Abstract
Free full text

Selective Pharmacologic Therapies for Dry Eye Disease Treatment: Efficacy, Tolerability, and Safety Data Review from Preclinical Studies and Pivotal Trials
Associated Data
Abstract
Keratoconjunctivitis sicca, also known as dry eye disease (DED), is a prevalent, multifactorial disease associated with compromised ocular lubrication, ocular surface inflammation and damage, and ocular symptoms. Several anti-inflammatory, topical ophthalmic therapies are available to treat clinical signs and symptoms of DED in the USA and Europe. Cyclosporine A (CsA)-based formulations include an ophthalmic emulsion of 0.05% CsA (CsA 0.05%), a cationic emulsion (CE) of CsA 0.1% (CsA CE), and an aqueous nanomicellar formulation of 0.09% CsA (OTX-101). Lifitegrast is a 5% ophthalmic solution of a lymphocyte function-associated antigen 1 antagonist that is believed to target T cell activation and recruitment to inhibit ocular inflammation. Here we provide a comprehensive review summarising preclinical studies and pivotal trial data for these treatments to provide a complete understanding of their efficacy and safety profile. Overall, data in the evaluated studies show a favourable risk–benefit profile for the use of targeted topical anti-inflammatory pharmacologic treatments in patients with DED. Pivotal trials for CsA 0.05%, CsA CE, OTX-101, and lifitegrast clearly demonstrate treatment efficacy compared to vehicle across treatments with no serious ocular treatment-emergent adverse events (TEAEs). Patients using ophthalmic treatments reported ocular TEAEs more frequently than those treated with vehicle; however, relatively few TEAEs led to treatment discontinuation. The specific signs and symptoms of DED that improve with treatment vary with the treatment prescribed. Long-term and direct comparative studies between treatments are needed to further understand treatment differences in efficacy and safety profiles.
Key Summary Points
| Several topical pharmacologic therapies are approved for the treatment of dry eye disease; however, there are no head-to-head pivotal trials comparing these treatments. |
| A comprehensive review summarising data from preclinical studies and pivotal trials for cyclosporine ophthalmic emulsion 0.05%, cyclosporine emulsion 0.1%, cyclosporine ophthalmic solution 0.09%, and lifitegrast ophthalmic solution 5% was conducted to provide a complete understanding of their efficacy and safety profile. |
| Overall, these topical ophthalmic therapies are safe and well tolerated and demonstrate clinically and statistically significant improvements in signs and symptoms of dry eye disease. |
| Clinical data show a favourable risk–benefit profile for the use of targeted topical anti-inflammatory pharmacologic treatments in patients with dry eye disease; although many patients treated with these agents experience ocular treatment-emergent adverse events, the rate of treatment discontinuation is relatively low. |
| The specific signs and symptoms of dry eye disease that improve vary with the treatment prescribed. |
Introduction
Dry eye disease (DED), also known as keratoconjunctivitis sicca, is a prevalent, multifactorial disease of the ocular surface, in which there is a loss of tear film homeostasis accompanied by ocular symptoms [1]. Factors that contribute to the development of DED include tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities [1]. A key characteristic of DED is the chronic cycle of inflammation triggered by tear film instability and hyperosmolarity [2, 3]. An increase in inflammatory mediators at the ocular surface tissue amplifies the inflammatory response, perpetuates the disease, and ultimately leads to ocular surface damage [2].
There are a number of clinical signs and symptoms of DED that often function independently rather than interdependently and are not highly correlated [4, 5]. Key DED symptoms include ocular irritation, pain, dryness, foreign body sensation, and visual disturbance; objective clinical signs include tear film instability and hyperosmolarity, reduced tear volume, ocular surface inflammation and damage, and neurosensory abnormalities [1, 4, 5]. There are several methods for clinically assessing DED signs and symptoms, such as corneal and conjunctival staining to identify ocular surface damage and ocular surface symptom patient questionnaires [6, 7]. A low association between DED signs and symptoms makes integrating dry eye clinical research into practice challenging.
Treatment for DED often begins with patient education, environmental modification, and over-the-counter artificial tears, with patients progressing to pharmacologic treatments if non-pharmacologic options are inadequate [8]. Several topical pharmacologic therapies are approved for the treatment of DED. These therapies inhibit ocular surface inflammation that leads to clinical manifestations of DED as well as ocular surface damage. Cyclosporine A (CsA), an immunomodulatory agent with anti-inflammatory properties, is the active pharmaceutical ingredient (API) in several topical preparations. CsA inhibits calcineurin and blocks T lymphocyte activity and the subsequent release of proinflammatory mediators [9, 10]. CsA 0.05% (Restasis®, 0.05% ophthalmic emulsion, Allergan, Irvine, CA) is an ophthalmic oil-in-water anionic emulsion approved in the USA (since 2002) indicated to increase tear production in patients whose tear production is presumed to be suppressed as a result of ocular inflammation associated with DED [11]. A cationic emulsion (CE) of CsA 0.1% (CsA CE; Ikervis® [ciclosporin ophthalmic emulsion], Santen Pharmaceutical, Osaka, Japan) is approved in Europe (since 2015) to treat severe keratitis in patients with DED that has not improved with tear substitutes [12]. An aqueous nanomicellar formulation of 0.09% CsA (OTX-101; Cequa™ [cyclosporine ophthalmic solution 0.09%], Sun Pharmaceutical Industries, Inc., Cranbury, NJ) is approved in the USA (since 2018) to increase tear production in patients with DED [13]. Lifitegrast 5% ophthalmic solution (Xiidra®, Novartis, East Hanover, NJ) is a lymphocyte function-associated (LFA) antigen 1 antagonist approved in the USA (since 2016) for the treatment of both signs and symptoms of DED [14]. Lifitegrast decreases T cell activation and recruitment by blocking the interaction between the integrin LFA antigen 1 and intercellular adhesion molecule 1, thereby inhibiting inflammation. Lastly, loteprednol etabonate 0.25% is a unique proprietary mucus-penetrating particle vehicle (Eysuvis™, Kala Pharmaceuticals, Watertown, MA) indicated for short-term treatment (up to 2 weeks) of the signs and symptoms of DED [15]. As loteprednol etabonate 0.25% is a limited duration treatment with no pivotal trials to date, it is not included in this review.
Preclinical studies and pivotal trials have established the safety and efficacy of DED treatments. In clinical trials, the active treatment is typically directly compared against the vehicle, a treatment that resembles the active drug but does not include the active component. There are no head-to-head pivotal trials comparing topical ophthalmic DED treatments. Therefore, a comprehensive review summarising preclinical studies and pivotal trials data for these treatments can be valuable in providing a more complete understanding of their efficacy and safety profile. This review examines the efficacy, tolerability, and safety data from preclinical studies and pivotal trials for topical DED treatments.
Selection of Included Publications
All publications selected for this review met the prespecified criteria of (1) industry-sponsored and (2) preclinical study, clinical trial for regulatory approval, or multi-year clinical trial. The treatments included were pharmacologic DED therapies approved in the USA and/or Europe. Data from these studies were summarised; no additional quantitative or statistical analyses were performed.
The quality of evidence for clinical outcomes discussed in this review was objectively assessed using the grading of recommendation, assessment, development, and evaluation (GRADE) approach [16–18]. Detailed methods for the GRADE approach have been previously published [17, 18]. Briefly, the GRADE system was used to assess both the quality of data from included studies and the overall quality of evidence for each outcome stratified by treatment. GRADE scores range from 1 (very low quality) to 4 (high quality). For each outcome, an initial quality score was given on the basis of whether the evidence for the outcome was from primarily randomised controlled trials (starting score of 4) or non-randomised controlled trials (starting score of 2). Next, the five primary GRADE criteria (risk of bias, inconsistency, indirectness, imprecision, and publication bias) were assessed for each outcome using a modified checklist to ensure consistent scoring [17]. Three additional criteria (magnitude of effect, dose response, and effect of confounding factors) were also assessed to determine if the quality of evidence for an outcome should be upgraded; however, these criteria were only applied to outcomes that started with an initial quality score of 2 [18]. Last, the initial quality score was adjusted on the basis of the results for each of the GRADE assessment criteria, and an overall score for quality of evidence was determined. Supplementary Table 1 shows the summary of findings for each outcome by treatment type.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
CsA 0.05%
The first ophthalmic treatment for DED in the USA was CsA 0.05%, an oil-in-water anionic emulsion formulation approved in 2002. CsA 0.05% was the only Food and Drug Administration-approved topical CsA treatment available in the USA until 2018 [19, 20].
Clinical Pivotal Trials
Efficacy
The efficacy of CsA 0.05% was demonstrated in two pivotal clinical trials and one phase 4 trial (Table 1). The first pivotal trial compared the efficacy of 0.05%, 0.1%, 0.2%, and 0.4% CsA to vehicle in patients with moderate-to-severe DED [21]. No dose–response relationship was observed; all formulations significantly improved ocular signs and symptoms of DED over 12 weeks of treatment compared to baseline (Table 2, P <
< 0.050) [21]. CsA 0.1% demonstrated consistent improvements in conjunctival staining (P
0.050) [21]. CsA 0.1% demonstrated consistent improvements in conjunctival staining (P ≤
≤ 0.016) and Schirmer’s tear test scores and CsA 0.05% demonstrated consistent improvements in patient symptoms such as ocular dryness (P
0.016) and Schirmer’s tear test scores and CsA 0.05% demonstrated consistent improvements in patient symptoms such as ocular dryness (P ≤
≤ 0.036). As higher doses of CsA did not show further benefit compared to the 0.05% and 0.1% doses, only the lower doses were utilised for future development [21].
0.036). As higher doses of CsA did not show further benefit compared to the 0.05% and 0.1% doses, only the lower doses were utilised for future development [21].
