The Rhesus factor, or Rh factor, is a certain type of protein found on the outside of red blood cells. People are either Rh-positive (they have the protein) or Rh-negative (they don’t have the protein). This is important when you’re Rh-negative and pregnant with a fetus who’s Rh-positive.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
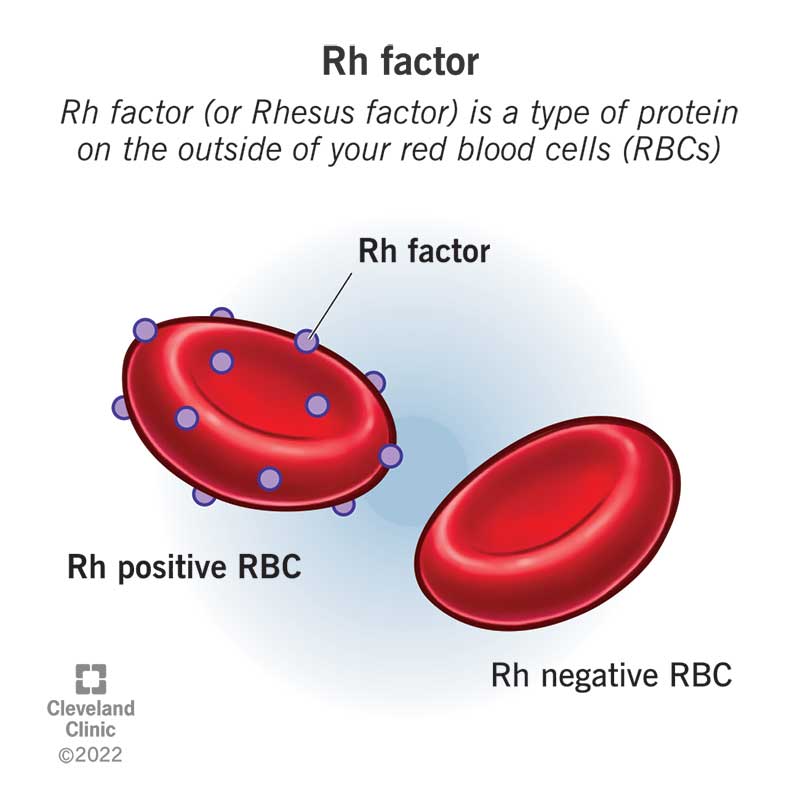
Rh factor (or Rhesus factor) is a type of protein on the outside or surface of your red blood cells. You inherit the protein, which means you get your Rh factor from your biological parents. If you have the protein, you’re Rh-positive. If you don’t have the protein, you’re Rh-negative. The majority of people, about 85%, are Rh-positive.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
During pregnancy, complications may occur if you’re Rh-negative and the fetus is Rh-positive. This is called Rh factor incompatibility. Treatments are available to prevent complications of Rh incompatibility.
The protein on the surface of your red blood cells determines your blood type. Each blood type also has a positive or negative factor. The positive or negative next to the blood type is your Rh factor. Your Rh factor doesn’t cause problems or hurt your health in any way. It only becomes important when blood types are mixed together, like during pregnancy and childbirth.
The most common blood types are:
Your Rh factor doesn’t affect your overall health, but it’s important to know your Rh status if you’re pregnant.
Rh incompatibility occurs when a person who’s Rh-negative becomes pregnant with a fetus with Rh-positive blood. With Rh incompatibility, your immune system reacts to this difference (known as incompatibility) and creates antibodies. These antibodies drive an immune system attack against the fetus’s red blood cells, which your body thinks are foreign objects. This is called Rh sensitization. Your pregnancy care provider can prevent this from happening by giving you a shot (injection) of immune globulin.
Advertisement
During pregnancy, you don’t share blood with the fetus you’re carrying. However, a small amount of blood from the fetus can mix with your blood during labor and delivery (either vaginal or cesarean). It can also happen during:
Complications don’t usually happen during a person’s first pregnancy. This is because it’s unlikely that your blood will mix with the fetus’s blood until delivery, which means antibodies won’t form until after the fetus is born. However, your provider still tests your Rh factor even if it’s your first pregnancy.
Rh incompatibility becomes a problem if you become pregnant a second time and have another Rh-positive fetus. In this case, your body will produce antibodies. These antibodies put the second fetus at risk for complications. Once your body realizes the fetus is Rh-positive, antibodies can pass into the fetus’s blood and attack its red blood cells. This is called Rh disease. Rh disease can be life-threatening for the fetus.
