Abstract
Free full text

Induction of Innate Immunity against Herpes Simplex Virus Type 2 Infection via Local Delivery of Toll-Like Receptor Ligands Correlates with Beta Interferon Production
Abstract
Toll-like receptors (TLRs) constitute a family of innate receptors that recognize and respond to a wide spectrum of microorganisms, including fungi, bacteria, viruses, and protozoa. Previous studies have demonstrated that ligands for TLR3 and TLR9 induce potent innate antiviral responses against herpes simplex virus type 2 (HSV-2). However, the factor(s) involved in this innate protection is not well-defined. Here we report that production of beta interferon (IFN-β) but not production of IFN-α, IFN-γ, or tumor necrosis factor alpha (TNF-α) strongly correlates with innate protection against HSV-2. Local delivery of poly(I:C) and CpG oligodeoxynucleotides induced significant production of IFN-β in the genital tract and provided complete protection against intravaginal (IVAG) HSV-2 challenge. There was no detectable IFN-β in mice treated with ligands for TLR4 or TLR2, and these mice were not protected against subsequent IVAG HSV-2 challenge. There was no correlation between levels of TNF-α or IFN-γ in the genital tract and protection against IVAG HSV-2 challenge following TLR ligand delivery. Both TNF-α−/− and IFN-γ−/− mice were protected against IVAG HSV-2 challenge following local delivery of poly(I:C). To confirm that type I interferon, particularly IFN-β, mediates innate protection, mice unresponsive to type I interferons (IFN-α/βR−/− mice) and mice lacking IFN regulatory factor-3 (IRF-3−/− mice) were treated with poly(I:C) and then challenged with IVAG HSV-2. There was no protection against HSV-2 infection following poly(I:C) treatment of IFN-α/βR−/− or IRF-3−/− mice. Local delivery of murine recombinant IFN-β protected C57BL/6 and IRF-3−/− mice against IVAG HSV-2 challenge. Results from these in vivo studies clearly suggest a strong correlation between IFN-β production and innate antiviral immunity against HSV-2.
The innate immune response represents the first line of defense against microbial pathogens. This system is a universal and ancient form of host defense against infection. It has the ability to recognize pathogens via pattern recognition receptors. Toll-like receptors (TLRs) are the best-characterized family of pattern recognition receptors. TLRs recognize conserved epitopes of various microbial components, known as pathogen-associated molecular patterns, that are expressed on infectious agents and are typically needed for survival (2, 7, 15, 16, 25). In general, these epitopes are common to an entire class of pathogen without the need for clonal differentiation of host cells (1). It is now evident that the 11 known mammalian TLRs each recognize distinct ligands and utilize multiple overlapping signaling pathways which result in innate defense against invading pathogens (7, 15, 25, 34, 36). Examples of pathogen-associated molecular patterns include lipopolysaccharide (LPS) (ligand for TLR4), peptidoglycan (PGN) (ligand for TLR2), flagellin (ligand for TLR5), double-stranded RNA (ligand for TLR3), bacterial CpG DNA (ligand for TLR9), and profilin (ligand for TLR11). Upon ligand binding, TLRs activate signaling through the Toll/interleukin-1 domain found in the cytoplasmic tails of these proteins. These signaling pathways can be divided into common (MyD88-dependent) and specific (MyD88-independent) categories. TLR2, -5, -7, -8, -9, and -11 signaling is MyD88 dependent, while TLR3 and -4 signaling can be mediated through both MyD88-dependent and -independent pathways.
Recently, the role of TLRs in innate immunity has been studied extensively and it has been shown that TLR binding by ligands triggers the activation of transcription factors that lead to induction of antimicrobial factors, including inflammatory cytokines and antimicrobial peptides (15). As such, TLR ligands have multiple clinical uses, including the induction of protective innate immunity, cancer therapy, improvement of responses to vaccines, and reduction of allergic responses (33). Recent studies have shown that TLRs are involved in innate immunity in a variety of ways. Specifically, activation of TLR3 and -4 signaling pathways has been shown to activate a family of genes, the type I interferons (IFNs), which are involved in antiviral responses (32). The type I IFNs, which include IFN-α and IFN-β, are known factors in the antiviral immune response (18, 31). The antiviral effects of these IFNs have been explored, and it has been demonstrated that they inhibit all stages of herpes simplex virus (HSV) replication (31). TLR3, -4, -7, and -9 are known to induce type I IFN responses through the activation of IFN regulatory factors (IRFs), including IRF-3 and IRF-7 (6). In addition to its recognition by TLR3, double-stranded RNA is recognized by the cytoplasmic RNA helicases RIG-I and MDA5, resulting in activation of IRF-3 and production of type I IFNs in a TLR-independent fashion (35).
