Abstract
Free full text

Avian Influenza Virus (H5N1): a Threat to Human Health
Abstract
Pandemic influenza virus has its origins in avian influenza viruses. The highly pathogenic avian influenza virus subtype H5N1 is already panzootic in poultry, with attendant economic consequences. It continues to cross species barriers to infect humans and other mammals, often with fatal outcomes. Therefore, H5N1 virus has rightly received attention as a potential pandemic threat. However, it is noted that the pandemics of 1957 and 1968 did not arise from highly pathogenic influenza viruses, and the next pandemic may well arise from a low-pathogenicity virus. The rationale for particular concern about an H5N1 pandemic is not its inevitability but its potential severity. An H5N1 pandemic is an event of low probability but one of high human health impact and poses a predicament for public health. Here, we review the ecology and evolution of highly pathogenic avian influenza H5N1 viruses, assess the pandemic risk, and address aspects of human H5N1 disease in relation to its epidemiology, clinical presentation, pathogenesis, diagnosis, and management.
INTRODUCTION
The highly pathogenic avian influenza (HPAI) H5N1 virus, which is panzootic in poultry, continues to spread and pose a major challenge to animal and human health (50, 260). Since pandemic influenza virus has its origins in avian influenza viruses (252), HPAI H5N1 virus has to be considered a potentially serious pandemic threat. New influenza virus pandemics in the 21st century are a certainty, but whether H5N1 will be the next pandemic virus is far from certain. What is already true, however, is that H5N1 viruses are taking a huge toll on the poultry industry in many developing countries, and this directly or indirectly impacts both economic and social well-being. The potential impact of HPAI H5N1 virus (and human reaction to its spread) on wildlife and ecology has received less attention but is also worthy of consideration (180).
While the H5N1 virus transmits zoonotically from infected poultry to humans, often with fatal consequences, such transmission remains inefficient. Although the virus replicates efficiently in diseased humans, it has not yet adapted to efficient human-to-human transmission. H5N1 therefore continues to challenge our understanding of interspecies transmission of influenza viruses. Here, we review the biology and ecology of HPAI H5N1 viruses in the broader context of animal and human influenza viruses in general. We discuss options for the control of H5N1 transmission in animals and humans and assess its pandemic risk. We specifically address aspects of human H5N1 disease in relation to its epidemiology, clinical presentation, pathogenesis, diagnosis, and management.
THE VIRUS
Biological Properties
Influenza A viruses are enveloped RNA viruses with an eight-segmented, single-stranded, negative-sense genome belonging to the family Orthomyxoviridae. Influenza virus type A (and type B) causes recurrent epidemics almost every year, leading to significant human morbidity and mortality. However, only influenza A virus is associated with influenza virus pandemics, where an antigenically novel influenza virus emerges to spread rapidly worldwide in an immunologically naïve population. In past pandemics, 20 to 30% of the global population was infected within the first year, and in this regard, influenza A viruses are unique human pathogens. The last century witnessed three such pandemics, in 1918 (the so-called “Spanish flu”), 1957 (“Asian flu”), and 1968 (“Hong Kong flu”). The pandemic of 1918 is believed to have claimed over 40 million lives, while those of 1957 and 1968 are each believed to have led to over 4 and 1 million deaths, respectively (38, 252).
The eight gene segments of influenza A virus encode 10 proteins: hemagglutinin (HA), neuraminidase (NA), matrix proteins M2 and M1, nonstructural (NS) proteins NS1 and NS2, the nucleocapsid, and the three polymerases, the PB1 (polymerase basic 1), PB2, and PA (polymerase acidic) proteins (252). For some influenza viruses, the PB1 gene has recently been discovered to encode an additional protein, the PB1-F2 protein (30). Influenza type A viruses are subtyped based upon the HA and NA antigens, which are surface proteins found on the viral envelope (153). Mutation in these genes is selected for by herd-immune selection pressure in the host, leading to a directional antigenic change over time (“antigenic drift”), thereby explaining the repeated epidemics observed with influenza A or B virus. The segmented genome of influenza viruses also allows for genetic reassortment to occur when two influenza viruses infect the same cell (18, 142). This provides influenza viruses a powerful option for the generation of genetic diversity for interspecies transmission and to evade host immune responses through a major antigenic change (“antigenic shift”). Pandemics arise at infrequent intervals when an influenza virus with a completely novel HA (and sometimes NA) acquires the ability for efficient and sustained human-to-human transmission in a population that is immunologically naïve to the virus surface proteins (HA and NA). The H2N2 influenza virus responsible for the pandemic of 1957 arose through genetic reassortment, where the prevailing human influenza A virus (H1N1) acquired the HA (H2), NA (N2), and PB1 genes from an avian virus (101, 120, 187, 252). Similarly, the pandemic of 1968 arose through the acquisition of a novel HA (H3) and the PB1 gene from an avian source (6, 101). In contrast, the pandemic of 1918 is believed to have arisen through the direct adaptation of a purely avian virus to efficient transmission in humans (226), although the lack of genetic information on relevant avian precursors and on the pre-1918 human viruses precludes a definitive conclusion on this matter (62). Thus, pandemic influenza virus is a zoonosis, and avian viruses play a critical role in its genesis (194). Since the pandemics of 1957 and 1968 arose in southern China, this region has been identified as a hypothetical pandemic epicenter (196).
Ecology of Influenza Viruses
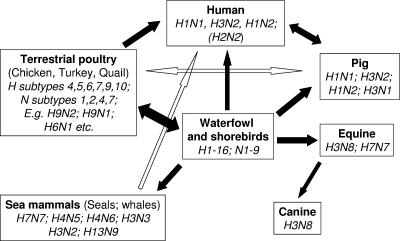
Sixteen subtypes of HA (H1 to H16) and nine subtypes of NA (N1 to N9) are recognized in aquatic birds (53, 252). While many of these subtypes can be consistently detected in wild aquatic waterfowl, only few subtypes have established themselves in mammalian species such as humans (HA [H1, H2, and H3] and NA [N1 and N2]), pigs (HA [H1 and H3] and NA [N1 and N2]), horses (H3N8 and H7N7), and dogs (H3N8) (Fig. (Fig.1).1). Indeed, only some of the diverse influenza virus subtypes found in aquatic birds have established themselves as low-pathogenicity avian influenza (LPAI) virus in terrestrial poultry such as chicken, turkey, and quail (e.g., subtypes H9 and H6) (see below).
Both human and avian influenza viruses have established stable virus lineages in pigs, possibly a reflection of the fact that receptors for both avian and human influenza viruses are present on the porcine epithelium (90). For these reasons, pigs have been regarded as being a possible intermediate host (“mixing vessel”) for the generation of pandemic influenza virus through reassortment (139). Human influenza viruses that have become established in pigs include classical swine H1N1 and H3N2 viruses and reassortants thereof (H1N2 and H3N1) (164, 169, 188, 197). The 1918 H1N1 virus appears to have entered human and pig populations, although the epidemiological evidence favors the initial host as being humans (225). Avian-like H1N1 viruses have established themselves in pigs in Europe (139, 188). In addition, other viruses have been transiently detected in pig populations. These include avian virus subtypes H1N1 (Asia), H4N6 (Canada), H9N2 (China), and H5N1 (Asia) (33, 71, 164, 169).
More recently, equine H3N8 viruses have been transmitted to racing dog populations in the United States, possibly facilitated by the practice of feeding horsemeat to racing dogs, another example of a human intervention that promoted interspecies transmission of viruses (37). Overall, there are strong barriers to interspecies transmission that prevent the adaptation of influenza viruses to new hosts (see below). It is likely that these prevent the more frequent emergence of pandemics from the wide diversity of HA subtypes prevalent in waterfowl.
Highly Pathogenic Avian Influenza Virus
Two subtypes of influenza A virus (H5 and H7) are known to give rise to HPAI virus in terrestrial poultry (chicken and turkeys). The HPAI virus phenotypes of these viruses are related largely, though not exclusively, to mutations giving rise to multiple basic amino acids in the connecting peptide between the HA1 and HA2 domains of the HA0 precursor protein (84, 109). In the viral life cycle, posttranslational cleavage of the precursor HA molecule (HA0) into two subunits (HA1 and HA2) by host proteases is essential for productive virus replication, since this generates a fusogenic domain mediating the fusion between the viral envelope and the endosomal membrane. This may occur extracellularly by trypsin-like proteases that are restricted in tissue distribution to the respiratory and gastrointestinal tracts. However, when multiple basic amino acids are introduced into the HA cleavage site, the HA0 precursor becomes cleavable by a wide range of proteases (e.g., furins [PC6-like]) with ubiquitous tissue distribution (105, 246). This permits productive virus replication in organs outside the respiratory and gastrointestinal tracts, including the brain, resulting in fulminant disseminated disease with high mortality, leading to HPAI virus (84). The acquisition of a carbohydrate side chain near the cleavage site can modulate the pathogenicity of a virus by masking the accessibility of the proteases to the cleavage site (102, 84).
In the 31 years from 1959 to 1990, there were nine HPAI virus outbreaks recorded in Europe, North America, and Australia, and these outbreaks were contained by the “stamping out” of infected flocks (1). In the 11 years since 1990, there have been 10 further HPAI virus outbreaks, including in Asia. The current HPAI H5N1 virus outbreak (from 2003 onwards) is, however, unprecedented in scale and geographic distribution. These viruses are now panzootic across three continents, leading to huge economic losses, and have transmitted to humans with lethal consequences. The expansion of intensive poultry husbandry, which is the fastest growing livestock industry globally, with an estimated 16 billion chickens and 1 billion ducks worldwide, is likely facilitating the increasing frequency and scale of HPAI virus outbreaks. Furthermore, the commercialized large-scale poultry industry is now associated with the movement of live poultry and poultry products over long distances, thereby facilitating the transmission of infection.
On the basis of the genetic sequence of HA and the biological properties of the virus, it appears that the avian influenza viruses that contributed to the origin of the pandemics of 1957 and 1968 were LPAI viruses of chicken and other terrestrial poultry. Therefore, for pandemic preparedness, surveillance of poultry and other avian species must be directed at healthy as well as diseased birds. On the other hand, reconstruction of the H1N1 virus causing the “Spanish flu” pandemic of 1918 suggests that this virus may have had high pathogenicity for terrestrial poultry even though it did not have the multibasic cleavage site in the HA that characterizes HPAI virus (236). However, direct proof of high pathogenicity of the 1918 virus for chickens is still awaited.
BIRD-TO-HUMAN TRANSMISSION OF AVIAN INFLUENZA VIRUSES
Barriers of Interspecies Transmission
Avian influenza viruses do not efficiently infect humans or nonhuman primates (7, 152). Conversely, human viruses do not efficiently replicate in ducks (78). The viral and host factors that determine host restriction are poorly understood (83, 84, 116, 156, 249) and are believed to be determined by multiple viral genetic determinants including the viral HA and NA genes as well as other internal genes such as the nucleoprotein and the PB2 genes.
The HA of human influenza viruses binds to cell sialic acid linked to galactose by an α-2,6 linkage (SA α-2,6) found on human cells, while avian viruses have a predilection for sialic acid linked to galactose by α-2,3 linkages (SA α-2,3) found on avian (e.g., duck) epithelia (181). This receptor specificity was believed to be one of the factors responsible for the species barrier that keeps avian viruses from readily infecting humans. More recently, it has been shown that the epithelial cells of the lower respiratory tract (viz., terminal bronchioles and alveolar epithelial cells) have both SA α-2,3 and SA α-2,6 receptors. Furthermore, fluorescein-labeled virus was shown to bind efficiently to epithelial cells of the terminal bronchioles and alveoli, and avian-like H5N1 viruses were shown to infect and replicate in ex vivo cultures of human lung fragments (159, 192, 243). Although the putative SA α-2,3 receptors for H5N1 viruses appear to be lacking in the upper respiratory tract, H5N1 viruses are able to replicate in ex vivo organ cultures of the upper respiratory tract (159). On the other hand, some H5N1 viruses isolated from humans appear to have acquired mutations in HA associated with a change in affinity from SA α-2,3 and SA α-2,6 receptors (263), although such mutations were not by themselves sufficient for these viruses to be efficiently transmitted from human to human. Thus, the paradigm of SA α-2,3 and SA α-2,6 receptors in explaining the tissue tropism and host restriction of avian influenza viruses probably deserves to be reassessed. Novel technologies such as glycan microarrays are revealing that the situation is indeed complex, with different virus strains binding to novel structures such as sulfated and sialylated glycans in addition to the conventional SA α-2,3 and SA α-2,6 (57, 212, 213). Additional information about the glycans on the surface of host cells combined with data on the predilections of virus binding to these structures are likely to provide new biological insights with regard to interspecies transmission of avian influenza viruses.