Table 1
Differences in study design, patient demographics, and disposition of included studies
| Design | Treatment arms | Dose and duration | Follow-up period (months) | Patient Demographics Age, yrs (mean ± SD) Male, n (%) Majority race | Key inclusion criteria |
|---|---|---|---|---|---|
| Hwang et al. (2020) [26] | |||||
| Preclinical | CsA 0.05% 1:50 | Once, 24 hours | 24 hours | N/A N/A N/A | N/A |
| CsA CE 1:50 | |||||
| CsA CE 1:100 | |||||
| Sall et al. (2000) [22] | |||||
| Multicentre, randomised, double-masked, parallel-group, 6-month, vehicle-controlled, phase 3 | CsA 0.05% (n = 293) | 1 drop in both eyes BID for 6 months | 1, 3, 4, 6 | 58.7 ± 13.9 49 (16.7) Caucasian | Adults diagnosed with moderate-to-severe DED Schirmer’s test ≤5 mm/5 min in ≥1 eye Sum of corneal and interpalpebral conjunctival staining of ≥+5 with CFS ≥+2 OSDI score of 0.1 Subjective Facial Expression Scale score ≥3 |
| Vehicle (n = 292) | 59.9 ± 14.3 59 (20.2) Caucasian | ||||
| Stevenson et al. (2000) [21] | |||||
| Randomised, multicentre, double-masked, parallel-group, dose-response controlled, phase 2 | CsA 0.05% (n = 31) | 1 drop in both eyes BID for 84 days | 1, 2, 3 | 59 (range: 31–88) 26 (16.0) Caucasian | ≥21 years of age with diagnosis of DED with or without Sjögren’s syndrome refractory to conventional management Schirmer’s test 7 mm/5 min in ≥1 eye CFS ≥1 in either eye ≥1 moderate dry eye-related symptom(s) |
| Vehicle (n = 33) | |||||
| Stonecipher et al. (2016) [23] | |||||
| Prospective, single-centre, open-label, phase 4 | CsA 0.05% (n = 40) | 1 drop in both eyes BID for 6 months | 1, 6 | 59.4 ± 9.1 5 (12.5) Caucasian | Adults with history of bilateral DED Use of or desire to use artificial tear substitutes within past 6 months Score of ≥2 for at least 1 dry eye symptom OSDI score >12 Schirmer’s test <10 mm/5 min CFS of 2–4 in ≥1 region and central corneal staining ≥2 Conjunctival redness score ≥1 |
| Baudouin et al. (2017) [28] | |||||
| Multicentre, double-masked, randomised, parallel-group, controlled, phase 3 | CsA CE (n = 241) | 1 drop QD in both eyes for 6 months | 1, 3, 6 | 57.6 ± 12.9 36 (14.9) Caucasian | Moderate-to-severe DED refractory to conventional management ≥1 symptoms of ocular discomfort in at least 1 eye (eligible eye) Eligible eye TBUT ≤8 seconds, CFS score 2–4 (modified Oxford scale), Schirmer’s test score ≥2 mm/5 min and <10 mm/5 min, and a corneal and conjunctival staining score ≥4 (Van Bijsterveld scale) No use of systemic or topical CsA, tacrolimus, or sirolimus within 6 months prior to study entry No use of topical corticosteroids or prostaglandins within 1 month before study entry |
| Vehicle (n = 248) | 58.8 ± 12.7 40 (16.1) Caucasian | ||||
| Baudouin et al. (2017) [29] | |||||
Multicentre, double-masked, randomised, vehicle-controlled, parallel-group, phase 3, 6 month period (part 1), followed by an open-label 6 month follow-up period (part 2) | CsA CE (n = 154)* CsA CE/CsA CE (n = 128)† | 1 drop QD for 12 months | 6, 9, 12 | NR NR NR | Adults with severe DED, as determined by CFS score = 4 (modified Oxford scale) Schirmer’s test ≥2 mm/5 min and <10 mm/5 min; OSDI score ≥23 |
Vehicle (n = 91)* Vehicle/CsA CE (n = 79)† | NR NR NR | ||||
| Leonardi et al. (2016) [27] | |||||
| Multicentre, randomised, double-masked, vehicle-controlled, parallel-group, phase 3 | CsA CE (n = 154) | 1 drop in both eyes QD for 6 months | 1, 3, 6 | 60.8 ± 13.5 28 (18.2) NR | Adults with severe DED CFS score = 4 (modified Oxford scale) Schirmer’s test 2–10 mm/5 min OSDI score ≥23 |
| Vehicle (n = 91) | 62.1 ± 11.8 8 (8.8) NR | ||||
| Burade et al. (2020) [34] | |||||
| Preclinical | OTX-101 0.09% BID (n = 11) | 10 μL in conjunctival sac of both eyes QD or BID for 60 days | 0.5, 1, 1.5, 2 | 0.31 - 0.36 77 (100) N/A | NOD mice spontaneously develop Sjögren’s syndrome. This disease model manifests typical features of dry eye and secretory dysfunction |
| OTX-101 0.09% QD (n = 11) | |||||
| CsA 0.05% BID (n = 11) | |||||
| CsA CE QD (n = 11) | |||||
| Vehicle BID (n = 11) | |||||
| Untreated Healthy C57Bl6/J (n = 11) | |||||
| Untreated NOD (n = 11) | |||||
| Goldberg et al. (2019) [36] | |||||
| Randomised, multicentre, vehicle-controlled, double-masked, phase 3 | OTX-101 0.09% (n = 371) | 1 drop in both eyes BID for 84 days | 1, 2, 3 | 58.4 ± 14.1 56 (15.1) Caucasian | Adults with a self-reported history of DED ≥6 months Clinical diagnosis of bilateral DED at screening Conjunctival staining score 3–9 Global symptom score ≥40 |
| Vehicle (n = 373) | 59.5 ± 14.7 62 (16.6) Caucasian | ||||
| Karpecki et al. (2019) [42] | |||||
| Open-label, single-centre, single-arm, phase 1 | OTX-101 0.09% (n = 16) | 1 drop in both eyes BID for 7 days | 0.23, 0.27, 0.30 | 38.2 ± 10.9 10 (62.5) Caucasian | Adults with BMI 18–32 kg/m2; medically healthy No nicotine/tobacco use Non-diseased eyes IOP 10–21 mm Hg in each eye Corrected visual acuity >20/40 in each eye |
| Malhotra et al. (2019) [37] | |||||
| Randomised, multicentre, double-masked, vehicle-controlled, pooled analysis of phase 2b/3 and phase 3 studies | OTX-101 0.09% (n = 523) | 1 drop in both eyes BID for 84 days | 1, 2, 3 | 58.6 ± 14.2 86 (16.4) Caucasian | Adults with a self-reported history of DED ≥6 months Clinical diagnosis of bilateral DED Conjunctival staining score 3–9 in same eye at screening and baseline visits Snellen VA >20/200 in each eye |
| Vehicle (n = 525) | 59.5 ± 14.4 94 (17.9) Caucasian | ||||
| Sheppard et al. (2020) [39] | |||||
| Randomised, multicentre, double-masked, vehicle-controlled, pooled analysis of phase 2b/3 and phase 3 studies | OTX-101 0.09% (n = 311) | 1 drop in both eyes BID for 84 days | 1, 2, 3 | 60.6 ± 13.4 46 (14.8) Caucasian | Adults with a self-reported history of DED ≥6 months Clinical diagnosis of bilateral DED Conjunctival staining score 3–9 in same eye at screening and baseline visits Snellen VA >20/200 in each eye SANDE score ≥40 at both screening and baseline visits |
| Vehicle (n = 310) | 61.7 ± 13.0 58 (18.7) Caucasian | ||||
| Sheppard et al. (2021) [40] | |||||
| Randomised, multicentre, double-masked, vehicle-controlled, phase 3 treatment phase with subsequent long-term, open-label extension phase | OTX-101 0.09% (n = 371) § OTX-101 0.09% /OTX-101 0.09% (n = 129)¶ | 1 drop in both eyes BID for 84 days | 1, 2, 3, 7, 10, 13, 16 | 58.4 ± 14.1 56 (15.1) Caucasian 58.4 ± 15.5 20 (15.5) NR | Adults with a self-reported history of DED ≥6 months Clinical diagnosis of bilateral DED Conjunctival staining score 3–9 in same eye at screening and baseline visits Snellen VA >20/200 in each eye SANDE score ≥40 at both screening and baseline visits |
Vehicle (n = 373)§ Vehicle/OTX-101 0.09% (n = 129)¶ | 59.5 ± 14.7 62 (16.6) Caucasian 61.5 ± 14.2 22 (17.1) NR | ||||
| Smyth-Medina et al. (2019) [38] | |||||
| Randomised, multicentre, double-masked, vehicle-controlled, pooled analysis of phase 2b/3 and phase 3 studies | OTX-101 0.09% (n = 523) | 1 drop in both eyes BID for 84 days | 0.5, 1, 1.5, 2, 3 | 58.6 ± 14.2 86 (16.4) Caucasian | Adults with a clinical diagnosis of bilateral DED for ≥6 months Conjunctival staining score 3–9 in same eye at screening and baseline visits |
| Vehicle (n = 525) | 59.5 ± 14.4 94 (17.9) Caucasian | ||||
| Tauber et al. (2018) [35] | |||||
| Randomised, multicentre, double-masked, vehicle-controlled, dose-ranging, phase 2b/3 | OTX-101 0.05% (n = 151) | 1 drop in both eyes BID for 84 days | 0.5, 1, 1.5, 2, 3 | 61.9 ± 13.3 32 (21.2) Caucasian | Adults with a self-reported history of DED for ≥6 months Diagnosis of bilateral DED Snellen VA of ≥20/200 Conjunctival staining score 3–9 SANDE score ≥40 at screening and baseline visits |
| OTX-101 0.09% (n = 152) | 59.2 ± 14.6 30 (19.7) Caucasian | ||||
| Vehicle (n = 152) | 59.3 ± 13.8 32 (21.1) Caucasian | ||||
| Weiss et al. (2019) [33] | |||||
| Preclinical | Single dose OTX-101 0.05% (n = 20) | Single bilateral distribution of treatment | 0.25, 0.5, 1, 2, 4, 8, 12, 24, 48, 72 hours | NR NR N/A | NR |
| Single dose CsA 0.05% (n = 20) | |||||
| Repeat dose OTX-101 0.01% (n = 10) | 4 bilateral instillations per day for 7 days | 4, 7 days | |||
| Repeat dose OTX-101 0.05% (n = 20) | |||||
| Repeat dose OTX-101 0.1% (n = 20) | |||||
| Repeat dose CsA 0.05% (n = 20) | |||||
| Chung et al. (2018) [45] | |||||
| Preclinical | Lifitegrast OPUS-1 Rabbits (n = 25) | Rabbits: 1.75 mg/eye/dose BID for 5 days Dogs: One 10 mL dose IV and one 30 μL dose in eye | Rabbits: 0.25, 0.5, 1, 3, and 8 hours Dogs: 0.25, 0.5, 1, 1.5, 2, 4, 8, 24, 48, 72, 96, 120, 144, and 168 hours | Rabbits: ≥0.5 N/A Dogs: 0.50–0.58 6 (54.5) N/A | N/A |
Lifitegrast OPUS-2 Rabbits (n = 25) | |||||
14C-lifitegrast Dogs (n = 10) | |||||
| Donnenfeld et al. (2016) [52] | |||||
| Prospective, randomised, multicentre, double-masked, vehicle-controlled phase 3 | Lifitegrast 5.0% (n = 221) | 1 drop in both eyes BID for 360 days | 0.5, 3, 6, 9, 12 | 58.8 ± 12.4 56 (25.3) Caucasian | Adults with a self-reported history of DED BCVA of 0.7 logMAR or better CFS score ≥2 in ≥1 region VAS ≥40 for eye dryness or discomfort Use of artificial tears within 6 months Schirmer’s test 1–10 mm |
| Vehicle (n = 111) | 61.0 ± 13.2 26 (23.4) Caucasian | ||||
| Holland et al. (2017) [49] | |||||
| Randomised, double-masked, multicentre, vehicle-controlled, phase 3 | Lifitegrast (n = 355) | 1 drop in both eyes BID for 84 days | 0.5, 1.5, 3 | 58.8 ± 14.1 87 (24.5) Caucasian | Adults with a self-reported history of DED BCVA of ≥0.7 logMAR; CFS score ≥2 in ≥1 region VAS ≥40 for EDS in both eyes; conjunctival redness score ≥1 in ≥1 eye Use of artificial tears within 30 days Positive response in at least 1 eye at visits 1 and 2 based on these criteria: ICSS ≥0.5 and Schirmer’s test 1–10 mm |
| Placebo (n = 356) | 58.6 ± 14.8 87 (24.4) Caucasian | ||||
| Nichols et al. (2018) [53] | |||||
| Prospective, multicentre, randomised, double-masked, vehicle-controlled, phase 3 | Lifitegrast (n = 355) | 1 drop in both eyes BID for 84 days | 0.5, 1.5, 3 | 58.8 ± 14.1 87 (24.5) Caucasian | Adults with a self-reported history of DED Schirmer’s test 1–10 mm EDS score VAS ≥40 Corneal staining score ≥2 in ≥1 region Artificial tear use within 30 days of study |
| Placebo (n = 356) | 58.6 ± 14.8 87 (24.4) Caucasian | ||||
| Nichols et al. (2019) [54] | |||||
| Multicentre, randomised, prospective, double-masked, placebo-controlled, parallel-arm, pooled analysis of phase 2 and phase 3 studies | Lifitegrast (n = 1287) | 1 drop in both eyes BID for 84 or 360 days | 3, 12 | 59.3 ± 13.3 291 (22.6) Caucasian | Adults with DED Corneal staining score ≥2 Redness score ≥1 Schirmer’s test 1–10 mm Change in ICSS ≥1; ICSS ≥0.5 ODS ≥3 at 2 consecutive time points during CAE 1 and 2 Artificial tear use within 30 days of study EDS score VAS ≥40 |
| Placebo (n = 1177) | 59.6 ± 13.7 298 (25.3) Caucasian | ||||
| Paskowitz et al. (2012) [51] | |||||
| Prospective, randomised, double-masked, phase 1b | Lifitegrast 0.1% (n = 4) | 1 drop in test eye BID for 1 week | NR | NR NR NR | Adults scheduled for pars plana vitrectomy |
| Lifitegrast 1.0% (n = 4) | |||||
| Lifitegrast 5.0% (n = 5) | |||||
| Pepose et al. (2019) [50] | |||||
| Prospective, single-arm, open-label, 12-week, longitudinal, phase 4 | Lifitegrast (n = 26) | 1 drop in both eyes BID for 84 days | 0.5, 1.5, 3 | 67.4 ± 9.6 3 (11.5) Caucasian | Adults diagnosed with DED VAS score ≥40 In Group 1: tear osmolarity 308–320 mOsm/L in ≥1 eye In Group 2: tear osmolarity ≥320 mOsm/L in ≥1 eye |
| Semba et al. (2012) [48] | |||||
| Prospective, randomised, double-masked, vehicle-controlled, parallel-arm, phase 2 | Lifitegrast 0.1% (n = 57) | 1 drop in both eyes BID for 84 days | 0.5, 1.5, 3 | 63.1 ± 13.1 10 (17.5) Caucasian | Adults with history of bilateral DED Use or desire to use artificial tear substitutes within past 6 months Conjunctival redness CFS ≥2 Schirmer’s test 1–10 mm BCVA of ≥0.7 logMAR |
| Lifitegrast 1.0% (n = 57) | 63.6 ± 11.9 17 (29.8) Caucasian | ||||
| Lifitegrast 5.0% (n = 58) | 62.3 ± 12.2 11 (19.0) Caucasian | ||||
| Placebo (n = 58) | 60.4 ± 12.9 13 (22.4) Caucasian | ||||
| Sheppard et al. (2014) [46] | |||||
| Multicentre, randomised, prospective, double-masked, placebo-controlled, parallel-arm, phase 3 | Lifitegrast 5.0% (n = 293) | 1 drop in both eyes BID for 84 days | 0.5, 1.5, 3 | 60.2 ± 12.2 64 (21.8) Caucasian | Adults with history of bilateral DED Use or desire to use artificial tear substitutes within past 6 months Conjunctival redness CFS ≥2 Schirmer’s test 1–10 mm BCVA of ≥0.7 logMAR |
