weeks, of whom 8% reported attending 3 or more gatherings; 104 (10%) reported attending at least 1 gathering of 100 or more.

Sankey diagram showing participant mobility for essential and nonessential services and public transportation use in the past 2 weeks. Participant responses are depicted in each rectangular node, with flows proportional to how many individuals responded: for example, individuals who responded “yes” to both essential services and nonessential services are reflected in the flow connecting the 2 “yes” nodes for these variables. Individuals who have ever tested positive for SARS-CoV-2 are shown in red, whereas all others are shown in gray. A total of 51 (5%) participants responded “yes” to all mobility questions, and 39 (4%) responded “no” to all; 17 (31%) of those who tested positive for SARS-CoV-2 responded “yes” to all and 2 (4%) responded “no” to all. The thickness of the flow is directly proportional to the number of respondents who report that behavior. Abbreviation: SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Adoption of NPIs
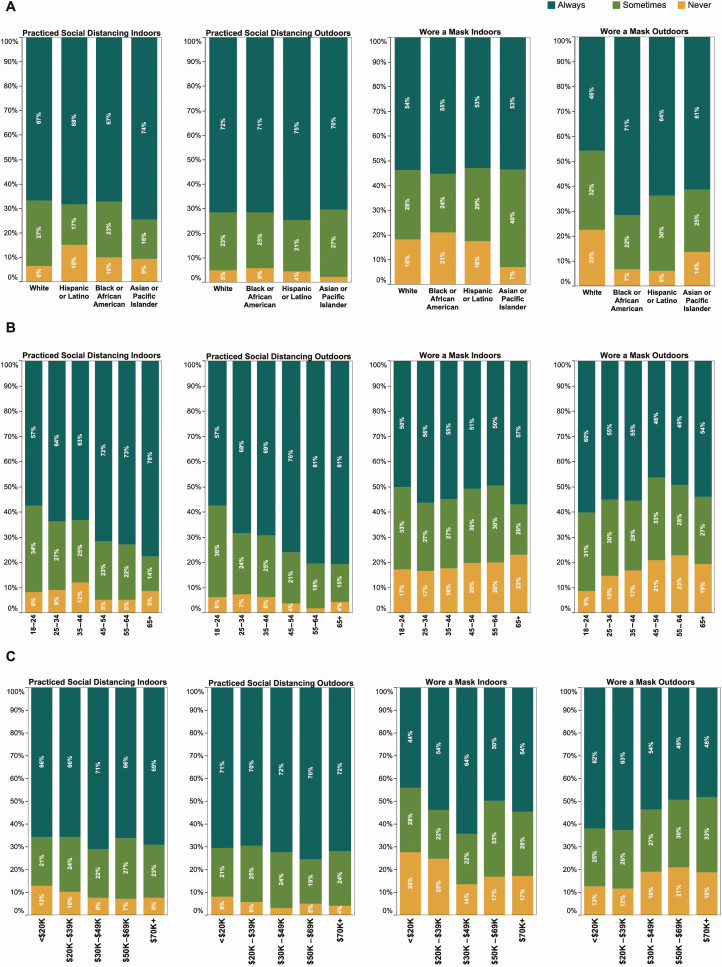
The majority reported practicing social distancing when visiting indoor and outdoor locations, although adoption of social distancing increased with age. For example, 81% of those over the age of 65 reported always practicing social distancing at outdoor activities, compared to 58% of those aged 18–24 (P < .001; Figure 2). About half (53%) reported that they always wore a mask when visiting indoor and outdoor locations; 17% and 19% reported never wearing a mask when visiting indoor or outdoor locations, respectively. While age was not significantly associated with self-reported mask use, race and income were. About three-fourths (72%) of Blacks reported always wearing a mask outdoors, compared to 44% of Whites (P < .001). Further, 62% of those with a household income less than $20 000/year reported always wearing a mask outdoors, compared to 48% of those with household income of $70 000 or greater (P = .018).
SARS-CoV-2 Infection and Access to Testing
Overall, 55 participants (5.3%) self-reported ever testing positive for SARS-CoV-2 infection. Participants who self-reported having tested positive were significantly more likely to be male, younger, self-identify as Black/African American or Hispanic/Latino, and be required to travel outside of home for work (Table 1). The distribution of self-reported SARS-CoV-2 positivity by Maryland counties is presented in Supplementary Figure S4.
