Abstract
Background
Silver-Russell syndrome (SRS) is characterized by growth failure and dysmorphic features. Major (epi)genetic causes of SRS are loss of methylation on chromosome 11p15 (11p15 LOM) and maternal uniparental disomy of chromosome 7 (upd(7)mat). However, IGF2, CDKN1C, HMGA2, and PLAG1 mutations infrequently cause SRS. In addition, other imprinting disturbances, pathogenic copy number variations (PCNVs), and monogenic disorders sometimes lead to SRS phenotype. This study aimed to clarify the frequency and clinical features of the patients with gene mutations among etiology-unknown patients with SRS phenotype.
Results
Multigene sequencing was performed in 92 out of 336 patients referred to us for genetic testing for SRS. The clinical features of the patients were evaluated based on the Netchine-Harbison clinical scoring system. None of the patients showed 11p15 LOM, upd(7)mat, abnormal methylation levels for six differentially methylated regions (DMRs), namely, PLAGL1:alt-TSS-DMR on chromosome 6, KCNQ1OT1:TSS-DMR on chromosome 11, MEG3/DLK1:IG-DMR on chromosome 14, MEG3:TSS-DMR on chromosome 14, SNURF:TSS-DMR on chromosome 15, and GNAS A/B:TSS-DMR on chromosome 20, PCNVs, or maternal uniparental disomy of chromosome 16. Using next-generation sequencing and Sanger sequencing, we screened four SRS-causative genes and 406 genes related to growth failure and/or skeletal dysplasia. We identified four pathogenic or likely pathogenic variants in responsible genes for SRS (4.3%: IGF2 in two patients, CDKN1C, and PLAG1), and five pathogenic variants in causative genes for known genetic syndromes presenting with growth failure (5.4%: IGF1R abnormality (IGF1R), SHORT syndrome (PIK3R1), Floating-Harbor syndrome (SRCAP), Pitt-Hopkins syndrome (TCF4), and Noonan syndrome (PTPN11)). Functional analysis indicated the pathogenicity of the CDKN1C variant. The variants we detected in CDKN1C and PLAG1 were the second and third variants leading to SRS, respectively. Our patients with CDKN1C and PLAG1 variants showed similar phenotypes to previously reported patients. Furthermore, our data confirmed IGF1R abnormality, SHORT syndrome, and Floating-Harbor syndrome are differential diagnoses of SRS because of the shared phenotypes among these syndromes and SRS. On the other hand, the patients with pathogenic variants in causative genes for Pitt-Hopkins syndrome and Noonan syndrome were atypical of these syndromes and showed partial clinical features of SRS.
Conclusions
We identified nine patients (9.8%) with pathogenic or likely pathogenic variants out of 92 etiology-unknown patients with SRS phenotype. This study expands the molecular spectrum of SRS phenotype.
Keywords: Silver-Russell syndrome, Multigene sequencing, Functional analysis, CDKN1C, PLAG1, IGF1R, SHORT syndrome, Floating-Harbor syndrome, Pitt-Hopkins syndrome, Noonan syndrome
Background
Silver-Russell syndrome (SRS) is a clinically and genetically heterogeneous disorder characterized by growth failure and dysmorphic features [1]. Recently, the Netchine-Harbison clinical scoring system (NH-CSS) has been adopted as the clinical diagnostic criteria of SRS [1]. NH-CSS has the following six key features: (1) small for gestational age (SGA), (2) postnatal growth failure, (3) relative macrocephaly at birth, (4) protruding forehead, (5) body asymmetry, and (6) feeding difficulties and/or low body mass index [1]. The patients with four or more NH-CSS criteria have a diagnosis of SRS [1]. Among these patients, patients satisfying NH-CSS criteria including both relative macrocephaly and protruding forehead, but with normal molecular testing, are classified as “clinical SRS” [1]. In addition, many patients with SRS show clinical features such as triangular face, fifth finger clinodactyly, and/or brachydactyly [2]. Patients meeting only three NH-CSS criteria, but who have clinically suspected SRS were recommended to receive genetic testing for SRS as well as patients with four or more NH-CSS criteria [1].
The major (epi)genetic causes of SRS are loss of methylation on chromosome 11p15 (11p15 LOM) and maternal uniparental disomy of chromosome 7 (upd(7)mat) [1]. Among patients without 11p15 LOM or upd(7)mat, other imprinting disturbances such as Temple syndrome, maternal uniparental disomy of chromosome 16 (upd(16)mat), maternal uniparental disomy of chromosome 20, pathogenic copy number variations (PCNVs), and mutations in IGF2 on the paternal allele and CDKN1C on the maternal allele, which are causative genes for SRS, were identified in some cases [1]. Recently, HMGA2 on 12q14 and PLAG1 on 8q12 were proposed as the new responsible genes for SRS [3, 4]. Patients with mutations of these SRS-causative genes have a risk of transmitting the disorder [1, 3, 4]. In addition, some monogenic disorders such as 3-M syndrome, Mulibrey nanism, SHORT syndrome, Floating-Harbor syndrome, and IMAGe syndrome are recognized as differential diagnoses of SRS [1].
To clarify the frequency and clinical features of the patients with gene mutations among etiology-unknown patients with SRS phenotype, we performed multigene sequencing for four SRS-causative genes and 406 genes related to growth failure and/or skeletal dysplasia in 92 patients with SRS phenotype who did not have 11p15 LOM, upd(7)mat, other imprinting disturbances, or PCNVs.
Results
Molecular analysis
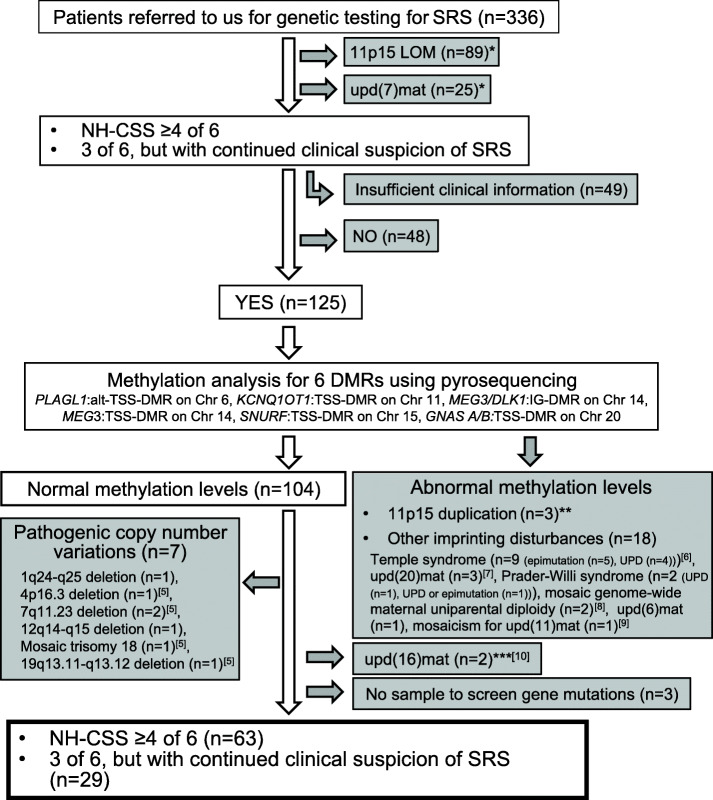
We analyzed 92 SRS phenotypic patients out of 336 patients referred to us for genetic testing for SRS. The clinical features of the patients were evaluated based on the Netchine-Harbison clinical scoring system. None of the patients had 11p15 LOM, upd(7)mat, abnormal methylation levels for six differentially methylated regions (DMRs), namely, PLAGL1:alt-TSS-DMR on chromosome 6, KCNQ1OT1:TSS-DMR on chromosome 11, MEG3/DLK1:IG-DMR on chromosome 14, MEG3:TSS-DMR on chromosome 14, SNURF:TSS-DMR on chromosome 15, and GNAS A/B:TSS-DMR on chromosome 20, PCNVs, or upd(16)mat (Fig. 1) [5–10]. We performed multigene screening for four genes responsible for SRS and 406 genes related to growth failure and/or skeletal dysplasia (Additional file 1: Table S1). All rare variants were evaluated based on the American College of Medical Genetics Standards and Guidelines [11]. We extracted the variants classified as “pathogenic” or “likely pathogenic.” We detected nine patients (9.8%) with pathogenic or likely pathogenic variants out of 92 etiology-unknown patients with SRS phenotype. Four variants were in responsible genes for SRS (4.3%: IGF2 in two patients, CDKN1C, and PLAG1) and five variants were in causative genes for known genetic syndromes presenting with growth failure (5.4%: IGF1R abnormality (IGF1R), SHORT syndrome (PIK3R1), Floating-Harbor syndrome (SRCAP), Pitt-Hopkins syndrome (TCF4), and Noonan syndrome (PTPN11)) (Table 1 and Additional file 2: Figure S1).
