Abstract
Free full text

COVID‐19 pneumonia in a pediatric sickle cell patient requiring red blood cell exchange
Abstract
Patients with sickle cell disease are already at high risk for respiratory complications, which SARS‐CoV‐2 can rapidly worsen. The case emphasizes the importance of efficiently maximizing standard therapies in sickle cell patients with COVID‐19.
Abstract
Patients with sickle cell disease are already at high risk for respiratory complications, which SARS‐CoV‐2 can rapidly worsen. The case emphasizes the importance of efficiently maximizing standard therapies in sickle cell patients with COVID‐19.
1. INTRODUCTION
We report the case of a 10‐year‐old girl with sickle cell disease who developed COVID‐19 and acute chest syndrome who required red blood cell exchange and remdesivir treatment. The case highlights the importance of maximizing standard therapies; notably, this patient improved without steroids or immunosuppressive therapies.
Patients with sickle cell disease experience a variety of complications related to the underlying pathophysiology of the disease. Common complications include acute chest syndrome (ACS), vaso‐occlusive pain crises, splenic sequestration, and immune suppression due to functional asplenia. 1 Acute chest syndrome is one of the leading causes of death in patients with sickle cell disease. 1 Pediatric patients more commonly have ACS secondary to viral respiratory illnesses than adults; however, data from the 2009 H1N1 influenza pandemic demonstrate that certain viruses can be a trigger for ACS in both adult and pediatric patients. 2
SARS‐CoV‐2, the coronavirus strain that is causing the COVID‐19 pandemic, has also been shown to cause respiratory complications in both patients with and without sickle cell disease. Given that patients with sickle cell disease have a higher risk at baseline of respiratory complications, there is understandable concern regarding COVID‐19 infection in this population. There are minimal data on pediatric patients with sickle cell disease who develop COVID‐19 other than case reports. 3 , 4 We report the case of a pediatric patient with sickle cell disease who tested positive for SARS‐CoV‐2 and developed rapidly worsening respiratory distress.
2. CASE PRESENTATION
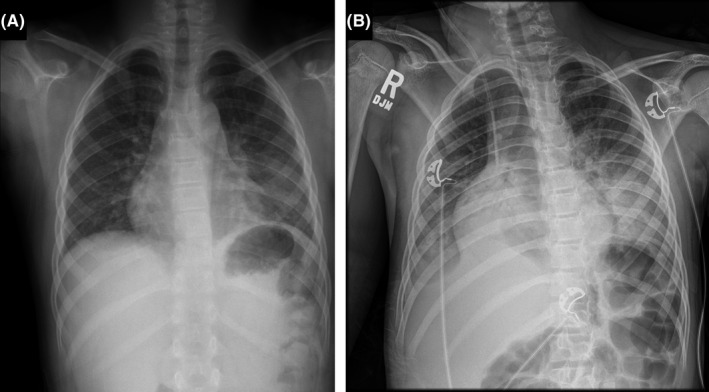
A 10‐year‐old girl with a known diagnosis of sickle cell disease (hemoglobin SS genotype) presented to the Monroe Carell Jr Children's Hospital at Vanderbilt Emergency Department with 1 day of fever and mild chest pain. Laboratories demonstrated a hemoglobin of 10.0 grams/deciliter with a reticulocyte count of 0.254 × 106 cells/microliter, consistent with her baseline levels. White blood cell count was normal. Chest radiograph revealed a left lower lung opacity, consistent with pneumonia and acute chest syndrome (Figure 1A). Polymerase chain reaction testing was positive for SARS‐CoV‐2. At the time of initial presentation, she was admitted and administered ceftriaxone and azithromycin. She continued to have fevers, but she did not require supplemental oxygen and had no evidence of respiratory distress. She was discharged home after 2 days of observation to complete a course of azithromycin and amoxicillin‐clavulanic acid.