Recently, we and others (3, 5, 13, 28, 29) have shown that HSV type 2 (HSV-2) infection can be prevented by delivering CpG DNA or poly(I:C) to the mucosal surface prior to infection. However, the mechanisms of this innate antiviral protection were not fully defined. In this study, we have investigated the factor(s) involved in this innate antiviral response. We have found a correlation between IFN-β induction and protection against intravaginal (IVAG) HSV-2 infection. Our data show that IRF-3 activation and subsequent IFN-α/β signaling are required for poly(I:C)-induced innate protection against IVAG HSV-2 challenge. Finally, local delivery of murine recombinant IFN-β (mrIFN-β) alone protected C57BL/6 (B6) and IRF-3−/− mice against subsequent IVAG HSV-2 challenge.
MATERIALS AND METHODS
Mice.
Female C57BL/6 and 129SVPasCrl mice, 8 to 12 weeks old, were purchased from Charles River Laboratory (Quebec, Canada). TNF-α−/− and IFN-γ−/− mice were purchased from Jackson Laboratory. Breeding pairs of mice unresponsive to type I interferons (IFN-α/βR−/− mice) were kindly provided by Rolf M. Zinkernagel (Zürich, Switzerland). Breeding pairs of IRF-3−/− mice were kindly provided by Tadatsugu Taniguchi (Japan). All mice followed a 12-h-day and 12-h-night schedule and were maintained under standard temperature-controlled conditions as outlined by the Canadian Council on Animal Care.
Viruses, cells, and reagents.
HSV-2 strain 333 was grown and viral titers were determined as previously described (23). C57BL/6 murine embryonic fibroblasts (MEFs) were grown in 10% alpha minimal essential medium. Synthetic CpG phosphorothioate oligodeoxynucleotide (ODN) (no. 1826) was provided by McMaster University's Molecular Biology Institute (MOBIX) (Hamilton, Ontario, Canada). LPS (L26-54), PGN, and poly(I:C) were purchased from Sigma (Oakville, Ontario, Canada). Plasmid containing bacterial flagella (FliC) was kindly provided by Steven B. Mizel, Wake Forest University (North Carolina). Recombinant FliC was then purified using a His tag affinity column from Pierce Biotechnology (Rockford, IL). Medroxyprogesterone (Depo-Provera) was purchased from Upjohn (Don Mills, Ontario, Canada).
Generation of mrIFN-β.
The murine IFN-β gene was amplified from murine genomic DNA by use of primers 5′-CAGAATTCGCTTCCATCATGAACAACAG-3′ (sense) and 5′-TGCTCGAGGTTTTGGAAGTTTCTGGTAA-3′ (antisense). The resulting PCR product was cut with EcoRI/XhoI and cloned into pMT/V5-HisA (Invitrogen). S2 Drosophila melanogaster cells grown in Schneider's Drosophila media (Invitrogen) were cotransfected with either pMT/mIFN-β/V5-His or pMT/EGFP/V5-His and pCO-BLAST (Invitrogen) by use of Cellfectin (Invitrogen) according to the manufacturer's instructions. Stable transfectants were selected using 25 mg/ml blasticidin (Invitrogen). Supernatants were prepared by culturing stable transfectants (murine IFN-β [mIFN-β] expressing or green fluorescent protein [GFP] expressing) in serum-free Schneider's Drosophila media lacking antibiotics supplemented with 500 mM copper sulfate to induce transgene expression. After 72 h, supernatants were collected, filtered, and frozen. Supernatants were assayed for mIFN-β content by use of an enzyme-linked immunosorbent assay (ELISA) for mIFN-β (PBL BioMedical).
Treatment of mice with TLR ligands or mrIFN-β.
B6 and IRF-3−/− mice, 6 to 8 weeks old, were subcutaneously injected with 2 mg of progesterone per mouse. Doses and times of TLR ligand delivery were chosen based on our previous works (5, 29). Four days later, B6 mice were anesthetized and treated vaginally with CpG ODN (25 μg/mouse), poly(I:C) (100 μg/mouse), LPS (5 μg/mouse), PGN (100 μg/mouse), FliC (80 μg/mouse), or mrIFN-β (5,000 pg/mouse). IRF-3−/− mice were also treated with poly(I:C) (100 μg/mouse), CpG ODN (25 μg/mouse), or mrIFN-β (5,000 pg/mouse).
Genital HSV-2 inoculation and vaginal virus titration.
Six- to eight-week-old mice were injected subcutaneously with 2 mg progesterone/mouse 4 days prior to treatment. Twenty-four hours after treatment with different TLR ligands, mice were anesthetized, placed on their backs, and infected IVAG with a lethal dose of 1 × 104 PFU of HSV-2 in 10 μl of phosphate-buffered saline (PBS) for at least 45 min while being maintained under anesthetic. Vaginal washes were collected daily after infection (days 1 to 3) by pipetting two 30-μl doses of PBS into and out of the vagina six to eight times. Viral titers in IVAG washes were determined by plaque assay on monolayers of Vero cells as previously described (23). Treated mice were also monitored daily for genital pathology and survival for up to 4 weeks. Pathology was scored on a five-point scale: 0, no infection; 1, slight redness of external vagina; 2, swelling and redness of external vagina; 3, severe swelling of external vagina and hair loss in the surrounding area; 4, ulceration of vaginal tissue, redness, and swelling; 5, continued ulceration, redness, and swelling and sometimes paralysis in back legs (mice were sacrificed at this point).
