Abstract
Background
The provision of nutritional support for patients in intensive care units (ICUs) varies widely both within and between institutions. We tested the hypothesis that evidence-based algorithms to improve nutritional support in the ICU would improve patient outcomes.Methods
A cluster-randomized controlled trial was performed in the ICUs of 11 community and 3 teaching hospitals between October 1997 and September 1998. Hospital ICUs were stratified by hospital type and randomized to the intervention or control arm. Patients at least 16 years of age with an expected ICU stay of at least 48 hours were enrolled in the study (n = 499). Evidence-based recommendations were introduced in the 7 intervention hospitals by means of in-service education sessions, reminders (local dietitian, posters) and academic detailing that stressed early institution of nutritional support, preferably enteral.Results
Two hospitals crossed over and were excluded from the primary analysis. Compared with the patients in the control hospitals (n = 214), the patients in the intervention hospitals (n = 248) received significantly more days of enteral nutrition (6.7 v. 5.4 per 10 patient-days; p = 0.042), had a significantly shorter mean stay in hospital (25 v. 35 days; p = 0.003) and showed a trend toward reduced mortality (27% v. 37%; p = 0.058). The mean stay in the ICU did not differ between the control and intervention groups (10.9 v. 11.8 days; p = 0.7).Interpretation
Implementation of evidence-based recommendations improved the provision of nutritional support and was associated with improved clinical outcomes.Free full text

Multicentre, cluster-randomized clinical trial of algorithms for critical-care enteral and parenteral therapy (ACCEPT)
Abstract
Background
The provision of nutritional support for patients in intensive care units (ICUs) varies widely both within and between institutions. We tested the hypothesis that evidence-based algorithms to improve nutritional support in the ICU would improve patient outcomes.
Methods
A cluster-randomized controlled trial was performed in the ICUs of 11 community and 3 teaching hospitals between October 1997 and September 1998. Hospital ICUs were stratified by hospital type and randomized to the intervention or control arm. Patients at least 16 years of age with an expected ICU stay of at least 48 hours were enrolled in the study (n = 499). Evidence-based recommendations were introduced in the 7 intervention hospitals by means of in-service education sessions, reminders (local dietitian, posters) and academic detailing that stressed early institution of nutritional support, preferably enteral.
Results
Two hospitals crossed over and were excluded from the primary analysis. Compared with the patients in the control hospitals (n = 214), the patients in the intervention hospitals (n = 248) received significantly more days of enteral nutrition (6.7 v. 5.4 per 10 patient-days; p = 0.042), had a significantly shorter mean stay in hospital (25 v. 35 days; p = 0.003) and showed a trend toward reduced mortality (27% v. 37%; p = 0.058). The mean stay in the ICU did not differ between the control and intervention groups (10.9 v. 11.8 days; p = 0.7).
Interpretation
Implementation of evidence-based recommendations improved the provision of nutritional support and was associated with improved clinical outcomes.
Critical illness can lead to hypermetabolism and subsequent malnutrition.1,2 Malnutrition is strongly associated with increased morbidity and mortality rates among seriously ill patients.3,4 Thus, standards of care for patients with critical illness include nutritional support. Recent reviews suggest that enteral nutrition (EN) is associated with lower septic morbidity rates and that parenteral nutrition (PN) may be associated with increased rates of complications and death.5,6,7 Immune-enhancing diets may be beneficial for elective surgical patients but have no benefit and may harm the critically ill patient.6
If EN is preferable, starting sooner may be better. Data from the few animal and clinical studies on this topic support this hypothesis.7 However, recent observational studies have documented low rates of “optimal” use of EN in the critical care setting.8,9,10 EN is often started several days after admission, patients do not tolerate adequate amounts of EN, and PN is used excessively in some patients (up to 60% in some countries).8,9,10 Using an audit of intensive care units (ICUs) in community and teaching hospitals, our Critical Care Research Network (CCR-Net) also documented delays in the institution of nutritional support that included both enteral and parenteral routes.11 Several studies have shown that using nurse-directed feeding protocols or algorithms increases the amount of EN delivered daily12,13 and that enhancing delivery may improve outcomes in some patients.14 Protocols may improve this process.
We report a prospective, cluster-randomized clinical trial in the ICUs of community and teaching hospitals that tested the hypothesis that an evidence-based algorithm for nutritional support in critically ill patients, accompanied by a multifaceted implementation strategy, would improve the provision of nutritional support and patient outcomes.
