Abstract
Free full text
Extracellular Proteolysis in Transgenic Mouse Models of Breast Cancer
Abstract
Growth and invasion of breast cancer require extracellular proteolysis in order to physically restructure the tissue microenvironment of the mammary gland. This pathological tissue remodeling process depends on a collaboration of epithelial and stromal cells. In fact, the majority of extracellular proteases are provided by stromal cells rather than cancer cells. This distinct expression pattern is seen in human breast cancers and also in transgenic mouse models of breast cancer. The similar expression patterns suggest that transgenic mouse models are ideally suited to study the role of extracellular proteases in cancer progression. Here we give a status report on protease intervention studies in transgenic models. These studies demonstrate that proteases are involved in all stages of breast cancer progression from carcinogenesis to metastasis. Transgenic models are now beginning to provide vital mechanistic insight that will allow us to combat breast cancer invasion and metastasis with new protease-targeted drugs.
Introduction
Breast cancer progression is accompanied by increased expression of proteases that are capable of degrading the extracellular matrix (ECM) leading to cancer cell invasion and eventually to dissemination of cancer cells to other organs. The proteolytic capability of breast cancers is reminiscent of the inherent proteolytic capability of the healthy mammary gland. Extracellular proteases are necessary for the dynamic tissue remodeling that takes place during normal mammary gland development and pregnancy cycling (reviewed in [1]). During development, the invasive phenotype of terminal end buds is associated with a controlled proteolytic digestion of ECM in the fat pad, and side branching of the newly formed ducts requires a focal degradation of basement membrane. The proliferative response of the epithelium during pregnancy and lactation is accompanied by limited proteolytic activity. In contrast, the involution of the lactating gland to a resting gland after weaning restructures the entire gland and requires extensive degradation of ECM and basement membranes. Extracellular proteases are thus more abundant during involution than at any other stage during development and the pregnancy cycle. The similarity between the proteolytic repertoire of the normal gland and the proteolytic capability of mammary cancers is best illustrated by the fact that the cellular expression patterns of individual proteolytic components are very alike, especially when comparing involution and cancer [2]. In terms of extracellular proteolysis, breast cancer in many ways resembles a mammary gland in a state of continuous and uncontrolled tissue remodeling.
Matrix Metalloproteases and Plasminogen Activators
Two families of extracellular proteases have been extensively studied in relation to mammary gland morphogenesis and cancer. These are the matrix metalloproteases (MMPs) and the group of serine proteases that govern the activation of plasminogen (Plg). Figure 1 illustrates the connected extracellular proteolytic network of the MMPs and the Plg activation system (PA system).
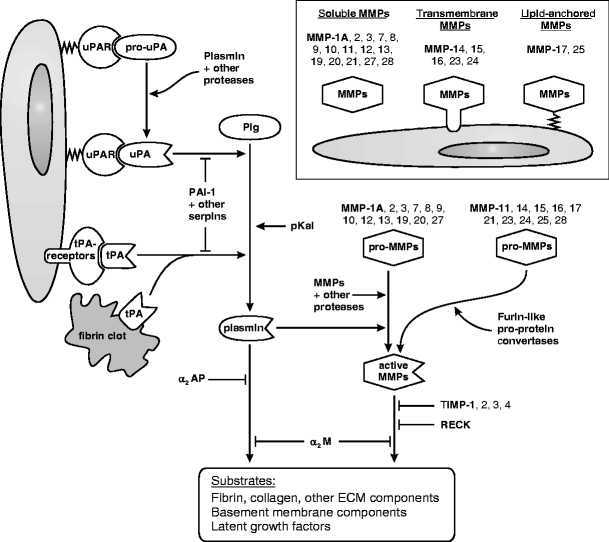
The PA and MMP systems in the mouse. Plasmin and MMPs are two major sources of extracellular proteolysis. Plg is converted to the active protease plasmin by one of three Plg activators, uPA, tPA, and pKal. The generation of plasmin is enhanced by the binding of uPA to the cell surface receptor uPAR, and by the binding of tPA to coagulated fibrin or to cell surface proteins (annexin II [86] and CKAP4 [87]). The conversion of pro-uPA to active uPA may be initiated by several proteases, depending on the tissue in question. Additional pro-uPA is then activated by plasmin in a positive feed-back loop. The PA system is tightly controlled by several serine protease inhibitors (serpins); the primary and most specific inhibitors are the Plg activator inhibitor PAI-1 that targets uPA and tPA, and the plasmin inhibitor α2-antiplasmin (α2AP). Major substrates of plasmin include fibrin, fibronectin, laminin, and other ECM proteins, latent TGF-β and other growth factors, and pro-MMPs. The 22 different mouse MMPs are all extracellular, and are either soluble or membrane-anchored. Like the serine proteases of the PA system, the MMPs are also synthesized as inactive proforms that require proteolytic activation. Ten of the 22 pro-MMPs, including the membrane-anchored MMPs, have a furin cleavage site and may be activated by furin-like proprotein convertases before they are secreted. The remaining pro-MMPs are activated extracellularly, typically by plasmin or by other MMPs. The MMP system is counterbalanced by a group of four inhibitors, TIMPs, that have varying specificities for individual MMPs. In addition, the membrane-anchored MMP inhibitor RECK regulates a subgroup of MMPs including MMPs-2, -9, and -14 [88]. An excess of plasmin or MMP activity may ultimately be cleared by α2-macroglobulin (α2M) which is a non-specific protease scavenger. The MMPs are collectively able to degrade any component of the ECM. Important substrates for the MMPs as a group include the native fibrillar collagens and all four major components of the basement membrane: collagen type IV, laminin, nidogen/entactin, and heparan sulfate proteoglycans.
The liver-derived proenzyme Plg is found in high concentration throughout the body. In contrast, expression of the specific urokinase- and tissue-type Plg activators (uPA and tPA) is induced locally and thus determines where and when Plg is converted to the active protease plasmin [3, 4]. Plasmin, activated by uPA, is important for a number of tissue remodeling processes that, in addition to pregnancy cycling of the mammary gland [5], include wound healing [6] and embryo implantation [7]. In contrast, tPA is acknowledged to be primarily involved in thrombolysis and neurobiology [3, 4] but is also active during wound healing [8]. A newly identified Plg activator, plasma kallikrein (pKal), is involved in adipocyte differentiation in the involuting mammary gland [9] and in wound healing [8].