Fig. 1.
Flowchart of inclusion criteria. A total of 336 patients were referred to us for genetic testing for Silver-Russell syndrome (SRS) from 2002 to 2018. Our study included 92 patients without pathogenic copy number variations or abnormal methylation levels for ten differentially methylated regions (DMRs), namely, H19/IGF2:IG-DMR, PEG10:TSS-DMR, MEST:alt-TSS-DMR, PLAGL1:alt-TSS-DMR, KCNQ1OT1:TSS-DMR, MEG3/DLK1:IG-DMR, MEG3:TSS-DMR, SNURF:TSS-DMR, ZNF597:TSS-DMR, and GNAS A/B:TSS-DMR. 11p15 LOM, loss of methylation on chromosome 11p15; upd(7)mat, maternal uniparental disomy of chromosome 7; NH-CSS, Netchine-Harbison clinical scoring system; Chr, chromosome; upd(20)mat, maternal uniparental disomy of chromosome 20; upd(6)mat, maternal uniparental disomy of chromosome 6; upd(11)mat, maternal uniparental disomy of chromosome 11; upd(16)mat, maternal uniparental disomy of chromosome 16. *We evaluated clinical features of only a part of the patients according to the Netchine-Harbison clinical scoring system. **The duplicated region of two patients with 11p15 duplications did not include the H19/IGF2:IG-DMR. Thus, these patients showed normal methylation levels of the H19/IGF2:IG-DMR. The duplicated region of the remaining one patient included the H19/IGF2:IG-DMR. The methylation level of the H19/IGF2:IG-DMR in this patient was low normal, and we did not recognize 11p15 LOM. ***We began upd(16)mat screening in 2016. As such, we performed upd(16)mat screening for only a part of the patients with pathogenic copy number variations and patients with abnormal methylation levels of the DMRs related to known imprinting disorders before 2016
Table 1.
Pathogenic or likely pathogenic variants detected in this study
| Patient | Pathogenic or likely pathogenic variants in the responsible genes for SRS | Pathogenic variants in causative genes for known genetic syndromes presenting with growth failure | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Patient 1 [12] | Patient 2 [12] | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Patient 7 | Patient 8 | Patient 9 | |
| Gene | IGF2 | IGF2 | CDKN1C | PLAG1 | IGF1R | PIK3R1 | SRCAP | TCF4 | PTPN11 |
| Variant | c.209G>A | c.211T>C | c.947G>A | c.589C>T | c.1457delC | c.1892G>A | c.7376delC | c.1102_1103delCA | c.844A>G |
| p.(Cys70Tyr) | p.(Cys71Arg) | p.(Arg316Gln) | p.(Arg197*) | p.(Ser487Profs*21) | p.(Arg631Gln) | p.(Pro2459Leufs*16) | p.(Gln368Glyfs*6) | p.(Ile282Val) | |
| Genetic diagnosis | SRS | SRS | SRS | SRS | IGF1R abnormality | SHORT syndrome | Floating-Harbor syndrome | Pitt-Hopkins syndrome | Noonan syndrome |
| Inheritance | De novo | De novo or paternal | Mother (carrier) | Mother (affected) | Father (carrier) | De novo | De novo | De novo | De novo |
| Allele | Paternal | Paternal | Maternal | Maternal | Paternal | NE | NE | NE | NE |
| Karyotype | 46,XY | 46,XY | 46,XX | 46,XX | NE | 46,XY | 46,XY | 46,XX | 46,XY |
| Allele frequency | |||||||||
| gnomAD [13] | None | None | None | None | None | None | None | None | None |
| HGVD [14] | None | None | None | None | None | None | None | None | None |
| 4.7KJPN [15] | None | None | None | None | None | None | None | None | None |
| In silico pathogenicity prediction | |||||||||
| CADD [16] | 1% most deleterious | 1% most deleterious | 1% most deleterious | 1% most deleterious | 1% most deleterious | 1% most deleterious | 1% most deleterious | 1% most deleterious | 1% most deleterious |
| (PHRED score) | 27.4 | 27.2 | 32.0 | 37.0 | 35.0 | 33.0 | 27.2 | 35.0 | 23.6 |
| MutationTaster [17] (score) | Disease causing | Disease causing | Disease causing | Disease causing | Disease causing | Disease causing | Disease causing | Disease causing | Disease causing |
| 1.000 | 1.000 | 0.662 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | |
| SIFT [18] (score) | Damaging | Damaging | Damaging | – | – | Damaging | – | – | Damaging |
| 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | |||||
| PP2_HVAR [19] (score) | Probably damaging | Probably damaging | Probably damaging | – | – | Probably damaging | – | – | Benign |
| 0.975 | 0.933 | 0.982 | 0.941 | 0.088 | |||||
| M-CAP [20] (score) | Possibly pathogenic | Possibly pathogenic | Possibly pathogenic | – | – | Possible pathogenic | – | – | Possibly pathogenic |
| 0.867 | 0.887 | 0.964 | 0.568 | 0.033 | |||||
| ACMG classification [11] criteria | Pathogenic | Likely pathogenic | Likely pathogenic | Pathogenic | Pathogenic | Pathogenic | Pathogenic | Pathogenic | Pathogenic |
| PS2, PM1, PM2, PP3, PP4 | PM1, PM2, PP3, PP4 | PS3, PM2, PM5a, PP3 | PVS1, PM2, PP1, PP3 | PVS1, PM2, PP3 | PS1, PS2, PM2, PP3 | PSV1, PS1, PS2, PM2, PP3 | PSV1, PS2, PM2, PP3, PP4 | PS1, PS2, PM2 | |
Accession number IGF2 NM_000612.6, CDKN1C NM_000076.2, PLAG1 NM_002655.3, IGF1R NM_000875.5, PIK3R1 NM_181523.3, SRCAP NM_006662.3, TCF4 NM_001083962.2, and PTPN11 NM_002834.5
