Abstract
Free full text

Likelihood of COVID-19 vaccination by subgroups across the US: post-election trends and disparities
ABSTRACT
The coronavirus disease 2019 (COVID-19) pandemic has disproportionately impacted older individuals, those with lower educational attainment, and Black and Hispanic populations, yet vaccine hesitancy remains prevalent. Because widespread uptake of COVID-19 vaccines is critical to end the pandemic, addressing vaccine hesitancy is an important public health priority. Between April 1, 2020 and March 16, 2021, we have repeatedly surveyed a nationally representative online panel of adults and have tracked their stated likelihood of getting COVID-19 vaccinations. We present new evidence that in recent months disparities in self-reported likelihood of COVID-19 vaccination have narrowed by race/ethnicity, with an increasing proportion of Black individuals and Hispanic individuals indicating that they are likely to get a vaccine. At the same time, younger adults have progressively become less likely than older adults to state they will get a COVID-19 vaccine. Most vaccine-hesitant individuals are concerned about both vaccine efficacy and safety and do not trust the vaccine development or vaccine approval process. We conclude that outreach efforts to minority populations may be achieving their objectives in raising confidence in COVID-19 vaccines, but special outreach efforts are needed to address both vaccine hesitancy among younger adults and mistrust in the vaccine development and approval process.
The coronavirus disease 2019 (COVID-19) pandemic has caused enormous morbidity and mortality across the United States (US), with older adults and racial and ethnic minorities disproportionately affected.1,2 The first two vaccines were approved by the Food and Drug Administration (FDA) and recommended by the Advisory Committee on Immunization Practices (ACIP) and the Centers for Disease Control (CDC) in December 2020;3 a third was approved in February 2021,4 and more approvals will likely come in the near future. Resolution of the pandemic depends on public acceptance and uptake of COVID-19 vaccines. In addition, with increasing SARS-CoV-2 variants, booster doses or subsequent vaccinations will likely be needed.5–7
Since March 2020, several US-based studies have investigated the public’s interest in receiving COVID-19 vaccines, including cross-sectional studies8–18 and longitudinal studies of online panels.19–21 A concerning finding has been the large disparities in COVID-19 vaccine interest, with younger individuals, racial/ethnic minorities, and those who affiliate with the Republican party reporting less willingness to be vaccinated. Since the US election in November 2020 and the first vaccine approvals in December 2020, there has been both a rapid ramp-up of COVID-19 vaccination across the US and an enormous effort on the part of the CDC, states, local governments, and community organizations to raise confidence in COVID-19 vaccines through public relations announcements, newscasts, and outreach efforts to hard-to-reach populations. It is not yet known whether these efforts have reduced disparities in interest in COVID-19 vaccines.
Since April 2020, we have been surveying a nationally representative sample of US adults about their intent to receive a COVID-19 vaccine.19,22 The goal of the current analysis is to evaluate trends over time in the intent to receive a COVID-19 vaccine among the general US population and among the subgroups that might have greater hesitancy based upon prior surveys, particularly younger adults, racial/ethnic minorities, and individuals with a Republican party affiliation. In particular, this analysis will focus on trends and disparities that have emerged since the US election in November 2020, which has been widely reported on as a turning point in population-level vaccination attitudes. Our aim is to assess whether disparities in vaccine likelihood have widened or narrowed since the US election and whether post-election trends differ across our subgroups of interest.