A layer of mucin covers the respiratory epithelium, forming a barrier that the virus has to penetrate before it can attach to the cell surface (191). This also plays an important role in host susceptibility and tissue tropism. Mucin is rich in sialic acids that act as decoys, trapping the virus and preventing it from reaching the cell surface (5, 147). By cleaving sialic acids in mucus that would otherwise impede the spread of the virus, NA promotes its spread within the respiratory tract.
The NA of avian influenza viruses has a predilection for the hydrolyzation of the avian SA α-2,3 Gal linkage rather than the mammalian SA α-2,6 linkage. A balance between the activity of HA in virus attachment and NA in virus release needs to be maintained for optimal viral replication (245). Deletions in the stalk of the NA reduces the effective enzymatic activity of the NA (12). The H5N1 viruses that have adapted to terrestrial poultry (e.g., chicken) in Hong Kong in 1997 and more recently (2002 to present) have deletions in the stalk region of NA (127), which perhaps allows the virus' NA activity to balance the weaker interaction of the H5 HA with the viral receptor of chicken compared to that of aquatic birds.
Avian influenza viruses typically have Glu627 in the PB2 gene, while human viruses have Lys627. This mutation may be associated with temperature sensitivity (146) and seems to be involved in host adaptation (217), possibly by playing a role in adaptation to replication and transmission within mammals. The role of PB2 in the pathogenesis of H5N1 viruses is dealt with below (see “Pathogenesis of Human Influenza H5N1 Viruses”). During the emergence of the pandemic viruses of 1957 and 1968, in addition to the novel HA (and also, in 1957, NA), the PB1 gene was also acquired from the avian influenza virus precursor (101). In minireplicon systems investigating the compatibility of avian and human polymerase components, an avian PB1 appeared to provide a replicative advantage in mammalian cells (154). However, in other studies, human virus reassortants carrying avian PB1 appeared to have reduced replication competence (204). Thus, the role of avian PB1 in the emergence of pandemic influenza virus reassortants still remains unclear. The importance of the polymerase complex in the adaptation to new hosts is being increasingly recognized and is discussed further below (55, 184).
Transmission of Avian Influenza Viruses to Humans
The ability of avian influenza A viruses of subtypes H1N1, H3N8, H3N2, H6N2, H6N1, H9N2, H4N8, and H10N7 to replicate in humans was investigated by experimental infection of 81 healthy human volunteers (7). Some volunteers experimentally infected with H4N8, H10N7, or H6N1 virus had evidence of viral replication in the nasopharynx, and some had mild upper respiratory symptoms. None of them had evidence of rising antibody titers using the conventional hemagglutination inhibition (HI) test. Neutralizing antibody responses were not assessed. Attempts to artificially transfer H6N1 from one volunteer to another were unsuccessful. Volunteers infected with avian H1N1, H3N2, H3N8, H6N2, or H9N2 virus had no evidence of virus replication in the nasopharynx, but some of them had serological responses to the infecting virus. It was speculated that natural infections by human viruses of subtypes H1 or H3 and N1 or N2 may have provided cross-reacting immunity that prevented avian virus replication. These findings highlight the fact that avian influenza viruses can infect humans, at least following experimental challenge, and also that conventional HI tests underestimate such infections.
Human sera collected in southern China from the late 1970s to the early 1980s had evidence of antibodies to a number of LPAI virus subtypes (e.g., H4, H5, H6, H7, H10, and H11), as assessed by the single radial hemolysis test (194) (K. F. Shortridge, personal communication). Human seroprevalence apparently correlated with the isolation rates of viruses in ducks, with some exceptions (e.g., H7). The seroprevalence for H5 viruses ranged from 0% (Hong Kong) to 2.3% (Jiangsu Province). It should be noted that this H5 seroprevalence likely reflects exposure to low-pathogenicity H5 viruses present in ducks; it does not provide evidence of continued exposure to the current HPAI H5N1 virus.
Human Disease Caused by Non-H5 Avian Influenza Viruses
Besides H5N1, the direct transmission of avian influenza viruses of subtypes H7N7, H9N2, and H7N3 has been associated with human disease (Table (Table1).1). It is notable that the virus subtypes causing zoonotic human disease have been largely those known to cause infection in terrestrial poultry. It is unclear whether this reflects the increased probability of an exposure event (chickens being more abundant than ducks and human exposure to poultry being more common than exposure to aquatic wild birds) or whether viruses that have adapted to terrestrial poultry have a greater propensity to transmit to humans. Of note, terrestrial poultry such as chicken and quail have SA α-2,6 receptors that bind human influenza viruses (56, 247). This may explain the observation that H9N2 viruses, which are endemic in quail and chickens in Asia, have a predilection to bind to both human SA α-2,6 and avian SA α-2,3 receptors (148). It may also explain why only a smaller subset (e.g., H9 and H6) of the diverse HA subtypes present in aquatic birds has become endemic in terrestrial poultry. It raises the possibility that terrestrial poultry may facilitate the adaptation of avian influenza virus to more efficient binding to the human SA α-2,6 receptors.
TABLE 1.
Human disease caused by interspecies transmission of avian influenza viruses without prior reassortment
| Yr | Antigenic description and interspecies transmission event |
|---|---|
| Pre-1997 | H1N1, 1918 Spanish flu pandemic? |
| H7N7, sporadic conjunctivitis | |
| 1997 | H5N1 in Hong Kong, 18 cases and 6 deaths |
| 1998, 1999, 2003 | H9N2 in Hong Kong and Guangdong |
| 2003 | H5N1 diagnosed in Hong Kong (likely acquired in Fujian Province, People's Republic of China) and in mainland China |
| 2003 | H7N7 in Holland; 78 cases of conjunctivitis, 7 with flu-like illness, 4 others, 1 death |
| 2004 | H7N3 in Canada; conjunctivitis |
| 2004-present | H5N1 disease and death in southeast and east Asia, central Asia, the Middle East, and Africa |
H7N7 virus was isolated from the blood clot of a man with clinical features compatible with a hepatitis-like illness, but the relationship of this isolate to the disease is unclear (22, 42). There are also reports of self-limited conjunctivitis caused by H7N7 viruses after accidental infection in the laboratory, after infection of an animal (seal) handler, and from backyard poultry (4, 119, 227, 253). During the large-scale 2003 outbreak of H7N7 virus in Dutch poultry, active case finding among exposed persons and their close contacts identified a total of 89 laboratory-confirmed infections in humans (112), amounting to approximately 2% of the estimated number of people potentially exposed to the virus. The highest infection rates were observed in veterinarians and persons involved in the culling of chickens. During the same outbreak, human-to-human transmission of H7N7 virus was suggested for three individuals who had not been in direct contact with infected poultry but were family members of poultry workers with symptomatic H7N7 infections (112). Most of these patients (83 of 85) presented with conjunctivitis, while seven patients presented with a febrile flu-like illness (54, 112). Five patients with conjunctivitis also had a flu-like illness. A veterinarian who had visited an affected farm subsequently developed pneumonia complicated by acute respiratory distress syndrome (ARDS) and multiorgan failure and succumbed to his illness (54).
An outbreak of HPAI H7N3 virus in poultry farms in British Columbia, Canada, led to self-limited conjunctivitis and flu-like illness in two people exposed to infected poultry (79, 239). H7N3 virus was isolated from both patients. Poultry workers exposed to poultry affected by LPAI and HPAI virus outbreaks of H7N3 virus in Italy had evidence of H7 seropositivity in 3.8% of those tested (176).
It is notable that H7-subtype influenza viruses have a tropism for the conjunctiva. Viral load was higher in the conjunctival swabs than in respiratory specimens, supporting this contention (54). It was reported that the conjunctiva contains a predominance of SA α-2,3 receptors, which may explain this tropism of the virus (163). Interestingly, other avian viruses (e.g., H5N1), which also have an SA α-2,3 binding preference, do not appear to cause conjunctivitis, although the conjunctiva may conceivably provide a portal of entry for the virus.
Avian (low-pathogenicity) H9N2 viruses have repeatedly infected humans in Hong Kong and in Guangdong, giving rise to a mild flu-like illness (19, 74, 131, 171). These virus strains belonged to the A/Duck/Hong Kong/Y280/97-like or the A/Quail/Hong Kong/G1/97-like virus lineages. Although H9N2 viruses bind human SA α-2,6 receptors (148), no human-to-human transmission was detected.
ECOLOGY OF AVIAN INFLUENZA A VIRUS (H5N1)
Emergence and Spread of Avian Influenza H5N1 Virus
The HPAI H5N1 virus lineage currently endemic in Asia was first detected in diseased geese in Guangdong Province, People's Republic of China, and designated A/Goose/Guangdong/1/96 (262). The H5N1 bird flu incident in Hong Kong in 1997 was the first known instance of a purely avian virus causing severe human disease and death, with 18 human cases, 6 of whom died (36, 218, 266). The slaughter of all (1.5 million) poultry in the farms and markets of Hong Kong aborted this outbreak. This virus (H5N1/97) was in fact a reassortant virus with the HA (H5) being derived from A/Goose/Guangdong/1/96 and the other genes being derived from H9N2 and H6N1 viruses prevalent in quail (72, 82, 262). The viral NA had a deletion in the stalk region of the NA, which is associated with the adaptation of influenza viruses to terrestrial poultry such as chickens. While the H5N1/97 virus was not seen since the poultry slaughter of December 1997, continued surveillance of poultry in Hong Kong revealed the presence of A/Goose/Guangdong/1/96-like viruses in imported geese (68). From 2000 onwards, a series of reassortants were detected in ducks, chicken, and other terrestrial poultry, with the HA being derived from the A/Goose/Guandong/1/96-like lineage but with the internal gene segments being derived from other influenza viruses from birds (Fig. (Fig.2)2) (67, 69). A diversity of genotypes (a genotype is a designation that reflects the constellation of eight gene segments of the virus) was seen in 2001 and 2002, but by 2003, genotype Z began to emerge as a dominant genotype in terrestrial poultry in southern China. It had again acquired a deletion in the stalk region of the NA (not identical but overlapping that observed in H5N1 viruses in Hong Kong in 1997) that characterizes adaptation to terrestrial poultry. HPAI H5N1 virus was also documented in ducks in mainland China since 1999 (26), in Geese in Vietnam during 2001 (158), and in imported duck meat from China in 2001 (138, 238), indicating that these viruses continued to circulate in ducks and geese in the region. In addition, in 2002, HPAI H5N1 virus was documented in dead wild birds in Hong Kong (46, 69). Some of these viruses, especially those of genotype Z, acquired pathogenicity for aquatic birds such as ducks and led to severe neurological disease (46). This was unusual, since even HPAI viruses are usually nonlethal for ducks.
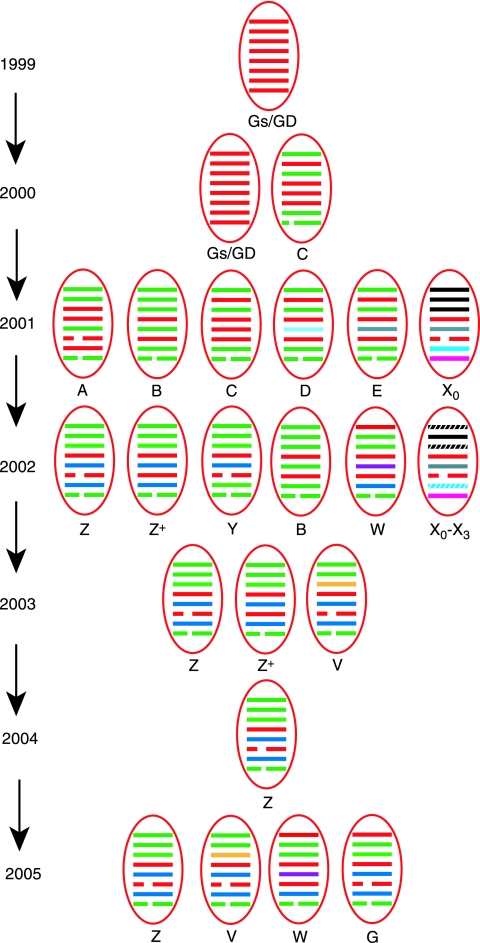
Genetic reassortment and emergence of influenza A virus (H5N1) in Asia from 1999 to 2005. The eight gene segments (represented by horizontal bars) starting from top downwards are PB2, PB1, PA, HA, NP, NA, M, and NS. Each color represents a distinct virus lineage. Red represents the A/Goose/Guangong/1/96-like lineage. Distinct genotypes (i.e., gene constellations) are denoted by a letter. The origin of the 1997 virus in Hong Kong is not represented here but was a separate reassortment event with only the HA being derived from A/Goose/Guangdong/1/96 and the other seven gene segments being derived from H9N2 and H6N1 avian influenza viruses found in quail. (Adapted from reference 127 by permission from Macmillan Publishers Ltd.)
