Abstract
Free full text

Satiety Associated with Calorie Restriction and Time-Restricted Feeding: Peripheral Hormones
ABSTRACT
Calorie restriction (CR) is a common approach to inducing negative energy balance. Recently, time-restricted feeding (TRF), which involves consuming food within specific time windows during a 24-h day, has become popular owing to its relative ease of practice and potential to aid in achieving and maintaining a negative energy balance. TRF can be implemented intentionally with CR, or TRF might induce CR simply because of the time restriction. This review focuses on summarizing our current knowledge on how TRF and continuous CR affect gut peptides that influence satiety. Based on peer-reviewed studies, in response to CR there is an increase in the orexigenic hormone ghrelin and a reduction in fasting leptin and insulin. There is likely a reduction in glucagon-like peptide-1 (GLP-1), peptide YY (PYY), and cholecystokinin (CCK), albeit the evidence for this is weak. After TRF, unlike CR, fasting ghrelin decreased in some TRF studies, whereas it showed no change in several others. Further, a reduction in fasting leptin, insulin, and GLP-1 has been observed. In conclusion, when other determinants of food intake are held equal, the peripheral satiety systems appear to be somewhat similarly affected by CR and TRF with regard to leptin, insulin, and GLP-1. But unlike CR, TRF did not appear to robustly increase ghrelin, suggesting different influences on appetite with a potential decrease of hunger after TRF when compared with CR. However, there are several established and novel gut peptides that have not been measured within the context of CR and TRF, and studies that have evaluated effects of TRF are often short-term, with nonuniform study designs and highly varying temporal eating patterns. More evidence and studies addressing these aspects are needed to draw definitive conclusions.
Introduction
Obesity rates have been increasing since the 1980s, and between 2000 and 2018 the prevalence of obesity increased from 30.5% of the US population to 42.4% (1). Weight loss and maintenance have become critical aspects of health care owing to the increased risk of disease associated with obesity as well as economic costs and poor quality of life. Weight gain or weight loss occurs when energy intake and energy expenditure become unbalanced. On the energy intake side, the behavior surrounding eating is complex and numerous factors affect how appetite is perceived and acted on. Rooted in biology, circulating hormones (2–6), neural components (6–12), and cellular/molecular pathways (13) may play important roles in determining satiation or satiety. On the environmental side, demographics, the food environment, social/economic, and psychological circumstances also are factors. Although the current article focuses on the biological aspects of appetite regulation in the context of energy intake regulation, it is important to understand social/demographic/economic/cultural determinants as well and all are active areas of investigation.
Individuals may choose a variety of dietary approaches involving calorie restriction (CR) to achieve the goal of inducing weight loss. A constant daily level of CR has traditionally been used to elicit an energy deficit, causing related changes to hunger and satiety signaling as the body responds to a change in energy balance. However, recent insights into the importance of circadian signaling have demonstrated that the daily window in which one consumes calories may have an impact on the metabolic factors related to food regulation (14–16). As a result, time-restricted feeding (TRF), when one limits the hours of the day during which one consumes one's meals and extends the time spent fasting, has become a popular dietary pattern used to achieve weight loss. These alterations to biochemical signaling and neural networks may elicit slight changes in appetite and satiety, but to our knowledge, the differences between TRF and constant daily CR in this area have not been investigated. Further, the change in appetite and satiety within the circadian cycle in TRF or CR compared with ad libitum eating has not been examined.
Several hormones are linked to orexigenic and anorexigenic aspects of eating behavior (17) such as ghrelin, glucagon-like peptide-1 (GLP-1), cholecystokinin (CCK), peptide YY (PYY3-36), glucose-dependent insulinotropic polypeptide (GIP), pancreatic polypeptide (PP), insulin, amylin, and leptin (18). Numerous other peptides have been hypothesized to affect appetite (19–22). The current article focuses on those that have been studied within the context of CR and TRF in humans. Appetite describes the overall drive to eat food that manifests in searching/foraging behaviors, as well as choosing what foods to eat (23), whereas satiety reduces appetite and affects the frequency of meals throughout the day. The magnitude of food consumed in each meal influences satiation—the feeling of “fullness" that increases during food consumption and which may bring about the end of a single meal, although factors other than fullness can result in the termination of a meal (24, 25).
Hunger and satiety mechanisms that are associated with food intake behavior also play a critical role in both weight loss and weight maintenance. The focus of this review is to present evidence about how hormonal hunger and satiety signals are affected by TRF and CR paradigms, to glean insight into what that might mean for adherence to these regimes. A companion review will address the evidence with regard to the central neuroendocrine systems affected by TRF and CR.
CR
CR involves a consistent reduction in daily caloric intake, but without malnourishment or underconsumption of essential vitamins, minerals, and trace elements (26), and is often touted as the best antiaging intervention (27). By design, CR places an individual in a negative energy balance when the energy consumed is less than what is expended, making it integral to losing weight in overweight/obese individuals (28). CR can be achieved by several approaches including diet, exercise, and appetite-altering pharmacological and surgical interventions. Of particular note, leptin, ghrelin (29), insulin (30), PYY3-36, and CCK-8 (31) have been evaluated under fasting and CR paradigms. The current report will focus on CR of 15%–75% restriction whether it was intended for weight loss or not, and its effect on pathways of peripheral and central regulation of satiety.
TRF
Fasting is defined by brief periods of ceasing caloric intake and differs from starvation, which is a degenerative condition of prolonged malnutrition. Intermittent fasting (IF) is a broader term used to describe a range of extended fasting periods. This may include alternate-day fasting (ADF), where one fasts every other day or undertakes a 1- to 2-d fast each week with the remaining days following an ad libitum feeding pattern. Another subset of temporal dietary patterns under the umbrella of IF is referred to as TRF. A TRF dietary pattern calls for daily periods of fasting, traditionally defined by avoiding energy intake while allowing for water intake during a certain time frame (32). There are variations in TRF allowing individuals to follow a 12- to 21-h fasting period, with an ad libitum feeding cycle lasting from 3 to 12 h (33). A common TRF pattern calls for fasting 16 h of the day and eating freely for the remaining 8 h (16:8 diet), and it may have gained popularity because it is a reasonable approach in comparison with some of the more restrictive feeding windows (34).
Traditional CR diets typically do not restrict feeding times but focus on decreasing caloric intake by 15%–40% (35). TRF does not necessarily result in CR because it can be adhered to with normative caloric intake (36). However, decreased feeding windows may cause an individual to consume less energy (14). Also eating meals closer together in time, as happens during a 16:8 diet, can reduce the time available to empty gastric contents between meals, potentially reducing the capacity for caloric intake (37). Fasting catalyzes a shift to using endogenous substrate stores, causing a spectrum of metabolic reactions dependent on the time spent in an energy deficit. This can affect the orchestration of hormonal hunger and satiety signals by the hypothalamus, a key regulator of neuroendocrine signaling in response to energy status (38). Few studies have directly assessed the effects of TRF on appetite, typically including a few select hormones as part of a study with aims centered on metabolic effects (14, 36).
Current Status of Knowledge: Hormonal Control of Food Intake
Studies were identified by searching the PubMed and Google Scholar electronic databases for peer-reviewed, English-language publications. The search terms included “leptin," “insulin," “ghrelin," “GLP-1/glucagon-like peptide-1/GLP," “PYY/PYY3-36/peptide YY," “amylin/IAPP/islet/insulinoma amyloid polypeptide/DAP/diabetes-associated peptide," “GIP/gastric inhibitory peptide/glucose‐dependent insulinotropic polypeptide," “PP/pancreatic polypeptide," “CCK/cholecystokinin," and “orexin" with “calorie/caloric restriction" and “time-restricted feeding/TRF" and “weight loss." Only reports with human participants were included, with the exception of orexin and while addressing the background of each hormone. Acute feeding challenges that involved single-meal or single-day protocols were excluded. Tables 1 and 2 are summaries of outcomes from studies that have looked at either CR or TRF, respectively, and their effect on satiety hormones. Figure 1 presents a graphical summary of satiety hormones, and their interplay at the level of the gastrointestinal tract, along with highlighting the overarching changes seen in CR and TRF conditions in the fasted state.
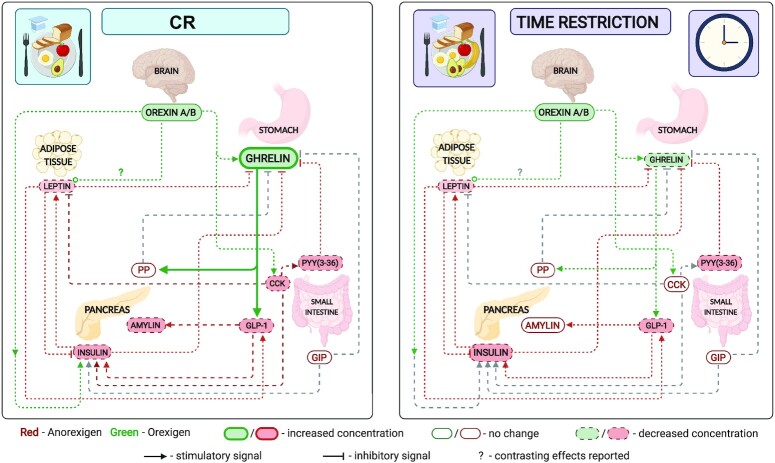
Effect of CR and TRF on circulating satiety hormones. Left: CR; right: time restriction. An overview of the relation of circulating satiety hormones and a comparison of the change in fasting satiety hormones in response to CR or TRF. Several satiety hormones decrease in both CR and TRF (leptin, insulin, and PYY); however, the orexigenic hormones ghrelin and orexin differ. Although orexin decreases in CR, there is also an increase in circulating ghrelin, suggesting either an increase or no change in hunger and a decrease in satiety during the fasting state. Ghrelin decreases and orexin remains unchanged in TRF, suggesting a decrease in both hunger and satiety signals in the fasting state. Created with Biorender.com. CCK, cholecystokinin; CR, calorie restriction; GIP, glucose-dependent insulinotropic polypeptide; GLP-1, glucagon-like peptide-1; PP, pancreatic polypeptide; PYY, peptide YY; TRF, time-restricted feeding.
