Abstract
Aims
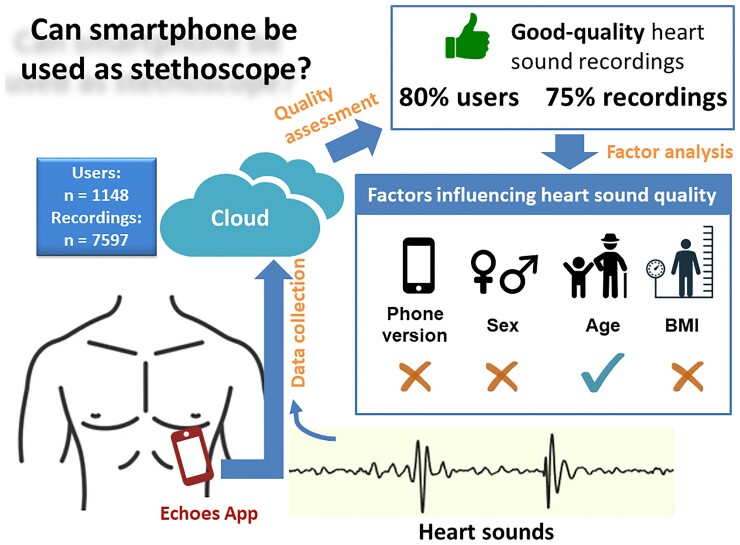
Smartphones are equipped with a high-quality microphone which may be used as an electronic stethoscope. We aim to investigate the factors influencing quality of heart sound recorded using a smartphone by non-medical users.Methods and results
An app named Echoes was developed for recording heart sounds using iPhone. Information on phone version and users' characteristics including sex, age, and body mass index (BMI) was collected. Heart sound quality was visually assessed and its relation to phone version and users' characteristics was analysed. A total of 1148 users contributed to 7597 heart sound recordings. Over 80% of users were able to make at least one good-quality recording. Good-, unsure- and bad-quality recordings amounted to 5647 (74.6%), 466 (6.2%) and 1457 (19.2%), respectively. Most good recordings were collected in the first three attempts of the users. Phone version did not significantly change the users' success rate of making a good recording, neither was sex in the first attempt (P = 0.41) or the first three attempts (P = 0.21). Success rate tended to decrease with age in the first attempt (P = 0.06) but not the first three attempts (P = 0.70). BMI did not significantly affect the heart sound quality in a single attempt (P = 0.73) or in three attempts (P = 0.14).Conclusion
Smartphone can be used by non-medical users to record heart sounds in good quality. Age may affect heart sound recording, but hardware, sex, and BMI do not alter the recording.Free full text

Smartphone as an electronic stethoscope: factors influencing heart sound quality
Abstract
Aims
Smartphones are equipped with a high-quality microphone which may be used as an electronic stethoscope. We aim to investigate the factors influencing quality of heart sound recorded using a smartphone by non-medical users.
Methods and results
An app named Echoes was developed for recording heart sounds using iPhone. Information on phone version and users’ characteristics including sex, age, and body mass index (BMI) was collected. Heart sound quality was visually assessed and its relation to phone version and users’ characteristics was analysed. A total of 1148 users contributed to 7597 heart sound recordings. Over 80% of users were able to make at least one good-quality recording. Good-, unsure- and bad-quality recordings amounted to 5647 (74.6%), 466 (6.2%) and 1457 (19.2%), respectively. Most good recordings were collected in the first three attempts of the users. Phone version did not significantly change the users’ success rate of making a good recording, neither was sex in the first attempt (P =
= 0.41) or the first three attempts (P
0.41) or the first three attempts (P =
= 0.21). Success rate tended to decrease with age in the first attempt (P
0.21). Success rate tended to decrease with age in the first attempt (P =
= 0.06) but not the first three attempts (P
0.06) but not the first three attempts (P =
= 0.70). BMI did not significantly affect the heart sound quality in a single attempt (P
0.70). BMI did not significantly affect the heart sound quality in a single attempt (P =
= 0.73) or in three attempts (P
0.73) or in three attempts (P =
= 0.14).
0.14).
Conclusion
Smartphone can be used by non-medical users to record heart sounds in good quality. Age may affect heart sound recording, but hardware, sex, and BMI do not alter the recording.