The MMPs constitute a large family of 22 extracellular metalloproteinases in mice (24 in humans) [10, 11] (an updated list of human and mouse proteases is available at http://web.uniovi.es/degradome/). MMPs are essential for a number of physiological tissue remodeling processes during ontogenesis and adult life, including mammary gland development [12, 13], bone development [14], wound healing [15], and embryo implantation [7]. During mammary gland development MMP-2 is involved in ductal elongation, and MMPs-2 and -3 are involved in ductal branching [13]. MMP-3 is also rate limiting for adipocyte differentiation during post-lactational involution [16]. The ductal tree is eventually fully formed in mice that are deficient in MMP-2, -3 or several other MMPs, indicating that the remaining MMPs are able to replace their activity in a functional overlap.
Several members of the MMP and PA systems are involved in breast cancer progression. We will focus on the role played by these extracellular protease families during the various stages of breast cancer progression, from the initial hyperplastic lesion to disseminated disease, with particular emphasis on the insight gained from transgenic mouse models.
Mouse Models of Breast Cancer
The mouse mammary gland is ideally suited to study cancer progression for a number of reasons. First of all, there are many similarities between the human and mouse mammary glands (for detailed reviews see [17, 18]). Human and mouse mammary glands contain the same epithelial cell types: the ductal epithelial cells, luminal (milk secreting) epithelial cells, and the myoepithelial cells. They also contain adipose tissue and stroma, although the composition of the stroma differs between the human and mouse glands. One of the few differences between the species is that the epithelium in the mouse gland is surrounded by adipose tissue and a relatively sparse stroma, whereas the human mammary epithelium is encompassed by a specialized fibroblastoid stroma and is not in direct contact with adipocytes. The epithelial structure in the mature nulliparous mouse gland is also much less developed compared to the human gland and consists only of a branching but otherwise naked ductal tree. In contrast, the mature ductal tree in non-pregnant women contains groups of acini at the end of terminal ducts, named terminal ductal lobular units (TDLU). The mouse epithelium develops similar lobuloalveolar structures transiently during the estrus cycle in certain mouse strains [19] and always during early pregnancy, and in this way the resting human gland is structurally more similar to the pregnant mouse gland. In some transgenic breast cancer models, the earliest hyperplastic lesions may also resemble TDLU-like structures [20].
A second ideal feature of the mouse mammary gland is that it is readily accessible for monitoring tumor growth and for other experimental procedures. This has lead to the development of numerous transplanted models, chemically induced models and transgenic models. We will limit our discussion to the transgenic and chemically induced models since there are inherent problems of transplanted models that may introduce bias. Depending on the study design, these obstacles can include: (1) a species barrier between proteolytic components supplied by the transplant and the host (as documented for human and mouse uPA and its receptor uPAR [21]); and (2) a cellular inconsistency with respect to protease expression in the sense that the majority of proteolytic components are supplied by stromal cells in human breast cancers while epithelial-based cancer cell lines often express the very same proteolytic components [22]. This is presumably due to genetic alterations that have occurred during in vitro culture. Furthermore, (3) when gene-deficient mice are used as hosts for syngeneic transplantation, it is possible that a tumor-suppressive phenotype in the protease-deficient host is due to an immune response directed at the protease-producing transplant.
A third advantage of the mammary gland for cancer research is that there are more transgenic models of mammary cancer than for any other cancer form, primarily because relatively specific promoters are available for targeting oncogene expression to the mammary epithelium. The promoters most frequently used stem from the whey acidic protein (WAP) gene, and the mouse mammary tumor virus long terminal repeat (MMTV). The promoters are not equally active at all stages of mammary gland development and the pregnancy cycle [23]. The MMTV promoter is active during puberty but is greatly enhanced during pregnancy. The WAP promoter is primarily active from mid pregnancy and during lactation. Accordingly, cancer progression is accelerated by pregnancies in most transgenic models and some models only develop tumors after a number of pregnancies.
Finally, the tumor histopathology of several transgenic models is very similar to human breast cancers [17]. The histopathology seen in a single mouse model is, however, relatively uniform and often characteristic of the inducing oncogene, and in this way no single model replicates the variability of tumor phenotypes seen among different breast cancer patients [17, 24]. This drawback is to be expected, considering the fact that transgenic models rely on a well-defined initiating oncogene in mice with a homogenous genetic background (inbred strains). In contrast, human breast cancers arise from combinations of multiple mutations in women with heterogenous genetic backgrounds. A notable similarity between mouse and human tumors is the development of a reactive stroma and the appearance of extracellular proteolysis in the tumor microenvironment. There are, however, also significant drawbacks to the use of transgenic models, such as the fact that they express oncogenes in the entire mammary epithelium (or at least a large part of it) often giving rise to multiple tumors and in some models a general hyperplasia of the entire gland. By contrast, human tumors derive from a single site, therefore resulting in a single tumor in the breast.