The Understanding America Study (UAS) and analysis
Data for this analysis come from a nationally representative subsample of the Understanding America Study (UAS),19,22 a probability-based internet panel of approximately 9,000 adults aged 18 years or older that is representative of the non-institutionalized US population. Panel members are recruited using address-based sampling, and tablets and broadband internet are provided if needed. Surveys are in English or Spanish. From April 1, 2020 to February 16, 2021, the UAS invited a subsample of the online panel to participate in biweekly surveys about the COVID-19 pandemic.19 Respondents were randomly assigned to an invitation day, and invitations were distributed over the course of 14 days. Since February 17, 2021, this invitation period has been doubled – invitations are now distributed over the course of 28 days. Once respondents are invited into each survey wave, they are given 14 days to respond. Following best survey practices,23 incentives are provided to encourage respondents to complete each survey at a rate of 20 USD per 30 minutes of survey time (and proportionately less for shorter surveys). To encourage respondents to complete the interview on their assigned day, they receive an additional 1 USD incentive if they complete the survey on the day they receive their invitation. For survey waves fielded prior to February 17, 2021, over 90% of responses were received within the first 2 weeks of fielding; for surveys fielded since February 17, 2021, over 90% of responses are received within the first 4 weeks of fielding. Thus, a two-week sample of surveys collected prior to February 17, 2021 is comparable in size to a four-week sample of surveys collected since February 17, 2021.
We use a graphical format to describe trends in vaccination likelihood since April 2020, presenting 2-week averages that span April 1, 2020, to March 16, 2021. We present our statistical analyses in a table format. To evaluate post-election trends, our statistical analyses focus on two time points: the two-week period of October 28th-November 10th, 2020, which occurred around the US Presidential election (6,396 respondents, response rate 78%), and the four-week period of February 17-March 16, 2021, which is comparable in sample size to prior two-week periods and was the most recent survey period available (5,891 respondents, response rate 71%).
In each survey wave, respondents were asked the question: “How likely are you to get vaccinated for coronavirus once a vaccine is available to the public? (very likely, somewhat likely, somewhat unlikely, very unlikely, or unsure). We classified “very likely” or “somewhat likely” responses as likely to vaccinate; we included those who already had a COVID-19 vaccine as likely to vaccinate. We interpreted “very unlikely,” “somewhat unlikely,” and “unsure” responses as indicative of COVID-19 vaccine hesitancy.
We examined how trends in vaccination likelihood varied according to demographics (age group, sex, race and ethnicity, and educational attainment) and political affiliation (Democratic party, Republican party, or other).
To assess reasons for hesitancy about COVID-19 vaccinations, we analyzed five questions on the most recent survey (February 17-March 16, 2021). First, we asked about level of agreement with statements regarding benefits or side effects of the vaccines. To explore deeper concerns about vaccine effectiveness or harms, we asked respondents to estimate the likelihood that a vaccinated individual might still catch coronavirus or the likelihood that the vaccine will cause serious side effects or long-term harm. Finally, we asked two questions about level of trust in the vaccine development process in general and about the governmental approval process for COVID-19 vaccines.
We graphed trends in the likelihood of getting a COVID-19 vaccination for the entire population and for racial/ethnic subgroups (Figure 1). We calculated percentages and margins of error (based on a 95% confidence level) with adjustment for survey sampling weights. We performed a cross-sectional analysis (Table 1) of reported intentions in the most recent February 17-March 16, 2021 survey using a multivariable Poisson regression model with robust standard errors, showing differences between groups as risk ratios with 95% confidence intervals (CIs). To assess trends since the US election, we also analyzed the change in intentions between the October 28-November 10, 2020 survey and the most recent February 17-March 16, 2021 survey. We used linear regression models of changes in intentions with cluster-robust standard errors, with clustering at the respondent level and summarized changes over time using least squares means and 95% CIs. We used significance levels of 0.05 and Holm’s correction to account for multiple hypothesis testing. Finally, we used descriptive statistics to summarize vaccine perceptions among individuals who were hesitant about COVID-19 vaccines (Table 2).
Table 1.