A person who’s Rh-negative is at risk for Rh incompatibility if they become pregnant with a fetus who is Rh-positive. This chart helps determine the fetus’s risk for Rh incompatibility:
| Pregnant Biological Parent | Other Biological Parent | Fetus’s RH factor | Risk Level |
|---|---|---|---|
| Rh-positive | Rh-positive | Rh-positive | None |
| Rh-negative | Rh-negative | Rh-negative | None |
| Rh-positive | Rh-negative | Could be either | None |
| Rh-negative | Rh-positive | Could be either | High. Rh immune globulin (RhoGAM®) is necessary. |
| Pregnant Biological Parent | |||
| Rh-positive | |||
| Other Biological Parent | |||
| Rh-positive | |||
| Fetus’s RH factor | |||
| Rh-positive | |||
| Risk Level | |||
| None | |||
| Rh-negative | |||
| Other Biological Parent | |||
| Rh-negative | |||
| Fetus’s RH factor | |||
| Rh-negative | |||
| Risk Level | |||
| None | |||
| Rh-positive | |||
| Other Biological Parent | |||
| Rh-negative | |||
| Fetus’s RH factor | |||
| Could be either | |||
| Risk Level | |||
| None | |||
| Rh-negative | |||
| Other Biological Parent | |||
| Rh-positive | |||
| Fetus’s RH factor | |||
| Could be either | |||
| Risk Level | |||
| High. Rh immune globulin (RhoGAM®) is necessary. |
The Rh factor test is a simple blood test (called a type and screen) that every pregnant person gets in the first trimester of pregnancy (usually at your first prenatal appointment). The Rh factor test determines your Rh factor. This is important during pregnancy because if you’re Rh-negative and the fetus is Rh-positive, you have a condition called Rh factor incompatibility.
A blood test diagnoses Rh incompatibility. If you become pregnant, your obstetrician will test you to determine if you’re Rh-negative. If you’re Rh-positive, nothing else happens.
If you’re Rh-negative and your antibody screen is negative, your provider will give you Rh immune globulin to prevent antibody formation. You’ll typically get this around 28 weeks of pregnancy and then again within 72 hours of delivery if the fetus is Rh-positive. You may get a dose in early pregnancy if your provider believes your blood has mixed with the fetus’s blood.
Rh immune globulin (RhIg or RhoGAM®) is a medication that stops your body from making Rh antibodies. It’s only helpful if your body hasn’t already made Rh antibodies. You receive it as a shot (injection). Rh immunoglobulin shots are usually very successful in treating Rh-incompatibility during pregnancy. Detecting Rh incompatibility early in pregnancy is the best way to prevent serious complications.
Advertisement
If your body already has Rh antibodies, the fetus is at risk for Rh disease. Since Rh immune globulin won’t be helpful, the best treatment is close monitoring for the remainder of your pregnancy. There’s a small chance your provider will want to deliver early, but this depends on how severe the fetus’s Rh disease is.
Rh incompatibility doesn’t affect the pregnant person. In a fetus, it can cause hemolytic anemia. Hemolytic anemia destroys the fetus’s red blood cells faster than it can replace them.
The effects of Rh incompatibility can range from mild to severe. These effects may also include:
For mild side effects, the fetus may not need any treatment. Most fetuses recover fully if they have a mild case of Rh disease.
For severe cases, the fetus may receive a blood transfusion. This procedure helps replace its red blood cells. Providers can use special lights to help reduce bilirubin levels in fetuses that have jaundice. You may need to give birth early to avoid serious complications of anemia.
Since the development of Rh immune globulin injections, Rh disease occurs infrequently.
Treatment with Rh immune globulin won’t help if an Rh-negative person has already made antibodies. This is why it’s important to know your Rh factor and get treatment as soon as possible.
Advertisement
Because Rh factor is genetic, it’s not possible to choose which Rh type the fetus has. The best prevention is to find out your Rh factor.
If you’re Rh-negative, getting RhIg injections after every possible contact with Rh-positive blood between you and the fetus reduces the risk of them getting Rh disease. Rh incompatibility doesn’t affect your health, only the fetus’s health.
Finding out if you have Rh factor incompatibility early will make it so that your provider can give you Rhlg injections. It’s the best way to ensure the fetus stays healthy.
A note from Cleveland Clinic
Knowing your Rh status is important during pregnancy (or before) because it can prevent potential complications. Luckily, your pregnancy care provider tests your blood to determine if you’re Rh-positive or Rh-negative early in pregnancy. Rh factor incompatibility only becomes an issue during pregnancy when you’re Rh-negative and the fetus is Rh-positive. Your provider treats Rh incompatibility with an injection of Rh immunoglobulin (RhIg). Try not to worry — your provider will keep a close eye on you and get you the treatment you need to prevent any complications.
Advertisement
Last reviewed on 11/10/2022.
Learn more about the Health Library and our editorial process.