ELISAs for IFN-α, IFN-β, TNF-α, and IFN-γ.
Tumor necrosis factor alpha (TNF-α) and IFN-γ ELISAs were conducted using Quantikine murine kits from R&D Systems (Minneapolis, MN) according to the manufacturer's instructions. IFN-α and IFN-β ELISAs were conducted using PBL biomedical kits from PBL (Piscataway, NJ). The IFN-α ELISA kit detects mouse IFN-αA, IFN-α1, IFN-α4, IFN-α5, IFN-α6, and IFN-α9, with a detection limit of 10 pg/ml.
Bioassay for type I interferon activity.
To detect the biological activity of IFN-β in the supernatants of mrIFN-β-expressing S2 cells, we used a standard vesicular stomatitis virus plaque reduction assay. The supernatants were serially diluted and transferred onto MEFs plated in 12-well plates. Standard recombinant IFN-β (rIFN-β) was also serially diluted in duplicate and transferred onto the MEFs in order to quantify the results. The MEFs with supernatants were incubated at 37°C for 24 h. The supernatants were then removed, and the cells were infected with 200 μl of vesicular stomatitis virus with predetermined viral titers for 1 h. The plates were then overlaid with methylcellulose, incubated for 24 h, and then stained for plaque count. The plaque count of the rIFN-β serially diluted samples was used to quantify the amount of rIFN-β in the S2 supernatants. Supernatants from GFP-expressing S2 cells were used as a control.
Histomorphology of the genital tract.
To study the effects of TLR ligands on vaginal tissue morphology, progesterone-treated mice received CpG ODN (25 μg/mouse), poly(I:C) (100 μg/mouse), LPS (5 μg/mouse), peptidoglycan (100 μg/mouse), or FliC (80 μg/mouse). After 24 h, vaginal tissue was removed, fixed in 4% paraformaldehyde, embedded in paraffin, and sectioned at 7 mm for hematoxylin and eosin staining.
Statistical analysis.
Statistical differences of the viral titers were determined by analysis of variance followed by Tukey's test. The statistical significances of the survival rates were determined by the χ2 test. A P value of <0.05 was considered statistically significant. An unpaired t test was used to find the significant differences in cytokine production.
RESULTS
Vaginal delivery of only certain TLR ligands mediates protection against IVAG HSV-2 infection.
While our previous findings demonstrated that ligands for TLR3 and -9 conferred protection against IVAG HSV-2 infection (5, 29), the activities of additional TLR ligands remained to be studied. Our results show that protection against HSV-2 is 100% effective using poly(I:C) and CpG ODN IVAG treatments, 50% effective using FliC, and ineffective using PGN and LPS treatments (Fig. (Fig.1a).1a). We also examined viral titers in the vaginal washes following IVAG HSV-2 challenge (Fig. (Fig.1b).1b). No virus was detected in the vaginal washes from mice treated with poly(I:C) or CpG ODN, while viral titers in the vaginal washes from mice treated with other TLR ligands showed no significant reduction compared to titers from control mice. Thus, only stimulation of TLR3 and TLR9 limits virus replication and induces complete survival following IVAG HSV-2 challenge.
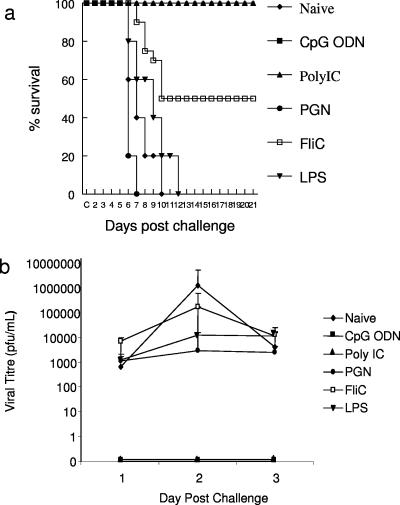
Vaginal delivery of certain TLR ligands increases resistance to IVAG HSV-2 infection in B6 mice. Six- to eight-week-old female B6 mice were treated with CpG ODN (100 μg/mouse, n = 20), poly(I:C) (100 μg/mouse, n = 20), PGN (100 μg/mouse, n = 10), FliC (80 μg/mouse, n = 10), or LPS (5 μg/mouse, n = 20) or left untreated 24 h prior to IVAG HSV-2 challenge (1 × 104 PFU/mouse). Challenged mice were monitored daily for genital pathology, survival, and vaginal virus titers. (a) poly(I:C)- and CpG-treated mice showed 100% survival compared to LPS- or PGN-treated or untreated mice. FliC-treated mice showed 50% protection. (b) Vaginal HSV-2 titers were examined on days 1 to 3 following viral challenge. B6 mice treated with poly(I:C) and CpG had no viral titers, while all other groups showed significant viral titers.