| Placebo (n = 295) | 61.1 ± 11.8 78 (26.4) Caucasian | ||||
| Tauber et al. (2015) [47] | |||||
| Multicentre, randomised, prospective, double-masked, vehicle-controlled, parallel-arm, phase 3 | Lifitegrast 5.0% (n = 358) | 1 drop in both eyes BID for 84 days | 0.5, 1.5, 3 | 58.7 ± 13.9 73 (20.4) Caucasian | Adults with a self-reported history of DED Use of artificial tears within past 30 days BCVA of ≥0.7 logMAR CFS score ≥2 in ≥1 region VAS ≥40 for EDS in both eyes Conjunctival redness score ≥1 in ≥1 eye EDS score VAS ≥40 Positive response in ≥1 eye at visits 1 and 2 ICSS ≥0.5 and Schirmer’s test 1–10 mm |
| Vehicle (n = 360) | 58.9 ± 14.3 95 (26.4) Caucasian | ||||
BCVA best-corrected visual acuity, BID twice daily, BMI body mass index, CAE controlled adverse environment, CFS corneal fluorescein staining, CsA 0.05% cyclosporine ophthalmic emulsion 0.05%, CsA CE 0.1% (1 mg/mL) cyclosporine A cationic emulsion, DED dry eye disease, EDS eye dryness score, ICSS inferior corneal staining score, IOP intraocular pressure, IV intravenous, logMAR logarithm of the minimum angle of resolution in both eyes, min minimum, N/A not applicable, NOD NOD.B10.H2b, NR not reported, ODS ocular discomfort score, OSDI Ocular Surface Disease Index, OTX-101 cyclosporine ophthalmic solution 0.09%, QD once daily, SANDE Symptom Assessment iN Dry Eye, SD standard deviation, TBUT tear break-up time, VA visual acuity, VAS visual analogue scale
*Part 1, 0–6 months of treatment
†Part 2, 6–12 months of CsA CE
§Treatment phase
¶Open-label extension
Table 2
Summary of statistically significant between-group differences (P <
< 0.05) in clinical efficacy
0.05) in clinical efficacy
| Intervention | Efficacy endpoints* | Time point# | Estimate by group | |
|---|---|---|---|---|
| Treatment | Comparison† | |||
| Sall et al. 2000 [22] | ||||
| CsA 0.05% | CFB in corneal staining | Month 4 | NR | NR |
| Month 6 | NR | NR | ||
| Mean CFB in Schirmer’s score (anaesthetised) | Month 3 | NR | NR | |
| Decrease in artificial tear use | Month 6 | NR | NR | |
| CFB in blurred vision | Month 1 | NR | NR | |
| Month 3 | NR | NR | ||
| Month 4 | NR | NR | ||
| Month 6 | NR | NR | ||
| Stevenson et al. 2000 [21] | ||||
| CsA 0.05% | Improvement in sandy or gritty feeling | Treatment week 12 | NR | NR |
| Post-treatment week 2 | NR | NR | ||
| Post-treatment week 4 | NR | NR | ||
| Improvement in ocular dryness | Post-treatment week 4 | NR | NR | |
| Baudouin et al. 2017 [28] | ||||
| CsA CE | Mean CFB in CFS | Month 1 | − 0.8 0.8 | − 0.5 0.5 |
| Month 3 | − 0.9 0.9 | − 0.7 0.7 | ||
| Month 6 | − 1.1 1.1 | − 0.8 0.8 | ||
Percent of patients with
| Month 6 | 50.2% | 42.0% | |
| Median HLA-DR expression CFB | Month 6 | − 21,875.6 21,875.6 | − 1334.2 1334.2 | |
| Leonardi et al. 2016 [27] | ||||
| CsA CE | Mean adjusted CFB in CFS | Month 3 | NR | NR |
| Month 6 | − 1.76 1.76 | − 1.42 1.42 | ||
| Ocular surface inflammation (HLA-DR expression) | Month 1 | 52,306.0 | 66,825.0 | |
| Month 6 | 49,917.0 | 76,062.0 | ||
| Goldberg et al. 2019 [36] | ||||
| OTX-101 0.09% | Percentage of eyes with an increase of ≥ 10 mm from baseline in Schirmer’s test scores 10 mm from baseline in Schirmer’s test scores | Day 84 | 16.6 (95% CI 13.4, 19.7) | 9.2 (95% CI 6.8, 11.7) |
| Mean CFB in total corneal staining scores | Day 28 | − 0.8 0.8 ± ± 1.9 1.9 | − 0.6 0.6 ± ± 1.8 1.8 | |
| Day 56 | − 1.3 1.3 ± ± 1.9 1.9 | − 0.9 0.9 ± ± 2.0 2.0 | ||
| Day 84 | − 1.4 1.4 ± ± 2.0 2.0 | − 1.2 1.2 ± ± 2.2 2.2 | ||
| Percentage of eyes with clear central corneas | Day 28 | 54.1 | 47.3 | |
| Day 56 | 61.7 | 52.1 | ||
| Day 84 | 65.0 | 56.9 | ||
LS mean CFB In total conjunctival staining | Day 56 | NR | NR | |
| Day 84 | NR | NR | ||
| Malhotra et al. 2019 [37] | ||||
| OTX-101 0.09% | LS mean CFB in CFS total scores | Day 28 | − 0.9 0.9 ± ± 0.1 0.1 | − 0.5 0.5 ± ± 0.1 0.1 |
| Day 56 | NR | NR | ||
| Day 84 | − 1.4 1.4 ± ± 0.1 0.1 | − 0.9 0.9 ± ± 0.1 0.1 | ||
| Sheppard et al. (2020) [39] | ||||
| OTX-101 0.09% | ITT population: Percentage of eyes with increase in Schirmer’s score ≥ ≥ 10 mm from baseline 10 mm from baseline | Day 84 or at early discontinuation | 16.6 | 9.0 |
ITT population: Percentage of eyes with increase in Schirmer’s score > > 5 mm from baseline 5 mm from baseline | Day 84 or at early discontinuation | 28.1% | 17.7% | |
| ITT population: Schirmer’s score | Day 84 or at early discontinuation | 14.6 ± ± 9.9 9.9 | 12.8 ± ± 9.2 9.2 | |
Subgroup with Schirmer’s score < < 10 mm: Percentage of eyes with increase in Schirmer’s score 10 mm: Percentage of eyes with increase in Schirmer’s score ≥ ≥ 10 mm from baseline 10 mm from baseline | Day 84 or at early discontinuation | 18.7 | 10.2 | |
Subgroup with Schirmer’s score < < 10 mm: Percentage of eyes with increase in Schirmer’s score 10 mm: Percentage of eyes with increase in Schirmer’s score > > 5 mm from baseline 5 mm from baseline | Day 84 or at early discontinuation | 31.0% | 19.6% | |
Subgroup with Schirmer’s score < < 10 mm: Schirmer’s score 10 mm: Schirmer’s score | Day 84 or at early discontinuation | 9.9 ± ± 7.7 7.7 | 8.1 ± ± 6.6 6.6 | |
| Sheppard et al. (2021) [40] | ||||
| OTX-101 0.09% (worse eye) | Percentage of patients with Schirmer’s score increase of ≥ 10 mm from baseline 10 mm from baseline | Week 12 | 20.5 | 11.3 |
| Mean CFB in Schirmer’s scores | Week 12 | 4.0 ± ± 7.8 7.8 | 2.2 ± ± 6.8 6.8 | |
LS mean ± ± SE CFB in total conjunctival staining SE CFB in total conjunctival staining | Week 8 | − 1.5 1.5 ± ± 0.1 0.1 | − 0.9 0.9 ± ± 0.1 0.1 | |
| Week 12 | − 1.7 1.7 ± ± 0.1 0.1 | − 1.1 1.1 ± ± 0.1 0.1 | ||
| Percentage of patients with clear central corneas | Week 4 | 55.1 | 45.6 | |
| Week 12 | 64 | 55.3 | ||
| Smyth-Medina et al. (2019) [38] | ||||
| OTX-101 0.09% | Mean total conjunctival staining score in both eyes | Day 28 | NR | NR |
| Day 56 | NR | NR | ||
| Day 84 | 3.9 ± ± 2.3 2.3 | 4.5 ± ± 2.5 2.5 | ||
| Mean inferior conjunctival staining score in both eyes | Day 28 | NR | NR | |
| Day 56 | NR | NR | ||
| Day 84 | 1.1 ± ± 0.7 0.7 | 1.3 ± ± 0.7 0.7 | ||
| Mean superior conjunctival staining score in both eyes | Day 28 | NR | NR | |
| Day 56 | NR | NR | ||
| Day 84 | 0.7 ± ± 0.6 0.6 | 0.9 ± ± 0.7 0.7 | ||
| Mean lateral conjunctival staining score in both eyes | Day 56 | NR | NR | |
| Day 84 | 0.6 ± ± 0.7 0.7 | 0.8 ± ± 0.7 0.7 | ||
| Tauber et al. (2018) [35] | ||||
| OTX-101 0.09% | LS mean CFB in total conjunctival staining scores | Day 84 | NR | NR |
| Mean CFB in total CFS scores | Day 28 | NR | NR | |
| Day 84 | NR | NR | ||
| Mean CFB in Schirmer’s test scores | Day 84 | 3.5 mm | 0 mm | |
| Holland et al. (2017) [49] | ||||
| Lifitegrast | Mean CFB in eye dryness score (VAS) | Day 14 | 7.9¶ (95% CI 4.3, 11.4) | |
| Day 42 | 9.3¶ (95% CI 5.4, 13.2) | |||
| Day 84 | 7.2¶ (95% CI 3.0, 11.3) | |||
| Semba et al. (2012) [48] | ||||
| Lifitegrast | Percentage of subjects demonstrating an increase of inferior corneal staining > > 1.0 point CFB 1.0 point CFB | Day 84 | 0 | 16.1 |
| Percentage of subjects demonstrating improvement in OSDI visual-related score | Day 84 | 50.0% | 19.6% | |
| Inferior corneal staining score mean CFB | Day 84 | NR | NR | |
| Sheppard et al. (2014) [46] | ||||
| Lifitegrast | Mean CFB in inferior CFS score | Day 84 | NR | NR |
Percentage of subjects with ≥ reduction in inferior corneal staining score | Day 84 | 22.2 | 13.9 | |
| Mean CFB in total CFS score | Day 84 | NR | NR | |
| Mean CFB in superior CFS score | Day 84 | NR | NR | |
| Mean CFB in nasal conjunctival staining score | Day 14 | NR | NR | |
| Day 42 | NR | NR | ||
| Day 84 | NR | NR | ||
| Mean CFB in total conjunctival staining score | Day 14 | NR | NR | |
| Day 84 | NR | NR | ||
Proportion of subjects with ≥ 1.0-point reduction in nasal conjunctival staining 1.0-point reduction in nasal conjunctival staining | Day 84 | 24.6% | 15.6% | |
| Mean eye dryness score | Day 42 | NR | NR | |
| Day 84 | NR | NR | ||
| Mean ocular discomfort score | Day 84 | NR | NR | |
| Tauber et al. (2015) [47] | ||||
| Lifitegrast | Eye dryness (VAS) CFB | Day 84 | − 35.3 35.3 ± ± 28.6 28.6 | − 22.75 22.75 ± ± 28.4 28.4 |
Data presented as mean ±
± SD, unless indicated otherwise
SD, unless indicated otherwise
CFB change from baseline, CFS corneal fluorescein staining, CI confidence interval, CsA 0.05% cyclosporine ophthalmic emulsion 0.05%, CsA CE 0.1% (1 mg/mL) cyclosporine A cationic emulsion, F Fisher exact test, HLA-DR human leukocyte antigen DR, ITT intent-to-treat, lifitegrast lifitegrast ophthalmic solution 5.0%, LS least squares, NR not reported, OSDI ocular surface disease index, OTX-101 cyclosporine ophthalmic solution 0.09%, SE standard error, SD standard deviation, VAS visual analogue scale
*Only endpoints with statistically significant between-group results are included in this table
†Comparison group is vehicle, unless indicated otherwise
§Nominal p value
¶Treatment effect
#Time points reported as published
In the second pivotal trial, Sall et al. compared the efficacy of CsA 0.05% and 0.1% to vehicle in patients with moderate-to-severe DED. Both concentrations significantly improved corneal staining and Schirmer’s scores over 6 months of treatment, but treatment with CsA 0.05% led to earlier and more consistent improvements [22]. Furthermore, CsA 0.05% significantly improved the subjective efficacy endpoints of blurred vision and need for concomitant artificial tears compared to vehicle (Table 2) [22]. These results are comparable to the first pivotal trial, which demonstrated similar significant improvements from baseline in the subjective efficacy endpoint (sandy or gritty feeling) with CsA 0.05% compared to vehicle after 12 weeks of treatment (P ≤
≤ 0.027), which was sustained through 4 weeks post-treatment (Table 2) [21].
0.027), which was sustained through 4 weeks post-treatment (Table 2) [21].
A phase 4, open-label study confirmed the clinical benefit of CsA 0.05% as a treatment for DED (Table 2). Patients with bilateral DED administered CsA 0.05% twice daily (BID) for 6 months; inferior corneal, central corneal, total corneal, and total ocular surface (total corneal +
+ conjunctival) fluorescein staining significantly improved from baseline to 6 months (P
conjunctival) fluorescein staining significantly improved from baseline to 6 months (P <
< 0.001) [23]. Patients also showed significant improvements from baseline in composite and visual function scores of the Ocular Surface Disease Index (OSDI; P
0.001) [23]. Patients also showed significant improvements from baseline in composite and visual function scores of the Ocular Surface Disease Index (OSDI; P ≤
≤ 0.041), Schirmer’s test scores (P
0.041), Schirmer’s test scores (P =
= 0.010), and tear film break-up time (P
0.010), and tear film break-up time (P <
< 0.001), and reported significant improvement in ocular discomfort and dry eye symptoms (P
0.001), and reported significant improvement in ocular discomfort and dry eye symptoms (P <
< 0.001) [23]. After 6 months of treatment with CsA 0.05%, 35.1% and 18.9% of patients achieved at least 5 mm or at least 10 mm improvement in the average eye Schirmer score, respectively, compared to baseline [23].
0.001) [23]. After 6 months of treatment with CsA 0.05%, 35.1% and 18.9% of patients achieved at least 5 mm or at least 10 mm improvement in the average eye Schirmer score, respectively, compared to baseline [23].
Safety
Clinical studies found few adverse effects (AEs) reported with the use of CsA 0.05% and no severe topical or systemic adverse safety findings [21–23]. Over 6 months of treatment in the open-label, phase 4 study, one patient (2.5%) reported one systemic AE (headache) considered treatment-related [23]. Overall, CsA 0.05% was well tolerated by patients. In one study, 1.7% of patients discontinued CsA 0.05% treatment because of ocular burning and stinging [22] (Table 3). The most commonly reported treatment-emergent AEs (TEAEs) with use of CsA 0.05% were instillation site burning and stinging [22, 23] (Table 4). Ocular burning, ocular stinging/pain, and ocular discharge were reported in 14.7%, 3.4%, and 3.1% of CsA 0.05% patients and 6.5%, 1.4%, and 2.4% of vehicle patients, respectively [22]. Generally, CsA 0.05% had a higher rate of most TEAEs compared to the vehicle; however, an exception was visual disturbance, which occurred in 1.7% and 4.1% of CsA 0.05% and vehicle patients, respectively [22]. Most TEAEs in the CsA 0.05% pivotal trials were mild to moderate.
