Abstract
Introduction
Dengue fever (DF) has become a disease of public health concern. It is a mosquito-borne virus infection caused by one of the four serotypes of the dengue virus, and the disease is prevalent in the tropical and subtropical regions of the world, with a global burden in the Americas. Yearly, about 390 million cases of new infection are estimated to occur.Aims of the study
This study was aimed atdetermining the knowledge, attitude and practices regarding dengue fever amongst health workers in a tertiary health institution in Sokoto state , Nigeria.Methods
A descriptive cross-sectional study was carried out at the Usmanu Danfodiyo University Teaching Hospital, Sokoto, among 367 health-care workers who had worked in the hospital for at least 1 year before the study were selected using a systematic sampling method. Data were collected by trained resident doctors using a standardized, pretested questionnaire and analyzed using SPSS version 20 with a significance set at P > 0.05.Results
There was high awareness (95.1%) among the respondents, with seminars and lectures in school as the most familiar information sources. A more significant proportion, 87.8%, 93.2%, and 76.6%, of the respondents had adequate knowledge, positive attitude, and appropriate DF practice, respectively. Nurses and laboratory scientists had higher practice scores compared to other health-care workers (P = 0.016).Conclusion
Capacity building of health-care workers, especially the primary care physicians on surveillance, proper diagnosis, and treatment, is needed to avoid missing cases or misdiagnosis of cases, especially in developing and underdeveloped countries with limited health resources care service delivery.Free full text

A cross-sectional survey of knowledge, attitude, and practices toward dengue fever among health workers in a tertiary health institution in Sokoto state, Nigeria
Abstract
Introduction:
Dengue fever (DF) has become a disease of public health concern. It is a mosquito-borne virus infection caused by one of the four serotypes of the dengue virus, and the disease is prevalent in the tropical and subtropical regions of the world, with a global burden in the Americas. Yearly, about 390 million cases of new infection are estimated to occur.
Aims of the Study:
This study was aimed atdetermining the knowledge, attitude and practices regarding dengue fever amongst health workers in a tertiary health institution in Sokoto state , Nigeria.
Methods:
A descriptive cross-sectional study was carried out at the Usmanu Danfodiyo University Teaching Hospital, Sokoto, among 367 health-care workers who had worked in the hospital for at least 1 year before the study were selected using a systematic sampling method. Data were collected by trained resident doctors using a standardized, pretested questionnaire and analyzed using SPSS version 20 with a significance set at P > 0.05.
Results:
There was high awareness (95.1%) among the respondents, with seminars and lectures in school as the most familiar information sources. A more significant proportion, 87.8%, 93.2%, and 76.6%, of the respondents had adequate knowledge, positive attitude, and appropriate DF practice, respectively. Nurses and laboratory scientists had higher practice scores compared to other health-care workers (P = 0.016).
Conclusion:
Capacity building of health-care workers, especially the primary care physicians on surveillance, proper diagnosis, and treatment, is needed to avoid missing cases or misdiagnosis of cases, especially in developing and underdeveloped countries with limited health resources care service delivery.
Introduction
Dengue fever (DF) has become a disease of public health concern—the most important arboviral infection globally.[1] It is a mosquito-borne viral infection caused by one of the four serotypes of the dengue virus.[2] The disease is prevalent in the tropical and subtropical regions of the world.[2,3,4] It has been estimated that around 50% of the world population lives in areas where the disease transmission is favorable.[5,6] The global burden is seen in the Americas region with annual 1.5 million cases, and around 3 million cases of the disease were reported in 2019 by the Pan America Health Organization.[7,8] Africa is another region with notable cases,[1] and currently, the disease is endemic in 128 countries.[9,10,11] Yearly, about 390 million new infection cases are estimated to occur,[12] more than estimated by the WHO.[9]
Aedes aegypti and Aedes aldopicus transmit DF—the two mosquitoes responsible for transmitting the disease among humans.[2] DF can develop into a severe form of infection called dengue hemorrhagic fever and can lead to severe complications and even death.[1]
There are two main types of dengue diseases, DF and dengue hemorrhagic fever, and infection due to a particular serotype confers immunity against it; however, an individual can still be infected by other serotypes.[13] Currently, there is no vaccine neither specific treatment for the disease; therefore, controlling the mosquito vectors is critical in the prevention of the disease[14,15]
In Nigeria, the first case of dengue was isolated in the 1960s, but the disease is not among the list of reportable cases in Nigeria,[16] despite the number of diagnosed fevers of unknown cause. A seroprevalence of 30.8, 17.2, and the recent report of 73 among febrile patients have been reported.[17,18,19]
Knowledge, attitude, and health-care workers' practices on the disease are critical for early diagnosis and disease prevention, especially by family physicians who are usually the first contacts for patients.[20,21] The purpose of the current study is to assess the knowledge, attitude, and practices regarding DF among health-care workers (HCWs) in a tertiary health institution in Sokoto, northwestern Nigeria. It is hoped that this will further deepen the study subjects' knowledge and help identify gaps for further interventional studies.