Demographic and individual predictors of likelihood of getting a coronavirus vaccine
| February 17 – March 16, 2021 | Change from October 28-November 10, 2020 to February 17 – March 16, 2021 | ||||||
|---|---|---|---|---|---|---|---|
| Percent Likely to Get Vaccine | Adjusted Risk Ratio (95% CI) | P Value | Unadjusted Change in Percent (95% CI) | P Value | Adjusted Change in Percent (95% CI) | P Value | |
| Overall | 64.2% | 10.4% (8.4%, 12.3%) | <.001 | 10.4% (8.4%, 12.3%) | <.001 | ||
| Sex | |||||||
 Female Female | 60.2% | - REF - | 11.8% (9.0%, 14.5%) | <.001 | 12.7% (8.8%, 16.6%) | <.001 | |
 Male Male | 68.5% | 1.10 (1.04, 1.16) | <.001 | 9.0% (6.3%, 11.7%) | <.001 | 9.8% (6.0%, 13.6%) | <.001 |
| Age (y) | |||||||
 18–49 18–49 | 55.9% | - REF - | 5.5% (2.7%, 8.3%) | <.001 | 2.9% (−0.8%, 6.6%) | .119 | |
 50–64 50–64 | 68.2% | 1.29 (1.20, 1.38) | <.001 | 15.2% (11.6%, 18.8%) | <.001 | 12.6% (8.5%, 16.6%) | <.001 |
 65–74 65–74 | 78.5% | 1.44 (1.34, 1.54) | <.001 | 13.8% (9.2%, 18.4%) | <.001 | 12.2% (6.9%, 17.5%) | <.001 |
 75+ 75+ | 86.4% | 1.59 (1.46, 1.72) | <.001 | 18.7% (12.4%, 24.9%) | <.001 | 17.4% (10.5%, 24.3%) | <.001 |
| Education | |||||||
 High School or Less High School or Less | 54.3% | - REF - | 11.4% (7.6%, 15.1%) | <.001 | 11.5% (7.0%, 16.0%) | <.001 | |
 Some College Some College | 59.1% | 1.11 (1.03, 1.21) | .008 | 11.1% (7.4%, 14.8%) | <.001 | 11.4% (6.9%, 15.9%) | <.001 |
 Bachelor’s or More Bachelor’s or More | 78.9% | 1.38 (1.29, 1.48) | <.001 | 8.8% (6.4%, 11.2%) | <.001 | 10.9% (7.0%, 14.7%) | <.001 |
| Race/Ethnicity | |||||||
 Non-Hispanic White Non-Hispanic White | 64.9% | - REF - | 9.2% (7.0%, 11.3%) | <.001 | 12.1% (9.8%, 14.5%) | <.001 | |
 Hispanic Hispanic | 61.9% | 0.93 (0.85, 1.03) | .175 | 16.0% (9.4%, 22.6%) | <.001 | 19.4% (12.7%, 26.2%) | <.001 |
 Non-Hispanic Black Non-Hispanic Black | 56.5% | 0.77 (0.69, 0.86) | <.001 | 16.6% (10.3%, 22.8%) | <.001 | 17.1% (10.7%, 23.5%) | <.001 |
 Non-Hispanic Asian Non-Hispanic Asian | 83.8% | 1.16 (1.06, 1.27) | .002 | 6.2% (−0.1%, 12.6%) | .055 | 9.9% (2.917%, 0%) | .006 |
 Other Other | 60.0% | 0.93 (0.79, 1.09) | .371 | −6.6% (−15.9%, 2.8%) | .169 | −2.3% (−11.8%, 7.2%) | .634 |
| Political Influence | |||||||
 Democratic Party Democratic Party | 80.1% | - REF - | 15.7% (12.7%, 18.8%) | <.001 | 15.9% (12.2%, 19.7%) | <.001 | |
 Republican Party Republican Party | 53.4% | 0.64 (0.60, 0.68) | <.001 | 7.8% (4.5%, 11.1%) | <.001 | 9.2% (4.7%, 13.8%) | <.001 |
 Other Other | 54.7% | 0.71 (0.66, 0.77) | <.001 | 5.6% (1.8%, 9.3%) | .003 | 8.6% (3.9%, 13.3%) | <.001 |
Bolded p-values indicate significance at the 0.05 level (Feb. 17 – March 16 adjusted risk ratios), or significance after Holm-Bonferroni correction (change from Oct. 28-Nov. 10 to Feb. 17 – March 16). Adjustments are for all variables in the table.
Individuals who have already received a COVID-19 vaccine were included as “Likely”.
Table 2.
