Abstract
Free full text

Stress-Related Factors in Cannabis Use and Misuse: Implications for Prevention and Treatment
Abstract
We examined the role of stress as a risk factor and motivation for cannabis use/misuse. A systematic review of studies gathered from PsychINFO and MEDLINE databases was conducted. Findings suggest that cannabis is commonly used as a stress-coping strategy. Negative life events, trauma, and maladaptive coping were all related to consumption. Cannabis use for stress-coping purposes was most evident when examining chronic as compared with experimental use. While many individuals may be able to use cannabis without consequences, there appears to be a subset of individuals who experience greater life stress and who may be more likely to use for stress-coping purposes. These individuals may be at greatest risk for addiction. Chronic use may potentiate stress-related motivation to use/abuse cannabis and is associated with decision making deficits and alterations in brain-stress pathways that may exacerbate compulsive drug-seeking and sensitize individuals to stress-related drug use. Overall, stress-coping interventions and harm reduction focused on reducing the amount ingested may facilitate prevention and recovery efforts.
Introduction
Many people view cannabis (or marijuana) as a benign substance with relatively minor negative consequences that should be tolerated for medicinal and recreational purposes (e.g., Zimmer & Morgan, 1997). Permissive beliefs about cannabis are likely fueled by the harmless and even comical manner in which the drug is portrayed in venues of popular culture. However, others argue that there are, in fact, a number of adverse consequences related to cannabis use that could potentially create a significant public health problem should its use increase (Hall & Babor, 2000). The scientific community has not given the study of cannabis the attention it deserves given the popularity of its use, and a more cautious approach to understanding the causes and effects of cannabis use is needed (Hall & Babor, 2000).
Cannabis is the most widely used illicit substance in the United States (Substance Abuse & Mental Health Services Administration, 2003). Its use is increasing among college students, in most student subgroups, and across students enrolled in all types of colleges (Gledhill-Hoyt, Lee, Strote, & Wechsler, 2000). This escalation in use appears to be related to a heightened use of cannabis among younger adolescents as well as increased experimentation and movement toward regular use of the drug after age 18 (Gledhill-Hoyt et al. 2000). More than 50% of adolescents residing in the United States experiment with cannabis and, of those who try the drug more than once, a third eventually escalate to regular use (Gruber & Pope, 2002). For heavier users, symptoms of withdrawal can develop, making it increasingly difficult to quit (Budney, Novy, & Hughes, 1999; Budney, Moore, Vandrey, & Hughes, 2003). Moreover, cannabis use is associated with a number of social, emotional, health, and legal consequences (Degenhardt & Hall, 2006; Dennis et al., 2002; Gruber & Pope, 2002; Hubbard, Franco, & Onaivi, 1999; Khalsa, Genser, Francis, & Martin, 2002; McArdle, 2006; Office of National Drug Control Policy, 2004) and may even serve as a “gateway” to using and abusing other illicit drugs (Fergusson & Horwood, 2000; Fergusson, Horwood, & Swain-Campbell, 2002; Kandel, 2003; Lynskey, Heath, Bucholz, Slutske, Madden, Nelson, Statham, & Martin, 2003).
These findings suggest that prevention and intervention efforts are necessary and must be directed at both college-aged and secondary school-aged students in order to be most effective (Dennis et al., 2002; Gledhill-Hoyt, et al. 2000). However, prevention and intervention cannot be optimally employed until the factors that lead individuals to experiment with and continue to use cannabis are better understood.
Purpose of the Review
It has been substantiated that individuals turn to substances for recreational and social reasons, to enhance and maintain positive internal states, to cope with stress, and/or to reduce or avoid aversive internal states (Goeders, 2004; Johnston & O’Malley, 1986; Sinha, 2005). However, not all drug users report using a given substance for all of the same reasons, and reasons for and expectancies of use vary according to drug type and extent or pattern of use (Boys, Marsden, Griffiths, Fountain, Stillwell, & Strang, 1999; Johnston & O’Malley, 1986; Schafer & Brown, 1991; Simons, Correia, Carey, & Borsari, 1998; Simons, Correia, & Carey, 2000). While there are many risk factors associated with cannabis consumption (van den Bree & Pickworth, 2005; von Sydow, Lieb, Pfister, Hofler, & Wittchen, 2002), and many motives for use (Simons et al. 1998, 2000), we specifically focus on stress for two reasons: first, the body’s stress arousal system is directly affected by cannabis ingestion, and 2) it has consistently been cited as important both in maintaining cannabis use but also as a reason for chronic use.