From December 2003 onward, Japan, South Korea, Vietnam, Thailand, Indonesia, mainland China, Cambodia, Laos, and Malaysia reported outbreaks of HPAI H5N1 virus disease (http://gamapserver.who.int/mapLibrary/app/searchResults.aspx) (199). The viruses introduced into Japan and South Korea were genotype V viruses, but those that became dominant in Vietnam, Thailand, Cambodia, Indonesia, and southern China were the Z genotype virus, which first emerged in 2002 and has since become the dominant virus genotype in terrestrial poultry (Fig. (Fig.2)2) (127). In 2004 and early 2005, H5N1 viruses in Asia revealed significant genetic and antigenic heterogeneity (2, 28, 203). Viruses in mainland China were diverse and comprised multiple geographically related sublineages of multiple genotypes (28).
In contrast, viruses found in Vietnam, Thailand, Cambodia, and Malaysia (Z genotype) formed one closely related clade (clade 1), while those found in Indonesia (Z genotype) formed another group of closely related viruses (clade 2.1). This suggested that the viruses responsible for the poultry outbreaks in Indochina on the one hand and in Indonesia on the other were each common-source introductions and that the perpetuation of H5N1 viruses in Indochina and Indonesia, respectively, were until recently maintained within poultry rather than through the repeated reintroduction of viruses from external sources. However, more recently isolated H5N1 viruses from Vietnam suggest that genetically distinct viruses are now being introduced, likely via legal or illegal poultry trade (203).
In May 2005, an outbreak of H5N1 led to the death of over 6,000 migratory waterfowl in Qinghai Lake in western China (27, 29, 134). This is a major breeding site for migratory birds whose flyways extend to India, Siberia, and southeast Asia. The species affected were bar-headed geese (Anser indicus), black-headed gulls (Larus ichthyaetus), brown-headed gulls (Larus brunnicephalus), ruddy shelducks (Tadorna ferruginea), and a limited number of great cormorants (Phalacrocorax carbo). Smaller numbers of whooper swans, black-headed cranes, and pochards were also affected. It is unclear whether the virus was brought to Qinghai by bird migration or whether it was acquired locally from infected poultry. However, this was the first sustained major outbreak within wild bird populations to be documented. Subsequently, H5N1 outbreaks in wild birds or in poultry were reported in Siberia (July 2005), Mongolia and Kazakhstan (August 2005), Romania, Croatia, and Turkey (October 2005). Wild bird infections with or without poultry disease were noted in a number of other Middle Eastern and European countries in 2006. Infection was detected in poultry flocks in Nigeria and India in February 2006. Recurrences of wild bird outbreaks affecting similar bird species occurred in Liaoning and Qinghai, People's Republic of China, in April 2006 (http://www.fao.org/docs/eims/upload//211696/EW_asia_August06.pdf).
Surveillance carried out in six provinces of southern China from July 2005 to June 2006 revealed that the geographically distinct H5 sublineages documented in previous years (see above) (28) had been replaced largely by one dominant sublineage (clade 2.3) (202). Viruses isolated recently from human cases from China also belonged to this same sublineage, as did H5N1 viruses isolated in 2006 from poultry in Malaysia and Laos and from wild birds in Hong Kong. This suggests the emergence and predominance of this sublineage in southern China and southeast Asia (202). Comparable data from other parts of China and Asia are lacking.
By July 2006, 54 countries across three continents had been affected by this H5N1 panzootic virus, and transmission to humans and to other species has been reported in some of these countries (Table (Table2)2) (http://gamapserver.who.int/mapLibrary/app/searchResults.aspx). Over 209 million poultry have died or been culled since January 2004 (50).
TABLE 2.
Cumulative number of confirmed human cases of avian influenza A virus (H5N1) reported to the WHO as of 3 February 2007a
| Country | Date of report of first case | No.
| |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2003
| 2004
| 2005
| 2006
| 2007b
| Totalb
| ||||||||
| Cases | Deaths | Cases | Deaths | Cases | Deaths | Cases | Deaths | Cases | Deaths | Cases | Deaths | ||
| Vietnam | 11 January 2004c | 3 | 3 | 29 | 20 | 61 | 19 | 0 | 0 | 0 | 0 | 93 | 42 |
| Thailand | 23 January 2004 | 0 | 0 | 17 | 12 | 5 | 2 | 3 | 3 | 0 | 0 | 25 | 17 |
| Cambodia | 2 February 2005 | 0 | 0 | 0 | 0 | 4 | 4 | 2 | 2 | 0 | 0 | 6 | 6 |
| Indonesia | 21 July 2005 | 0 | 0 | 0 | 0 | 19 | 12 | 56 | 46 | 6 | 5 | 81 | 63 |
| China | 19 November 2005d | 1 | 1 | 0 | 0 | 8 | 5 | 13 | 8 | 0 | 0 | 22 | 14 |
| Turkey | 5 January 2006 | 0 | 0 | 0 | 0 | 0 | 0 | 12 | 4 | 0 | 0 | 12 | 4 |
| Iraq | 30 January 2006 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 2 | 0 | 0 | 3 | 2 |
| Azerbaijan | 14 March 2006 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 5 | 0 | 0 | 8 | 5 |
| Egypt | 20 March 2006 | 0 | 0 | 0 | 0 | 0 | 0 | 18 | 10 | 1 | 1 | 19 | 11 |
| Djibouti | 12 May 2006 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 |
| Nigeria | 3 February 2007 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 |
| Total | 4 | 4 | 46 | 32 | 97 | 42 | 116 | 80 | 8 | 7 | 271 | 165 | |
Transmission within Poultry and Wild Birds
From 2003 to 2004, those Asian countries that detected the introduction of H5N1 virus infection into their poultry flocks early (e.g., Japan, South Korea, and Malaysia) were successful in rapidly eradicating the infection by aggressive “stamping-out” policies. However, once the virus becomes entrenched, it becomes extremely difficult to eradicate (199, 229). The reasons for this are multiple but include a high prevalence of backyard flocks, mixed chicken and duck rearing, asymptomatic virus shedding in ducks, live-poultry markets, and legal and illegal wildlife trade (141, 86). A high proportion of village households in Asia have backyard poultry, with many of them having chickens and ducks as well as pigs in close proximity (141). Almost 70% of poultry production in Asia is in backyard flocks, where biosecurity is impossible to implement and which is associated with poor access to veterinary services, leading to nonrecognition or delayed recognition of disease outbreaks. The lack of effective compensation schemes for affected flocks may lead to the underreporting of disease.
Live-poultry markets, especially those permanent markets where unsold poultry are held overnight within the market, are known to amplify and maintain avian influenza viruses within them. Virus isolation rates in these live-poultry markets are generally higher than those detected in incoming poultry, and thus, these markets are an ideal site for avian influenza virus surveillance (J. S. M. Peiris and Y. Guan, unpublished data). Once viruses enter such a market with incoming poultry, they continue to circulate and amplify within the poultry market. Virus transmission can be interrupted only by a “rest day,” when the market is completely emptied of poultry (118). Such surveillance studies in southern China have documented significant HPAI H5N1 virus isolation rates from apparently healthy birds, especially in ducks and geese (28, 127). Virus isolation rates increase in the cooler winter months (28, 127). Furthermore, while live-poultry markets are a “dead end” for poultry (which end up being slaughtered), they are not dead ends for virus transmission. There is evidence that in addition to amplifying and perpetuating virus within them, these poultry markets serve as a source of infection of poultry farms via the movement of empty cages and personnel (117). This is perhaps accentuated by the fact that small-holder poultry farmers whose flocks have developed H5N1 disease try to salvage some of their investment by selling the surviving chickens to such poultry markets and slaughterhouses. In village-level studies of disease in backyard flocks, recent purchase of poultry was a risk factor for introduction of disease (244). In summary, the data from Hong Kong and southeast Asia indicate that far from being “dead ends” in the transmission cycle, these live-poultry markets are a key factor in the maintenance of virus in the poultry marketing system. It is unclear whether these markets play a similar role in other Asian countries such as Vietnam and Indonesia. If so, it provides one option for intervention to interrupt virus transmission.
Ducks may be infected with H5N1 HPAI viruses without showing overt signs of illness and continue to shed virus for up to 17 days (86, 214, 215). While replicating within a duck, H5N1 viruses appear to lose virulence for ducks and also undergo an antigenic change, which allows the virus to persist and reinfect in the face of a serological response to the initial virus (86). Although such viruses are less virulent for ducks, they retain virulence for chickens and remain HPAI viruses. In some regions of Asia, ducks are led to graze on harvested rice fields and may be moved large distances over time. Thus, infected free-range ducks may serve as “Trojan horses,” introducing virus into local farms and backyard flocks within unsuspecting villages. Studies in Thailand have demonstrated that an abundance of free-grazing ducks is a risk factor for the persistence and spread of HPAI virus (63, 206).
Other factors that may help to spread HPAI virus include fighting cocks that are moved from place to place, even across country borders, for cockfights. A well-organized trade in poultry, poultry products, and other birds (e.g., pet birds) within countries and also (often illegally) across borders promotes the dissemination of the virus. Birds exported as a part of the extensive trade in pet birds have also been occasionally found to be infected with HPAI H5N1 virus (199, 242). Religious practices that foster large-scale bird release in some Asian countries have led to a major trade in passerine birds (R. T. Corlett, personal communication), and this may provide an additional route for the spread of avian influenza viruses. Furthermore, poultry feces are often used as fertilizer or for feeding fish, and their movement provides an opportunity for the dissemination of infection. Vaccination of poultry without adequate safeguards (e.g., unvaccinated sentinels and serological surveillance to differentiate infected from vaccinated birds) (23, 221) to detect low-level virus circulation within poultry flocks may itself contribute to increasing the likelihood of the silent spread of H5N1 in vaccinated poultry (186).
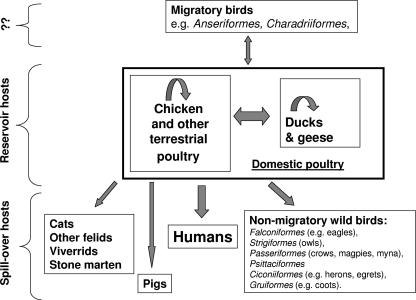
A range of influenza viruses are endemic in wild birds, particularly aquatic waterfowl. In past HPAI virus outbreaks in poultry, it was believed that a precursor low-pathogenicity H5- or H7-subtype virus was introduced into domestic poultry flocks and thereby acquired mutations in the HA connecting peptide that conferred high pathogenicity for poultry (91). Since 2002, a range of feral bird species has been affected by HPAI H5N1 virus (46, 113, 145). What remained unclear until the Qinghai Lake outbreak in 2005 (see above) (29) was whether the HPAI H5N1 virus can maintain transmission within such wild bird and migrating bird populations.
In contrast to the great genetic diversity of H5N1 viruses in China and other parts of Asia (28), those viruses causing disease in wild birds or poultry in Mongolia, Siberia, Iraq, Turkey, Central Europe, Germany, Italy, Nigeria, Egypt, and India all were phylogenetically closely related to each other and to the Qinghai-like lineage (clade 2.2) of viruses (45, 168, 251). Given the great genetic diversity of H5N1 viruses in Asia (28), it is striking that only a narrow spectrum of this genetic diversity (i.e., the Qinghai-like clade 2.2) has contributed to the recent spread westward to Europe and southward to India (45, 168, 251). Among 390 H5N1 viruses isolated during prospective surveillance of poultry markets in six provinces in southern China carried out from July 2005 to June 2006, only one Qinghai-like (clade 2.2) virus was identified (202), although data from other parts of China are lacking. If the movement of poultry or poultry products was responsible for introducing H5N1 into these diverse central Asian, European, African, and Indian locations, it is difficult to explain why only one sublineage was responsible for this rapid expansion in geographic extent and why it happens to be the same sublineage responsible for the largest outbreak of disease in wild birds in Qinghai Lake.
It should be noted that the bird species that manifest mortality may not necessarily be the species that carry the virus over long distances. While the movement of poultry and poultry products cannot be completely excluded as contributing to this recent spread of the H5N1 virus, the genetic evidence, taken together with the epidemiological evidence, is suggestive that this geographic expansion of the virus in 2005 was contributed to largely by bird migration likely amplified by local or regional movement of poultry products. An integrated analysis of phylogenetics, migratory bird movements, and poultry trade has suggested that the movement of poultry and poultry products may have been the dominant vector in the outbreak of H5N1 infection during 2003 and 2004 in Asia and its continued endemicity but that migrating birds appear likely to be implicated in the westward spread of the virus to Europe and the Middle East from 2003 to 2006 (107).
It is still unclear, however, whether wild migrating birds now provide a reservoir for HPAI H5N1 virus (50). This distinction is fundamental for control strategies. If wild birds invariably acquire the virus from infected poultry, this implies that the control of poultry infection will lead to the eradication of the virus. If, on the other hand, wild birds are one reservoir for HPAI H5N1 virus, even the eradication of poultry infection will not lead to the eradication of this pathogenic virus, and it will continue to seed new poultry outbreaks. The reemergence of H5N1 in Europe (Hungary) in January 2007 and the preliminary reports that the virus in Hungary has high genetic homology to those found in Europe in early 2006 may indicate that the Qinghai-like clade 2.2 viruses may indeed have become entrenched in wild bird populations. (http://www.promedmail.org/pls/promed/ [archive no. 20070130.0389]). However, a more detailed analysis is awaited. The bird species found to be infected with H5N1 have been summarized (107, 180).
