Abstract
Free full text

Syphilitic Gumma: A Rare Form of Cutaneous Tertiary Syphilis
Dear Editor:
Syphilis is the Great Masquerader and a syphilitic gumma is now extremely rare type of tertiary syphilis, which is easy to be misdiagnosed and requires high suspicion index.
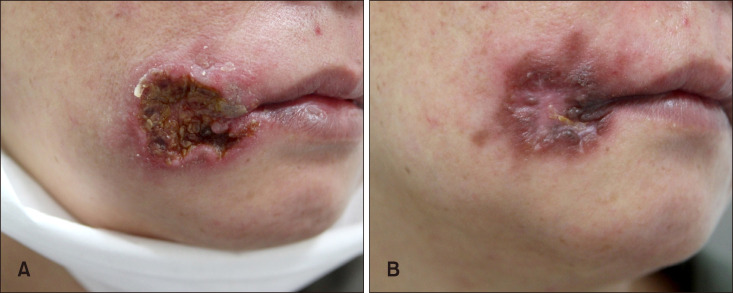
A 48-year-old woman presented with a painless ulcerated plaque on her face for 2 months. At another hospital, she had been treated with antibiotic and antiviral therapies with repetitive dressings, which was not successful. She was previously healthy and denied trauma and skin cancer history. Physical examination showed a 4×4 cm crater-shaped plaque with crusts and oozing (Fig. 1A). We received the patient's consent form about publishing all photographic materials. Provisional diagnosis included pyoderma gangrenosum and squamous cell carcinoma. Skin biopsy demonstrated extensive necrosis and large areas of granulomatous inflammation within the dermis (Fig. 2A), including numerous multinucleated giant cells (Fig. 2B) and marked lymphoplasmacytic infiltrates (Fig. 2C). A rapid plasma regain test was reactive (1:16), and fluorescent treponemal antibody-absorption (FTA-ABS) tests for immunoglobulin M (IgM) and immunoglobulin G were both positive. A human immunodeficiency virus (HIV) test was negative. Only then did the patient mention that she was inadequately treated for syphilis 20 years ago. Taken together, she was finally diagnosed with a syphilitic gumma. Further work up including cerebrospinal fluid analysis did not reveal any evidence of internal organ involvement. The lesion was significantly improved after three intramuscular injections of 2.4 million units of penicillin G (Fig. 1B). Since then she has become lost to follow-up.

Almost one-third of patients with primary or secondary syphilis who were untreated can develop the late manifestations such as cutaneous syphilis, neurosyphilis, or cardiovascular syphilis1. Cutaneous tertiary syphilis accounts for about 16% of them1. The time to progress to tertiary syphilis varies from several months to 35 years after infection2,3. When dealing with patients associated with HIV, it should be kept in mind that HIV may modify the natural course and therapeutic response of syphilis, making the patients vulnerable to an accelerated progression2. Cutaneous tertiary syphilis can be divided into two forms. A noduloulcerative type, the more common variant, occurs as superficial, flat nodules or plaques which progressively grow to build a serpiginous configuration resembling granuloma annulare. The second, a gumma is appears as a non-tender nodular lesion with central punched-out necrosis, exhibiting the deeper and more destructive features1. Histologically, both contain granulomas with large aggregates of lymphocytes, plasma cells, and multinucleated giant cells. However, caseation necrosis is rarely observed in noduloulcerative lesions but extensively found in gummas3. Silver stains or immunohistochemical stains for Treponema pallidum are not sensitive due to the scarcity of the organism3.
As cutaneous tertiary syphilis clinically simulates many other skin diseases, its diagnosis should depend on a comprehensive interpretation of the patient's medical history, pathologic findings, and serology results. An excellent response to intramuscular benzathine penicillin G (3 weekly) can give an additional guarantee of the diagnosis4. When it manifests as an oral lesion, it is sometimes difficult to determine the stages. Especially, the primary oral syphilis required differential diagnosis. However, it usually occurs as a solitary chancre involving the lips and tongue which develops within 1 to 3 weeks after direct contact with a syphilitic patient5. Because FTA-ABS IgM can be positive regardless of the stages, FTA-ABS test is not useful in distinguishing the stages. In the present case, the history of having syphilis 20 years ago and having no recent suspicious contact helped us diagnose the patient as cutaneous tertiary syphilis.
Although the prevalence of syphilis has continued to decline, the late manifestation from patients who had syphilis in the past can constantly emerge. Thus, awareness of this unusual clinical presentation is necessary to appropriately diagnose and treat patients with cutaneous tertiary syphilis.
References
Articles from Annals of Dermatology are provided here courtesy of Korean Dermatological Association and Korean Society for Investigative Dermatology
Full text links
Read article at publisher's site: https://doi.org/10.5021/ad.2018.30.6.749
Read article for free, from open access legal sources, via Unpaywall:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7992438
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/134005195
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.5021/ad.2018.30.6.749
Article citations
Syphilitic gumma presenting as squamous cell carcinoma of Vulva: A case report.
Gynecol Oncol Rep, 55:101478, 08 Aug 2024
Cited by: 0 articles | PMID: 39252759 | PMCID: PMC11381446
Round Bodies Detected by Treponema pallidum Immunohistochemical Stain in Two Cases of Cutaneous Syphilitic Gummata.
Am J Dermatopathol, 46(1):31-35, 01 Jan 2024
Cited by: 1 article | PMID: 37982491 | PMCID: PMC11465137
The Continued Rise of Syphilis: A Case Report to Aid in Identification of the Great Imitator.
J Educ Teach Emerg Med, 8(2):V11-V15, 30 Apr 2023
Cited by: 0 articles | PMID: 37465660 | PMCID: PMC10332677
Challenges in the Diagnosis of Tertiary Syphilis: Case Report with Literature Review.
Int J Environ Res Public Health, 19(24):16992, 17 Dec 2022
Cited by: 1 article | PMID: 36554872 | PMCID: PMC9778711
Review Free full text in Europe PMC
Large syphilitic gumma on the face mimicking dermatitis artefacta.
Postepy Dermatol Alergol, 39(5):996-997, 01 Oct 2022
Cited by: 0 articles | PMID: 36457678 | PMCID: PMC9704452
Go to all (7) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Cerebral Syphilitic Gumma in Immunocompetent Man, Japan.
Emerg Infect Dis, 24(2):395-396, 01 Feb 2018
Cited by: 3 articles | PMID: 29350164 | PMCID: PMC5782894
Squamous cell carcinoma on a syphilitic gumma: A unique presentation.
Indian J Sex Transm Dis AIDS, 36(1):89-91, 01 Jan 2015
Cited by: 3 articles | PMID: 26392665 | PMCID: PMC4555910
Spinal Intramedullary Syphilitic Gumma: An Unusual Presentation of Neurosyphilis.
World Neurosurg, 95:622.e17-622.e23, 21 Jul 2016
Cited by: 7 articles | PMID: 27452967
Spinal Cord Syphilitic Gumma Presenting with Brown-Séquard Syndrome: A Case Report and Literature Review.
Ann Clin Lab Sci, 49(2):265-270, 01 Mar 2019
Cited by: 5 articles | PMID: 31028074
Review