Methods
Study Area and Design: A cross-sectional descriptive study design was carried out among health workers at the Usmanu Danfodiyo University Teaching Hospital (UDUTH), located within Sokoto city. UDUTH is a tertiary health center and serves as a referral center to many hospitals from Nigeria's northwestern region.
Study population and Eligibility: The study population comprises health workers (doctors, pharmacists, laboratory scientists, and nurses) who had worked in the hospital for at least 1 year before this study and came in contact with patients from time to time (inclusion criteria).
Sample Size and Sampling Technique: A sample size of 367 was calculated for the study based on an assumption of 35% from a previous study[22] who had adequate knowledge of the disease. The various health workers' list was obtained from the institution's staff officer, and study subjects were selected proportional to size using a systematic sampling method.
Data Collection and Analysis: Participants' knowledge, attitude, and practices regarding DF that were assessed using a standardized pretested semistructured questionnaire consisting the questions on knowledge, attitude, and practice were administered by trained research assistants. Consent was obtained from the participants before the application of the instrument. Sociodemographic characteristics were also collected. The questionnaires were checked for completeness and entered into SPSS version 20 for subsequent analysis. Mean, standard deviations, proportions calculated, and logistic regression analysis were conducted to identify the relationships among the interests' variables. Correct responses to each question on knowledge and practice attract one mark and zero for incorrect answers, and a cut-off score of >60% was considered for adequate knowledge and appropriate practice. Similarly, concerning attitude, a correct response to strongly agree or agree was given a score of 1, while any response to strongly disagree, disagree, or not sure was awarded 0 scores. The attitude scores were finally graded as a percentage, with ≥60% being positive attitude. The level of significance was set at P < 0.05.
Ethical approval
The approval to conduct the study was granted by the Research and Ethics committee of the Usmanu Danfodiyo University Teaching hospital. Participation was voluntary, and all the information collected from the respondents was treated with uttermost confidentiality. Before the data collection, informed consent was obtained from the respondents.
Results
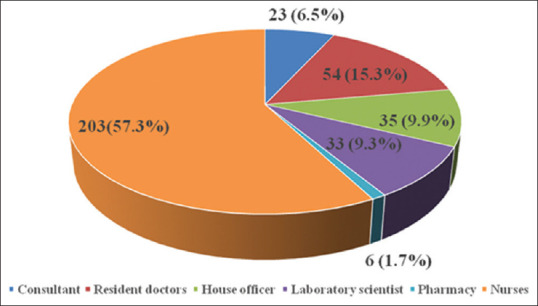
Over a third, 128 (36.7%) of the respondents were below 30 years of age, and only 27 (7.7%) were 50 years and above; the mean age was 35.1 ± 8.3 years. Majority of the respondents were males 219 (60.0%), practiced Islam 242 (67.2%), and married 248 (70.9%). Almost half 170 (47.6%) of the respondents were Hausa by tribe [Table 1]. Over half, 203 (57.3%) of the respondents were nurses, and only 6 (1.7%) were pharmacists [Figure 1].
Table 1
Sociodemographic Characteristics of Respondents
| Variables | Frequency (%) |
|---|---|
| Age in years | |
 <30 <30 | 140 (38.8) |
 30-34 30-34 | 58 (16.0) |
 35-39 35-39 | 66 (18.3) |
 40-44 40-44 | 41 (11.4) |
 45-49 45-49 | 29 (8.0) |
 ≥50 ≥50 | 27 (7.5) |
 Total Total |  361 (100) 361 (100) |
| Mean±SD | 35.1±8.3 |
| Gender | |
 Female Female | 142 (40.0) |
 Male Male | 219 (60.0) |
 Total Total | 365 (100) |
| Religion | |
 Christianity Christianity | 119 (32.8) |
 Islam Islam | 242 (67.2) |
 Total Total | 361 (100) |
| Marital status | |
 Single Single | 105 (26.9) |
 Married Married | 248 (70.9) |
 Separated Separated | 3 (0.9) |
 Divorced Divorced | 1 (0.3) |
 Widowed Widowed | 4 (1.1) |
 Total Total | 361 (100) |
| Tribe | |
 Hausa Hausa | 170 (47.6) |
 Fulani Fulani | 43 (12.0) |
 Yoruba Yoruba | 48 (13.4) |
 Igbo Igbo | 45 (12.6) |
 aOthers aOthers | 55 (14.3) |
 Total Total | 357 (100) |
aOthers-Tiv, Zuru, Kabba, Edo
More than 90% (347) of the respondents heard of DF, with seminars and lectures in school being the commonest sources of information regarding the disease. However, less than half 167 (48.1%) had experience in reporting suspected DF cases.