A comprehensive list of transgenic breast cancer models is available at http://emice.nci.nih.gov/ and has recently been reviewed [23]. Here we will focus on models that have been studied in relation to extracellular proteolysis. Table 1 summarizes the studies that describe MMP or PA system intervention in transgenic and chemically induced breast cancer models. It is evident from Table 1 that the role of proteases has almost exclusively been studied in models, in which one of the four oncoproteins ErbB-2 (neu) [25], Ras [26], Wnt1 [27], or the polyomavirus middle T antigen (PymT) [28] are induced by the MMTV promoter. ErbB-2 is often overexpressed in human breast cancers. Ras and the downstream effector proteins of Wnt1 and PymT are also frequently activated in human breast cancer, although mutation/overexpression of Ras and Wnt1 are infrequent in breast cancer and there is no cellular counterpart of the PymT oncogene [23]. In all four transgenic models, tumor incidence is 100% or at least approaches 100% depending on the time allowed for observation [29–32]. Tumor incidence has only in a few cases [29, 32] been affected in protease intervention studies (Table 1). Tumor onset in the ErbB-2, Ras, and Wnt1 models can be accelerated by multiple pregnancies [25, 30, 32] and mice used for experiments are frequently mated continuously, at least in the Ras and Wnt1 models [30, 32]. The PymT model is exceptionally fast even in non-pregnant mice, where the average tumor latency is approximately 1.5 months [31] compared to 4–7 months for multiparous mice in the three other models [25, 30, 32]. In all four models the tumors metastasize primarily to the lungs although the models differ in aggressiveness. The PymT model is the most aggressive and the Wnt1 model the least aggressive [31, 32]. A notable exception to the use of transgenic models in protease studies is the chemically induced mammary tumors that are induced by orally administered 7,12-dimethylbenzanthracene (DMBA) with or without hormone supplementation [33, 34]. The DMBA model is primarily a carcinogenesis model, since the tumors generally do not progress to form metastases [33, 34].
Table 1
PA system and MMP intervention studies in transgenic and chemically induced breast cancer models.
| Proteolytic intervention | Mouse br.ca. model | Phenotypic effect on mammary neoplasia | Reference | ||||||
|---|---|---|---|---|---|---|---|---|---|
| tumor incidence | tumor onset | tumor growth rate | final tumor size | lung metastasis incidence | lung metastasis burden | comments and additional phenotypes | |||
| Plg activation system | |||||||||
| Plg null | MMTV-PymT | ↔ | ↔ (↓ trend) | ↔ | ↔ | ↓ | ↓ | reduced metastasis in 129:BSw:FVB mixed strain but not in FVB mice | [44] and unpublished data |
| uPA null | MMTV-PymT | ↔ | ↔(↓ trend) | ↔ | ↔ | ↔ | ↓ | + reduced lymph node metastasis | [31] |
| PAI-1 null | MMTV-PymT | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ (↑ trend) | tumor vascularization not affected | [45] |
| uPAR null | MMTV-PymT | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | no phenotype in the FVB strain | unpublished data |
| MMP protease family | |||||||||
| MMP overexpression | |||||||||
| MMTV-MMP-3 transgene | none | yes* | *tumors develop in the CD1 mouse strain but not in mixed B6:DBA mice | [33, 61], see comment in [90] | |||||
| WAP-MMP-3 transgene | none | yes* | *tumors develop in the CD1 mouse strain but not in FVB mice | [62], see comment in [90] | |||||
| MMTV-MMP-7 transgene | none | no | hyperplasia in multiparous mice but no tumors develop spontaneously | [29] | |||||
| MMTV-MMP-14 transgene | none | yes | tumors develop spontaneously | [63] | |||||
| MMTV-MMP-3 transgene | DMBA gavage | ↓ | ↓ | opposite expectation | [33] | ||||
| MMTV-MMP-3 transgene | DMBA gavage + MMTV-TGFα | ↔ | ↔ | [33] | |||||
| MMTV-MMP-7 transgene | MMTV-neu | ↑ | ↑ | ↔ | ↔ | [29] | |||
| MMTV-MMP-7 transgene | ApcMin + ENU | ↔ | [91] | ||||||
| MMP inhibition | |||||||||
| MMP inhibitor-treatment (galardin/GM6001) | MMTV-PymT | ↓ | ↓ | ↓ | unpublished data | ||||
| MMP-2 null | MMTV-PymT | ↔ | ↔ | ↔ | ↔ | ↓ | ↓ | Fingleton and Matrisian, pers. comm. | |
| MMP-7 null | MMTV-PymT | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | Fingleton and Matrisian, pers. comm. | |
| MMP-7 null | ApcMin + ENU | ↓ | transient reduction in number of mammary tumors | [91] | |||||
| MMP-9 null | MMTV-PymT | ↔ | ↔ | ↔ | ↔ | ↓ | ↓ | reduced metastasis in mixed B6:FVB mouse strain but not in FVB mice | Fingleton and Matrisian, pers. comm. |
| MMP-9 null | MMTV-neu | ↑ | (meeting report [67]) | ||||||
| MMP-11 null | MMTV-ras | ↔ | ↓ | ↓ | ↑ | bidirectional effect | [30] | ||
| MMP-11 null | DMBA gavage | ↓ | ↓ | ovarian and mammary carcinomas | [66] | ||||
| MMP-13 null | MMTV-PymT | ↔ | ↔ | ↔ | ↔ | ↔ | ↔ | unpublished data | |
| WAP-TIMP-1 transgene | WAP-MMP-3 | ↓ | reduced incidence of hyperplasias, no tumors develop | [62] | |||||
| Albumin-TIMP-1 transgene | DMBA gavage + MPA | ↓ | early hyperplasia not affected | [34] | |||||
| Albumin-TIMP-1 transgene | MMTV-PymT | ↔ | ↓ | ↓ | ↔ | [34] | |||
| MMTV-TIMP-1 transgene | DMBA gavage + MPA | ↔ | [34] | ||||||
| MMTV-TIMP-1 transgene | MMTV-PymT | ↔ | ↔ | ↔ | [34] | ||||
| MMTV-TIMP-2 transgene | MMTV-Wnt1 | ↓ | ↓ | ↓ | ↓ | reduced mean vessel size in tumors | [32] | ||
| TIMP-2 gene therapy | MMTV-neu | ↓ | ↓ | [92] | |||||
Abbreviations: ApcMin multiple intestinal neoplasia model in mice with a mutated Apc allele; B6, C57BL/6J; BSw Black Swiss; DMBA 7,12-dimethylbenzanthracene; ENU N-ethyl-N-nitrosourea; MMP matrix metalloprotease; MMTV mouse mammary tumor virus long terminal repeat promoter; MPA medroxyprogesterone acetate; PAI-1 Plg activator inhibitor-1; Plg plasminogen; PymT polyomavirus middle T antigen; TIMP tissue inhibitor of metalloproteases; uPA urokinase plasminogen activator; uPAR uPA receptor; WAP whey acidic protein promoter.
