Abstract
Free full text

COVID-19 conspiracy beliefs, health behaviors, and policy support
Abstract
Conspiracy theories have been proliferating during the COVID-19 pandemic. Evidence suggests that belief in conspiracy theories undermines engagement in pro-health behaviors and support for public health policies. Moreover, previous work suggests that inoculating messages from opinion leaders that expose conspiracy theories as false before people are exposed to them can help to prevent belief in new conspiracies. Goals of this study were to: (a) explore associations between COVID-19 conspiracy beliefs with SARS-CoV-2 vaccine intentions, cooperation with public health recommendations, and support for public health policies among U.S. adults and (b) investigate trusted sources of COVID-19 information to inform strategies to address conspiracy beliefs. A cross-sectional, online survey was conducted with 845 U.S. adults in April 2020. Data were analyzed using analyses of variance and multivariable regressions. One-third (33%) of participants believed one or more conspiracies about COVID-19. Participants who believed conspiracies reported that their intentions to vaccinate were 3.9 times lower and indicated less support for COVID-19 public health policies than participants who disbelieved conspiracies. There were no differences in cooperation with public health recommendations by conspiracy belief endorsement in the multivariable regression analysis. Although there were some key differences in trusted sources of COVID-19 information, doctor(s) were the most trusted source of information about COVID-19 overall with 90% of participants trusting doctor(s). Doctor(s) may play a role in addressing COVID-19 conspiracy theories before people are exposed to them to promote COVID-19 prevention efforts.
Conspiracy theories have been proliferating rapidly during the COVID-19 pandemic, including that COVID-19 is part of a government bioweapons program, 5G cell towers are spreading COVID-19, and pharmaceutical companies are encouraging the spread of COVID-19 for profit [1,2]. Conspiracy theories are explanations of significant events as secret plots concocted by powerful and malevolent institutions, groups, and/or people [3,4]. Evidence suggests that belief in conspiracy theories undermines engagement in pro-health behaviors and support for public health policies, including within the contexts of previous disease outbreaks, such as Ebola [4,5]. Understanding the impacts of conspiracy beliefs on pro-health behaviors and policy support in the context of COVID-19 is critical for informing COVID-19 prevention and treatment strategies. The current study, therefore, explored associations between conspiracy beliefs and pro-health behaviors and policy support during the beginning of the COVID-19 pandemic in the USA.
Conspiracy theories help to satisfy social-psychological motives, including epistemic (understanding one’s environment), existential (feeling safe and in control), and social (maintaining positive images of one’s self and group) motives [3]. Particularly relevant to the COVID-19 pandemic, conspiracy theories satisfy an existential motive by helping people feel safe in their environment. Supporting this, evidence suggests that people are more likely to believe conspiracy theories when they feel anxious, powerless, and unable to control their outcomes [3], as well as in times of crisis and when faced with large-scale events with serious consequences [6]. Pandemics such as COVID-19 are powerful contexts wherein individuals may turn to conspiracy theories in an attempt to restore feelings of safety and control. Medical conspiracy beliefs are additionally rooted partly in medical mistrust or a general suspicion of and lack of confidence in medical organizations and providers [5,7]. Medical conspiracy theories were prevalent in the USA even before the start of the COVID-19 pandemic. A nationally representative study conducted in 2013 suggested that most U.S. adults were aware of at least one of six popular medical conspiracy theories (e.g., the Food and Drug Administration is preventing access to cures to disease due to pressure from pharmaceutical companies) and 49% of adults agreed with one or more theory [4].
People who believe conspiracies are less likely to engage in a variety of pro-health behaviors [4]. As examples, people who endorse conspiracy beliefs are less likely to get annual physical exams, visit the dentist, and use sunscreen [4]. In the context of COVID-19, considerable hope is being placed on the promise of a SARS-CoV-2 vaccine to end the COVID-19 pandemic. Yet, conspiracy beliefs have undermined vaccination efforts to such a degree that they have been implicated in recent resurgences of polio and measles [8,9]. Some preliminary evidence suggests that COVID-19 conspiracy beliefs are associated with a lower rate of compliance with public health guidance to prevent the spread of COVID-19, such as minimizing time spent outside the home, maintaining social distance from people outside of one’s household, and handwashing [10,11].