Introduction
The stethoscope has a history of over 200 years and still serves as a simple non-invasive tool to listen to patient’s sounds from lungs, heart and intestines.1 Conventional binaural stethoscopes comprise of a chestpiece and two earpieces. By putting the chestpiece against the patient’s skin, the doctor can listen to the patient’s sounds through the two earpieces. The electronic stethoscope was invented in the 1970s, allowing storage, replay and processing of sounds.2,3 However, the digital phonocardiogram has not been widely adopted, partly because of the emergence and popularity of novel imaging techniques such as echocardiography in the 1980s.4
Recent research is creating new interest in cardiac sounds, thanks to the miniaturization of sound sensors, development of signal processing techniques and popularization of artificial intelligence algorithms.5 The electronic stethoscope has now been shown to deliver a higher sensitivity to sound than its conventional counterpart.6 Some handheld electronic stethoscopes allow simultaneous recordings of heart sound and electrocardiogram and are marketed to help in remote monitoring.7
All electronic stethoscopes have the same mechanism of action that converts mechanical vibrations to digital signals. Since a decade the widely used smartphones are equipped with a high-quality microphone which may be used for recording heart sounds. This possibility will create some promising applications for the public to learn heart disease and for remote monitoring of patients at home. Several mobile App prototypes such as iStethoscope and CPstethoscope have been introduced for recording heart sounds and have been downloaded millions of times.8,9 However, to the best of our knowledge, there is currently no scientific report about the potential factors that influence the quality of heart sound recording. These factors may come from hardware such as phone version and from user’s characteristics such as age, sex and body mass index (BMI).
To this purpose, we investigated the effect of phone version as well as user characteristics on the quality of recorded heart sounds using the Echoes App that allows recording, processing, and storage of heart sounds by means of an iPhone.
Methods
Echoes app
The Echoes app is the result of a primarily public-engagement study, aiming to convert a smartphone microphone into an electronic stethoscope, so that non-medical persons can listen to their own heart sounds and learn more about cardiovascular disease. However, in the current state, it does not provide any diagnosis or treatment suggestion. The study has been approved by the ethical committee of King’s College London (LRS-20/21-20985) and conforms to the European Union General Data Protection Regulation on data protection and privacy. The information sheet for participants is available online.10
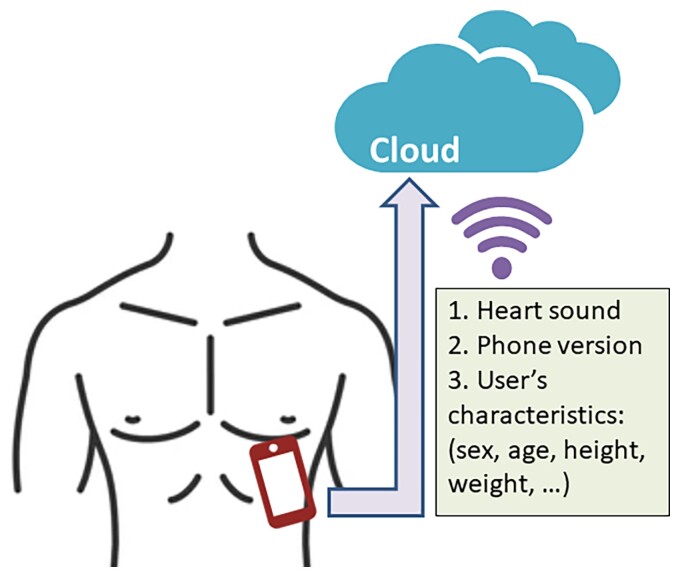
The Echoes app, utilizing built-in microphone of smartphone to record heart sounds, is currently available for iPhone only. On launching the app, the users are asked to provide consent for data collection and management. Then a few tips pop up to guide the user to better record heart sounds. These tips include asking the user to remove phone case, finding one of four spots for recording, adjusting microphone amplification factor, placing the phone on the skin, taking a breath out, pressing start recording button, replaying to listen to heart sound, and if possible, retrying the recording. More details on the user’s instructions can be found in Supplementary material online, Figure S1. After the user’s completion of recording, the heart sounds are filtered using homemade signal processing algorithms to remove background noises. The filtered heart sounds are then replayed to allow the user to listen. Raw data stored in.wav audio format are uploaded through the Internet to Google Firebase database. The user is also asked to voluntarily provide anonymous basic demographics including age, sex, height, weight and if applicable any cardiac conditions. An illustration of data collection and storage is shown in Figure 1.
Data processing
The users’ demographic data and raw heart sound recordings were automatically downloaded using Python Firebase API called Pyrebase for offline analysis.11 During the whole analysis, data were only accessible by a researcher (H.L.).
Visual assessment of heart sound quality
All raw heart sound recordings were plotted using Python software to observe signal morphologies. Then the heart sound quality was visually assessed per recording by one observer (H.L.). Each recording was assigned to one of the following three categories: good quality, unsure quality and bad quality. Good-quality signal was defined by at least 1 heartbeat where both the first (S1) and the second heart sound (S2) were clearly visible in the raw recordings. Bad-quality signal was defined by absence of any heartbeat with S1 and S2. Unsure-quality signal was defined if the observer deemed the signal to be in need of further processing for reliable identification of any heartbeats. To test the inter-observer variability of this visual quality assessment approach, the second assessor (J.L.) independently evaluated a subsample of 1000 heart sound recordings randomly selected from the heart sound database according to the criteria above.