A feature of any transgenic model that is particularly relevant to extracellular proteolysis is the transition from pre-invasive (carcinoma in situ, CIS) to invasive breast carcinoma. Most human pre-invasive lesions are ductal CIS (DCIS), and in these lesions the carcinoma cells accumulate in the ducts confined by the myoepithelial cell layer and the basement membrane. Proteolytic degradation of the basement membrane leads to depolarization of the myoepithelial cells and offers the carcinoma cells access to the surrounding periductal stroma [35, 36]. In some human breast carcinomas the tumor suppressive myoepithelium surrounding an emerging tumor can persist for a relatively long period of time. In the MMTV-PymT model the late stage tumors resemble human invasive ductal breast cancer, but the myoepithelium is lost very early in tumor progression and it is therefore a poor model of the CIS stage ([20] and unpublished data). The lack of an intact myoepithelium, as seen in the MMTV-PymT model, does not necessarily make the neoplastic cells invasive. These lesions fall in the broad category of mammary intraepithelial neoplasia (MIN), which includes CIS-like lesions but is used more generally in mouse tumors to describe pre-malignant epithelial cells that have significant nuclear atypia and are surrounded by an intact basement membrane [37]. A few transgenic breast cancer models have been described to develop CIS lesions with morphologic similarities to human DCIS and later progress into invasive breast cancer. These include the C3(1)-SV40-T prostate cancer model that also develops mammary lesions [38], the WAP-SV40-T model [39], and the MMTV-neu models [17]. However, the CIS stage has not been the focus of protease intervention studies so far.
Protease Expression in Transgenic Breast Cancer Models
Extracellular proteases are generally absent in resting mammary glands but are present as the gland undergoes the pregnancy cycle. The levels of a number of extracellular proteolytic components are particularly upregulated during post-lactational mammary gland involution. These include uPA, tPA, MMPs-2, -3, -9, -11, and their corresponding inhibitors PAI-1 and TIMP-1 [5, 40–42]. The upregulated proteases and protease inhibitors are presumably required for the orderly restructuring of the lactating gland to a virgin-like state (discussed later). During breast cancer development, a similar proteolytic program is activated in the diseased gland and extracellular proteases are abundant in invasive breast cancers of both humans and mice. Figure 2 gives a schematic comparison of the expression patterns of MMP and PA system components in human breast cancer and in the MMTV-PymT transgenic breast cancer model, which has been used to analyze the expression of several extracellular proteases. One study used laser microdissection to isolate cancer cells and stromal cells followed by quantitative RT-PCR to examine the expression level of MMPs and the PA system [43]. The study concluded that stromal tissue adjacent to cancer cells expresses higher levels of uPA, PAI-1 and MMPs-2, -3, -11, -13, and -14 than the cancer tissue. The predominantly stromal expression patterns of all these components in the MMTV-PymT model has been confirmed by in situ hybridization [31, 43–46]. Using immunohistochemistry, uPAR expression was found primarily in fibroblasts, endothelial cells, and in some macrophages in the MMTV-PymT model (unpublished data). In situ hybridization was used in another study on MMTV-PymT tumors to determine the expression pattern of four of the membrane-type MMPs: the transmembrane MMPs-14, -15, and -16 and the GPI-linked MMP-17 [46]. MMPs-14 and -16 were detected in the stroma whereas MMP-15 was the only protease found predominantly in the epithelium. MMP-17 expression was not observed in the MMTV-PymT tumors. The majority of these findings reflect the mRNA expression data for human breast cancer, since uPA [47], PAI-1 [48], and MMPs-2 [49], -3 [50], -11 [49], -13 [35], and -14 [51] all are found predominantly in the stroma (see suppl. data to review by Egeblad and Werb 2002 [10]). Immunoreactivity for uPAR is also primarily found in the stroma [52]. Figure 3 provides two examples of this close correlation between human and transgenic mouse tumors: MMP-13 is focally expressed in stromal cells in patient material [35] and in MMTV-PymT transgenic tumors [43] (Fig. 3c–d). Similarly, the primary uPA inhibitor PAI-1 is expressed in stromal cells in MMTV-PymT mice [45] and in breast cancer patients [48] (Fig. 3e–f). The PAI-1-producing stromal cells were identified as myofibroblasts in the human samples. It is of note that this cell type is uncommon in the normal mouse and human glands but is abundant in tumors from both transgenic mice (unpublished data) and breast cancers patients [53].

Expression of MMPs and PA components in breast tumors in humans and in MMTV-PymT transgenic mice. MMPs and PA components are expressed by cancer cells or stromal cells in breast tumors or are present as ubiquitous plasma-derived proteins. The predominant source of each mRNA/protein is illustrated for human ductal breast cancer and for the MMTV-PymT model in mice. Only those proteases and related components that have been analyzed in the MMTV-PymT model are included in the comparison. Only mRNA analyses are included except for uPAR, which was analyzed by immunohistochemistry in both species. The “Not detected” category includes proteases that were sporadically expressed in the tumors. The data for the MMTV-PymT model: uPA [31]; PAI-1 [45]; uPAR, MMPs-7, -9, -10 (unpublished data); MMPs-2, -3, -11, -13, -14, uPA, PAI-1 [43]; MMPs-14, -15, -16, -17 [46]. The data for invasive ductal breast cancer: uPA [47]; PAI-1 [48]; uPAR [52]; MMP-2 [49]; MMP-3 [50], MMP-7 [89]; MMP-9 [72]; MMP-10 [89]; MMP-11 [49]; MMP-13 [35]; MMP-14 [51].