TABLE 1
Summary of circulating satiety signals in response to CR protocols included in this review1
| Hormone (and form) | Study | Study type | Duration of intervention | Study participants | Calorie restriction amount | Weight loss? | Change due to CR (fasting) | Change due to CR (postprandial) | Interpretive comments |
|---|---|---|---|---|---|---|---|---|---|
| Leptin | Krishnan et al. (54) | RCT, controlled feeding | 12 wk | 71 M&W; BMI range: 28–37 kg/m2; age: 32.5 ± 9.5 y | 500-kcal/d deficit | ↓6.1 ± 0.4 kg | ↓8.3 ng/mL | NA | |
| Trepanowski et al. (53) | RCT, semicontrolled feeding | 24 wk | 23 W, 6 M; BMI: 35 ± 1 kg/m2; age: 44 ± 2 y | 25% energy restriction | ↓7.7% ± 1.0% | ↓23.00 ng/mL | NA | ||
| Wadden et al. (47) | RCT, semicontrolled feeding | 40 wk total: 20 wk wt loss + 20 wk wt maintenance | 49 W; BMI: 36.4 ± 4.5 kg/m2; age: 45 ± 9.6 y | 1–20 wk: 1000–1200 kcal/d (LCD) vs. 1200 kcal/d (control); 21–40 wk: 1200–1800 kcal/d (both groups) | 20 wk: −12.7 ± 6.1 kg (LCD) vs. −9.0 ± 7.3 kg (control); 40 wk: −12.8 ± 9.1 kg (LCD) vs. −12.0 ± 10.6 kg (control) | 20 wk: −25.6 ± 15.9 kg (LCD) vs. −17.1 ± 11.8 kg (control); 40 wk: −19.4 ± 16.3 kg (LCD) vs. −14.8 ± 12.8 kg (control) | NA | Did not analyze if these changes in body weight or leptin differed from baseline values. Change in leptin concentrations did not correlate with weight loss | |
| Näätänen et al. (46) | RCT, semicontrolled feeding | 31 wk total: 7 wk wt loss + 24 wk wt maintenance | 61 W, 21 M; BMI: 34.2 ± 2.5 kg/m2; age: 49.3 ± 9.3 y | 600 kcal/d (VLCD) for wt loss (7 wk); then individualized calorie recommendations + intervention foods (31 wk) | ↓12.0 ± ± 3.5 kg 3.5 kg | ↓60.3% (7 wk); ↓31.7% (31 wk) | NA | ||
| Essah et al. (60) | RCT, parallel-arm intervention | 8 wk | 25 W, 5 M; BMI: 35.5 ± 0.6 kg/m2; age: 42.8 ± 2.0 y | 500-kcal/d deficit | −3.7 ± 0.7 kg/m2 | No significant change* | NA | Did not analyze if body weight change was significant from baseline | |
| Jensen et al. (55) | RCT, parallel-arm intervention | 12 wk | 55 W, 19 M; BMI: 32.6 ± 5.5 kg/m2; age: 13.3 ± 2 y | 20% energy restriction | ↓1.8 kg | ↓10.85 ng/mL | NA | ||
| McNeil et al. (64) | RCT, parallel-arm intervention | 6 mo | 93 W; BMI: 32.1 ± 4.3 kg/m2; age: 58.1 ± 4.8 y | 600- to 800-kcal/d deficit | ↓4.8 ± 4.6 kg | ↓7.4 ± 13.3 ng/mL | NA | ||
| Sumithran et al. (58) | Single-arm, semicontrolled feeding | 62 wk total: 10 wk wt loss + 52 wk wt maintenance | 23 W, 11 M; BMI: 34.7 ± 3.7 kg/m2; age: 56 ± 10.6 y | 500–550 kcal/d (VLCD) for wt loss (10 wk); then individualized calorie recommendations (62 wk) | ↓13.5 ± 0.5 kg (10 wk); ↓7.9 ± 1.1 kg (62 wk) | ↓21.1 ng/mL (10 wk); ↓11.9 ng/mL (62 wk) | NA | Adjusted for fat mass and ratio of leptin:fat mass was lower immediately after wt loss (10 wk) than after wt maintenance (62 wk) | |
| Mars et al. (44) | Single-arm, semicontrolled feeding | 2 d | 34 M; BMI: 22.3 ± 1.6 kg/m2; age: 23 ± 3 y | 62% energy restriction | None | ↓0.8 μg/mL | NA | Authors reported values in μg/mL, although the correct unit is likely to be ng/mL, which would fall within the range of normal concentrations for humans (see Considine et al. (75) DOI: 10.1056/NEJM199602013340503) | |
| Wolfe et al. (45) | Single-arm intervention | 4 wk | 15 W; BMI: 23.3 ± 1.3 kg/m2; age: 22 ± 3 y | 1000–1200 kcal/d | ↓3.4 ± 2.1 kg | ↓7.3 ng/mL | NA | ||
| Dunn et al. (50) | Single-arm intervention, controlled feeding | 10 d | 15 W; BMI: 39 ± 6 kg/m2; age: 39 ± 8 y | 800 kcal/d | −3.0 kg (~2.8% reduction) | ↓9.00 ng/mL | NA | ||
| Chearskul et al. (56) | Single-arm intervention, controlled feeding | 9 wk | 12 M; BMI: 37.2 ± 1.8 kg/m2; age: 33–64 y | 1800 kJ/d (~430kcal/d) | ↓17.4 kg (~15% reduction) | ↓11.9 ng/mL | NA | 8 wk of weight loss with supplements + 1 wk of “light meal" for maintenance | |
| Lecoultre et al. (61) | Single-arm intervention | 6 mo | 24 M&W; BMI: 27.5 ± 0.2 kg/m2; age: 37 ± 2 y | 25% energy restriction vs. 890 kcal/d (LCD) | ↓11.4% ± 0.6% | ↓7.4 ng/mL vs. ↓7.7 ng/mL (LCD) | 24 h leptin mesor: ↓6.5 ng/mL vs. ↓9 ng/mL (LCD) | ||
| Camps et al. (63) | Single-arm intervention, controlled feeding | 8 wk | 59 W, 23 M; BMI: 31.9 ± 3.0 kg/m2; age: 41 ± 8 y | 2.1 MJ/d (~500 kcal/d) | ↓10.7 ± 4.1 kg | ↓13.9 μg/L | NA | ||
| Fogteloo et al. (48) | Single-arm intervention | 3 wk | 23 W, 7 M; BMI: 32 ± 0.83 kg/m2; age: 42 ± 3 y | 500-kcal/d deficit | Not specified during dietary lead-in phase | ↓5.37 ng/mL | NA | ||
| Cummings et al. (59) | Single-arm intervention | 6 mo total: 3 mo wt loss + 3 mo wt maintenance | In dietary wt loss group: 8 W, 5 M; BMI: 35.6 ± 1.6 kg/m2; age: 42.9 ± 2.4 y | 1000 kcal/d for wt loss (3 mo); then individualized calorie recommendations (6 mo) | ↓17.4% ± 1.5% (6 mo) | ↓37.7 ng/mL (6 mo) | NA | ||
| Insulin | Krishnan et al. (54) | RCT, controlled feeding | 12 wk | 71 M&W; BMI range: 28–37 kg/m2; age: 32.5 ± 9.5 y | 500-kcal/d deficit | ↓6.1 ± 0.4 kg | ↓1.48 μIU/mL | No significant change from baseline, or difference from control group* | |
| Trepanowski et al. (53) | RCT, semicontrolled feeding | 24 wk | 23 W, 6 M; BMI: 35 ± 1 kg/m2; age: 44 ± 2 y | 25% energy restriction | ↓7.7% ± 1.0% | ↓4.4 μIU/mL | NA | ||
| Heilbronn et al. (78), Larson-Meyer et al. (83) | RCT, semicontrolled feeding | 6 mo | 13 W, 11 M; BMI: 27.7 ± 1.6 kg/m2; age: 38 ± 6 y | 25% energy restriction (CR) vs. (VLCD) 890 kcal/d until 15% wt loss | ↓10.4% ± 0.9% (CR) vs. ↓13.9% ± 0.7% (LCD) | Approximately ↓2 μIU/mL in both groups* | NA | ||
| Sumithran et al. (58) | RCT, semicontrolled feeding | 62 wk total: 10 wk wt loss + 52 wk wt maintenance | 23 W, 11 M; BMI: 34.7 ± 3.7 kg/m2; age: 56 ± 10.6 y | 500–550 kcal/d (VLCD) for wt loss (10 wk); then individualized calorie recommendations (62 wk) | ↓13.5 ± 0.5 kg (10 wk); ↓7.9 ± 1.1 kg (62 wk) | ↓8.6 mU/L (10 wk); ↓3.9 mU/L (62 wk) | 4-h AUC: ↓21.3 mU/L × 4 h (10 wk); ↓15.8 mU/L × 4 h (62 wk) | ||
| Coutinho et al. (105) | RCT, semicontrolled feeding | 12 wk | 12 W, 2 M; BMI: 35.1 ± 4.2 kg/m2; age: 39.1 ± 9 y | 33% energy restriction | ↓11.8 kg (~12.5% reduction) | ↓Significantly lower than baseline* | ↓Significantly lower than baseline* | ||
| Näätänen et al. (46) | RCT, semicontrolled feeding | 31 wk total: 7 wk wt loss + 24 wk wt maintenance | 61 W, 21 M; BMI: 34.2 ± 2.5 kg/m2; age: 49.3 ± 9.3 y | 600 kcal/d (VLCD) for wt loss (7 wk); then individualized calorie recommendations + intervention foods (31 wk) | ↓12.0 ± ± 3.5 kg 3.5 kg | ↓38.4% (7 wk); ↓32.6% (31 wk) | NA | ||
| Essah et al. (60) | RCT, parallel-arm intervention | 8 wk | 25 W, 5 M; BMI: 35.5 ± 0.6 kg/m2; age: 42.8 ± 2.0 y | 500-kcal/d deficit | −3.7 ± 0.7 kg/m2 | No significant change* | No significant change* | Did not analyze if body weight change was significant from baseline | |
| Jensen et al. (55) | RCT, parallel-arm intervention | 12 wk | 55 W, 19 M; BMI: 32.6 ± 5.5 kg/m2; age: 13.3 ± 2 y | 20% energy restriction | ↓1.8 kg | ↓2.0 mU/L | NA | ||
| Chearskul et al. (56) | Single-arm, controlled feeding | 9 wk | 12 M; BMI: 37.2 ± 1.8 kg/m2; age: 33–64 y | 1800 kJ/d (~430 kcal/d) | ↓17.4 kg (~15% reduction) | −8.81 mU/L | 4-h AUC: ↓201.3 mmol/L × 4 h | 8 wk of weight loss with supplements + 1 wk of “light meal" for maintenance. Reporting results after week 9 vs. baseline | |
| Adam et al. (84) | Single-arm, semicontrolled feeding | 18 wk to tal: 6 wk wt loss + 12 wk wt maintenance | 23 W, 9 M; BMI: 30.0 ± 2.5 kg/m2; age: 44 ± 9 y | 600 kcal/d (VLCD) for wt loss (6 wk); no specific diet instruction (12 wk) | ↓7 kg (0–6 wk); ↓6 kg (0-12 wk) | No change (0–6 wk); 0.1 mU/L (0–12 wk) | 2-h AUC: no significant difference between time points* | ||
| Nymo et al. (82) | Single-arm, semicontrolled feeding | 12 wk total: 8 wk wt loss + 4 wk wt maintenance | 13 W, 18 M; BMI: 36.7 ± 4.5 kg/m2; age: 43 ± 10 y | 550–660 kcal/d (ketogenic VLCD) for wt loss (8 wk); then individualized calorie recommendations (12 wk) | ↓18.3 kg (9 wk); ↓18.4 kg (13 wk) | ↓Significantly lower at 9 wk and 13 wk for all participants* | 2.5-h AUC: ↓Significant decrease at 9 wk and 13 wk in all participants* | ||
| Iepsen et al. (81) | Single-arm, semicontrolled feeding | 60 wk total: 8 wk wt loss + 52 wk wt maintenance | 20 M&W; BMI: 33.5 ± 2.2 kg/m2; age: 43.4 ± 9.6 y | 810 kcal/d (LCD) for wt loss (8 wk); then individualized calorie recommendations (60 wk) | ↓12.5 kg (0–8 wk); ↓10.2 kg (0–60 wk) | ↓26.8 pmol/L (0–8 wk); ↓11.9 pmol/L (0–60 wk) | 180-min iAUC: −6377 pmol/L × 180 min (0–8 wk); −7808 pmol/L × 180 min (0–60 wk) | iAUC not significantly different compared with screening at any time point | |
| Mars et al. (44) | Single-arm, semicontrolled feeding | 2 d | 34 M; BMI: 22.3 ± 1.6 kg/m2; age: 23 ± 3 y | 62% energy restriction | None | ↓1.7 μU/mL | NA | ||