Stress has been conceptualized as a relationship between an individual and his or her environment that is appraised as exceeding the individual’s coping resources and has the potential to endanger the person’s well-being (Lazarus & Folkman, 1984). The relationship between stress and substance use is well established (Goeders, 2003; 2004; Sinha, 2001; 2005; Turner & Lloyd, 2003; Wills, 1990). However, a comprehensive synthesis and evaluation of studies examining the specific association between stress and cannabis use is lacking. Thus, we conducted a literature review examining the extent to which individuals seek cannabis for stress-coping or tension-reduction purposes. We examined the extent to which family dysfunction, stressful life events (including traumatic stress), and maladaptive methods of coping with stress are related to cannabis use and misuse. Furthermore, we examined whether stress related cannabis use is most prominent in regular and chronic users or in all categories of cannabis users. Finally, we looked at how stress and chronic cannabis use may lead to decision-making deficits that can exacerbate stress and how stress-related alterations associated with cannabis abuse can sensitize individuals to the effects of stress and stress-related cannabis use.
Method
Studies included in this review were drawn from comprehensive MEDLINE (1950–2007) and PsycINFO (1967 – 2007) searches using various combinations of the following keywords: cannabis, marijuana, motives, stress, life events, coping, emotion regulation, trauma, traumatic stress, HPA, and decision-making. A manual search was also performed by scanning reference lists of reviewed articles in order to identify relevant articles that were not selected in our computerized search. The criteria for inclusion in the review were: (a) publication in English and (b) a focus on stress-related factors associated with cannabis use or misuse (e.g., negative family life events, traumatic stress, coping).
Importantly, we focused on the construct of psychological stress and not stress-related psychiatric disorders. The only exception was Posttraumatic Stress Disorder (PTSD) which requires traumatic stress exposure as a diagnostic criterion. Furthermore, while pain associated with medical problems can be stressful, we did not review studies that examined the use of cannabis for pain management (medically supervised or otherwise). Finally, dissertation research was excluded from the review. Due to the breadth of research on this topic, studies with more sophisticated designs and which have more focused goals and informative findings are described in greater detail.
Coping Motives and Cannabis Consumption
According to stress-coping models of addiction, substances are commonly used to cope with life stress by functioning to reduce negative affect and/or increase positive affect (Wills & Hirky, 1996). The model predicts that substance use is most likely when life stress is high and when adaptive coping resources are impoverished (Wills, 1990). Support for this model derives from a wealth of research indicating a robust relationship between stress and substance use (Goeders, 2003; Goeders, 2004; Sinha, 2001; Wills, 1990).
For cannabis users in particular, stress has been cited as a significant factor for its use. Hendlin and Haas (1985) described a series of studies of adolescents and adults who were heavy long-term cannabis users. Their findings, derived from a series of intensive interviews, indicated that cannabis served a number of purposes for adolescents, one of which was to help modify disturbing emotions, particularly intense anger directed toward their parents. For adults, it provided an escape or relief from problems and helped ease the anger and frustration caused by unhappy relationships. Additional support for the model was provided by Crutchfield and Gove (1984) who analyzed data from a national probability sample of adults and found that 15% of cannabis smokers reported using to cope when upset or having personal problems. Consistent with this study, Lee, Neighbors, and Woods (2007) found that 18% of recent high school graduates who used cannabis reported using for stress-coping purposes. On the other, hand higher rates of cannabis consumption for stress-coping purposes have also been reported.
Segal, Cromer, Hobfoll, and Wasserman (1982) examined self-reported reasons for drug use among a sample of detained and adjudicated juveniles. All respondents reported cannabis use, and 51% of the sample reported using more than once per day. Their findings indicated that over 50% of the sample reported using cannabis to “make them feel mellow,” and that this reason was given much less frequently for any other drug category (stimulants, hallucinogens, depressants, & narcotics), suggesting greater use of cannabis for tension reduction as compared with other drugs. Other researchers investigated the characteristics and patterns of cannabis use in adults who had used cannabis regularly for 10 or more years and found that the most common reason for cannabis use (reported by 61%) was to relax and relieve tension (Reilly, Didcott, Swift, & Hall, 1998). Through large surveys of American high school seniors participating in the “Monitoring the Future” study, Johnston and O’Malley (1986) examined reasons for cannabis use according to participants’ degree of involvement with the drug. Participants were categorized into experimental users if they used 1–2 times in their lifetime, occasional users if they used 3–9 times, heavier users if they used 10 or more times, and daily users (a subset of the category of heavier users) if they used on 20 or more occasions in the past 30 days. The investigators found that 72% of daily cannabis users (the most severe group) reported smoking to relax or relieve tension, 36% to escape from problems, 29% to alleviate anger or frustration, and 28% to get through the day. These percentages changed as other groups were examined with 7% of experimental users, 19% of occasional users, and 53% of heavier users using to relax or relieve tension, 3% of experimental users, 11% of occasional users, and 26% of heavier users using to get away from problems, 1% of experimental users, 2% of occasional users, and 11% of heavier users using to get through the day, and 1% of experimental users, 6% of occasional users, and 18% of heavier users using to alleviate anger or frustration. These findings suggested that smoking cannabis for coping-related reasons is reported more frequently by heavier users than by experimental or occasional users, suggesting that coping motives may be more prominent in chronic use of the drug. More recently, Boys, Marsden, and Strang (2001) examined the profiles of young poly-substance users (between ages 16–22; 96.2% lifetime cannabis users) and found that 97% of cannabis users reported using in the past year to help them relax, 69% to feel better when down or depressed, and 58% to help them stop worrying about a problem. Hathaway (2003) presented experienced, mostly long-term and frequent cannabis users aged 18 to 55 with a list of 20 possible reasons for using cannabis and asked them to rate the importance of each. The author found that cannabis use as a coping mechanism was among the most important reasons for use with relaxation being the top reason and over half of the sample reporting other coping motives (to forget your worries; to blow off steam; to see the world with fresh eyes; to feel less anxious) as at least “important” for their use. Green, Kavanagh, and Young (2003) reviewed the literature examining self-reports of cannabis effects that may be associated with ongoing cannabis use and found that, while there was much variation in cannabis effects, relaxation was the most frequently reported effect and reason for use. Finally, Green, Kavanagh, and Young (2004) used a two-group longitudinal design to examine reasons for cannabis use in adult men with and without psychosis. Their findings indicated that, at baseline and follow-up, those with psychosis most commonly reported using cannabis to positively alter their mood (36% and 42%), to help cope with negative affect (27% and 29%), and for social activity reasons (38% and 29%). Those without psychosis most commonly reported using cannabis to relax (34% and 43%), and for social activity reasons (49% and 51%).