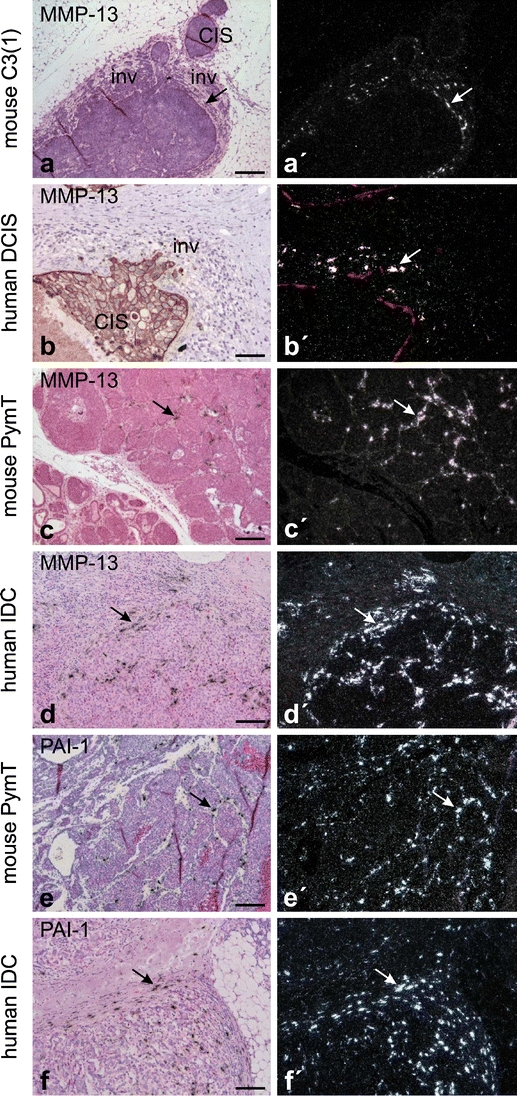
Examples of protease expression in breast cancer from transgenic mice and humans. Expression of MMP-13 during early invasion in mouse C3(1)-SV40-T breast carcinoma (a) and in human ductal carcinoma in situ (DCIS) (b). MMP-13 is focally expressed in periductal fibroblast-like cells (arrows in a, a’, and b’) in areas with early cancer cell invasion (inv) and is not expressed in adjacent non-invasive areas with in situ carcinoma (CIS). Expression of MMP-13 in invasive MMTV-PymT carcinoma (c) and in human invasive ductal carcinoma (IDC) of the breast (d). Focal expression of MMP-13 is seen in fibroblast-like cells located in the stroma surrounding invasive cancer cells in both mouse and human breast cancers (arrows in c and d). Expression of PAI-1 in invasive MMTV-PymT carcinoma (e) and in human IDC of the breast (f). The expression of PAI-1 is seen in fibroblast-like cells located in the stroma surrounding invasive cancer cells in both the mouse and human breast cancers (arrows in e and f). All panels are in situ hybridization using 35S-labeled probes. Panels a, c–f are counterstained with haematoxylin and eosin, whereas b is combined with pan-cytokeratin immunohistochemistry and (b’) with CK14 immunohistochemistry for myoepithelial cells [35]. Bars: a,c, 200 μm; b, 100 μm; d–f, 150 μm.
Recently, the MMTV-Wnt1 model has also been used to study the expression levels of a number of MMPs during mammary tumor formation by RT-PCR and in situ hybridization [32]. MMPs-2, -3, -9, -13, and -14 displayed increased expression levels in hyperplastic glands and mammary tumors. MMPs-2, -3, and -9 were exclusively expressed in the stroma, while MMPs-13 and -14 were found predominantly in the cancer cells and to a lesser extent also in stromal cells. Again, most of these MMPs have been reported with similar expression patterns in human breast cancer, although MMPs-13 and -14 are predominantly stromal in ductal breast cancer [35, 51]. It is noteworthy that the MMTV-PymT and MMTV-Wnt1 models have broadly similar but not identical localization and expression of MMPs.
The initial expression of proteases in human breast cancer may be associated with the transition from DCIS to invasive ductal carcinoma. The transition to invasive cancer can be identified histopathologically in some DCIS lesions, particularly facilitated by immunohistochemical staining of myoepithelial cells and intraductal neoplastic cells. Expression studies of MMPs in human DCIS material have shown that MMP-13 is focally upregulated in microinvasive foci (Fig. 3b) in contrast to MMPs-2, -11, and -14, which are all more broadly expressed in the samples [35]. All four of these MMPs are expressed in periductal (myo)fibroblasts, indicating an intense stromal involvement during early invasion. Brummer et al. found that TIMP-1 is also upregulated in areas of early invasion [54]. Mimicking the human situation, the C3(1)-SV40-T model develops DCIS-like lesions, in which MMP-13 is upregulated specifically in those DCIS-like structures that show signs of invasion (Fig. 3a). In human samples, uPA and uPAR are also focally upregulated in areas of microinvasion together with MMP-13, suggesting that plasmin-directed proteolysis coincides with MMP activity in the transition to invasive cancer [36].
Thus, the extracellular proteases expressed in transgenic breast cancer models generally mirror those identified in human breast cancer both in terms of expression and localization. These findings suggest that transgenic models are useful tools for the study of protease involvement in breast cancer invasion and metastasis.
Functional Studies of Proteases in Breast Cancer Progression
Proteases in Post-lactational Mammary Gland Involution
Mammary gland involution following weaning can to some extent be regarded as a surrogate model for the role of proteases in breast cancer invasion due to the extensive tissue remodeling and extracellular proteolysis taking place. The first, reversible stage of involution is prematurely activated in Plg-deficient mice likely due to increased milk stasis during lactation [55]. However, the second, protease-dependent and irreversible stage of involution seems to be delayed in Plg-deficient mice [5]. Involution is eventually accomplished in Plg-deficient mice probably due to compensating action of other proteases including MMPs. In support of this hypothesis, implantation of TIMP-1 slow release pellets into involuting mammary glands delays alveolar regression [40], and likewise TIMP-3 null mice exhibit accelerated involution [56]. In contrast, transgenic overexpression of TIMP-1 in luminal cells did not provoke an involution phenotype [16, 57], which may be a cell-of-origin effect since endogenous TIMP-1 is produced by stromal cells during involution [40, 58]. Similarly, the accelerated involution observed in mice that overexpress MMP-3 in luminal cells [57, 59] could be an effect of overexpressing a stromal protein in luminal cells, and is not supported by evidence from MMP-3 null mice that do not show a change in mammary apoptosis [16, 57]. The fact that the PA system and the MMPs are required for the controlled tissue remodeling of the involuting mammary gland, suggests that it is the inherent proteolytic repertoire of the mammary gland that is reactivated in breast cancers.