| Cummings et al. (59) | Single-arm intervention | 6 mo total: 3 mo wt loss + 3 mo wt maintenance | In dietary wt loss group: 8 W, 5 M; BMI: 35.6 ± 1.6 kg/m2; age: 42.9 ± 2.4 y | 1000 kcal/d for wt loss (3 mo); then individualized calorie recommendations (6 mo) | ↓17.4 ± 1.5 kg (6 mo) | ↓30.1 mU/L (6 mo) | NA | This study also looked at plasma ghrelin after gastric bypass surgery | |
| Ghrelin (active) | Krishnan et al. (54) | RCT, semicontrolled feeding | 12 wk | 71 M&W; BMI range: 28–37 kg/m2; age: 32.5 ± 9.5 y | 500-kcal/d deficit | ↓6.1 ± 0.4 kg | ↑49 pg/mL | No significant change from baseline, or difference from control group* | |
| Coutinho et al. (105) | RCT, semicontrolled feeding | 12 wk | 12 W, 2 M; BMI: 35.1 ± 4.2 kg/m2; age: 39.1 ± 9 y | 33% energy restriction | ↓11.8 kg (~12.5% reduction) | Slight increase but not significantly different from baseline* | Not significantly different from baseline* | ||
| Sumithran et al. (58) | RCT, semicontrolled feeding | 62 wk total: 10 wk wt loss + 52 wk wt maintenance | 23 W, 11 M; BMI: 34.7 ± 3.7 kg/m2; age: 56 ± 10.6 y | 500–550 kcal/d (VLCD) for wt loss (10 wk); then individualized calorie recommendations (62 wk) | ↓13.5 ± 0.5 kg (10 wk); ↓7.9 ± 1.1 kg (62 wk) | ↑57.1 pg/mL (10 wk); ↑25.9 pg/mL (62 wk) | 4-h AUC: ↑47.1 pg/mL × 4 h (10 wk); ↑18.7 pg/mL × 4 h (62 wk) | ||
| Jensen et al. (55) | RCT, parallel-arm intervention | 12 wk | 55 W, 19 M; BMI: 32.6 ± 5.5 kg/m2; age: 13.3 ± 2 y | 20% energy restriction | ↓1.8 kg | +4.65 pg/mL | NA | ||
| Dunn et al. (50) | RCT, parallel-arm intervention | 10 d | 15 W; BMI: 39 ± 6 kg/m2; age: 39 ± 8 y | 800 kcal/d | −3.0 kg (~2.8% reduction) | −15.00 pg/mL | NA | Not significantly different from baseline | |
| Nymo et al. (82) | Single-arm, semicontrolled feeding | 12 wk total: 8 wk wt loss + 4 wk wt maintenance | 13 W, 18 M; BMI: 36.7 ± 4.5 kg/m2; age: 43 ± 10 y | 550–660 kcal/d (ketogenic VLCD) for wt loss (8 wk); then individualized calorie recommendations (12 wk) | ↓18.3 kg (9 wk); ↓18.4 kg (13 wk) | ↑Significantly higher at 13 wk for all participants* | 2.5-h AUC: ↑Significantly higher at 13 wk for all participants* | ||
| Total ghrelin | Näätänen et al. (46) | RCT, semicontrolled feeding | 31 wk total: 7 wk wt loss + 24 wk wt maintenance | 61 W, 21 M; BMI: 34.2 ± 2.5 kg/m2; age: 49.3 ± 9.3 y | 600 kcal/d (VLCD) for wt loss (7 wk); then individualized calorie recommendations + intervention foods (31 wk) | ↓12.0 ± ± 3.5 kg 3.5 kg | ↑17.4% (7 wk); ↑8.5% (31 wk) | NA | |
| Iepsen et al. (81) | Single-arm, semicontrolled feeding intervention | 60 wk total: 8 wk wt loss + 52 wk wt maintenance | 20 M&W; BMI: 33.5 ± 2.2 kg/m2; age: 43.4 ± 9.6 y | 810 kcal/d (LCD) for wt loss (8 wk); then individualized calorie recommendations (62 wk) | ↓12.5 kg (0–8 wk); ↓10.2 kg (0–60 wk) | ↑228.4 pg/mL (0–8 wk); ↑157.8 pg/mL (0–60 wk) | 180-min dAUC: ↑10,708 pg/mL × 180 min (0–8 wk); ↑10,395 pg/mL × 180 min (0–60 wk) | iAUC after wt loss period not significantly different from screening values | |
| Cummings et al. (59) | Single-arm intervention | 6 mo total: 3 mo wt loss + 3 mo wt maintenance | In dietary wt loss group: 8 W, 5 M; BMI: 35.6 ± 1.6 kg/m2; age: 42.9 ± 2.4 y | 1000 kcal/d for wt loss (3 mo); then individualized calorie recommendations (6 mo) | ↓17.4% ± 1.5% (6 mo) | ↑Significantly higher than preintervention values* | 24-h AUC: ↑2220 pg/mL × 24 h (24% increase) (6 mo) | ||
| GLP-1 | Krishnan et al. (54) | RCT, controlled feeding | 12 wk | 71 M&W; BMI range: 28–37 kg/m2; age: 32.5 ± 9.5 y | 500-kcal/d deficit | ↓6.1 ± 0.4 kg | +0.27 pM | No significant change from baseline, or difference from control group* | |
| Sumithran et al. (58) | RCT, semicontrolled feeding | 62 wk total: 10 wk wt loss + 52 wk wt maintenance | 23 W, 11 M; BMI: 34.7 ± 3.7 kg/m2; age: 56 ± 10.6 y | 500–550 kcal/d (VLCD) for wt loss (10 wk); then individualized calorie recommendations (62 wk) | ↓13.5 ± 0.5 kg (10 wk); ↓7.9 ± 1.1 kg (62 wk) | ↓6.0 pg/mL (10 wk); ↓3.3 pg/mL (62 wk) | 4-h AUC: −0.4 pg/mL × 4 h (10 wk); −3.8 pg/mL × 4 h (62 wk) | ||
| Coutinho et al. (105) | RCT, semicontrolled feeding | 12 wk | 12 W, 2 M; BMI: 35.1 ± 4.2 kg/m2; age: 39.1 ± 9 y | 33% energy restriction | ↓11.8 kg (~12.5% reduction) | ↓Significantly lower than baseline* | Not significantly different from baseline* | ||
| Jensen et al. (55) | RCT, parallel-arm intervention | 12 wk | 55 W, 19 M; BMI: 32.6 ± 5.5 kg/m2; age: 13.3 ± 2 y | 20% energy restriction | ↓1.8 kg | −12.9 pg/mL | NA | ||
| Nymo et al. (82) | Single-arm, semicontrolled feeding | 12 wk total: 8 wk wt loss + 4 wk wt maintenance | 13 W, 18 M; BMI: 36.7 ± 4.5 kg/m2; age: 43 ± 10 y | 550–660 kcal/d (ketogenic VLCD) for wt loss (8 wk); then individualized calorie recommendations (12 wk) | ↓18.3 kg (9 wk); ↓18.4 kg (13 wk) | Significantly lower at 9 wk in men only* | 2.5-h AUC | ||
| Adam et al. (84) | Single-arm, semicontrolled feeding | 18 wk total: 6 wk wt loss + 12 wk wt maintenance | 23 W, 9 M; BMI: 30.0 ± 2.5 kg/m2; age: 44 ± 9 y | 600 kcal/d (VLCD) for wt loss (6 wk); no specific diet instruction (12 wk) | ↓7 kg (0–6 wk); ↓6 kg (0–12 wk) | −2.1 pmol/L (0–6 wk); −0.6 pmol/L (0–12 wk) | 2-h AUC: −6.0 pmol/L × 2 h (0–6 wk); −1.7 pmol/L × 2 h (0–12 wk) | 6- and 12-wk fasting and AUC values not significantly different from screening | |
| Iepsen et al. (81) | Single-arm, semicontrolled feeding | 60 wk total: 8 wk wt loss + 52 wk wt maintenance | 20 M&W; BMI: 33.5 ± 2.2 kg/m2; age: 43.4 ± 9.6 y | 810 kcal/d (LCD) for wt loss (8 wk); then individualized calorie recommendations (62 wk) | ↓12.5 kg (0–8 wk); ↓10.2 kg (0–60 wk) | +0.6 pmol/L (0–8 wk); −0.1 pmol/L (0–60 wk) | 180-min iAUC: ↑488 pmol/L × 180 min (0–8 wk); ↑803 pmol/L × 180 min (0–60 wk)4 | Fasting concentration not significantly different from screening values | |
| Amylin | Krishnan et al. (54) | RCT, controlled feeding | 12 wk | 71 M&W; BMI range: 28–37 kg/m2; age: 32.5 ± 9.5 y | 500-kcal/d deficit | ↓6.1 ± 0.4 kg | −0.77 pM | No significant change from baseline, or difference from control group* | |
| Sumithran et al. (58) | RCT, semicontrolled feeding | 62 wk total: 10 wk wt loss + 52 wk wt maintenance | 23 W, 11 M; BMI: 34.7 ± 3.7 kg/m2; age: 56 ± 10.6 y | 500–550 kcal/d (VLCD) for wt loss (10 wk); then individualized calorie recommendations (62 wk) | ↓13.5 ± 0.5 kg (10 wk); ↓7.9 ± 1.1 kg (62 wk) | ↓40.9 pg/mL (10 wk); ↓30.2 pg/mL (62 wk) | 4-h AUC: −55.3 pg/mL × 4 h (10 wk); −36.7 pg/mL × 4 h (62 wk) | ||
| Jensen et al. (55) | RCT, parallel-arm intervention | 12 wk | 55 W, 19 M; BMI: 32.6 ± 5.5 kg/m2; age: 13.3 ± 2 y | 20% energy restriction | ↓1.8 kg | −8 pg/mL | NA | ||
| GIP | Krishnan et al. (54) | RCT, controlled feeding | 12 wk | 71 M&W; BMI range: 28–37 kg/m2; age: 32.5 ± 9.5 y | 500-kcal/d deficit | ↓6.1 ± 0.4 kg | −5 pg/mL | No significant change from baseline, or difference from control group* | |
| Sumithran et al. (58) | RCT, semicontrolled feeding study | 62 wk total: 10 wk wt loss + 52 wk wt maintenance | 23 W, 11 M; BMI: 34.7 ± 3.7 kg/m2; age: 56 ± 10.6 y | 500–550 kcal/d (VLCD) for wt loss (10 wk); then individualized calorie recommendations (62 wk) | ↓13.5 ± 0.5 kg (10 wk); ↓7.9 ± 1.1 kg (62 wk) | ↓4.0 pg/mL (10 wk); +4.1 pg/mL (62 wk) | 4-h AUC: ↑23.2 pg/mL × 4 h (10 wk); ↑24.5 pg/mL × 4 h (62 wk) | ||
| Jensen et al. (55) | RCT, parallel-arm intervention | 12 wk | 55 W, 19 M; BMI: 32.6 ± 5.5 kg/m2; age: 13.3 ± 2 y | 20% energy restriction | ↓1.8 kg | −5.55 pg/mL | NA | ||
| Iepsen et al. (81) | Single-arm, semicontrolled feeding | 60 wk total: 8 wk wt loss + 52 wk wt maintenance | 20 M&W; BMI: 33.5 ± 2.2 kg/m2; age: 43.4 ± 9.6 y | 810 kcal/d (LCD) for wt loss (8 wk); then individualized calorie recommendations (62 wk) | ↓12.5 kg (0–8 wk); ↓10.2 kg (0–60 wk) | +3.3 pmol/L (0–8 wk); +3.7 pmol/L (0–60 wk) | 180-min iAUC: ↑3096 pmol/L × 180 min (0–8 wk); +21 pmol/L × 180 min (0–60 wk) | iAUC not significantly different after weight maintenance period | |
| PP | Sumithran et al. (58) | RCT, semicontrolled feeding | 62 wk total: 10 wk wt loss + 52 wk wt maintenance | 23 W, 11 M; BMI: 34.7 ± 3.7 kg/m2; age: 56 ± 10.6 y | 500–550 kcal/d (VLCD) for wt loss (10 wk); then individualized calorie recommendations (62 wk) | ↓13.5 ± 0.5 kg (10 wk); ↓7.9 ± 1.1 kg (62 wk) | +2.6 pg/mL (10 wk); −3.4 pg/mL (62 wk) | 4-h AUC: +40.5 pg/mL × 4 h (10 wk); ↑44.7 pg/mL × 4 h (62 wk) | |
| Jensen et al. (55) | RCT, parallel-arm intervention | 12 wk | 55 W, 19 M; BMI: 32.6 ± 5.5 kg/m2; age: 13.3 ± 2 y | 20% energy restriction | ↓1.8 kg | −10.65 pg/mL | NA | ||
| PYY3-36 | Krishnan et al. (54) | RCT, controlled feeding | 12 wk | 71 M&W; BMI range: 28–37 kg/m2; age: 32.5 ± 9.5 y | 500-kcal/d deficit | ↓6.1 ± 0.4 kg | −3.3 pg/mL (PYY3-36) | No significant change from baseline, or difference from control group* | |