Overall, these studies provide evidence that using cannabis to cope with stress or relieve tension is common and may be most prominent in heavier users of the drug. Furthermore, there is some evidence that compared with other illicit drugs cannabis may be most commonly used for stress reduction. Using cannabis for coping purposes may be more prominent in chronic cannabis users possibly because they are unable to use alternative coping or never had the skills for adaptive coping. It is also possible that stress systems are affected by chronic drug use making stress-related motivation to use more salient for chronic users.
A number of studies provide additional support for a role of stress in cannabis consumption by demonstrating an association between coping-motives and cannabis use and/or use-related problems. For example, Boys et al. (1999) interviewed young substance users (aged 16–21) on their perceptions of the function of substance use and perceived likelihood of using substances in the future. They found that perceived mood alteration (to help relax, to feel better when low or depressed, to make activities less boring) was associated with past 90 day frequency and intensity of cannabis use and intent to use cannabis in the future. McKay, Murphy, McGuire, Rivinus, and Maisto (1992) investigated reasons for substance use in a sample of incarcerated adolescents and found that “negative reasons” (when experiencing unpleasant emotions, physical discomfort, and conflict with others) were correlated with their frequency of cannabis use. Chabrol, Massot, and Mullet (2004) examined how drug-related beliefs are related to cannabis use and dependence in a sample of high school students. Using a dependence/non-dependence variable as the criterion, the authors found that relief-oriented beliefs (e.g., “Cannabis helps one to relax and calms anxiety; Cannabis use is the only way to reduce suffering.”) was the only significant predictor of cannabis dependence among users. Anticipatory beliefs (e.g., “To have a nice time, one can take cannabis.”) and permissive beliefs (e.g., “Cannabis is less serious than taking hard drugs.”) did not predict cannabis dependence. However, all three factors were significant in the model that predicted cannabis use, with permissive beliefs being the dominant factor. In an undergraduate sample, Simons et al. (1998) found that coping motives directly predicted cannabis use but not problems, with the relationship being stronger for women than it was for men, and coping motives were associated with cannabis use problems but indirectly through use. In a later study using undergraduates, Simons and colleagues found that coping motives were directly associated with both cannabis use and cannabis use problems (Simons, Gaher, Correia, Hansen, & Christopher, 2005). Lee, Neighbors and Woods (2007) found that coping motives were associated with greater cannabis use-related problems in recent high school graduates. Finally, Bonn-Miller, Zvolensky, and Bernstein (2007) found that coping motives were associated with the frequency of past 30-day cannabis use in young adult cannabis smokers even after controlling for number of years of cannabis use and current levels of alcohol and nicotine use. Furthermore, these authors found that anxiety sensitivity was related to coping motives for cannabis use, but not to other motives.
There is also some evidence that coping motives may be more prominent when examining continuing cannabis use as compared with initial use of the drug. For example, Copeland, Swift, and Rees (2001) investigated the clinical characteristics of adults seeking treatment for cannabis use disorders and found that the most commonly reported reasons for initial use were curiosity, availability, and peer pressure. High rates of co-morbid psychological distress were found in their sample, and stress relief was the most commonly reported benefit and reason for continuing cannabis use.
Overall, this body of literature provides evidence that cannabis users, and especially more chronic users, report that they commonly and consciously seek out the drug for stress-relief and that coping motives are related to cannabis use and use-related problems. The greater coping-related use seen in heavier users may be related to a greater expectancy of positive drug effects (Schafer & Brown, 1991), less pre-morbid ability to cope with stress, or alterations in stress and reward systems as a function of chronic use and cannabis dependence. In the following sections, we will examine some of the stress-related factors associated with early onset cannabis use and continuing consumption.