Effect of local delivery of TLR ligands on vaginal tissue.
Since we observed such a marked difference in the effects of local delivery of TLR ligands against IVAG HSV-2 challenge, we first examined whether the protection was a result of local changes in the vaginal mucosa. There was a rapid proliferation of the vaginal epithelium in all treatment groups, except mice treated with LPS, compared to results with naïve mice (Fig. (Fig.2).2). Treatments with CpG (Fig. (Fig.2b),2b), PGN (Fig. (Fig.2d),2d), and FliC (Fig. (Fig.2e)2e) also resulted in neutrophil infiltration to the epithelium and vaginal lumen. Treatment with poly(I:C) (Fig. (Fig.2c)2c) caused little or no inflammation compared to CpG ODN treatment, which showed the highest level of inflammation in the submucosa. Thickening of the vaginal epithelium and induction of inflammatory cells, such as neutrophils, did not correlate with TLR-induced innate protection against IVAG HSV-2 challenge.
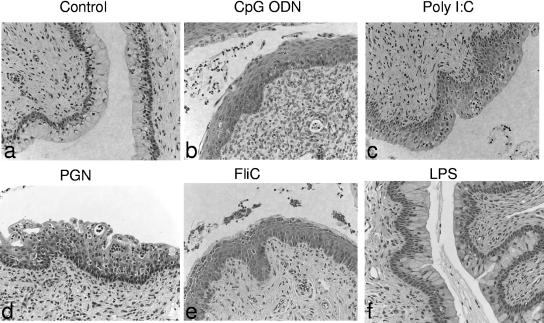
Effects of TLR ligands on morphology of genital mucosa. Six- to eight-week-old female B6 mice were treated with progesterone and, 4 days later, received CpG ODN (100 μg/mouse), poly(I:C) (100 μg/mouse), PGN (100 μg/mouse), FliC (80 μg/mouse), LPS (5 μg/mouse), or PBS (control). Twenty-four hours later, vaginal tissues were isolated and processed for histological testing. Photomicrographs represent cross-sections of vaginal tissues from mice from the various treatment groups. Magnification, ×200.
Mucosal delivery of TLR ligands induced the production of IFN-β and/or TNF-α but not that of IFN-α or IFN-γ.
We and others have reported that some TLR ligands induce innate protection against HSV-2 (1, 5, 29); however, there has been no report on the main factor(s) responsible for this protection. To identify the factor(s) that plays a role in innate immunity, we examined the cytokine environment in vivo. We examined the production of IFN-γ, IFN-α, IFN-β, and TNF-α in vaginal washes following mucosal delivery of TLR ligands. There was no detectable level of IFN-γ or IFN-α in the vaginal washes of these mice (Fig. (Fig.3).3). TNF-α was induced at either 12 or 24 h following IVAG treatment with all TLR ligands (Fig. (Fig.3a).3a). In particular, TFN-α was elevated at both 12 and 24 h posttreatment with CpG ODN, poly(I:C), and PGN, while it was detectable only at 12, but not at 24 h, posttreatment with FliC and LPS. Poly(I:C) treatment showed the highest level of IFN-β in the vaginal washes, followed by CpG ODN treatment (Fig. (Fig.3b).3b). Treatment with other TLR ligands, however, had no or very low levels of detectable IFN-β.
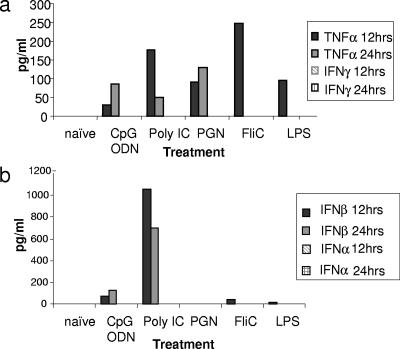
Local delivery of certain TLR ligands in B6 mice induced production of TNF-α and IFN-β. Six- to eight-week-old female B6 mice were treated with CpG ODN (100 μg/mouse), poly(I:C) (100 μg/mouse), PGN (100 μg/mouse), FliC (80 μg/mouse), or LPS (5 μg/ml) or left untreated. Vaginal washes from five mice were collected at 12 and 24 h posttreatment, pooled, and used to measure levels of TNF-α, IFN-γ, IFN-β, and IFN-α by use of ELISA. No IFN-γ (a) or IFN-α (b) was detected in these washes; however, all treatments caused the production of TNF-α (a). IFN-β production (b) was seen with CpG ODN- and poly(I:C)-treated mice, while no or very little IFN-β was detected in the washes of PGN-, LPS-, and FliC-treated mice. The experiments were repeated two times with similar results.
Local delivery of poly(I:C) protected TNF-α−/− and IFN-γ−/− mice against IVAG HSV-2 challenge.