Perceptions among individuals who are hesitant about COVID-19 vaccines
| Perceptions among individuals who are hesitant about the COVID-19 vaccines* | |
|---|---|
| Statements about coronavirus vaccines | Percent who agree with the statement |
Vaccines for coronavirus:
| 62%66%74%47% |
Percent chance that someone who is vaccinated against the coronavirus could still catch it: [Best guess, 0–100% visual linear scale]
| 28%18%34%20% |
Percent chance that a coronavirus vaccine will cause serious side effects or long-term health problems for someone who has been vaccinated: [Best guess, 0–100% visual linear scale]
| 31%18%33%18% |
How much do you trust the process in general (not just for COVID-19) to develop safe vaccines for the public?
| 3%15%38%44% |
How much do you trust the governmental approval process to ensure the COVID-19 vaccine is safe for the public?
| 1%9%34%56% |
*Hesitant individuals are defined as: those who have not received a COVID-19 vaccine and state they are very unlikely, unlikely, or unsure about whether they will receive a vaccine once it is available.
**For these two questions, responses reflect percent who disagree with the statement.
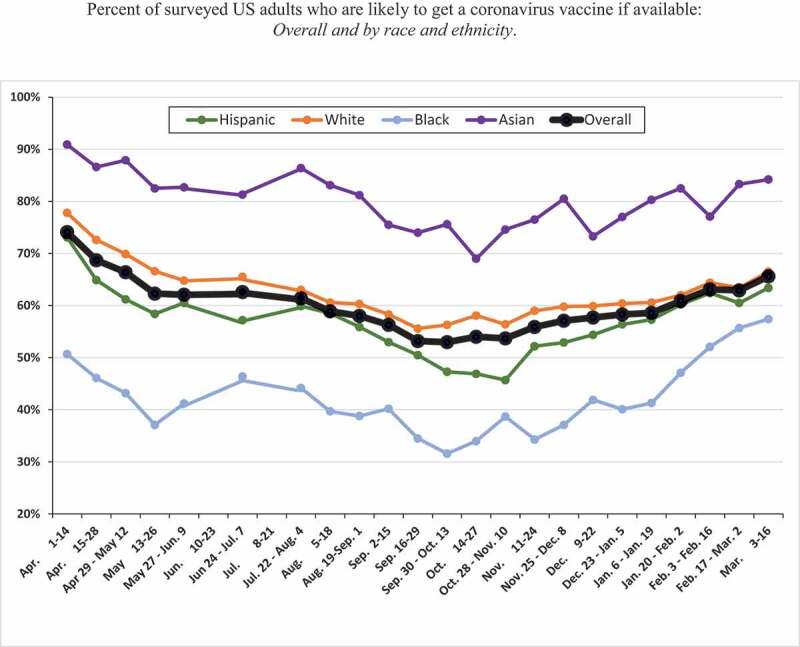
The figure shows likelihood of getting a coronavirus vaccine, or a self-report of having been vaccinated, for each two-week period from April 1, 2020, to March 16, 2021, except for June 10–23 and July 8–21, 2020 (surveys were not done during those two periods). The margin of error for 95% confidence level ranged from: Hispanic (5.1%-7.3%%), White (1.8%-2.9%), Black (5.2%-8.7%), Asian (4.8%-8.0%), Overall (1.7%-2.5%) per survey period
Findings: post-election likelihood of vaccination overall and by subgroups
For all US adults (Figure 1), the likelihood of getting a coronavirus vaccine increased from 54% in October 28-November 10, 2020 to 66% by March 3–16, 2021. As shown in Table 1, disparities still exist in March 2021. Males are more likely than females to state that they are likely to be vaccinated (69% vs. 60%, p < .001). Stated likelihood of vaccination increases by age group, with only 56% of young adults aged 18–49 years stating they are likely to be vaccinated compared to 79% of adults aged 65–74 years and 86% of adults aged 75 years or older. Individuals with some college (59%) or a Bachelor’s degree or higher (79%) are more likely to state they are likely to be vaccinated than those with a high school degree or less education (54%). Non-Hispanic Asian individuals (84%) are more likely than whites (65%) to state they intend to get vaccinated, while Black individuals (57%) are less likely and Hispanic individuals (62%) are similar to whites. Finally, individuals who affiliate with the Democratic party (80%) are far more likely to state they intend to get vaccinated than those who affiliate with the Republican party (53%), or have some other affiliation (55%), p < .0001 for each comparison with Democrats.
