Abstract
Background
In several European countries safer injecting rooms have reduced the public disorder and health-related problems of injection drug use. We explored factors associated with needle-sharing practices that could potentially be alleviated by the availability of safer injecting rooms in Canada.Methods
The Vancouver Injection Drug User Study is a prospective cohort study of injection drug users (IDUs) that began in 1996. The analyses reported here were restricted to the 776 participants who reported actively injecting drugs in the 6 months before the most recent follow-up visit, during the period January 1999 to October 2000. Needle sharing was defined as either borrowing or lending a used needle in the 6-month period before the interview.Results
Overall, 214 (27.6%) of the participants reported sharing needles during the 6 months before follow-up; 106 (13.7%) injected drugs in public, and 581 (74.9%) reported injecting alone at least once. Variables independently associated with needle sharing in a multivariate analysis included difficulty getting sterile needles (adjusted odds ratio [OR] 2.7, 95% confidence interval [CI] 1.8-4.1), requiring help to inject drugs (adjusted OR 2.0, 95% CI 1.4-2.8), needle reuse (adjusted OR 1.8, 95% CI 1.3-2.6), frequent cocaine injection (adjusted OR 1.6, 95% CI 1.1-2.3) and frequent heroin injection (adjusted OR 1.5, 95% CI 1.04-2.1). Conversely, HIV-positive participants were less likely to share needles (adjusted OR 0.5, 95% CI 0.4-0.8), although 20.2% of the HIV-positive IDUs still reported sharing needles.Interpretation
Despite the availability of a large needle-exchange program and targeted law enforcement efforts in Vancouver, needle sharing remains an alarmingly common practice in our cohort. We identified a number of risk behaviours--difficulty getting sterile needles, needle sharing and reuse, injection of drugs in public and injecting alone (one of the main contributing causes of overdose)--that may be alleviated by the establishment of supervised safer injecting rooms.Free full text

Unsafe injection practices in a cohort of injection drug users in Vancouver: Could safer injecting rooms help?
Abstract
Background
In several European countries safer injecting rooms have reduced the public disorder and health-related problems of injection drug use. We explored factors associated with needle-sharing practices that could potentially be alleviated by the availability of safer injecting rooms in Canada.
Methods
The Vancouver Injection Drug User Study is a prospective cohort study of injection drug users (IDUs) that began in 1996. The analyses reported here were restricted to the 776 participants who reported actively injecting drugs in the 6 months before the most recent follow-up visit, during the period January 1999 to October 2000. Needle sharing was defined as either borrowing or lending a used needle in the 6-month period before the interview.
Results
Overall, 214 (27.6%) of the participants reported sharing needles during the 6 months before follow-up; 106 (13.7%) injected drugs in public, and 581 (74.9%) reported injecting alone at least once. Variables independently associated with needle sharing in a multivariate analysis included difficulty getting sterile needles (adjusted odds ratio [OR] 2.7, 95% confidence interval [CI] 1.8–4.1), requiring help to inject drugs (adjusted OR 2.0, 95% CI 1.4–2.8), needle reuse (adjusted OR 1.8, 95% CI 1.3–2.6), frequent cocaine injection (adjusted OR 1.6, 95% CI 1.1–2.3) and frequent heroin injection (adjusted OR 1.5, 95% CI 1.04–2.1). Conversely, HIV-positive participants were less likely to share needles (adjusted OR 0.5, 95% CI 0.4–0.8), although 20.2% of the HIV-positive IDUs still reported sharing needles.
Interpretation
Despite the availability of a large needle-exchange program and targeted law enforcement efforts in Vancouver, needle sharing remains an alarmingly common practice in our cohort. We identified a number of risk behaviours — difficulty getting sterile needles, needle sharing and reuse, injection of drugs in public and injecting alone (one of the main contributing causes of overdose) — that may be alleviated by the establishment of supervised safer injecting rooms.