On day five of symptoms, 2 days after discharge, the patient developed worsening fevers, as well as onset of vomiting, rapid breathing, and worsening chest pain. Upon representation to the emergency department, she was febrile to 39.6 degrees Celsius with a heart rate of 127 beats/minute, respiratory rate of 36 breaths/minute, and blood pressure of 124/76 millimeters of mercury (mm/Hg). Due to oxygen saturations as low as 82% on room air, she received supplemental oxygen at 2 liters/minute via nasal cannula. Chest X‐ray showed worsening bilateral opacities and left middle lobe opacification (Figure 1B). Per our protocol for patients with ACS, ceftriaxone and azithromycin were administered to cover common causative organisms. Clindamycin was added due to concern for a secondary staphylococcal infection. Laboratory analysis revealed a normal white blood cell count, hemoglobin of 8.7 grams/deciliter, and platelets of 517 × 103 cells/millimeter. 3 Reticulocyte count was 0.117 × 106 cells/microliter. She had a ferritin of 3899 nanograms/milliliter (mL) and C‐reactive protein of 115.1 micrograms/liter. Troponin‐I was <0.01 nanograms/mL, and quantitative D‐dimer was 7.74 micrograms/mL. Her hemoglobin S percentage was 77.1%. Overnight, she remained febrile and tachypneic despite antipyretics with a maximum temperature of 40 degrees Celsius, respiratory rate of 54 breaths/minute, and her oxygen requirement increased to 4 liters/minute. Laboratories demonstrated worsening anemia with hemoglobin of 7.2 grams/deciliter and reticulocyte count decreased from admission to 0.094 × 106 cells/microliter. White blood cell count and platelet count remained stable. Given her clinical decline and potential for further rapid decompensation, the decision was made to proceed with a red blood cell (RBC) exchange. She tolerated automated RBC exchange procedure without complication, with a postprocedure hemoglobin S percentage of 21.7%. She received a total of 857 milliliters of blood during the exchange process.
Remdesivir was started the day of exchange transfusion given her ongoing oxygen requirement, and she received a loading dose of 150 milligrams (mg) and then four subsequent daily doses of 75 mg for a total of five doses. Prophylactic dosing of enoxaparin (0.5 mg/kilogram/dose, given twice daily) was started due to the increased risk of thrombosis noted independently in adult patients with both COVID‐19 5 and sickle cell disease. 6
Following the automated RBC exchange, she continued to improve and weaned off oxygen support by day four in the hospital. She was discharged on day six of hospitalization and will follow‐up in our pediatric sickle cell clinic via telemedicine.
3. DISCUSSION
SARS‐CoV‐2 contributes to pulmonary disease by infecting the pulmonary capillary endothelial cells, which leads to a pulmonary inflammation response that contributes to pulmonary edema and impaired oxygen diffusion capacity across the alveolar‐capillary membrane. 7 The COVID‐19 inflammation response is also thought to result in microthrombi formation, leading to additional pulmonary damage. 7 Given that red blood cells from patients with sickle cell disease, who at baseline have decreased RBC oxygen carrying capacity, increased inflammation, and increased thrombotic complications, it is easy to postulate that the additive effects of COVID‐19 and sickle cell disease can lead to severe, rapid pulmonary decompensation.
Case series from France 3 and New York 4 have described small groups of pediatric patients with sickle cell disease diagnosed with COVID‐19 (seven and four patients total, respectively), with over half of the patients requiring automated RBC exchange transfusion (four from the French cohort and two from the New York cohort). All patients in these studies who underwent automated RBC exchange transfusion survived and had a favorable respiratory status at the time of hospital discharge. We hypothesize that the replacement of the sickle RBC cells with normal RBC cells via exchange transfusion will decrease the levels of pulmonary inflammation and increase oxygen carrying capacity in sickle cell patients with COVID‐19.
Given the paucity of information surrounding pediatric sickle cell patients diagnosed with COVID‐19, we took a proactive approach to management with RBC exchange transfusion on day two of her hospitalization along with remdesivir administration. 8 This patient is the only pediatric patient with sickle cell disease in the literature to receive remdesivir in conjunction with RBC exchange, which we believe together improved her outcome. We considered Multisystem Inflammatory Syndrome in Children (MIS‐C); however, her inflammatory laboratories were difficult to interpret in the setting of ACS and the timing was felt to be more consistent with acute COVID‐19.