In the prior 2 weeks, 102 persons reported wanting or needing a SARS-CoV-2 test, of whom 62 (61%) were able to get a test. Of those tested, 18 (29%) tested positive, and 16 (89%) reported subsequent hospitalization (see Supplementary Figure S5). While 18 (29%) reported getting a test the same day they wanted/needed it, about a third (34%) reported waiting 3 or more days. Over half (53%) reported waiting 3 or more days to receive a test result; 7 (11%) had not received their results at the time of the survey.
Association Between Prior SARS-CoV-2 Infection Status, Travel History, and Adoption of NPIs
In an unadjusted analysis, a self-reported history of SARS-CoV-2 infection was significantly more frequent among those who were younger, male, and Black/African American or Hispanic/Latino (P values < .05 for all; Table 2). SARS-CoV-2 infection was also significantly more common among those who reported using public transportation, attending a place of worship, visiting friends or family, attending gatherings of more than 10 people and more than 100 people, and visiting indoor or outdoor venues where people gather (P values < .05 for all; Supplementary Figure S6). Infection was significantly less common in those who reported strict social distancing indoors and outdoors (P values < .05 for both).
Table 2.
Factors Associated With Ever Testing Positive for Severe Acute Respiratory Syndrome Coronavirus 2, by Univariable and Multivariable Logistic Regression
| Variable | Ever tested positive OR (95% CI) | Ever tested positive aOR (95% CI) |
|---|---|---|
| Race/ethnicity | ||
 White White | Ref. | Ref. |
 Black/African American Black/African American | 3.03 (1.62–5.66) | 1.06 (.44–2.54) |
 Hispanic/Latino Hispanic/Latino | 4.14 (1.81–9.47) | 2.75 (.87–8.70) |
| Age, per 5-year increase | .69 (.61–.78) | .84 (.71–.99) |
| Male gender | 2.00 (1.13–3.45) | 1.55 (.69–3.47) |
| Annual household income | ||
 <$20 000 <$20 000 | Ref. | … |
 $20 000–$39 000 $20 000–$39 000 | .92 (.38–2.27) | … |
 $40 000–$49 000 $40 000–$49 000 | .77 (.26–2.25) | … |
 $50 000–$69 000 $50 000–$69 000 | .48 (.18–1.29) | … |
 $70 000+ $70 000+ | .57 (.25–1.28) | … |
| Work outside the home | 3.61 (2.08–6.29) | … |
| Practice social distancing indoors | ||
 Never Never | Ref. | Ref. |
 Sometimes Sometimes | .71 (.31–1.63) | .26 (.08–.90) |
 Always Always | .30 (.14–.67) | .32 (.10–.99) |
| Practice social distancing outdoors | ||
 Never Never | Ref. | Ref. |
 Sometimes Sometimes | .70 (.28–1.73) | .34 (.10–1.19) |
 Always Always | .19 (.08–.46) | .10 (.03–.33) |
| Used public transport | ||
 Never Never | Ref. | Ref. |
 Once or twice Once or twice | 8.06 (3.80–17.1) | 6.00 (2.13–16.9) |
 3–7 times 3–7 times | 12.2 (5.64–26.3) | 3.80 (1.18–12.3) |
 More than 7 times More than 7 times | 18.8 (7.59–46.4) | 4.29 (1.12–16.5) |
| Attended gathering of >10 people | ||
 Never Never | Ref. | … |
 Once or twice Once or twice | 3.37 (1.56–7.25) | … |
 3–7 times 3–7 times | 15.5 (7.22–33.4) | … |
 More than 7 times More than 7 times | 28.7 (10.4–78.7) | … |
| Attended gathering of >100 people | ||
 Never Never | Ref. | … |
 Once or twice Once or twice | 6.51 (2.77–15.3) | … |
 3–7 times 3–7 times | 26.4 (11.37–61.4) | … |
 More than 7 times More than 7 times | 34.0 (13.2–87.7) | … |
| Visited place of worship | ||
 Never Never | Ref. | Ref. |
 Once or twice Once or twice | 2.91 (1.06–8.02) | 1.41 (.38–5.31) |
 3 or more times 3 or more times | 23.9 (12.5–45.9) | 16.0 (5.97–42.7) |
| Visited friends or family | ||
 Never Never | Ref. | … |
 Once or twice Once or twice | 1.12 (.52–2.42) | … |
 3–7 times 3–7 times | 3.87 (1.77–8.46) | … |
 More than 7 times More than 7 times | 5.42 (1.89–15.6) | … |
| Went to a grocery store/pharmacy | ||
 Never Never | Ref. | … |
 Once or twice Once or twice | .43 (.17–1.13) | … |
 3–7 times 3–7 times | .69 (.27–1.81) | … |
 More than 7 times More than 7 times | 2.23 (.77–6.51) | … |
| Went to an indoor bar, restaurant, salon, or other indoor establishment | ||
 Never Never | Ref. | … |
 Once or twice Once or twice | 1.10 (.53–2.29) | … |
 3–7 times 3–7 times | 4.14 (1.98–8.68) | … |
 More than 7 times More than 7 times | 9.76 (3.83–24.9) | … |