The incidence of fatal overdoses and the emergence of the HIV epidemic among injection drug users (IDUs) have led to wider recognition that illicit drug use is a public health problem. Public health initiatives aimed at preventing overdoses and disease transmission among IDUs are referred to as harm reduction.1 In addition to prevention, harm reduction aims to protect drug users by enabling them to inject safely until they can be helped off drugs.2
A cornerstone of harm reduction is making sterile needles available through needle-exchange programs and other means.3 Although needle exchange is accepted as a public health intervention in many cities in Canada, the apparent tolerance of drug use associated with it has made needle exchange controversial in some smaller Canadian settings and in many countries around the world.4 Nevertheless, overwhelming evidence indicates that needle-exchange programs can substantially reduce HIV risk behaviour and the transmission of bloodborne infections, including HIV.5,6,7,8 However, such programs have not been sufficient to prevent HIV epidemics in all settings. This is true of Vancouver's Downtown Eastside, where an HIV epidemic, characterized by a peak annual incidence rate of 18%, was documented in 1997 despite the presence of a needle-exchange program.9 The inability of the program to prevent this epidemic was later attributed to specific local factors, including a high prevalence of cocaine injection.10
As in many other settings, a primary response to the HIV epidemic was to increase targeted law enforcement efforts in the Downtown Eastside so that greater numbers of police officers could patrol the neighbourhood's alleys and other areas where drug use is concentrated.11 Currently in Canada the vast majority of resources aimed at preventing the harms of drugs are now allocated to policing. In British Columbia, 82% of the total direct costs associated with illicit drug use are accounted for by law enforcement.12 Despite the resources provided to law enforcement, the incidence of hepatitis C and HIV infection in Vancouver's Downtown Eastside indicate that a substantial number of IDUs continue to share needles.13 Furthermore, the region continues to experience an epidemic of overdoses, 312 occurring on average each year since 1996.14
A harm reduction intervention that has been highly effective elsewhere is safer injecting rooms, which are legally sanctioned and supervised facilities where IDUs can inject pre-obtained illicit drugs. Within these facilities, IDUs are provided access to health care and other services as well as sterile injecting equipment.15,16 Although safer injecting rooms have not been established in North America, over 45 of them now operate in about a dozen European cites, and a facility has recently opened in Australia.15 The reported benefits of these facilities include improved health and social functioning of clients, reductions in public disorder (e.g., drug injection, intoxication and discarding of needles in public), reductions in overdoses and reductions in risk behaviours for disease transmission.15,16,17,18,19
Several cities in Canada, including Vancouver,20 are considering scientific evaluations of safer injecting rooms. These proposals have met resistance from community groups expressing fear that the drug epidemic in Canada is such that the European experience is unlikely to be replicated here.21,22 Therefore, we conducted analyses to examine factors associated with needle sharing among Vancouver IDUs and to evaluate whether any of these factors could potentially be alleviated by the establishment of safer injecting rooms.
Methods
Beginning in May 1996 people who had injected illicit drugs in the previous month were recruited into the Vancouver Injection Drug User Study. In brief, over 1400 subjects were recruited through self-referral and street outreach efforts. Eligible subjects were those who had injected illicit drugs at least once in the previous month, resided in the Greater Vancouver area and provided written informed consent. At baseline and semi-annually, subjects provided blood samples and completed an interviewer-administered questionnaire. The questionnaire was designed to elicit demographic data and information about drug use, HIV risk behaviours and drug treatment.
For our analyses, we included baseline data and data from the most recent follow-up questionnaire available (administered during January 1999 to October 2000). Demographic characteristics such as age, sex and ethnic background were derived from the baseline questionnaire. To evaluate current drug injection practices, information such as drug use and health-related characteristics such as HIV status were obtained from the most recent follow-up questionnaire.
We chose needle sharing as the dependent variable because this behaviour has been shown to have the highest risk of HIV transmission among IDUs. Needle sharing was defined as either the lending or borrowing of a used needle in the 6 months before the follow-up visit. We did not restrict our analyses to needle sharing with either casual or intimate partners, because we have recently shown that both risk behaviours are associated with HIV seroconversion among IDUs in Vancouver.23 People who had not injected drugs in the 6 months before the most recent follow-up visit were excluded from our analyses, because we sought to evaluate predictors of needle sharing among people who were actively injecting drugs. We also examined, and report on briefly in this article, the proportion of IDUs who reported sharing needles as defined above in the cohort during the prior 5 follow-up visits.