SRS Silver-Russell syndrome, NE not examined, gnomAD Genome Aggregation Database, HGVD Human Genetic Variation Database, 4.7KJPN allele and genotype frequency panel from 4.7 K Japanese individuals, CADD Combined Annotation Dependent Depletion, SIFT Sorting Intolerant From Tolerant, PP2 Polymorphism Phenotyping v2, M-CAP Mendelian Clinically Applicable Pathogenicity
aA different missense variant (p.(Arg316Trp)) was reported in a patient with Bechwith-Wiedemann syndrome [21]
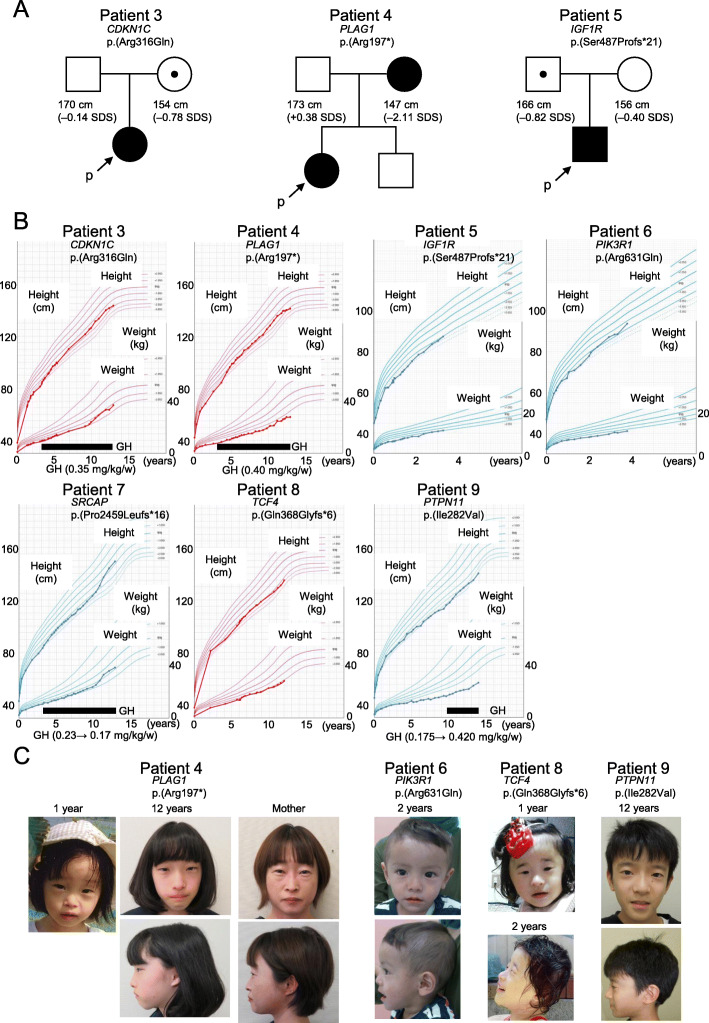
Patients 1 and 2 with IGF2 variants were already reported [12]. Both two variants, p.(Cys70Tyr) and p.(Cys71Arg), were predicted to disrupt S-S bindings in the IGF2 protein [22]. Patient 3 showed a rare variant, p.(Arg316Gln), causing amino acid alteration at the C-terminal of CDKN1C protein in the PCNA-binding domain[23]. This variant was inherited from her mother with normal height (Fig. 2a). To confirm pathogenicity of this variant, we performed functional analysis. Patient 4 showed a nonsense variant, p.(Arg197*), in PLAG1. Her mother with severe short stature also had the same variant (Fig. 2a). Patient 5 demonstrated a pathogenic frameshift variant, p.(Ser487Profs*21), in IGF1R. His father without severe short stature also showed the same variant (Fig. 2a). Patient 6 showed a missense variant, p.(Arg631Gln), in PIK3R1. This variant was previously reported in the patient with SHORT syndrome [24]. Patient 7 showed a frameshift variant, p.(Pro2459Leufs*16), in SRCAP, which is the causative gene for Floating-Harbor syndrome[25]. Patient 8 had a novel frameshift variant, p.(Gln368Glyfs*6), in TCF4. TCF4 is a causative gene for Pitt-Hopkins syndrome [26]. Patient 9 had a missense variant, p.(Ile282Val), in PTPN11, which was previously reported as a pathogenic gene mutation for Noonan syndrome [27]. Both parents of patients 6, 7, 8, and 9 did not have the variants identified in their children.
Fig. 2.
Clinical findings of the patients identified in this study. a Pedigrees of patients with variants inherited from their parents. b Growth charts. c Photographs of the patients and the mother of patient 4. Patients 1 and 2 were already reported [12]. SDS, standard deviation score; GH, growth hormone
Functional analysis
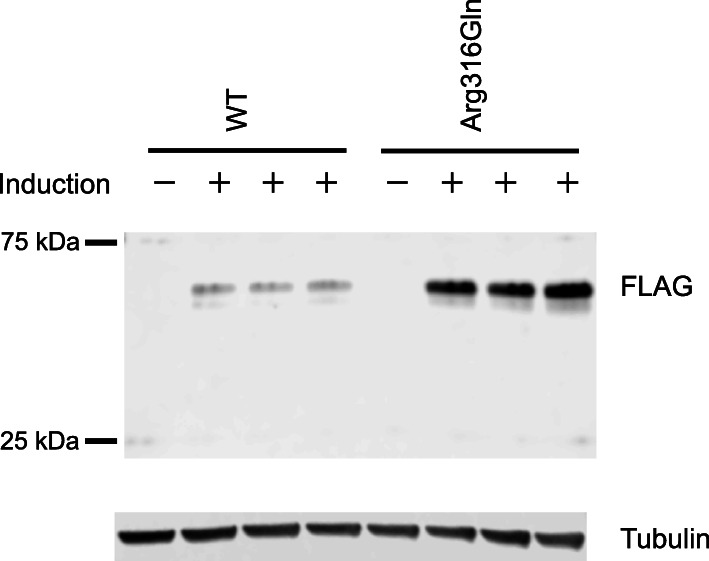
To evaluate the effect of the identified CDKN1C variant (Arg316Gln) on protein expression, we created expression vectors encoding the CDKN1C protein, expressed each CDKN1C protein, and detected them with Western blotting. The analysis revealed that the protein expression level of Arg316Gln-CDKN1C was higher than that of wildtype (WT)-CDKN1C (Fig. 3), suggesting that the variant positively affected the stability of CDKN1C protein.
Fig. 3.
Results of Western blot analysis. The doxycycline-inducible protein expression level of Arg316Gln-CDKN1C was higher than that of WT-CDKN1C. The experiment was conducted in triplicate. WT, wildtype
Clinical analysis
Clinical features of the nine patients with pathogenic or likely pathogenic variants are summarized in Table 2. All four patients with variants in the genes responsible for SRS (IGF2, CDKN1C, and PLAG1) had a diagnosis of “clinical SRS.” However, only two out of five patients with variants in causative genes for known genetic syndromes had a diagnosis of “clinical SRS.” Patients 1 and 2 with IGF2 variants showed motor and intellectual developmental delay, genital features, and high NH-CSS score (≥ 5/6) including feeding difficulties[12]. Patient 3 with a CDKN1C variant satisfied four NH-CSS criteria, but she did not show body asymmetry. She did not show other clinical features such as adrenal insufficiency or metaphyseal dysplasia, which were observed in the patients with IMAGe syndrome with gene mutation in the PCNA-binding domain of CDKN1C [23]. Growth hormone (GH) therapy was performed from 3 to 12 years old and was effective for her height (Fig. 2b). Her intellectual development was normal. Patient 4 with a PLAG1 variant met NH-CSS criteria, including protruding forehead (Fig. 2c), but she did not show body asymmetry. She demonstrated severe feeding difficulties requiring cyproheptadine for appetite stimulation and enteral nutrient. Although she had diagnosed attention-deficit hyperactivity disorder (ADHD) and was not good at her studies, she showed apparently normal intellectual development and went to a regular class at school. After GH therapy was started, she developed hypothyroidism and required levothyroxine. Her father and brother were within normal height; however, her mother with the same variant was 147 cm tall (− 2.11 standard deviation score (SDS)) (Fig. 2a). She was born at term with the weight of 2150 g. She did not have typical facial features of SRS, such as protruding forehead and triangular face in adulthood (Fig. 2c). Unfortunately, her photograph at infancy was not available.
Table 2.