Data from adult patients with COVID‐19 also suggest that dexamethasone can improve outcomes in patients. 9 We elected to avoid steroid therapy, given the pediatric sickle cell data that suggest that steroids can contribute to increased pain and development of vaso‐occlusive crises, 10 , 11 and she continued to demonstrate overall improvement without this intervention.
As the COVID‐19 pandemic continues, it is likely that more pediatric patients with sickle cell disease will present with concurrent acute chest syndrome and COVID‐19 infection. We recommend early and aggressive treatment with standard therapies in pediatric patients with both sickle cell disease and COVID‐19. More prospective data are necessary to help pediatric providers consider the wide variety of both historical and novel treatment options and subsequently select the best combination for their patients with sickle cell disease.
CONFLICT OF INTEREST
The authors indicate they have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTIONS
Dr SCW and Dr MLM: conceptualized the study, drafted the initial manuscript, researched the literature, and reviewed and revised the manuscript. Dr HH and Dr DED: provided expert guidance on COVID‐19 and reviewed and revised the manuscript. Dr EJV: provided expert guidance on sickle cell disease and reviewed and revised the manuscript. Dr SCB: conceptualized the study and revised the manuscript critically for important intellectual content. All authors: approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
ETHICAL APPROVAL
The manuscript was drafted following written permission from the patient's parent.
ACKNOWLEDGMENTS
We gratefully acknowledge the patient and her family, as well as the efforts of the entire medical team involved in this patient's care.
Notes
Walker SC, Murphy ML, Hendricks H, Dulek DE, Volanakis EJ, Borinstein SC. COVID‐19 pneumonia in a pediatric sickle cell patient requiring red blood cell exchange. Clin Case Rep. 2021;9:1367–1370. 10.1002/ccr3.3774 [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
REFERENCES
Articles from Clinical Case Reports are provided here courtesy of Wiley
Full text links
Read article at publisher's site: https://doi.org/10.1002/ccr3.3774
Read article for free, from open access legal sources, via Unpaywall:
https://onlinelibrary.wiley.com/doi/pdfdirect/10.1002/ccr3.3774
Citations & impact
Impact metrics
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1002/ccr3.3774
Article citations
Clinical outcomes of COVID-19 in patients with sickle cell disease and sickle cell trait: A critical appraisal of the literature.
Blood Rev, 53:100911, 20 Nov 2021
Cited by: 29 articles | PMID: 34838342 | PMCID: PMC8605823
Review Free full text in Europe PMC
COVID-19 pneumonia in a pediatric sickle cell patient requiring red blood cell exchange.
Clin Case Rep, 9(3):1367-1370, 12 Jan 2021
Cited by: 2 articles | PMID: 33768846 | PMCID: PMC7981740
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Exchange red blood cell pheresis in a pediatric patient with severe complications of sickle cell anemia.
Transfusion, 21(4):443-446, 01 Jul 1981
Cited by: 6 articles | PMID: 7268869
Impact of COVID-19 Infection on 24 Patients with Sickle Cell Disease. One Center Urban Experience, Detroit, MI, USA.
Hemoglobin, 44(4):284-289, 28 Jul 2020
Cited by: 27 articles | PMID: 32722950
SARS-CoV-2 Infection Presenting as Acute Chest Syndrome in a Child With Hemoglobin SD-Los Angeles Disease: A Case Report and Review of Literature.
J Pediatr Hematol Oncol, 45(2):82-87, 26 Sep 2022
Cited by: 0 articles | PMID: 36162052
Review
COVID-19 in pediatric oncology from French pediatric oncology and hematology centers: High risk of severe forms?
Pediatr Blood Cancer, 67(7):e28392, 08 May 2020
Cited by: 49 articles | PMID: 32383827 | PMCID: PMC7235489

 1
1