Univariate and multivariate analyses were performed to determine factors associated with current needle sharing practices. Sociodemographic and behavioural characteristics considered in the analyses included age, sex, ethnic background, education level, HIV status, and self-report at baseline of ever having had a diagnosis of mental illness. We also considered information on the receipt of methadone treatment, being refused drug treatment, being refused sterile needles at pharmacies and requiring help injecting.
Characteristics of drug use considered in our analyses included difficulty getting sterile needles, frequency of cocaine and heroin injection, average use of needles (once v. more than once), nonfatal overdoses, injection in public, safety of needle disposal and frequency of injecting alone. As we have done previously,9,10 frequent cocaine or heroin use was defined as injection of the drug once or more daily. Safe needle disposal was defined as the placement of needles in a “safe place” or a sharps container or the return of needles to the needle-exchange program. To evaluate the effect of police activities on drug use, we considered the number of subjects who reported that police activities affected their source of drugs.
Statistical analyses were used to compare IDUs who shared needles and those who did not share needles in the 6 months before the most recent follow-up visit. Categorical explanatory variables were analyzed using Pearson's χ2 test, and continuous variables were analyzed using the Wilcoxon rank-sum test. All variables that were statistically significant at the 0.05 cutoff point were considered in a logistic regression analysis. All reported p values are two-sided.
Results
Since the study's inception, 124 participants have died (28 of HIV/AIDS, 41 of an overdose and 55 of other causes). A total of 962 participants responded to at least 1 questionnaire during the period January 1999 to October 2000 and were therefore eligible for our study. Compared with the 351 participants who did not come in for the most recent follow-up, those included in our study were more likely to be female (p = 0.001), Aboriginal (p = 0.001), HIV-positive at last follow-up (p = 0.001), older (p < 0.001) and have a high school education (p = 0.006). No significant differences were found between the groups with regard to difficulty acquiring clean needles (p = 0.30), frequency of cocaine injection (p = 0.72) or heroin injection (p = 0.93), or need for help injecting (p = 0.84). Of the 962 participants eligible for our study, 776 (80.7%) reported injecting drugs in the 6 months before the most recent follow-up visit and were therefore included in our analyses; 562 (72.4%) reported not sharing needles and 214 (27.6%) reported sharing needles in that 6-month period. The proportions of active IDUs who reported needle sharing at the 4 follow-up visits before the study period were 31.2%, 22.7%, 23.5% and 25.5% respectively. Of the 247 HIV-positive IDUs, 20.2% reported sharing needles in the 6 months before the most recent follow-up visit. Of the 776 IDUs in our study, 106 (13.7%) injected drugs in public, and 581 (74.9%) injected alone at least once.
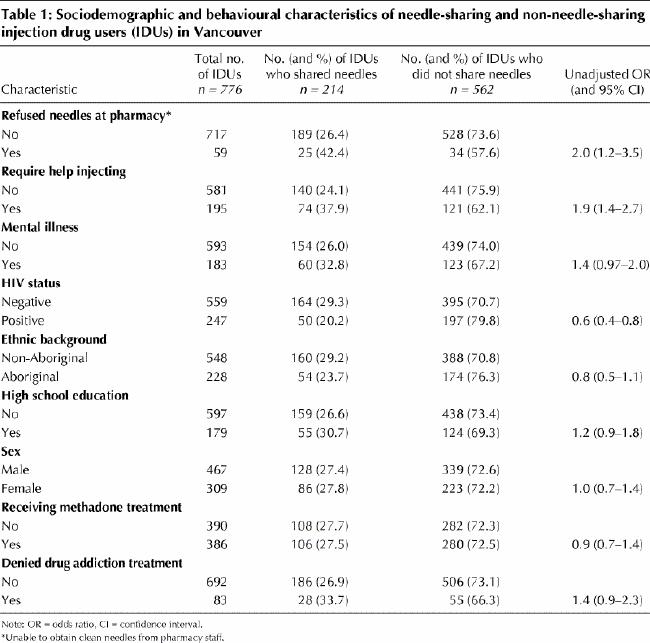
The results of the univariate analysis of sociodemographic and health-related characteristics are shown in Table 1. Being refused sterile needles at pharmacies (odds ratio [OR] 2.0) and requiring help to inject drugs (OR 1.9) were positively associated with sharing needles. Although not achieving statistical significance, having a diagnosis of mental illness was associated with sharing needles (OR 1.4, p = 0.07). Alternatively, being older (OR 0.97 per year of age [95% CI 0.95–0.99]; data not shown), and being HIV positive (OR 0.6) were inversely associated with needle sharing. We found no evidence that ethnic background, education level, sex, receipt of methadone treatment or being refused drug addiction treatment were associated with needle sharing.