People who believe conspiracies may also be less supportive of public health policies to address pandemics. Underlying conspiracy beliefs is a distrust of public institutions [12,13]. Thus, people who believe conspiracies may oppose public health policies that empower the very public institutions that they distrust. During the 2014 Ebola epidemic, people who believed in conspiracy theories about Ebola reported less support for quarantine policies [5]. Associations between conspiracy beliefs and policy support may be concerning given that it has been argued that misperceptions and mistrust among the public swayed public policy responses to Ebola and may be particularly influential during election periods [14].
It is possible to address conspiracy beliefs, but the timing and source of intervention content appear to be keys to intervention success. Previous work suggests that inoculating messages, which expose conspiracy theories as false before people are exposed to them, can help to prevent belief in new conspiracies and enhance vaccine intentions [15,16]. Moreover, messages from opinion leaders denouncing conspiracy beliefs may be particularly effective [15,16]. Therefore, identifying opinion leaders who are trusted by people who believe conspiracies may inform intervention strategies to inoculate against belief in conspiracy theories. There have been many leaders sharing information during the COVID-19 pandemic, including individuals on social media, President Trump, representatives from state and local governments, Anthony Fauci (the director of the National Institute of Allergy and Infectious Diseases), and doctor(s).
The current study explored associations between COVID-19 conspiracy beliefs and SARS-CoV-2 vaccine intentions, cooperation with public health recommendations, and support for public health policies among U.S. adults. It was hypothesized that people who believed COVID-19 conspiracies would report lower vaccine intentions, cooperation with public health recommendations, and support for public health policies surrounding COVID-19. Additionally, the study investigated trusted sources of information about COVID-19 to inform strategies to intervene in conspiracy beliefs.
Methods
Procedures and participants
U.S. adults aged 18 or older were invited to participate in an online, cross-sectional survey on April 13–14, 2020, advertised on Amazon Mechanical Turk, a crowdsourcing website that can be used to connect researchers with participants [17,18]. The survey included 109 items and took an average of 10.56 min to complete, and participants were compensated $2. Participants were excluded if they reported having experienced COVID-19 (n = 72), failed data screens (n = 20), completed the survey in less than 3 min (n = 14), or completed multiple surveys from the same IP address (n = 29). Of the 980 people who completed the survey, 845 were included in analyses. The study received institutional review board approval from the University of Delaware, and participants provided electronic informed consent.
Measures
Given that validated scales to measure COVID-19 related constructs were generally not yet available in April 2020, we adapted measures from previous studies of infectious diseases (e.g., HIV; [19]), as well as COVID-19 surveys conducted by research and news organizations [19,20]. Items were tailored based on information and recommendations regarding COVID-19 available at the time [19,21,22]. Supplementary Appendix A includes all COVID-19 measures used in this study.
Conspiracy beliefs were measured with six items modeled after a measure of HIV conspiracy beliefs [23]. Items included: “The coronavirus is a myth to force vaccinations on people,” “There is no such thing as the coronavirus,” “Coronavirus was developed by the government as part of a bioweapons program,” “Big Pharma is encouraging the spread of coronavirus to make money,” “5G is causing the coronavirus,” and “The government could cure coronavirus, but chooses not to for financial gain.” Participants indicated whether they agreed or disagreed with each belief. Consistent with previous work focusing on whether individuals disbelieve or believe conspiracies [4], a conspiracy belief variable was created by categorizing responses to represent disagreement with all conspiracy beliefs versus agreement with one or more conspiracy beliefs. Modeled after a poll conducted by NPR, PBS NewsHour, and Marist, participants were asked about the extent that they trusted several sources of information about COVID-19, including from social media, President Trump, state and local governments, Anthony Fauci, and their doctor(s) on scales from not at all (1) to a great deal (4) [20].