We have observed that local delivery of TLR ligands induced production of significant amounts of TNF-α. However, there was no correlation between induction of TNF-α and protection against IVAG HSV-2 challenge. To confirm this, we treated TFN-α−/− mice with poly(I:C) and then challenged them with IVAG HSV-2. Poly(I:C) provided complete protection against IVAG HSV-2 challenge in the absence of TNF-α (Fig. (Fig.4).4). IFN-γ also plays an important role in innate defense against IVAG HSV-2 infection (4). However, innate antiviral protection was not associated with IFN-γ production. Local delivery of poly(I:C) or CpG ODN in IFN-γ−/− mice also provided complete protection against IVAG HSV-2 challenge (Fig. (Fig.4).4). Thus, although both TNF-α and IFN-γ are induced following TLR ligand stimulation, neither is essential for survival against IVAG HSV-2 infection.
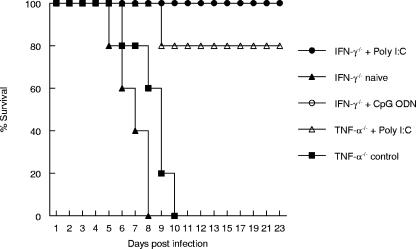
Local delivery of poly(I:C) provides innate protection against IVAG HSV-2 challenge in the absence of IFN-γ or TNF-α. Six- to eight-week-old female IFN-γ−/− mice were treated with poly(I:C) (100 μg/mouse, n = 10) or CpG ODN (100 μg/mouse, n = 10) or left untreated (n = 10). Six- to eight-week-old female TNF-α−/− mice were also treated with poly(I:C) (100 μg/mouse, n = 5) or left untreated (n = 5). Twenty-four hours posttreatment, mice were challenged IVAG with their lethal doses of HSV-2. Challenged mice were monitored daily for genital pathology, survival, and vaginal virus titers. Poly(I:C)-treated IFN-γ−/− mice and TNF-α−/− mice showed 100% and 80% survival, respectively. All control untreated mice died within 10 days after IVAG HSV-2 infection.
IFN-β signaling is required for TLR ligand-induced innate protection against HSV-2 infection.
In order to determine whether type I IFNs, particularly IFN-β, play a key role in innate protection against vaginal HSV-2 infection, mice unresponsive to type I IFNs (IFN-α/βR−/− mice) or unable to produce IFN-β (IRF-3−/− mice) were used. Treatment of IFN-α/βR−/− mice with poly(I:C) showed high levels of IFN-β production (Fig. (Fig.5a).5a). However, when poly(I:C)- or CpG ODN-treated IFN-α/βR−/− mice were challenged with HSV-2, all IFN-α/βR−/− mice succumbed to infection; in contrast, congenic control 129SVPasCrl mice treated with poly(I:C) showed 100% survival (Fig. (Fig.5b).5b). Interestingly, poly(I:C)- or CpG ODN-treated IFN-α/βR−/− mice reached end point faster than control untreated mice. IRF-3 is a key transcription factor responsible for IFN-β production, particularly in nonimmune cells, such as fibroblasts and epithelial cells. To determine if local delivery of poly(I:C) leads to IFN-β production in the absence of IRF-3, IRF-3−/− mice were treated with poly(I:C). There was no detectable IFN-β in the vaginal washes from poly(I:C)-treated IRF-3−/− mice compared to those from C57BL/6 controls (Fig. (Fig.5a).5a). Moreover, poly(I:C)-treated IRF-3−/− mice were not protected against IVAG HSV-2 challenge (Fig. (Fig.5c).5c). However, local delivery of CpG ODN completely protected IRF-3−/− mice against subsequent IVAG HSV-2 challenge (Fig. (Fig.5c).5c). Thus, IRF-3 is an essential component of IFN-β production and subsequent protection following IVAG HSV-2 infection.