Table 1
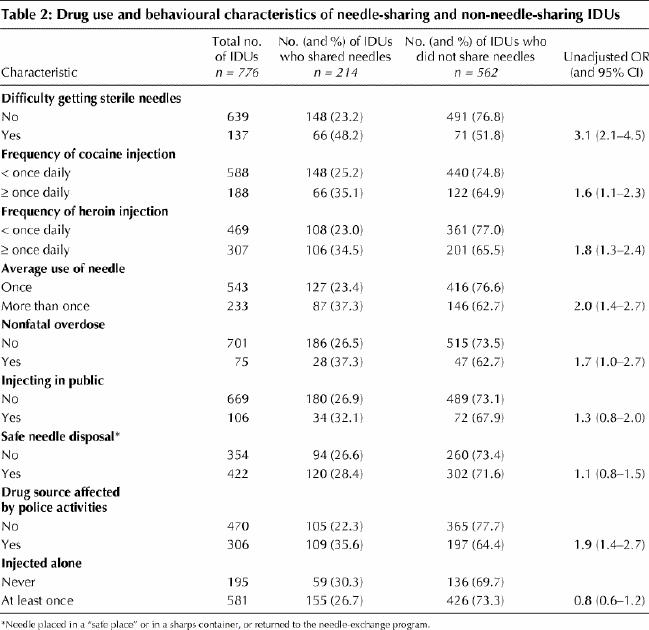
The results of the univariate analysis of drug use and behavioural characteristics are shown in Table 2. Factors positively associated with needle sharing were difficulty getting sterile needles (OR 3.1), frequent cocaine injection (OR 1.6), frequent heroin injection (OR 1.8), use of needles more than once on average (OR 2.0), nonfatal overdose (OR 1.7) and reporting that police activities had affected the source of drugs (OR 1.9). We found no evidence that injection in public, unsafe needle disposal or injecting alone were associated with needle sharing.
Table 2
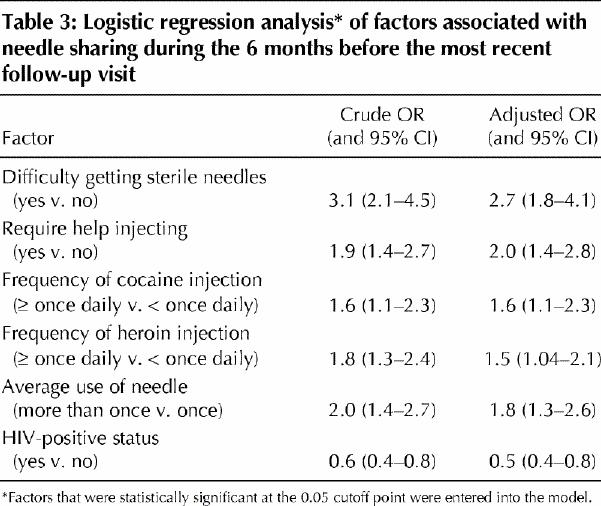
The variables that were found to be independently associated with needle sharing in the stepwise logistic regression analyses are listed in Table 3. Difficulty getting sterile needles (adjusted OR 2.7), requiring help to inject drugs (adjusted OR 2.0), frequent cocaine injection (adjusted OR 1.6), frequent heroin injection (adjusted OR 1.5) and use of needles more than once on average (adjusted OR 1.8) were all positively associated with needle sharing. HIV-positive status was inversely associated with needle sharing (adjusted OR 0.5).