Methods
The study consisted of a run-in phase followed by cluster randomization of hospitals to the intervention or control group. Cluster randomization reduces the risk of contamination between groups, but individual patient characteristics can still be evaluated by appropriate analysis.15
Patient enrolment into both phases of the study occurred from October 1997 to September 1998. Patients were included if they were at least 16 years of age and were expected to stay in the ICU at least 48 hours. Patients were excluded if they were expected to be receiving sufficient nutrition orally to meet their daily energy requirements within 24 hours after ICU admission, were admitted for palliative care, were moribund and not expected to survive for more than 6 hours, or were suspected to be brain dead. The Ethics Review Board at the University of Western Ontario waived the requirement for informed consent on the basis that the intervention was a quality-improvement initiative.
The study was conducted in 11 community and 3 teaching hospitals in Ontario. All hospitals that volunteered for the study were members of the CCR-Net,16 admitted both medical and surgical patients and had 6 to 30 ICU beds. Randomization, stratified by teaching status, was performed by means of a random-number table. One hospital declined to comply with the study intervention after learning that it had been randomly assigned to the intervention group. Since its loss would have led to problems with power, the hospital agreed to continue collecting data for the control group, and a hospital with similar stratification factors that had not yet been allocated to a study arm was assigned to the intervention group. Outcomes were analyzed with these 2 sites excluded and included (per-protocol analysis).
To standardize the type of EN, a closed EN system (Ultrapak; Nestlé Clinical Nutrition, Toronto, Ont.) was provided to all ICUs for the study. The ICUs switched to its use during the run-in phase and continued using it until the end of the study. No other intervention was performed during the run-in phase.
An evidence-based consensus conference held in November 1996 had reviewed the available evidence and developed evidence-based recommendations for nutritional support. The panelists — 5 physicians (4 intensive care physicians and 1 gastroenterologist), 5 dietitians and 1 epidemiologist — represented both teaching and community hospitals.
Before the conference, a literature review of 10 topics had been conducted with the use of English-language studies identified in MEDLINE. The panelists were presented with critical appraisals and the full text of relevant studies. Evidence was graded and evidence-based recommendations were developed by means of Browman and colleagues' Clinical Practice Guidelines Development Cycle.17 Consensus on the final recommendations, in the form of an algorithm, was reached through informal discussions between all participants. The key points were an emphasis on early nutrition, preference for the enteral route (with a list of conditions that required the parenteral route) and frequent re-evaluation. Recommendations for tolerance of tube feeding and for managing feeding-associated diarrhea were also created.