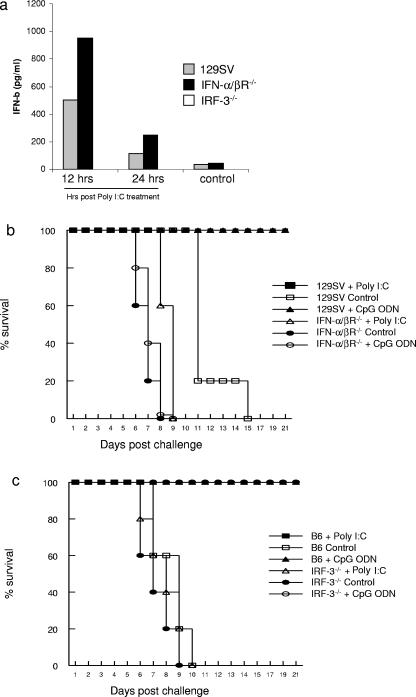
Treatment of IFN-α/βR−/− or IRF-3−/− mice with poly(I:C) does not provide protection against vaginal HSV-2 challenge. (a) Six- to eight-week-old female IFN-α/βR−/−, 129SVPasCrl (129SV) (congenic control for IFN-α/βR−/− mice), or IRF-3−/− mice were treated with poly(I:C) (100 μg/mouse) or left untreated. Vaginal washes were collected at 12 and 24 h posttreatment, pooled (n = 5), and used to measure levels of IFN-β by use of ELISA. Poly(I:C) induced significant levels of IFN-β in IFN-α/βR−/− mice. However, IRF-3−/− mice treated with poly(I:C) showed no detectable IFN-β in the vaginal washes. Vaginal washes from four mice were pooled for ELISA. The experiment was repeated two times with similar results. (b) Six- to eight-week-old female IFN-α/βR−/− mice and their congenic controls were treated with poly(I:C) (100 μg/mouse, n = 10) or CpG ODN (25 μg/mouse, n = 5) or left untreated (n = 5) 24 h prior to IVAG HSV-2 challenge. Challenged mice were monitored daily for genital pathology and survival. Poly(I:C)- or CpG ODN-treated 129SVPasCrl mice showed 100% survival compared to untreated 129SVPasCrl control mice. There was no protection against IVAG HSV-2 challenge in poly(I:C)- or CpG ODN-treated IFN-α/βR−/− mice compared to results with untreated control mice. (c) Six- to eight-week-old female IRF-3−/− mice and their congenic control B6 mice were treated with poly(I:C) (100 μg/mouse) or CpG ODN (25 μg/mouse) or left untreated 24 h prior to IVAG HSV-2 challenge. Challenged mice were monitored daily for genital pathology and survival. Poly(I:C)- or CpG ODN-treated B6 mice showed 100% survival compared to untreated B6 control mice. There was no protection against IVAG HSV-2 challenge in poly(I:C)-treated IRF-3−/− mice compared to results with untreated control mice. All IRF-3−/− mice treated with CpG ODN survived against IVAG HSV-2 challenge.
Local delivery of mrIFN-β provides protection against IVAG HSV-2 challenge in B6 and IRF-3−/− mice.
Since we have seen a strong correlation between innate antiviral protection and IFN-β production, we then examined if local delivery of biologically active mrIFN-β alone could provide protection against subsequent IVAG HSV-2 challenge of B6 or IRF-3−/− mice. Interestingly, local delivery of S2 cell supernatant, 25 μl/mouse containing 2 × 105 pg/ml of mrIFN-β, provided strong innate antiviral immunity against subsequent IVAG HSV-2 challenge in both B6 and IRF-3−/− mice (Fig. (Fig.6).6). All B6 and IRF-3−/− mice receiving local delivery of control S2 cell supernatant succumbed to subsequent IVAG HSV-2 challenge. Thus, IFN-β is capable of providing protection against vaginal HSV-2 infection.
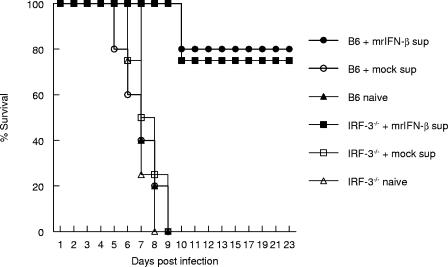
Local delivery of mrIFN-β provides innate protection against vaginal HSV-2 challenge of B6 and IRF-3−/− mice. Six- to eight-week-old female IRF-3−/− mice (n = 8) or control B6 mice (n = 10) were treated with cell supernatants containing mrIFN-β (mrIFN-β sup) or mock supernatants (mock sup) or left untreated. Twenty-four hours posttreatment, mice were challenged with IVAG HSV-2. Challenged mice were monitored daily for genital pathology and survival. Local delivery of mrIFN-β provided B6 mice with 80% protection and IRF-3−/− mice with 75% protection against subsequent IVAG HSV-2 challenge. Mice treated with mock supernatants showed no protection against IVAG HSV-2 challenge compared to naïve mice.
DISCUSSION
TLRs have been shown to induce initial inflammatory and immune reactions by binding to conserved epitopes of microbial pathogens (25). Several TLR ligands have been shown to induce the expression of type I IFN genes (6-9), which are cytokines known to inhibit viral replication (18). The focus of this paper was to determine which TLR ligand treatments induce innate antiviral responses against HSV-2 and the mechanism behind this protection. Here we have clearly shown that innate antiviral responses against HSV-2 following TLR stimulation were strongly correlated with the production of IFN-β.
In this study, experiments were undertaken first to examine the abilities of various TLR ligands to induce innate defense against HSV-2 and second to identify the factor(s) that is responsible for any observed protection. We and others have reported previously that TLR3 and TLR9 ligands confer protection against HSV-2 both in vitro and in vivo (3, 5, 24, 28-30). However, the roles of ligands for TLR2 and -5 have not been studied previously. Here we first wanted to test the abilities of other TLR ligands to induce antiviral responses in vivo. Complete protection against IVAG HSV-2 challenge was seen only by treatment with poly(I:C) and CpG ODN, while treatment with FliC gave only 50% protection against IVAG HSV-2 challenge. We did not see any protection with PGN or LPS treatment.