The recently isolated H5N1 viruses have shown the ability to cross species barriers and infect a range of mammalian species including humans. Tigers, leopards, and cats have been infected by H5N1 virus by feeding on infected poultry or bird carcasses (103, 205, 265). Owsten's civets were infected in an animal rescue center in Vietnam, although these animals were not fed infected poultry products (180). In these instances, virus disseminated to involve multiple organs including the brain. There is serological evidence of occasional infection of pigs by H5N1 virus, although the virus does not appear to have become endemic in pigs (33). Experimental inoculation of pigs has led to infection but has not led to the transmission of infection from pig to pig (33, 89). Overall, the possible role of mammals as intermediate hosts in the transmission of H5N1 virus to humans is still poorly explored (115). This is particularly relevant since some patients with H5N1 disease have no obvious exposure to poultry (97, 151). Evidence of subclinical infection of cats exposed to infected birds (126) and reports of cats dying of H5N1 disease in a household in Iraq affected by poultry deaths (265) highlight the possibility that such secondary vectors may be potentially important as a source of infection of humans. Current knowledge of the ecology of the current H5N1 outbreak is summarized in Fig. Fig.33.
INFLUENZA H5N1 VIRUS IN HUMANS
Transmission and Epidemiology
The first human disease caused by H5N1 was reported in Hong Kong in 1997, with 18 cases and six deaths (see above) (36, 218, 266). The source of human infection appeared to be live-poultry markets where chickens, ducks, geese, and other species of minor poultry (e.g., quail, pheasant, chukka, pigeon, etc.) were sold for human consumption (151, 195). In February 2003, as the world was girding itself to confront severe acute respiratory syndrome, H5N1 disease was diagnosed in Hong Kong in a father and son who had just returned from a holiday in Fujian Province, People's Republic of China (170). These two patients were infected by a genotype Z virus, except that it did not have a deletion in the stalk region of the NA (designated genotype Z+) (69). This virus had an amino acid replacement at position 227 (H3 numbering) in the receptor binding pocket of the HA that changed its receptor binding profile to recognize both the avian SA α-2,3 as well as the human SA α-2,6 receptors (193). However, by itself, this did not appear to change its capacity for human-to-human transmission. In retrospect, another case of H5N1 occurred in Beijing, People's Republic of China, in November 2003 (268). Subsequently, with the increasing spread of H5N1 disease in poultry, further human cases from Vietnam, Thailand, Cambodia, Indonesia, and elsewhere were reported (Table (Table2).2). In a number of instances, the detection of a human case in a region was the first indication of the presence of poultry infection in that locality. Taken together, the human cases appear to increase in the winter and spring months (260). This correlates with the seasonality observed in virus detection in poultry (28, 127).
Since HPAI H5N1 virus in poultry is associated with the presence of infectious virus in many organs, as well as the excretion of large amounts of virus in the feces and other secretions, sick poultry are a major source of human infection (138, 222). Most human cases of H5N1 infection were associated with the direct handling of infected poultry, slaughtering or preparing sick poultry for consumption, consumption of uncooked poultry products such as raw blood, or close contact with live poultry (8, 34, 44, 151, 232, 259). Since H5N1 infection may not always be overtly symptomatic, especially so in ducks, even asymptomatic poultry may pose an infection risk, e.g., at wet markets, in areas of endemicity (127, 215). Contact with a contaminated environment, such as water and poultry feces used as fertilizer or fish feed, has been suspected to be a source of infection in human H5N1 cases who had no direct exposure to poultry (39, 97). In bird-to-human transmission, the likely portal of virus entry is via the respiratory tract, the gastrointestinal tract, or the conjunctiva. Cats experimentally infected with H5N1 virus after feeding on infected chickens showed evidence of viral replication in gastrointestinal plexi. However, this is not seen in those infected via the respiratory route (179). In humans, the possibility of intestinal infection is supported by reports of H5N1-infected patients who presented with diarrhea as the only initial symptom as well as by patients who reported consumption of raw duck blood as the sole exposure to poultry (3, 8, 39). In addition, the presence of infectious virus in fecal material may indicate virus replication in the human gastrointestinal tract (39, 40, 240).
There are a number of enigmas with regard to human H5N1 infection and disease. In spite of large-scale outbreaks of H5N1 viruses among poultry in densely populated areas and presumably massive exposure of humans to the virus, the number of reported H5N1 patients has so far been relatively small (244). In Hong Kong in 1997, where there was excellent surveillance for symptomatic influenza virus, there were still only small numbers of cases in spite of the exceedingly heavy virus load in retail poultry markets, where 20% of poultry were infected (195). Seroepidemiological studies following the 1997 H5N1 outbreak in Hong Kong have shown that mildly symptomatic or asymptomatic infections had occurred in a few individuals exposed to infected patients or poultry (15, 16, 98). Similar studies of persons at risk for H5N1 exposure during the recent H5N1 outbreaks have shown little or no evidence of human-to-human transmission in unprotected health care workers exposed to H5N1 patients (129, 189). Similarly, villagers, poultry workers, and poultry cullers in Vietnam, Thailand, Indonesia, and Cambodia who are heavily exposed to infected poultry rarely have clinical or asymptomatic (serological) evidence of infection (244). In contrast, around 10% of poultry stall holders in Hong Kong in 1997 had serological evidence of H5N1 infection without presenting as overt H5N1 disease (15), although it is unclear whether the seropositivity represented recent infection with HPAI H5N1 virus or prior infection by LPAI H5-subtype viruses known to be present in ducks. Although more serosurveillance data are needed to address the possibility that the number of actual cases may be underestimated, the observations so far suggest the inefficient transmission of current H5N1 viruses from infected poultry to humans. Therefore, the question is not why humans get infected with H5N1 disease but why so many who are heavily exposed to the virus in areas where the virus is endemic fail to be infected, symptomatically or asymptomatically, by a virus that seems to be ubiquitous (244). Conversely, while the affected cases in Hong Kong in 1997 had significantly more exposure to live-poultry markets, approximately 30% of them had no obvious source of infection (151). Similar observations were made elsewhere (97).
Among the human H5N1 cases, there is a significant number of family clusters (8, 97, 165, 259). It is difficult to ascertain whether these clusters represent infection from a common environmental source or limited human-to-human transmission. Excluding a common source of infections is epidemiologically exceedingly difficult, and only unusual circumstances allow unequivocal proof of this (241). The lower case incidence and lower case fatality rates for H5N1 in those over 40 years of age remain unexplained (see above). Taken overall, it appears that while exposure to a source of H5N1 infection is necessary, such exposure alone is not sufficient to explain the observed epidemiology of H5N1 disease. Other as-yet-undetermined factors appear to be crucial in determining who gets infected and ill. Among other possibilities, the role of host genetic susceptibility factors and hitherto-unrecognized host resistance mechanisms (185) deserve investigation.
The Clinical Spectrum of Human H5N1 Infections
The age of cases ranged from 3 months to 75 years, with a median age of 18 years (260). The first symptoms of influenza H5N1 virus develop 2 to 4 days after the last exposure to sick poultry, but longer incubation times of up to 8 days have been reported. It is unknown whether and to what extent virus is shed during this time (8, 34, 97, 166, 232, 266). Most patients with influenza H5N1 virus present with symptoms of fever, cough, and shortness of breath and radiological evidence of pneumonia (8, 34, 232, 266). Abnormalities on chest radiographs are often bilateral and include diffuse, patchy, or interstitial infiltrates and segmental or lobular consolidation with air bronchograms. The pneumonia usually seems to be of primary viral origin with no evidence of bacterial superinfection in most cases. This is supported by postmortem examinations of a small number of patients (170, 230, 240). The propensity of current H5N1 viruses to cause lower respiratory tract infections is in accord with the presence of avian-type SA α-2,3 Gal receptors to which avian viruses can bind in human bronchiolar and alveolar cells (192, 243). Unlike human infections with H7 viruses, conjunctivitis or upper respiratory symptoms do not seem to be prominent in H5N1-infected patients (34, 232, 266). Frequently occurring nonrespiratory symptoms include diarrhea, vomiting, and abdominal pain. In some reported cases, diarrhea was the presenting symptom, preceding other clinical manifestations (3, 39).
Central nervous system (CNS) involvement in H5N1 influenza virus infection has been observed for one patient whose illness was characterized by diarrhea, convulsions, and progressive coma and from whom H5N1 virus was isolated from cerebrospinal fluid and blood specimens (39). This patient's sister had also died of an undiagnosed illness of a similar nature 2 weeks earlier, and this may suggest a possible genetic predisposition to this particular disease manifestation (39). Although neurotropism of current H5N1 viruses has been noted in mammals such as mice, ferrets, and felids (103, 133, 180, 224), CNS manifestations in human H5N1 disease seem to be rare. It has been noted that seasonal influenza virus may also rarely lead to CNS disease (150, 219). Fatal H5N1 disease has been reported during pregnancy, but it is unclear (so far) whether transmission to the fetus has also occurred (198).
It should be noted that milder cases of H5N1 disease presenting as uncomplicated flu-like illness were reported in Hong Kong in 1997 (266) and in more recent outbreaks following epidemiological investigations of index cases (97). Overall, in the recent outbreaks, it is unclear whether the milder spectrum of human H5N1 disease is being missed through a lack of adequate surveillance and diagnostic testing of mild cases.
The clinical course of influenza H5N1 virus is often characterized by a rapid progression of lower respiratory tract disease, necessitating mechanical ventilation within days of admission to a hospital (8, 34, 232, 266). The median duration from the time of onset to hospitalization was 4 days, and that from the time of onset to death for the fatal cases was 9 days (260). Progression to respiratory failure is frequently associated with manifestations of ARDS. Other reported complications include multiorgan failure with renal and cardiac dysfunction, Reye's syndrome, pneumothorax, pulmonary hemorrhage, and ventilator-associated pneumonia (8, 34, 232, 266).
Laboratory results characteristically seen in severe cases of H5N1 disease include lymphopenia, often with an inverted ratio of CD4-positive lymphocytes to CD8-positive lymphocytes, thrombocytopenia and increased serum levels of liver transaminases, and, in some cases, hypoalbuminemia and elevation of lactate dehydrogenase and creatine kinase levels (8, 34, 97, 166, 232, 266). High serum levels of cytokines and chemokines have been observed in several H5N1-infected patients, suggesting a role of cytokine dysregulation in the pathogenesis of H5N1 disease (see below) (40, 170, 230). In most cases, the immediate cause of death was respiratory failure.
Epidemiological analysis of the 256 confirmed H5N1 cases reported to the WHO between November 2003 and November 2006 (260) revealed that over half of all cases occurred under in patients under the age of 20 years, and 89% of the patients were under 40 years of age. This skew in age distribution is not explainable by the population-age structure of the affected countries (201). Based on reported cases, the mortality of human influenza H5N1 virus was 60% (260). While this case fatality rate may be exaggerated because of biased case detection, it seems to be clear that the severity of human H5N1 disease is very different from that caused by seasonal influenza viruses. In contrast to human influenza virus, case fatality rates of H5N1 disease were highest in the 10- to 19-year age group (76%) and lowest in those over 50 years (40%), although the number of cases in the age group of 50 years or over was small (n = 15) (260). This unusual age distribution of case incidence and case fatality may reflect age-related patterns of exposure or risk behavior (e.g., close contact with sick poultry) or age-related host resistance.
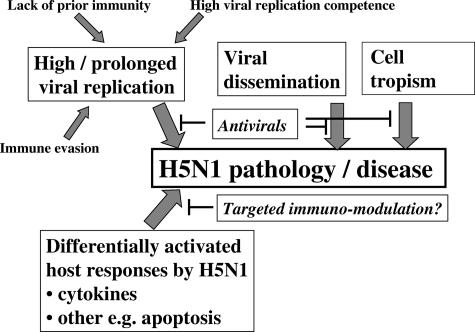
Pathogenesis of Human Influenza H5N1 Virus
Human H5N1 disease is clinically and pathologically distinct from seasonal human influenza virus caused by H3N2 or H1N1 viruses (see above). An understanding of the pathogenesis of human H5N1 disease may derive from three sources: the clinical findings, virology, and pathology of human H5N1 disease; relevant animal models; and studies of cell-virus interactions in vitro or ex vivo. While viral dissemination may contribute to the unusual disease presentation, the primary pathology that contributes to death in most patients is the rapidly progressing fulminant primary viral pneumonia that often progresses to ARDS. The target cells for H5N1 replication in the respiratory tract are not fully defined, but alveolar pneumocytes and macrophages have been identified by immunohistochemistry in autopsies (240), virus binding studies (243), and ex vivo infection of lung fragment cultures (159). Since both H5N1 and human H1N1 influenza viruses can replicate in the alveolar epithelium as well as the nasopharyngeal epithelium (159), a differential tropism of H5N1 virus within the respiratory tract is unlikely to be a key explanation for the unusual pathogenicity of H5N1 viruses.