| Iepsen et al. (81) | Single-arm, semicontrolled feeding | 60 wk total: 8 wk wt loss + 52 wk wt maintenance | 20 M&W; BMI: 33.5 ± 2.2 kg/m2; age: 43.4 ± 9.6 y | 810 kcal/d (LCD) for wt loss (8 wk); then individualized calorie recommendations (62 wk) | ↓12.5 kg (0–8 wk); ↓10.2 kg (0–60 wk) | ↓10.1 pg/mL (0–8 wk); +6.2 pg/mL (0–60 wk) | 180-min iAUC: ↑2470 pg/mL × 180 min (0–8 wk); ↑1188 pg/mL × 180 min (0–60 wk) | ||
| PYY (total) | Sumithran et al. (58) | RCT, semicontrolled feeding | 62 wk total: 10 wk wt loss + 52 wk wt maintenance | 23 W, 11 M; BMI: 34.7 ± 3.7 kg/m2; age: 56 ± 10.6 y | 500–550 kcal/d (VLCD) for wt loss (10 wk); then individualized calorie recommendations (62 wk) | ↓13.5 ± 0.5 kg (10 wk); ↓7.9 ± 1.1 kg (62 wk) | ↓17.7 pg/mL (10 wk); ↓17.2 pg/mL (62 wk) | 4-h AUC: ↓9.2 pg/mL × 4 h (10 wk); ↓15.0 pg/mL × 4 h (62 wk) | |
| Coutinho et al. (105) | RCT, semicontrolled feeding | 12 wk | 12 W, 2 M; BMI: 35.1 ± 4.2 kg/m2; age: 39.1 ± 9 y | 33% energy restriction | ↓11.8 kg (~12.5% reduction) | Not significantly different from baseline* | Not significantly different from baseline* | ||
| Näätänen et al. (46) | RCT, semicontrolled feeding | 31 wk total: 7 wk wt loss + 24 wk wt maintenance | 61 W, 21 M; BMI: 34.2 ± 2.5 kg/m2; age: 49.3 ± 9.3 y | 600 kcal/d (VLCD) for wt loss (7 wk); then individualized calorie recommendations + intervention foods (31 wk) | ↓12.0 ± ±  3.5 kg 3.5 kg | ↓6.7% (7 wk); not significantly different than baseline at 31 wk* | NA | ||
| Essah et al. (60) | RCT, parallel-arm intervention | 8 wk | 25 W, 5 M; BMI: 35.5 ± 0.6 kg/m2; age: 42.8 ± 2.0 y | 500-kcal/d deficit | −3.7 ± 0.7 kg/m2 | ↓9.4 pg/mL | AUC: ↓1.7 × 103 pg/mL × h | Did not analyze if body weight change from baseline was significant | |
| Jensen et al. (55) | RCT, parallel-arm intervention | 12 wk | 55 W, 19 M; BMI: 32.6 ± 5.5 kg/m2; age: 13.3 ± 2 y | 20% energy restriction | ↓1.8 kg | +2.75 pg/mL | NA | ||
| McNeil et al. (64) | Randomized trial, parallel-arm intervention | 6 mo | 93 W; BMI: 32.1 ± 4.3 kg/m2; age: 58.1 ± 4.8 y | 600- to 800-kcal/d deficit | ↓4.8 ± 4.6 kg | +4.7 ± 31.5 pg/mL | NA | Only presenting changes in CR group | |
| Nymo et al. (82) | Single-arm, semicontrolled feeding | 12 wk total: 8 wk wt loss + 4 wk wt maintenance | 13 W, 18 M; BMI: 36.7 ± 4.5 kg/m2; age: 43 ± 10 y | 550–660 kcal/d (ketogenic VLCD) for wt loss (8 wk); then individualized calorie recommendations (12 wk) | ↓18.3 kg (9 wk); −18.4 kg (13 wk) | No significant change* | 2.5-h AUC: significant increase at 9 wk in women only* | ||
| CCK-8 | Sumithran et al. (58) | RCT, semicontrolled feeding | 62 wk total: 10 wk wt loss + 52 wk wt maintenance | 23 W, 11 M; BMI: 34.7 ± 3.7 kg/m2; age: 56 ± 10.6 y | 500–550 kcal/d (VLCD) for wt loss (10 wk); then individualized calorie recommendations (62 wk) | ↓13.5 ± 0.5 kg (10 wk); ↓7.9 ± 1.1 kg (62 wk) | ↓0.5 fmol/mL (10 wk); −0.1 fmol/mL (62 wk) | 4-h AUC: ↓0.5 fmol/mL × 4 h (10 wk); −0.3 fmol/mL × 4 h (62 wk) | |
| Chearskul et al. (56) | Single-arm, controlled feeding | 9 wk | 12 M; BMI: 37.2 ± 1.8 kg/m2; age: 33–64 y | 1800 kJ/d (~430 kcal/d) | ↓17.4 kg (~15% reduction) | −0.57 pmol/L | 4-h AUC: Approximately ↓12 pmol/L × 4 h | 8 wk of weight loss with supplements + 1 wk of “light meal" for maintenance | |
| CCK | Krishnan et al. (54) | RCT, controlled feeding | 12 wk | 71 M&W; BMI range: 28–37 kg/m2; age: 32.5 ± 9.5 y | 500-kcal/d deficit | ↓6.1 ± 0.4 kg | +0.13 pg/mL | No significant change from baseline, or difference from control group* | |
| Coutinho et al. (105) | RCT, semicontrolled feeding | 12 wk | 12 W, 2 M; BMI: 35.1 ± 4.2 kg/m2; age: 39.1 ± 9 y | 33% energy restriction | ↓11.8 kg (~12.5% reduction) | Not significantly different from baseline* | ↓Significantly lower than baseline* | ||
| Nymo et al. (82) | Single-arm, semicontrolled feeding | 12 wk total: 8 wk wt loss + 4 wk wt maintenance | 13 W, 18 M; BMI: 36.7 ± 4.5 kg/m2; age: 43 ± 10 y | 550–660 kcal/d (ketogenic VLCD) for wt loss (8 wk); then individualized calorie recommendations (12 wk) | ↓18.3 kg (9 wk); ↓18.4 kg (13 wk) | No significant change* | 2.5-h AUC: ↓Significantly lower at 9 wk for all participants* | ||
| Orexin (orexin-A) | Valenzano et al. (149) | Single-arm intervention | 8 wk | 10 W, 10 M; BMI: 32.19 ± 4.78 kg/m2; age: 48 ± 10 y | 700–900 kcal/d (ketogenic VLCD) | ↓12.6 kg | ↑6.33 pg/mL | NA |
*Values not reported.
TABLE 2
Summary of circulating satiety signals in response to TRF protocols included in this review1
| Hormone (and form) | Study | Study type | Duration of intervention | Study participants | Fasting: feeding window, h:h | Intentional CR? | Weight loss? | Change due to TRF (fasting) | Change due to TRF (postprandial) | Interpretive comments |
|---|---|---|---|---|---|---|---|---|---|---|
| Leptin | Ravussin et al. (65) | RCT, controlled feeding, crossover (3.5–5 wk washout) | 4 d | 4 W, 7 M; BMI: 30.1 ± 2.7 kg/m2; age: 32 ± 7 y | 18 h:6 h vs. 12 h:12 h (control) | No | −0.2 ± 0.1 kg (change relative to control) | ↓4 ± 1 ng/mL (am); no significant change (pm)* | NA | |
| Parr et al. (71) | RCT, controlled feeding, crossover design (10 d washout) | 5 d | 11 M; BMI: 32.2 ± 2.0 kg/m2; age: 38 ± 5 y | 16 h:8 h vs. 9 h:15 h (extended feeding) | No | Not reported | Not reported | 24-h AUC: no significant difference between groups | ||
| Carlson et al. (69) | RCT, controlled feeding, crossover (11 wk washout) | 8 wk | 10 W, 5 M; BMI: 23.4 ± 0.5 kg/m2; age: 45.0 ± 0.7 y | 20 h:4 h (1 meal/d) vs. 3 meals/d | No | ↓1.4 kg | −4.1 ng/mL | NA | No specific eating time window for control period | |
| Sutton et al. (70) | RCT, controlled feeding, crossover design (7 wk washout) | 5 wk | 8 M; BMI: 32.2 ± 4.4 kg/m2; age: 56 ± 9 y | 18 h:6 h vs. 12 h:12 h (control) | No | −0.5 ± 0.3 kg | −0.6 ± 1.0 ng/mL | NA | Participants were diagnosed with prediabetes | |
| Moro et al. (36) | RCT, parallel-arm intervention | 8 wk | 34 M; wt: 84.6 ± 6.2 kg; age: 29.21 ± 3.8 y | 16 h:8 h vs. 11 h:13 h (control) | No | −0.97 ± 1.58 kg | −0.36 ± 0.31 ng/mL | NA | Adjusted for fat mass | |
| Zouhal et al. (66) | Parallel-arm design with control | 30 d + 21 d postintervention | 34 M; BMI: 33.3 ± 1.3 kg/m2; age: 24.2 ± 3.6 y | 15–16 h:9–8 h (Ramadan fasting) | No | ↓3.3 kg (30 d); ↓2.3 kg (21 d post) | ↓0.39 ng/mL (30 d); ↑0.32 ng/mL (21 d post) | NA | ||
| Alzoghaibi et al. (68) | Single-arm intervention | 2 wk | 8 M; BMI: 23.7 ± 3.5 kg/m2; age: 26.6 ± 4.9 y | 15–16 h:9–8 h (Ramadan fasting) | No | −2.8 kg | Not reported | Mesor: −17.9 pg/mL; amplitude: −3.6 pg/mL; acrophase: −2.8 pg/mL | ||
| Al-Rawi et al. (67) | Single-arm intervention | 23–30 d | 17 W, 40 M; BMI: 29.9 ± 5.02 kg/m2; age: 38.4 ± 11.2 y | 15 h:9 h (Ramadan fasting) | No | ↓1.6 kg/m2 | ↓2.4 pg/mL | NA | ||
| Insulin | Sutton et al. (70) | RCT, controlled feeding, crossover design (10 d washout) | 5 wk | 8 M; BMI: 32.2 ± 4.4 kg/m2; age: 56 ± 9 y | 18 h:6 h vs. 12 h:12 h (control) | No | −0.5 ± 0.3 kg | ↓3.4 ± 1.6 mU/L | 3-h OGTT: ↓26 ± 9.0 mU/L (mean); ↓35 ± 13 mU/L (peak) | Participants were diagnosed with prediabetes |
| Carlson et al. (69) | RCT, controlled feeding, crossover (11 wk washout) | 8 wk | 10 W, 5 M; BMI 23.4 ± 0.5 kg/m2; age: 45.0 ± 0.7 y | 20 h:4 h (1 meal/d) vs. 3 meals/d | No | ↓1.4 kg | −0.8 ± 0.7 mU/mL (am) | 2-h OGTT: not significantly different between groups* | Fasting insulin and insulin response to OGTT were not significantly different between groups, although plasma glucose concentrations were significantly higher within the first 80 min | |
| Parr et al. (71) | RCT, controlled feeding, crossover design (10 d washout) | 5 d | 11 M; BMI: 32.2 ± 2.0 kg/m2; age: 38 ± 5 y | 16 h:8 h vs. 9 h:15 h (extended feeding) | No | Not reported | Not reported | 24-h AUC: −114 ± 197 mIU/mL × h ; no significant difference in peak insulin* | ||
| Cienfuegos et al. (93) | RCT, parallel-arm intervention | 8 wk | 53 W, 5 M; BMI: 36.7 ± 1 kg/m2; age: 46.3 ± 2.3 y | 20 h:4 h vs. 18 h:6 h vs. non-TRF controls | No | ↓3.2% ± 0.4% | ↓2.3 ± 1.5 mIU/mL [20:4] vs. ↓1.9 ± 1.1 mIU/mL [18:6] | NA | Fasting insulin and HOMA-IR decreased significantly compared with controls; however, there was no difference between the 4 h and 6 h groups | |
| Che et al. (91) | RCT, parallel-arm intervention | 14 wk: 2 wk baseline + 12 wk intervention | 55 W, 65 M; BMI: 26.25 ± 2.05 kg/m2; age: 48.5 ± 9.44 y | 14 h:10 h vs. no timing restriction (mean eating window: 15.25 ± 1.41 h) | No | ↓2.98 ± 0.43 kg | ↓0.43 ± 0.18 mIU/L | NA | Participants with diagnosed type 2 diabetes mellitus. Insulin sensitivity (HOMA-IR, HOMA-β) significantly improved compared with controls | |
| Lowe et al. (86) | RCT, parallel-arm intervention | 12 wk | 46 W; 70 M; BMI: 32.7 ± 4.2 kg/m2; age: 46.5 ± 10.5 y | 16 h:8 h vs. 3 structured meals per day + snacks | No | −0.94 kg | −0.50 mU/L | NA | ||
| Moro et al. (36) | RCT, parallel-arm intervention | 8 wk | 34 M; wt: 84.6 ± 6.2 kg; age: 29.21 ± 3.8 y | 16 h:8 h vs. 11 h:13 h (control) | No | −0.97 ± 1.58 kg | −1.01 mU/mL | NA | ||