We have found previously that local delivery of CpG ODN induces rapid thickening of the vaginal epithelium and significant recruitment of inflammatory cells (5). To examine if these events occur with other TLR ligands and whether they correlate with protection against IVAG HSV-2 challenge, we examined the vaginal mucosa following treatment with TLR ligands. We observed that the thickening of the vaginal epithelium occurs in both protected and nonprotected groups. Although local delivery of PGN or FliC induced similar changes in the vaginal epithelium, including thickening and recruitment of inflammatory cells such as neutrophils, these mice were not protected against IVAG HSV-2 challenge compared to mice treated with poly(I:C) or CpG ODN. There are reports that depletion of neutrophils leads to higher viral load in the genital tract (26). However, in these previous studies, anti-Gr1 antibody, which also depletes an important subset of IFN-producing dendritic cells, was used for neutrophil depletion. Moreover, it has been reported that susceptibility to genital HSV-2 infection is increased due to progesterone treatments or oophorectomy, which are also associated with higher numbers of neutrophils in the genital tract (11, 12, 19). Although we have seen no correlation between thickening of the vaginal epithelium and TLR ligand-induced innate protection against IVAG HSV-2 challenge, the mechanism(s) behind this process is yet to be investigated. One might speculate that TLR ligands could induce cell proliferation in the vaginal epithelium but could not induce innate antiviral responses.
We next sought to determine the factors mediating this protection by investigating the innate antiviral cytokine environment. It has been well-documented that various cytokines from the interferon family, such as IFN-α, IFN-β, and IFN-γ, play important roles in protection against HSV-2 (4, 6, 10, 18, 20-22, 32). There have also been studies showing TNF-α as a potent antiviral cytokine (24, 27, 30). Based on these findings, we investigated various cytokines to determine whether any of them could be responsible for the protection in vivo. We and others (5, 24) have reported previously that poly(I:C), LPS, and CpG ODN do not increase IFN-γ production in RAW 264.7 cells. Our mouse model showed that treatment with TLR ligands did not induce the production of detectable levels of IFN-γ. Treatment of IFN-γ−/− mice with poly(I:C) or CpG ODN confirmed that IFN-γ is not crucial for the TLR ligand-induced innate antiviral immunity. Next, we examined the role of IFN-α in the observed protection. Results of our study demonstrated that local delivery of poly(I:C), LPS, PGN, CpG ODN, and FliC did not induce detectable levels of IFN-α, as assayed by ELISA. The detection limit of the kit was about 10 pg/ml, and it recognized six different IFN-α species. This suggests that IFN-α may not be the mediating factor in this innate protection against HSV-2.
We have reported recently that treatment of RAW 264.7 cells with TLR ligands induces the production of TNF-α (10). Other studies have shown that TLR2 and TLR4 activation in RAW 264.7 cells is associated with TNF-α production (17). However, recent studies have demonstrated that neutralizing TNF-α with anti-TNF-α antibody has no effect on the viral replication in RAW 264.7 cells (22). Our mouse model showed that local delivery of TLR ligands induced significant production of TNF-α in the genital mucosa; however, this did not correlate with protection against IVAG HSV-2 challenge. Specifically, high levels of TNF-α secretion are seen with LPS and PGN treatment; however, there was no survival in either of these two groups following HSV-2 challenge. Moreover, TNF-α−/− mice were protected against IVAG HSV-2 challenge following local delivery with poly(I:C). Thus, it appears that TNF-α induction is not responsible for the innate immune protection seen following local delivery of TLR ligands.
The last cytokine to be examined was IFN-β. We have reported previously that IFN-β is important in the protection against HSV-2 in RAW 264.7 cells treated with interleukin-15 (10). Also, by use of gene expression models, IFN-β induction has been shown to occur in RAW 264.7 cells treated with TLR ligands (32). In this study, the levels of IFN-β produced directly correlated with the percentages of survival we saw in the mice treated with different TLR ligands.
To confirm that IFN-β is critical in the innate protection against vaginal HSV-2 challenge, we used IFN-α/βR−/− mice, which are unresponsive to IFN-β. We found that treatment of these mice with poly(I:C) resulted in IFN-β production; hence, the ability to produce IFN-β is not affected. However, poly(I:C)- or CpG ODN-treated mice did not survive vaginal HSV-2 challenge. IFN-α/βR−/− mice succumbed to infection even more quickly than naïve wild-type congenic controls, while wild-type poly(I:C)-treated mice showed 100% protection. This clearly indicates the crucial role of type I IFNs (IFN-α/β) in the innate protection against HSV-2. Although IFN-α/βR−/− mice lack signaling for both IFN-α and IFN-β, we have already determined that TLR ligands do not induce significant levels of IFN-α. Therefore, we sought to attribute our findings to the role of IFN-β in this model. In nonimmune fibroblasts and epithelial cells, IRF-3 is an important transcription factor in virus-mediated IFN-β production. Local delivery of poly(I:C) in IRF-3−/− mice induced no detectable levels of IFN-β, and the mice were not protected against subsequent IVAG HSV-2 challenge. However, as expected, local delivery of CpG ODN provided complete protection against IVAG HSV-2 infection in IRF-3−/− mice. This observation suggests that in the vaginal mucosa, nonimmune fibroblasts and/or epithelial cells are the primary producers of IFN-β, as opposed to immune cells, which produce predominantly IFN-α and require IRF-7 for full activation (14). Finally, to confirm the key role of IFN-β in the innate protection against IVAG HSV-2 infection, we examined whether mrIFN-β alone could protect B6 and IRF-3−/− mice against IVAG HSV-2 challenge. Interestingly, local delivery of mrIFN-β provided protection against HSV-2 challenge. While poly(I:C) is a known ligand of TLR3, it is likely that the cytoplasmic RNA helicases RIG-I and MDA5 also play a role in IFN-β induction in response to this stimulus.