Intentions to access a COVID-19 vaccination was assessed with the item: “When a vaccine becomes available for the coronavirus, how likely are you to get it?” Participants indicated likelihood on a five-point Likert-type scale. To aid with interpretability of results and comparison to previous work on conspiracy beliefs and vaccination [4], responses were dichotomized to represent whether participants were likely (including responses somewhat likely, likely, and very likely) or unlikely (including responses unlikely and not at all likely) to access the vaccine. Participants were asked about the extent to which they were complying with public health recommendations with eight items modeled after a similar measure by RTI International [19]. Participants indicated whether they were washing their hands for 20 s, using disinfectants, staying home as much as possible, avoiding public places, wearing a face covering in public, staying 6 feet or more away from others in public, covering their mouth and nose when they cough and sneeze, and cleaning frequently touched surfaces daily on a scale from never (1) to always (5). A mean score was created (Cronbach’s α = 0.84). A six-item measure of support for COVID-19-related public policies was modeled after a similar measure by RTI International [19], updated with items reflecting policies described by the National Governors Association [21]. Participants indicated whether they supported stay-at-home or shelter-in-place orders, canceling or postponing mass gatherings, school closures, workplaces and businesses temporarily closing, travel bans, and closures of nonessential businesses. Responses were provided on a Likert-type scale ranging from strongly disagree (1) to strongly agree (5). A mean score was created (Cronbach’s α = 0.93).
Additionally, several variables were measured and included as controls within analyses. Knowledge about COVID-19 was measured with 10 items, including facts about COVID-19 (e.g., “Most people who are infected with the coronavirus recover from it”) that participants indicated were true (1), false (0), or did not know the answer (0) [19,22]. A proportion of correct knowledge answers was calculated. Medical mistrust was measured with seven items from a validated scale (e.g., “You’d better be cautious when dealing with health care organizations”), with responses ranging from strongly disagree (1) to strongly agree (4) [7]. A mean score was calculated (Cronbach’s α = 0.88). Participants reported sociodemographic characteristics, including their age, gender, race/ethnicity, and education. Participants also reported what state they resided in, which was coded to represent regions of the U.S., including the Northeast (CT, MA, ME, NH, NJ, NY, PA, RI, and VT), Southeast (AL, AR, DC, DE, FL, GA, KY, LA, MD, MS, NC, SC, TN, VA, and WV), Midwest (IA, IL, IN, KS, MI, MN, MO, ND, NE, OH, SD, and WI), Southwest (AZ, NM, OK, and TX), and West (AK, CA, CO, HI, ID, MT, NC, OR, UT, WA, and WY).
Statistical Analysis
Participant sociodemographic characteristics, related psychosocial constructs, intentions to access a COVID-19 vaccine, compliance with public health recommendations, and COVID-19 public health policy support were explored stratified by whether participants believed versus disbelieved conspiracy belief(s) using t-testsand chi-square tests. Trusted sources of COVID-19 information by conspiracy belief endorsement was explored via bar graphs and analyses of variance. Associations between conspiracy belief endorsement with pro-health behaviors and policy support were examined with logistic and linear regression analyses controlling for relevant psychosocial constructs (i.e., knowledge and medical mistrust) and sociodemographic characteristics (i.e., age, gender, race, education, and U.S. region). All analyses were conducted using SPSS version 26.0.
Results
One-third (33.0%) of the participants reported agreeing with one or more conspiracy beliefs. Participants who believed conspiracies agreed with an average of 3.11 conspiracy beliefs (standard deviation = 1.80). As shown in Table 1, participants who believed conspiracies were slightly younger than participants who disbelieved conspiracies. A higher percentage of participants identifying as Black and other races/ethnicities and a higher percentage of participants with college degree(s) believed conspiracies than participants who disbelieved conspiracies. A higher percentage of participants from the Southwest and West believed conspiracies than participants who were from the Midwest, Northeast, and Southeast. Participants who believed conspiracies also had less knowledge about COVID-19 and reported greater medical mistrust than participants who disbelieved conspiracies. Seventy-two point nine percent of participants who believed conspiracies intended to get a COVID-19 vaccine in contrast to 92.0% of participants who disbelieved conspiracies. Participants who believed conspiracies reported complying with public health recommendations to a lesser extent and were less supportive of COVID-19 public health policies than participants who disbelieved conspiracies.