Table 3
Interpretation
Despite targeted police efforts and a large needle-exchange program in Vancouver's Downtown Eastside, 27.6% of the IDUs included in our study reported sharing needles, and 9.7% had had a nonfatal overdose in the 6 months before the most recent follow-up visit. Having difficulty getting sterile needles, needing help injecting, reusing needles, and frequent cocaine and heroin injection were all associated with needle sharing.
Several of our findings suggest that barriers to sterile needle use persist despite the presence of a large needle-exchange program.9 Although expanding the program would likely help to reduce needle sharing further, several risk factors remained independently associated with needle sharing after adjustment for difficulty getting needles. Furthermore, 19.1% of the participants included in our study shared needles even though they did not report having difficulty getting sterile needles. All of these factors suggest that expansion of the needle-exchange program alone will not be sufficient to eliminate this risk.
Several conditions, such as lack of experience or physical disability, may place IDUs in need of help with injections. The high prevalence of assisted injection has been documented in other settings,24 although the strong association with HIV risk behaviour has not been previously established to our knowledge. Again, adequate availability of sterile needles will probably not be sufficient to mitigate this risk behaviour.
We also found that subjects who were HIV-positive were half as likely as HIV-negative IDUs to share needles. This suggests a benefit of HIV testing and counselling in this community.25 However, despite substantial outreach services offering testing and counselling to IDUs in Vancouver, only 15.0% of the participants in our study had ever had an HIV test before recruitment into the study (unpublished data).
Another major problem associated with injection drug use is death from overdose. In Canada, British Columbia has the highest number of such deaths per capita, with about 4.7 per 100 000 population annually, and in several recent years illicit drugs have been the leading cause of death among adults 30 to 49 years of age.12,14 Although needle-exchange programs have been associated with reductions in overdoses,26 overdoses continue to occur all too frequently among IDUs.
Several of the variables we examined highlight the public disorder problems associated with injection drug use. For instance, in the 6 months before the most recent follow-up visit 13.7% of the participants in our study reported injecting drugs in public and 45.6% reported that they did not always practise safe needle disposal.
We found a positive association between police activities and needle sharing. Although further study of this association is required, the potentially negative consequences of policing efforts on HIV risk behaviour, such as creating fear of possessing needles, have been reported elsewhere.27,28
Our study has several limitations. Compared with the IDUs included in our study, those who did not come in for the most recent follow-up had a number of characteristics (e.g., younger and more likely to be HIV negative) that may make them more likely to be involved in needle sharing. Furthermore, it has been shown previously that IDUs may substantially underreport HIV risk behaviour and that HIV testing and counselling that accompany cohort studies such as ours may reduce risk behaviour over time.29,30 Therefore, we may have underestimated the extent of needle sharing among IDUs.
In summary, our data demonstrate a continued health crisis among IDUs. Furthermore, the proportion of IDUs who reported needle sharing did not decrease over the past 5 follow-up visits, despite the presence of a large needle-exchange program and targeted law enforcement efforts.
Meanwhile, in several European cities, the risk factors we identified have proven amenable to improvement through the establishment of safer injecting rooms as part of comprehensive harm reduction strategies. Increases in HIV testing and counselling, health and social functioning, and drug addiction treatment have occurred among clients of safer injecting rooms in these cities.15,16,31 Conversely, the incidence of HIV risk behaviour including needle sharing, hospital admissions, improper needle disposal, drug injection in public places and death from overdose have all decreased.15,16,31,32 In fact, there has not been a fatal overdose in a safer injecting room since their establishment in the mid-1980's.17 In the present study we did not evaluate safer injecting rooms per se. We have merely identified risk factors among IDUs that have proven amenable to improvement through the availability of such facilities in other settings.15,16,31,32 Given the high prevalence of HIV risk behaviours, overdoses and other health-related concerns that persist in Vancouver, it is crucial to evaluate whether the European experience with safer injecting rooms can be replicated in Canada.