For validation purpose, examples of good-, unsure- and bad-quality heart sounds were processed using a time-frequency analysis method called S-transform.12 The S-transform projects the one-dimensional heart sound signals to a two-dimensional time-frequency plane for better observations of signal components. S-transform was only used for representative heart sound examples of good, unsure and bad quality in order to confirm whether our proposed visual assessment of heart sound quality was consistent with the advanced signal processing technique.
Factors affecting heart sound quality
Heart sounds classified as good quality were deemed interpretable for analysis. Success rate was defined by the proportion of users who made at least 1 good-quality recording within a given number of attempts. We analysed the factors affecting the users’ success rate, including hardware (i.e. iPhone version) and the users’ demographics including sex, age, and BMI [calculated by weight (kilogram) divided by height (metre) squared]. We could not analyse the effect of recording location on heart sound quality because all recordings from those users who indicated recording location were at the same area (Spot 1 of the app) on the chest.
Statistical analysis
Count data were expressed as number (percentage). Skewed data including number of recordings per user were expressed as median [interquartile range (IQR)]. Time-frequency analysis was performed using MATLAB R2018b (MathWorks). To reduce the effect of level of education on our analysis, all known users including university researchers, app programmers, app designers and intern students were excluded from the heart sound database. Relations between success rate and time of measurement, phone version, sex, age and BMI were analysed using Mann–Kendall trend test. Comparisons between two groups (male vs. female, age group and BMI group) were performed with χ2 test. When analysing the relations between iPhone version, sex, age, BMI and heart sound quality, we excluded groups with less than 10 users. All statistical analyses were performed using PyCharm 2021.2.2 (JetBrains s.r.o.). Statistical significance was defined as a two-tailed P value <0.05.
Results
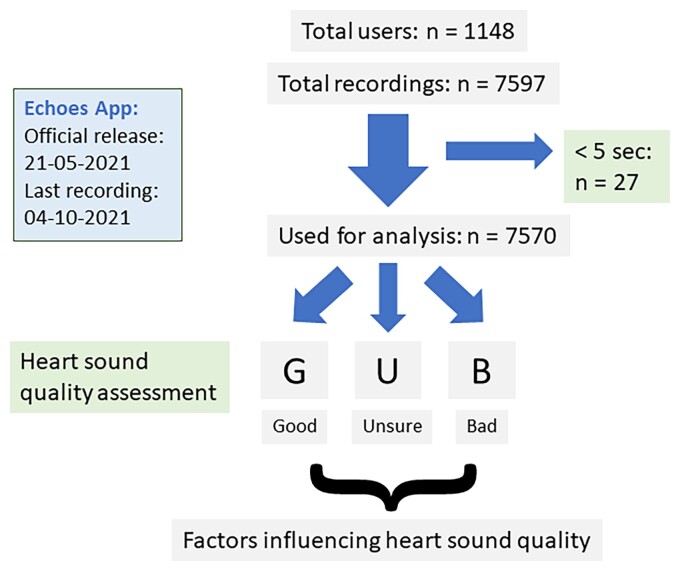
Data processing
The Echoes app was officially released on 21 May 2021 and advertised through social media channels such as Twitter and several newsletters.13–16 For the current analysis, data were collected between 21 May and 4 October 2021. A total of 7597 recordings from 1148 users were obtained (Figure 2). The median number of recordings was 3 (IQR 2–6) per user. After excluding 27 recordings with duration less than 5 seconds, 7570 recordings were visually assessed for heart sound quality.
Visual heart sound quality assessment
Good-, unsure-, and bad-quality recordings amounted to 5647 (74.6%), 466 (6.2%), and 1457 (19.2%), respectively. A total of 80.1% (919/1148) users were able to make at least one good-quality recording. Median number of attempts needed to make the first good-quality recording was 1 (IQR 1–1) per user. Interobserver agreement of heart sound quality was 84.7% in the 1000 randomly selected subsamples (see Supplementary material online, Table S1). For good-, unsure-, and bad-quality recordings, the agreements of the second assessor with the first assessor were 89.1% (672/754), 41.0% (25/61), and 81.1% (150/185), respectively. Most (61.4%, 94/153) of disagreements occurred in the category of ‘Unsure-quality’.
Examples of good- (A), unsure- (B), and bad-quality (C) heart sounds are shown in Figure 3, including time-frequency spectrum (upper strip) and raw signals (lower strip). Audio files of these examples are also available online.17 The good-quality recording (Figure 3AA) clearly showed two major heart sound components (i.e. S1 and S2). Sound energies of S1 were preponderant below 100 Hz, while S2 had energies spreading beyond 100 Hz. In some heartbeats, the third (S3) and/or fourth heart sound (S4) that usually have a low signal amplitude, were also visible. The unsure-quality recording (Figure 3BB) did not show clear S1 and S2 heart sound components in raw signals, though a few high-amplitude vibrations seemed to appear regularly. Using time-frequency analysis in these unsure-quality signals, S1 showed as low-frequency clusters occurring at a regular interval, followed by S2 in high-frequency regions. The bad-quality recording (Figure 3CC) did not show any recurring components, neither in raw signals nor in the time-frequency spectrum.