| Hutchison et al. (87) | Randomized crossover intervention (2 wk washout) | 7 d | 15 M; BMI: 33.9 ± 0.8 kg/m2; age: 55 ± 3 y | 15 h:9 h (morning TRF vs. evening TRF) | No | −0.8 ± 0.3 kg | No significant change* | No significant change* | Body weight was significantly lower after 7 d, but no difference between groups. Participants were diagnosed with type 2 diabetes | |
| Gabel et al. (14) | Single-arm intervention, compared with historical controls from previous studies | 12 wk | 41 F, 5 M; BMI: 34.5 ± 1 kg/m2; age: 49 ± 2 y | 16 h:8 h vs. non-TRF controls | No | ↓2.6% ± 0.5% | −2.6 μIU/mL (TRF) vs. ±1.1 μIU/mL (CR) | NA | ||
| Alsubheen et al. (89) | Parallel-arm design with control | 30 d | 17 M; BMI: 27.0 ± 4.8 kg/m2; age: 33.6 ± 8.6 y | 18 h:6 h (TRF) vs. unreported for control group | No | ↓2.1 kg vs. +0.4 kg (control) | −20 ± 62 pmol/L (TRF), not reported for control group | NA | ||
| Wilkinson et al. (88) | Single-arm intervention | 14 wk | 6 W, 13 M; BMI: 33.06 ± 4.76 kg/m2; age: 59 ± 11.14 y | 14 h:10 h | No | ↓3.30 ± 3.20 kg | −3.63 ± 8.01 mIU/mL | NA | Participants with diagnosed metabolic syndrome. Fasting insulin was reduced by ~21% and HOMA-IR was reduced by 30%, but both were not statistically significant | |
| Li et al. (92) | Single-arm intervention | 5 wk | 15 W; BMI: 29.75 ± 4.31 kg/m2; age: 18–31 y | 16 h:8 h | No | ↓1.3 kg | ↓3.3 mU/mL | 120-min OGTT AUC: ↓4280 mU/L × min | Participants with diagnosed polycystic ovarian syndrome. Significant decrease in HOMA-IR was also reported | |
| Aksungar et al. (90) | Single-arm intervention | 2 y total: 12 mo CR + 1 mo TRF (Ramadan fasting) +11 mo CR | 23 W; BMI: 34.15 ± 2.15 kg/m2; age: 36 ± 3.12 y | 15 h:9 h only during TRF period | Yes, during CR periods only: mean caloric intake was 1518 ± 212 kcal/d | TRF: −473 ± 146 g; CR: ↓1250 ± 372 g | TRF: +0.15 mU/mL | NA | Insulin decreased during CR periods (primarily in the first 12 mo), but no significant change during TRF period | |
| Ghrelin (active) | Ravussin et al. (65) | RCT, controlled feeding, crossover (3.5–5 wk washout) | 4 d | 4 W, 7 M; BMI: 30.1 ± 2.7 kg/m2; age: 32 ± 7 y | 18 h:6 h vs. 12 h:12 h (control) | No | −0.2 ± 0.1 kg (change relative to control) | ↓43 ± 15 pg/mL (am); ↓22 ± 12 pg/mL (pm) | NA | |
| Sutton et al. (70) | RCT, controlled feeding, crossover design (7 wk washout) | 5 wk | 8 M; BMI: 32.2 ± 4.4 kg/m2; age: 56 ± 9 y | 18 h:6 h vs. 12 h:12 h (control) | No | −0.5 ± 0.3 kg | −5.7 ± 6.6 pg/mL | NA | Participants were diagnosed with prediabetes | |
| Zouhal et al. (66) | Parallel-arm with control intervention | 30 d | 34 M; BMI: 33.3 ± 1.3 kg/m2; age: 24.2 ± 3.6 y | 15–16:9–8 h (Ramadan fasting) | No | ↓3.3 kg (30 d); ↓2.3 kg (21 d post) | −28.33 pg/mL (30 d); +16.67 pg/mL (21 d post) | NA | ||
| Abedelmalek et al. (107) | Single-arm intervention | 30 d | 11 M; BMI: 24.1 ± 0.8 kg/m2; age: 22.11 ± 0.2 y | 15 h:9 h (Ramadan fasting) | No | −4.2 kg | ↑Significantly higher after TRF than at baseline* | NA | Participants were soccer players | |
| Ghrelin (total) | Alzoghaibi et al. (68) | Single-arm intervention | 2 wk | 8 M; BMI: 23.7 ± 3.5 kg/m2; age: 26.6 ± 4.9 y | 15–16:9–8 h (Ramadan fasting) | No | −2.8 kg | Not reported | Mesor: +1.0 pg/mL; amplitude: +0.1 pg/mL, acrophase: +1.9 pg/mL | No significant change from baseline in circadian rhythm of ghrelin |
| Ghrelin (unspecified) | Carlson et al. (69) | RCT, crossover (11 wk washout) intervention | 8 wk | 10 W, 5 M; BMI: 23.4 ± 0.5 kg/m2; age: 45.0 ± 0.7 y | 20 h:4 h (1 meal/d) vs. 3 meals/d | No | ↓1.4 kg | −4.1 ng/mL | NA | |
| Hutchison et al. (87) | Randomized crossover intervention (2 wk washout) | 7 d | 15 M; BMI: 33.9 ± 0.8 kg/m2; age: 55 ± 3 y | 15 h:9 h (morning TRF vs. evening TRF) | No | ↓0.8 ± 0.3 kg | Lower with early am TRF than pm TRF* | Lower with pm TRF than am TRF | Participants were diagnosed with type 2 diabetes. Body weight was significantly lower after 7 d, but there was no difference between groups | |
| Al-Rawi et al. (67) | Single-arm intervention | 23–30 d | 17 W, 40 M; BMI: 29.9 ± 5.02 kg/m2; age: 38.4 ± 11.2 y | 15 h:9 h (Ramadan fasting) | No | ↓1.6 kg/m2 | ↓106 pg/mL | NA | ||
| GLP-1 | Ravussin et al. (65) | RCT, controlled feeding, crossover (3.5–5 wk washout) | 4 d | 4 W, 7 M; BMI: 30.1 ± 2.7 kg/m2; age: 32 ± 7 y | 18 h:6 h vs. 12 h:12 h (control) | No | −0.2 ± 0.1 kg (change relative to control) | ↓0.8 ± 0.3 pmol/mL (am); no significant change in pm* | NA | |
| Sutton et al. (70) | RCT, controlled feeding, crossover design (7 wk washout) | 5 wk | 8 M; BMI: 32.2 ± 4.4 kg/m2; age: 56 ± 9 y | 18 h:6 h vs. 12 h:12 h (control) | No | −0.5 ± 0.3 kg | −1.2 ± 1.0 pmol/mL | NA | Participants were diagnosed with prediabetes | |
| Parr et al. (71) | RCT, controlled feeding, crossover design (10 d washout) | 5 d | 11 M; BMI: 32.2 ± 2.0 kg/m2; age: 38 ± 5 y | 16 h:8 h vs. 9 h:15 h (extended feeding) | No | Not reported | Not reported | 24-h AUC: no significant difference between groups* | ||
| Hutchison et al. (87) | Randomized crossover intervention (2 wk washout) | 7 d | 15 M; BMI: 33.9 ± 0.8 kg/m2; age: 55 ± 3 y | 15 h:9 h (morning TRF vs. evening TRF) | No | ↓0.8 ± 0.3 kg | ↓Significantly lower than preintervention* | No significant change* | Participants were diagnosed with type 2 diabetes. Body weight was significantly lower after 7 d, but there was no difference between groups | |
| Zouhal et al. (66) | Parallel-arm design with control | 30 d | 34 M; BMI: 33.3 ± 1.3 kg/m2; age: 24.2 ± 3.6 y | 15–16 h:9–8 h (Ramadan fasting) | No | ↓3.3 kg (30 d); ↓2.3 kg (21 d post) | ↓0.03 ng/dL (30 d); −0.02 ng/dL (21 d post) | NA | ||
| Amylin | Hutchison et al. (87) | Randomized crossover intervention (2 wk washout) | 7 d | 15 M; BMI: 33.9 ± 0.8 kg/m2; age: 55 ± 3 y | 15 h:9 h (morning TRF vs. evening TRF) | No | −0.8 ± 0.3 kg | No significant change* | No significant change* | Participants were diagnosed with type 2 diabetes. Body weight was significantly lower after 7 d, but there was no difference between groups |
| GIP | Parr et al. (71) | RCT, controlled feeding, crossover design (10 d washout) | 5 d | 11 M; BMI: 32.2 ± 2.0 kg/m2; age: 38 ± 5 y | 16 h:8 h vs. 9 h:15 h (extended feeding) | No | Not reported | Not reported | 24-h AUC: no significant difference between groups* | |
| Hutchison et al. (87) | Randomized crossover intervention (2 wk washout) | 7 d | 15 M; BMI: 33.9 ± 0.8 kg/m2; age: 55 ± 3 y | 15 h:9 h (morning TRF vs. evening TRF) | No | ↓0.8 ± 0.3 kg | No significant change* | No significant change* | Participants were diagnosed with type 2 diabetes. Body weight was significantly lower after 7 d, but there was no difference between groups | |
| PYY3-36 | Ravussin et al. (65) | RCT, controlled feeding, crossover (3.5–5 wk washout) | 4 d | 4 W, 7 M; BMI: 30.1 ± 2.7 kg/m2; age: 32 ± 7 y | 18 h:6 h vs. 12 h:12 h (control) | No | −0.2 ± 0.1 kg (change relative to control) | No significant change in am*; ↑17 ± 6 pg/mL (pm) | NA | |
| PYY (total) | Zouhal et al. (66) | Parallel-arm design with control | 30 d | 34 M; BMI: 33.3 ± 1.3 kg/m2; age: 24.2 ± 3.6 y | 15–16 h:9–8 h (Ramadan fasting) | No | ↓3.3 kg (30 d); ↓2.3 kg (21 d post) | ↓0.04 μg/mL (30 d); no difference from baseline to 21 d post | NA | |
| Sutton et al. (70) | RCT, controlled feeding, crossover design (7 wk washout) | 5 wk | 8 M; BMI: 32.2 ± 4.4 kg/m2; age: 56 ± 9 y | 18 h:6 h vs. 12 h:12 h (control) | No | −0.5 ± 0.3 kg | ↓23 ± 7.0 pg/mL | NA | Participants were diagnosed with prediabetes | |
| Parr et al. (71) | RCT, controlled feeding, crossover design (10 d washout) | 5 d | 11 M; BMI: 32.2 ± 2.0 kg/m2; age: 38 ± 5 y | 16 h:8 h vs. 9 h:15 h (extended feeding) | No | Not reported | Not reported | 24-h AUC: no significant difference between groups* | ||
| PYY (unspecified) | Hutchison et al. (87) | Randomized crossover intervention (2 wk washout) | 7 d | 15 M; BMI: 33.9 ± 0.8 kg/m2; age: 55 ± 3 y | 15 h:9 h (morning TRF vs. evening TRF) | No | −0.8 ± 0.3 kg | No significant change* | No significant change* | Participants were diagnosed with type 2 diabetes. Body weight was significantly lower after 7 d, but there was no difference between groups |
| CCK | Zouhal et al. (66) | Parallel-arm design with control | 30 d | 34 M; BMI: 33.3 ± 1.3 kg/m2; age: 24.2 ± 3.6 y | 15–16 h:9–8 h (Ramadan fasting) | No | ↓3.3 kg (30 d); ↓2.3 kg (21 d post) | ↓0.05 ng/dL (30 d); +0.01 ng/dL (21 d post) | NA | |
| Orexin | Almeneessier et al. (151) | Single-arm intervention | 30 d | 8 M; BMI: 24.4 ± 3.8 kg/m2; age: 25.4 ± 3.5 y | 15 h:9 h (Ramadan fasting) | No | −1.6 kg | ↑0.8 ng/mL | +0.8 ng/mL (mid-day), not significantly different at other time points throughout the day | Significant changes observed between baseline and the first week of Ramadan fasting. Pattern of orexin concentrations was flipped between baseline and fasting periods |
*Values not reported.