Proteases in Hyperplasia and Carcinogenesis
The earliest stages of mammary carcinogenesis including the initial genetic alterations in the epithelial cells were previously considered to be independent of the surrounding stroma and extracellular proteolysis. It now seems that the structural integrity of the stroma is an essential factor in preventing carcinogenesis [60]. In fact, disruption of the ECM and cellular microenvironment caused by overexpression of MMPs-3, -7 or -14 in the mammary gland is sufficient to initiate mammary epithelial hyperplasia [29, 61–63]. Transgenic mice overexpressing MMP-3 or MMP-14 even develop tumors in the absence of a transgene-supplied oncogene, and a fraction of the tumors undergo malignant transformation [62, 63]. Similar transgenic overexpression of Plg activators has not been reported for the mammary gland, but a K14-uPA/uPAR double transgene elicits extensive skin hyperplasia [64]. The MMP transgenes all direct MMP expression to the mammary epithelium, using either MMTV or WAP promoters. Only MMP-7 is expressed by normal mammary epithelium [65], while MMPs-3 and -14 are expressed by the mammary stroma during development and in the mature gland [46, 61]. Thus, tumor growth and malignancy have only been reported in cases where extracellular proteases were expressed by cells that would not normally produce them. Nevertheless, ectopically expressed proteases act as independent tumor promoters, presumably by compromising the growth-inhibitory role of the stroma, and eventually lead to genetic instability as if they were conventional oncogenes.
In light of the independent tumorigenic ability of some MMP transgenes, it is not surprising that tumor onset in transgenic breast cancer models is promoted by increased MMP activity and delayed by decreased MMP activity in some studies (Table 1). Tumor onset is thus promoted by MMP-7 overexpression in the MMTV-neu model [29] and delayed by MMP-11 deficiency in the MMTV-ras model [30] or by TIMP-2 overexpression in the MMTV-Wnt1 model [32]. Similarly, the incidence of DMBA-induced mammary tumors is reduced in MMP-11-deficient [66] and in TIMP-1-overexpressing mice [34]. The results of two studies were inconsistent with the general finding: MMP-3 overexpression resulted in reduced rather than increased tumor incidence in the DMBA model [33], and MMP-9 deficiency led to increased tumorigenesis in the MMTV-neu model [67]. This suggests that some MMPs may have a protective function in mammary tumorigenesis, similar to the protective role of MMP-8 in chemical carcinogenesis of the skin [68].
In contrast to the documented influence of some of the MMPs on tumor initiation, the PA system (including genetic deficiency in Plg [44], uPA [31], PAI-1 [45], or uPAR [unpublished data]) does not affect tumor onset in the MMTV-PymT model. Neither does TIMP-1 overexpression [34] or genetic deficiencies of MMPs-2, -7, -9 (Fingleton and Matrisian, personal communication) or MMP-13 (unpublished data) in the MMTV-PymT model. At present it is difficult to determine whether these differences reflect the nature of the different proteases or perhaps that the very early tumor onset, which takes place during puberty in the MMTV-PymT model, is less sensitive to the proteolytic environment.
Proteases in Tumor Growth and Vascularization
Mammary hyperplasias and CIS lesions are generally supplied with oxygen and nutrients by the pre-existing vasculature of the mammary gland. Tumor expansion beyond a certain stage requires the formation of new blood vessels. Angiogenesis, the sprouting of new vessels from existing vasculature, depends on proteolytic dissection of the endothelial basement membrane and other ECM components. Endothelial cells penetrate a newly deposited fibrin-rich matrix and use it as a temporary scaffold for vessel structure [69]. Accordingly, the fibrinolytic capacity of the PA system is crucial for vascularization in certain experimental settings, and PAI-1 may play a dual role as a protease inhibitor and cell migration mediator [3]. In tumors from breast cancer patients, endothelial cells are a considerable source of uPA, PAI-1 and uPAR suggesting a possible role in vascularization [47, 48, 52]. This has not been experimentally confirmed in transgenic tumors thus far (Table 1). In the MMTV-PymT model, tumors grow equally fast in the genetic absence or presence of Plg [44], uPA [31], PAI-1 [45] or uPAR (unpublished data), indicating that vascularization is not rate limiting for tumor growth in these cases. It is likely that functional redundancy with other proteolytic components compensates for the absence of a single component in the intact tumor. Even in PAI-1-deficient tumors, vascular density was not significantly different from wild type tumors [45]. It is also possible that vascularization of spontaneous tumors can be partially accomplished by endothelial precursor cells in a process termed vasculogenesis that may be independent of proteases or depend on a different subset of proteases [11].
Deficiency of MMP-9 reduces tumor growth in transgenic models of skin or β-cell islet tumors, most likely due to a requirement for MMP-9 to release vascular endothelial growth factor (VEGF) from ECM deposits in order to activate the angiogenic response [70, 71]. In human breast tumors MMP-9 is expressed by a subset of inflammatory cells and vascular pericytes, which could suggest a similar role of MMP-9 in breast cancer vascularization [72]. However, the evidence is less clear in transgenic breast cancer models (Table 1). Final tumor size in MMTV-PymT-transgenic mice is not significantly affected by single gene deficiencies of MMPs-2, -7, -9 (Fingleton and Matrisian, personal communication), or MMP-13 (unpublished data). Deficiency of a single MMP may be compensated by the presence of other MMPs. In contrast, simultaneous inhibition of a number of MMPs through a liver-specific TIMP-1 transgene significantly reduced final tumor size (by 42%) in MMTV-PymT mice [34]. Transgenic overexpression of TIMP-2 also caused a significant reduction in tumor growth rate and reduced the mean blood vessel size in MMTV-Wnt1 mammary tumors, providing direct evidence for an effect on vascularization [32]. MMP-11 may be important at this stage, since MMP-11-deficient mice develop significantly smaller tumors in the DMBA [66] and MMTV-ras [30] models. Surprisingly, a broad spectrum MMP inhibitor (galardin) only resulted in a 50% reduction in final tumor size in the MMTV-PymT model (unpublished data). It is possible that some MMPs promote while others inhibit tumor growth and vascularization, and the net effect of inhibiting a whole range of MMPs is rather limited. A protective role against tumor growth and vascularization has been observed in non-mammary models for MMP-3 [73] and MMP-19 [74].