Table 3
Adverse events leading to treatment discontinuation
| Study | Treatment | Adverse event | Treatment n (%) | Comparator n (%) |
|---|---|---|---|---|
| Sall et al. (2000) [22] | CsA 0.05% | Any TEAE | 19 (6.5) | 13 (4.5) |
| Burning and stinging | 5 (1.7) | 5 (1.7) | ||
| Stevenson et al. (2000) [21] | CsA 0.05% | Any ocular TEAE | 0 | 2 (6.0) |
| Stonecipher et al. (2016) [23] | CsA 0.05% | Any non-ocular TEAE | 2 (5.0) | NA |
| Baudouin et al. (2017) [28] | CsA CE | Any ocular TEAE | 24 (9.9) | 18 (7.2) |
| Baudouin et al. (2017) [29] | CsA CE | Any TEAE | 21 (13.6)* 10 (7.8)† | 9 (10.0)* |
| Any ocular TEAE | 18 (11.7)* 9 (7.0)† | 6 (6.7)* | ||
| Treatment-related TEAE | 16 (10.4)* 8 (6.3)† | 5 (5.6)* | ||
| Instillation site pain | 5 (3.9)† | |||
| Goldberg et al. (2019) [36] | OTX-101 | Instillation site pain | 9 (2.4) | 0 |
| Sheppard et al. (2021) [40] | OTX-101 | Any TEAE | 25 (9.7) | NA |
| Smyth-Medina et al. (2019) [38] | OTX-101 | Any TEAE | 15 (2.9) | 5 (1.0) |
| Tauber et al. (2018) [35] | OTX-101 | Any TEAE | 5 (3.3) | 6 (3.9) |
| Donnenfeld et al. (2016) [52] | Lifitegrast | Any TEAE | 27 (12.3) | 10 (9.0) |
| Any ocular TEAE | 18 (8.2) | 6 (5.4) | ||
| Instillation site reaction | 4 (1.8) | 0 | ||
| Lacrimation increased | 3 (1.4) | 1 (0.9) | ||
| Visual acuity reduced | 3 (1.4) | 0 | ||
| Instillation site irritation | 2 (0.9) | 2 (1.8) | ||
| Vision blurred | 2 (0.9) | 1 (0.9) | ||
| Instillation site pain | 2 (0.9) | 1 (0.9) | ||
| Any non-ocular TEAE | 9 (4.1) | 4 (3.6) | ||
| Dysgeusia | 4 (1.8) | 0 | ||
| Holland et al. (2017) [49] | Lifitegrast | Any TEAE | 21 (5.9) | 9 (2.5) |
| Any ocular TEAE | 17 (4.8) | 6 (1.7) | ||
| Instillation site reaction | 5 (1.4) | 2 (0.6) | ||
| Instillation site irritation | 4 (1.1) | 0 | ||
| Any non-ocular TEAE | 6 (1.7) | 3 (0.8) | ||
| Nichols et al. (2018) [53] | Lifitegrast | Instillation site reaction | 5 (1.4) | 2 (0.6) |
| Instillation site irritation | 4 (1.1) | 0 | ||
| Nichols et al. (2019) [54] | Lifitegrast | Any TEAE | 90 (7.0) | 31 (2.6) |
| Any ocular TEAE | 71 (5.5) | 18 (1.5) | ||
| Instillation site pain | 8 (0.6) | 1 (0.1) | ||
| Instillation site irritation | 13 (1.0) | 2 (0.2) | ||
| Instillation site reaction | 12 (0.9) | 2 (0.2) | ||
| Any non-ocular TEAE | 24 (1.9) | 13 (1.1) | ||
| Dysgeusia | 6 (0.5) | 0 | ||
| Semba et al. (2012) [48] | Lifitegrast | Any TEAE | 6 (10.3) | 1 (1.7) |
| Tauber et al. (2015) [47] | Lifitegrast | Any TEAE | 26 (7.2) | 3 (0.8) |
| Any ocular TEAE | 23 (6.4) | 2 (0.6) | ||
| Any non-ocular TEAE | 6 (1.7) | 1 (0.3) |
CsA 0.05% cyclosporine ophthalmic emulsion 0.05%, CsA CE 0.1% (1 mg/mL) cyclosporine A cationic emulsion, TEAE treatment-emergent adverse event, NA not applicable, OTX-101 cyclosporine ophthalmic solution 0.09%
*Part 1, 0–6 months of treatment
†Part 2, 6–12 months of CsA CE
Table 4
Summary of the most common (occurring in more than 5% of patients) TEAEs
| Study | Treatment | Adverse event | Treatment, n (%) | Vehicle, n (%) |
|---|---|---|---|---|
| Sall et al. (2000)§ [22] | CsA 0.05% | Burning eye | 43 (14.7) | 19 (6.5) |
| Stonecipher et al. (2016) [23] | CsA 0.05% | Instillation site burn | 3 (7.5) | NA |
| Instillation site pain | 3 (7.5) | |||
| Eye irritation | 2 (5.0) | |||
| Baudouin et al. (2017)* [28] | Eye irritation | 39 (16.1) | 6 (2.4) | |
| CsA CE | Instillation site irritation | 22 (9.1) | 4 (1.6) | |
| Eye pain | 17 (7.0) | 7 (2.8) | ||
| Baudouin et al. (2017)*† [29] | CsA CE | Instillation site pain | 10 (7.8) | NA |
| Leonardi et al. (2016)* [27] | CsA CE | Instillation site pain | 45 (29.2) | 8.1 (8.9) |
| Goldberg et al. 2019 [36] | OTX-101 0.09% | Instillation site pain | 90 (24.2) | 16 (4.3) |
| Conjunctival hyperaemia | 30 (8.1) | 19 (5.1) | ||
| Karpecki et al. (2019)* | OTX-101 0.09% | Eye irritation | 1 (6.2) | NA |
| Eye pain | 1 (6.2) | |||
| Eye pruritis | 1 (6.2) | |||
| Malhotra et al. (2019) [37] | OTX-101 0.09% | Instillation site pain | 114 (21.8) | 21 (4.0) |
| Conjunctival hyperaemia | 30 (5.7) | 19 (3.6) | ||
| Sheppard et al. (2020) [39] | OTX-101 0.09% | Instillation site pain | 114 (21.8) | 21 (4.0) |
| Conjunctival hyperaemia | 30 (5.7) | 19 (3.6) | ||
| Sheppard et al. (2021) [40] | OTX-101 0.09% | Instillation site pain | 59 (22.9) | NA |
| Conjunctival hyperaemia | 26 (10.1) | |||
| Punctate keratitis | 16 (6.2) | |||
| Smyth-Medina et al. (2019) [38] | OTX-101 0.09% | Instillation site pain | 114 (21.8) | 21 (4.0) |
| Conjunctival hyperaemia | 30 (5.7) | 19 (3.6) | ||
| Tauber et al. (2018) [35] | OTX-101 0.09% | Instillation site pain | 23 (15.1) | 5 (3.3) |
| Donnenfeld et al. (2016) [52] | Lifitegrast | Dysgeusia | 36 (16.4) | 2 (1.8) |
| Instillation site irritation (burning) | 33 (15.0) | 5 (4.5) | ||
| Instillation site reaction | 29 (13.2) | 2 (1.8) | ||
| Visual acuity reduced | 25 (11.4) | 7 (6.3) | ||
| Dry eye | 4 (1.8) | 6 (5.4) | ||
| Holland et al. (2017) [49] | Lifitegrast | Instillation site irritation | 65 (18.2) | 11 (3.1) |
| Dysgeusia | 46 (12.9) | 1 (0.3) | ||
| Instillation site reaction | 45 (12.6) | 19 (5.4) | ||
| Nichols et al. (2018) [53] | Lifitegrast | Instillation site irritation | 4.7 (18.2) | 0.5 (3.1) |
| Instillation site reaction | 3.3 (12.6) | 0.9 (5.4) | ||
| Nichols et al. (2019) [54] | Lifitegrast | Instillation site irritation | 195 (15.2) | 33 (2.8) |
| Dysgeusia | 186 (14.5) | 4 (0.3) | ||
| Instillation site reaction | 158 (12.3) | 27 (2.3) | ||
| Instillation site pain | 126 (9.8) | 25 (2.1) | ||
| Semba et al. (2012) [48] | Lifitegrast | Any instillation site condition¶ | 35 (60.3) | 9 (15.5) |
| Conjunctival haemorrhage | 3 (5.2) | 0 | ||
| Sheppard et al. (2014) [46] | Lifitegrast | Instillation site irritation | 69 (24.0) | 12 (4.0) |
| Instillation site pain | 63 (22.0) | 11 (4.0) | ||
| Instillation site reaction | 50 (17.0) | 2 (1.0) | ||
| Instillation site pruritis | 19 (7.0) | 6 (2.0) | ||
| Tauber et al. (2015) [47] | Lifitegrast | Dysgeusia | 58 (16.2) | 1 (0.3) |
| Instillation site irritation | 28 (7.8) | 5 (1.4) | ||
| Instillation site reaction | 25 (7.0) | 4 (1.1) | ||
| Reduced visual acuity | 18 (5.0) | 23 (6.4) |
CsA 0.05% cyclosporine ophthalmic emulsion 0.05%, CsA CE 0.1% (1 mg/mL) cyclosporine A cationic emulsion, N/A not applicable, TEAE treatment-emergent adverse event, OTX-101 cyclosporine ophthalmic solution 0.09%
*Noted as treatment-related TEAEs
†Part 2 of study
§TEAEs listed occurred cyclosporine groups combined
¶Includes all adverse events at the site of treatment administration (e.g. discomfort, irritation, pain)
Findings from these pivotal trials demonstrated significant improvements in ocular signs and symptoms of moderate-to-severe DED with few AEs, indicating a favourable risk–benefit profile for CsA 0.05%. Improvements in objective measures, such as corneal staining and Schirmer’s tear test scores, in addition to subjective measures like blurred vision and the use of artificial tears, suggest that treatment with CsA 0.05% improves the underlying pathophysiology of DED. While effective in managing DED signs and symptoms, CsA 0.05% is accompanied by a higher rate of most TEAEs compared to using the vehicle, although few of these led to treatment discontinuation. The results from these three clinical trials demonstrate that the clinical benefit of CsA 0.05% is accompanied by minimal patient risk.
CsA CE 0.1%
In 2015, CsA CE became the first topical CsA treatment for patients with DED available in Europe [19]. In contrast to the anionic emulsion CsA 0.05%, CsA CE is a cationic nanoemulsion of CsA 0.1%. Encapsulation of CsA in a CE creates a net positive charge of the oil nanodroplets, which may improve the residence time and the ocular bioavailability of CsA compared to other formulations [24, 25].
Preclinical Studies
Preclinical studies provide valuable information relating to the efficacy and mechanism of action of DED treatments. In an in vitro dry eye model, human corneal epithelial cells were subjected to desiccation stress and then treated with CsA 0.05% 1:50, CsA CE 1:50, CsA CE 1:100, or control (Table 1). Cellular inflammation was evaluated through production of the inflammatory cytokine tumour necrosis factor alpha (TNFα), the phosphorylated proinflammatory factors nuclear factor kappa B (NF-κB) and inhibitor of kappa B alpha (IκBα), and activation of the NF-κB/IκBα pathway. Apoptotic effects were determined through quantification of the proapoptotic protein, Bax, and the antiapoptotic protein, B cell lymphoma-extra large. Levels of the cell proliferation and survival factors phosphorylated extracellular signal-regulated kinase 1/2 and phosphorylated protein kinase B were quantified to investigate cell survival [26].
CsA CE 1:50 and 1:100 had dose-dependent and more potent anti-inflammatory and antiapoptotic effects than CsA 0.05% [26]. Additionally, CsA CE 1:50 decreased cellular levels of inflammatory factors (P <
< 0.05) while increasing expression of antiapoptotic factors compared to CsA 0.05%-treated and untreated cells (P
0.05) while increasing expression of antiapoptotic factors compared to CsA 0.05%-treated and untreated cells (P <
< 0.05). Cell proliferation and survival factors were significantly increased in CsA CE-treated cells compared to CsA 0.05%-treated and untreated cells (P
0.05). Cell proliferation and survival factors were significantly increased in CsA CE-treated cells compared to CsA 0.05%-treated and untreated cells (P <
< 0.05); there was no significant difference in these factors when cells were treated with CsA 0.05% or the control [26]. These preclinical findings suggest that CsA CE may provide improved anti-inflammatory benefits compared to CsA 0.05% treatment. Comparative clinical studies are needed to confirm these preclinical findings.
0.05); there was no significant difference in these factors when cells were treated with CsA 0.05% or the control [26]. These preclinical findings suggest that CsA CE may provide improved anti-inflammatory benefits compared to CsA 0.05% treatment. Comparative clinical studies are needed to confirm these preclinical findings.