Footnotes
This article has been peer reviewed.
Acknowledgments: We thank Bonnie Devlin, Caitlin Johnston, Robin Brooks, Suzy Coulter, Steve Kain, Guillermo Fernandez, John Charette, Will Small and Nancy Laliberté for their research and administrative assistance. We also thank all of the participants in the Vancouver Injection Drug User Study.
The study was supported by the US National Institutes of Health (grant no. RO1 DA11591). Mr. Wood is supported by the Canadian Institutes for Health Research and the British Columbia Health Research Foundation. Dr. Schechter holds a tier I Canada Research Chair in HIV/AIDS and Urban Population Health.
Competing interests: None declared.
Correspondence to: Dr. Martin T. Schechter, Professor and Head, Department of Health Care and Epidemiology, University of British Columbia, 5804 Fairview Ave., Vancouver BC V6T 1Z3; fax 604 822-4994; [email protected]
References
Articles from CMAJ : Canadian Medical Association Journal are provided here courtesy of Canadian Medical Association
Full text links
Free to read at www.cmaj.ca
http://www.cmaj.ca/cgi/content/abstract/165/4/405
Free to read at www.cmaj.ca
http://www.cmaj.ca/cgi/content/full/165/4/405
Free to read at www.cmaj.ca
http://www.cmaj.ca/cgi/reprint/165/4/405.pdf
Citations & impact
Impact metrics
Article citations
Perceptions of provider awareness of traditional and cultural treatments among Indigenous people who use unregulated drugs in Vancouver, Canada.
BMC Health Serv Res, 24(1):266, 02 Mar 2024
Cited by: 0 articles | PMID: 38429744 | PMCID: PMC10908172
Uptake of SARS-CoV-2 vaccination among structurally-marginalized people who use drugs in Vancouver, Canada.
Sci Rep, 13(1):17930, 20 Oct 2023
Cited by: 1 article | PMID: 37863999 | PMCID: PMC10589278
Experiencing homelessness and progression through the HIV cascade of care among people who use drugs.
AIDS, 37(9):1431-1440, 05 Apr 2023
Cited by: 5 articles | PMID: 37070552 | PMCID: PMC10330029
Prevalence and correlates of using opioids alone among individuals in a residential treatment program in Michigan: implications for overdose mortality prevention.
Harm Reduct J, 19(1):135, 03 Dec 2022
Cited by: 2 articles | PMID: 36463189 | PMCID: PMC9719663
Injecting drugs alone during an overdose crisis in Vancouver, Canada.
Harm Reduct J, 19(1):125, 17 Nov 2022
Cited by: 5 articles | PMID: 36397146 | PMCID: PMC9670082
Go to all (132) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Requiring help injecting as a risk factor for HIV infection in the Vancouver epidemic: implications for HIV prevention.
Can J Public Health, 94(5):355-359, 01 Sep 2003
Cited by: 44 articles | PMID: 14577743 | PMCID: PMC6979944
Recent incarceration independently associated with syringe sharing by injection drug users.
Public Health Rep, 120(2):150-156, 01 Mar 2005
Cited by: 54 articles | PMID: 15842116 | PMCID: PMC1497693
Changes in injecting practices associated with the use of a medically supervised safer injection facility.
J Public Health (Oxf), 29(1):35-39, 17 Jan 2007
Cited by: 81 articles | PMID: 17229788
Needle exchange and the HIV epidemic in Vancouver: lessons learned from 15 years of research.
Int J Drug Policy, 23(4):261-270, 11 May 2012
Cited by: 43 articles | PMID: 22579215 | PMCID: PMC3392518
Review Free full text in Europe PMC
Funding
Funders who supported this work.
NIDA NIH HHS (2)
Grant ID: R01 DA011591
Grant ID: R01 DA11591