Long-term regulators
Leptin
Leptin, a 146-amino-acid peptide hormone, is released from white adipose tissue, mammary epithelial cells, and bone marrow (39), and readily crosses the blood–brain barrier (40). Secretion and production of leptin are dependent on triglyceride stores (41), making it a unique hormone that can influence food intake through both acute and long-term signals of energy status (42). Originally, leptin was thought to induce satiety, decrease food intake, and increase energy expenditure and weight loss (39), and recent evidence suggests that sensitization/desensitization and resistance to leptin affect how leptin functions (43). Fasting leads to decreases in both stored and circulating triglyceride levels, thus decreasing the magnitude of leptin secretion.
CR and weight loss are known influencers of leptin. CR results in a reduction in leptin (44–46), independent of weight loss (47, 48), and disrupts its chrono-rhythmicity. This reduction in leptin has been associated with reduction in both subjective appetite and compensatory food intake; however, there is a lack of clarity about whether decreases in leptin are proportional to the level of caloric compensation (44). CR reduces dopamine receptor availability and increases motivation and sensitivity to reward (49), which have been linked to the reduction in leptin in circulation (50).
Several studies have shown that both chronic (continuous) and intermittent CR, as a set reduction of dietary energy (~500 kcal/d), a percentage of the total required intake (15%–75% of total required energy intake), or very-low-calorie diets (VLCDs) (430–800 kcal/d), for 3–24 wk, reduce serum leptin (45, 51–59) when compared with no CR. However, no significant change in fasting leptin concentrations was reported after 8 wk of a 500-kcal/d deficit CR diet (60), and after 20 wk with an intake of 1000–1200 kcal/d (47). The decrease in leptin was seen both with and without significant weight loss, suggesting that the change in leptin is likely due to the acute negative energy balance. In the CALERIE (Comprehensive Assessment of Long-Term Effects of Reducing Intake of Energy) study, a 6-mo CR with intake 25% below required energy needs, not just fasting but 24-h diurnal leptin was dampened (61). An ~11-kg drop in body weight among individuals who were overweight was associated with a 44% reduction in 24-h mean circulating leptin. With weight loss and CR, there is a resultant metabolic adaptation, in the form of reduced 24-h and sleeping energy expenditure (62). In the CALERIE study, the metabolic adaptation resulted in a ~125-kcal/d reduction on average, and the decrease in leptin was an independent determinant of this metabolic adaptation (61). This association has been shown in other CR intervention trials as well (47, 63) and attributed largely to movement economy (63). However, the change in leptin does not explain the entirety of this metabolic adaptation (64). In summary, fasting leptin is reduced after CR; however, whether this is sustained through diurnal and meal-induced changes remains unknown.
Similarly to CR, in some studies, TRF (6 h, 8 h, or 12 h or Ramadan feeding regimens), without intentional CR or weight loss, has been shown to reduce fasting leptin concentrations (36, 65–69). In contrast, in studies where TRF was practiced without CR, with or without weight loss, leptin concentrations were not affected (70, 71). After CR, when energy intake returns to prerestricted conditions, leptin concentrations also rise to match prerestriction values (46). In free-living conditions, the rise in caloric intake is proposed to be due to the decrease in satiety, partly due to the lesser anorexigenic effect resulting from the reduced leptin in circulation. The evidence suggests that CR, with or without TRF, lowers circulating leptin. Although this would increase caloric intake to compensate acutely (weeks to months), the effect this has on appetite and food intake in the long run (years) remains contested, and a unifying theory of its effects is yet to be established.
Insulin
Insulin is a peptide hormone, comprised of a 21-amino-acid A chain and a 30-amino-acid B chain. It is released from pancreatic β-cells in the islets of Langerhans (72) primarily in response to the absorption of glucose, although other signals (73) and nutrients (74) can influence its secretion, and elicits a corresponding increase in intracellular calcium concentrations (73). Insulin has a central effect on the brain, orchestrating alterations to energy balance, metabolism, appetite, and neural activity (76). Insulin that is released into the systemic circulation, in the postprandial state, crosses the blood–brain barrier (77), binds to insulin receptors located across the brain, elicits an anorexigenic effect, and diminishes orexigenic signals. Owing to insulin's sensitivity to long-term energy balance as well as acute energy fluctuations, it may function as a contributor to both long- and short-term regulation of hunger and satiety signals.
CR to 20%–75% of total required energy intake; ketogenic, very-low-energy diets (430–660 kcal/d); and 500- to 750-kcal restriction of the total daily energy intake required for maintenance for durations of 3 wk–6 mo have been shown to reduce fasting insulin (34, 44, 46, 53–55, 58, 59, 78–81), postprandial/all-day insulin (56, 58, 82), insulin-like signaling, and insulin sensitivity (83). In contrast, very few studies reported no significant change in fasting insulin after 8- to 18-wk interventions in normal-weight or obese adults on caloric deficits ranging from VLCDs (430 kcal/d) to 500- to 600-kcal/d deficits (56, 60, 84). However, other metabolic benefits, such as reduction in circulating cholesterol (LDL, VLDL), triglycerides, and insulin resistance, are concurrent (82), and CR is often recommended in managing and preventing type 2 diabetes (85). Based on the studies reviewed here, a majority of the evidence suggests a reduction in insulin after CR.
TRF, along with CR, has been deemed safe and effective in managing body weight in individuals with type 2 diabetes (80). TREAT (Time-Restricted Eating on Weight Loss Trial) identified that CR, both with and without TRF (16:8), resulted in no change in insulin, suggesting no unique impact from TRF (86). Several TRF regimens lasting from 5 d to 12 wk, studying varying feeding-fasting temporal patterns (14–20 h fasting, 4- to 10-h eating windows), with or without concurrent CR or weight loss, showed no effect of TRF on fasting or postprandial insulin (14, 36, 69, 71, 87–90). In contrast, TRF (5 wk–12 wk) reduced fasting and postprandial insulin in men with prediabetes, without weight loss (70); men and women with type 2 diabetes, accompanied by weight loss (91); women with polycystic ovarian syndrome, accompanied by weight loss (92); and normal healthy individuals, accompanied by weight loss (93). It is important to note here that other IF regimens like ADF or 2-d/wk fasting protocols have shown consistent success in reducing fasting insulin (94), but data from within-day TRF appear less consistent. In summary, there is weak evidence to suggest insulin is reduced after TRF, but often studies that fall under the general umbrella of IF protocols fail to differentiate between ADF, TRF, or other fasting regimens (95).
Acute-phase regulators
Ghrelin
Ghrelin is a 28-amino-acid peptide hormone that is primarily produced and secreted from the X/A cells in the stomach, specifically the gastric fundus region (96). Ghrelin is secreted preprandially and circulating concentrations peak immediately before meal initiation, then fall within 1 h of meal consumption (97). This gives rise to ghrelin's classification as the “hunger hormone," even though it is unclear if it causes or reflects hunger (98). Ghrelin has been shown to stimulate growth hormone release from the anterior pituitary, as well as influence homeostatic controls of food intake and appetite, taste sensations, and reward behaviors (99). Ghrelin stimulates gastric motility and gastric acid secretion in anticipation of food intake (100). A review by Briggs and Andrews (101) suggests the prevailing theory is that ghrelin influences appetite and hunger by stimulating neuropeptide Y/Agouti-related peptide (NPY/AgRP) neurons in the arcuate nucleus of the hypothalamus and the paraventricular nucleus (PVN).
Circulating ghrelin concentrations follow a diurnal pattern in humans and rodents that occurs owing to the suppression of ghrelin by sleep, and which is independent of meals (102). Ghrelin also increases during fasting, whereas refeeding leads to a reduction of plasma concentrations (103, 104). There is inconsistency in the form of ghrelin reported across studies, with some reporting the active (acylated) form and others reporting total ghrelin. Despite this, CR led to significant increases in fasting (46, 54, 58, 59, 82) and postprandial concentrations (58, 59, 81, 82) of plasma ghrelin, with some exceptions (50, 55, 105). In addition, following a VLCD (800 kcal/d) over 8 wk led to higher ghrelin concentrations, which remained higher beyond 1 y of weight maintenance, after the initial loss (81). This sustained elevation has been associated with the continuous “grazing" pattern of food intake (106), which could consequently contribute to increased energy intake and a higher probability of regaining weight in the long term. Overall, it is likely that fasting and postprandial ghrelin concentrations increase following a CR regimen.
The ability of a TRF dietary pattern to modulate ghrelin concentrations remains unclear. Studies have shown no significant differences in fasting ghrelin concentration following an isocaloric TRF regimen (4–8 wk) when compared with controls (66, 68–70), regardless of whether it was accompanied by weight loss. In contrast, some studies have shown significant decreases in fasting ghrelin concentrations with TRF regimens lasting between 4 d and 30 d when compared with baseline measures (65, 67), also regardless of whether the TRF was accompanied by weight loss. One study that reported on soccer players that observed Ramadan fasting noted significantly higher concentrations of ghrelin post-Ramadan than preintervention values, which was accompanied by significant weight loss (107). However, the fact that they are athletes and physically active suggests the involvement of exercise-induced appetitive changes, setting it apart from the other studies discussed in this section. Major concerns while interpreting from the collection of TRF studies are the lack of standardized TRF regimens, duration of the interventions, and lack of postprandial measurements. Case in point, Hutchison et al. (87) tested the differences between early morning TRF (eating window between 08:00 and 17:00) and afternoon TRF (eating window between 12:00 and 21:00) in free-living adults with overweight or obesity. After 7 d on the assigned TRF regimen, fasting ghrelin concentrations were significantly lower in the early morning TRF group, but postprandial ghrelin incremental area under the curve (iAUC) was lower in the afternoon TRF group, suggesting that timing of the eating window can play a role in the diurnal modulation of ghrelin concentrations by TRF (87). In summary, TRF, with or without CR or weight loss, does not increase fasting ghrelin (unlike CR) and may even reduce it. Future research, factoring in the time of day for restriction and conducted for longer durations (>5 wk), is necessary for clarifying the effect of TRF on ghrelin.