Clinical Pivotal Trials
Efficacy
Two clinical pivotal trials investigated the efficacy of CsA CE 0.1% (Table 1). The phase 3 SANSIKA study in patients with severe DED had two parts—a vehicle-controlled, double-masked 6-month phase where patients were randomised to CsA CE 0.1% or vehicle, followed by a 6-month, open-label extension (OLE) where all patients received CsA CE 0.1% [27, 28]. Treatment with once daily (QD) CsA CE 0.1% for 6 months led to significantly greater improvements in corneal damage and ocular surface inflammation compared to vehicle (Table 2) [27]. Both vehicle- and CsA CE 0.1%-treated patients demonstrated improved corneal fluorescein staining (CFS) scores over 6 months, but treatment with CsA CE 0.1% resulted in a significantly greater decrease from baseline than vehicle after 3 months of treatment and was sustained through 6 months of treatment (P =
= 0.024 and P
0.024 and P =
= 0.037, respectively). Ocular surface inflammation was assessed by human leukocyte antigen DR (HLA-DR) expression; CsA CE demonstrated significantly decreased HLA-DR expression at 1- and 6-month time points (Table 2) [27].
0.037, respectively). Ocular surface inflammation was assessed by human leukocyte antigen DR (HLA-DR) expression; CsA CE demonstrated significantly decreased HLA-DR expression at 1- and 6-month time points (Table 2) [27].
Despite the significant differences between CsA CE 0.1% and vehicle in clinical signs of DED in the SANSIKA double-masked comparative study period, both treatments demonstrated substantial improvements in DED symptoms from baseline to 6 months with no significant difference between treatments [27]. Adjusted mean change in OSDI score from baseline to month 6 (95% confidence interval) was − 13.6 (−
13.6 (− 17.0,
17.0, −
− 10.0) and
10.0) and −
− 14.1 (−
14.1 (− 18.6,
18.6, −
− 9.5) for CsA CE 0.1% and vehicle, respectively (P
9.5) for CsA CE 0.1% and vehicle, respectively (P =
= 0.858). This emphasises that the vehicle for CsA CE, an unpreserved cationic oil-in-water nanoemulsion, may have the ability to improve DED symptoms on its own.
0.858). This emphasises that the vehicle for CsA CE, an unpreserved cationic oil-in-water nanoemulsion, may have the ability to improve DED symptoms on its own.
Efficacy results from the OLE phase of the SANSIKA study reiterated the findings from the 6-month, double-masked, comparative phase. Corneal fluorescein staining scores continued to improve while reductions in HLA-DR expression were primarily maintained in patients who received CsA CE 0.1% throughout the comparative and OLE phases. Patients who received vehicle during the comparative phase and then received CsA CE 0.1% in the OLE phase exhibited improved mean (± standard deviation [SD]) CFS scores from month 6 to 12 (2.5
standard deviation [SD]) CFS scores from month 6 to 12 (2.5 ±
± 1.1 vs 2.0
1.1 vs 2.0 ±
± 1.3, respectively) and similarly reduced median HLA-DR levels from month 6 to 12 (76,062 vs 57,728 arbitrary units of fluorescence, respectively). These findings emphasise the benefit of the active component of CsA CE 0.1% [28].
1.3, respectively) and similarly reduced median HLA-DR levels from month 6 to 12 (76,062 vs 57,728 arbitrary units of fluorescence, respectively). These findings emphasise the benefit of the active component of CsA CE 0.1% [28].
The randomised, double-masked SICCANOVE study compared the efficacy of CsA CE 0.1% to vehicle in patients with moderate-to-severe DED over 6 months of treatment (Table 1) [29]. After 1 month of treatment, patients receiving CsA CE 0.1% demonstrated significantly greater improvements in mean CFS change from baseline (CFB) than the vehicle group; this improvement was sustained through 6 months of treatment (Table 2). As in SANSIKA, both CsA CE 0.1% and vehicle groups in SICCANOVE had notable improvements in the coprimary symptom efficacy endpoint, mean change (± SD) in global ocular discomfort (visual analogue scale [VAS]) score, from baseline to 6 months with no significant difference between groups (−
SD) in global ocular discomfort (visual analogue scale [VAS]) score, from baseline to 6 months with no significant difference between groups (− 12.82
12.82 ±
± 18.59 vs
18.59 vs −
− 11.21
11.21 ±
± 19.34, respectively; P
19.34, respectively; P =
= 0.808) [29]. However, at month 6, significantly more patients in the CsA CE group vs vehicle had at least a 25% improvement in global VAS score (50.2% vs 42.0%, P
0.808) [29]. However, at month 6, significantly more patients in the CsA CE group vs vehicle had at least a 25% improvement in global VAS score (50.2% vs 42.0%, P =
= 0.048), indicating a greater number of patients with a clinically relevant reduction in ocular discomfort [29].
0.048), indicating a greater number of patients with a clinically relevant reduction in ocular discomfort [29].
Safety
Safety analyses in the SICCANOVE and SANSIKA studies demonstrated that CsA CE 0.1% was well tolerated by patients and the safety profile was as expected on the basis of other CsA formulations. Most TEAEs were mild or moderate; numerically higher incidence of severe ocular TEAEs was observed with patients using CsA CE 0.1% compared to vehicle [27, 29]. In SICCANOVE, 38.0% of CsA CE 0.1% patients reported an ocular treatment-related AE after 6 months of treatment, whereas 16.4% of vehicle patients reported treatment-related AEs [29]. Eye irritation and eye pain were the most common TEAEs in the CsA CE 0.1% and vehicle groups, respectively (Table 4). In SANSIKA, during the 6-month comparative phase, treatment-related AEs were reported by 37.0% and 21.1% of CsA CE 0.1% and vehicle patients, respectively [27]. In patients who continued on CsA CE 0.1% for the OLE phase, 14.8% reported treatment-related AEs through 6 and 12 months [28]. Instillation site pain was the most frequently reported treatment-related ocular AE in SANSIKA for both groups in the comparative and OLE study periods (Table 4) [27, 28]. Overall, 6.7–11.7% of all patients in SICCANOVE and SANSIKA discontinued because of ocular TEAEs, with patients receiving CsA CE 0.1% having slightly higher discontinuation rates (Table 3).
Baudouin et al. measured systemic CsA levels in a subset of 85 CsA CE patients in SICCANOVE; four patients had quantifiable, albeit negligible systemic CsA levels [29]. Similarly in SANSIKA, most systemic CsA levels were not detectable or, if measurable, were deemed negligible [27, 28].
The risk–benefit profile of CsA CE 0.1% is consistent with other CsA-based treatments. The SICCANOVE and SANSIKA studies established the clinical benefit of CsA CE compared to vehicle for the treatment of clinical signs of DED. Improvements in DED symptoms are observed with CsA CE 0.1%, but no significant improvement was found over treatment with vehicle [27–29]. As expected, patients receiving CsA CE 0.1% typically reported more TEAEs than patients using vehicle only (Table 4) [27, 29]. However, despite a higher incidence of TEAEs in CsA CE 0.1%-treated patients, the percentage of patients who discontinued treatment because of an ocular TEAE is relatively comparable between CsA CE 0.1% (9.9%) and vehicle-treated (7.2%) groups (Table 3) [29]. This highlights the favourable risk–benefit profile of CsA CE 0.1%.
CsA 0.09% Solution
The clear, aqueous, nanomicellar CsA 0.09% solution, OTX-101, was approved in the USA in 2018 to increase tear production in patients with DED and is designed to provide high CsA delivery to target ocular tissues [30]. Ocular delivery of CsA is enhanced as the novel formulation optimises the encapsulation of CsA in the micelle core through hydrophobic interaction [30, 31]. Improved bioavailability in ocular tissues may affect duration of efficacy, which patients report to influence their satisfaction [32].
Preclinical Studies
A preclinical study in New Zealand white rabbits evaluated the ocular distribution, tolerability, and systemic exposure of CsA after administration of OTX-101 as a single dose and a repeated dose instilled four times per day for 7 days; multiple doses of OTX-101 (0.01%, 0.05%, 0.1%) were compared to CsA 0.05% (Table 1) [33]. OTX-101 approximately doubled the CsA concentration in the conjunctiva and cornea after a single (OTX-101 0.05%) or repeat (OTX-101 0.05% and OTX-101 0.1%) dose compared with CsA 0.05% [33]. Even with the demonstrated ocular tissue CsA concentrations with OTX-101, no signs of toxicity were found. However, there was notable accumulation in ocular tissues with both CsA 0.05% and OTX-101 in the repeated dose phase, which suggests a dose regimen of four times per day may be excessive and could increase likelihood of toxicity development.
A head-to-head study in NOD.B10.H2b mice compared the efficacy of OTX-101 0.09% (administered QD or BID), CsA 0.05% BID, and CsA CE 0.1% QD (Table 1) [33, 34]. Efficacy assessments included tear volume, corneal staining, conjunctival goblet cell density, and interleukin-1β cytokine levels. Over 60 days of treatment, OTX-101 0.09% BID significantly increased tear volume compared with CsA 0.05% on day 30, 45, and 60 (P <
< 0.05, P
0.05, P <
< 0.001, and P
0.001, and P <
< 0.001, respectively) and CsA CE 0.1% on day 60 (P
0.001, respectively) and CsA CE 0.1% on day 60 (P <
< 0.05) [34]. Mice treated with OTX-101 0.09% BID also had significantly higher goblet cell density compared to the placebo and untreated diseased control groups, emphasising that OTX-101 improves ocular surface hydration [34]. Overall, OTX-101 BID had greater increases in tear volume and goblet cell density compared to CsA 0.05% and CsA CE treatments, supporting the efficacy of OTX-101 0.09% BID in treating patients with DED. There were no statistical differences observed between treatment groups for corneal staining or interleukin-1β cytokine levels [34].
0.05) [34]. Mice treated with OTX-101 0.09% BID also had significantly higher goblet cell density compared to the placebo and untreated diseased control groups, emphasising that OTX-101 improves ocular surface hydration [34]. Overall, OTX-101 BID had greater increases in tear volume and goblet cell density compared to CsA 0.05% and CsA CE treatments, supporting the efficacy of OTX-101 0.09% BID in treating patients with DED. There were no statistical differences observed between treatment groups for corneal staining or interleukin-1β cytokine levels [34].
Clinical Pivotal Trials
Efficacy
Numerous pivotal clinical trials investigated the efficacy of OTX-101 0.09% in the treatment of patients with DED. These studies include a phase 2b/3 dose-ranging and phase 3 trials on the safety and efficacy of OTX-101 [35, 36]. Further analyses have been conducted in pooled data from the OTX-101 phase 2b/3 and phase 3 trials [37–39]. Lastly, a phase 3 worse-eye efficacy analysis and a 1-year OLE evaluated long-term safety of OTX-101 in patients with DED [40]. Study design details are presented in Table 1.
The phase 2b/3 study evaluated the efficacy of two concentrations of OTX-101, 0.05% and 0.09%, compared to its vehicle over 84 days [35]. Efficacy assessments included both ocular signs and symptoms. Both OTX-101 groups demonstrated significant improvement at day 84 in mean CFB in total conjunctival lissamine green staining scores, CFS scores, and Schirmer's test scores compared to vehicle (Table 2) [35]. Patient-reported symptoms assessing the frequency and severity of dryness and/or irritation (modified “symptom assessment in dry eye” [SANDE] questionnaire) improved in both vehicle and OTX-101 groups by approximately 30%; there were no significant differences between groups [35]. Results from this study led to the decision to advance OTX-101 0.09% for further clinical development [35].
Results from the OTX-101 0.09% pivotal phase 3 trial built upon the phase 2b/3 results. Assessments included CFS, conjunctival lissamine staining, modified SANDE scores, and the percentage of eyes with a clinically meaningful improvement (increase of at least 10 mm) in Schirmer’s test score after treatment for 84 days [36]. A significantly greater proportion of eyes treated with OTX-101 0.09% achieved an increase of at least 10 mm in the Schirmer’s test score at day 84 (16.6% vs 9.2%), indicating a significant increase in tear production compared to vehicle (P <
< 0.001) (Table 2). The OTX-101 0.09%-treated eyes also demonstrated significantly improved CFS compared to vehicle (P
0.001) (Table 2). The OTX-101 0.09%-treated eyes also demonstrated significantly improved CFS compared to vehicle (P <
< 0.01) at days 28, 56, and 84 and significantly improved conjunctival staining compared to vehicle (P
0.01) at days 28, 56, and 84 and significantly improved conjunctival staining compared to vehicle (P <
< 0.001) at days 56 and 84 (P
0.001) at days 56 and 84 (P =
= 0.007) (Table 2) [36]. Lastly, a significantly larger percentage of eyes treated with OTX-101 0.09% demonstrated clear central corneas compared with the vehicle group; this difference emerged by day 28 (P
0.007) (Table 2) [36]. Lastly, a significantly larger percentage of eyes treated with OTX-101 0.09% demonstrated clear central corneas compared with the vehicle group; this difference emerged by day 28 (P =
= 0.04) of treatment and lasted throughout day 84 (P
0.04) of treatment and lasted throughout day 84 (P =
= 0.02) [36].
0.02) [36].
Analysis of the worse eye (defined for Schirmer’s test and conjunctival staining assessments as the eye with lower baseline Schirmer’s score and for CFS assessments as the eye with lower baseline CFS score) further confirmed the efficacy of OTX-101 0.09% for improving objective signs of DED [40]. Treatment with OTX-101 0.09% significantly improved the percentage of eyes with complete corneal clearing and total conjunctival staining as early as week 4 (P =
= 0.010) and week 8 (P
0.010) and week 8 (P <
< 0.001) compared to vehicle, respectively (Table 2) [40].
0.001) compared to vehicle, respectively (Table 2) [40].