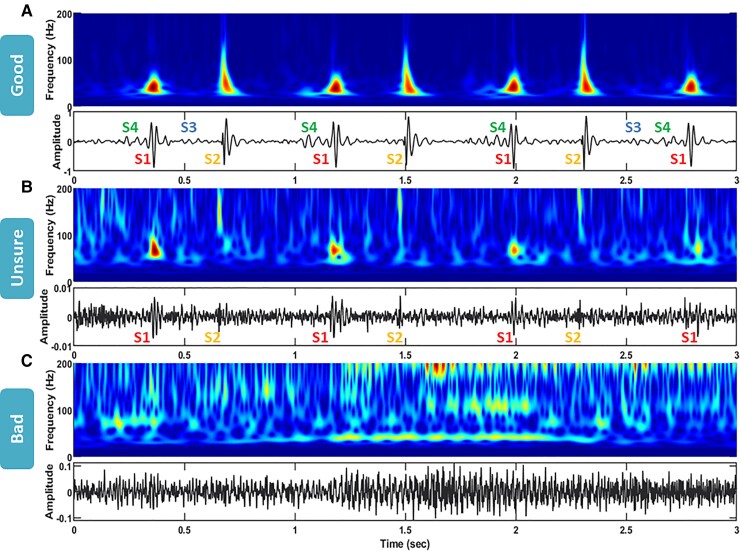
Time-frequency colourmap (upper strip) and raw signal (lower strip) of good- (A), unsure- (B), and bad-quality (C) raw heart sound recordings. The time-frequency colourmaps show how heart sound frequency (vertical axis) changes with time (horizontal axis), with heart sound energy ranging from low (in blue) to high (in red). In raw signals, locations of first- (S1), second- (S2), third- (S3), and fourth heart sound (S4) are labelled.
Time of measurement
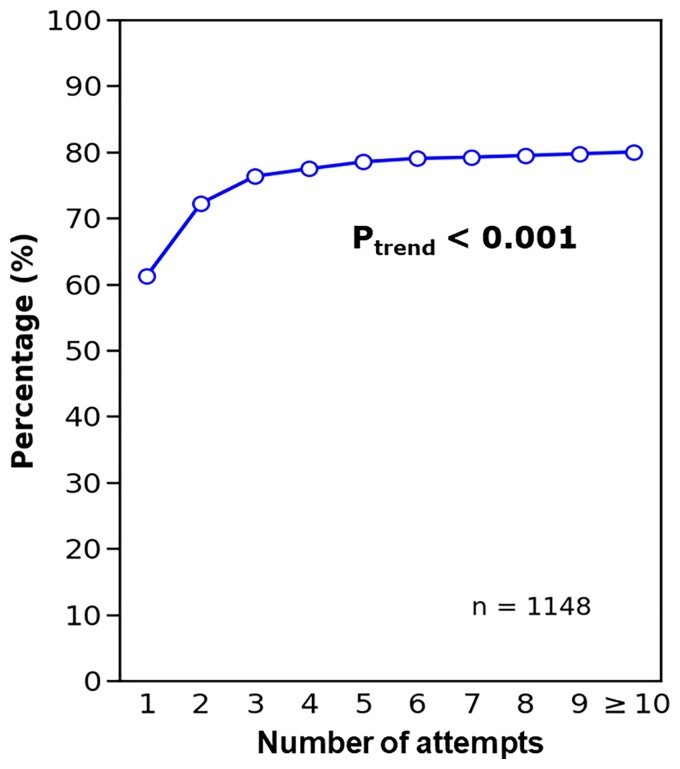
The influence of increasing user experience on sound quality was evaluated using the Mann–Kendall trend test. The proportion of users who made a good-quality recording significantly increased with the number of attempts to measure heart sound (P <
< 0.001; Figure 4). For the first attempt, ~60% of new users made a good-quality recording, which percentage increased to ~75% in the subsequent two attempts. From the fourth attempt and further, the success rate barely improved and approached ~80%, indicating that most users ‘learned’ how to use the app within the first three attempts.
0.001; Figure 4). For the first attempt, ~60% of new users made a good-quality recording, which percentage increased to ~75% in the subsequent two attempts. From the fourth attempt and further, the success rate barely improved and approached ~80%, indicating that most users ‘learned’ how to use the app within the first three attempts.