Stress-related Risk Factors Implicated in Cannabis Use and Misuse
Family Dysfunction and Stressful Life Events
Being raised in an environment with few models of adaptive coping and experiencing negative life events may place individuals at risk for substance use by elevating stress, reducing reinforcement from the social environment, and making the coping functions of substance use appear more attractive (Wills & Hirky, 1996). As such, family dysfunction, social disadvantage, and negative life events are all aversive life circumstances or experiences that can increase an individual’s risk for early onset cannabis use and later addiction.
Indeed, general family dysfunction and especially dysfunction concomitant with childhood abuse or parental substance abuse has been associated with higher rates of adolescent cannabis consumption (Gruber & Pope, 2002). Family disruption and poor family relations may set forth a developmental trajectory toward experimental and problematic cannabis use. For instance, Butters (2002) examined the impact of family stress on adolescent cannabis use and found that those reporting family disruption (e.g., from death or divorce) were 79% more likely to use cannabis than those who did not report family dysfunction. Of those who were already using cannabis, those reporting family disruption were 87% more likely to progress to problem use. In addition, degree of poor family relationships increased the likelihood that one would use cannabis by 22%, and among those who were already using cannabis, this factor increased the odds that one would use cannabis problematically by 15%. A secondary analysis indicated that those experiencing school problems were more likely to use cannabis and progress to problematic use. Interestingly, family disruption did not directly influence the progression to problem cannabis use once this school problem variable was added to the model. However, family disruption increased the odds of experiencing problems with school. Overall, it was concluded that, “while familial disruption through divorce or death, for example, may contribute to the initial choice to use cannabis, it may be that the impact of this stressor on other aspects of a youth’s life contributes to their progression to problem level use (p. 651).”
As part of a longitudinal study in which children were followed from birth, Fergusson and Horwood (1997) asked adolescents at age 16 about the frequency of their cannabis use over the past year and classified them into three groups: those who never used cannabis, those who used 1–9 times, and those who used 10 or more times. Groups were then compared on family and social background characteristics. Their findings indicated that those who used by age 16, and particularly frequent users, were more likely to come from socially disadvantaged backgrounds, to have experienced family adversity as children, to have formed affiliations with substance using or delinquent peers in adolescence, to have reported poorer attachments with parents, and to have had more adjustment problems by the age of 16. In another longitudinal study, researchers found that low socioeconomic status in childhood and low parental attachment in adolescence were associated with cannabis use by age 15 (McGee, Williams, Poulton, & Moffitt, 2000). A later prospective study found that adolescents reared in non-intact step-father families or families where there was conflict between adults in the home had higher rates of cannabis use disorders as young adults (Hayatbakhsh, Najman, Jamrozik, Mamun & Alati, 2006). McCubbin, Needle, and Wilson (1985) examined the relationship between family functioning and adolescent cannabis use using data from a three-year panel study of families selected randomly from a list of families enrolled in a local health maintenance organization and found that the accumulation of family stressors and strains predicted marijuana use in girls but not boys. Baer, McLaughlin, Burnside, Pokorny, and Garmezy (1987) found that seventh graders reported using more cannabis if they also reported experiencing more stressful life events and less family cohesiveness. Barnes, Barnes, and Patton (2005) found that high scores on father’s alcoholism and family life stress, and low scores on family cohesion were associated with heavy (once a week or more) versus moderate (less than once a week) cannabis use in sample of youth aged 14–25. Other researchers prospectively examined risk factors for incident cannabis use and progression to abuse and dependence in a sample of 14 to 24 year olds followed over a four-year period and found that unsatisfactory relationships with mothers and growing up without both parents increased the risk for incident use (von Sydow et al. 2002). Moreover, these authors found that deprived socioeconomic status and parental death before age 15 increased the risk for progression to dependence.
Using semiparametric group-based mixture modeling, Windle and Wiesner (2004) examined data from an adolescent school sample and identified five trajectory groups characterizing patterns of change in frequency of cannabis use across four waves of assessments during adolescence. These groups were labeled Abstainers, Experimental Users, Decreasers, Increasers, and High Chronics. Group comparisons on adolescent risk factors were then made to identify predictors of each trajectory group. Findings indicated that the High Chronics had more stressful life events relative to the other groups, and Abstainers had the lowest levels of stressful life events.
Using a composite score for alcohol, tobacco, and cannabis use, researchers prospectively found that negative life events were positively related to initial levels of adolescent substance use as well as to growth in use over time (Wills, Sandy, Yaeger, Cleary, & Shinar, 2001). Finally, Siqueira, Diab, Bodian, and Rolnitzky (2001) examined the relationship of stress with cannabis use status (never user, experimenter, & frequent user) in a sample of inner-city clinic based adolescents and young adults (aged 12–21) using a cross-sectional survey. Their findings indicated that, while experimenters and frequent users of cannabis reported more negative life events than non-users, they did not report greater perceived stress. The authors suggested that certain life events may not lead to greater perceived stress or that the physiological effects of frequent use may have distanced users from perceived stress in the face of an increased number of negative life events.