The majority of the respondents, 309 (84.0%), knew DF is transmitted when mosquito bites and more than half 208 (56.7%) knew Aedes mosquito as the responsible vector for the transmission of the disease. A total of 144 (44.4%) of the subjects knew that ponds and rivers are breeding grounds for the vector. The majority of the respondents (75.4%) knew that DF could be spread from human to human. They also knew that fever 341 (94.7%), nausea and vomiting 331 (93.8%), bleeding 325 (91.3%), headache 329 (94.3%), rash 257 (75.4%), and abdominal pain 275 (79.5%) are symptoms of DF [Table 2].
Table 2
Knowledge of HCWs Regarding Dengue Fever
| Knowledge of causes, spread, and symptoms of dengue fever Variables | Frequency |
|---|---|
| Ever heard of dengue fever | |
 Yes Yes | 347 (95.1) |
 No No | 18 (4.9) |
| Source of information regarding DF | |
 Radio/Television Radio/Television | 74 (20.3 |
 Seminars Seminars | 181 (49.6) |
 Lectures in school Lectures in school | 94 (25.8) |
 Others Others | 16 (4.4) |
| Experience in reporting suspected dengue fever case | |
 Yes Yes | 167 (48.1) |
 No No | 180 (51.9) |
| Transmission of dengue fever | |
 Bite of mosquito Bite of mosquito | 309 (84.0) |
 Needle stick injury Needle stick injury | 5 (1.3) |
 Through sexual intercourse Through sexual intercourse | 6 (1.5) |
 Through the bite of ticks Through the bite of ticks | 7 (2.1) |
 Airborne Airborne | 9 (2.3) |
 Drinking dirty water Drinking dirty water | 14 (3.9) |
 Houseflies Houseflies | 2 (0.5) |
 Don’t know Don’t know | 16 (4.4) |
| Type of mosquito involved in transmission | |
 Aedes Aedes | 208 (56.7) |
 Culex Culex | 37 (9.9) |
 Anopheles Anopheles | 51 (13.8) |
 Don’t know Don’t know | 72 (19.6) |
| Breeding ground for the vector* | |
 Pond/Rivers Pond/Rivers | 144 (44.4) |
 Cans Cans | 38 (11.7) |
 Roof gutters Roof gutters | 97 (29.9) |
 Water containers Water containers | 105 (32.4) |
| DF can be spread from human to human | |
 Yes Yes | 261 (75.4) |
 No No | 85 (24.6) |
| Fever is a symptom of DF | |
 Yes Yes | 341 (94.7) |
 No No | 19 (5.3) |
| Nausea and vomiting are symptoms of DF | |
 Yes Yes | 331 (93.8) |
 No No | 22 (6.2) |
| Bleeding is a symptom of DF | |
 Yes Yes | 325 (91.3) |
 No No | 31 (8.7) |
| Muscular pain is a symptom of DF | |
 Yes Yes | 330 (93.5) |
 No No | 23 (6.5) |
| Headache is a symptom of DF | |
 Yes Yes | 329 (94.3) |
 No No | 20 (5.7) |
| Rash is associated with DF | |
 Yes Yes | 257 (75.4) |
 No No | 84 (24.6) |
| Abdominal pain is a symptom of DF | |
 Yes Yes | 275 (79.5) |
 No No | 71 (20.5) |
| Graded knowledge on causes, spread, and symptoms | |
 Inadequate knowledge (<60%) Inadequate knowledge (<60%) | 36 (10.0) |
 Adequate knowledge (≥60%) Adequate knowledge (≥60%) | 325 (90.0) |
*Multiple responses
Almost all the respondents knew that mosquito spray with insecticides 338 (95.8%), mosquito mat/coil/vaporizers 295 (86.0%), windows and door screen 307 (87.4%), cleaning of garbage/trash 318 (91.9%), preventing water stagnation 344 (96.6%), and pouring chemical in standing water 299 (86.9%) can prevent DF infection.
Almost all the respondents were knowledgeable about the vector characteristics. However, 141 (46.1%) of the respondents knew that the vector frequently bites during the morning and daytime 175 (55.2%) [Table 3].