In pooled phase 2b/3 and 3 analyses, OTX-101 0.09% improved total corneal staining, and therefore corneal surface integrity, after only 4 weeks of treatment, and this improvement was maintained throughout the study [37]. The individual zones of the cornea were also assessed; the central, inferior, lateral, and medial zones all had significantly improved corneal clearing with OTX-101 0.09% compared to vehicle (P =
= 0.001) at all time points, with the exception of the lateral zone on day 28 [37]. A significantly high correlation between reduced central corneal staining and improved visual acuity (VA) was found on day 84 (P
0.001) at all time points, with the exception of the lateral zone on day 28 [37]. A significantly high correlation between reduced central corneal staining and improved visual acuity (VA) was found on day 84 (P =
= 0.012) [37], which is important as impaired visual function is associated with central corneal epithelial damage in DED [41]. Another pooled analysis showed treatment with OTX-101 significantly improved total conjunctival staining compared with vehicle at 28 days and was maintained through 84 days (Table 2) [38]. Conjunctival staining in the inferior and superior zones at all time points and in the lateral zone on days 56 and 84 was also significantly reduced in eyes treated with OTX-101 compared with vehicle (Table 2) [38]. In a pooled analysis, significantly more eyes receiving OTX-101 had an increase in Schirmer’s score of at least 10 mm from baseline at day 84 in both the intent-to-treat population (P
0.012) [37], which is important as impaired visual function is associated with central corneal epithelial damage in DED [41]. Another pooled analysis showed treatment with OTX-101 significantly improved total conjunctival staining compared with vehicle at 28 days and was maintained through 84 days (Table 2) [38]. Conjunctival staining in the inferior and superior zones at all time points and in the lateral zone on days 56 and 84 was also significantly reduced in eyes treated with OTX-101 compared with vehicle (Table 2) [38]. In a pooled analysis, significantly more eyes receiving OTX-101 had an increase in Schirmer’s score of at least 10 mm from baseline at day 84 in both the intent-to-treat population (P <
< 0.0001) and a subgroup population of patients with an unanaesthetised Schirmer’s test score of less than 10 mm at baseline (P
0.0001) and a subgroup population of patients with an unanaesthetised Schirmer’s test score of less than 10 mm at baseline (P =
= 0.0001) (Table 2) [39]. Additionally, treatment with both OTX-101 and vehicle led to improved DED symptoms (SANDE scores) from baseline to day 84, but there was no difference in improvement between OTX-101 and vehicle (P
0.0001) (Table 2) [39]. Additionally, treatment with both OTX-101 and vehicle led to improved DED symptoms (SANDE scores) from baseline to day 84, but there was no difference in improvement between OTX-101 and vehicle (P =
= 0.354) [39].
0.354) [39].
Safety
Safety findings in the OTX-101 pivotal trials are consistent with the established safety and tolerability profiles of topical ophthalmic CsA. The phase 1 safety study showed systemic exposure to CsA was negligible in healthy participants after BID ocular administration of OTX-101 for 7 days and QD on day 8 [42]. Over the study period, three participants reported a total of three ocular TEAEs; all were mild and resolved without additional treatment (Table 4).
The majority of ocular AEs reported in the phase 2b/3 and phase 3 OTX-101 studies were mild to moderate [35, 36]. In the phase 2b/3 trial, four (2.6%) patients in the vehicle group reported a serious TEAE vs zero patients in the OTX-101 0.09% group. The most common TEAE in both the phase 2b/3 and phase 3 studies was instillation site pain, occurring more often in OTX-101-treated patients compared to vehicle (Table 4) [35, 36]. The number of patients who discontinued from either study was low (less than 4%) and similar between OTX-101 and vehicle groups (Table 3) [35, 36]. The percentage of patients discontinuing treatment because of TEAEs and the most common TEAEs are summarised in Table 3 and and44.
The 1-year OLE following the 12-week treatment phase from the OTX-101 phase 3 clinical trial is the longest follow-up of OTX-101 in patients with DED (Table 1). The safety and tolerability profile in the long-term safety phase was consistent with results from the 12-week treatment phase [40]. Patients most commonly reported instillation site pain (22.9%), followed by conjunctival hyperaemia (10.1%) and punctate keratitis (6.2%) (Table 4) [40]. Over the 1-year safety phase, 9.7% of patients discontinued treatment because of TEAEs (Table 3) [40]. These findings support the long-term tolerability of OTX-101 for the treatment of DED.
Overall, these numerous pivotal trials on the safety and efficacy of OTX-101 show a favourable risk–benefit profile. The clinical benefit of OTX-101 compared to vehicle has been thoroughly established, as it significantly improves objective signs of tear production, conjunctival staining, or corneal staining in patients with moderate-to-severe DED. OTX-101 also improved symptoms of DED, although it was not significant compared to vehicle [35, 36]. As consistent with other CsA-based treatments, more patients taking OTX-101 reported TEAEs compared to vehicle; however, most of these TEAEs were mild to moderate in severity and did not lead to treatment discontinuation [36–38].
Lifitegrast Ophthalmic Solution 5%
Lifitegrast, the small molecule LFA-1 antagonist formerly known as SAR 1118, was a first-in-class integrin anti-inflammatory specifically engineered for the treatment of DED. By inhibiting T cell adhesion to intercellular adhesion molecule 1 (ICAM-1), lifitegrast blocks the interaction between the integrin LFA antigen 1 and ICAM-1, thereby inhibiting the inflammatory cascade associated with DED [43, 44]. The US Food and Drug Administration approved lifitegrast in 2016 for the treatment of signs and symptoms of DED.
Preclinical Studies
The ocular distribution, pharmacokinetic (PK), and excretion profile of lifitegrast was investigated in two preclinical animal models examining the exposure of lifitegrast across anterior and posterior ocular tissues and in plasma of female pigmented rabbits, and the excretion profile of lifitegrast after topical administration in male and female Beagle dogs (Table 1) [45]. In the ocular distribution and PK rabbit study, two slightly different lifitegrast formulations were examined (formulations from phase 3 trials OPUS-1 and OPUS-2) (Table 1) [46, 47]. The distribution and exposure of lifitegrast was generally highest in the anterior segment tissues after 5 days BID of treatment. The highest lifitegrast concentrations were seen in the conjunctiva and cornea, the target tissues for DED treatment, and low concentrations were observed in posterior segment tissues [45]. There were no significant differences between the formulations in distribution and exposure in the plasma and ocular tissues. Rapid elimination of radiolabeled lifitegrast (14C-lifitegrast) was found in the Beagle study after intravenous or topical ophthalmic administration. Approximately 90% of elimination occurred in the first 48 h post intravenous dose, primarily through faecal excretion [45]. These findings suggest minimal metabolism of lifitegrast in vivo and that it reaches the intended ocular surface tissues for DED treatment; furthermore, off-target AEs are unlikely [45].
Clinical Pivotal Trials
Efficacy
One phase 2 and three phase 3 trials assessed the efficacy of lifitegrast (Table 1) [46–49]. Overall, lifitegrast significantly improved both the clinical signs and symptoms of DED compared to treatment with vehicle.
The phase 2 trial evaluated the therapeutic potential of LFA-1 inhibition by assessing the efficacy of 84 days of treatment with multiple lifitegrast concentrations (0.1%, 1.0%, 5.0%) compared to vehicle in patients with DED [48]. A dose-dependent reduction in the progression of corneal staining was observed, with lifitegrast 5.0% showing the greatest improvement in inferior corneal staining mean CFB compared to vehicle at day 84 (P =
= 0.021) [48]. Additionally, lifitegrast demonstrated symptomatic improvement of DED; a significantly greater percentage of patients treated with lifitegrast demonstrated improvement in the OSDI visual-related score at day 84 vs vehicle (50.0% vs 19.6%, P
0.021) [48]. Additionally, lifitegrast demonstrated symptomatic improvement of DED; a significantly greater percentage of patients treated with lifitegrast demonstrated improvement in the OSDI visual-related score at day 84 vs vehicle (50.0% vs 19.6%, P <
< 0.0001) (Table 2) [48].
0.0001) (Table 2) [48].
The OPUS-1 pivotal phase 3 trial further confirmed the therapeutic clinical responses of lifitegrast from the phase 2 study [46]. Lifitegrast significantly reduced CFS (regions: inferior, P =
= 0.001; superior, P
0.001; superior, P =
= 0.039; total, P
0.039; total, P =
= 0.015) and conjunctival lissamine staining (nasal and total regions) over 84 days of treatment (P
0.015) and conjunctival lissamine staining (nasal and total regions) over 84 days of treatment (P <
< 0.05) (Table 2) [46]. Significant improvements in conjunctival staining were observed as early as day 14 for both nasal (P
0.05) (Table 2) [46]. Significant improvements in conjunctival staining were observed as early as day 14 for both nasal (P =
= 0.002) and total (P
0.002) and total (P =
= 0.015) regions (Table 2). Additionally, lifitegrast significantly improved symptoms of ocular discomfort at day 84 (P
0.015) regions (Table 2). Additionally, lifitegrast significantly improved symptoms of ocular discomfort at day 84 (P =
= 0.027) and eye dryness at day 42 (P
0.027) and eye dryness at day 42 (P =
= 0.044) and day 84 (P
0.044) and day 84 (P =
= 0.029) compared with vehicle [46]. The OPUS-1 study demonstrated that lifitegrast reduced inflammatory changes of the ocular surface associated with DED as early as week 2 when administered BID over a 12-week treatment period [46].
0.029) compared with vehicle [46]. The OPUS-1 study demonstrated that lifitegrast reduced inflammatory changes of the ocular surface associated with DED as early as week 2 when administered BID over a 12-week treatment period [46].
A second confirmatory pivotal phase 3 study (OPUS-2) built on the OPUS-1 results but with some key differences, including not using a controlled adverse environment as a screening method, requiring a minimal threshold of disease severity at baseline, and requiring recent use of artificial tears [47]. In contrast to the OPUS-1 trial, there were no differences in inferior or total CFS or conjunctival lissamine staining between lifitegrast and vehicle groups. However, lifitegrast demonstrated significant improvement vs vehicle in symptoms of eye dryness score (P <
< 0.0001), ocular discomfort score (nominal P
0.0001), ocular discomfort score (nominal P =
= 0.001), and eye discomfort score (nominal P
0.001), and eye discomfort score (nominal P <
< 0.0001) [47].
0.0001) [47].
In the final phase 3 pivotal trial (OPUS-3) the primary efficacy end point was change from baseline to day 84 in eye dryness score [49]. Additional VAS items assessed included burning/stinging, itching, foreign body sensation, eye discomfort, photophobia, pain; ocular discomfort score was a secondary efficacy end point. Patients treated with lifitegrast experienced greater improvement in eye dryness than patients treated with vehicle at days 14, 42, and 84 (Table 2). Additionally, greater improvements for lifitegrast over vehicle at day 42 were seen in itching (nominal P =
= 0.032), foreign body sensations (nominal P
0.032), foreign body sensations (nominal P =
= 0.042), and eye discomfort (nominal P
0.042), and eye discomfort (nominal P =
= 0.005), but these differences were not apparent at day 84 [49].
0.005), but these differences were not apparent at day 84 [49].
A phase 4, open-label, 12-week study measured longitudinal changes in DED signs and symptoms [50]. Over 12 weeks of treatment, statistically significant reductions from baseline were observed for all DED symptoms (dryness, burning, foreign body sensation, pain, photophobia, itching, and blurred vision) at week 6 and 12 (P <
< 0.010) [50]. In contrast, no significant changes from baseline in clinical signs were noted at any time point over the 12-week treatment period. Therefore, this study adds to the body of literature demonstrating the efficacy of lifitegrast for treatment of DED symptoms.
0.010) [50]. In contrast, no significant changes from baseline in clinical signs were noted at any time point over the 12-week treatment period. Therefore, this study adds to the body of literature demonstrating the efficacy of lifitegrast for treatment of DED symptoms.
Safety
Numerous pivotal trials demonstrated that lifitegrast ophthalmic solution 5.0% is generally safe and well tolerated for the treatment of DED. Patients scheduled for vitrectomy participated in a phase 1b study, in which they received one of three lifitegrast concentrations (0.1%, 1.0%, or 5.0%) BID for 7 days (Table 1) [51]. In addition to AE monitoring, lifitegrast concentrations were measured in samples of aqueous and vitreous fluid. All AEs were mild and transient; no severe ocular or systemic AEs were reported. Patients receiving the 5.0% dose achieved pharmacologically relevant levels of lifitegrast in the aqueous humour, while lifitegrast was undetectable in vitreous fluid for all patients except one (1.0 ng/ml).
The phase 2 and phase 3 pivotal trials reiterated that lifitegrast was well tolerated with no reports of serious ocular TEAEs [46–49]. The most common (occurring in more than 5% of patients) TEAEs in these trials are summarised in Table 4. TEAEs rarely led to treatment discontinuation; however, more patients treated with lifitegrast discontinued treatment because of TEAEs compared to patients treated with vehicle (Table 3). The most common ocular TEAE that led to treatment discontinuation was consistently instillation site irritation [47, 49].
A 1-year safety trial (SONATA) further demonstrated the long-term safety and tolerability of lifitegrast compared with vehicle in patients with DED [52]. Over 12 months, no serious ocular TEAEs were reported. The rate of discontinuations due to any TEAE was 12.3% and 9.0% in lifitegrast and vehicle groups, respectively (Table 3). The most common ocular TEAE was instillation site irritation, reported in 15.0% and 4.5% of patients administered lifitegrast and vehicle, respectively [52]. The safety profile of lifitegrast in SONATA was consistent with the shorter-term pivotal trials; no new safety concerns were identified and no evidence of systemic toxicity was found in this 1-year study [52].