Overall, these studies suggest that family dysfunction, poor family relations, and negative life events may increase the risk for early onset cannabis consumption and the progression to heavier use. Stressful life events may translate to cannabis use behavior by elevating distress and increasing negative affect. Indeed, negative affect has been associated with greater initial levels of adolescent substance use as well as with greater levels of use over time (Wills, Sandy, Shinar, & Yeager, 1999). Emotional distress has been found to precede the initiation of substance use in adolescents (Tschann, Adler, Irwin, Millstein, Turner, & Kegeles, 1994), and trying cannabis for the first time when under psychological distress can increase one’s risk for escalated use (Kaplan, Martin, Johnson, & Robbins, 1986). Stress-reduction expectancies of cannabis use may be learned vicariously before ever trying the drug and may be reinforced by the social context of use as well as the drug’s physiological effects (Schafer & Brown, 1991). The negative reinforcement that follows from cannabis use under stressful circumstances may increase the future attractiveness of the drug when faced with similarly distressing situations. Early life stress may also predispose individuals to affiliate with deviant, substance using peers who facilitate availability and social acceptance of drugs (Hundleby & Mercer, 1987; Wills, Walker, Mendoza, & Ainette, 2006). Ultimately, stressful life circumstances, including growing up in a dysfunctional family and experiencing negative life events, may set individuals on a pathway toward early onset cannabis use, greater coping-related use, and an increased risk for cannabis addiction.
Traumatic Stress
Trauma represents the most extreme form of negative life event, and there is evidence that cannabis may be used to cope with traumatic stress (e.g., childhood maltreatment, disaster, domestic and community violence, combat trauma) and the negative emotional after-effects (e.g., post-traumatic stress symptoms) of trauma. Childhood maltreatment is of particular concern as it is commonly an ongoing high-intensity negative life event that can serve as a marker for severe family dysfunction as well as being a traumatic stressor in and of itself (Gold, 2000; Gold, Hyman, & Andres-Hyman, 2004). Childhood maltreatment may disrupt the maturation of self-regulatory systems that enable an individual to modulate and tolerate aversive affective states (Cicchetti & Toth, 2005; Hein, Cohen, & Campbell, 2005). It may also alter brain-stress responding (Bugental, 2004, DeBellis, 2002; Heim & Nemeroff, 2001; Heim, Newport, Heit, Graham, Wilcox, Bonsall, Miller, & Nemeroff, 2000) and sensitize individuals to the effects of subsequent life stressors (Glaser, Os, Portegijs, & Myin-Germeys, 2006; Harkness, Bruce, & Lumley, 2006). Furthermore, the dysfunctional family environment that commonly surrounds childhood maltreatment can cause deficits in coping skills necessary to effectively overcome life stress or alleviate related distress (Gold, 2000; Gold, Hyman, & Andres-Hyman, 2004). In this section, we will discuss childhood maltreatment along with other types of trauma as severe negative life events that can influence cannabis consumption. As far as sequelae are concerned, we will focus on Posttraumatic Stress Disorder (PTSD) as this disorder requires exposure to a traumatic stressor as a diagnostic criterion.
A number of studies provide evidence that childhood abuse and other early life traumatic events (e.g., early exposure to community violence) may influence cannabis consumption. For example, Harrison, Fulkerson, and Beebe (1997) surveyed large numbers of public school students in grades 6, 9, and 12 and found that physical and sexual abuse was associated with an increased chance of using cannabis for both boys and girls in all grades. Abuse victims were more likely to say that they used substances for multiple reasons including to escape from their problems and to cope with painful emotions. Other researchers found that homeless youth with a history of sexual abuse were more likely to use cannabis than those without sexual abuse histories (Rew, Taylor-Seehafer, & Fitzgerald, 2001). Kilpatrick, Acierno, Saunders, Resnick, Best, and Schnurr (2000) interviewed a large sample of adolescents about their substance abuse, victimization experiences, family substance use, and posttraumatic reactions and found that childhood abuse and witnessing violence increased the risk of developing a cannabis use disorder. Furthermore, having PTSD independently increased the risk of developing a cannabis use disorder. Widom, Marmorstein, and White (2006) found that when maltreated children were prospectively followed into middle adulthood, they were more likely to report cannabis use and use-related problems during the past year as compared to matched controls. In a series of studies conducted by Lipschitz and colleagues (Lipschitz, Rasmusson, Anyan, Cromwell, & Southwick, 2000; Lipschitz, Rasmusson, Anyan, Gueorguieva, Billingslea, Cromwell, & Southwick, 2003) young inner-city females (aged 12–21 years) presenting at a clinic for routine medical care were asked about trauma exposure, PTSD symptoms, and substance use. They reported exposure to a range of community and family-based traumas (e.g., witness homicide, threatened with a weapon, sexual and physical abuse), and those who developed full and partial PTSD reported greater cannabis use. Other researchers examined contributions to cannabis dependence in a large sample of young adult twins and found that child sexual abuse and parental separation were related to higher rates of cannabis dependence in women while parental conflict was associated with increased rates of cannabis dependence in men (Lynskey, Heath, Nelson, Bucholz, Madden, Slutske, Statham, & Martin, 2002). This group later found that childhood sexual abuse was associated with increased risk for subsequent cannabis use and, among users, cannabis abuse/dependence (Nelson, Heath, Lynskey, Bucholz, Madden, Statham, & Martin, 2006). Overall, these studies demonstrate a relationship between high intensity early life stress and cannabis consumption.