We have demonstrated a clear correlation between IFN-β secretion and protection from HSV-2 TLR ligands in vivo. This correlation suggests a vital role for IFN-β in the innate protection against HSV-2 infection and supports further study in this area. It is yet to be determined how IFN-β, following local delivery of TLR ligands, exerts its antiviral activity against HSV-2. From our previous work, we know that HSV-2 enters the epithelial cells, but it is not clear at which step the viral replication is blocked. An understanding of TLR ligands in innate antiviral responses may provide new insights in defense against viral infections, including HSV and human immunodeficiency virus type 1 infections.
Acknowledgments
We thank Steven B. Mizel for providing plasmid containing FliC, Jonathan Bramson for providing S2 Drosophila cells, Rolf M. Zinkernagle and Ken L. Rosenthal for providing breeding pairs of IFN-α/βR−/− mice, and Tadatsugu Taniguchi via Thomas Moran for providing breeding pairs of IRF-3−/− mice. We also thank Randy MacKenzie, Mary Jo Smith, Mary Bruni, Jennifer Newton, Amanda Kwant, and Amy Patrick for technical assistance.
This work was supported by grants from the Hospital for Sick Children Foundation and the Canadian Institutes of Health Research (CIHR) to Ali A. Ashkar. Ali A. Ashkar is a recipient of a career award in health sciences from Rx&D/CIHR.
REFERENCES
Articles from Journal of Virology are provided here courtesy of American Society for Microbiology (ASM)
Full text links
Read article at publisher's site: https://doi.org/10.1128/jvi.01036-06
Read article for free, from open access legal sources, via Unpaywall:
https://jvi.asm.org/content/jvi/80/20/9943.full.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1128/jvi.01036-06
Article citations
Influence of the Composition of Cationic Liposomes on the Performance of Cargo Immunostimulatory RNA.
Pharmaceutics, 15(9):2184, 23 Aug 2023
Cited by: 2 articles | PMID: 37765155 | PMCID: PMC10535620
Mucosal CCL28 Chemokine Improves Protection against Genital Herpes through Mobilization of Antiviral Effector Memory CCR10+CD44+ CD62L-CD8+ T Cells and Memory CCR10+B220+CD27+ B Cells into the Infected Vaginal Mucosa.
J Immunol, 211(1):118-129, 01 Jul 2023
Cited by: 4 articles | PMID: 37222480
Does IFITM3 link inflammation to tumorigenesis?
BMB Rep, 55(12):602-608, 01 Dec 2022
Cited by: 4 articles | PMID: 36404597 | PMCID: PMC9813432
Review Free full text in Europe PMC
Type I interferon regulates proteolysis by macrophages to prevent immunopathology following viral infection.
PLoS Pathog, 18(5):e1010471, 05 May 2022
Cited by: 4 articles | PMID: 35512020 | PMCID: PMC9113601
Immunoregulatory Functions of Interferons During Genital HSV-2 Infection.
Front Immunol, 12:724618, 18 Aug 2021
Cited by: 4 articles | PMID: 34484233 | PMCID: PMC8416247
Review Free full text in Europe PMC
Go to all (72) article citations
Data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
NK and NKT cell-independent contribution of interleukin-15 to innate protection against mucosal viral infection.
J Virol, 79(7):4470-4478, 01 Apr 2005
Cited by: 39 articles | PMID: 15767447 | PMCID: PMC1061577
Toll-like receptor (TLR)-3, but not TLR4, agonist protects against genital herpes infection in the absence of inflammation seen with CpG DNA.
J Infect Dis, 190(10):1841-1849, 18 Oct 2004
Cited by: 103 articles | PMID: 15499542
Role of IFN-alpha/beta signaling in the prevention of genital herpes virus type 2 infection.
J Reprod Immunol, 74(1-2):114-123, 07 Nov 2006
Cited by: 32 articles | PMID: 17092567
The role of toll-like receptor ligands/agonists in protection against genital HSV-2 infection.
Am J Reprod Immunol, 59(1):35-43, 01 Jan 2008
Cited by: 24 articles | PMID: 18154594
Review