Clinical features of the patients with pathogenic or likely pathogenic variants
| Patient | Patients with pathogenic or likely pathogenic variants in the responsible genes for SRS | Patients with pathogenic variants in causative genes for known genetic syndromes presenting with growth failure | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Patient 1 [12] | Patient 2 [12] | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Patient 7 | Patient 8 | Patient 9 | |
| Genetic diagnosis | SRS | SRS | SRS | SRS | IGF1R abnormality | SHORT syndrome | Floating-Harbor syndrome | Pitt-Hopkins syndrome | Noonan syndrome |
| Gene | IGF2 | IGF2 | CDKN1C | PLAG1 | IGF1R | PIK3R1 | SRCAP | TCF4 | PTPN11 |
| Variant | p.(Cys70Tyr) | p.(Cys71Arg) | p.(Arg316Gln) | p.(Arg197*) | p.(Ser487Profs*21) | p.(Arg631Gln) | p.(Pro2459Leufs*16) | p.(Gln368Glyfs*6) | p.(Ile282Val) |
| Sex | Male | Male | Female | Female | Male | Male | Male | Female | Male |
| Age at the last examination (years) | 8 | 15 | 12 | 12 | 3 | 3 | 12 | 12 | 13 |
| Gestational age (weeks:days) | 36:0 | 37:4 | 33:1 | 38:5 | 39:3 | 41:1 | 38:2 | 36:0 | 33:6 |
| Birth length in cm (SDS)a | 34.5 (− 3.85) | 39.0 (− 3.54) | 38.3 (− 1.95) | 42.0 (− 3.12) | 45.0 (− 2.11) | 47.0 (− 1.65) | 43.0 (− 2.49) | 38.0 (− 2.97) | 45.0 (+ 0.47) |
| Birth weight in g (SDS)a | 1164 (− 4.23) | 1336 (− 4.23) | 1120 (− 2.85) | 1804 (− 3.28) | 2292 (− 2.22) | 2386 (− 3.01) | 2332 (− 1.90) | 1508 (− 2.79) | 2130 (+ 0.04) |
| Birth OFC in cm (SDS)a | 31.0 (− 0.72) | 30.8 (− 1.49) | 28.1 (− 1.12) | 32.0 (− 0.86) | 32.9 (− 0.28) | 33.0 (− 0.54) | 32.0 (− 0.80) | 28.5 (− 2.28) | 31.8 (+ 0.68) |
| Height at 24 months in cm (SDS)b,c | 70.9 (− 4.63) | 72.5 (− 4.29) | 75.1 (− 3.34) | 77.6 (− 3.42) | 78.9 (− 2.38) | 77.9 (− 2.50) | 79.2 (− 3.37) | 81.4 (− 1.44) | 80.7 (− 2.20) |
| BMI at 24 months (SDS)b,c | − 2.70 | − 1.19 | − 1.26 | − 2.76 | − 2.09 | − 1.94 | 0.44 | − 3.19 | − 1.29 |
| Height at the last examination in cm (SDS)b | 108.8 (− 3.26) | 141.5 (− 4.68) | 143.5 (− 1.73) | 141.6 (− 2.06) | 87.9 (− 2.03) | 93.8 (− 1.27) | 149.2 (− 0.76) | 134.9 (− 2.33) | 140.1 (− 3.09) |
| Weight at the last examination in kg (SDS)b | 14.6 (− 5.25) | 30.5 (− 5.81) | 36.9 (− 1.22) | 28.0 (− 2.99) | 11.5 (− 1.79) | 11.2 (− 2.70) | 38.6 (− 0.85) | 28.1 (− 2.17) | 26.6 (− 4.31) |
| GH treatment | 6 years~ | 7 ~ 15 years | 3 ~ 12 years | 3 ~ 12 years | − | − | 3 years~ | − | 9 years~ |
| SGAd | + | + | + | + | + | + | + | + | − |
| Postnatal growth failurec,e | + | + | + | + | + | + | + | − | + |
| Relative macrocephaly at birthf | + | + | + | + | + | + | + | − | − |
| Protruding forehead | + | + | + | + | + | + | − | + | + |
| Body asymmetry | − | + | − | − | − | − | − | − | − |
| Feeding difficulties and/or low BMI | + | + | − | + | + | − | − | + | + |
| NH-CSS | 5/6 | 6/6 | 4/6 | 5/6 | 5/6 | 4/6 | 3/6 | 3/6 | 3/6 |
| Triangular face | + | + | + | + | + | + | + | − | + |
| Fifth finger clinodactyly | + | + | − | + | + | − | + | + | − |
| Fifth finger brachydactyly | + | + | − | + | + | − | + | + | + |
| Present characteristic features of genetic syndrome caused by the pathogenic variant | SGA, postnatal growth failure, feeding difficulties, triangular face, high plasma IGF-1 levels | SGA, postnatal growth failure, protruding forehead, triangular face, micrognathia, dental delay, low-set ears | SGA, postnatal growth failure, relative macrocephaly, triangular face, delayed bone age in early childhood, speech delay, bulbous nose, broad fingertips | Narrow forehead, thin lateral eyebrows, wide nasal bridge/ridge/tip, flared nasal alae, full cheeks/prominent midface, wide mouth/full lips/cupid bow upper lip, thickened/overfolded helices, severe developmental delay, breathing regulation anomalies (intermittent hyperventilation, apnea) (10 years~) | Postnatal growth failure, triangular face, chest deformity, cubitus valgus, hypertelorism | ||||
| Absent characteristic features of genetic syndrome caused by the pathogenic variant | Microcephaly, pectus excavatum, developmental delay | Lipoatrophy, inguinal hernia, deep-set eyes, Rieger abnormality, hyperextensibility of joints, speech delay, sensorineural deafness | Long eyelashes, deep-set eyes, short philtrum | Myopia, constipation, unstable gait | Pulmonary valve stenosis, hypertrophic cardiomyopathy, lymphedema, disordered bleeding, cryptorchidism, down-slanting of palpebral fissures, ptosis, low-set ears, low posterior hairline, webbed neck | ||||
| Development | |||||||||
| Motor developmental delay | + | + | − | − | − | − | − | + | − |
| Age at head control (months) | 5 | 6 | 4 | 4 | 4 | 4 | Unknown | 12 | 4 |
| Age at sitting without support (years) | 1.0 | 0.8 | 0.6 | 0.7 | 0.5 | 0.7 | Unknown | Unknown | 0.8 |
| Age at walking without support (years) | 1.5 | 1.3 | 1.0 | 1.0 | 1.3 | 1.3 | Unknown | 4.8 | 1.1 |
| Speech delay | + | + | − | − | − | − | + | + | − |
| IQ/DQ (age at examination) | 77 (3 years) | 79 (6 years) | Unknown | Unknown | NE | NE | Unknown | 17 (6 years) | NE |
| Other features | Cleft palate, hypospadias, bifid scrotum, hypoplastic finger nails | Cleft palate, hypospadias, syndactyly | Left inguinal hernia, café au lait spot, Mongolian spot, bronchial asthma, dysmenorrhea | ADHD, hypothyroidism (5 years~) | − | − | Perthes disease, hematoma in the left temporal lobe, atopic dermatitis | − | − |
| Paternal height in cm (SDS) | Unknown | 169 (− 0.31) | 170 (− 0.14) | 173 (+ 0.38) | 166 (− 0.82) | 170 (− 0.14) | 174 (+ 0.55) | 170 (− 0.14) | 187 (+ 2.78) |
| Maternal height in cm (SDS) | 150 (− 1.54) | 159 (+ 0.17) | 154 (− 0.78) | 147 (− 2.11) | 156 (− 0.40) | 158 (− 0.02) | 161 (+ 0.55) | 156 (− 0.40) | 167 (+ 1.70) |
SRS Silver-Russell syndrome, SDS standard deviation score, OFC occipitofrontal circumference, BMI body mass index, GH growth hormone, SGA small for gestational age, NH-CSS Netchine-Harbison clinical scoring system, IQ intelligence quotient, DQ developmental quotient, NE not examined, ADHD attention-deficit hyperactivity disorder
aBirth length, weight, and OFC were evaluated by the sex- and the gestational age-matched Japanese reference data (http://jspe.umin.jp/medical/chart_dl.html)
b Postnatal height, BMI, and weight were evaluated by the sex- and the age-matched Japanese reference data (http://jspe.umin.jp/medical/chart_dl.html)
cIf we did not get information at 24 ± 1 months, we used the data at the nearest measure available older than 25 months
dBirth length and/or birth weight ≤ − 2 SDS
eHeight at 24 ± 1 months ≤ − 2 SDS or height ≤ − 2 SDS below mid-parental target height. Mid-parental target height was calculated as follows: ((father’s height + mother’s height)/2) + 6.5 cm for boys and − 6.5 cm for girls.