Table 3
Knowledge of HCWs Prevention and Vector Characteristics
| Variables | Frequency |
|---|---|
| Prevention of dengue fever | |
| Mosquito spray with insecticides can prevent DF | |
 Yes Yes | 338 (95.8) |
 No No | 15 (4.2) |
| Mosquito mat/coil/liquid vaporizer can prevent DF | |
 Yes Yes | 295 (86.0) |
 No No | 48 (14.0) |
| Windows and door screen can prevent DF | |
 Yes Yes | 304 (87.4) |
 No No | 44 (12.6) |
| Cleaning house can prevent DF | |
 Yes Yes | 329 (93.2) |
 No No | 24 (6.8) |
| Cleaning of garbage/trash can prevent DF | |
 Yes Yes | 318 (91.9) |
 No No | 28 (8.1) |
| Preventing water stagnation can prevent DF | |
 Yes Yes | 344 (96.6) |
 No No | 12 (3.4) |
| Application of mosquito-eating fish can prevent DF | |
 Yes Yes | 218 (64.7) |
 No No | 119 (35.3) |
| Pouring chemicals in standing water can prevent mosquito breeding | |
 Yes Yes | 299 (86.9) |
 No No | 45 (13.1) |
| Covering water containers can prevent breeding of mosquitoes | |
 Yes Yes | 311 (90.4) |
 No No | 33 (9.4) |
| Cutting bushes around the house can prevent breeding of mosquitoes | |
 Yes Yes | 337 (94.9) |
 No No | 18 (5.1) |
| Vector characteristics of dengue | |
| The vector breeds in water storage jars/containers | |
 Yes Yes | 303 (88.9) |
 No No | 38 (11.1) |
| The vector breeds in coolers, tires, and pots | |
 Yes Yes | 236 (70.7) |
 No No | 98 (29.3) |
| The vector breeds in dirty water | |
 Yes Yes | 324 (93.6) |
 No No | 22 (6.4) |
| The vector breeds in garbage/trash | |
 Yes Yes | 288 (83.5) |
 No No | 57 (16.5) |
| The vector breeds in plants/vegetation | |
 Yes Yes | 266 (79.9) |
 No No | 67 (20.1) |
| The vector frequently bite in the morning | |
 Yes Yes | 141 (46.1) |
 No No | 162 (53.5) |
| The vector frequently bite in the day time | |
 Yes Yes | 175 (55.2) |
 No No | 142 (44.8) |
| The vector frequently bite in the evening | |
 Yes Yes | 188 (60.3) |
 No No | 124 (39.7) |
| The vector frequently bite at night | |
 Yes Yes | 146 (47.2) |
 No No | 163 (52.8) |
| The vector bites both day and night | |
 Yes Yes | 88 (27.8) |
 No No | 228 (72.2) |
There were some misconceptions concerning the treatment of DF as only a third 116 (34.0%) felt that patients with the disease who had no warning signs should be hospitalized and that antibacterial 123 (36.5%) and antiviral drugs 148 (44.3%) should be given to patients suspected of having DF.
Overall, most 318 (87.8%) of the respondents had adequate DF knowledge [Table 4].
Table 4
Knowledge of HCWs on the Treatment of Dengue Fever
| Variables | Frequency |
|---|---|
| Patients with dengue fever without warning signs should be hospitalized | |
 Yes Yes | 116 (34.0) |
 No No | 225 (66.0) |
| Patients with dengue without warning signs but with other existing diseases should be hospitalized | |
 Yes Yes | 306 (89.7) |
 No No | 35 (10.3) |
| Patients with dengue fever with warning signs should be hospitalized | |
 Yes Yes | 328 (95.3) |
 No No | 16 (4.7) |
| Patients with severe dengue should be hospitalized | |
 Yes Yes | 335 (97.7) |
 No No | 8 (2.3) |
| Intravenous fluids hydration should be given to patients suspected to have dengue fever | |
 Yes Yes | 310 (90.9) |
 No No | 31 (9.1) |
| Paracetamol should be given to patients suspected to have dengue fever | |
 Yes Yes | 254 (75.1) |
 No No | 84 (24.9) |
| Antibacterial drugs should be given to patients suspected to have dengue fever | |
 Yes Yes | 123 (36.5) |
 No No | 214 (63.5) |
| Antiviral drugs should be given to patients suspected to have dengue fever | |
 Yes Yes | 148 (44.3) |
 No No | 186 (55.7) |
| Overall graded knowledge of HCWs | |
 Inadequate knowledge (<60%) Inadequate knowledge (<60%) | 44 (12.2) |
 Adequate knowledge (≥60%) Adequate knowledge (≥60%) | 318 (87.8) |
The sociodemographic variables had no significant impact on years of experience and overall (graded) knowledge of HCWs regarding the disease. Less than half (45.0%) of the respondents with adequate knowledge had ≥10 years of experience, and this was statistically significant (P = 0.011) [Table 5].
Table 5
Correlates of Overall Graded Knowledge of HCWs Regarding Dengue Fever
| Variables | Overall graded knowledge | Test statistics, P | |
|---|---|---|---|
|
| |||
| Inadequate (<60%) Frequency (%) | Adequate (≥60%) Frequency (%) | ||
| Age (years) | |||
 <34 <34 | 23 (54.8) | 147 (48.7) | χ2=0.55 |
 ≥34 ≥34 | 19 (45.2) | 155 (51.3) | P=0.51 |
| Gender | |||
 Female Female | 19 (44.2) | 123 (38.8) | χ2=0.46 |
 Male Male | 24 (55.8) | 194 (61.2) | P=0.51 |
| Religion | |||
 None None | 0 (0.0) | 2 (0.6) | χ2=1.26 |
 Christian Christian | 13 (30.2) | 99 (31.6) | P=0.74 |
 Islam Islam | 28 (65.1) | 205 (65.5) | |
 Others Others | 2 (4.7) | 7 (2.2) | |
| Marital status | |||
 Unmarried Unmarried | 11 (26.8) | 89 (29.3) | χ2=0.105 |
 Married Married | 30 (73.2) | 215 (70.7) | P=0.855 |
| Years of experience | |||
 <10 <10 | 28 (77.8) | 154 (55.0) | χ2=6.78 |
 ≥10 ≥10 | 8 (22.2) | 126 (45.0) | P=0.011* |
*P<0.05
The association between respondents' cadres and overall DF knowledge was significant (P < 0.001). Consultants, resident doctors, house officers, pharmacists, and nurses had higher knowledge scores than the laboratory scientists.