Adult victims of domestic violence, and particularly sexual violence, may also cope through cannabis use. Kalichman, Williams, Cherry, Belcher, and Nachimson (1988) surveyed women living in low-income housing and found that those who had engaged in unwanted sex because a male partner threatened or used force were more likely to use cannabis than those who were not sexually coerced. This finding was supported by Wingood, DiClemente, and Raj (2000) who examined a sample of women residing in domestic violence shelters and found that those who reported both partner sexual and physical abuse were more likely to use cannabis to cope with the abuse than those who reported physical abuse alone.
Combat trauma, including participation in wartime atrocities, has been associated with cannabis use. For example, Bremner, Southwick, Darnell, and Charney (1996) assessed the longitudinal course of PTSD symptoms and substance abuse in Vietnam combat veterans with chronic PTSD at various time points after the war. Their findings indicated that substance use increased in parallel with PTSD symptoms and that cannabis helped alleviate hyperarousal symptoms. Yager, Laufer, and Gallops (1984) interviewed Vietnam veterans 6 to 15 years following discharge from military service and found that those who participated in atrocities reported more stress symptoms and greater use of cannabis than did other veterans. Finally, Koenen, Lyons, Goldberg, Simpson, Williams, Toomey, Eisen, True, and Tsuang (2003) examined data collected from a large sample of male twin pairs who were members of the Vietnam Era Twin (VET) Registry and found that combat exposure adjusted for PTSD increased the risk for cannabis dependence. However, combat-related PTSD was not uniquely associated with an increased risk of cannabis dependence in this study.
Disaster trauma has also been associated with increased cannabis use. This is evidenced by a series of studies conducted on substance use increases following the September 11th terrorist attack. In an initial study, Vlahov, Galea, Resnick, Ahern, Boscarino, Bucuvalas, Gold, and Kilpatrick (2002) assessed increases in substance use among Manhattan residents (over age 17) five to eight weeks following the attack using a random-digit dial telephone survey. They found that among those surveyed, 3.2% reported an increase in cannabis use. Importantly, those who increased their cannabis use were more likely to experience PTSD and depression than those who did not. Next, Vlahov, Galea, Ahern, Resnick, and Kilpatrick (2004) compared reports of increased substance use in adult Manhattan residents one and six months after the September 11th terrorist attack using data from two random-digit-dial surveys. Their findings indicated that the proportion of respondents who increased their use of cigarettes, alcohol, and cannabis was 30.8% at the first time-point and 27.3% at the second time-point. Interestingly, while the prevalence of increased use declined for cigarettes and alcohol between the two time-points, it increased for cannabis. Finally, Schiff, Zweig, Benbenishty, and Hasin (2007) found that close physical exposure to terrorist acts predicted greater cannabis use among Israeli youth, even after controlling PTSD and depressive symptomatology.
It is important to note that not all studies have found an effect of trauma exposure and/or having a PTSD diagnosis on cannabis consumption or cannabis-related disorders. For example, Chilcoat and Breslau (1998) analyzed data from a longitudinal study of young adults (randomly selected from the membership list of a health maintenance organization in Michigan) and found that neither trauma exposure in the absence of PTSD nor having a PTSD diagnosis increased the specific risk for cannabis abuse or dependence. Sexual abuse was not found to be associated with cannabis use or use-related disorders in a recent prospective study (von Sydow et al., 2002). Koenen et al. (2003) found that while Vietnam combat exposure adjusted for PTSD increased the risk for cannabis dependence, combat-related PTSD was not uniquely associated with an increased risk of cannabis dependence. Finally, using prospective pre-disaster and post-disaster data, Reijneveld, Crone, Verhulst, and Verloove-Vanhorick (2003) analyzed the effects of a severe disaster (a fire in a café that killed 14 and wounded 250 adolescents) on the substance use of adolescents five months after the disaster and found that, while affected adolescents reported larger increases in excessive drinking than controls, they did not report more cannabis use. However, the authors of this study noted that the proportion of adolescents who were injured in the fire was larger in those lost to follow-up than in the analysis group, which suggests that the effects of the disaster may have been underestimated.
Overall, however, the majority of studies appear to support the contention that traumatic stress is associated with increased risk for cannabis use and misuse across adolescence and adulthood. Trauma may increase distress, render normal coping attempts ineffective, and lead to the initiation or escalation of cannabis use for stress-relief. Childhood trauma, especially within the home, may also lead to family estrangement and greater affiliation with deviant, drug using peers who encourage cannabis consumption.