fHead circumference at birth ≥ 1.5 SDS above birth length and/or weight SDS
Patients 5, 6, and 7 had genetically diagnosed IGF1R abnormality, SHORT syndrome, and Floating-Harbor syndrome, respectively, which have phenotypic overlap with SRS [1]. Patient 5 with five NH-CSS criteria showed many clinical features observed in the patients with IGF1R abnormality, such as growth failure and triangular face [28]. His plasma IGF-1 level was 121 ng/mL (+ 1.36 SDS) at 1 year old [29]. The father of patient 5 with the same IGF1R abnormality was 166 cm tall (− 0.82 SDS) and was born appropriate for gestational age (Fig. 2a). Patient 6 satisfying NH-CSS criteria had many symptoms of SHORT syndrome, such as prenatal and postnatal growth failure, characteristic facial features, and dental delay, but he did not show lipoatrophy nor hyperextensibility of joints (Fig. 2c) [24]. Patient 7 had three NH-CSS criteria and triangular face, fifth finger clinodactyly, and brachydactyly, together with Floating-Harbor syndrome-like clinical features, such as delayed bone age in his childhood, speech delay, bulbous nose, and broad fingertips [25]. GH treatment for SGA-short stature was started at 3 years old. During GH treatment, the dose was reduced due to development of Perthes disease (Fig. 2b). Hematoma in the left temporal lobe was incidentally detected by head magnetic resonance imaging. In addition, he suffered from severe atopic dermatitis.
Patients 8 and 9 had genetically diagnosed Pitt-Hopkins syndrome and Noonan syndrome, respectively, which are associated with growth failure [26, 30]. Patient 8 showed three NH-CSS criteria, including protruding forehead with fifth finger clinodactyly and brachydactyly together with severe developmental delay, but not breathing regulation anomalies characteristic of Pitt-Hopkins syndrome [26], when she was referred to us for genetic examination (Fig. 2c). Patient 9 had three NH-CSS criteria and triangular face and fifth finger brachydactyly together with only partial clinical features of Noonan syndrome, such as chest deformity, cubitus valgus, and hypertelorism (Fig. 2c) [30].
Discussion
Out of the 92 patients with SRS phenotype, we identified four patients (4.3%) with pathogenic or likely pathogenic variants in responsible genes for SRS, and five patients (5.4%) with pathogenic variants in causative genes for known genetic syndromes showing growth failure. To our knowledge, three studies about multigene screening of etiology-unknown patients with SRS phenotype using next-generation sequencing have been reported (Additional file 3: Table S2) [3, 31, 32]. The numbers and clinical features of the patients, target genes, methods of multigene sequencing, and molecular analyses before multigene sequencing are different among these studies. Our study is the largest multigene sequencing study to date, including only the patients evaluated based on NH-CSS, and showed that around 10% of etiology-unknown patients with SRS phenotype are caused by pathogenic or likely pathogenic variants of the causative genes for SRS or genetic syndromes related to growth failure. In addition, our study included a single familial case and previous studies also reported two familial cases (Additional file 3: Table S2) [3, 31]. Because onsets in almost all of the patients with 11p15 LOM and upd(7)mat are sporadic [1], family history in patients with SRS phenotype suggests other mechanisms of their etiologies.
In this study, we identified patients 1 and 2 with IGF2 variants, which were previously reported [12], and patient 3 with a CDKN1C variant. This variant detected in patient 3 is the second variant in CDKN1C leading to SRS. CDKN1C protein inhibits cell growth [23]. Consistent with this, loss-of-function mutations result in Beckwith-Wiedemann syndrome showing overgrowth and gain-of-function mutations in the PCNA-binding domain lead to SRS and IMAGe syndrome presenting with growth failure [23, 33, 34]. Only one gain-of-function mutation in CDKN1C was reported in SRS patients until now [33, 34]. The novel CDKN1C variant found in the present study (Arg316Gln) was located in the last amino acid (C-terminal) in the protein, and we showed that the amino acid substitution causes increased protein expression in vitro. Considering the location of the variant, it is likely that the variant increases the amount of protein without changing the native biochemical function of the protein. Therefore, we speculate that the increased CDKN1C protein function (i.e., gain-of-function CDKN1C mutation) caused the disease phenotype in patient 3. According to the result of the functional analysis, this variant was classified as “likely pathogenic” [11]. Both patient 3 and the previously reported patient did not show body asymmetry [33, 34]. The absence of body asymmetry is reasonable because CDKN1C mutations derive from the germline, unlike mosaic distribution of 11p15 LOM leading to body asymmetry in many patients [1]. The mother of patient 3 showing normal height had the same variant. This variant is most likely on her paternal allele.
We identified the third pathogenic PLAG1 variant in patient 4. Both our patient and previously reported patients with PLAG1 mutations did not show body asymmetry [3]. Our patient showed relative macrocephaly; however, two out of three previously reported patients did not [3]. In addition, patient 4 developed ADHD and hypothyroidism, but these clinical findings were not described in the previously reported patients [3]. We also tried to compare the severity of growth failure of the patients with pathogenic PLAG1 variants with that of the patients with other (epi)genetic causes of SRS, namely, 11p15 LOM, upd(7)mat, and IGF2 and HMGA2 mutations. SDS of birth length in patient 4 with a pathogenic variant in PLAG1 was − 3.12, which was comparable with those in the three previously reported patients with PLAG1 mutations (− 2.3, − 2, and − 2.78) [3]. At birth, the lengths of the three patients with HMGA2 mutations in the literature were − 1.3, − 3.9, and − 4.8 SDS, respectively [3, 4]. Birth lengths of previously reported patents with 11p15 LOM, upd(7)mat, and IGF2 mutations were − 4.13 ± 2.01, − 3.18 ± 1.16, and − 4.2 ± 0.9 SDS, respectively [2, 12]. Patients with pathogenic PLAG1 variants and upd(7)mat may show milder growth failure than those with 11p15 LOM and IGF2 and HMGA2 mutations. Further accumulation of patients will clarify the clinical features of SRS caused by PLAG1 variants.
We diagnosed the genetic causes of patients 5, 6, and 7 as IGF1R abnormality, SHORT syndrome, and Floating-Harbor syndrome, respectively. IGF1R abnormality, SHORT syndrome, and Floating-Harbor syndrome are differential diagnoses of SRS because of the shared phenotypes among these syndromes and SRS [1]. Because patients 5 and 6 did not have relative microcephaly and lipoatrophy/hyperextensibility of joints, respectively, which are characteristic clinical features of IGF1R abnormality and SHORT syndrome [24, 28], clinical diagnosis of those in both patients might be difficult. In addition, when patient 6 was referred to us at 2 years of age, his characteristic features of SHORT syndrome were not yet detectable. The medical conditions of infantile patients or patients without typical clinical features of a specific genetic disease may be misdiagnosed as SRS by attending physicians. Two additional matters are also worth pointing out. First, the father of patient 5 who had the same IGF1R frameshift variant did not show severe short stature. This may be because of phenotypic variability in the patients with IGF1R abnormality [28]. To our knowledge, four patients with pathogenic or likely pathogenic heterozygous variants in IGF1R were reported to have inherited them from parents with normal stature [28, 35]. Second, patient 7 with Floating-Harbor syndrome suffered from Perthes disease. Recently, Milani et al. reported a patient with Floating-Harbor syndrome complicated by Perthes disease [36]. Our patient also developed hematoma in the left temporal lobe. Three Floating-Harbor syndrome patients with intracranial hemorrhage with a background of cerebral aneurysm have been reported [37], although our patient did not show aneurysm. Perthes disease and intracranial hemorrhage may be characteristic features of Floating-Harbor syndrome.