Table 1
| Descriptive statistics stratified by conspiracy belief endorsement
| Total sample | Conspiracy disbelief | Conspiracy belief | Difference | |
|---|---|---|---|---|
| % (N) or M (SD) | % (n) or M (SD) | % (n) or M (SD) | t(df) or X2(df) | |
| Sample size | 100 (845) | 67.0 (566) | 33.0 (279) | |
| Sociodemographic characteristics | ||||
| Age (range: 18–74) | 40.15 (11.67) | 40.85 (11.92) | 38.71 (11.04) | t(829) = 2.48* |
| Gender (%) | ||||
 Man Man | 58.6 (495) | 57.8 (327) | 60.2 (168) | X 2(2) = 1.07 |
 Woman Woman | 40.9 (346) | 41.9 (237) | 39.1 (109) | |
 Nonbinary Nonbinary | 0.48 (4) | 0.4 (2) | 0.7 (2) | |
| Race/ethnicity (%) | X 2 (4) = 30.09** | |||
 Asian Asian | 3.6 (30) | 3.7 (21) | 3.2 (9) | |
 Black Black | 10.2 (86) | 7.1 (40) | 16.5 (46) | |
 Latinx Latinx | 3.0 (25) | 2.7 (15) | 3.6 (10) | |
 White White | 77.0 (651) | 82.0 (464) | 67.0 (187) | |
 Other Other | 6.3 (53) | 4.6 (26) | 9.7 (27) | |
| Education (%) | X 2 (2) = 5.05* | |||
 High school degree or less High school degree or less | 22.7 (191) | 25.0 (141) | 18.1 (50) | |
 College degree(s) College degree(s) | 77.3 (651) | 75.0 (424) | 81.9 (227) | |
| U.S. region | X 2 (4) = 42.67** | |||
 Midwest Midwest | 19.8 (166) | 22.3 (125) | 14.8 (41) | |
 Northeast Northeast | 21.4 (179) | 25.0 (140) | 14.1 (39) | |
 Southeast Southeast | 32.0 (268) | 32.4 (182) | 31.0 (86) | |
 Southwest Southwest | 11.8 (99) | 8.7 (49) | 18.1 (50) | |
 West West | 15.0 (126) | 11.6 (65) | 22.0 (61) | |
| Psychosocial constructs | ||||
 COVID-19 knowledge (proportion) COVID-19 knowledge (proportion) | 0.87 (0.20) | 0.95 (0.10) | 0.70 (0.25) | t(843) = 20.46** |
 Medical mistrust (range: 1–4) Medical mistrust (range: 1–4) | 1.98 (0.87) | 2.39 (0.60) | 3.03 (0.47) | t(842) = −15.58** |
| COVID-19 outcomes | ||||
 Likely to get COVID-19 vaccine (%) Likely to get COVID-19 vaccine (%) | 85.8 (723) | 92.0 (521) | 72.9 (277) | X 2 (1) = 55.72** |
 Public health recommendation compliance Public health recommendation compliance | 3.42 (0.511) | 3.48 (0.46) | 3.28 (0.57) | t(843) = 5.45** |
 COVID-19 public health policy support COVID-19 public health policy support | 3.52 (0.62) | 3.63 (0.57) | 3.29 (0.65) | t(843) = 7.65** |
df degrees of freedom; SD standard deviation.
*p ≤ .05, **p ≤ .01.
As shown in Table 2, results of logistic and linear regression analyses suggested that participants who believed conspiracies reported that they were 3.93 times less likely to get a COVID-19 vaccine once one became available. Women, as well as participants with a high school education or less, also reported that they would be less likely to get a vaccine. Conspiracy beliefs were not associated with public health recommendation compliance in the multivariable analysis. Participants with less COVID-19 knowledge, men, white participants, participants with a high school education or less, and participants from the Midwest and West reported complying with public health recommendations to a lesser extent. Conspiracy beliefs were associated with less COVID-19 public health policy support. Participants with less COVID-19 knowledge and participants with a high school education or less also reported less COVID-19 public health policy support.