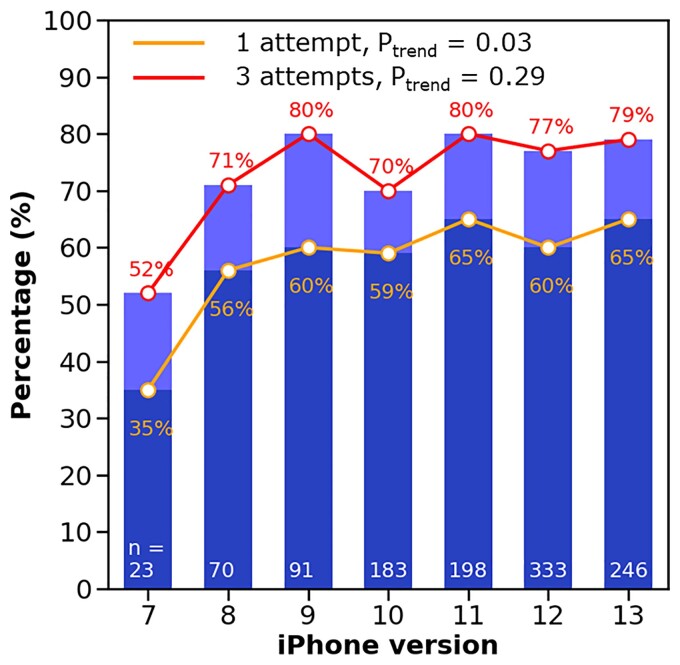
Phone version
The relationship between iPhone version and proportion of users who succeeded in making a good-quality recording in one attempt (orange line) and in three attempts (red line) is shown in Figure 5. The proportion significantly increased when more recent iPhones were used for the first attempt (P =
= 0.03), but not for the first three attempts (P
0.03), but not for the first three attempts (P =
= 0.29). However, the significance was mainly driven by the lowest success rate in the users of iPhone 7 in both the first attempt and the first three attempts. Actually, the success rate did not change markedly from iPhone versions 8 to 13, fluctuating within 10% (for the first attempt: 55–65%; for the first three attempts: 70–80%). These numbers showed a good hardware support when using iPhone to record heart sounds.
0.29). However, the significance was mainly driven by the lowest success rate in the users of iPhone 7 in both the first attempt and the first three attempts. Actually, the success rate did not change markedly from iPhone versions 8 to 13, fluctuating within 10% (for the first attempt: 55–65%; for the first three attempts: 70–80%). These numbers showed a good hardware support when using iPhone to record heart sounds.
Sex and age
Sex was reported in 184 (16%) users, including 92 males and 92 females. Success rate did not differ between males and females in the first attempt (P =
= 0.41; Figure 6AA) and in the first 3 attempts (P
0.41; Figure 6AA) and in the first 3 attempts (P =
= 0.21). Compared with females, the users who did not report their sex had a significantly lower success rate in one attempt (P
0.21). Compared with females, the users who did not report their sex had a significantly lower success rate in one attempt (P =
= 0.002) and in three attempts (P
0.002) and in three attempts (P =
= 0.003). This might indicate that the ones who reported their sex and/or age might have done so because they were much more confident in their recordings (they had a higher success rate).
0.003). This might indicate that the ones who reported their sex and/or age might have done so because they were much more confident in their recordings (they had a higher success rate).
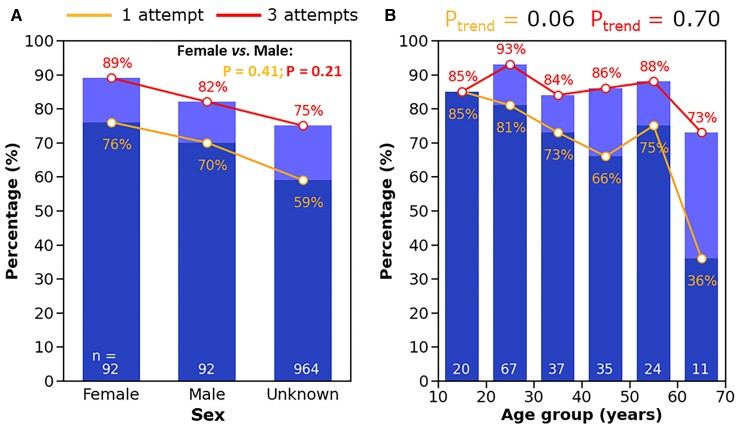
Changes of percentage of users having a good-quality heart sound recording with sex and age. Orange line and dark blue boxes indicate the percentage of heart sound recordings rated with good quality in the first attempt by the users, while red line and light blue boxes in the first three attempts.
Age (35 ±
± 14 years; range: 10–69 years) was reported in 194 users. When grouping the users’ age by every decade, in the first attempt, success rate of making a good-quality recording tended to decrease with age (P
14 years; range: 10–69 years) was reported in 194 users. When grouping the users’ age by every decade, in the first attempt, success rate of making a good-quality recording tended to decrease with age (P =
= 0.06; Figure 6BB). However, this trend diminished when the first three attempts were taken into consideration, indicating good learning capability of more advanced-age users (P
0.06; Figure 6BB). However, this trend diminished when the first three attempts were taken into consideration, indicating good learning capability of more advanced-age users (P =
= 0.70).
0.70).