Patients 8 and 9 had genetically diagnosed Pitt-Hopkins syndrome and Noonan syndrome, respectively. In general, the clinical features of both Pitt-Hopkins syndrome and Noonan syndrome are not very similar to those of SRS [26, 30]. Especially, Pitt-Hopkins syndrome is not a differential diagnosis for SRS at all [26]. Patient 8 showed atypical features of Pitt-Hopkins syndrome, such as SGA and mild protruding forehead, and typical features of this syndrome, such as severe developmental delay, but not breathing abnormalities, when she was referred to us [26]. Because patients with 11p15 LOM and upd(7)mat infrequently show severe developmental delay [38], this symptom suggests other etiologies. The phenotype of patient 9 was not typical of Noonan syndrome. Noonan syndrome has variable clinical expressivity [30]. A single patient with a PTPN11 mutation clinically suspected as SRS was reported [39]. Atypical clinical features, in some monogenic disorders, may result in clinical suspicion for SRS by presenting physicians.
Our sequencing analysis was performed in the context of an exploratory study using a multigene panel including four genes responsible for SRS and 406 genes related to growth failure and/or skeletal dysplasia. Interpreting the results of a sequencing analysis is easier using a multigene panel compared to whole-exome sequencing (WES) since the former involves a smaller number of detected rare variants. With regard to the screening of SRS phenotypic patients using a multigene panel, the genes included in the panel should focus on the genes responsible for SRS and the causative genes for genetic syndromes with clinical features that overlap with those of SRS to simplify the assessment of the results.
Our results confirmed the importance of relative macrocephaly and protruding forehead among NH-CSS criteria due to the high prevalence of “clinical SRS” in four patients with variants in the responsible genes for SRS (IGF2, CDKN1C, and PLAG1) and the low prevalence of “clinical SRS” in five patients with variants in causative genes for known genetic syndromes. For etiology-unknown patients who are not “clinical SRS,” genetic disorders other than SRS may be considered.
In this study, multigene sequencing showed various pathogenic or likely pathogenic variants in SRS phenotypic patients with unknown etiology. Disease-specific medical management and genetic counseling based on a precise genetic diagnosis can be used to improve the prognosis and quality of life of these patients. For example, GH therapy should be performed carefully in patient 5 with IGF1R abnormality and patient 6 with SHORT syndrome, due to insulin resistance and a high risk of developing diabetes mellitus [24, 28]. Similarly, a regular cardiac follow-up to screen for hypertrophic cardiomyopathy should be carried out in patient 9 with Noonan syndrome [30].
Conclusions
We identified nine patients (9.8%) with pathogenic or likely pathogenic variants in 92 etiology-unknown patients with SRS phenotype. Notably, we identified the second CDKN1C and the third PLAG1 variants leading to SRS. As a result, this study expands the molecular spectrum of SRS phenotype.
Methods
Patients
We included 92 patients out of 336 patients referred to us for genetic testing for SRS from 2002 to 2018 in this study. The inclusion criteria of this study are summarized in Fig. 1. For 92 patients with SRS phenotype, we ruled out 11p15 LOM and upd(7)mat by methylation analysis. None of the patients showed abnormal methylation levels for six DMRs, namely, PLAGL1:alt-TSS-DMR on chromosome 6, KCNQ1OT1:TSS-DMR on chromosome 11, MEG3/DLK1:IG-DMR on chromosome 14, MEG3:TSS-DMR on chromosome 14, SNURF:TSS-DMR on chromosome 15, and GNAS A/B:TSS-DMR on chromosome 20, or PCNVs. Furthermore, we excluded upd(16)mat by methylation analysis. Methylation analysis was performed by combined bisulfite restriction analysis or pyrosequencing and copy number analysis was performed using the SurePrint G3 Human CGH Array Kit 8x60K (catalog number G4450A, Agilent Technologies, Palo Alto, CA, USA) as previously reported [2,5, 40]. Our 92 patients were all Japanese, apart from two patients from Canada and the USA.
Clinical information of the patients was collected from attending physicians by questionnaire. Attending physicians consisted of general pediatricians, neonatologists, pediatric endocrinologists, and pediatric geneticists. Of the 92 patients, 63 patients satisfied NH-CSS. The remaining 29 patients met only three NH-CSS criteria but were clinically suspected as having SRS. Because triangular face, fifth finger clinodactyly, and/or brachydactyly were frequently observed in SRS patients [2] and patients are often considered as having SRS based on these features by their attending physicians, we regarded these features as clinical findings related to SRS. For patients under 23 months old, the score for postnatal growth retardation was excluded from the NH-CSS criteria.
Molecular analysis
Using next-generation sequencing, we performed mutation screening for four genes responsible for SRS and 406 genes related to growth failure and/or skeletal dysplasia (Additional file 1: Table S1). We selected these 406 genes based on the previous reports by Meyer et al. [31] and Wang et al. [39]. Out of 92 patients, four patients were analyzed by WES and the remaining 88 patients were screened using target resequencing. For WES, enriched libraries generated using SureSelect Human All Exon V6 kit (Agilent Technologies, Santa Clara, CA, USA) were sequenced on a Hiseq X or Novaseq 6000 (Illumina, San Diego, CA, USA) operated in a 150-bp paired-end mode. For target resequencing, enriched libraries generated using a custom-made HaloPlex Target Enrichment System (Agilent Technologies, Santa Clara, CA, USA) were sequenced on a Hiseq 1500/2500/X (Illumina, San Diego, CA, USA) operated in a 100-bp paired-end mode. For WES and target resequencing, x20 coverage on average was reached in 98.7% and 89.2% of regions of interest, respectively.
Sequence reads were processed, mapped, and analyzed as previously reported [41]. In brief, adaptor sequences were removed using cutadapt 1.7.1/1.14. Sequence reads were mapped against the human reference genome data (hg19/GRCh37) using the Burrows-Wheeler Aligner 0.7.12/0.7.13. The PCR duplicates were removed by Picard 1.130/2.1.1. The Genome Analysis Toolkit 3.3/3.5 was used to perform local realignment, base quality score recalibration, and variant calling. Subsequently, we extracted rare variants based on the Genome Aggregation Database [13], Human Genetic Variation Database [14], 4.7KJPN [15], and in-house control data. Conformation and segregation of the rare variants were performed by Sanger sequencing using a standard technique. The primer sequences and experimental conditions are available on request.
Because PLAG1 is a new responsible gene for SRS, this gene was not included in the target genes of our custom-made HaloPlex Target Enrichment System. For the 88 patients subjected to target resequencing, we performed Sanger sequencing for the coding regions and splice sites of PLAG1 (NM_002655.3) following long PCR amplification using KOD FX Neo (Toyobo, Osaka, Japan) according to the manufacturer’s instructions. The primer sets used for Sanger sequencing are shown in Additional file 4: Table S3.
The rare variants detected by sequencing were evaluated on the bases of the American College of Medical Genetics Standards and Guidelines [11]. We extracted the variants classified as “pathogenic” or “likely pathogenic.” For in silico pathogenicity prediction, we adopted CADD [16], MutationTaster [17], SIFT [18], PolyPhen-2 (HumVar) [19], and M-CAP [20].