Table 2
| Logistic and linear regressions predicting COVID-19 outcomes
| Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|
| COVID-19 vaccine likelihood | Public health recommendation compliance | COVID-19 public health policy support | |||||
| B (SE) | OR | 95% CI | B (SE) | Beta | B (SE) | Beta | |
| Conspiracy belief endorsement | −1.37 (0.28) | 0.26** | 0.15–0.44 | −0.04 (0.05) | −0.04 | −0.14 (0.06) | −0.11* |
| Psychosocial controls | |||||||
 COVID−19 knowledge COVID−19 knowledge | 0.92 (0.56) | 2.51 | 0.84–7.49 | 0.74 (0.11) | 0.29** | 0.79 (0.13) | 0.26** |
 Medical mistrust Medical mistrust | −0.07 (0.20) | 0.71 | 0.63–1.37 | 0.02 (0.03) | 0.02 | −0.02 (0.04) | −0.02 |
| Sociodemographic characteristics | |||||||
 Age Age | −0.01 (0.01) | 0.99 | 0.98–1.02 | 0.01 (0.01) | 0.04 | 0.01 (0.01) | 0.01 |
 Gender: man Gender: man | 0.45 (0.22) | 1.56* | 1.02–2.39 | −0.16 (0.03) | −0.16** | −0.08 (0.04) | −0.06 |
 Race: Black Race: Black | −0.47 (0.32) | 0.63 | 0.33–1.18 | 0.14 (0.06) | 0.09* | 0.13 (0.07) | 0.06 |
 Race: Asian, Latino(a), Other Race: Asian, Latino(a), Other | −0.07 (0.32) | 0.93 | 0.49–1.75 | 0.06 (0.05) | 0.04 | 0.05 (0.06) | 0.03 |
 Education: high school or less Education: high school or less | −0.89 (0.25) | 0.41** | 0.25–0.66 | −0.09 (0.04) | −0.07* | −0.10 (0.05) | −0.07* |
 U.S. region: Midwest U.S. region: Midwest | 0.39 (0.34) | 1.47 | 0.75–2.87 | −0.16 (0.05) | −0.13** | −0.11 (0.06) | −0.07 |
 U.S. region: Southeast U.S. region: Southeast | 0.05 (0.29) | 1.06 | 0.60–1.86 | −0.09 (0.05) | −0.08 | −0.07 (0.06) | −0.05 |
 U.S. region: Southwest U.S. region: Southwest | 0.85 (0.44) | 2.34 | 1.00–5.56 | −0.04 (0.06) | −0.03 | −0.04 (0.08) | −0.02 |
 U.S. region: West U.S. region: West | 0.45 (0.36) | 1.57 | 0.77–3.20 | −0.13 (0.06) | −0.09* | −0.04 (0.07) | −0.02 |
| Constant | 1.73 (0.85) | 5.62* | 2.85 (0.15) | 3.02 (0.18) |
CI confidence interval; OR odds ratio; SE standard error.
*p ≤ .05, **p ≤ .01.
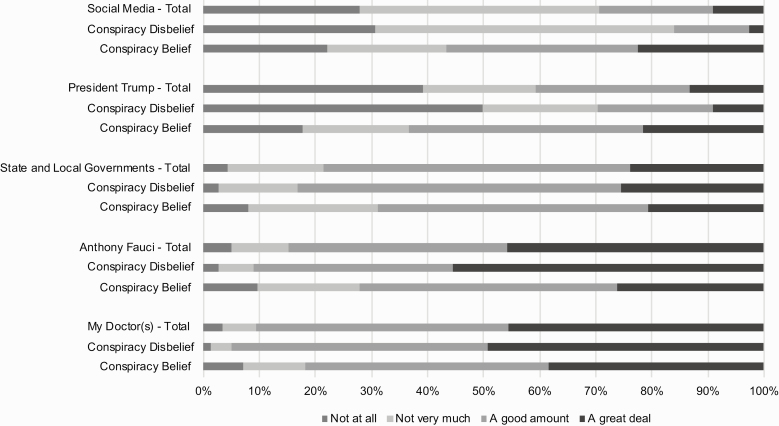
As shown in Fig. 1, participants who believed conspiracies reported greater trust in COVID-19 information from social media (F(1,844) = 120.94, p < .01, Cohen’s d = 0.51) and President Trump (F(1,843) = 108.80, p < .01, Cohen’s d = 0.76) in comparison to participants who disbelieved conspiracies. Participants who believed conspiracies reported slightly less trust in information from state and local governments (F(1,843) = 19.61, p < .01, Cohen’s d = 0.32), Anthony Fauci (F(1,844) = 91.82, p < .01, Cohen’s d = 0.69), and their doctor(s) (F(1,841) = 31.04, p < .01, Cohen’s d = 0.41). Despite these differences, participants who believed conspiracies reported having the most trust in COVID-19 information from their doctor(s). In this sample, 90.6% of all participants reported trusting information about COVID-19 from their doctor(s) “a good amount” or “a great deal.”