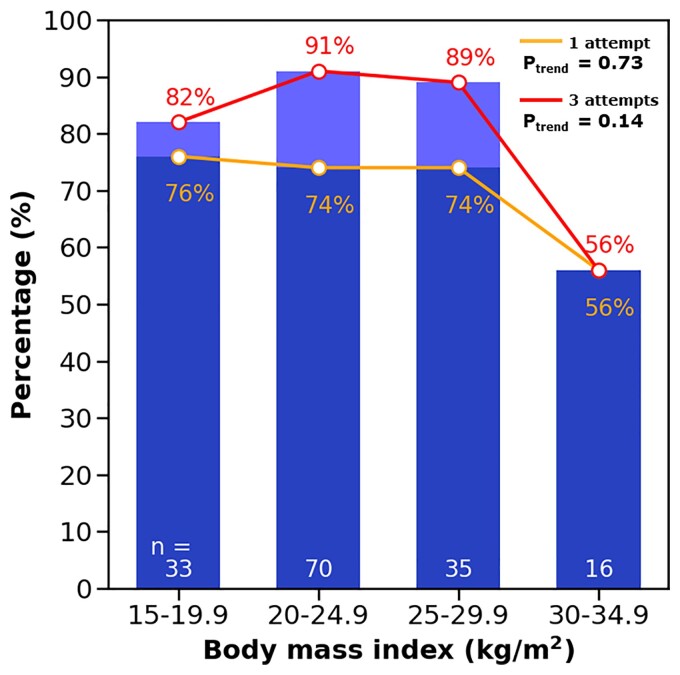
BMI
Body weight and height were reported in 154 (13%) users. BMI (23.6 ±
± 4.2 kg/m2; range: 15.1–34.5 kg/m2) was calculated and grouped in 5 kg/m2 bins (Figure 7). Success rate did not significantly decrease with BMI, neither in one attempt (P
4.2 kg/m2; range: 15.1–34.5 kg/m2) was calculated and grouped in 5 kg/m2 bins (Figure 7). Success rate did not significantly decrease with BMI, neither in one attempt (P =
= 0.73) nor in three attempts (P
0.73) nor in three attempts (P =
= 0.14). However, success rate dropped for BMI >30 kg/m2. In fact, the success rate did not change from the first attempt to the first three attempts in the highest BMI group (56% vs. 56%).
0.14). However, success rate dropped for BMI >30 kg/m2. In fact, the success rate did not change from the first attempt to the first three attempts in the highest BMI group (56% vs. 56%).
Discussion
Principal findings
Principal findings of this study are that (i) three quarters of the participants from the non-medical participants recorded good-quality heart sounds by means of a mobile phone; (ii) approximately three of four raw unfiltered heart sound recordings are of good-quality and 80% of users manage to record a good-quality recording; (iii) a maximum of three attempts is needed to obtain a good-quality recording of heart sound; and (iv) iPhone version and sex do not affect heart sound recordings, but BMI >
> 30 kg/m2 and age >60 years seem to lead to lower quality recordings.
30 kg/m2 and age >60 years seem to lead to lower quality recordings.
Can smartphone be used to record heart sounds?
Nowadays, most smartphones are equipped with a high-quality microphone having a frequency response of 20 Hz–20 kHz. This range is more than sufficient to cover the frequency range of heart sounds (20–200 Hz).18 The App iStethoscope was the first piece of software developed for auscultation of heart sound.8 It was optimized for iPhone 3G devices and also shown to work effectively on 4, 4S, 5, 5C, and 5S iPhones. This finding was supported by another study which tested the accuracy of iPhone microphones using 20 Hz to 20 kHz sounds, and reported that for the early versions of iPhone (iPhone 3Gs to iPhone 5), the difference in sound pressure level was not significant between a professional sound recorder and iPhone microphones.19 Our study extends these studies by showing that the more recent versions of iPhone from 7 to 13 also work for heart sound measurement, although the success rate of obtaining good-quality recordings tends to be lower for iPhone 7.
The only study on Android phones for heart sound collection reported that heart sounds can be recorded in hospital settings using an app (CPstethoscope) on Samsung and LG phones.9 Among the 46 patients enrolled, the researchers were able to distinguish among normal, third heart sound, fourth heart sound, systolic murmur and diastolic murmur. However, in this small-sample-size pilot study, the heart sounds were measured by researchers who had professional knowledge about cardiovascular anatomy.
Our study was a large-scale study that distributed an app among over 1100 non-medical public users. The results showed that the smartphone could not only record the most distinctive components (S1 and S2) of heart sound, but also the low-amplitude and low-frequency extra heart sound components (S3 and S4; examples in Figure 3AA) that are normally difficult to hear by experienced doctors using stethoscope. Moreover, our study shows good utilization of the app among the first-time users for heart sound measurement. However, we did not investigate the possibility to use the smartphone-recorded heart sounds for clinical diagnosis, because this would require additional personalized medical information and therefore also stricter privacy settings.