| Went to a beach, pool, or other outdoor gathering place | ||
 Never Never | Ref. | … |
 Once or twice Once or twice | 2.45 (1.16–5.18) | … |
 3–7 times 3–7 times | 9.30 (4.47–19.3) | … |
 More than 7 times More than 7 times | 8.28 (2.56–26.7) | … |
| Mask wearing in public indoors | ||
 Never or sometimes Never or sometimes | … | … |
 Always Always | .63 (.36–1.09) | … |
| Always wear mask in public outdoors | ||
 Never or sometimes Never or sometimes | … | … |
 Always Always | 1.06 (.61–1.85) | … |
| Number of close contacts indoors | ||
 0 0 | Ref. | … |
 1 1 | 3.96 (1.41–11.2) | … |
 2–5 2–5 | 4.46 (1.92–10.3) | … |
 6–10 6–10 | 4.87 (1.72–13.8) | … |
 >10 >10 | 6.16 (1.72–22.0) | … |
| Number of close contacts outdoors | ||
 0 0 | Ref. | … |
 1 1 | 5.90 (2.00–17.4) | … |
 2–5 2–5 | 6.30 (2.54–15.6) | … |
 6–10 6–10 | 9.58 (3.31–27.7) | … |
 >10 >10 | 4.26 (.83–21.9) | … |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; OR, odds ratio; Ref., reference.
In a multivariable analysis, a history of SARS-CoV-2 infection remained significantly more likely among younger respondents, those who took public transportation (adjusted odds ratio [aOR] for more than 7 times vs never, 4.3; 95% confidence interval [CI], 1.1 – 16.5), and those who visited a place of worship (aOR for those who visited ≥ 3 times vs never, 16.0; 95% CI, 6.0 – 42.7), and significantly less common among those who always practiced social distancing (aOR for indoor social distancing, 0.32 [95% CI, .10–.99]; aOR for outdoor social distancing, 0.10 [95% CI, .03–.33]; Table 2). Associations were similar in sensitivity analyses of self-reported SARS-CoV-2 infection in the prior 2 weeks (Supplementary Table S7).
DISCUSSION
We utilized an online panel survey to provide a rapid, cost-efficient snapshot of travel patterns and NPI adoption across population subgroups in Maryland. These data indicate that nonessential travel and uneven NPI adoption could influence community transmission of SARS-CoV-2 infection. Over two-thirds of the respondents reported recent travel for nonessential services; self-reported SARS-CoV-2 infections were significantly more common among those who reported using public transport or visiting places of worship, and significantly less common among those who always practiced social distancing. Significant differences in NPI adoption were observed by age, race, and income, suggesting that communication campaigns should tailor messaging to specific subgroups.
Positive dose-response relationships were demonstrated between recent movement and prior SARS-CoV-2 infection. The more frequently an individual participated in an activity, the more likely they were to have tested positive. Additionally, consistent with ecologic analyses [21], lower levels of SARS-CoV-2 positivity were observed among those always practicing social distancing. Indeed, when adjusting for movement types, social distancing, and other demographic factors associated with positivity, most associations between recent movement and SARS-CoV-2 positivity were no longer statistically significant. This supports public health messaging that incorporating appropriate NPIs while visiting indoor and outdoor venues helps reduce SARS-CoV-2 transmission. Importantly, this was not the case for using public transport and visiting a place of worship in the prior 2 weeks, which remained significantly associated with SARS-CoV-2 positivity even after adjustment. Of course, while mask use is mandated for public transport, social distancing may be challenging and the use of public transport may reflect necessity versus a personal choice. While in Maryland, although many religious gatherings moved to remote services, indoor religious gatherings were allowable with restrictions at the time of the survey. We specifically surveyed about physically visiting places of worship, but were unable to discriminate the reasons why persons attended a place of worship (eg, service vs food distribution vs Narcotics Anonymous). It is important to note that data on movement and NPI adoption, albeit self-reported, was limited to the prior 2 weeks to minimize recall bias.