Proteases in Cancer Metastasis
In order to successfully form metastases, cancer cells must enter the lymphatic system or the bloodstream, survive in circulation and arrest in the vasculature, extravasate and finally be able to proliferate in the new tissue. There are several metastasizing transgenic models, but the majority of models metastasize rather infrequently and only when the primary tumors are quite large. In addition to the MMTV-PymT [28] and MMTV-neu [25] models, very few other breast cancer models metastasize sufficiently to allow rigorous quantification (reviewed in [75]). Metastasis can be greatly accelerated by combining e.g. an MMTV-neu model with a second mammary-specific transgene for VEGF or transforming growth factor-β1 (TGFβ1) [75–77], but these models require more elaborate breeding. Proteases are intimately associated with metastasis. A classic example is the osteolytic bone metastases that are so frequent in breast cancer patients. Breast cancer cells and the resident osteoclasts stimulate each other in a feed-back activation loop. Cancer cells stimulate MMP-dependent degradation of the collagen type I rich bone matrix by osteoclasts [78, 79]. As a consequence of bone lysis, latent growth factors are released from their deposits within the bone ECM, and are available to stimulate further cancer cell proliferation. Unfortunately, transgenic models generally metastasize to the lungs and in this way the models do not exactly mimic the organ preference of metastatic breast cancer in humans.
The PA system plays a unique role in metastasis at least in the MMTV-PymT model that metastasizes to the lungs [28] and lymph nodes [31] (Table 1). uPA [31], PAI-1 [45], and uPAR (unpublished data) are all expressed both in the primary tumor and in the lung metastases. Metastasis is significantly reduced in both Plg-deficient and uPA-deficient mice, while these gene deficiencies have no significant effect on the primary MMTV-PymT tumors [31, 44]. Absence of the specific uPA inhibitor PAI-1 has a slight metastasis-promoting effect, but the difference is not significant perhaps due to the presence of alternative uPA inhibitors [45]. Deficiency of uPAR does not significantly affect metastasis in the inbred FVB strain (unpublished data).
Plg and uPA may promote metastasis due to their fibrinolytic ability. Fibrin-deficient mice have not been studied in a transgenic model, but they are less susceptible to spontaneous metastasis from transplanted tumors [80] and lung colonization by tail vein-injected cells [81], suggesting that fibrin is important for sustained adhesion of circulating cancer cells in the target organ. Thus, metastasis may depend on an intact and balanced system of fibrin formation and fibrinolysis. Alternatively, Plg and uPA may promote metastasis by releasing growth factors from the ECM. Overexpression of relevant ECM-sequestered growth factors promotes breast cancer progression and metastasis in transgenic models [76, 77, 82, 83]. These growth factors include the possible plasmin substrates VEGF, TGFβ, and FGF (fibroblast growth factor), as well as the possible uPA substrate HGF (hepatocyte growth factor).
There is also considerable evidence linking the MMPs to invasion and metastasis (reviewed in [10, 84]). In MMTV-PymT mice treated with the broad spectrum MMP inhibitor galardin, the average lung metastasis volume is reduced by approximately 99%, in the context of primary tumors that are only reduced by half (unpublished data). Metastasis incidence is also reduced in MMTV-PymT mice that overexpress TIMP-1 through a liver-specific transgene, but the reduction is less pronounced and is absent with a mammary gland-specific TIMP-1 transgene [34]. It will take a considerable effort to define which MMPs are responsible for the metastasis reduction observed with these inhibitors. MMP-9 deficiency results in reduced metastasis in the MMTV-PymT model, although this phenotype was mouse strain dependent (Fingleton and Matrisian, personal communication). Deficiency of MMP-2, which is abundantly expressed in the stroma of MMTV-PymT tumors [43], also results in reduced metastasis in the same model (Fingleton and Matrisian, personal communication). MMPs-2 and -9 have previously been associated with invasion and metastasis in a number of studies [84]. In contrast, there is no effect on metastasis in MMTV-PymT mice that are deficient in either MMP-7 (Fingleton and Matrisian, personal communication) or MMP-13 (unpublished data). Similarly, overexpression of MMP-7 in mammary glands has no effect on lung metastasis in the MMTV-neu model [29].
MMP-11 may play an unexpected role in actually preventing metastasis. In the MMTV-ras model, MMP-11 deficiency results in a higher number of metastases despite a lower number and volume of primary tumors [30]. Apparently, the transition to invasive carcinoma is greatly accelerated in the MMP-11 null mice, indicative of a protective function of MMP-11. A similar protective role against metastasis has been reported in non-mammary models for MMP-3 [73] and MMP-12 [85]. Thus, while the general MMP inhibitor galardin has a large inhibitory effect on metastasis, several single MMP knock-out studies report no effect or even the opposite effect on metastasis in breast cancer models. This demonstrates the potential of MMP inhibitors in preventing spontaneous metastasis but also underlines the necessity of evaluating a second generation of MMP inhibitors for clinical trials that are more specific than previous compounds. Transgenic models with a well-characterized involvement of MMPs in metastasis could be a useful tool in testing such compounds.
Conclusion and Future Perspectives
Transgenic breast cancer models are invaluable research tools because they recapitulate the entire process from the initial genetic events in normal cells to metastatic disease. Furthermore, the very similar expression patterns of extracellular proteases in human and mouse breast cancer samples suggest that transgenic mouse models are ideally suited to study the role of proteases in carcinogenesis and the progression to invasion and metastasis.