GLP-1
GLP-1, an incretin, is a 30-amino-acid peptide hormone (108) secreted from the L cells in the small intestine in response to nutrients in the luminal intestinal space. GLP-1 is known to influence glucose homeostasis, by inducing insulin secretion and reducing glucagon secretion and gastric motility (109). The significant effects of GLP-1 in modulating circulating blood glucose have led to the development and use of pharmaceutical agonists to lower blood glucose and manage body weight (110).
Iepsen et al. (81) reported no change in fasting but an increase in postprandial GLP-1 after following a VLCD (800 kcal/d) for 8 wk, which was sustained at 52 wk. Another VLCD (550–660 kcal/d), conducted by Nymo et al. (82), resulted in an increase in postprandial GLP-1 AUC at <1–3 wk. In contrast, Adam et al. (84) reported a reduction in postprandial GLP-1 after a 6-wk VLCD (~600 kcal/d), which returned to baseline after 3 mo of sustained weight maintenance. A VLCD (10 wk, 500–550 kcal/d) also resulted in a small but significant reduction in GLP-1, not immediately after CR, but at the 62-wk follow-up test (58). A less severe restriction of calories (intake reduced by 500 kcal/d or 20%) did not affect fasting or postprandial GLP-1 concentrations (54, 55). In summary, CR has reduced fasting GLP-1 concentrations, although not consistently. The lack of similarity in these interventions is important to note, with large variability in the sample type, extent of CR, duration of the study, and follow-up testing times. The inconsistencies between studies make it difficult to reach conclusions about the physiological effect of CR on GLP-1.
In the context of TRF, no change in fasting, postprandial, or all-day GLP-1 was reported following a 16:8 TRF regimen after 5 d (71) and after 5 wk (70). On the other hand, a Ramadan-type feeding regimen was evaluated by Zouhal et al. (66) and reported a reduction in fasting GLP-1. This reduction in fasting GLP-1 was also seen after a 18:6 TRF intervention for 4 d (65) and a 15:9 TRF intervention for 7 d (87); however, no differences in postprandial GLP-1 were reported. In summary, TRF appears to reduce fasting GLP-1; however, the evidence for this stems from very short-term studies (spanning days), and longer-term studies are needed to corroborate this possibility.
Amylin
Amylin, or islet/insulinoma amyloid polypeptide (IAPP)/diabetes-associated peptide (DAP), is a 37-amino-acid peptide hormone (111, 112). Amylin is colocalized, copacked, and cosecreted with insulin (molar ratio 1:15, respectively) from the pancreatic β cells within the islets of Langerhans, in response to a stimulus in the form of nutrient intake. Amylin acts by reducing food intake and promotes negative energy balance (113). We have learned from rat model studies that exogenous amylin injected intraperitoneally has been shown to reduce meal size, in a dose-dependent manner (114), and irrespective of whether the amylin is administered peripherally or centrally, its effects appear to be mediated via central mechanisms (115).
Sumithran et al. (58) reported that after 10 wk of CR (500–550 kcal/d) in 50 obese men and women, there was a decrease in fasting and 30-min postprandial amylin. A 500-kcal/d reduction in energy intake for 12 wk did not affect fasting or postprandial amylin, in a group of obese men and women (54). Further, in 74 adolescent participants (10–17 y old), compared with a control group with no dietary restriction, a 20% CR as part of either a low-carbohydrate (35% carbohydrate; 30% protein; 35% fat) or low-fat diet (55% carbohydrate; 30% protein; 25% fat) for 12 wk (55) resulted in no significant differences in fasting amylin. The contrasting findings may relate to the extent and/or duration of CR, and future research is needed to definitively determine the effects of CR on amylin. One study assessed the effects of 15:9 TRF on amylin; no effect on fasting or postprandial amylin was reported (87). Overall, amylin may be reduced after CR in response to a VLCD, but it is unclear if this would be the case if the CR was more moderate. The evidence evaluating the effect of TRF on amylin is insufficient to draw conclusions.
PP
PP is a 36-amino-acid peptide, primarily produced in the F cells of the pancreatic islets of Langerhans, but is also secreted in smaller quantities from the large intestine (116). PP diminishes gastric emptying, motility, and contraction of the gallbladder as well as preventing exocrine secretions from the pancreas through vagal signaling, contributing to satiation from the current meal episode. PP binds to Y4 receptors from the family of G-coupled protein receptors, which are found in the hypothalamus, stomach, pancreas, duodenum, ileum, and colon (116, 117). PP rises with caloric intake with peaks typically being observed 15 min into the postprandial state, yet values have remained high 6 h after an 830-calorie meal (116, 118).
After a VLCD (10 wk, 500–550 kcal/d, adults), mean (fasting and postprandial combined) PP concentration was higher than at baseline after initial weight loss and remained elevated at the 62-wk weight maintenance follow-up period (58). The study did not report significant changes in fasting PP. However, postprandial PP AUC was higher at week 10 and week 62 than at baseline. Contradictory to this, in a study comparing a 20% CR with no CR in adolescents (for 12 wk), there were no changes in PP at fasting, and postprandial time points were not measured (55). So, it appears that severe CR or significant weight loss can induce changes in postprandial PP, whereas fasting values do not change with moderate or severe CR. Future studies need to confirm this observation. To our knowledge, PP has not been evaluated in any TRF study to date. Hence, although CR could increase PP over the long term, further studies need to measure PP in both CR and TRF regimens to better understand their effects.
GIP
GIP is a 42-amino-acid polypeptide functioning as an incretin much like GLP-1. GIP is secreted from/by the K cells of the duodenum and jejunum in response to carbohydrates and lipids in the small intestine (108). GIP activity increases insulin secretion from pancreatic β-cells in hyperglycemic conditions and increases glucagon secretion from α-cells in euglycemic conditions. Additional downstream actions of GIP include upregulation of lipoprotein lipase and increasing lipogenesis (108). GIP and GLP-1 work additively to increase insulin secretion but do not appear to have the additive effect on reducing food intake seen in animal models (119). As insulin concentrations rise after a meal, GIP secretion falls, creating a negative feedback loop (120).
Whereas fasting concentrations of GIP remained unaffected by CR (54, 55, 58, 81), postprandial GIP iAUC was elevated after weight loss (58, 81), but this was not observed in all the studies (54, 55). After a severe CR (800 kcal/d), 1 study found postprandial GIP concentrations increased, only to return to baseline concentrations after 1 y of weight maintenance (81), whereas another study showed GIP increased with CR and remained higher than baseline concentrations after 62 wk of weight maintenance (58). Two studies have looked at the effect of TRF on GIP. One study in obese adults following a 16:8 TRF regimen compared with a 9:15 regimen reported that total GIP AUC was not significantly different between the groups (71). Early morning or afternoon feeding times in TRF did not affect fasting or postprandial concentrations of GIP in a different study (87). In summary, although CR may result in higher postprandial GIP, there was no effect observed at fasting, and in the very short term (5–7 d) TRF does not appear to affect GIP. Longer-duration interventions, with replicated study designs, are needed to draw more accurate conclusions about the effect of both CR and TRF on GIP.
PYY
PYY is a peptide hormone secreted from L cells primarily in the ileum and large intestine in response to food intake, especially protein ingestion, and postprandial concentrations are thought to be proportional to the number of calories ingested (121). PYY circulates as PYY1-36 and PYY3-36 and the latter is thought to be primarily involved in regulating food intake (122). In the current report, owing to a lack of studies that only focused on PYY3-36, we have summarized studies that reported on both PYY and PYY3-36.
Peripheral infusion of PYY3-36 in humans leads to decreased food intake and increased feelings of fullness during a standard meal, although higher infusions lead to increased feelings of nausea, and these higher infusions were considered to be pharmacological (as opposed to physiological) doses (123). A 90-min infusion of PYY3-36, reported to be in the physiological concentration range by Batterham et al. (124), reduced total calorie intake by 33% in humans. Moreover, 12 h after the 90-min infusion, no reported differences in fullness were reported. Taken together this indicates that PYY3-36 plays a bigger role in acute satiety and satiation. In addition, PYY3-36 (along with GLP-1) inhibits gastric acid secretion, gastric emptying, and gastrointestinal motility, known as the “ileal brake" (125).
Weight loss trials utilizing VLCDs (~500–810 kcal/d) demonstrated decreases in fasting PYY in most (46, 58, 81), but not all, studies (82). However, the effects of VLCDs on postprandial PYY are inconsistent, possibly due to the differing study designs and PYY forms that were measured in each study. Essah et al. (60) found a decrease in fasting and postprandial total PYY after 8 wk of a moderate CR (500-kcal deficit/d). In contrast, another study also using a 500-kcal deficit/d CR regimen reported no significant changes in fasting or postprandial PYY3-36 concentrations after a 12-wk controlled-feeding weight-loss trial in obese men and women (54). Similarly, Jensen et al. (55) reported no effect of a 20% CR on fasting PYY3-36 in 74 adolescents. McNeil et al. (64) reported no significant changes in total PYY after 6 mo of a 600- to 800-kcal/d restriction; however, they did report negative associations between fasting PYY concentrations and weight change and fat-free mass change. In summary, extreme CR may likely reduce PYY, but mild to moderate CR has inconsistent effects on PYY.
The effects of TRF on PYY or PYY3-36 are varied. Ravussin et al. (65) observed an increase after a 6-h evening fast in PYY3-36 after a 4-d trial of early morning TRF in obese adults. In contrast, in a 5-d feeding study, a 16:8 TRF regimen (no CR) did not lead to a difference in PYY 21-h AUC in overweight and obese men (n = 11) (71). In agreement with these findings, Hutchison et al. (87) found no change in fasting or 3-h postprandial PYY in men at risk of type 2 diabetes (n = 15) after 7 d following a 15:9 TRF regimen (no forced CR). On the contrary, another study in overweight men with prediabetes (n = 8) following an 18:6 TRF regimen for 5 wk (weight stable and no CR) reported a decrease in fasting PYY (70). Ramadan fasting reduced fasting PYY concentrations in obese men after 30 d (66). These studies suggest that the reduction of fasting PYY in response to TRF may require a >7-d intervention duration. More research is needed to verify this and to explore the long-term effects of TRF on postprandial PYY or PYY3-36 concentrations.
CCK
CCK was one of the first gut-related hormones discovered to have effects on food intake and satiety (126, 127). CCK is synthesized in I cells found throughout the gastrointestinal tract, but primarily concentrated in the duodenum and jejunum (128). The presence of dietary lipids and proteins in the gut triggers CCK secretion from these cells and stimulates the release of bile acids and pancreatic juices into the duodenum, increasing intestinal motility, and decreases gastric emptying rate (129). The preprohormone is a peptide residue containing 115 amino acids and can be cleaved into varying lengths (CCK-5, CCK-33, CCK58, and CCK-83) by different enzymes (130, 131), although CCK-8 is frequently investigated and therefore better understood (132). Using a meal challenge protocol, infusion of exogenous CCK in humans led to a significant decrease in food intake and feelings of satiety immediately after the infusion (133). Hyperphagia and morbid obesity have resulted from loss of function mutations of CCK receptor A in humans (127). Several rodent studies reported that total food intake did not decrease long term, thus showing that CCK infusion failed to have longer-lasting effects on overall food intake and satiety (134); however, recent evidence using a CCK analog targeting the CCK-1 receptor in domestic pigs has reported decreased food intake after 13 wk (135). Thus, whether CCK has long-term effects on food consumption is still under active investigation.