Functional analysis
We established HEK293 cell lines that stably express N-terminal 3xFLAG-tagged human CDKN1C cDNA (WT or Arg316Gln) in the presence of doxycycline. The doxycycline-inducible piggyBac backbone vector has been described previously [42]. We introduced the human CDKN1C cDNA sequence (WT or Arg316Gln) into the backbone vector with the Gibson assembly technique. HEK293 cells were co-transfected with each piggyBac vector and the piggyBac transposase expression vector (System Biosciences, Mountain View, CA, USA) using Lipofectamine 3000 (Thermo Fisher Scientific, Waltham, MA, USA). Stable cells were established according to the manufacturer’s protocol.
Whole cell lysates were prepared from inducible stable cells maintained with or without 1 μg/mL doxycycline for 48 h. We performed Western blotting with anti-FLAG M2 antibody (Sigma-Aldrich, St Louis, MO, USA) and anti-tubulin antibody (Abcam, Cambridge, UK) as primary antibodies.
Supplementary information
Additional file 1: Table S1. File format: Excel spreadsheet. Gene list screened in this study.
Additional file 2: Figure S1. File format: PowerPoint. Chromatograms of identified pathogenic or likely pathogenic variants. Arrows indicate mutated nucleotides.
Additional file 3: Table S2. File format: Excel spreadsheet. Summary of multigene screening studies for etiology-unknown patients with SRS phenotype using next-generation sequencing
Additional file 4: Table S3. File format: Excel spreadsheet. Primers utilized to detect mutations in PLAG1
Acknowledgements
We are grateful to all patients and their parents for their cooperation. We thank the attending physicians for providing us with detailed clinical data and materials for molecular studies.
Abbreviations
- ADHD
Attention-deficit hyperactivity disorder
- DMR
Differentially methylated region
- 11p15 LOM
Loss of methylation on chromosome 11p15
- GH
Growth hormone
- NH-CSS
Netchine-Harbison clinical scoring system
- PCNV
Pathogenic copy number variation
- SDS
Standard deviation score
- SGA
Small for gestational age
- SRS
Silver-Russell syndrome
- upd(7)mat
Maternal uniparental disomy of chromosome 7
- upd(16)mat
Maternal uniparental disomy of chromosome 16
- WES
Whole-exome sequencing
- WT
Wildtype
Authors’ contributions
Molecular analysis was performed by TI, AN, KM, KN, KY, and TF. Functional analysis was performed by TI, MIO, KTN, and SN. Detailed clinical data and materials for molecular studies were provided by JN, YM, YH, HS, SS, YK, NM, and TO. The study was designed and coordinated by MK. The paper was written by TI and MK, and reviewed and edited by SN, AO, and MF. All the authors read and approved the final manuscript.
Funding
This work was supported by grants from the National Center for Child Health and Development (28-6, 2019B4), the Japan Agency for Medical Research and Development (AMED) (20ek0109373h0003), the Foundation for Growth Science, and Takeda Science Foundation.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board Committee at the National Center for Child Health and Development (committee’s reference number: 518) and performed after obtaining written informed consent to participate in this study from the patients or the patients’ parents.
Consent for publication
We obtained written informed consent from the patients or the patients’ parents to publish patients’ clinical and molecular information as well as facial photographs.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Takanobu Inoue, Email: [email protected].
Akie Nakamura, Email: [email protected].
Megumi Iwahashi-Odano, Email: [email protected].
Kanako Tanase-Nakao, Email: [email protected].
Keiko Matsubara, Email: [email protected].
Junko Nishioka, Email: [email protected].
Yoshihiro Maruo, Email: [email protected].
Yukihiro Hasegawa, Email: [email protected].
Hiroshi Suzumura, Email: [email protected].
Seiji Sato, Email: [email protected].
Yoshiyuki Kobayashi, Email: [email protected].
Nobuyuki Murakami, Email: [email protected].
Kazuhiko Nakabayashi, Email: [email protected].
Kazuki Yamazawa, Email: [email protected].
Tomoko Fuke, Email: [email protected].
Satoshi Narumi, Email: [email protected].
Akira Oka, Email: [email protected].
Tsutomu Ogata, Email: [email protected].
Maki Fukami, Email: [email protected].
Masayo Kagami, Email: [email protected].
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13148-020-00865-x.
References
- 1.Wakeling EL, Brioude F, Lokulo-Sodipe O, O'Connell SM, Salem J, Bliek J, et al. Diagnosis and management of Silver-Russell syndrome: first international consensus statement. Nat Rev Endocrinol. 2017;13:105–124. doi: 10.1038/nrendo.2016.138. [DOI] [PubMed] [Google Scholar]
- 2.Fuke T, Mizuno S, Nagai T, Hasegawa T, Horikawa R, Miyoshi Y, et al. Molecular and clinical studies in 138 Japanese patients with Silver-Russell syndrome. PLoS One. 2013;8:e60105. doi: 10.1371/journal.pone.0060105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abi Habib W, Brioude F, Edouard T, Bennett JT, Lienhardt-Roussie A, Tixier F, et al. Genetic disruption of the oncogenic HMGA2-PLAG1-IGF2 pathway causes fetal growth restriction. Genet Med. 2018;20:250–258. doi: 10.1038/gim.2017.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Crescenzo A, Citro V, Freschi A, Sparago A, Palumbo O, Cubellis MV, et al. A splicing mutation of the HMGA2 gene is associated with Silver-Russell syndrome phenotype. J Hum Genet. 2015;60:287–293. doi: 10.1038/jhg.2015.29. [DOI] [PubMed] [Google Scholar]
- 5.Inoue T, Nakamura A, Fuke T, Yamazawa K, Sano S, Matsubara K, et al. Genetic heterogeneity of patients with suspected Silver-Russell syndrome: genome-wide copy number analysis in 82 patients without imprinting defects. Clin Epigenetics. 2017;9:52. [DOI] [PMC free article] [PubMed]
- 6.Kagami M, Nagasaki K, Kosaki R, Horikawa R, Naiki Y, Saitoh S, et al. Temple syndrome: comprehensive molecular and clinical findings in 32 Japanese patients. Genet Med. 2017;19:1356–66. [DOI] [PMC free article] [PubMed]
- 7.Kawashima S, Nakamura A, Inoue T, Matsubara K, Horikawa R, Wakui K, et al. Maternal uniparental disomy for chromosome 20: physical and endocrinological characteristics of five patients. J Clin Endocrinol Metab. 2018;103:2083–8. [DOI] [PubMed]
- 8.Yamazawa K, Nakabayashi K, Kagami M, Sato T, Saitoh S, Horikawa R, et al. Parthenogenetic chimaerism/mosaicism with a Silver-Russell syndrome-like phenotype. J Med Genet. 2010;47:782–5. [DOI] [PMC free article] [PubMed]
- 9.Luk HM, Ivan Lo FM, Sano S, Matsubara K, Nakamura A. Ogata T, et al. Silver-Russell syndrome in a patient with somatic mosaicism for upd(11)mat identified by buccal cell analysis. Am J Med Genet A. 2016;170:1938–41. [DOI] [PMC free article] [PubMed]
- 10.Inoue T, Yagasaki H, Nishioka J, Nakamura A, Matsubara K, Narumi S, et al. Molecular and clinical analyses of two patients with UPD(16)mat detected by screening 94 patients with Silver-Russell syndrome phenotype of unknown aetiology. J Med Genet. 2019;56:413–8. [DOI] [PMC free article] [PubMed]
- 11.Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24. [DOI] [PMC free article] [PubMed]
- 12.Masunaga Y, Inoue T, Yamoto K, Fujisawa Y, Sato Y, Kawashima-Sonoyama Y, et al. IGF2 mutations: report of five cases, review of the literature, and comparison with H19/IGF2:IG-DMR epimutations. J Clin Endocrinol Metab. 2020;105:116–25. [DOI] [PubMed]
- 13.Genome Aggregation Database. http://gnomad.broadinstitute.org. Accessed 5 Mar 2020.
- 14.Human Genetic Variation Database. http://www.hgvd.genome.med.kyoto-u.ac.jp. Accessed 5 Mar 2020.