Factors affecting heart sound quality
We found that despite a high success rate (~80%) of recording a good-quality heart sound among the users, a few factors still affected the use of our app. The fact that success rate increased with time of measurement, especially in the first three attempts, indicates the possibility of improving the app design to better guide the users to quickly learn how to use the app in the first few attempts in the future. For example, compared with the static user’s guidance in the current app, we may use a video to guide the users how to use the app properly. Regarding hardware, iPhone version does not seem to relate to heart sound quality, indicating similar or even the same microphone sensor used in the series of products. Signal quality is not markedly different between sexes, showing a good understanding of the app in both sexes. The decreased proportion of users who were able to make a good-quality recording with age warranted a better design of the app to guide the old-age users to record heart sounds. However, despite the lower success rate among the elderly for the first attempt of the app, actually these users quickly learned how to correctly use the app in the next two attempts, as evidenced by the higher increase of success rate from the first attempt to the first three attempts compared to their younger counterparts. Yet this finding may need to be confirmed in a larger scale study in the future.
Advantages of using smartphone for recording heart sounds
The huge amount of smartphone users (6.38 billion in 2021) provides a unique opportunity to turn the built-in microphone to an electronic stethoscope for both health education among the public.20 A further possible application, not yet investigated here, is to use the smartphone-built-in microphone for medical purposes in patients. Because almost everybody owns a smartphone, the patients may record their heart sounds at home and during natural conditions as opposed to the outpatient clinic. Since the solution does not incur any extra cost contrary to buying a professional electronic stethoscope, those who are living in underdeveloped or remote areas short of medical resources can use the app for health-related purposes. From this perspective, turning smartphone into an electronic stethoscope provides a solution to reduce health system costs in these areas.
Digital stethoscopes as well as smartphones have the advantage that the signals can be stored and objectively analyzed, while the conventional analogue stethoscopes rely on the well-trained doctors’ ears that possibly introduce interobserver variability in interpretation of the signals.21,22 The abilities of digital stethoscope may be further enhanced by combining with automatic algorithms including machine learning algorithms. For example, the PASCAL Classifying Heart Sounds Challenge using heart sounds collected from the iPhone-based app (iStethoscope Pro) has stimulated the development of multiple algorithms including convolutional neural network, deep learning algorithm and artificial neural network for automatic segmentation and classification of heart sounds.23–26
Future perspectives
Our study analyzed an increasingly expanding heart sound dataset of the Echoes app. Our findings support further development of the app for not just public engagement purposes but also for medical purposes. As a low-cost and easy-to-use solution, our app may be deployed on a large scale in areas with insufficient medical resources to help screen and monitor patients with cardiovascular diseases. An example is to use the app to screen for congenital and valvular heart diseases which mostly produce systolic and/or diastolic murmurs but which may be too late to be intervened at an advanced stage. Another potential application is to use the app for heart rate and rhythm managements in patients with chronic cardiovascular diseases such as atrial fibrillation. Atrial fibrillation creates the irregularities of not only rhythm but also amplitude of the heart sounds. In this respect, heart sounds may serve as a valuable tool in supporting electrocardiogram for evaluation of arrhythmias. In particular, our app enables the users’ self-recording of transient arrhythmias in conditions like paroxysmal atrial fibrillation and premature ventricular contraction at home for further hospital consultation.
Since built-in microphone of smartphone is more sensitive to vibrations falling in audible frequency range (≥20 Hz), it may be combined with the built-in inertial measurement unit of the phone for a better measurement of lower-frequency vibrations such as seismocardiogram. For example, the built-in accelerometer may be put on the chest of a patient in supine position to record seismocardiogram.27 However, before applying the app to the patients, further preliminary tests in hospital settings may help improve the usability of the app and establish its role in conjunction with other existing monitoring methods such as electrocardiogram.
Limitations
Our study had a few limitations. Firstly, the user cohort may not represent a general population because smartphone users are likely younger and more educated, the latter certainly in regard to this app. It seems likely that a truly general population may show worse results and should be a topic for further research. Secondly, we assessed heart sound quality by eyeballing, primarily judging the presence of S1 and S2 and the amount of noise, which might have introduced subjective bias. For the current goal (public awareness), this appears sufficient, as audible S1 and S2 provide a sense of the beating heart. The usefulness of recognizing pathological heart sounds including S3, S4 and murmurs, has to be investigated in a future study involving patients. In addition, the Echoes app was only available for iPhone. In the future, we need to develop the app for Android users who account for more than half of overall smartphone users. A further limitation came from the low proportion of users who filled in their personal information (e.g. sex and age) or indicated the specific location for recording heart sounds on the chest wall. Improvements of the user interface are necessary to guide the users to submit these data. Whether some other factors such as dimensions or weight of the phone would affect heart sound quality may also be worthy of investigation. Furthermore, some modifications including enlargement of font size and simplification of texts are crucial since the users with heart diseases are frequently old. Lastly, our current version of the Echoes app only allows to record up to 7 s of heart sounds. This may be extended to a longer period such as 30 s for more robust evaluation of heart rhythm and rate.