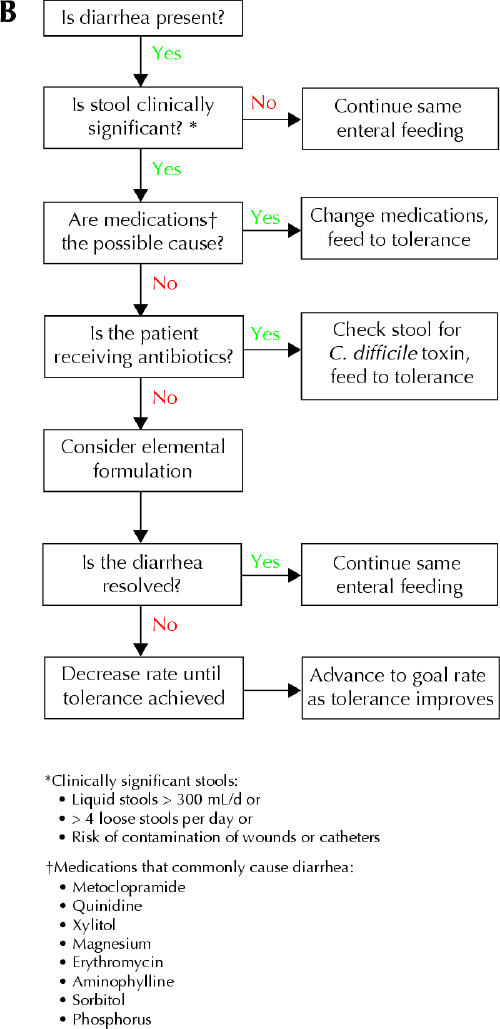
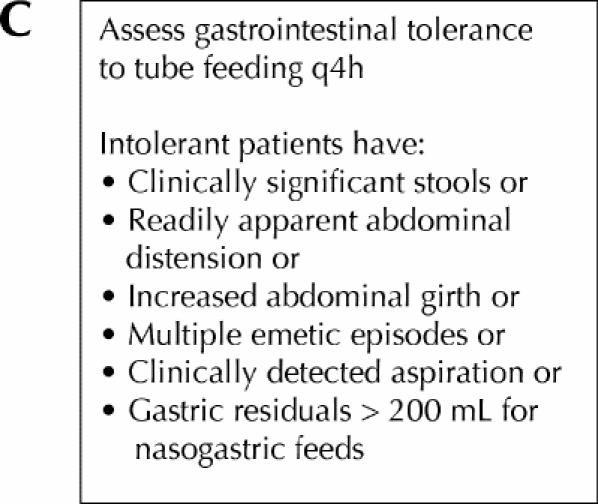
At the intervention hospitals the recommendations from the consensus conference, in the form of algorithms (Fig. 1), were implemented in the ICUs by means of approaches that have proven to be effective in changing physicians' practice patterns.18 First, at each ICU, immediately before the site began to use the algorithms, recognized academic opinion leaders (intensive care physicians from the coordinating centre and the epidemiologist managing the trial) provided an in-service educational session (a single didactic lecture) to describe the evidence supporting the recommendations and the clinical trial design to the physicians, nurses, respiratory therapists and dietitian. Second, laminated copies of the algorithms were posted at each ICU, and pocket cards were provided for the dietitian to give to the nurses and physicians. Third, the dietitian audited and recorded nutritional support daily and provided immediate feedback to the health care team to optimize compliance with the recommendations. All other aspects of patient care were at the discretion of the health care team.
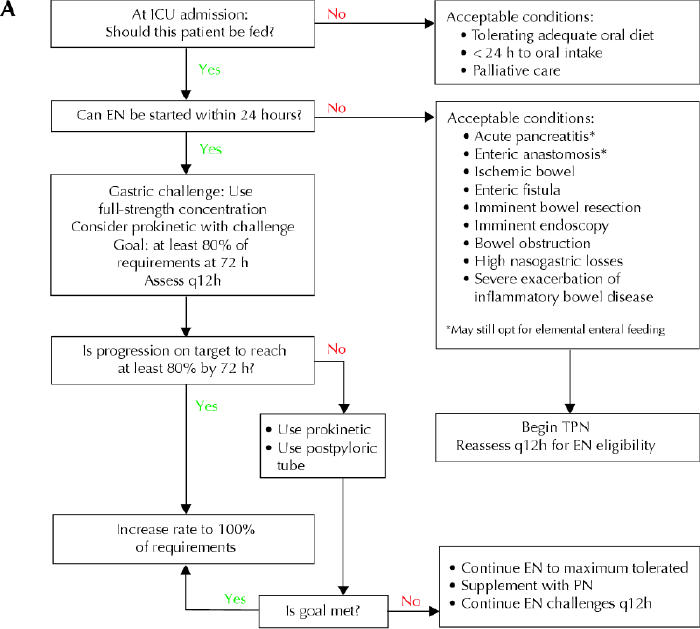
Fig. 1: Algorithms A, B and C (depicted on this page and the next one) for critical-care nutritional support, developed in 199617 and used in the intervention hospitals to guide selection and management and assist in the assessment of diarrhea associated with tube feeding and tolerance to tube feeding. ICU = intensive care unit, EN = enteral nutrition, TPN = total parenteral nutrition, PN = parenteral nutrition, C. = Clostridium.
All patient admissions were recorded in a minimum data set that included hospital and ICU admission and discharge dates and status, along with variables for calculating the APACHE II score for illness severity. These data were collected independently of the current study. An additional data set was used to capture the following daily: nutritional support, contraindications to nutritional support and reasons for changes to the amount or route of nutritional support.
At the control hospitals the dietitian collected the additional data required for the study but did not receive any further guidance or instructions regarding the provision of feedback.
At all of the hospitals, assessment of the patients' detailed nutritional requirements and prescription were left to the discretion of the ICU dietitian. All sites used the Harris–Benedict equation to estimate energy requirements. Two teaching hospital ICUs (1 in each group) used direct measurement of energy expenditure to adjust the nutritional prescription. Protein was provided at conventional rates, about 1.5 g protein/kg ideal body weight.
Except in the 2 larger teaching hospitals, the dietitians dedicated only a portion of their time to the ICU patients, but workload was not measured.