The OPUS-3 trial evaluated the ocular comfort of lifitegrast [53]. Drop comfort plays a large role in overall ocular tolerability of DED treatment and may not only affect patient treatment preference but also adherence and ultimately the effectiveness of treatment. The drop comfort score ([DCS]; scale, 0–10; 0 =
= very comfortable, 10
very comfortable, 10 =
= very uncomfortable) was assessed over 12 weeks of treatment with lifitegrast or vehicle. DCS was measured at each time point at 0, 1, 2, and 3 min post-instillation, and up to 15 min until DCS was at most 3 [53]. Over the first 3 min following administration, mean DCS for the vehicle group was lower than in the lifitegrast group. By 3 min, post-instillation, lifitegrast DCS improved and 64–66% of lifitegrast-treated patients had DCS less than 3 [53]. Notably, there were also consistent improvements in DCS over time, with mean DCS less than 3 achieved more rapidly across visits.
very uncomfortable) was assessed over 12 weeks of treatment with lifitegrast or vehicle. DCS was measured at each time point at 0, 1, 2, and 3 min post-instillation, and up to 15 min until DCS was at most 3 [53]. Over the first 3 min following administration, mean DCS for the vehicle group was lower than in the lifitegrast group. By 3 min, post-instillation, lifitegrast DCS improved and 64–66% of lifitegrast-treated patients had DCS less than 3 [53]. Notably, there were also consistent improvements in DCS over time, with mean DCS less than 3 achieved more rapidly across visits.
A pooled analysis of safety findings from the five clinical trials (phase 2, OPUS-1, OPUS-2, OPUS-3, and SONATA) furthermore established the favourable safety profile of lifitegrast for the treatment of DED [54]. This pooled analysis covered more than 2400 patients with DED, presenting an extremely comprehensive data set that characterised the safety and tolerability of lifitegrast (Table 1). The pooled analysis confirmed that across individual trials, lifitegrast BID appears to be safe and well tolerated [54]. Overall, treatment discontinuations due to TEAEs were low; however, the proportion of patients that discontinued in the lifitegrast group (7.0%) was higher than that in the vehicle group (2.6%) (Table 3). Although the most common ocular TEAEs (instillation site irritation, instillation site reaction, and instillation site pain) were reported more frequently in lifitegrast patients, less than 2% of patients discontinued treatment because of these TEAEs [54]. The most common non-ocular TEAE reported was dysgeusia (Table 4), which results from normal tear drainage through the nasolacrimal duct into the nose and oropharynx, but discontinuations due to dysgeusia were very low (Table 3) [54].
The comprehensive efficacy and safety data for lifitegrast show promising therapeutic benefit as a treatment for DED with low safety risk. Pivotal trials comparing lifitegrast treatment to treatment with vehicle demonstrate improved efficacy for treating symptoms of DED in patients with moderate-to-severe baseline disease [49]. Lifitegrast may improve clinical signs of DED as well; however, most of the evidence is in patients with mild-to-moderate DED [49]. As is common with topical ophthalmic treatments, more TEAEs are reported in lifitegrast patients compared to vehicle-treated; however, most TEAEs are mild to moderate in severity and few lead to treatment discontinuation. The long-term safety analysis confirms the lifitegrast safety profile is maintained over extended treatment duration [52].
Efficacy, Safety, and Tolerability of DED Treatments
While a surplus of data is available regarding the efficacy, safety, and tolerability of CsA 0.05%, CsA CE 0.1%, OTX-101 0.09%, and lifitegrast, comparative studies for DED treatments are lacking. Here we summarise primary efficacy and safety results across the treatments. Table 1 presents key differences in study design parameters and patient populations in the pivotal trials included in this review, which should be taken into consideration when comparing results from different studies. A summary of all statistically significant key efficacy findings for each treatment compared to its vehicle control is shown in Table 2.
Efficacy
Conjunctival Staining
Conjunctival staining is an objective sign of DED and correlates with disease severity [4]. Reduced conjunctival staining correlates with improved underlying ocular surface inflammation and likely improved ocular surface integrity [55, 56]. Mean CFB in conjunctival staining scores published in pivotal trials for CsA 0.05% [21], CsA CE [28], OTX-101 0.09% [35, 36, 38, 40], and lifitegrast [46, 47] are shown in Fig. 1.
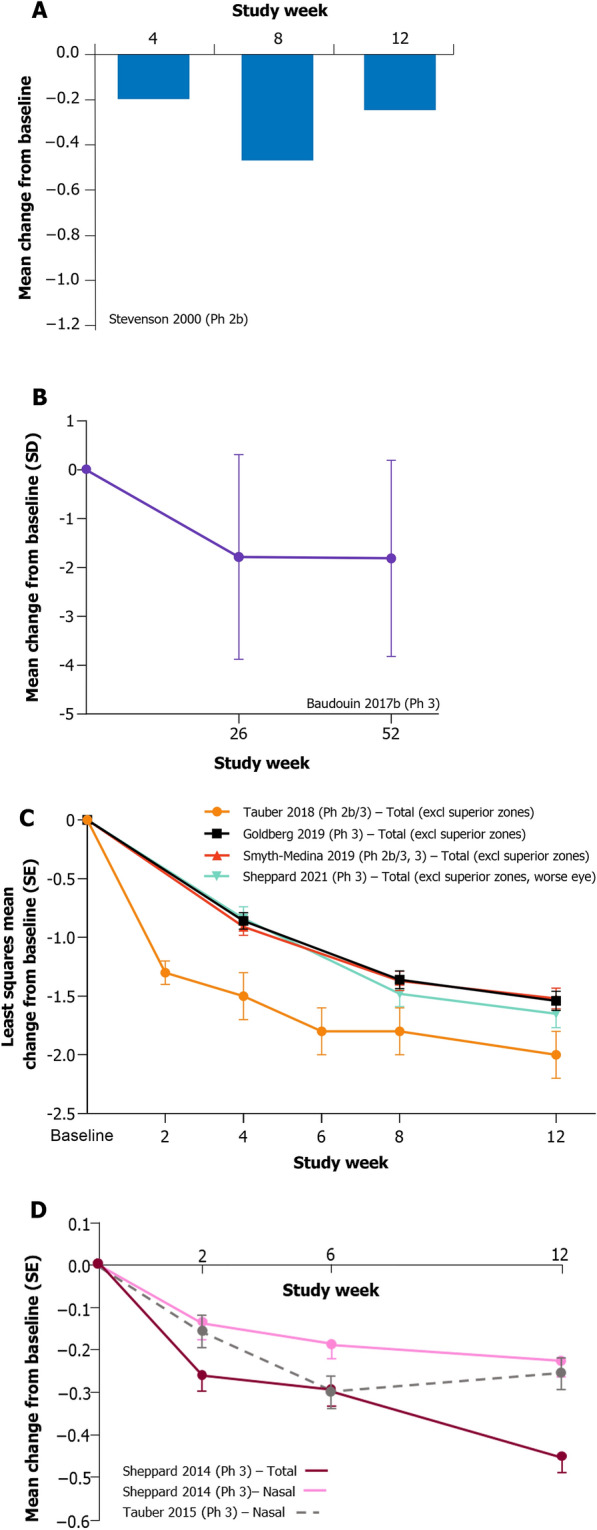
Change from baseline in conjunctival staining score with a CsA 0.05%, b CsA CE, c OTX-101 0.09%, and d lifitegrast treatments. CsA 0.05% cyclosporine ophthalmic emulsion 0.05%, CsA CE 0.1% (1 mg/mL) cyclosporine A cationic emulsion, lifitegrast lifitegrast ophthalmic solution 5.0%, OTX-101 cyclosporine ophthalmic solution 0.09%, Ph phase, SD standard deviation, SE standard error
All treatments improved conjunctival staining compared to baseline. Pivotal trials for CsA 0.05%, OTX-101 0.09%, and lifitegrast analysed conjunctival staining through 12 weeks of treatment, whereas CsA CE followed patients for 12 months and assessed conjunctival staining at 6 and 12 months. Over 12 weeks, patients treated with OTX-101 0.09% had the numerically largest improvements in conjunctival staining, followed by lifitegrast and CsA 0.05%, respectively. It should be noted that OTX-101 0.09% data is presented as least squares mean CFB, unlike the other studies that present mean CFB. While patients with DED receiving CsA CE for 12 months had substantial long-term improvements in mean (± SD) conjunctival staining at month 6 (−
SD) conjunctival staining at month 6 (− 1.8
1.8 ±
± 2.1) and month 12 (−
2.1) and month 12 (− 1.8
1.8 ±
± 2.0), there was a large amount of variability between patients, indicating that this improvement was not consistent for all CsA CE-treated patients [28].
2.0), there was a large amount of variability between patients, indicating that this improvement was not consistent for all CsA CE-treated patients [28].
Corneal Staining
Corneal fluorescein staining is used to quantify corneal surface damage [57]. Improvement in CFS may indicate an improvement in corneal surface integrity [57]. Mean CFB in corneal staining score in the pivotal trials for CsA 0.05% [22], OTX-101 0.09% [35, 37], and lifitegrast [46–48] are shown in Fig. 2. OTX-101 and lifitegrast studies presented staining in individual corneal zones in addition to total corneal staining.
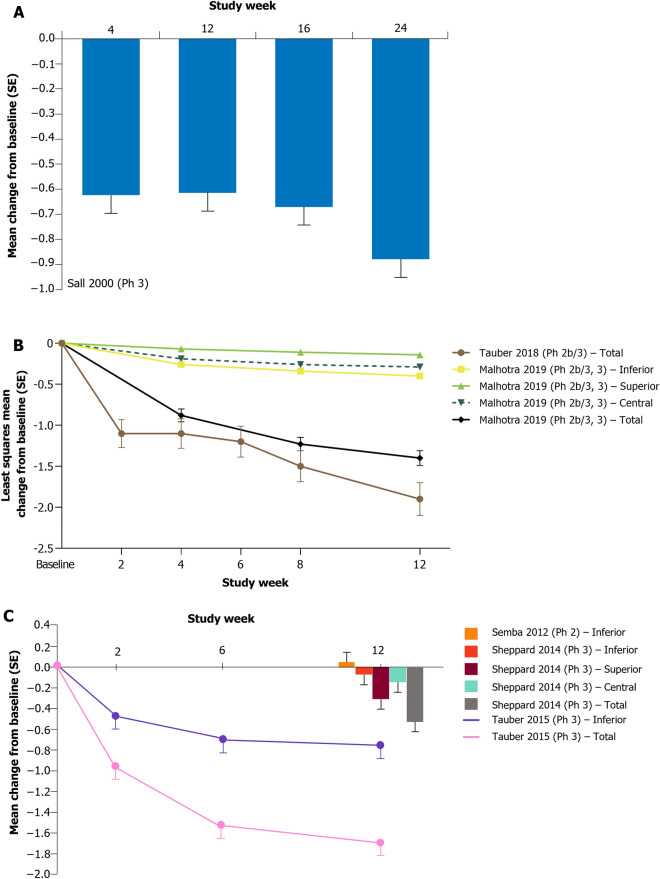
Change from baseline in corneal staining score with a CsA 0.05%, b OTX-101 0.09%, and c lifitegrast treatments. CsA 0.05% cyclosporine ophthalmic emulsion 0.05%, lifitegrast lifitegrast ophthalmic solution 5.0%, OTX-101 cyclosporine ophthalmic solution 0.09%, Ph phase, SE standard error
Treatment with CsA 0.05%, OTX-101 0.09%, and lifitegrast all showed improvement in CFS from baseline to the end of the study treatment. OTX-101 0.09% and lifitegrast were assessed over 12 weeks, while CsA 0.05% treatment was assessed over 24 weeks. Across the different pivotal trials, OTX-101 0.09% had the greatest numerical improvements in total CFS (least squares mean CFB), while lifitegrast showed a comparable level of improvement, followed by CsA 0.05%. The inferior zone demonstrated consistently improved staining across studies after 12 weeks of treatment with both OTX-101 0.09% and lifitegrast (Fig. 2) [37, 47]. Patients with DED receiving lifitegrast in OPUS-2 [47] had greater baseline disease severity (as assessed by baseline inferior CFS scores) compared to OPUS-1 [46], which may explain the greater improvement observed in OPUS-2.
Tear Production
Reduced quality or quantity of tears on the ocular surface as a result of DED may affect VA [58]. Schirmer’s tear test evaluates tear volume in DED. Mean CFB in Schirmer’s tear test scores for CsA 0.05% [22], CsA CE [27, 28], and OTX-101 [35, 39, 40] are shown in Fig. 3.
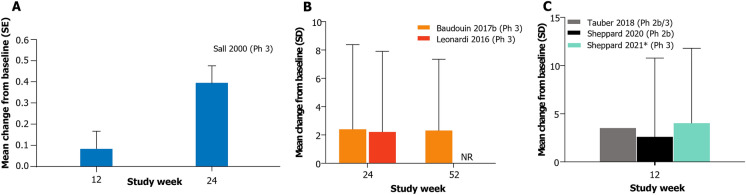
Change from baseline in Schirmer’s test score with a CsA 0.05%, b CsA CE, and c OTX-101 0.09%. *Worse eye analysis. CsA 0.05% cyclosporine ophthalmic emulsion 0.05%, CsA CE 0.1% (1 mg/mL) cyclosporine A cationic emulsion, NR not reported, OTX-101 cyclosporine ophthalmic solution 0.09%, Ph phase, SD standard deviation, SE standard error
Tear production often improved in patients with DED where it was assessed. Patients treated with OTX-101 demonstrated large numerical improvements in Schirmer’s test score mean CFB, followed by CsA CE and CsA 0.05%, respectively. However, both OTX-101 and CsA CE treatments were associated with large variability across patients in Schirmer’s test score mean CFB.
The percentage of eyes with an increase in Schirmer’s scores of at least 5 mm and at least 10 mm were reported for both OTX-101 and CsA 0.05% [23, 39]. In patients treated with OTX-101 for 3 months, the percentages of eyes with an increase in Schirmer’s score of at least 5 mm and at least 10 mm from baseline were 28.1% and 16.6%, respectively [39]. After 6 months of treatment with CsA 0.05%, 35.1% of patients achieved at least 5 mm improvement in Schirmer’s score and 18.9% of patients achieved at least 10 mm improvement in the Schirmer’s score [23].