Maladaptive Coping and Poor Self-Control
When facing a stressor, individuals who have difficulty solving problems or conflicts constructively (e.g., they avoid the problem or resort to physical or verbal aggression) may experience greater distress and be more likely to seek out substances for immediate stress relief (Unger, Sussman, & Dent, 2003; Wills & Hirky, 1996). Stress may also increase drug craving (Hyman, Fox, Hong, Doebrick, & Sinha, 2007; Sinha, 2001), and for those who are actively trying to refrain from using substances, expenditure of energy to control negative affect could result in a depletion of self-control strength needed to fight the urge to use substances (see Muraven & Baumeister, 2000).1 Those individuals with the most mature affect regulation skills would theoretically expend the least amount of energy to regulate affect and would best conserve resources necessary to resist substance use. Ultimately, deficient problem solving, conflict-resolution, and emotion regulation skills may all play a role in the initiation and perpetuation of substance use behavior. Investigators have found some support for this contention with regard to cannabis consumption.
Using a composite score for cigarette, alcohol, and cannabis use, Wills, Sandy, Yaeger, Cleary, and Shinar (2001) prospectively found that coping through disengagement (e.g., anger and avoidant coping) was related to higher initial levels of adolescent substance use as well as greater growth in use over time. Kaplan et al. (1986) conducted a longitudinal analysis to understand why some people become regular cannabis users while others only use occasionally. Their sample consisted of young adults who had used cannabis at least once in their lifetime and who provided data in the seventh grade and again as young adults. The results of their path analysis indicated that avoidance coping was associated with escalated cannabis use. Unger et al. (2003) examined the relationship between interpersonal conflict tactics and substance use among continuation high-school students and found that the use of physical aggression to handle interpersonal conflict was associated with a higher risk for cannabis use. Siqueira et al. (2001) found that, compared to adolescents who never used cannabis, frequent users and experimenters used more anger coping and less parental support coping. Eftekhari, Turner, and Larimer (2004) examined the relationships between anger expression and avoidant coping to cannabis use in incarcerated adolescents and found that outward expressions of anger (e.g., yelling, slamming doors) and avoidant coping were risk factors for greater frequency of cannabis use and more use-related consequences. Interestingly, higher levels of inwardly expressed anger (e.g., boiling inside) were related to lower levels of cannabis use. The authors suggested that those with higher levels of outwardly expressed anger may have less control over impulses than their peers or that angry acting out may reflect a more widespread pattern of problematic behavior that includes greater substance use. McCubbin, Needle, and Wilson (1985) found that adolescent boys’ efforts to express tensions and frustrations through getting angry, yelling, blaming others, and complaining was associated with greater cannabis use. Simons and Carey (2002) found that while affect lability was not associated with lifetime frequency of cannabis use in college students, it was associated with use-related problems. Wills and Stoolmiller (2002) followed a sample of young adolescents from 6th grade through 9th grade and found that good self-control (self-soothing, dependability, planning, and problem solving) deterred involvement in early substance use (using a composite score of cigarette, alcohol, and cannabis use frequency for analyses) whereas poor self-control (impatience, distractibility, & proneness to anger) was related to higher initial levels of substance use and greater rate of escalation of substance use over time. In a later study, Wills et al. (2006) reported that good behavioral control (planfulness, problem solving, cognitive effort, and self-reinforcement) and good emotional control (ability to self-soothe, ability to control and suppress anger and sadness) were inversely related to substance use (measured using a composite score for tobacco, alcohol, and cannabis) whereas poor behavioral control (impulsiveness, distractibility) and poor emotional control (anger reaction, anger rumination, sadness rumination, and negative affect lability) were positively associated with substance use. Furthermore, poor behavioral control was related to affiliation with deviant peers, and poor emotional control was related to coping motives for substance use.
Together, these studies demonstrate that maladaptive methods of solving problems and difficulties regulating affect may influence cannabis use outcomes. Coping through outward expressions of anger may push away sources of support that serve as buffers to stress. Coping in this manner may also lead to an increased number of stressful events at home, school, or work (e.g., they may result in school suspension or job loss). These negative events, in turn, can result in heightened distress and subsequent cannabis consumption for stress-relief. While coping through avoidance may provide a temporary escape from problems and associated distress, coping through avoidance does nothing to solve the problem at hand and can potentially result in further difficulties (i.e., avoiding a court appearance may provide a temporary escape but result in further legal action). Problems can then exacerbate as a result of avoidance coping and lead to greater distress and continued cannabis use for stress-relief. Difficulties regulating affect may further aggravate problems by making individuals more sensitive to stress and more impulsive (e.g., acting out aggressively; immediately seeking out drugs to cope) when faced with difficult life situations.