The primary outcomes were hospital mortality, length of ICU stay and length of hospital stay. Mortality was analyzed with the group-specific adjusted χ2 approach.19,20,21 Outcomes based on length of stay or count data (e.g., days from ICU admission to feeding, number of days fed), which may have a Poisson distribution, were analyzed with the approach of Rao and Scott.22 Baseline imbalance and the proportion of patients receiving EN, PN or no feeds by day were assessed by comparing the cluster-specific means and performing a standard 2-sample t test,23 a robust, conservative test that is widely supported by evidence from simulation studies and theoretical papers.24 Although with only 7 hospitals per group and a dichotomous outcome variable there is no fully satisfactory method of controlling for covariates, an extension of Poisson regression can be used to adjust for a mixture of cluster-level and individual-level covariates. The effects of factors found to be in imbalance at baseline were investigated with a negative binomial model.25
With cluster randomization, outcomes within study centres are not independent, and the sample size required to obtain a prespecified power in such a trial is often much greater than that required in a simple randomized trial. The ratio of the total number of subjects required with cluster randomization to the number required with simple randomization, known as the design effect,26,27,28 can be calculated with knowledge of the intracluster correlation coefficient (ρ) and the average cluster size. Wherever appropriate, we report group-specific design effects (C1 and C2).15
We conducted initial sample-size simulations using conservative assumptions for cluster size (50 patients) and intracluster correlations (0.05)29 that suggested that 12 to 14 sites with about 35 to 75 patients per site would be needed to detect an absolute increase in appropriate nutritional support from 47% to 70%, measures obtained from the study of Inman and Davidson.11
We considered p values of less than 0.05 to be statistically significant. A p value of less than 0.10 but greater than 0.05 was considered to indicate a trend toward significance. We considered all secondary analyses to be exploratory and hypothesis-generating and therefore did not adjust for multiple comparisons.
Results
During the run-in phase, before randomization, there were no significant differences between the 2 groups of ICU patients in the appropriately randomized hospitals in age, APACHE II score, mortality rate, or lengths of stay in the ICU and the hospital (Table 1), or in admission source, ICU admission diagnosis and other demographic traits. Patient flow during the subsequent, randomized phase is shown in Fig. 2. Baseline characteristics of the patients enrolled in the randomized phase in the appropriately randomized hospitals are shown in Table 2. Significantly more patients in the intervention ICUs were admitted from the operating room. Most of these patients had undergone emergency surgery. The 2 study arms enrolled a similar proportion of potentially eligible patients whose stay was greater than 48 hours (83% v. 82%, p = 0.17, t test of cluster-specific means).
Table 2
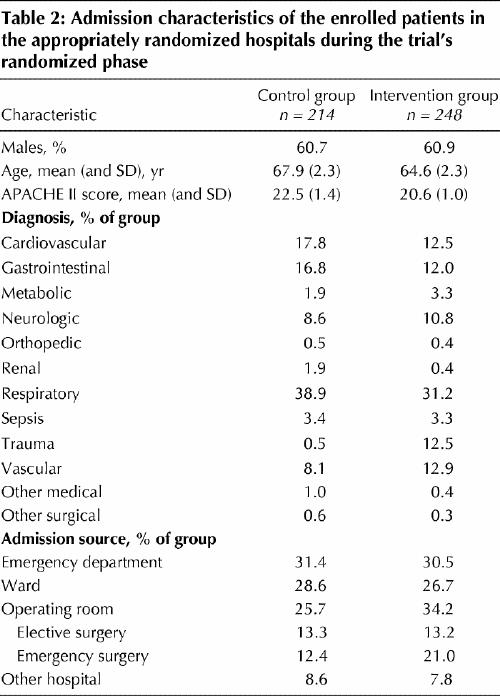
Table 1
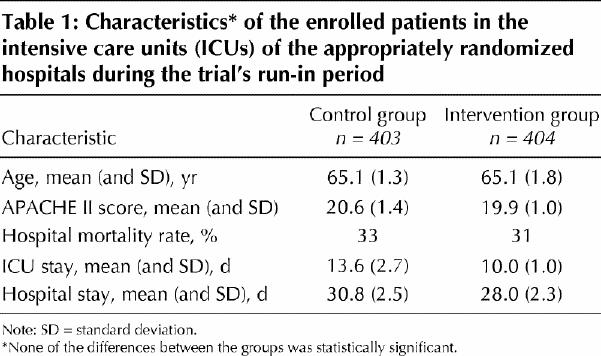
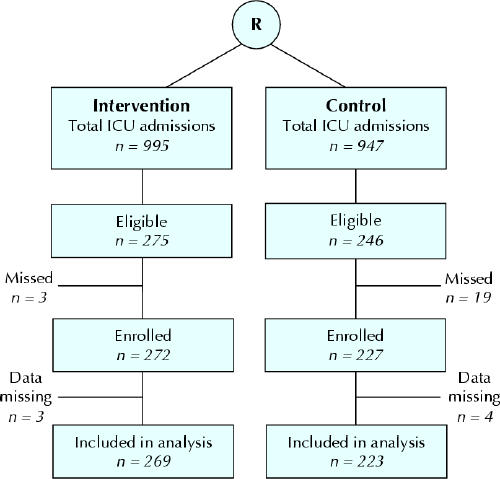
Fig. 2: Patient flow during the randomized phase in the 7 intervention and 7 control ICUs. “Data missing” refers to the primary outcome (mortality and length of stay). Complete data on nutritional support were available for 487 patients. The 2 inappropriately randomized hospitals contributed 84 admissions (9 eligible and enrolled patients) to the control group and 58 admissions (22 eligible and 21 enrolled patients) to the intervention group. R = randomization.