The majority of the respondents opined that DF is a serious illness 275 (78.2%) but can be prevented, 233 (66.6%) and there is a need for treatment, and hospitalization 224 (65.9%) and 246 (73.7%) agreed that any community with suspected symptoms should seek for medical advice. Almost all 330 (93.2%) respondents had a positive attitude toward DF. The majority (76.2%) of the subjects strongly believed that DF is a serious health problem and were of the strong belief that they were at risk of contracting the illness; similarly, a greater proportion (65.7%) believed that the government has a responsibility in ensuring that the vector breeding places are adequately controlled.
Overall, 330 (93.2%) of the study subjects had a positive attitude toward the illness. However, no significant relationship was seen between the sociodemographic variables, including years of experience and overall (graded) attitude of HCWs regarding DF. Nurses had higher attitude scores compared with laboratory scientists, and this was statistically significant (P = 0.025) [Tables [Tables66 and and77].
Table 6
The attitude of HCWs toward Dengue Fever
| Variables | Frequency (%) |
|---|---|
| Dengue is a serious illness | |
 Strongly agree Strongly agree | 275 (78.2) |
 Agree Agree | 66 (18.8) |
 Disagree Disagree | 4 (1.1) |
 Strongly disagree Strongly disagree | 2 (0.6) |
 Not sure Not sure | 5 (1.4) |
| You are at risk of getting dengue fever | |
 Strongly agree Strongly agree | 147 (42.6) |
 Agree Agree | 116 (33.6) |
 Disagree Disagree | 35 (10.1) |
 Strongly disagree Strongly disagree | 22 (6.4) |
 Not sure Not sure | 25 (7.2) |
| Dengue fever can be prevented | |
 Strongly agree Strongly agree | 233 (66.6) |
 Agree Agree | 100 (28.6) |
 Disagree Disagree | 5 (1.4) |
 Strongly disagree Strongly disagree | 8 (2.3) |
 Not sure Not sure | 4 (1.1) |
| There is a need for treatment and hospitalized for dengue fever | |
 Strongly agree Strongly agree | 224 (65.9) |
 Agree Agree | 104 (30.6) |
 Disagree Disagree | 3 (0.9) |
 Strongly disagree Strongly disagree | 7 (2.1) |
 Not sure Not sure | 2 (0.6) |
| Government has a responsibility for the control of mosquito breeds | |
 Strongly agree Strongly agree | 228 (65.7) |
 Agree Agree | 94 (27.1) |
 Disagree Disagree | 15 (4.3) |
 Strongly disagree Strongly disagree | 5 (1.4) |
 Not sure Not sure | 5 (1.4) |
| Do you feel that dengue is a major problem for your patient population | |
 Strongly agree Strongly agree | 138 (39.7) |
 Agree Agree | 110 (31.6) |
 Disagree Disagree | 69 (19.8) |
 Strongly disagree Strongly disagree | 12 (3.4) |
 Not sure Not sure | 19 (5.5) |
| Your patient feel that dengue infection is a major problem for their health | |
 Strongly agree Strongly agree | 127 (36.4) |
 Agree Agree | 121 (34.7) |
 Disagree Disagree | 56 (16.0) |
 Strongly disagree Strongly disagree | 13 (3.7) |
 Not sure Not sure | 32 (9.2) |
| In your experience, do you think that a member of the community who exhibits symptoms of DF should seek medical attention | |
 Strongly agree Strongly agree | 246 (73.7) |
 Agree Agree | 66 (19.8) |
 Disagree Disagree | 14 (4.2) |
 Strongly disagree Strongly disagree | 6 (1.8) |
 Not sure Not sure | 2 (0.6) |
| Graded attitude of HCWs | |
 Positive attitude (≥60%) Positive attitude (≥60%) | 330 (93.2) |
 Negative attitude (<60%) Negative attitude (<60%) | 24 (6.8) |
Table 7
Correlates of Overall Graded Attitude of HCWs Regarding Dengue Fever
| Variables | Overall graded attitude | Test statistics P | |
|---|---|---|---|
|
| |||
| Poor (<60%) | Good (≥60%) | ||
| Age (years) | |||
 <34 <34 | 9 (40.9) | 158 (50.2) | χ2=0.70 |
 ≥34 ≥34 | 13 (59.1) | 157 (49.8) | P=0.51 |