Human H5N1 disease differs from that of human influenza virus in terms of the viral load kinetics, virus dissemination beyond the respiratory tract, and induction of hypercytokinemia (40). The clinical manifestations of influenza H5N1 virus including diarrhea, liver, and renal dysfunction, severe lymphopenia, and reactive hemophagocytosis suggest pathology in multiple organs. This may suggest a wider tissue tropism of the virus or may be the manifestations of multiple-organ dysfunction that is related to the systemic effects of a severe “sepsis-like” syndrome. For example, it has been reported that Kuppfer cell-dependent hepatitis is not uncommon in “conventional” human influenza virus in the absence of virus infection in the liver (172).
Compared to human influenza virus, patients with H5N1 disease have detectable viral RNA in the respiratory tract for a longer period, presumably because of the lack of prior cross-reactive immunity (40, 96). Higher levels of viral RNA in the nasopharynx and detection of viral RNA in the serum were adverse prognostic factors (40). Virus has been isolated from the plasma, indicating the potential for systemic dissemination (35, 40). The demonstration of H5N1 RNA in feces from patients and in limited autopsy studies, together with the prominent diarrheal presentation of some patients with H5N1 disease, suggests that the virus very likely affects the gastrointestinal tract either as part of the initial infection or through subsequent dissemination (8, 40, 240). While the limited postmortem examinations reported so far revealed no evidence of viral replication or viral pathology in organs other than lungs and intestines (170, 230, 240), more studies, especially during the acute stage of infection, are essential to confirm or exclude the possibility of infection at sites other than the respiratory and gastrointestinal tracts.
While the mechanisms of pathogenesis of HPAI viruses such as H5N1 virus infection in chicken are well defined and are determined largely by the multibasic amino acids in the HA connecting peptide (see above) and the consequent broad tissue tropism of the virus, these findings cannot be directly extrapolated to mammals or to human disease. H5N1 viruses infect BALB/c mice without prior adaptation. Virulence of H5N1 viruses in mice, ferrets, felids, and viverrids (Owsten's civets) is associated with virus dissemination beyond the respiratory tract to involve multiple organs including the brain (26, 58, 66, 76, 99, 100, 179, 180). However, primates experimentally infected with H5N1 virus do not manifest virus dissemination, and pathology is restricted to the respiratory tract (177, 178). Animal models differ among each other and from humans with regard to the attachment of H5N1 virus to respiratory tissues. Fluorescently labeled H5N1 viruses bound more efficiently to the alveolar epithelium than tracheal epithelium in humans, ferrets, cats, and macaques, but the reverse was true in mice. Furthermore, while H5N1 virus attached to type 2 pneumocytes in human, cat, and ferret lungs, the virus bound predominantly to type 1 pneumocytes in macaques (243). Therefore, while mice are a convenient animal model for some purposes (e.g., vaccine-induced protection from virus challenge), the pathogenesis of H5N1 disease in mice probably differs from that in humans in important ways.
Virus virulence and dissemination in the BALB/c mouse model is determined by the amino acid replacements in the PB2 gene at position 627 (Lys) or 701 (Asn) and the presence of a multibasic amino acid motif in the HA connecting peptide (76, 128). H5N1 viruses also exhibit various levels of virulence in ferrets (66, 143, 144, 269), although this variation is not determined predominantly by PB2 Lys627 or the HA connecting peptide (66, 144). Some virus isolates from human H5N1 disease in Vietnam had the mutation PB2 Lys627, but no avian isolates in Vietnam examined so far did so (203). However, this mutation does not appear to correlate with clinical outcome in humans (40). Conversely, while avian H5N1 viruses of the Qinghai-like lineage have PB2 Lys627 (29), human infections with these viruses do not appear to be necessarily more virulent for humans (166). Interestingly, the same change (PB2 Lys627) was also found in an H7N7 virus isolated from an infected human who died of pneumonia during an HPAI virus outbreak in poultry in The Netherlands in 2003, while viruses isolated from mild human cases and from infected chickens contained Glu627 in PB2 (54). As the majority of avian viruses have PB2 Glu627 (the exception being the Qinghai lineage), it is conceivable that the PB2 Lys627 mutation may be one adaptation of the virus to the mammalian host. However, recent studies suggest that other amino acid changes in PB2, as well as changes in the other two subunits of the polymerase complex, PB1 and PA, also play a role in mammalian adaptation and virulence of HPAI viruses (55, 128, 184). Interestingly, the virulence of the reconstructed 1918 Spanish flu was also dependent on the whole polymerase gene complex rather than on individual mutations (235) and was attributed to enhanced virus replication competence. However, the replication competence of HPAI H5N1 viruses was comparable to that of human H1N1 viruses in primary human respiratory epithelial cells and macrophages (25, 32).
Occasionally, patients have presented with encephalitic disease, with evidence of virus isolation from the cerebrospinal fluid clearly demonstrating dissemination to the CNS (see above) (39). The question of whether H5N1 virus is neurotropic in humans is of fundamental importance in the choice of relevant animal models to investigate drug treatment and also to study pathogenesis. However, the majority of patients do not have encephalitic manifestations as a major component of their illness.
Patients with H5N1 disease have higher serum levels of proinflammatory cytokines and chemokines. Levels of macrophage attractant chemokines CXCL10 (IP-10), CXCL9 (Mig), and CCL-2 (monocyte chemoattractant protein 1) and of neutrophil attractant interleukin-8 (IL-8) were elevated to higher levels in plasma of patients with H5N1 disease than in plasma of patients with conventional human influenza virus and were significantly higher in H5N1 patients who died than in those who recovered (40, 170). IL-8 is believed to play a role in the development of ARDS (94). Furthermore, IL-10, IL-6, and gamma interferon levels were also more elevated in H5N1 disease (40). Gamma interferon is known to be a strong inducer of CXCL10 and CXCL9. The elevation of plasma cytokine levels was positively correlated with pharyngeal viral load (40) and may simply reflect more extensive viral replication and consequent direct viral pathology rather than being causative of the pathology observed in H5N1-infected patients. It is notable, however, that the gene expression profiles induced in primary human macrophages and primary human respiratory epithelial cells infected in vitro by comparable infecting doses of H5N1 and “human influenza” H1N1 (or H3N2) viruses are remarkably different. Compared with human H1N1 or H3N2 virus, it was found that H5N1 viruses hyperinduce a range of cytokines including tumor necrosis factor alpha, alpha and beta interferon, IL-1β, CCL2, CCL3, CCL4, CCL5, and CXCL10 from macrophages (32, 69). Similarly, H5N1 viruses differentially hyperinduced CXCL10, IL-8, IL-6, CCL2, beta interferon, and CCL5 from primary lung pneumocytes (25). Thus, many of the cytokines that were found to be elevated in the sera of patients with H5N1 disease were differentially up-regulated by the H5N1 virus in vitro, suggesting that the increased levels of cytokines in peripheral blood of patients with H5N1 disease may be mediated by the ability of H5N1 viruses to hyperinduce cytokine cascades. Thus, the elevated levels of cytokines and chemokines in human H5N1 disease may be a cause rather than a consequence of the severe pathology.
The NS1 protein is an NS protein that is known to play a role in modulating the host innate immune responses (59). While the H5N1-mediated cytokine hyperinduction in macrophages was mediated partly by the H5N1 virus NS gene segment (32), other gene segments also play an important role (J. S. M. Peiris, unpublished data). Studies in vivo of mice infected with a recombinant H1N1 virus possessing the 1997 H5N1 NS gene caused a cytokine imbalance in the lungs characterized by increased concentrations of proinflammatory cytokines and decreased levels of anti-inflammatory cytokines (132). In human influenza virus, the NS1 gene or its product contributes to viral virulence by allowing the virus to evade activating an interferon response in the host (59, 60, 114). Recombinant H1N1 viruses containing the NS gene of 1997 H5N1 viruses were more pathogenic in pigs, possibly by escaping the antiviral effects of interferons and tumor necrosis factor alpha (190). This enhanced virulence in pigs required the presence of glutamic acid instead of aspartate at position 92 (Glu92) of the H5N1 NS gene, but this amino acid change has not been found in recently discovered H5N1 viruses isolated from humans (2, 127, 203). In addition, the postsynaptic density protein-95, disc-large tumor suppressor protein, zonula occludes-1 (PDZ) ligand motif found in carboxy terminus of the NS1 of avian influenza virus has been identified as a potential virus virulence factor (162). The PDZ ligand binding motifs of NS1 of highly pathogenic H5N1 viruses isolated in 1997 and 2003 as well as the 1918 pandemic virus (all of avian origin) are able to bind cellular PDZ-containing proteins. However, NS1 of most low-pathogenicity human influenza viruses contain no such binding properties. Binding of viral NS1 to PDZ domain-containing proteins may disrupt PDZ domain protein-protein interactions and affect cell pathways including those that regulate cell signaling, protein trafficking, and maintaining cell polarity and organization.
Autopsy studies revealed that patients dying of H5N1 disease had massive macrophage infiltrates in the lung, which can be explained by the induction of macrophage-tropic chemokines (see above). Furthermore, those patients had evidence of reactive hemophagocytic syndrome, which is believed to be a cytokine-driven condition (170, 230).
The severe lymphopenia observed in patients and in animal models with H5N1 infection may be secondary to virus-induced apoptosis, as suggested by in vitro and murine experiments with H5N1 viruses (237, 267). Macrophages infected in vitro with H5N1 viruses differentially hyperinduce tumor necrosis factor-related apoptosis-inducing ligand and cause the apoptosis of cocultured lymphocytic cell lines (267). An alternative explanation for H5N1-associated lymphopenia may be the suppression of hematopoiesis in the bone marrow.
It is interesting that, in comparison to contemporary human H1N1 viruses, the reconstructed 1918 pandemic H1N1 virus was also reported to differentially activate host gene expression profiles in lungs of experimentally infected mice (223) and macaques (110). As with H5N1 viruses, the pathways differentially hyperinduced by the 1918 H1N1 virus in mouse lung were those associated with cytokine induction and apoptosis. This is particularly relevant because the clinical features of human H5N1 disease shares some features with the 1918 H1N1 pandemic, viz., a rapidly progressive primary viral pneumonia (in some cases, at least) and a higher case fatality rate in healthy adolescents and young adults. On the other hand, the gene expression profile of the 1918 H1N1-infected macaques indicated a reduced sensitivity to type I interferons (110).
In summary, the pathogenesis of avian influenza H5N1 viruses is likely to be multifactorial in nature, involving increased viral replication competence, viral dissemination, differences in tissue tropism, and differential gene expression responses in infected host cells (Fig. (Fig.4).4). While some of these mechanisms can be blocked by efficient antiviral therapy, a better understanding of the mechanisms underlying differential activation of host genes (123) may permit specifically directed immunomodulation to contribute to therapy of this disease.
Laboratory Diagnosis
This section addresses issues pertaining to laboratory diagnosis of human H5N1 disease and does not cover veterinary diagnosis. In view of the nonspecific nature of the illness, laboratory confirmation of H5N1 influenza virus is essential. Laboratory confirmation of a diagnosis of H5N1 disease is, however, challenging. It requires a high index of suspicion and the most sensitive detection methods available (e.g., reverse transcriptase PCR [RT-PCR]) and may require the testing of multiple specimens (97, 166). The options for diagnosing influenza virus in clinical specimens include virus culture, antigen detection, detection of viral nucleic acids by RT-PCR, and detection of rising titers of antibodies. In the absence of epidemiological links to areas with H5N1 influenza virus activity, further subtyping is not essential for routine diagnostics. However, in countries where avian influenza H5N1 virus is known to be active, patients with severe pneumonia of unexplained etiology should be investigated virologically for influenza virus and, if positive, further investigated using H5-subtype-specific assays so that appropriate therapy, infection control measures, and timely epidemiological investigations can be initiated. Therefore, there is a need for rapid diagnostic assays which distinguish influenza virus subtypes.
Clinical specimens for virus detection.