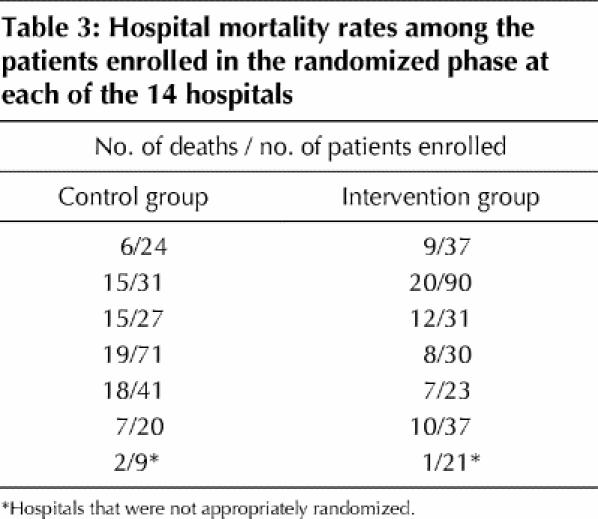
The rates of death in hospital among the enrolled patients are shown in Table 3. As Table 4 shows, with the inappropriately randomized hospitals excluded, there was a trend toward reduced mortality in the intervention hospitals (27% v. 37%, p = 0.058; C1 = 1.65, C2 = 1.79, ρ = 0.015). With all 14 hospitals included in a per-protocol analysis, the reduction was statistically significant (24% v. 37%, p = 0.047; C1 = 1.98, C2 = 2.18, ρ = 0.024). With the use of a negative binomial model (including only the appropriately randomized sites) to adjust for the covariate “source of admission” (“elective operative,” “emergency operative” or “other,” represented by a dummy variable), the reduction was statistically significant in the intervention hospitals (p = 0.035).
Table 4
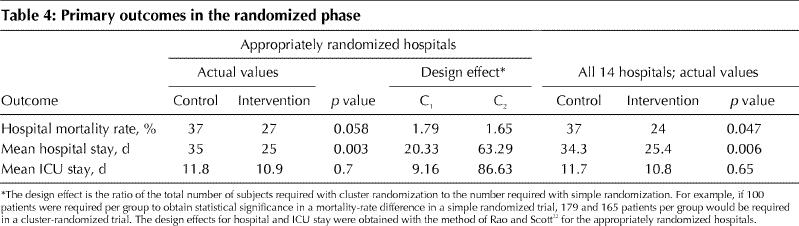
Table 3
The mean length of stay in hospital was 10 days less in the intervention arm than in the control arm (p = 0.003), but the mean length of stay in the ICU did not differ between the 2 groups (Table 4).
In the appropriately randomized hospitals, patients in the intervention hospitals received significantly more days of EN (6.7 v. 5.4 per 10 patient-days at risk, p = 0.042) and significantly more days of any feed (8.5 v. 6.9 per 10 patient-days at risk, p = 0.02) than patients in the control hospitals during their ICU stay. However, the total amount of energy delivered per patient-day, time from ICU admission to receiving enteral feeds, time required to achieve 80% of the calculated energy goal and the number of days on which 80% of the goal was achieved did not differ significantly between the 2 groups (Table 5). The proportion of patients receiving nutritional support is shown in Fig. 3.