| Gender | |||
 Female Female | 9 (37.5) | 131 (39.9) | χ2=0.05 |
 Male Male | 15 (62.5) | 197 (60.1) | P=1.00 |
| Religion | |||
 None None | 0 (0.0) | 2 (0.6) | χ2=1.44 |
 Christianity Christianity | 7 (30.4) | 103 (31.7) | P=0.698 |
 Islam Islam | 16 (69.6) | 212 (65.2) | |
 Others Others | 0 (0.0) | 8 (2.5) | |
| Marital status | |||
 Unmarried Unmarried | 7 (29.2) | 91 (29.1) | χ2=0.00 |
 Married Married | 17 (70.8) | 222 (70.9) | P=1.00 |
| Years of experience | |||
 <10 <10 | 12 (54.5) | 166 (57.8) | χ2=0.09 |
 ≥10 ≥10 | 10 (45.5) | 121 (42.2) | P=0.83 |
*P<0.05
The majority of the respondents, 269 (76.6%), had appropriate practice concerning DF. However, about half 160 (48.6%) of them would admit patients with DF without warning signs, 115 (35.1%) would give antibacterial drugs, while another 143 (43.6%) of the respondents will give antiviral drugs to patients suspected to have DF. Less than half (45%) of the HCWs agreed to have received any training on hemorrhagic fevers, including DF, in the last year [Tables [Tables88 and and99].
Table 8
The practice of HCWs Regarding Dengue Fever
| Variables | Frequency |
|---|---|
| Use mosquito spray to prevent mosquito bite | |
 Yes Yes | 313 (91.5) |
 No No | 29 (8.5) |
| Clean garbage/trash to prevent mosquito bite | |
 Yes Yes | 322 (94.7) |
 No No | 18 (5.3) |
| Prevent water stagnation at home | |
 Yes Yes | 339 (98.3) |
 No No | 6 (1.6) |
| Use window and/or door screens to prevent access to mosquitoes | |
 Yes Yes | 316 (93.2) |
 No No | 23 (6.8) |
| Admit patients with DF without warning signs | |
 Yes Yes | 160 (48.6) |
 No No | 169 (51.4) |
| Admit patients with DF without warning signs but with co-morbidities | |
 Yes Yes | 236 (72.6) |
 No No | 89 (27.4) |
| Admit patients with DF with warning signs | |
 Yes Yes | 277 (83.4) |
 No No | 55 (16.6) |
| Give IV fluid hydration to patients suspected to have DF | |
 Yes Yes | 257 (78.1) |
 No No | 72 (21.9) |
| Give Paracetamol to patients suspected to have DF | |
 Yes Yes | 230 (70.6) |
 No No | 96 (29.4) |
| Give antibacterial drugs to patients suspected to have DF | |
 Yes Yes | 115 (35.1) |
 No No | 213 (64.9) |
| Give antiviral to patients suspected to have DF | |
 Yes Yes | 143 (43.6) |
 No No | 185 (56.4) |
| Graded Practice of HCWs regarding DF | |
 Appropriate practice (≥60%) Appropriate practice (≥60%) | 269 (76.6) |
 Inappropriate practice (<60%) Inappropriate practice (<60%) | 82 (23.4) |
Table 9
Correlates of Overall Graded Practice of HCWs Regarding Dengue Fever
| Variables | Overall Graded Practice | Test statistics P | |
|---|---|---|---|
|
| |||
| Inappr. (<60%) Frequency (%) | Appr. (≥ 60%) Frequency (%) | ||
| Age (years) | |||
 <34 <34 | 41 (51.9) | 125 (49.0) | χ2=0.20 |
 ≥34 ≥34 | 38 (48.1) | 130 (51.0) | P=0.70 |
| Gender | |||
 Female Female | 36 (43.9) | 104 (39.0) | χ2=0.64 |
 Male Male | 46 (56.1) | 163 (61.0) | P=0.44 |
| Religion | |||
 None None | 0 (0.0) | 2 (0.8) | χ2=2.76 |
 Christianity Christianity | 29 (36.7) | 80 (30.2) | P=0.43 |
 Islam Islam | 49 (62.0) | 176 (66.4) | |
 Others Others | 1 (1.3) | 7 (2.6) | |
| Marital status | |||
 Unmarried Unmarried | 23 (30.3) | 74 (28.7) | χ2=0.07 |
 Married Married | 53 (69.7) | 184 (71.3) | P=0.78 |
| Years of experience | |||
 <10 <10 | 48 (70.6) | 129 (54.2) | χ2=5.82 |
 ≥10 ≥10 | 20 (29.4) | 109 (45.8) | P=0.018* |
*P<0.05
Most 48 (70.6%) of the respondents with inappropriate practice had <10 years of experience and this was statistically significant (c2 = 5.82, P = 0.018). Nurses and laboratory scientists had higher practice scores compared with other health professionals, and this was statistically significant (P = 0.016) [Table 10].