Although most studies report total CCK, some studies report CCK-8. Hence, in the current article we present data on both, which adds to inconsistencies making it challenging to understand the effect of CR or TRF on this hormone. Moderate reduction of daily total caloric intake by 500 kcal showed no significant changes in CCK after 12 wk at the fasting or postprandial state (54). On the other hand, a VLCD (430–660 kcal/d) along with weight loss led to decreases in postprandial CCK/CCK-8 AUC after 8 wk, but there were no changes in fasting CCK/CCK-8 concentrations (56, 58, 82, 105). In summary, VLCDs may reduce postprandial CCK/CCK-8, but moderate or less extreme forms of CR do not seem to affect fasting CCK/CCK-8 significantly.
Regarding TRF, Zouhal et al. (66) determined that fasting CCK concentrations in obese men dropped after 30 d of Ramadan fasting; however, concentrations increased back to baseline concentrations 21 d after the end of Ramadan. Aside from this, no other studies have looked at CCK or CCK-8 under TRF conditions, warranting further study.
Orexin
Orexins or hypocretins are hypothalamic neuropeptides (136). Orexin A (hypocretin 1) is a 33-amino-acid neuropeptide; orexin B (hypocretin 2) is a 28-amino-acid neuropeptide. These are produced by ~70,000 orexin-producing neurons in the dorsolateral hypothalamus (with projections to dorsal raphe nuclei, amygdala, basal forebrain, suprachiasmatic nucleus, locus coeruleus, and the spinal cord) and the perifornical area of the brain (137–139). Orexins act via the activation of G-protein coupled receptors—orexin-1 and -2 receptors (OX1R/OX2R), and both are present in different regions of the brain (136). OX1R has also been detected in testes, kidneys, adrenal glands, and throughout the gastrointestinal tract (stomach, ileum, colon, and colorectal epithelial cells) in humans (140, 141), suggesting they have roles to play in peripheral tissues. Orexin A is more potent than orexin B, and OX1R has a 100-fold higher affinity for orexin A than for orexin B (142). Although orexins are abundant in circulating cerebrospinal fluid, they are also present in the plasma (143) and are capable of rapidly crossing the blood–brain barrier by simple diffusion (137). They are implicated in sleep/arousal, spontaneous physical activity, reward-seeking, drug addiction, and food intake regulation (144). Orexins increase food intake and gastric motility: both intraperitoneal and intranasal administration result in increased food intake for ≤4 h after exposure (144, 145). Orexin precursors become more abundant (elevated mRNA expressions) during the fasted state because they are responsible for the fasting-induced increase in wakefulness that helps in food foraging behaviors (146). A rise in blood glucose inhibits orexin-secreting neurons, and excitatory activity ensues with reductions in glucose (147).
The effects of CR (50% for 6 d, rat model), without a change in feeding time, did not lead to changes in hypothalamic preproorexin mRNA levels (148) but the authors failed to measure protein concentrations in the brain or circulation. A ketogenic VLCD in adults (10 men and 10 women, 700–900 kcal/d) for 8 wk led to an increase in fasting plasma orexin-A concentrations (149). Because orexin stimulates food anticipatory activity (FAA) and leads to food intake, this likely would result in increased feelings of hunger and energy intake.
In regard to TRF, orexin is suspected to play an important role in changes of FAA (increased movement and wakefulness time) when feeding time is restricted in mice (150); however, evidence to support or negate this suspicion is both sparse and weak. In healthy men (n = 8) following a Ramadan fasting regimen, plasma orexin-A increased at the fasting time point, and the diurnal rhythm was flipped (inverted, based on 5 measurements in 24 h) in comparison with the nonfasting group (151). In rats, when food intake was restricted to 2 h/d for 3 wk, the activity of orexin-containing neurons increased in the lateral hypothalamus, which led to a downregulation of the orexin receptor gene in the PVN (152), effectively balancing the secretion of orexin with its activity via the OX2R receptor. More studies looking at the effect of orexin on TRF, for longer durations (>4 wk) as well as maintaining consistent hours of restriction, are necessary. At present the evidence suggesting an effect of TRF on orexin is inconclusive.
Conclusions
CR, either from VLCDs or from modest caloric restriction, with or without weight loss, increases fasting ghrelin and decreases fasting leptin and insulin. Reductions in orexin, amylin, and CCK after CR have been reported; however, the evidence for these is weak owing to very few studies evaluating these outcomes, nonuniform study designs, lack of consistency in the form reported (CCK compared with CCK8, total PYY compared with PYY3-36), and varying measurement assays. Potentially, these changes suggest a homeostatic response to counter the reduction in caloric intake, prompting an increase in energy consumption by reduced satiety.
TRF also reduces fasting concentrations of satiety signals: leptin, GLP-1 (with stronger evidence than CR), and PYY. The expected reduction in fasting insulin which is seen after CR is inconsistently observed after TRF. Also, based on the limited evidence available, after TRF, fasting ghrelin decreases or remains unchanged. Evidence with regard to changes in amylin, CCK, GIP, and PP after TRF is ambiguous or inadequate, warranting further study. Overall, in consideration of the circulating peripheral hormones, the hunger–satiety balance after CR likely tips toward hunger, which appears less likely following a TRF regimen. However, with the evidence available at this time, drawing firm conclusions about differences between CR and TRF is not possible owing to the variable study design aspects such as participants’ size and type, duration of intervention, lack of control group, and inconsistent TRF regimens. In addition, differing methodological parameters such as type of hormone measured (active compared with total forms), types of assays (ELISA, RIA, MS), and prepreparation of biological samples (addition of protease inhibitors, acidification) add to the challenge of comparing results across studies. Gut peptides/hormones are one of several factors affecting eating behavior, including cultural and socioeconomic determinants that are not included in this review, but play significant roles. Longer-term studies are needed to elucidate the response of these hormones to TRF (both with and without CR).
It is important to note the hormonal processes discussed here are integrated by the central mechanisms with other signals in the brain. These then manifest as satiation or feelings of satiety and ultimately influence energy intake regulation. In a companion review, the central mechanisms involved in the regulation of satiety after CR and TRF are presented.
Limitations and directions for future research
There are both overlapping as well as potentially distinct peripheral hormonal features affecting satiety in TRF and CR. Among several determinants, the balance of the hunger and satiety systems influences eating behavior and energy balance, and restricted eating times may potentially sway this balance. Whereas satiety systems are suppressed as a function of CR and TRF (with or without CR), the effect of TRF on hunger systems may set the 2 apart. However, more human studies are needed that compare CR alone, CR with TRF, and TRF alone, so that the actual mechanisms underlying hunger and satiety can be better understood. The number of studies that have looked at TRF in humans is small, and the variety of types of TRF tested are inadequate for empirical conclusions. This information is critical to our understanding of how these different approaches to eating are sustained and whether body weight changes are maintained in the long term.
Acknowledgments
We are grateful to Fanny Lee for her review of the manuscript. The authors’ responsibilities were as follows—SK and GPK: conceived the idea; SK, NLK, DKMT, and APT: were involved in critically assessing identified literature/articles; DKMT, APT, CER, and SK: were involved in developing the early manuscript versions; NLK: independently expanded and improved the manuscript; WFH and GPK: helped to critically assess the manuscript; and all authors: were involved in literature collection and read and approved the final manuscript.
Notes
The authors reported no funding received for this study.
Author disclosures: The authors report no conflicts of interest.
NLK and SK contributed equally to this work.
Abbreviations used: ADF, alternate-day fasting; CALERIE, Comprehensive Assessment of Long-Term Effects of Reducing Intake of Energy; CCK, cholecystokinin; CR, calorie restriction; FAA, food anticipatory activity; GIP, glucose-dependent insulinotropic polypeptide; GLP-1, glucagon-like peptide-1; iAUC, incremental area under the curve; IF, intermittent fasting; PP, pancreatic polypeptide; PVN, paraventricular nucleus; PYY, peptide YY; TRF, time-restricted feeding; VLCD, very-low-calorie diet.
Contributor Information
Debra K M Tacad, Obesity and Metabolism Research Unit, USDA-Agricultural Research Service Western Human Nutrition Research Center, Davis, CA, USA. Department of Nutrition, University of California Davis, Davis, CA, USA.
Ashley P Tovar, Department of Nutrition, University of California Davis, Davis, CA, USA.
Christine E Richardson, Department of Nutrition, University of California Davis, Davis, CA, USA.
William F Horn, Obesity and Metabolism Research Unit, USDA-Agricultural Research Service Western Human Nutrition Research Center, Davis, CA, USA.
Giri P Krishnan, Department of Medicine, School of Medicine, University of California San Diego, San Diego, CA, USA.
Nancy L Keim, Obesity and Metabolism Research Unit, USDA-Agricultural Research Service Western Human Nutrition Research Center, Davis, CA, USA. Department of Nutrition, University of California Davis, Davis, CA, USA.
Sridevi Krishnan, Department of Pediatrics, School of Medicine, University of California San Diego, San Diego, CA, USA.
References
Articles from Advances in Nutrition are provided here courtesy of American Society for Nutrition
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/123515069
Article citations
Time-restricted eating affects human adipose tissue fat mobilization.
Obesity (Silver Spring), 32(9):1680-1688, 28 Jul 2024
Cited by: 0 articles | PMID: 39073251
Circadian Interventions in Preclinical Models of Huntington's Disease: A Narrative Review.
Biomedicines, 12(8):1777, 06 Aug 2024
Cited by: 0 articles | PMID: 39200241 | PMCID: PMC11351982
Review Free full text in Europe PMC
AZGP1 in POMC neurons modulates energy homeostasis and metabolism through leptin-mediated STAT3 phosphorylation.
Nat Commun, 15(1):3377, 20 Apr 2024
Cited by: 3 articles | PMID: 38643150 | PMCID: PMC11032411
The impact of intermittent fasting on gut microbiota: a systematic review of human studies.
Front Nutr, 11:1342787, 12 Feb 2024
Cited by: 3 articles | PMID: 38410639 | PMCID: PMC10894978
Review Free full text in Europe PMC
Fasting diets: what are the impacts on eating behaviors, sleep, mood, and well-being?
Front Nutr, 10:1256101, 09 Jan 2024
Cited by: 0 articles | PMID: 38264193 | PMCID: PMC10803520
Review Free full text in Europe PMC
Go to all (10) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Satiety Associated with Calorie Restriction and Time-Restricted Feeding: Central Neuroendocrine Integration.
Adv Nutr, 13(3):758-791, 01 Jun 2022
Cited by: 6 articles | PMID: 35134815 | PMCID: PMC9156369
Review Free full text in Europe PMC
The effect of meal frequency in a reduced-energy regimen on the gastrointestinal and appetite hormones in patients with type 2 diabetes: A randomised crossover study.
PLoS One, 12(4):e0174820, 03 Apr 2017
Cited by: 12 articles | PMID: 28369078 | PMCID: PMC5378398
HIGH-FIBER DIET PROMOTES METABOLIC, HORMONAL, AND SATIETY EFFECTS IN OBESE WOMEN ON A SHORT-TERM CALORIC RESTRICTION.
Arq Gastroenterol, 60(2):163-171, 01 Apr 2023
Cited by: 0 articles | PMID: 37556741
PACAP intraperitoneal treatment suppresses appetite and food intake via PAC1 receptor in mice by inhibiting ghrelin and increasing GLP-1 and leptin.
Am J Physiol Gastrointest Liver Physiol, 309(10):G816-25, 03 Sep 2015
Cited by: 19 articles | PMID: 26336928 | PMCID: PMC4652141
 and
and 