Table 5
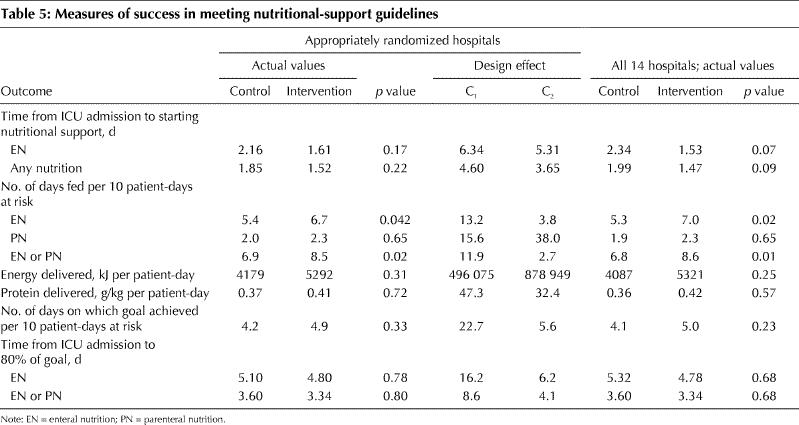
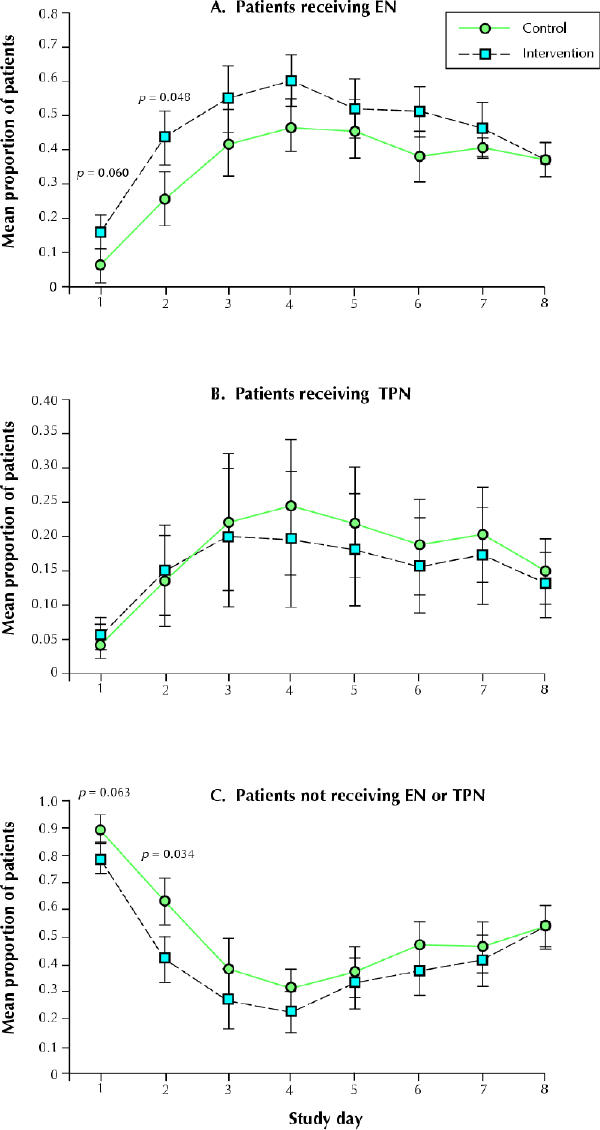
Fig. 3: Cluster-specific mean proportions, and 95% confidence intervals, of patients receiving nutritional support in the appropriately randomized control and intervention hospitals on each study day. Day 1 is the day of ICU admission. The p values were obtained from a t test of cluster-specific means.
Interpretation
In our multicentre, cluster-randomized trial we demonstrated that the implementation of evidence-based algorithms for nutritional support in the critically ill patient improves the provision of nutritional support, reduces hospital stay and may decrease the hospital mortality rate in both community and teaching hospitals. Providing adequate nutrition to the critically ill patient is considered a standard of care.7 However, many studies have documented that nutritional support of any type or quantity appears to be inadequate.8,9 The algorithms on their own can at best be considered a grade B recommendation (based on evidence of intermediate quality; level 1b, 2b, 2c).30 However, our study validates the algorithm and implementation process as a package and not the underlying evidence. It is also possible that our intervention caused changes in patient care that we did not measure. These factors are important to consider when updating the recommendations.