We have only begun to examine gene deficiencies and transgenic overexpression of the various PA and MMP components in transgenic models. The studies that have been performed so far suggest that no single MMP or PA system component is likely to be all-important for any stage in tumor progression. Practically all of the protease intervention studies report partial phenotypes such as delayed carcinogenesis, slower tumor growth or reduced metastasis, if they report any phenotype at all. The absence of any absolute phenotypes, such as prevention of metastasis, suggests that many of the proteases have mutually overlapping functions. The challenge for developing novel therapeutics in the future will be to identify those proteases that can be targeted simultaneously to obtain a synergistic tumor-suppressive effect.
Another area that has so far only been thoroughly examined in one or two transgenic models is the expression patterns of proteases. Using protease array data, it may be possible to draw some more detailed parallels between individual mouse models and certain histopathological subtypes of human breast cancers. It is very possible that the collective of transgenic breast cancer models available, rather than any single transgenic, will be needed to adequately model the heterogenous human disease. Another open question is whether certain proteases or inhibitors are up- or downregulated in response to certain gene deficiencies. This may provide vital information on functional overlap between individual proteases.
Transgenic breast cancer mice may prove to be very reliable models not only for basic research but also for testing experimental anti-proteolytic therapeutics, due to the high degree of similarity with human breast cancer. However, the transgenic models also present some significant challenges. A key issue is that the experimental drug has to cross-react with the mouse version of the protease. Therefore, it may be necessary in some cases to develop two drugs in parallel, one for each species. Due to the extracellular nature of the PA and MMP systems, these represent excellent targets for therapeutic monoclonal antibodies. An elegant method for targeting extracellular proteases in transgenic mice is the development of monoclonal anti-mouse antibodies by immunizing protease-deficient mice with the target protease. In conclusion, transgenic breast cancer models will further the identification of extracellular proteases critical to cancer invasion and metastasis, and aid the development of new agents against the spread of cancer.
Acknowledgments
We are grateful to Drs. Barbara Fingleton and Lynn Matrisian for sharing unpublished results, and to Dr. Fritz Rank for assistance with histopathological evaluation of tumor samples. The assistance of Mr. John Post in creating the artwork is greatly appreciated. This work was supported by grants from the Danish Cancer Research Foundation, the Copenhagen Hospital Corporation, the “Grosserer Alfred Nielsen og hustrus” foundation, the European Commission grant LSHC-CT-2003-503297, and the European Union research training grant for mammary gland biology RTN-2002-00246.
Abbreviations
| CIS | carcinoma in situ |
| DCIS | ductal CIS |
| DMBA | 7,12-dimethylbenzanthracene |
| ECM | extracellular matrix |
| MMP | matrix metalloprotease |
| MMTV | mouse mammary tumor virus long terminal repeat promoter |
| PA system | plasminogen activation system |
| PAI-1 | plasminogen activator inhibitor-1 |
| pKal | plasma kallikrein |
| Plg | plasminogen |
| PymT | polyomavirus middle T antigen |
| SV40-T | simian virus 40 large T antigen |
| TDLU | terminal ductal lobular unit |
| TGF-β | transforming growth factor-β |
| TIMP | tissue inhibitor of metalloproteases |
| tPA | tissue plasminogen activator |
| uPA | urokinase plasminogen activator |
| uPAR | urokinase receptor |
| VEGF | vascular endothelial growth factor |
| WAP | whey acidic protein promoter |
References
Articles from Journal of Mammary Gland Biology and Neoplasia are provided here courtesy of Springer
Full text links
Read article at publisher's site: https://doi.org/10.1007/s10911-007-9040-x
Read article for free, from open access legal sources, via Unpaywall:
https://link.springer.com/content/pdf/10.1007/s10911-007-9040-x.pdf
Citations & impact
Impact metrics
Citations of article over time
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1007/s10911-007-9040-x
Article citations
Plasmin and Plasminogen System in the Tumor Microenvironment: Implications for Cancer Diagnosis, Prognosis, and Therapy.
Cancers (Basel), 13(8):1838, 12 Apr 2021
Cited by: 42 articles | PMID: 33921488 | PMCID: PMC8070608
Review Free full text in Europe PMC
Mammary tumors in Sprague Dawley rats induced by N-ethyl-N-nitrosourea for evaluating terahertz imaging of breast cancer.
J Med Imaging (Bellingham), 8(2):023504, 01 Mar 2021
Cited by: 2 articles | PMID: 33928181 | PMCID: PMC8071784
S100A10 Has a Critical Regulatory Function in Mammary Tumor Growth and Metastasis: Insights Using MMTV-PyMT Oncomice and Clinical Patient Sample Analysis.
Cancers (Basel), 12(12):E3673, 07 Dec 2020
Cited by: 9 articles | PMID: 33297495 | PMCID: PMC7762402
Imaging Findings in Papillary Breast Lesions: An Analysis of Ductal Findings on Magnetic Resonance Imaging and Ultrasound.
J Comput Assist Tomogr, 42(4):542-551, 01 Jul 2018
Cited by: 3 articles | PMID: 29613991
Pulsed Terahertz Reflection Imaging of tumors in a spontaneous model of breast cancer.
Biomed Phys Eng Express, 4(6):065025, 23 Oct 2018
Cited by: 13 articles | PMID: 31275612 | PMCID: PMC6605103
Go to all (28) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Metastasis tumor antigen family proteins during breast cancer progression and metastasis in a reliable mouse model for human breast cancer.
Clin Cancer Res, 12(5):1479-1486, 01 Mar 2006
Cited by: 69 articles | PMID: 16533771
Transgenic expression of human cathepsin B promotes progression and metastasis of polyoma-middle-T-induced breast cancer in mice.
Oncogene, 30(1):54-64, 06 Sep 2010
Cited by: 54 articles | PMID: 20818432
The caM kinase, Pnck, is spatially and temporally regulated during murine mammary gland development and may identify an epithelial cell subtype involved in breast cancer.
Cancer Res, 60(19):5571-5577, 01 Oct 2000
Cited by: 19 articles | PMID: 11034105
WAP-TAg transgenic mice and the study of dysregulated cell survival, proliferation, and mutation during breast carcinogenesis.
Oncogene, 19(8):1010-1019, 01 Feb 2000
Cited by: 31 articles | PMID: 10713684
Review