Conclusions
A smartphone can be used to record heart sounds in non-medical population. Users of older age and higher BMI are likely to have lower quality heart sound recordings. The app solution may be useful for monitoring heart health on a large scale in the future.
Supplementary material
Supplementary material is available at European Heart Journal – Digital Health online.
Contributor Information
Hongxing Luo, Department of Physiology, Cardiovascular Research Institute Maastricht (CARIM), Maastricht University, P.O. Box 616, 6200 MD Maastricht, The Netherlands.
Pablo Lamata, School of Biomedical Engineering and Imaging Sciences, King's College London, 5th Floor Becket House, Lambeth Palace Road, London SE1 7EU, UK.
Salomé Bazin, Cellule Studio, Leyton Studios, 15 Argall Avenue, London E107QE, UK.
Thea Bautista, School of Biomedical Engineering and Imaging Sciences, King's College London, 5th Floor Becket House, Lambeth Palace Road, London SE1 7EU, UK.
Natsuki Barclay, School of Biomedical Engineering and Imaging Sciences, King's College London, 5th Floor Becket House, Lambeth Palace Road, London SE1 7EU, UK.
Mehrdad Shahmohammadi, Department of Biomedical Engineering, Cardiovascular Research Institute Maastricht (CARIM), Maastricht University, PO Box 616, 6200 MD Maastricht, The Netherlands.
Jolijn M Lubrecht, Department of Physiology, Cardiovascular Research Institute Maastricht (CARIM), Maastricht University, P.O. Box 616, 6200 MD Maastricht, The Netherlands.
Tammo Delhaas, Department of Biomedical Engineering, Cardiovascular Research Institute Maastricht (CARIM), Maastricht University, PO Box 616, 6200 MD Maastricht, The Netherlands.
Frits W Prinzen, Department of Physiology, Cardiovascular Research Institute Maastricht (CARIM), Maastricht University, P.O. Box 616, 6200 MD Maastricht, The Netherlands.
Funding
We have received funding from the Wellcome Trust Senior Research Fellowship (g.a. 209450/Z/17/Z) and the European Union Horizon 2020 research and innovation programme ‘Personalised In-silico Cardiology (PIC)’ under the Marie Sklodowska-Curie grant agreement No 764738. We have also been supported by the British Heart Foundation and Evelina Children’s Heart Organization.
References
Articles from European Heart Journal. Digital Health are provided here courtesy of Oxford University Press on behalf of the European Society of Cardiology
Full text links
Read article at publisher's site: https://doi.org/10.1093/ehjdh/ztac044
Read article for free, from open access legal sources, via Unpaywall:
https://academic.oup.com/ehjdh/article-pdf/3/3/473/46334308/ztac044.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/135256185
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1093/ehjdh/ztac044
Article citations
Deep Learning in Heart Sound Analysis: From Techniques to Clinical Applications.
Health Data Sci, 4:0182, 09 Oct 2024
Cited by: 0 articles | PMID: 39387057 | PMCID: PMC11461928
Review Free full text in Europe PMC
Artificial intelligence-enhanced patient evaluation: bridging art and science.
Eur Heart J, 45(35):3204-3218, 01 Sep 2024
Cited by: 0 articles | PMID: 38976371
Review
Beat-to-beat alterations of acoustic intensity and frequency at the maximum power of heart sounds are associated with NT-proBNP levels.
Front Cardiovasc Med, 11:1372543, 02 Apr 2024
Cited by: 0 articles | PMID: 38628311 | PMCID: PMC11018890
Review on the Advancements of Stethoscope Types in Chest Auscultation.
Diagnostics (Basel), 13(9):1545, 25 Apr 2023
Cited by: 6 articles | PMID: 37174938 | PMCID: PMC10177339
Review Free full text in Europe PMC
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Automated signal quality assessment of mobile phone-recorded heart sound signals.
J Med Eng Technol, 40(7-8):342-355, 23 Sep 2016
Cited by: 7 articles | PMID: 27659352
Development of a Smartphone App for Visualizing Heart Sounds and Murmurs.
Cardiology, 137(3):193-200, 26 Apr 2017
Cited by: 4 articles | PMID: 28441656
Smartphone Users' Persuasion Knowledge in the Context of Consumer mHealth Apps: Qualitative Study.
JMIR Mhealth Uhealth, 9(4):e16518, 13 Apr 2021
Cited by: 6 articles | PMID: 33847596 | PMCID: PMC8080138
The electronic stethoscope.
Biomed Eng Online, 14:66, 10 Jul 2015
Cited by: 64 articles | PMID: 26159433 | PMCID: PMC4496820
Review Free full text in Europe PMC
Funding
Funders who supported this work.
Wellcome Trust (1)
Unravelling the physics of the pressure drop in blood flow constrictions
Pablo Lamata, King's College London
Grant ID: 209450/Z/17/Z
Wellcome Trust Senior Research Fellowship (1)
Grant ID: 209450/Z/17/Z