Table 1 shows the unadjusted and adjusted change in self-reported likelihood of vaccination between the October 28-November 10, 2020 survey period and the February 17 – March 16, 2021 survey period. The analyses reveal several important findings. First, virtually all subgroups have increased their stated likelihood of vaccination since the US election, with increases ranging from 3 percentage points to 17 percentage points. Second, disparities have widened by age group. While adults aged 50 years or older experienced a 12–17 percentage point increase in their stated likelihood of vaccination, young adults aged 18–49 years experienced only a 3-percentage point increase in their stated likelihood of vaccination. Third, disparities by educational attainment did not widen but persist, with an 11-percentage point increase in vaccination likelihood occurring across all three educational groups. Fourth, disparities by race/ethnicity have narrowed. While all racial/ethnic groups except “other race” have experienced substantial increases in their stated likelihood of vaccination, the increase has been greater among Non-Hispanic Black and Hispanic respondents than among Non-Hispanic White respondents. Finally, disparities by political affiliation have widened. Since the election, individuals affiliated with the Democratic party have experienced a 16-percentage point increase in stated likelihood of vaccination while individuals affiliated with the Republican party have experienced a smaller, 9-percentage point increase in stated likelihood of vaccination.
Table 2 shows perceptions among individuals who are hesitant about COVID-19 vaccines. A very high percentage of vaccine-hesitant individuals reportedly believe that the vaccines have harmful side effects and may even lead to illness or death. A considerable number of vaccine-hesitant individuals did not think that the vaccines are effective or beneficial to society. Most vaccine-hesitant individuals stated that a very high percentage of people who are vaccinated can still catch coronavirus or will have serious side effects or long-term health problems. Finally, a high proportion of vaccine-hesitant individuals did not trust the general vaccine development process to make safe vaccines, and did not trust the governmental approval process to ensure that COVID-19 vaccines are safe for the public.
Conclusions
A high proportion of the US population needs to receive a COVID-19 vaccine in order to end the pandemic, although the exact threshold for achieving herd immunity is unknown.7 Our analyses illustrate both encouraging and concerning findings. One encouraging finding is that for the overall US population, the likelihood of vaccination has risen by 10-percentage points, from a nadir in late October/November 2020 to 63% by March 2021. A second encouraging finding is that all subgroups have increased their stated likelihood of vaccination. A third extremely encouraging finding is that Non-Hispanic Black and Hispanic populations have substantially increased their stated likelihood of vaccination, greater than the increase among Whites, so that the racial/ethnic gap has narrowed since the election.
Our study also highlights several concerning findings. First, the likelihood of COVID-19 vaccination remains low among young adults aged 18–49, individuals with high school or less education, and individuals affiliated with the Republican party. Second, disparities remain in the likelihood of vaccination by gender, age group, education, race/ethnicity, and political affiliation. Finally, a high proportion of vaccine-hesitant individuals are skeptical about both the effectiveness and safety of COVID-19 vaccines and also do not trust the vaccine development process or the governmental approval process.
The marked rise in interest in COVID-19 vaccines among Black and Hispanic populations and the simultaneous narrowing of racial/ethnic disparities in the public’s interest in COVID-19 vaccines is heartening and likely reflects the success of outreach efforts at local, state, and federal levels, as well as the influence of the media. Given the barriers to accessing COVID-19 vaccines among many Black and Hispanic communities,24 it is critical to pair this rising interest in vaccine with improved access to vaccines.25 Communities across the US are focusing heavily on outreach to vulnerable populations and will need to continue and even intensify these efforts, particularly because the initial phases of the vaccination campaign have focused upon older adults who are more likely to get a vaccine and the later phases now include all adult ages. In fact, most US states have opened vaccine eligibility to individuals aged 16 and older; the present study findings underscore that vaccine hesitancy in younger age groups remains high and this needs to be addressed in future outreach efforts.