Table 10
Knowledge, Attitude, and Practice of HCWs and Their Cadre
| Dependent variables | Consultant | Resident doctor | House officer | Laboratory scientist | Pharmacy | Nurses | P |
|---|---|---|---|---|---|---|---|
| Overall knowledge | 80.20±20.13 | 75.46±13.65 | 76.74±9.52 | 62.50±18.06 | 81.67±9.54 | 78.91±15.93 | 0.000** |
| Attitude | 77.86±24.08 | 82.27±13.37 | 81.33±12.76 | 75.20±15.91 | 71.88±16.09 | 83.91±14.90 | 0.025* |
| Practice | 67.19±24.17 | 69.76±21.28 | 67.53±19.63 | 71.21±20.41 | 69.09±23.71 | 77.67±21.29 | 0.016* |
**P<0.001; *P<0.05. One-way ANOVA: Analysis of variance
Discussion
DF is a global infection of public health importance, endemic in about 128 countries with an estimated prevalence of 3.9 billion.[12,23] HCWs, especially family physicians being the gatekeepers on health issues and first contacts with patients, are the core workforce expected to change this trend. Their overall operational capacity in dealing with DF is therefore of paramount importance. Our study investigated the knowledge, attitude, and practice of DF among HCWs in Sokoto. As shown in the data, and similar to another study carried out in Abidjan, Cote de'Ivoire,[24] more than half (54.8%) of the respondents were below 35 years of age, the active period of life with high chances of exposure to the outside environment. As expected, males constituted the majority (60%) of the study subjects, and this agrees with the findings of Tan et al.;[21] however, similar studies conducted in Tanzania and Quebec, Canada, showed female preponderance.[25,26] Our study's male dominance may not be unconnected with the low female school enrollment and our study area's sociocultural milieu.[27] Similar to another study elsewhere,[24] it was observed from our study that more than half (57.3%) of our respondents were nurses who also constituted the majority of the health workforce in the teaching hospital, but in contrast with other studies where doctors were the majority.[26,28,29]
Our study's findings showed that less than half (42%) of the study subjects had more than 10 years of working experience as health workers. Ekra et al. found a lower figure of 31% amongst their subjects.[24] In contrast to our findings, higher figures (51% and 65%) were observed in other studies elsewhere.[26,28]
The majority of our study subjects (95.1%) were aware of DF before now; varying levels of awareness ranging from 34.5% to 77% had been recorded in previous studies.[30,31,32] The high level of awareness amongst our study subjects compared with the other studies may not be unconnected with the fact that our study was amongst HCWs while the other studies were in the general population with varying levels of awareness as observed in the findings.
The commonest source of information on DF by our respondents was through hospital seminars and training during outbreaks, especially on other hemorrhagic fevers. This is in agreement with the findings of Ekra et al. in Abidjan, Cote d'Ivoire.[24]
The study revealed that most of the respondents had good knowledge of causes, spread, and DF symptoms with a score of 75% and above. This is not unexpected considering the background of the study subjects and the fact that working in a tertiary health and training institution exposes them to continuing medical education in the form of seminars and clinical meetings. However, lesser knowledge scores were reported among health workers in Tanzania and residents of Westmoreland, Jamaica.[25,33] In contrast to our findings, higher scores were reported from Pakistan and India.[34,35] On the knowledge of the HCWs on prevention and vector characteristics, more than 80% were quite knowledgeable; however, more than half (55.2%) of the respondents knew that the vector bites during the daytime. This is higher than the findings from the study of Kajeguka and his colleagues in Tanzania,[25] where only 26.3% of the participants knew that the mosquitoes that transmit DF are daytime biters. Similarly, other studies observed good knowledge of the transmission by Aedes mosquitoes.[36,37,38]
Findings from our study showed that the knowledge of DF treatment was good, with 67.7% of the participants scoring 75% and above; however, Kajeguka et al.,[25] in 2017, reported over treatment of malaria in the absence of diagnosis. Another study by Nguyen and his coresearchers revealed missed opportunities by primary health physicians to improve dengue prevention through communication.[39]
Overall, the majority (87.8%) of our respondents had adequate knowledge of the cause, transmission, treatment, and prevention of DF. This contrasts with other studies that found only 10.3% with high knowledge[40] and other studies with low knowledge levels from India, Pakistan, Thailand, and Jamaica.[32,33,40,41,42,43,44]
Furthermore, it was observed from our study that the majority of our subjects expressed a positive attitude toward DF. Studies elsewhere observed similar positive attitudes, although not as high as observed in this study.[33,40,40,45] The proportion of respondents that showed a positive attitude toward DF is not surprising, although it has been shown that good knowledge about DF could translate to positive attitudes.[46]