The finding that enhancing delivery of nutritional support translates into improved clinical outcomes is supported by the results of a recent study.14 Another study reported an increased rate of complications with early EN but used a pseudorandomization design and provided intermittent bolus feeding.31 The patients in our intervention group received enteral feeding significantly more often than the patients in our control group. Perhaps patients benefit from more frequent enteral feeding even if total energy needs are not met. Animal studies have shown that endotoxin-induced ischemia can be prevented by early EN,32 and adding subtherapeutic doses of EN to PN has favourable effects on bacterial translocation and nitrogen balance.33 Thus, EN may confer benefits independent of total energy and protein delivery. This hypothesis is supported by the results of a recent randomized trial involving 28 trauma patients: early EN (initiated 4.4 hours after ICU admission on average) resulted in less organ dysfunction than delayed feeding (initiated 36.5 hours after ICU admission on average).34 All patients in that study received supplemental PN, so the total delivered energy was similar in the 2 groups. Our study design did not allow us to determine whether the apparent benefit in hospital mortality rate and length of stay was directly due to the change in nutrition or due to an intermediate benefit, such as fewer infections.
Our results argue for the need to implement guidelines using a multifaceted strategy. Several studies have demonstrated that simply disseminating an algorithm or guideline rarely results in changes in clinical practice.18 The success of our intervention was likely enhanced by our use of 3 relevant, evidence-based implementation strategies in addition to disseminating the algorithms. These strategies — educational sessions provided by opinion leaders,35 educational outreach visits or academic detailing,36 and audit and feedback37 — have been shown to be effective for influencing clinical practice when used independently or in various combinations.35,36,37,38 The number of funded dietitians per ICU bed was recently reported to be associated with the successful application of nutritional support.39 When debriefed after our study, the dietitians in the intervention hospitals reported that they increased the time allocated to ICU patients by as much as 30%, mostly to discuss nutritional support with the physician and nurse. In contrast, several dietitians in the control hospitals stated that they usually had only enough time to collect data. Failure to place strong emphasis on change strategies will decrease the probability of positive improvements in nutrition practices and related outcomes. Although the local dietitian provided regular feedback to the staff, further reinforcement beyond the single didactic lecture might result in larger changes in nutritional support.
Evaluation in clusters helps prevent contamination, and the use of objective outcomes minimizes the effect of a nonblinded study. Both factors would tend to minimize the chance of finding a significant difference between the 2 groups of hospitals. Also, a Hawthorne effect may have occurred, since the dietitians in the intervention sites reported that the time they spent in the ICU increased as a result of the study. We are also unable to determine the relative value of each component of the intervention or whether the differences may have been due to some other, unintended effect. Unfortunately, 2 sites were crossed over after randomization but before implementation of the intervention. Our primary analysis excluded these 2 sites. A secondary analysis that included these 2 sites yielded similar differences between the 2 groups, but the trend toward reduced mortality became statistically significant. The clusters were balanced, as shown by the similarity in patient and outcome data obtained during the run-in phase. However, there were more immediate postoperative patients in the intervention hospitals during the randomized phase. After adjustment for admission source, analysis of the mortality data showed a significant effect of the intervention. We did not collect data on the presence of malnutrition, which could be an important determinant of response to nutritional support.5
In conclusion, we have demonstrated that evidence-based recommendations for nutritional support can be implemented as a set of algorithms and can improve nutritional support to critically ill patients, leading to a decrease in hospital mortality rate and length of stay. Because the study was conducted in teaching and community hospitals with a wide variety of patients, the results should be generally applicable. Our study also showed how a research network, such as the CCR-Net, can provide the foundation for measuring current practice, developing clinical recommendations and aligning these efforts.16 We recommend that current, evidence-based nutritional support guidelines be adopted with a suitable implementation strategy.