Discussion
Results of this study suggest that COVID-19 conspiracy beliefs may act as a barrier to some COVID-19 pro-health behaviors and policy support. Specifically, participants who believed one or more conspiracies about COVID-19 were close to four times less likely to report that they intended to get a SARS-CoV-2 vaccine once one becomes available and expressed less support of policies to prevent the spread of COVID-19 than participants who disbelieved conspiracies. These results replicate findings from previous studies, demonstrating that conspiracy beliefs undermine vaccination efforts [8,9] and policy support during disease outbreaks [5]. Preliminary evidence from studies conducted during the COVID-19 pandemic has suggested that conspiracy beliefs are additionally associated with less compliance with public health recommendations to prevent the spread of COVID-19 [10,11]. Although bivariate results of this study replicated these findings, the association became nonstatistically significant in multivariable analyses controlling for sociodemographic characteristics and psychosocial constructs (e.g., COVID-19 knowledge). Further replicating previous research [5], participants of the current study who believed conspiracies had greater medical mistrust and less COVID-19 knowledge than participants who disbelieved conspiracies.
Results of this study additionally provide insight into trusted sources of COVID-19 information among participants who believe versus disbelieve COVID-19 conspiracies. Participants who believed conspiracies reported that they trusted information about COVID-19 from social media and President Trump to a greater extent than participants who disbelieved conspiracies. Of concern, conspiracy theories appear to thrive on the internet and social media. For example, conspiracy theories and other forms of misinformation proliferated and quickly spread on Twitter during the 2014 Ebola outbreak [24]. Despite these differences, over 80% of participants who believed conspiracies and over 90% of participants who disbelieved conspiracies reported that they trusted information about COVID-19 from their doctor(s). This replicates a nationally representative poll conducted in 2019 indicating that over 90% of U.S. adults trust information about medical topics from doctors and other health care professionals [25]. Insight into trusted sources of information about COVID-19 may inform intervention efforts to address COVID-19 conspiracy beliefs.
Strengths, limitations, and future directions
This study was conducted at the beginning of the COVID-19 pandemic in the USA to gain rapid insight into associations between COVID-19 conspiracy beliefs, which had been proliferating rapidly during the pandemic, and pro-health behaviors and policy support. Such work can inform understanding of the extent to which conspiracy beliefs may undermine prevention and treatment efforts during the COVID-19 pandemic, as well as future disease outbreaks. The study is limited by its nonrepresentative convenience sample and investigation into an intended health behavior. Moreover, information regarding who or how many people declined to participate in the study is unavailable. Yet, these findings appear to replicate some findings from previous work with representative samples and measuring engagement in actual pro-health behaviors. For example, there was a 19% gap in SARS-CoV-2 vaccine intentions between participants who disbelieved versus believed COVID-19 conspiracies in this study. A previous nationally representative study documented a 14% gap in influenza vaccine uptake among participants who disbelieved medical conspiracies versus believed three or more medical conspiracies [4]. Similarly, over 90% of the overall sample trusted information about COVID-19 from their doctor(s), similar to a recent nationally representative poll in which over 90% of U.S. adults reported trusting information about medical topics from doctors and other health care professionals [25]. However, this study found that education was associated with greater endorsement of conspiracy beliefs in contrast to other work that has found that education is associated with lower endorsement of conspiracy beliefs [3]. Future work should continue to investigate the role of conspiracy beliefs in COVID-19 pro-health behaviors using representative samples with diverse educational backgrounds and medical record data when they become available.
Future work is also needed to validate measures in the context of COVID-19. Results of this study did not replicate findings from two initial studies suggesting that conspiracy beliefs are associated with less compliance with public health recommendations to prevent COVID-19 [10,11]. This may be, in part, due to differences in measures of conspiracy beliefs and public health recommendation compliance. Associations between conspiracy beliefs and pro-health behaviors may also change as the pandemic evolves. For example, the extent to which people are staying at home, avoiding public places, and wearing face coverings is changing as local policies and perceptions of the pandemic evolve. Longitudinal work can help to clarify associations between conspiracy beliefs on pro-health behaviors and policy support as the COVID-19 pandemic evolves.
Conclusions
It may be important to identify people who are at risk of believing conspiracies, prevent the development of new conspiracy beliefs, and dispel existing conspiracy beliefs to promote COVID-19 intervention strategies. Of note, considerable hope is being placed on the promise of a SARS-CoV-2 vaccine to end the COVID-19 pandemic. Scientists are undertaking intense research and development activities globally to discover and implement an effective vaccine [26], and top public health officials are “cautiously optimistic” that a vaccine will become available [27]. Yet, these results suggest that conspiracy beliefs can be a barrier to vaccine uptake, similar to previous epidemics [9].