- 15.4.7KJPN, allele and genotype frequency panel from 4.7 K Japanese individuals. https://jmorp.megabank.tohoku.ac.jp. Accessed 5 Mar 2020.
- 16.CADD (Combined Annotation Dependent Depletion). http://cadd.gs.washington.edu/score. Accessed 5 Mar 2020.
- 17.MutationTaster. http://www.mutationtaster.org. Accessed 5 Mar 2020.
- 18.SIFT (Sorting Intolerant From Tolerant). https://sift.bii.a-star.edu.sg. Accessed 5 Mar 2020.
- 19.PolyPhen-2 (HumVar). http://genetics.bwh.harvard.edu/pph2. Accessed 5 Mar 2020.
- 20.M-CAP (Mendelian Clinically Applicable Pathogenicity). http://bejerano.stanford.edu/mcap. Accessed 5 Mar 2020.
- 21.Lam WW, Hatada I, Ohishi S, Mukai T, Joyce JA, Cole TR, et al. Analysis of germline CDKN1C (p57KIP2) mutations in familial and sporadic Beckwith-Wiedemann syndrome (BWS) provides a novel genotype-phenotype correlation. J Med Genet. 1999;36:518–23. [PMC free article] [PubMed]
- 22.O'Dell SD, Day IN. Insulin-like growth factor II (IGF-II). Int J Biochem Cell Biol. 1998;30:767–71. [DOI] [PubMed]
- 23.Arboleda VA, Lee H, Parnaik R, Fleming A, Banerjee A, Ferraz-de-Souza B, et al. Mutations in the PCNA-binding domain of CDKN1C cause IMAGe syndrome. Nat Genet. 2012;44:788–92. [DOI] [PMC free article] [PubMed]
- 24.Avila M, Dyment DA, Sagen JV, St-Onge J, Moog U, Chung BHY, et al. Clinical reappraisal of SHORT syndrome with PIK3R1 mutations: toward recommendation for molecular testing and management. Clin Genet. 2016;89:501–6. [DOI] [PubMed]
- 25.Nikkel SM, Dauber A, de Munnik S, Connolly M, Hood RL, Caluseriu O, et al. The phenotype of Floating-Harbor syndrome: clinical characterization of 52 individuals with mutations in exon 34 of SRCAP. Orphanet J Rare Dis. 2013;8:63. [DOI] [PMC free article] [PubMed]
- 26.Zollino M, Zweier C, Van Balkom ID, Sweetser DA, Alaimo J, Bijlsma EK, et al. Diagnosis and management in Pitt-Hopkins syndrome: first international consensus statement. Clin Genet. 2019;95:462–78. [DOI] [PubMed]
- 27.Tartaglia M, Mehler EL, Goldberg R, Zampino G, Brunner HG, Kremer H, et al. Mutations in PTPN11, encoding the protein tyrosine phosphatase SHP-2, cause Noonan syndrome. Nat Genet. 2001;29:465–8. [DOI] [PubMed]
- 28.Walenkamp MJE, Robers JML, Wit JM, Zandwijken GRJ, van Duyvenvoorde HA, Oostdijk W, et al. Phenotypic features and response to GH treatment of patients with a molecular defect of the IGF-1 receptor. J Clin Endocrinol Metab. 2019;104:3157–71. [DOI] [PubMed]
- 29.Isojima T, Shimatsu A, Yokoya S, Chihara K, Tanaka T, Hizuka N, et al. Standardized centile curves and reference intervals of serum insulin-like growth factor-I (IGF-I) levels in a normal Japanese population using the LMS method. Endocr J. 2012;59:771–80. [DOI] [PubMed]
- 30.Romano AA, Allanson JE, Dahlgren J, Gelb BD, Hall B, Pierpont ME, et al. Noonan syndrome: clinical features, diagnosis, and management guidelines. Pediatrics. 2010;126:746–59. [DOI] [PubMed]
- 31.Meyer R, Soellner L, Begemann M, Dicks S, Fekete G, Rahner N, et al. Targeted next generation sequencing approach in patients referred for Silver-Russell syndrome testing increases the mutation detection rate and provides decisive information for clinical management. J Pediatr. 2017;187:206–12. [DOI] [PubMed]
- 32.Neuheuser L, Meyer R, Begemann M, Elbracht M, Eggermann T. Next generation sequencing and imprinting disorders: current applications and future perspectives: Lessons from Silver-Russell syndrome. Mol Cell Probes. 2019;44:1–7. [DOI] [PubMed]
- 33.Brioude F, Oliver-Petit I, Blaise A, Praz F, Rossignol S, Le Jule M, et al. CDKN1C mutation affecting the PCNA-binding domain as a cause of familial Russell Silver syndrome. J Med Genet. 2013;50:823–30. [DOI] [PubMed]
- 34.Sabir AH, Ryan G, Mohammed Z, Kirk J, Kiely N, Thyagarajan M, et al. Familial Russell-Silver syndrome like phenotype in the PCNA domain of the CDKN1C gene, a further case. Case Rep Genet. 2019;1398250. [DOI] [PMC free article] [PubMed]
- 35.Giabicani E, Willems M, Steunou V, Chantot-Bastaraud S, Thibaud N, Abi Habib W, et al. Increasing knowledge in IGF1R defects: lessons from 35 new patients. J Med Genet. 2020;57:160–8. [DOI] [PubMed]
- 36.Milani D, Scuvera G, Gatti M, Tolva G, Bonarrigo F, Esposito S, et al. Perthes disease: a new finding in Floating-Harbor syndrome. Am J Med Genet A. 2018;176:703–6. [DOI] [PubMed]
- 37.Menzies L, D'Arco F, Ganesan V, Hurst JA. Intracranial vascular pathology in two further patients with Floating-Harbor syndrome: proposals for cerebrovascular disease risk management. Eur J Med Genet. 2020;63:103785. [DOI] [PubMed]
- 38.Wakeling EL, Amero SA, Alders M, Bliek J, Forsythe E, Kumar S, et al. Epigenotype-phenotype correlations in Silver-Russell syndrome. J Med Genet. 2010;47:760–8. [DOI] [PMC free article] [PubMed]
- 39.Wang SR, Carmichael H, Andrew SF, Miller TC, Moon JE, Derr MA, et al. Large-scale pooled next-generation sequencing of 1077 genes to identify genetic causes of short stature. J Clin Endocrinol Metab. 2013;98:E1428–37. [DOI] [PMC free article] [PubMed]
- 40.Kagami M, Mizuno S, Matsubara K, Nakabayashi K, Sano S, Fuke T, et al. Epimutations of the IG-DMR and the MEG3-DMR at the 14q32.2 imprinted region in two patients with Silver-Russell syndrome-compatible phenotype. Eur J Hum Genet. 2015;23:1062–7. [DOI] [PMC free article] [PubMed]
- 41.Fukawatase Y, Toyoda M, Okamura K, Nakamura K, Nakabayashi K, Takada S, et al. Ataxia telangiectasia derived iPS cells show preserved x-ray sensitivity and decreased chromosomal instability. Sci Rep. 2014;4:5421. [DOI] [PMC free article] [PubMed]
- 42.Shima H, Koehler K, Nomura Y, Sugimoto K, Satoh A, Ogata T, et al. Two patients with MIRAGE syndrome lacking haematological features: role of somatic second-site reversion SAMD9 mutations. J Med Genet. 2018;55:81–5. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. File format: Excel spreadsheet. Gene list screened in this study.
Additional file 2: Figure S1. File format: PowerPoint. Chromatograms of identified pathogenic or likely pathogenic variants. Arrows indicate mutated nucleotides.
Additional file 3: Table S2. File format: Excel spreadsheet. Summary of multigene screening studies for etiology-unknown patients with SRS phenotype using next-generation sequencing
Additional file 4: Table S3. File format: Excel spreadsheet. Primers utilized to detect mutations in PLAG1
Data Availability Statement
Not applicable.