Acknowledgments
The following Ontario dietitians and institutions made this study possible: Marg Baltzer, London Health Sciences Centre, Victoria Campus, London; Teresa Banovac-Kennedy, Hotel Dieu Grace Hospital, Windsor; Chris Bean, Peterborough Regional Health Centre, Peterborough; Caryn Caryer and Heather Gibb, The Scarborough Hospital Corporation, General Division, Scarborough; Lisa Halford-Glew and Jodie Hoard, Grand River Hospital, Kitchener–Waterloo Health Centre, Kitchener; Vera Jovanovic, Trillium Health Centre, Mississauga Site, Mississauga; Sarah Kerr, Lakeridge Health Corporation, Oshawa Site, Oshawa; Sue MacNeil, Guelph General Hospital, Guelph; Jill Pikul, London Health Sciences Centre, University Campus, London; Elaine Roy and Binky Wu, Rouge Valley Health System, Centenary Health Centre Site, Toronto; Erika Schieman, St. Joseph's Health Centre, Sudbury Regional Hospital, Sudbury; Deborah Schroter Noppe, William Osler Health Centre, Memorial Hospital Campus, Brampton; Cindy Ulrich, St. Joseph's Health Care London, London; and Christine Vis-Kampen, York County Hospital, Newmarket. We also thank Kevin Inman for his considerable contribution to the initial study design and implementation and Greg Webster for his helpful suggestions and review of the manuscript.
Footnotes
This article has been peer reviewed.
Contributors: Drs. Doig and Sibbald conceived and designed the study; Ms. Morrison helped execute the design. Dr. Martin and Ms. Morrison acquired the data, Drs. Martin and Doig analyzed the data, and Drs. Martin, Doig, Heyland and Sibbald interpreted the data. Dr. Martin drafted the article; Drs. Doig and Heyland provided components for the draft. All authors revised the article critically for important intellectual content and approved the version to be published.
This study was supported by Nestlé Nutrition, Inc., Toronto, Ont. Dr. Heyland is a Career Scientist, Ontario Ministry of Health and Long-Term Care.
Competing interests: None declared.
Correspondence to: Dr. Claudio M. Martin, London Health Sciences Centre, 375 South St., London ON N6A 4G5; fax 519 667-6698; moc.sregor@mcrd
References
Articles from CMAJ : Canadian Medical Association Journal are provided here courtesy of Canadian Medical Association
Full text links
Free to read at www.cmaj.ca
http://www.cmaj.ca/cgi/content/abstract/170/2/197
Free to read at www.cmaj.ca
http://www.cmaj.ca/cgi/content/full/170/2/197
Free to read at www.cmaj.ca
http://www.cmaj.ca/cgi/reprint/170/2/197.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics

Discover the attention surrounding your research
https://www.altmetric.com/details/170541210
Article citations
Survey on Nutrition in Neurological Intensive Care Units (SONNIC)-A Cross-Sectional Survey among German-Speaking Neurointensivists on Medical Nutritional Therapy.
J Clin Med, 13(2):447, 13 Jan 2024
Cited by: 0 articles | PMID: 38256581 | PMCID: PMC10816503
Actively implementing an evidence-based feeding guideline for critically ill patients (NEED): a multicenter, cluster-randomized, controlled trial.
Crit Care, 26(1):46, 16 Feb 2022
Cited by: 12 articles | PMID: 35172856 | PMCID: PMC8848648
Continuing education meetings and workshops: effects on professional practice and healthcare outcomes.
Cochrane Database Syst Rev, 9:CD003030, 15 Sep 2021
Cited by: 60 articles | PMID: 34523128 | PMCID: PMC8441047
Review Free full text in Europe PMC
Effect of the Timing of Nutritional Support Team Intervention on Nutritional Status on Patients Receiving Enteral Nutrition.
Clin Nutr Res, 10(1):1-13, 22 Jan 2021
Cited by: 1 article | PMID: 33564648 | PMCID: PMC7850813
Barriers to the delivery of enteral nutrition in pediatric intensive care units: A national survey.
Int J Pediatr Adolesc Med, 8(3):186-190, 17 Dec 2020
Cited by: 3 articles | PMID: 34350333 | PMCID: PMC8319679
Go to all (182) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Effect of evidence-based feeding guidelines on mortality of critically ill adults: a cluster randomized controlled trial.
JAMA, 300(23):2731-2741, 01 Dec 2008
Cited by: 181 articles | PMID: 19088351
Energy deficit and length of hospital stay can be reduced by a two-step quality improvement of nutrition therapy: the intensive care unit dietitian can make the difference.
Crit Care Med, 40(2):412-419, 01 Feb 2012
Cited by: 43 articles | PMID: 21926572
Nutrition of the critically ill patient and effects of implementing a nutritional support algorithm in ICU.
J Clin Nurs, 15(2):168-177, 01 Feb 2006
Cited by: 41 articles | PMID: 16422734
Preliminary evidence for a medical nutrition therapy protocol: enteral feedings for critically ill patients.
J Am Diet Assoc, 106(8):1226-1241, 01 Aug 2006
Cited by: 40 articles | PMID: 16863719
Review