Virus has been isolated and viral RNA has been detected in respiratory specimens obtained from H5N1-infected patients for up to 16 days after the onset of illness, indicating that virus is shed and can be detected for prolonged periods (8). Nasopharyngeal aspirates (NPA) and nasopharyngeal, throat, and nose swabs have all been used for the detection of H5N1 virus, but it remains unclear which is the diagnostic specimen of choice, because parallel studies comparing different diagnostic specimens are limited. Nasal and pharyngeal swabs have been tested in parallel during recent outbreaks in southeast Asia, and this comparison suggests higher virus loads and consequent higher diagnostic yields in throat swabs than in nose swabs (8, 40, 97). NPA were successfully used for H5N1 diagnosis in Hong Kong during the H5N1 outbreak in 1997 (266), but data directly comparing diagnostic yields from NPA and pharyngeal swabs with other respiratory specimens are lacking. An advantage of NPA is that it provides the ideal specimen for the rapid diagnosis of many other respiratory virus infections (e.g., human influenza A or B virus, adenovirus, and parainfluenza virus), which may help to exclude a diagnosis of H5N1 influenza virus, although dual infections with other respiratory viruses remain a possibility. Limited data suggest that viral load is higher in the lower respiratory tract (e.g., endotracheal aspirates) than in throat or nose swabs (40). Thus, where available, endotracheal aspirates or bronchoalveolar lavages are likely to represent the optimal diagnostic specimens for the diagnosis of H5N1 disease.
H5N1 virus has also been isolated and viral RNA has been detected in feces and sera in some but not all H5N1 patients tested and in the cerebrospinal fluid of one patient (8, 39, 40, 240). However, for screening purposes, respiratory specimens remain the first choice. In H7N7-infected patients, conjunctival swabs appeared to be the specimen of choice for virus detection (54). However, there appears to be a significant difference in the tropisms of H7- and H5-subtype viruses for the human conjunctiva, with conjunctivitis being a common manifestation in H7N7 infections but not in H5N1 infection (see above). There is no systematic data on the utility (or lack thereof) of conjunctival swab specimens for the diagnosis of human H5N1 disease. Autopsy specimens are critical for confirming or excluding avian H5N1 influenza virus disease. If a full autopsy is not possible, paramortem biopsies are alternative options.
Specimens should be transported on ice and tested fresh upon receipt in the laboratory. For long-term storage of specimens for virus detection or isolation, they should be frozen at −70°C, ideally in multiple aliquots. Respiratory specimens should be placed into virus transport medium. WHO guidelines for specimen collection and laboratory testing for H5N1 diagnosis are available (see http://www.who.int/csr/disease/avian_influenza/guidelines/labtests/en/index.html).
Virus isolation.
H5N1 viruses can be isolated by inoculation of embryonated eggs or of Mardin-Darby canine kidney (MDCK) or other permissive cell lines. While culture of seasonal human influenza A viruses requires the addition of exogenous trypsin for growth in MDCK cells, H5N1 virus and other HPAI viruses are not dependent on exogenous trypsin supplements for growth. Virus culture still represents the “gold standard” for diagnosis, and virus isolates are essential for further genetic and antigenic characterization of avian influenza viruses. However, because of the length of time required for virus culture and the need for biosafety level 3 (BSL-3) laboratory facilities for culturing HPAI viruses, RT-PCR rather than virus isolation is usually the first diagnostic test applied to suspected clinical specimens.
Antigen detection.
Detection of viral antigens in clinical specimens by direct immunofluorescence and enzyme immunoassay (EIA) is widely used for the diagnosis of human influenza virus because of their rapidity. Presently, such testing is directed at conserved viral antigens (e.g., nucleoprotein and matrix protein) and does not differentiate human from avian influenza virus subtypes. The EIA-based methods are simple and convenient to use and could theoretically be applicable as point-of-care tests. Commercially available antigen detection EIA test kits have comparable analytical sensitivities for human and avian influenza viruses, but their overall sensitivity was >1,000-fold lower than that for virus isolation (24). Thus, currently, viral antigen detection tests, while having acceptable clinical sensitivity for the diagnosis of human influenza viruses, appear to have low clinical sensitivity for the diagnosis of avian influenza H5N1 virus (8, 97, 166, 170, 266). Aside from this apparently poor clinical sensitivity, a positive antigen test only confirms a diagnosis of influenza A virus. Thus, it would require additional subtype-specific diagnostic methods (e.g., RT-PCR or culture) to differentiate avian from human influenza virus. Although H5-subtype-specific antigen detection tests are now becoming available on an experimental basis and are undergoing evaluation for the diagnosis of diseased poultry, the current commercially available antigen detection tests seem to have limited clinical utility for the diagnosis of H5N1 disease in humans.
RT-PCR.
RT-PCR assays need to be targeted at genes (e.g., matrix gene) that are relatively conserved in order to detect all influenza A viruses and, separately, at the HA or NA genes to identify specific influenza A virus subtypes. Usually, a panel of such RT-PCR assays, which includes generic influenza A virus detection plus specific detection of H5, H3, and H1 subtypes, is used to investigate suspected human H5N1 disease. This strategy helps overcome potentially false-negative PCR results due to the mutation of the HA gene because a specimen with a positive matrix gene that is negative for H5, H3, and H1 would flag that specimen for more detailed investigation. Including the time needed for viral RNA extraction and analysis of the amplification products, the turnaround time for conventional RT-PCR assays is 6 to 8 h (or typically overnight). The use of real-time PCR shortens the turnaround time to around 4 to 6 h, increases sensitivity and specificity by the use of probes, and enables the quantitation of the viral target gene (39, 157). Even more importantly, because these are closed systems, the risk of PCR cross-contamination is minimized. The existence of several distinct sublineages and the high mutability of H5N1 viruses (28, 29, 202) pose a challenge for molecular diagnostics and necessitate continued evaluation, and possibly the modification of primers or probes, over time. Alternative molecular detection methods such as loop-mediated isothermal amplification tests have also been used, although they are not in routine use (88, 173).
Antibody detection.
The detection of H5N1-specific antibodies is essential for epidemiological investigations. Because of the delayed seroconversion and the need for paired sera, serology can provide retrospective confirmation of H5N1 infection. While HI is the preferred method for the detection of subtype-specific antibodies to human seasonal influenza viruses in human sera, conventional HI tests (using avian or human erythrocytes) have limited value for detecting antibodies against avian viruses in humans and other mammals because of low sensitivity (7, 104, 136, 182). Comparison of HI antibody tests with detection of neutralizing antibodies in H5N1-infected persons from the 1997 Hong Kong outbreak showed the latter to be more sensitive (182). Based on these observations, neutralization assays have become the methods of choice for the detection of H5-specific antibodies in humans. Using these assays, antibodies against H5N1 virus were generally detected 14 or more days after the onset of symptoms in patients infected during the 1997 Hong Kong outbreak (98). This is comparable to kinetics of the antibody response during primary infection with human influenza viruses.
While neutralization assays seem to be the most reliable methods for the detection of human antibodies to avian viruses, the requirement of BSL-3 laboratory facilities and the labor-intensiveness are important disadvantages. HI assays using horse erythrocytes have shown promising results for detecting antibodies against H5N1 viruses in humans and may provide a convenient alternative to neutralization tests and serve as a confirmatory test of a positive neutralization test result (211). Lentivirus pseudotyped with H5 HA may provide an alternative option for the serodiagnosis of H5N1 infection in mammals (154a).
Biosafety.
Laboratory procedures that involve virus culture (virus isolation and neutralization tests) should be carried out in BSL-3 laboratory facilities. In regions where the virus is not endemic, even procedures such as RT-PCR assays that do not involve the culture of live virus may be recommended to be done under BSL-3 containment. However, in regions where HPAI H5N1 virus is widespread in poultry, procedures that do not involve the amplification of infectious virus by culture, such as the extraction of viral RNA from clinical specimens for the purpose of RT-PCR assays, can, if necessary, be performed at BSL-2 containment with BSL-3 practices. Similarly, microbiological investigation of respiratory specimens from suspected H5N1 patients for alternative pathogens can also be carried out in BSL-2 containment. In view of the potential presence of infectious virus in stools and blood, it would also be prudent to perform any tests on such specimens within BSL-2 containment unless agents that reliably inactivate the virus are added in the course of the procedure. Tests with serum or plasma samples are best done after heat inactivation for 30 min at 56°C. WHO guidelines for the safe handling of specimens suspected to have H5N1 virus are available (http://www.who.int/csr/disease/avian_influenza/guidelines/handlingspecimens/en/index.html).
Antiviral Treatment and Other Options for Therapy
The adamantanes (amantadine and rimantadine) and the NA inhibitors (oseltamivir and zanamivir) are the two currently available classes of drugs that are specifically active against influenza viruses. The adamantanes are inhibitors of the ion channel activity of the M2 membrane protein of influenza A viruses. H5N1 viruses responsible for the 1997 outbreak in Hong Kong were susceptible to amantadine, and several H5N1 patients during the same outbreak were treated with this drug (266). However, no conclusions could be made regarding its clinical efficacy. The genotype Z clade 1 viruses infecting humans in Vietnam, Cambodia, and Thailand since 2003 contained Ser31Asn and Leu26Ile amino acid replacements in M2, which confer high-level resistance against amantadine (2, 28, 31, 127, 175). This has precluded the use of amantadine in these countries for the treatment of avian influenza H5N1 virus. Some but not all recently described H5N1 viruses isolated from avian species and from humans in other parts of Asia and Europe, especially those belonging to the Qinghai Lake-like (subclade 2.2) viruses, were susceptible to amantadine (29, 31, 97, 202, 258). Note that recent epidemic H3N2 strains have also acquired high levels of resistance to the adamantanes (17). Because of this, the adamantanes are no longer recommended for treating human seasonal influenza virus. It is relevant that if a pandemic H5N1 virus were to arise through reassortment with a human H3N2 virus, the reassortant, which is likely to carry the M gene segment of the human virus, will be resistant to amantadine, irrespective of the resistance status of the H5N1 parent virus.
H5N1 viruses isolated from untreated patients have been shown to be susceptible to oseltamivir and zanamivir in vitro (65, 125), and both NA inhibitors also showed therapeutic and prophylactic activities against the 1997 H5N1 strain in murine models (73, 124). However, murine studies suggest that, compared to the 1997 H5N1 virus, higher doses and prolonged administration of oseltamivir are needed to achieve similar antiviral effects against recently isolated H5N1 strains (264).
Treatment has been given to several patients infected with avian influenza viruses including H5N1, H7N7, and H7N3, but conclusive evidence for efficacy are unavailable because the relevant placebo-controlled trials have not been carried out and indeed are probably unethical to conduct (8, 54, 112, 232, 239). The available evidence relating to therapeutic options has been summarized (http://www.who.int/medicines/publications/WHO_PSM_PAR_2006.6.pdf). The limited clinical experience does not suggest a substantial impact of antiviral treatment on the mortality of human H5N1 influenza virus in the field setting. This may be explained at least in part by the relatively late presentation to hospitals (median of 4 days after the onset of illness) (260) and consequent delay in initiation of treatment in many patients. The inability of antiviral treatment to have an impact upon ongoing immune-mediated pathology may also have contributed to the poor clinical outcome. In addition, the dose and oral route of administration of oseltamivir, while perhaps sufficient and convenient for uncomplicated seasonal human influenza virus, may not be optimal in severely ill H5N1-infected patients for whom the pharmacokinetics may be different because they are often intubated and also apt to have diarrhea, which may adversely affect drug absorption. The availability of parenteral formulations of existing drugs would help to guarantee adequate drug levels in these patients. Finally, the emergence of drug-resistant viruses in patients on therapy may adversely affect the clinical efficacy of oseltamivir in H5N1 influenza virus. For human influenza virus, resistance to oseltamivir is rare in adults, but resistance rates of up to 18% have been observed in children (77, 108, 248). The higher resistance rates in children with human influenza virus may be explained in part by a lack of previous immunity in young children, which is associated with higher levels of viral replication and leads to an increased opportunity for mutation. Moreover, some of the children in studies in which high resistance rates were found may have received suboptimal dosing of the drug (77). Since all human cases of influenza H5N1 virus are in effect “primary infections,” it should not be surprising that antiviral resistance can occur during treatment of this infection, especially considering the high viral load in the human respiratory tract (40). The first report of oseltamivir resistance in human influenza H5N1 virus concerned the isolation of a minor subpopulation of resistant variants from a girl who received prophylactic once-daily treatment at the time of diagnosis (121). This patient was subsequently treated with oseltamivir at therapeutic twice-daily doses and survived. Studies using these viruses in vitro and in animals showed that as with human influenza viruses, the His274Tyr replacement in N1 of H5N1 responsible for oseltamivir resistance substantially reduced the fitness of the virus (121). Perhaps more concerning has been the isolation of major subpopulations of resistant viruses from two of seven H5N1-infected patients after a full 5-day course of oseltamivir at therapeutic doses, suggesting a high resistance rate during treatment of influenza H5N1 virus (41). In at least one of the two patients, both of whom died, the clinical course suggested a possible relationship between the emergence of resistant virus and therapeutic failure. On a more positive note, that same study also suggested that even when oseltamivir treatment is started later in the course of infection, viral clearance can occur in some patients, and this is associated with a favorable clinical outcome (41). Thus, in contrast to human influenza virus, where treatment after the first 48 h provides little clinical benefit, there may be a wider therapeutic window of clinical benefit in H5N1 disease (and also in a pandemic situation). This may be because of the differences in the viral load dynamics between human influenza virus (where the booster response due to prior cross-reactive immunity rapidly controls viral load) and H5N1 disease, where viral load remains high for many days into the illness because of the lack of cross-reactive immunity (see “Pathogenesis of Human Influenza H5N1 Virus”) (40).