Understandably, many people remain hesitant about these new COVID-19 vaccines. Knowing someone who was vaccinated and is now protected might be a powerful motivator for behavior change. Studies suggest that personalized stories by physicians and others may be more powerful in countering hesitancy than recitation of numbers or frightening examples.26,27 Thus, it is important for individuals and professionals to speak to others about their own COVID-19 vaccination experience and the feeling of protection that follows vaccination. Because disparities remain across all subgroups, trusted advisors and leaders across disciplines have an important role in educating their constituents about the benefit of vaccination. This is particularly important given our findings that vaccine-hesitant individuals lack trust in both the vaccines and in the vaccine-approval process.
A highly concerning finding is the large gap in likelihood of vaccination by gender, age and education. The gender gap may be partly related to concerns about impact on fertility or pregnancy, at least for young women. Although young adults are frequent spreaders of the virus, only about half of adults aged 18–49 years state they are likely to be vaccinated. It is possible that many young adults feel that high-risk individuals are getting vaccinated so they no longer need to receive the vaccine, or that vaccination is not necessary if they have already had COVID-19. Our findings regarding education level strongly suggest that messaging and outreach efforts must take literacy and health literacy into consideration.28,29 Overall, intense effort is needed to uncover effective methods to address the risk/benefit concerns for COVID-19 vaccines, and focused efforts are needed to educate subgroups via both tailored messages and strategies to optimize access to COVID-19 vaccines.
The marked disparity in the stated likelihood of vaccination by political affiliation, even after adjustment for demographic factors, highlights the potential role of political leaders in assuaging concerns among their constituents and using their power to sway public opinion toward healthy behaviors. Many public officials have posted photos of themselves being vaccinated. To the extent that COVID-19 vaccination has been politicized, it is critical for public officials to lead by example to protect their constituents and our nation.
Our study has multiple strengths. The probability-based online panel is large and nationally representative, by virtue of the fact that respondents are recruited by address-based sampling and are provided with internet enabled tablets if needed. Several studies have demonstrated the representativeness of such panels in comparison to other modes of data collection.30–33 In addition, the response rate is high per survey, and we incorporated information about receipt of COVID-19 vaccines. One limitation is insufficient survey sample size to assess the likelihood of vaccination among individuals with minority backgrounds other than Black, Hispanic, and Asian race/ethnicity. In addition, while we identified factors related to hesitancy for COVID-19, we cannot distinguish the relative importance of these factors.
We conclude that the likelihood of COVID-19 vaccination has risen overall and particularly among Black and Hispanic populations following the US election, with a narrowing of preexisting racial and ethnic disparities in the acceptance of these vaccines. At the same time, the likelihood of vaccination has not increased much among young adults, and disparities remain by gender, age, race/ethnicity, and education level. To reach herd immunity and achieve confidence in current and future COVID-19 vaccines, we will need to overcome vaccine hesitancy among the general population and all subgroups across the US by building trust in the vaccines and in the vaccine approval process.
Acknowledgments
We thank Paul Simon, MD, and Rashmi Shetgiri, MD, of the Los Angeles County Department of Public Health for their scholarly input on an early draft of this manuscript. None of the individuals received compensation for their contributions to this study. The research presented in this paper is that of the authors and does not reflect the official policy of the NIH or NSF.
Conceptualization: Szilagyi, Thomas, Shah, Vizueta, Kapteyn
Data curation: Cui
Formal Analysis: Cui, Vangala, Kapteyn
Funding acquisition: Szilagyi, Kapteyn
Investigation: Thomas, Kapteyn
Methodology: Szilagyi, Thomas, Shah, Vizueta, Kapteyn
Project administration: Szilagyi, Vizueta
Supervision: Szilagyi, Kapteyn
Visualization: Szilagyi, Cui, Vangala
Writing – original draft: Szilagyi
Writing – review & editing: All authors
Disclosure of potential conflicts of interest
Dr. Szilagyi reported receiving a grant from UCLA David Geffen School of Medicine - Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research Award Program for personnel and statistical time. Dr. Szilagyi reported receiving funding from NIH NCATS UCLA CTSI during the conduct of this study.