Symptoms of Dry Eye Disease
Treatment with lifitegrast demonstrated superior symptomatic DED improvement compared to vehicle. Lifitegrast significantly improved symptoms of eye dryness compared to vehicle in the OPUS-1, OPUS-2, and OPUS-3 trials, although it was not a primary symptom endpoint in OPUS-1 [46, 47, 53]. Patients treated with CsA 0.05%, CsA CE, and OTX-101 improved symptom scores relative to baseline, but these treatments did not consistently provide improved benefit over their respective vehicle. This finding may suggest that the vehicles for CsA-based treatments may have the ability to improve DED symptoms on their own, whereas the lifitegrast vehicle is less effective without the active treatment component. Therapies that successfully treat both DED signs and symptoms will provide the largest benefit to patients for both short- and long-term treatment. The poor correlation between objectively measured signs and patient-reported symptoms may be in part due to a lack of repeatable clinical tests, variability in patient populations, fluctuations in the disease process itself, seasonality, and the subjective nature of symptom scores [58].
Safety and Tolerability
Overall, all pharmacologic DED treatments were generally well tolerated by patients. The majority of AEs for all treatments in this review were mild or moderate and no long-term safety concerns were noted. While data show that patients who use ophthalmic treatments more frequently experience TEAEs than those treated with a vehicle, TEAEs leading to treatment discontinuation are typically infrequent (Table 3). The percentage of patients discontinuing treatment because of an ocular TEAE ranged between 5% and 10% and was comparable across treatments.
Ocular tolerability may ultimately influence the effectiveness of prescribed ophthalmic treatments. The API in these treatments, which enables the treatment benefit, may be accompanied by mild-to-moderate ocular discomfort, most frequently reported at the instillation site (Table 4). Instillation site pain was the most common TEAE in patients treated with CsA CE and OTX-101; the range of the percentage of patients reporting instillation site pain was 7.8–29.2% for CsA CE and 15.1–24.2% for OTX-101. The most common TEAE in CsA 0.05%-treated patients was burning eye, reported in 14.7% of patients. In patients treated with lifitegrast, instillation site irritation was the most common TEAE, ranging from 7.8% to 24.0% of patients. Although non-ocular, dysgeusia is a unique TEAE reported by patients using lifitegrast.
Overall, clinical data show a favourable risk–benefit profile for the use of targeted topical anti-inflammatory pharmacologic treatments in patients with DED. While a substantial proportion of patients with DED treated with these agents experience ocular TEAEs, the rate of treatment discontinuation is relatively low. As assessed using GRADE, we found the quality of evidence for most outcomes to be of moderate quality, primarily due to possible publication bias, as all the included studies were industry-sponsored and most included co-authors employed by the industry sponsor (Supplementary Table 1). Extensive efficacy data for topical ophthalmic treatments up to 12 weeks has been compiled and reported, yet long-term efficacy data remains scarce. Results vary across studies in which signs or symptoms improved with treatment; this phenomenon is not unexpected, as it has been established that DED signs and symptoms are not highly correlated [5, 59]. As there are no direct head-to-head clinical studies comparing DED treatments, comparisons between treatments should be interpreted with caution.
Clinical Implications
This is the first comprehensive comparative review summarising preclinical studies and pivotal trial data for CsA 0.05%, CsA CE, OTX-101, and lifitegrast treatments for DED to provide a complete understanding of their efficacy and safety profile. Overall, these topical ophthalmic therapies are safe and well tolerated and demonstrate clinically and statistically significant improvements in signs and symptoms of the disease.
Effective treatments with minimal side effects may substantially improve a patient’s quality of life. Restoration of visual function improves patient productivity and function in activities of daily living, such as driving and reading, as well as recreation [60]. Patients who are contact lens users or have a history of refractive surgeries may experience additional patient-specific benefits improving their overall quality of life [58, 60].
An earlier time to efficacy of DED treatments may help increase patient satisfaction and medication compliance. As TEAEs, although often mild or moderate, are more frequent with the use of DED treatments compared to their vehicle, a more rapid onset to efficacy improves patient confidence in therapeutic effects and may increase motivation to continue treatment regimen despite TEAEs [61]. Patients with DED treated with lifitegrast first exhibited significant improvement in efficacy parameters compared to vehicle after 2 weeks of treatment [46, 49]; CsA 0.05%, CsA CE, and OTX-101 treated patients demonstrated significant improvement after 4 weeks in at least one pivotal trial (Table 2) [22, 29, 35–38, 40]. Across pivotal trials, treatment with OTX-101 was frequently reported to improve efficacy parameters at 4 weeks, including mean CFB in total CFS score [35–37]; total, inferior, and superior conjunctival staining [38]; and percentage of patients with clear central corneas [36, 40].
Ocular tolerability may also increase patient compliance, adherence to treatment, and subsequently treatment efficacy [53, 61]. Treatment patterns such as adherence, persistence, and discontinuation were investigated in a retrospective, real-world claims database study in patients with DED using CsA 0.05% and lifitegrast [61]. Overall, there was low adherence to treatment (adherence rate less than 10%) and high incidence of treatment discontinuation over a 12-month follow-up period; 64.4% of lifitegrast patients discontinued treatment, while this proportion was 70.8% in CsA 0.05% patients [61]. Although White et al. only investigated CsA 0.05% and lifitegrast, these results may apply to other CsA-based anti-inflammatory treatments. Many factors likely play a role in treatment adherence and discontinuation rates, one being the delay of symptomatic relief after treatment initiation. Earlier clinical benefits may minimise patient discouragement and improve patient retention and dropout rates.
All currently approved ophthalmic treatments vary slightly in their indications. Differences in indications may lead to differences in patient populations receiving these treatments, making direct comparisons between treatments challenging. Additionally, this review highlights that the extent and type of clinical improvements vary across therapies; therefore, individual, patient-specific signs and symptoms and DED contributing factors are important to consider when developing treatment plans.
Conclusion
Topical anti-inflammatory ophthalmic treatments for DED appear generally well tolerated, with favourable and comparable safety profiles. Treatment with CsA 0.05%, CsA CE, OTX-101, or lifitegrast significantly improves DED signs or symptoms compared to their vehicle, although the specific signs and symptoms that improved vary with treatment. Long-term and direct comparative studies between treatments are needed to further understand the differences in efficacy and safety profiles between treatments.
Acknowledgements
Funding
The journal’s Rapid Service fees for this article were funded by Sun Pharmaceutical Industries, Inc.
Medical Writing and/or Editorial Assistance
Writing and editorial support for manuscript preparation were provided by Margaret Van Horn, PhD, of AlphaBioCom, LLC, and funded by Sun Pharmaceutical Industries, Inc.
Author Contributions
All authors participated in the conception/design of this review; provided critical interpretation of the data for presentation; and reviewed, edited, and approved all versions of the manuscript.
Disclosures
Bridgitte Shen Lee reports consultant fees from Lumenis; MacuHealth; Santen Pharmaceutical Co., Lt; research fees from Johnson & Johnson Vision; Kala Pharmaceuticals, SightGlass Vision; and speaker fees from Lumenis, RVL Pharmaceuticals and Sun Pharmaceutical Industries, Inc. Melissa Toyos reports consultant fees from Bausch & Lomb; Eyevance; Iridex; Mallinkrodt; Shire; Sun Pharmaceutical Industries, Inc.; and Zeiss; speaker fees from Bausch & Lomb; Iridex; Lumenis; Mallinkrodt; Shire; Sun Pharmaceutical Industries, Inc.; and Zeiss; research fees from Bausch & Lomb; DigiSight; Dompé Farmaceitici; Iridex; Kala Pharmaceuticals; Lumenis; Magellan; Mallinkrodt; MIXTO Lasering; Ocular Tech; Oculos; Opternative; ReVitaLid; Shire; Sun Pharmaceutical Industries, Inc.; and Zeiss; and miscellaneous fees from MIXTO Lasering. Paul Karpecki reports consultant fees from Akorn, Alcon Labs, Aldeyra, Allergan/AbbVie, Azura Pharmaceuticals, Bausch +
+ Lomb, BioTissue, BlephEx, Bruder Healthcare, Bruno Pharmaceuticals, Cambium Pharmaceuticals, Dompé, Eyedetec, Eyegate, Eyevance, Healthe, Imprimis, Johnson & Johnson Vision, Kala pharmaceuticals, KEPLR Vision, Konan Medical, Mallinckrodt, Neurolens, Novartis, Oasis Medical, Ocuphire, Oculus, OcuMedic, Osmotica, Oyster Point, RegenerEyes, Science Based Health, Sentiss Pharmaceuticals, Sight Sciences, Silk Technologies, Sun Pharmaceuticals, Surface Pharmaceuticals, Tarsus Medical, TearClear, Visant Medical, Vital Tears. Jessica Schiffbauer reports speaker fees from Eyevance. John D Sheppard reports personal fees from Allergan; Alcon; Avedro; Bausch & Lomb; Claris Bio; Clementia Pharma; Dompé; EyeDetec; EyeGate; Lacrisciences; Novartis; Ocular Therapeutix; Science Based Health; Senju; Shire; Sun Pharmaceutical Industries, Inc.; TearLab; TearScience; Tissue Tech; Topcon; and TopiVert; and other fees from Alcon/Novartis; Kala Pharmaceuticals; Novaliq; Noveome; Ocular Therapeutix; Shire; TearLab; and Visus.
Lomb, BioTissue, BlephEx, Bruder Healthcare, Bruno Pharmaceuticals, Cambium Pharmaceuticals, Dompé, Eyedetec, Eyegate, Eyevance, Healthe, Imprimis, Johnson & Johnson Vision, Kala pharmaceuticals, KEPLR Vision, Konan Medical, Mallinckrodt, Neurolens, Novartis, Oasis Medical, Ocuphire, Oculus, OcuMedic, Osmotica, Oyster Point, RegenerEyes, Science Based Health, Sentiss Pharmaceuticals, Sight Sciences, Silk Technologies, Sun Pharmaceuticals, Surface Pharmaceuticals, Tarsus Medical, TearClear, Visant Medical, Vital Tears. Jessica Schiffbauer reports speaker fees from Eyevance. John D Sheppard reports personal fees from Allergan; Alcon; Avedro; Bausch & Lomb; Claris Bio; Clementia Pharma; Dompé; EyeDetec; EyeGate; Lacrisciences; Novartis; Ocular Therapeutix; Science Based Health; Senju; Shire; Sun Pharmaceutical Industries, Inc.; TearLab; TearScience; Tissue Tech; Topcon; and TopiVert; and other fees from Alcon/Novartis; Kala Pharmaceuticals; Novaliq; Noveome; Ocular Therapeutix; Shire; TearLab; and Visus.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no data sets were generated or analysed during the current study.
References
Articles from Ophthalmology and Therapy are provided here courtesy of Springer
Full text links
Read article at publisher's site: https://doi.org/10.1007/s40123-022-00516-9
Read article for free, from open access legal sources, via Unpaywall:
https://link.springer.com/content/pdf/10.1007/s40123-022-00516-9.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/128820648
Article citations
Efficacy and Safety of Perfluorohexyloctane in Evaporative Dry Eye Disease Associated With Meibomian Gland Dysfunction: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.
Cureus, 16(8):e67920, 27 Aug 2024
Cited by: 0 articles | PMID: 39206330 | PMCID: PMC11357713
Review Free full text in Europe PMC
Recent United States Developments in the Pharmacological Treatment of Dry Eye Disease.
Drugs, 84(5):549-563, 23 Apr 2024
Cited by: 0 articles | PMID: 38652355 | PMCID: PMC11189955
Review Free full text in Europe PMC
Developments in Emerging Topical Drug Delivery Systems for Ocular Disorders.
Curr Drug Res Rev, 16(3):251-267, 01 Jan 2024
Cited by: 0 articles | PMID: 38158868
Review
Impact of dry eye disease treatment on patient quality of life.
Front Med (Lausanne), 11:1305579, 28 Feb 2024
Cited by: 3 articles | PMID: 38482530 | PMCID: PMC10932984
Review Free full text in Europe PMC
Dry eye disease caused by viral infection: Past, present and future.
Virulence, 15(1):2289779, 04 Dec 2023
Cited by: 1 article | PMID: 38047740 | PMCID: PMC10761022
Review Free full text in Europe PMC
Go to all (11) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Real-world treatment patterns of OTX-101 ophthalmic solution, cyclosporine ophthalmic emulsion, and lifitegrast ophthalmic solution in patients with dry eye disease: a retrospective analysis.
BMC Ophthalmol, 23(1):443, 02 Nov 2023
Cited by: 2 articles | PMID: 37919692 | PMCID: PMC10621228
One-Year Efficacy and Safety of 0.1% Cyclosporine a Cationic Emulsion in the Treatment of Severe Dry Eye Disease.
Eur J Ophthalmol, 27(6):678-685, 01 Nov 2017
Cited by: 33 articles | PMID: 28708219 | PMCID: PMC6380090
A Review of Topical Cyclosporine A Formulations-A Disease-Modifying Agent for Keratoconjunctivitis Sicca.
Clin Ophthalmol, 14:481-489, 20 Feb 2020
Cited by: 10 articles | PMID: 32109984 | PMCID: PMC7039096
Review Free full text in Europe PMC
Quintessence of currently approved and upcoming treatments for dry eye disease.
Graefes Arch Clin Exp Ophthalmol, 31 Aug 2024
Cited by: 0 articles | PMID: 39215848
Review
Funding
Funders who supported this work.

 1
1 