In addition to efforts to diagnose and treat H5N1 influenza virus early in the course of infection, antiviral strategies that minimize the risk of resistance development deserve attention. These include measures to optimize and guarantee adequate drug levels through intravenous therapy (e.g., intravenous zanamivir and peramivir) (20) or the use of combined antiviral treatment (87). The possibility of coadministering probenecid with oseltamivir to increase plasma levels of oseltamivir has been raised, but the pharmacodynamics of such therapy in severely ill patients remain unknown (85). The use of combination therapy with the aim of reducing antiviral resistance has been evaluated in animal models for the adamantanes and NA inhibitors (87). This option is constrained by the emergence of adamantane resistance in some recently isolated H5N1 virus isolates. Other options for antiviral combination with oseltamivir include ribavirin or the use of two NA inhibitors. There is limited cross-resistance between zanamivir and oseltamivir. However, administration of an inhaled drug to a severely ill patient poses a challenge. Furthermore, given the possibility that H5N1 may be a disseminated disease, monotherapy with a drug with activity limited to the upper respiratory tract may not be advisable. However, inhaled zanamivir may remain an option for chemoprophylaxis (see below). Key pharmacokinetic characteristics of currently available anti-influenza virus agents have been recently reviewed (256).
The NA subtypes phylogenetically cluster in to two groups: group 1 includes N1, N4, N5, and N8, while group 2 comprises that other five NA subtypes, including N2. Structural studies have revealed important differences between group 1 and group 2 NA, and these include regions adjacent to the enzymatic active site. These findings may provide incentives for the design of modified NA inhibitors that may better fit the enzymatic site of the group 1 NA, including the N1 subtype (183).
In addition, the development of novel drugs directed at alternative viral targets may need consideration. In view of its importance for adaptation and virulence of H5N1 viruses in humans, the viral polymerase complex may represent an attractive target for the design of novel drugs (184). Small peptides that have broad-spectrum activity in blocking virus entry have been described (93). Considering the potential role of cytokine dysregulation in the pathogenesis of influenza H5N1 virus, benefits of immunomodulatory therapy could also be hypothesized. Finally, passive immunotherapy using convalescent-phase serum is believed to have conferred clinical benefit in the 1918 pandemic (140), and neutralizing monoclonal antibodies have shown therapeutic efficacy in influenza A virus infection in mice with severe combined immunodeficiency (167). Thus, passive immunotherapy also remains a possible consideration for the management of human H5N1 disease (75).
Infection Control and Prophylaxis
Current knowledge concerning virus excretion patterns and periods of potential infectivity during the course of human infections with H5N1 viruses is limited. In its present from, the H5N1 virus is poorly transmissible from avians to humans and from humans to humans (see above). However, because of the uncertainty about the modes of human-to-human transmission, the high lethality of human disease, and the possibility that the virus may change to a strain capable of more efficient human-to-human transmission, enhanced infection control measures seem to be warranted (see http://www.who.int/csr/disease/avian_influenza/guidelines/infectioncontrol1/en/index.html). When available, full-barrier precautions (i.e., standard, contact, and airborne precautions) should be used when working in direct contact with suspected or confirmed H5N1-infected patients. These include hand hygiene, gowns, gloves, face shields or goggles, a particulate respirator (N95, EU FFP2, or equivalent), and negative-pressure isolation rooms. However, because airborne precautions (negative-pressure rooms and N95 respirators) may not be available in all health care facilities confronted with suspected patients, standard and droplet (surgical mask and gowns) precautions together with eye protection comprise the minimal infection control recommendations for managing such patients. Given the presence of infectious virus in the feces, it must be noted that diarrhea in H5N1 patients represents an additional route for nosocomial transmission (34, 39, 232, 240, 266).
Should the virus acquire the ability for efficient human-to-human transmission, it is likely that the modes of transmission will be similar to those of human influenza viruses, viz., droplet and direct contact with secretions or fomites (14) (see http://www.pandemicflu.gov/plan/healthcare/masksguidancehc.html). However, the contribution of aerosol transmission of human influenza virus remains controversial (228). The contribution of aerosol spread in a pandemic setting (with no prior immunity) cannot be excluded.
Oseltamivir and zanamivir have proven efficacy as seasonal or postexposure prophylaxis against human influenza virus (160). Offering prophylactic treatment (for 7 to 10 days after the last exposure) to persons with unprotected exposure to H5N1 influenza virus deserves consideration. Given the many clusters of cases within families, prophylactic treatment is particularly important for close family contacts of infected patients. Personnel with unprotected exposures such as those who have carried out aerosol-generating procedures on H5N1 patients may also be considered for chemoprophylaxis. Prophylactic treatment with oseltamivir has been offered to potentially exposed individuals during the poultry outbreaks of H7N7 and H7N3 viruses in The Netherlands and Canada, respectively (112, 239). A benefit of prophylaxis has been suggested during the Dutch outbreak; H7N7 infection was detected in 1 of 90 persons who reportedly received prophylaxis compared to 5 of 52 persons who had not taken oseltamivir.
Vaccines
The development of an effective pandemic vaccine poses significant challenges, more so with HPAI viruses such as H5N1. Recent reviews have addressed these issues in relation to H5N1 and H9N2 vaccines (64, 208, 209). Experience with H1N1 vaccines in 1976 demonstrated that in the absence of prior immune priming, immunogenicity of a vaccine will be lower than that of seasonal vaccines, and two doses are likely to be needed. Furthermore, whole-virus vaccines were more immunogenic (and reactogenic) than subunit or split-product vaccines (92). While the correlates of protection for epidemic vaccines are well understood, those for a pandemic vaccine are still unclear. For example, while epidemic seasonal vaccine immunogenicity is defined by HI titers induced in humans, natural infection with avian influenza viruses induces poor HA inhibition titers but better neutralization titers. The procedures and protective titers in neutralization tests have not been agreed upon. Furthermore, avian influenza virus HA is generally less immunogenic than mammalian influenza virus HAs (207). The reasons for this are poorly understood. However, some amino acid residues (e.g., N223) can enhance HI antibody titers of the H5 HA in ferrets (81).
HPAI viruses rapidly kill the embryonated eggs that are conventionally used for vaccine production before good viral antigen titers have had the opportunity to develop. Furthermore, the use of an nonattenuated HPAI virus as the vaccine seed virus necessitates vaccine-manufacturing plants that are at BSL-3 containment. Initially, these issues were addressed through the attempted use of low-pathogenicity surrogate vaccines (e.g., H5N3) (207, 210). Alternatively, the use of reverse genetics to remove the multibasic amino acids at the HA cleavage site is now being employed to generate a recombinant virus candidate with the HA and NA of the putative vaccine candidate on an A/PR8/34 backbone. A/PR8/34 grows to high titers in eggs, and such recombinants enhance the antigenic yield (250).
Since conventional killed subunit vaccines have relatively narrow cross-reactivity, it is important to match the vaccine candidate to the eventual pandemic virus. Given the antigenic diversity of H5N1 viruses currently circulating across Asia (see above) (28, 202), and since we have no way of predicting which of these variants, if any, will become pandemic, there is the dilemma regarding which H5 HA should be used for prepandemic vaccine development. A number of vaccine candidates may need to be developed so that the overall diversity can be encompassed. Currently, the WHO has identified prototype viruses of clade 1 (A/Vietnam/1203/04-like), clade 2.1 (A/Indonesia/5/05), clade 2.2 (A/Bar-Headed Goose/Qinghai/1A/05-like), and clade 2.3 (A/Anhui/1/05) (“Fujian-like sublineage”) for vaccine development (257). Alternatively, vaccine strategies that induce broad cross-immunity within the subtype need to be considered.
Candidate H5N1 vaccines for clade 1 viruses, i.e., A/Vietnam/1203/04 or A/Vietnam/1194/04, have been made using the plasmid-based reverse-genetics system (250). Phase 1 clinical trials with healthy adults have been completed. In dose-ranging studies without adjuvants, it was found that only two doses each containing 90 μg of HA induced antibody responses that would be acceptable for licensing (233). This is a much higher HA dose than is used in typical seasonal influenza virus vaccines and would make large-scale vaccine production impractical. H5N1 subunit vaccines adjuvanted with aluminum phosphate modestly increased immunogenicity but not to levels that would make large-scale H5N1 vaccine production a feasible proposition (13, 208, 209, 233). An alum-adjuvanted whole-virus H5N1 vaccine has provided more promising results, with two doses of 10 μg providing reasonable immunogenicity (130).
Clearly, alternative strategies need to be considered to improve immunogenicity as well as broaden cross-protection. Whole-virus vaccines are known to be more immunogenic in unprimed humans (92), and preliminary reports of adjuvanted whole-virus vaccines have provided more promising results (130). The role of alternative adjuvants (e.g., MF59) and priming doses or alternative routes of immunization are being considered (207). An alternative strategy is the use of cold-adapted live, attenuated vaccines. These vaccines (e.g., FluMist) are known to provide broader cross-protection than subunit vaccines for seasonal influenza virus. Recombinant viruses bearing the H5 and N1 antigens on the cold-adapted influenza virus backbone appear to confer broad cross-protection against challenge with antigenically diverse H5N1 viruses in mouse studies (43, 137, 220). Phase 1 human studies are in progress. While a live, attenuated vaccine may not be acceptable for the preemptive vaccination of human populations prior to the emergence of a pandemic because of the theoretical risk that such an live, attenuated H5N1 virus may reassort with a human influenza virus to generate a pandemic, once an influenza virus pandemic has started, this ceases to be a concern.
Other options that have been evaluated include recombinant baculovirus-expressed H5 HA vaccines and DNA vaccine strategies. Recombinant baculovirus-expressed H5 HA was safe but poorly immunogenic in phase 1 clinical trials (234). Mice immunized with DNA encoding the HA of homologous and distantly related H5 (H5N8) protected against virulent H5N1 virus challenge, although the protection afforded by the H5 of H5N8 was only partial (111). Adenovirus-vectored H5 vaccines were shown to induce broadly cross-reactive immunity to H5N1 viruses from different sublineages (80).
A “universal” influenza virus vaccine remains the elusive “holy grail” of influenza virus vaccinology. The M2 protein is present on the cell surface, albeit at low density. It is antigenically conserved across different subtypes but is poorly immunogenic following natural infections. The M2 antigen ectodomain is one option being explored as a strategy for a universal vaccine (155). DNA vaccines based on the virus nucleoprotein and others have also been explored. But these are still far from being available as likely vaccine candidates in the short term (49, 95).
Vaccines, even those of moderate efficacy, are an effective public health intervention to mitigate the impact of an influenza virus pandemic (52). However, even when effective strategies for the development of H5N1 vaccines have been developed, the production of sufficient vaccine to meet the needs of the global population in the event of a pandemic remains a logistical challenge. There is a gap between current influenza virus vaccine production capacities (based largely on the growth of vaccine virus in embryonated eggs) and the need engendered by a pandemic. The current global vaccine production capacity (300 million doses of seasonal trivalent vaccine) will allow 450 million people to be vaccinated with two doses of a monovalent vaccine containing 15 μg HA per dose. This is sufficient to meet only a fraction of the likely global demand for vaccines in the event of a pandemic. Approaches to address some of the bottlenecks in vaccine production include the use of cell culture-grown vaccines (161) and antigen-sparing strategies such as novel adjuvants or delivery systems. While intradermal vaccination has been successful as a dose-sparing strategy for seasonal vaccination (11), it may not be useful for pandemic vaccine delivery. Finally, increasing the utilization of seasonal influenza virus vaccination will improve global vaccine capacity in the event of a pandemic. The poor utilization of seasonal vaccines is partly attributed to an underappreciation of influenza virus-associated morbidity and mortality, especially in the tropics. However, recent studies conclusively demonstrated that influenza virus has a similar impact in warm as well as temperate regions (254, 255) and argue for increased utilization of seasonal influenza virus vaccines for high-risk groups in all geographic regions.
Poultry vaccines for HPAI H5N1 virus have hitherto been inactivated and adjuvanted or have been fowlpox vectored and have been reviewed elsewhere (http://www.fao.org/ag/againfo/programs/en/empres/vaccine_producers.htm) (48, 221). More recent strategies have included the development of in ovo vaccination with a nonreplicating human adenovirus encoding an H5 HA (231) and live, attenuated Newcastle disease vaccines that express the H5 HA (61). The role of poultry vaccines in controlling transmission in poultry is discussed below.