Inoculating messages from trusted opinion leaders can help to prevent belief in new conspiracies and enhance vaccine intentions [15,16]. Doctors were among the most trusted sources of COVID-19 information among all participants in this sample. Even participants who believed conspiracies trusted information about COVID-19 from their doctors more than from other sources, including from social media where conspiracy beliefs have proliferated during previous epidemics [24]. Doctors might play a role in educating the public about COVID-19 to inoculate them against COVID-19 conspiracies and dispel existing conspiracy beliefs [28]. Additionally, psychologists and other social and behavioral health experts are needed to continue to investigate strategies to address these beliefs. Multiple strategies are particularly needed given that not everyone has access to doctors and some doctors are publicly perpetuating COVID-19 conspiracy theories. Identifying and leveraging other sources of trusted health information may be important. History teaches us that our efforts to prevent and treat COVID-19 may be stunted unless conspiracy beliefs are proactively addressed.
Supplementary Material
ibaa090_suppl_Supplementary_Appendix_A
Acknowledgment
The authors are grateful to Kristina Holsapple for her assistance with survey programming.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare that they have no conflicts of interest.
Authors’ Contributions
V.A.E., N.M.B., E.C.H. and A.B.F. conceptualized the design of the study and acquired the data. V.A.E. and A.B.F. analyzed the data. All authors contributed to the interpretation of the data. V.A.E. drafted the manuscript and all authors revised it critically for important intellectual content. All authors approved the final version of this manuscript and agree to be accountable for all aspects of the work.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
Full text links
Read article at publisher's site: https://doi.org/10.1093/tbm/ibaa090
Read article for free, from open access legal sources, via Unpaywall:
https://academic.oup.com/tbm/article-pdf/10/4/850/33852211/ibaa090.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1093/tbm/ibaa090
Article citations
Association between beliefs in medical conspiracy theories and health behaviors among medical and healthcare students. Implications for professional practice.
BMC Med Educ, 24(1):1062, 28 Sep 2024
Cited by: 0 articles | PMID: 39342242 | PMCID: PMC11439324
COVID-19 Vaccine Hesitancy and Misinformation Endorsement among a Sample of Native Spanish-Speakers in the US: A Cross-Sectional Study.
Healthcare (Basel), 12(15):1545, 05 Aug 2024
Cited by: 0 articles | PMID: 39120248 | PMCID: PMC11311759
Understanding Reasons for Vaccination Hesitancy and Implementing Effective Countermeasures: An Online Survey of Individuals Unvaccinated against COVID-19.
Vaccines (Basel), 12(5):499, 05 May 2024
Cited by: 0 articles | PMID: 38793750 | PMCID: PMC11125705
COVID-19 vaccine hesitancy among adults in Liberia, April-May 2021.
PLoS One, 19(4):e0297089, 17 Apr 2024
Cited by: 0 articles | PMID: 38630778 | PMCID: PMC11023583
Acceptance and expectations of healthcare workers and community during the COVID-19 vaccine rollout in Bhavnagar city, western India: a qualitative exploration.
BMC Health Serv Res, 24(1):386, 27 Mar 2024
Cited by: 0 articles | PMID: 38539125 | PMCID: PMC10976747
Go to all (158) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S.
Soc Sci Med, 263:113356, 21 Sep 2020
Cited by: 370 articles | PMID: 32967786 | PMCID: PMC7502362
Patterns of Media Use, Strength of Belief in COVID-19 Conspiracy Theories, and the Prevention of COVID-19 From March to July 2020 in the United States: Survey Study.
J Med Internet Res, 23(4):e25215, 27 Apr 2021
Cited by: 46 articles | PMID: 33857008 | PMCID: PMC8083953
Cultural orientation, power, belief in conspiracy theories, and intentions to reduce the spread of COVID-19.
Br J Soc Psychol, 59(3):663-673, 27 Jun 2020
Cited by: 137 articles | PMID: 32592420 | PMCID: PMC7361833
Antecedents and consequences of COVID-19 conspiracy beliefs: A systematic review.
Soc Sci Med, 301:114912, 14 Mar 2022
Cited by: 89 articles | PMID: 35354105 | PMCID: PMC8920084
Review Free full text in Europe PMC
Funding
Funders who supported this work.