On the overall graded practice of preventing DF, most study subjects (76.6%) had appropriate practices. This is in agreement with findings from other studies elsewhere.[45,47] On the other hand, some other studies observed varying practice levels from 49.6% to 57.3%.[36,38,40] The difference between our study and these other studies may not be unrelated to the fact that ours was among health workers while these others were from community-based studies. The health workers are usually the first contacts of patients in all health facilities; therefore, the perception of being at risk of infection, frequent training, and continuous provision of information, education, and communication invariably strengthen good practices. Although education plays an essential role in enhancing good practices, it has been observed that education alone cannot be correlated with knowledge.[33] It is therefore not surprising that nurses in our study had better practice than other health workers. Ekra et al. observed similar findings from their study.[24]
In terms of correlates of overall graded knowledge and attitudes of the HCWs, there was no statistically significant association between sociodemographic variables, including years of experience. However, in terms of practice, HCWs with more than 10 years' experience were two times more likely to have fair practice compared with others. The overall knowledge score of DF between respondents' cadres was found significant (P < 0.001) among consultants, resident doctors, house officers, pharmacist, and nurses and had a higher knowledge score than the laboratory scientist probably due to the few numbers of cases seen or wrong laboratory investigation and diagnosis. Nurses had a significant higher attitude score compared with laboratory scientists (P = 0.025); however, nurses and laboratory scientists had significant higher practice scores compared with other health professionals (P = 0.016), and this could be due to safety precautions adopted, especially by these cadres of HCWs to limit exposure and contact with suspected patients and samples.
Summary
Findings from our study indicated that the respondents had high awareness about DF with seminars and lectures in school as the commonest sources of information. A greater proportion of the respondents had adequate knowledge, a positive attitude, and appropriate DF practice, respectively. The need to increase sensitization of HCWs on attitude and practice of DF prevention is timely and essential considering the population at risk globally and the impact of population growth, urbanization, and climate change. Surveillance, proper diagnosis, and treatment are needed to avoid missing cases or misdiagnosed cases, especially in developing and underdeveloped countries with limited resources in terms of health-care service delivery. Communicating the regular geographical distribution and global burden to alert HCWs is equally essential. The need to develop programs and activities aimed at capacity development of HCWs, especially the primary health-care physicians, to avoid missing or misdiagnosed cases of DF is critical.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
Articles from Journal of Family Medicine and Primary Care are provided here courtesy of Wolters Kluwer -- Medknow Publications
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/119590494
Article citations
Knowledge, attitudes, and practices of health care professionals regarding dengue fever: need for training and provision of diagnostic equipment in Togo in 2022, a cross-sectional study.
Front Public Health, 12:1375773, 10 Jun 2024
Cited by: 0 articles | PMID: 38915751 | PMCID: PMC11194359
Uncovering the knowledge gap: A web-based survey of healthcare providers' understanding and management of dengue fever in East Azerbaijan, Iran.
PLoS One, 19(6):e0305528, 21 Jun 2024
Cited by: 0 articles | PMID: 38905180 | PMCID: PMC11192336
Health professionals' knowledge on dengue and health facility preparedness for case detection: A cross-sectional study in Dar es Salaam, Tanzania.
PLoS Negl Trop Dis, 17(11):e0011761, 21 Nov 2023
Cited by: 2 articles | PMID: 37988330 | PMCID: PMC10662763
Anti-Arbovirus Antibodies Cross-React With Severe Acute Respiratory Syndrome Coronavirus 2.
Microbiol Spectr, 10(6):e0263922, 29 Nov 2022
Cited by: 5 articles | PMID: 36445096 | PMCID: PMC9769545
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Determinants of appropriate knowledge on human immunodeficiency virus postexposure prophylaxis among professional health-care workers in Sokoto, Nigeria.
J Family Med Prim Care, 7(2):340-345, 01 Mar 2018
Cited by: 3 articles | PMID: 30090775 | PMCID: PMC6060946
Knowledge, attitude, and practice regarding prevention of rheumatic heart disease among primary health-care workers in sokoto metropolis, Sokoto State, Nigeria.
Ann Afr Med, 22(1):61-69, 01 Jan 2023
Cited by: 2 articles | PMID: 36695224 | PMCID: PMC10064898
Awareness and attitude to deceased kidney donation among health-care workers in Sokoto, Nigeria.
Ann Afr Med, 17(2):75-81, 01 Apr 2018
Cited by: 2 articles | PMID: 29536961 | PMCID: PMC5875123
'Seven Plus One' a unique approach to assess the knowledge, attitude and practices for dengue prevention and control among frontline workers of a teaching institution in Rishikesh, Uttarakhand.
J Family Med Prim Care, 13(6):2209-2215, 14 Jun 2024
Cited by: 0 articles | PMID: 39027846 | PMCID: PMC11254040
Review Free full text in Europe PMC