OPTIONS FOR INTERVENTION
Controlling Transmission in Poultry
Those countries that detected the introduction of HPAI H5N1 virus into their poultry flocks early (e.g., Japan, South Korea, and Malaysia) and instituted control measures promptly and decisively succeeded in eradicating it. Others (e.g., Hong Kong) have devised strategies that enable them to keep the virus at bay, viz., eradication by “stamping out” followed by vaccination to prevent virus reintroduction (48, 199, 200). For those countries that are yet unaffected, the lessons from these examples are to (i) enhance surveillance and veterinary diagnostic capabilities for early detection of HPAI virus introduction, (ii) have contingency plans for a rapid response to deal with such an introduction, and, most importantly, (iii) not be complacent. In countries where HPAI H5N1 virus has become endemic, the challenges are much greater. The main objective, then, is to manage the risks to human health and to minimize transmission within poultry. Options for control remain enhanced community-based surveillance and education for early detection, stamping out of known infection through culling, movement controls, enhanced biosecurity of farms, and vaccination (50, 199, 200). H5 vaccines can interrupt transmission in addition to suppressing clinical disease (47). Vaccination may be successful as part of such an integrated strategy and as long as a good quality-controlled vaccine is used and is deployed with adequate safeguards to detect low-level circulation of virus in vaccinated flocks. These may include the use of unvaccinated sentinel birds within flocks and the use of serology testing that permits the differentiation of vaccine-derived antibody from that arising from natural infection (48). Vaccination programs should be accompanied by monitoring systems to assess the effectiveness of the program and maintain a high level of surveillance to detect the emergence of antigenic variants (199). While vaccine-induced antigenic drift may occur in poultry, this is not of itself a reason to preclude the use of vaccines as part of a comprehensive strategy of control (122, 216). The experience in Hong Kong indicates that vaccination is likely to be more successful when it is used to prevent virus reintroduction after successful control has achieved an elimination or reduction of endemicity by other means. If a vaccine is used as a single strategy to dampen existing endemic virus infection without other measures to reduce viral burden in poultry flocks, the chances of success may be poor (186).
Targeted local epidemiological studies that elucidate critical points in virus dissemination pathways that are amenable to intervention are still needed. For example, if “wet markets” are playing a role in viral amplification and spread (117, 118), this may provide options for intervention. Such strategies have been successfully implemented in Hong Kong. If there is a marked seasonal pattern in virus activity within poultry as demonstrated in southern China, for example (127), this may help identify the summer months, where virus transmission is at its lowest, as the time when interventions may be most likely to be successful in interrupting transmission. Given the likely role of ducks in the epidemiology of the infection, field studies on the efficacy of vaccination in ducks are urgently required (149). But most importantly, what is required for successful control is strong political commitment and determined implementation.
Control or Mitigation of a Pandemic
Simulation models of pandemics in silico have provided insights into the potential impact of options or combinations of options that may conceivably stop an incipient pandemic or mitigate its impact (51, 52, 135). Geographically targeted antiviral therapy together with social-distancing measures were demonstrated to have the potential to stop an emerging pandemic with a basic reproduction number of <1.8 if the interventions are deployed early enough. However, success is likely only if the emerging pandemic is detected within the first weeks of its emergence (51, 135). The problems of implementing this strategy in a rural developing country setting are formidable both in relation to early detection and in the logistics of implementation. Clusters of human-to-human transmission, even large ones as seen recently in North Sumatra, by themselves do not reliably herald a pandemic (http://www.who.int/csr/don/2006_05_31/en/index.html) (97). It is clear that spread beyond the immediate family has to be awaited before activating such a plan, narrowing the window of time available for such intervention even further.
A vaccine, even one of moderate effectiveness, is likely to have a substantial impact on attack rates in the course of a pandemic (52). Since nonpharmaceutical interventions are likely to be the measures most widely available on a global scale, there is an urgent need for community-based field trials or simulation model data upon which more authoritative recommendations can be based. Available evidence has been reviewed recently (9, 10). While there are no direct data for the efficacy of these interventions in a community setting, it was reasoned that hand hygiene measures may be of use, although the likely benefit of masks was less certain. Border restrictions or internal travel restrictions are unlikely to have a significant effect in mitigating the impact of an evolving pandemic. School closures may reduce the peak attack rates but may not significantly affect the overall attack rates (52). In a densely populated city (viz., Hong Kong), a simulation model of the efficacy of interventions in a pandemic suggested that a combination of household-based quarantine, case isolation, and targeted use of antiviral prophylaxis would have a significant impact in reducing the symptomatic attack rate, morbidity, and mortality, whereas contact tracing was not likely to provide a significant benefit (261).
WILL THE NEXT PANDEMIC VIRUS BE H5N1?
The requirements for the emergence of a pandemic virus are a novel HA (and possibly NA) subtype, lack of prior immunity in the human population, and the capacity for efficient and sustained human-to-human transmission. Contemporary H5N1 viruses have repeatedly zoonotically transmitted to humans and have occasionally manifested limited human-to-human transmission following close prolonged contact with infected individuals (241). It is the inability of this virus so far to become efficiently transmissible in humans that stands between a zoonotic disease and a pandemic one.
Given that multiple pandemics have emerged in past centuries (106, 174), it is highly likely that we will confront such pandemics in this 21st century. The ecological factors that predispose to the emergence of pandemic influenza virus have not abated. On the contrary, they have increased. The vastly enhanced travel and globalization of trade will conspire to enhance the rapid of spread of a pandemic virus and to accentuate its global economic impact. It may be argued that the availability of antibiotics and better supportive care may mitigate the impact of future pandemics. But we still remain largely ignorant about the pathogenesis of pandemic influenza virus and the basis for the apparent virulence of the 1918 pandemic virus or the apparent severity of recent H5N1 disease in humans.
However, predicting the virus subtype that will cause the next pandemic is far more daunting. The fact that this H5N1 lineage has been endemic in poultry for at least 10 years and that different genotypes of these viruses have repeatedly infected humans (69, 127, 218, 268) without becoming pandemic so far implies that such a change is likely to be a rare event that requires multiple genetic changes. Clearly, the increasing geographic spread of poultry infection increases the opportunity for such a rare event to occur.
The H5N1 virus may become pandemic through direct adaptation, as is believed to have occurred with the 1918 Spanish flu virus (225, 226), or through reassortment with a prevailing human influenza virus. Such reassortment may occur within a human fortuitously coinfected with H5N1 and a human influenza virus. It may also occur in an intermediate host such as a pig. The human H3N2 (unreassorted) virus is known to be endemic in pigs in southern China (169). H5N1 virus can infect pigs but does not appear to have become endemic in pig populations so far (33). However, given the close interaction between pigs and poultry in many households in Asia (141), there would be ample opportunity for H5N1 virus to coinfect a pig infected with human H3N2 virus.
In ferrets, H5N1 viruses fail to transmit from animal to animal, while human H3N2 viruses do. Interestingly, an artificially created recombinant with the H5 and N1 genes from H5N1 and the other six gene segments from the human H3N2 virus also failed to transmit from ferret to ferret (143). These findings support the contention that multiple genetic changes in the virus are probably required to generate a potentially pandemic virus. For example, as discussed above, mutant H5N1 viruses with affinity for SA α-2,6 receptors do not inevitably lead to efficient human-to-human transmission (192, 263). However, this does not mean that a combination of genetic changes that lead to the emergence of a pandemic virus will never occur. The enormous replicative capacity of a highly mutable virus and the complex ecology we now see with H5N1 viruses repeatedly crossing avian-mammalian species barriers mean that there is every possibility that a rare constellation of events may indeed occur, given time and opportunity. Indeed, the lessons of severe acute respiratory syndrome caution against such complacence.
On the other hand, there is no certainty that the next pandemic will be caused by H5N1 or even by another HPAI virus. The pandemics of 1957 and 1968 did not arise from HPAI viruses from poultry and were probably not heralded by major outbreaks of poultry disease. Therefore, H5N1 is not the only virus subtype that may cause the next influenza virus pandemic. Such a pandemic may well arise from other avian influenza viruses that are circulating asymptomatically (LPAI viruses) in poultry flocks (e.g., H9N2) or even wild birds. For example, H9N2 viruses are LPAI viruses and are endemic in poultry across a wide geographic range (East Asia to Middle East Asia) (21, 70). They have infected humans but cause only a mild flu-like illness (19, 131, 171) and are likely to remain unrecognized in humans. Poultry infection is similarly inconspicuous. Furthermore, H9N2 viruses have been detected in pigs (169) and have a receptor binding profile that can bind human-like receptors (148). Therefore, it is arguable that H9N2 viruses may be at least equally plausible candidates as the next pandemic virus.
CONCLUSION
The rationale for particular concern about an H5N1 pandemic is not its inevitability but its possible severe impact on human health. Such a pandemic, especially if it arises by direct adaptation rather than genetic reassortment with a preexisting human virus, could well be unusually virulent in humans. Thus, an H5N1 pandemic is an event of low probability but one of high human health impact. What is certain, however, is that the H5N1 panzootic already impacts human health via its economic and consequent nutritional impacts on rural societies and by occasional zoonotic transmission, leading to severe human disease with its attendant social impact. It is just as bad to die of protein malnutrition (because of the depletion of a major protein source for many people) as it is to die of zoonotic “bird flu.” Given the increasing geographical spread and the endemicity of H5N1 viruses in poultry across the world, and its possible (yet-to-be-proven) foothold within wild bird populations, H5N1 is likely to remain a serious threat to human health for quite some time to come. Clearly, there is every reason to attempt to control the current panzootic in poultry. If not, the attendant pandemic threat from H5N1 will continue to pose a predicament for public health.
Acknowledgments
We acknowledge research grant funding from a Croucher Foundation Award to J. S. M. Peiris, Public Health Research grant A195357 from the National Institute of Allergy and Infectious Diseases, and Wellcome Trust grant 067072/D/02/Z. M. D. de Jong is supported through the Oxford University Clinical Research Unit at the Hospital for Tropical Diseases, Viet Nam, funded by a Wellcome Trust grant (077078/Z/05/Z), and this review also represents his work conducted as part of the SE Asian Influenza Clinical Research Network supported by the National Institute of Allergy and Infectious Diseases (NIH N01-AO-00042).
We thank Frances Wong for secretarial assistance.
REFERENCES
Articles from Clinical Microbiology Reviews are provided here courtesy of American Society for Microbiology (ASM)
Full text links
Read article at publisher's site: https://doi.org/10.1128/cmr.00037-06
Read article for free, from open access legal sources, via Unpaywall:
https://europepmc.org/articles/pmc1865597?pdf=render
Citations & impact
Impact metrics
Article citations
Avian Influenza: Lessons from Past Outbreaks and an Inventory of Data Sources, Mathematical and AI Models, and Early Warning Systems for Forecasting and Hotspot Detection to Tackle Ongoing Outbreaks.
Healthcare (Basel), 12(19):1959, 01 Oct 2024
Cited by: 0 articles | PMID: 39408139 | PMCID: PMC11476403
Review Free full text in Europe PMC
VirID: Beyond Virus Discovery-An Integrated Platform for Comprehensive RNA Virus Characterization.
Mol Biol Evol, 41(10):msae202, 01 Oct 2024
Cited by: 0 articles | PMID: 39331699 | PMCID: PMC11523140
Can global health security frameworks measure One Health implementation in West Africa?A mixed-methods study.
BMC Public Health, 24(1):2113, 05 Aug 2024
Cited by: 0 articles | PMID: 39103806 | PMCID: PMC11299367
Role of miRNA in Highly Pathogenic H5 Avian Influenza Virus Infection: An Emphasis on Cellular and Chicken Models.
Viruses, 16(7):1102, 09 Jul 2024
Cited by: 2 articles | PMID: 39066264 | PMCID: PMC11281567
Review Free full text in Europe PMC
Modeling transmission of avian influenza viruses at the human-animal-environment interface in Cuba.
Front Vet Sci, 11:1415559, 11 Jul 2024
Cited by: 0 articles | PMID: 39055861 | PMCID: PMC11269842
Go to all (480) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
H5N1 outbreaks and enzootic influenza.
Emerg Infect Dis, 12(1):3-8, 01 Jan 2006
Cited by: 215 articles | PMID: 16494709 | PMCID: PMC3291402
Review Free full text in Europe PMC
The next influenza pandemic: lessons from Hong Kong.
J Appl Microbiol, 94 Suppl:70S-79S, 01 Jan 2003
Cited by: 32 articles | PMID: 12675938
[Current situation in human infections with highly pathogenic avian influenza viruses].
Nihon Rinsho, 68(9):1729-1735, 01 Sep 2010
Cited by: 0 articles | PMID: 20845756
(Highly pathogenic) avian influenza as a zoonotic agent.
Vet Microbiol, 140(3-4):237-245, 26 Aug 2009
Cited by: 64 articles | PMID: 19782482
Review
Funding
Funders who supported this work.
NIAID NIH HHS (2)
Grant ID: AI95357
Grant ID: N01-AO-00042
Wellcome Trust (2)
Grant ID: 067072/D/02/Z
Grant ID: 077078/Z/05/Z