While these data demonstrated a negative association between consistent indoor mask use and ever testing positive for SARS-CoV-2, this association failed to achieve statistical significance. The collection of data related to mask use is nuanced, as several factors that are challenging to collect can affect the efficacy of masks, such as fit, type of mask, frequency of touching/adjusting mask, and so forth. Further, guidance on mask use has been evolving since March, with the Centers for Disease Control and Prevention (CDC) only endorsing mask use on 3 April 2020, which could have affected associations with ever testing positive. In sensitivity analyses that restricted analyses to recent SARS-CoV-2 infection, consistent indoor mask use was significantly associated with a lower likelihood of infection.
These analyses could not establish temporality between exposures and SARS-CoV-2 positivity, and those who tested positive may have been more likely to practice these behaviors when they were infected or may have changed their behaviors after testing positive because of an altered risk perception. Sensitivity analyses demonstrating similar associations with recent SARS-CoV-2 infection and the dose-response associations observed suggest that reverse causality does not likely explain these associations. Regardless of directionality, these findings have implications for community transmission risk, particularly in light of incomplete understanding both of viral shedding and infectiousness among infected persons and of the role and duration of acquired immunity on protection from SARS-CoV-2 reinfection [22–25]. Of interest, these data were collected just as Maryland began to relax restrictions, and the state witnessed an uptick [18] in cases about a month after the survey, particularly among younger persons, the strata who reported maximum mobility in this survey.
Aside from the widescale adoption of NPIs, early diagnosis, appropriate contact tracing measures, and isolation and/or referral to care are critical to curtailing SARS-CoV-2 transmission [22]. It is vital that all persons who seek a test are able to obtain a test with minimal delays, followed by prompt receipt of results. In this sample, almost 40% of those who wanted a test were not able to get tested; even in those tested, there were significant delays, and over half waited 3 or more days for results. To effectively curb transmission, these delays need to be addressed.
We were limited in our ability to generalize results, because the sample cannot necessarily be considered to be representative of Maryland state. Indeed, self-reported positivity was more than double that estimated among those 18 and older by case-count data (2.5%) [26]. It is important to note, however, that there has not yet been a seroprevalence study in Maryland, and that case count data are subject to many biases, including who can access a test and how this access has changed over time. Most seroprevalence studies have demonstrated that prevalence is 6–24 times higher than what has been estimated by case count data [27]. Regardless, it is important to note that by using quotas for various key demographic characteristics, online samples such as ours can be structured to recruit samples with demographic distributions comparable to the target population [28]. Notably, despite the higher overall prevalence as compared to the case count data prevalence, the self-reported positivity rates reflect the distribution of cases in Maryland [18], with higher positivity among men, Hispanics, African-Americans, and younger populations. Also of importance, the proportion of respondents in the sample who reported taking the flu vaccine last year was 53.1% (data not shown), compared to the CDC [29] estimate of 52.3% in the 2018–19 flu season, suggesting this approach yields similar results as other commonly used approaches, such as random digit dialing.
We were additionally limited because individuals required Internet connectivity to participate; however, Internet access has been improving and has been facilitated by recent discounts offered by major providers. It is estimated that 86% of Maryland residents have Internet connectivity [30]. The sample also likely misses homeless populations and very low–income groups, 2 populations where NPI adoption may be especially challenging [31]. Among those with Internet connectivity, it is not possible to sample randomly, and the “frame error” of those willing to participate in such panels is likely large but cannot be proven to be systematic.
Despite these limitations, several advantages of the approach are also noteworthy. This sample of 1030 respondents was recruited in under 2 weeks at a cost of $3000. In a rapidly evolving epidemic where behaviors are constantly changing, this approach did not require face-to-face visits, maximizing participant safety and minimizing administration costs. Finally, any biases will likely remain constant over time, allowing for examining trends longitudinally in serial, cross-sectional samples using the same method. To monitor these trends, we developed an online interactive dashboard (sclipman.github.io/PandemicPulse).