Dr. Kapteyn reported receiving funding from University of Southern California (USC) for partial support for the USC survey team, grants from Bill and Melinda Gates Foundation for partial support for the UAS survey, grants from the National Institute on Aging for partial support for the UAS survey, and grants from National Science Foundation for partial support for the UAS during the conduct of the study.
Dr. Thomas reported receiving funding from the University of Southern California and the National Institute on Aging.
Role of the Funder/Sponsor
The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
Articles from Human Vaccines & Immunotherapeutics are provided here courtesy of Taylor & Francis
Full text links
Read article at publisher's site: https://doi.org/10.1080/21645515.2021.1929695
Read article for free, from open access legal sources, via Unpaywall:
https://www.tandfonline.com/doi/pdf/10.1080/21645515.2021.1929695?needAccess=true
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/108211688
Article citations
The impact of internet health information seeking on COVID-19 vaccination behavior in China.
BMC Public Health, 24(1):89, 04 Jan 2024
Cited by: 3 articles | PMID: 38178047 | PMCID: PMC10768267
Gender, Age and COVID-19 Vaccination Status in African American Adult Faith-Based Congregants in the Southeastern United States.
J Racial Ethn Health Disparities, 11(5):2827-2838, 14 Aug 2023
Cited by: 2 articles | PMID: 37580437
'They've all endorsed it…but I'm just not there:' a qualitative exploration of COVID-19 vaccine hesitancy reported by Black and Latinx individuals.
BMJ Open, 13(7):e072619, 20 Jul 2023
Cited by: 2 articles | PMID: 37474192 | PMCID: PMC10360437
Prevalence and factors of COVID-19 vaccine refusal among solid cancer patients in China: an application of the health belief model.
Front Public Health, 11:1236376, 03 Aug 2023
Cited by: 2 articles | PMID: 37601174 | PMCID: PMC10435902
Behind closed doors: Protective social behavior during the COVID-19 pandemic.
PLoS One, 18(6):e0287589, 28 Jun 2023
Cited by: 0 articles | PMID: 37379315 | PMCID: PMC10306218
Go to all (21) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Disparities in national and state estimates of COVID-19 vaccination receipt and intent to vaccinate by race/ethnicity, income, and age group among adults ≥ 18 years, United States.
Vaccine, 40(1):107-113, 18 Nov 2021
Cited by: 39 articles | PMID: 34852946 | PMCID: PMC8598948
The role of trust in the likelihood of receiving a COVID-19 vaccine: Results from a national survey.
Prev Med, 153:106727, 16 Jul 2021
Cited by: 62 articles | PMID: 34280405 | PMCID: PMC8284053
Racial/ethnic and nativity disparities in U.S. Covid-19 vaccination hesitancy during vaccine rollout and factors that explain them.
Soc Sci Med, 307:115183, 30 Jun 2022
Cited by: 20 articles | PMID: 35843179 | PMCID: PMC9242888
Interventions to increase COVID-19 vaccine uptake: a scoping review.
Cochrane Database Syst Rev, 8:CD015270, 03 Aug 2022
Cited by: 18 articles | PMID: 35920693 | PMCID: PMC9347311
Review Free full text in Europe PMC
Funding
Funders who supported this work.
NCATS NIH HHS (1)
Grant ID: UL1 TR001881
NIA NIH HHS (1)
Grant ID: U01 AG054580
National Center for Advancing Translational Sciences
National Institute on Aging (1)
Grant ID: 5U01AG054580-03
National Institutes of Health, through the Clinical and Translational Science Awards (CTSA) Program (1)
Grant ID: UL1TR001881
National Science Foundation (1)
Grant ID: #2028683