In conclusion, we present a rapid, cost-efficient approach of monitoring NPI adoption and adherence, which can help inform public health responses. While our survey illustrated this approach within a single state, the rapidity and efficiency of this methodology can be replicated in other settings, recognizing the highly variable and geographically localized SARS-CoV-2 transmission patterns and risk mitigation responses. Repeating these surveys over time can further unveil additional insights around changes in population behaviors, potentially informing adaptive responses to evolving disease dynamics. Overall, these data continue to highlight the role of movement and social distancing on SARS-CoV-2 transmission risk, and support public health messaging that strict social distancing during most activities can mitigate SARS-CoV-2 transmission. In Maryland, these data support targeted messaging to young adults, given their high rates of positivity and lower rates of NPI adoption; establishing partnerships with faith-based organizations could also be critical to curbing spread. Moreover, measures need to be implemented to make public transportation safe and to improve access to SARS-CoV-2 testing. Continued monitoring of NPI adoption, access to testing, and the subsequent impact on SARS-CoV-2 transmission in Maryland, as well as more broadly, will be critical for pandemic control.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
ciaa1313_suppl_Supplemental_Material
Notes
Acknowledgments. The authors thank Mr Adebola Adegbesan, who worked closely with the authors in the recruitment of the study sample, and Ms Hannah Manley, who assisted with data cleaning.
Disclaimer. The content is solely the responsibility of the authors and does not necessarily represent the official views of Johns Hopkins University or the National Institutes of Health.
Financial support. This work was supported by the Johns Hopkins Coronavirus Disease 2019 (COVID-19) Research Response Program. S. S. S. reports grants/products and advisory board fees from Gilead Sciences and grants/products from Abbott Diagnostics, outside the submitted work, and is funded by National Institute on Drug Abuse (grant number DP2DA040244). A. P. W. is funded by a Career Award at the Scientific Interface by the Burroughs Wellcome Fund and by the National Library of Medicine of the National Institutes of Health (grant number DP2LM013102).
Potential conflicts of interest. S. H. M. reports personal fees from Gilead Sciences, outside the submitted work. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
Articles from Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America are provided here courtesy of Oxford University Press
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1093/cid/ciaa1313
Article citations
The Impact of the Coronavirus Disease 2019 Pandemic on US Total Knee and Hip Arthroplasty Procedures in 2020.
Arthroplast Today, 27:101348, 23 Apr 2024
Cited by: 0 articles | PMID: 38690096 | PMCID: PMC11058713
The changing contributory role to infections of work, public transport, shopping, hospitality and leisure activities throughout the SARS-CoV-2 pandemic in England and Wales.
NIHR Open Res, 3:58, 03 Nov 2023
Cited by: 0 articles | PMID: 39286314 | PMCID: PMC11403290
Racial and ethnic disparities in COVID-19 diagnosis and adherence to mitigation behaviours in a national United States older adult sample.
Epidemiol Infect, 151:e175, 06 Oct 2023
Cited by: 2 articles | PMID: 37799056 | PMCID: PMC10600897
Exploring the COVID-19 Knowledge, Attitudes, and Practices (KAPs) in the Black Community: a Scoping Review.
J Racial Ethn Health Disparities, 11(1):273-299, 09 Feb 2023
Cited by: 4 articles | PMID: 36757610 | PMCID: PMC9910259
Review Free full text in Europe PMC
Erroneous Consonance. How inaccurate beliefs about physician opinion influence COVID-19 vaccine hesitancy.
Vaccine, 41(12):2093-2099, 20 Feb 2023
Cited by: 3 articles | PMID: 36822967 | PMCID: PMC9939402
Go to all (25) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Disparities and Temporal Trends in COVID-19 Exposures and Mitigating Behaviors Among Black and Hispanic Adults in an Urban Setting.
JAMA Netw Open, 4(9):e2125187, 01 Sep 2021
Cited by: 9 articles | PMID: 34581798 | PMCID: PMC8479580
Factors Associated with the Implementation of Non-Pharmaceutical Interventions for Reducing Coronavirus Disease 2019 (COVID-19): A Systematic Review.
Int J Environ Res Public Health, 18(8):4274, 17 Apr 2021
Cited by: 31 articles | PMID: 33920613 | PMCID: PMC8072790
Review Free full text in Europe PMC
Public Perceptions and Attitudes Toward COVID-19 Nonpharmaceutical Interventions Across Six Countries: A Topic Modeling Analysis of Twitter Data.
J Med Internet Res, 22(9):e21419, 03 Sep 2020
Cited by: 50 articles | PMID: 32784190 | PMCID: PMC7505256
Funding
Funders who supported this work.
Abbott Diagnostics
Burroughs Wellcome Fund
Gilead Sciences
Johns Hopkins Coronavirus Disease 2019 (COVID-19) Research Response Program
NIAID NIH HHS (1)
Grant ID: R01 AI160780
NIDA NIH HHS (2)
Grant ID: DP2DA040244
Grant ID: DP2 DA040244
NLM NIH HHS (1)
Grant ID: DP2 LM013102