Stress & Affiliation with Deviant Peers: A Pathway to Poor Modeling & Cannabis Availability
The popularity of cannabis and the ease with which it can be obtained may increase its attraction both as a recreational drug and stress-coping mechanism. Indeed, cannabis is readily available to most high-school students and to about half of all 8th graders (Gruber & Pope, Jr., 2002). A recent study found that a significant number of pre-teenage children are also exposed to drugs and that the greatest of this exposure is to cannabis (McIntosh, Gannon, McKeganey, & MacDonald, 2003). As stated earlier, stress may predispose young adolescents to affiliate with deviant peers who encourage drug use as a primary social activity (Wills et al. 2006). Deviant peers often function as suppliers of drugs and act as social models for drug use behavior (Hundleby & Mercer, 1987) possibly even with respect to coping-related use. For instance, they may suggest that one smoke cannabis when faced with a stressor even though other coping responses would likely be more adaptive. Associating with such individuals can create a skewed view of cannabis use as normative and lead to increased social and coping-related use and a greater likelihood of developing dependence. Associating with cannabis-using peers may also increase one’s likelihood of experiencing additional negative life events (e.g., arrest, school suspension) which may further increase stress and perpetuate coping-related use of cannabis.
Stress, Cannabis Use & Decision Making Ability
Heavy cannabis users show deficits in decision making ability such that they are motivated more by immediate rewards than by adverse consequences and are slow to learn from their mistakes (Bolla, Eldreth, Matochik, & Cadet, 2005; Whitlow, Liguori, Livengood, Hart, Mussat-Whitlow, Lamborn, Laurienti, & Porrino, 2004). They also demonstrate abnormalities in prefrontal brain-regions involved in making decisions (Bolla et al., 2005). While these studies suggest that heavy cannabis use may lead to poor decision making and associated brain dysfunction, it is also possible that poor decision making associated alterations in brain function predate cannabis use and contribute to greater use over time (Bolla et al., 2005; Whitlow et al., 2004).
Support for the former hypothesis was provided by a recent within- subject repeated measures laboratory study (Lane, Cherek, Tcheremissine, Lieving, & Pietras, 2005) where occasional cannabis users (averaging 7.4 uses in the past 30 days) were given placebo cigarettes and three doses of cannabis cigarettes (half of 1.77%, 1.77%, and 3.58%) and tested using a risk-taking measure. Findings indicated that cannabis significantly increased risky responding, with the 3.58% THC dose having an effect greater than placebo. Overall, this study provided evidence that high doses of cannabis may have direct pharmacological effects on risky decision making and that it may influence decision making by altering one’s sensitivity to consequences (Lane et al., 2005). Consequently, poor decision making associated with acute cannabis intoxication may lead to an increased number of adverse life events (e.g., arrest, incarceration) which, in turn, can lead to greater distress and continued cannabis use for stress-relief.
Psychological stress may also negatively affect the quality of decisions people make (Fishbein et al. 2006; Keinan, 1987). One recent study found that the negative effect of stress on substance use (including cannabis) was mediated through alterations in adolescents’ ability to make and execute pro-social decisions (Fishbein et al. 2006). In all, both chronic cannabis use and stress may disrupt decision-making capabilities and place individuals at increased risk for ongoing cannabis use.
Effects of Cannabis on Brain Stress & Reward Systems
Up until now, we have primarily focused on cannabis use as a response to stress. However, it is also important to consider the profound effects that cannabis itself can have on brain stress and reward systems, which may serve to shift the motivation for cannabis use from positive reinforcing aspects of the drug to negative reinforcing effects. Thus with greater drug use, abstinence related symptoms may contribute to a negative affect state and perpetuate stress-related motivation for drug use (Koob & Le Moal, 1997; 2001). Furthermore, chronic drug use has been found to alter stress responses and enhance drug craving and negative emotions during laboratory induction of stress and alcohol/drug cue exposure in addicted individuals compared to controls (Sinha, 2001; Sinha et al., 2003; Fox et al., 2008; Sinha et al. 2008), measures that contribute to relapse factors in other groups of drug abusers including cocaine dependent (Sinha et al., 2006) and alcohol dependent (Adinoff et al., 2005; Junghanns et al., 2005) populations.
There is evidence that cannabis activates the hypothalamic-pituitary-adrenal (HPA) axis (Brown & Dobs, 2002). Brain imaging data has shown alterations in cortico-limbic circuits that are involved in stress and reward regulation in chronic cannabis users (Eldreth et al., 2004), and recent cannabis use has also been shown to decrease activation in the frontal cortex during emotional stress in cocaine dependent individuals (Li et al., 2005). Several studies have shown that cannabis intake activates the CRF-HPA axis both following acute administration of cannabinoid receptor agonists and THC in animals and in humans (D’Souza et al., 2004; Kumar and Chen, 1983; Puder et al., 1982; Martin-Calderon et al., 1998) as well as during withdrawal (de Fonseca, Carrera, Navarro, Koob, & Weiss, 1997). A study by Weidenfeld, Feldman, and Mechoulam, (1994) also showed that chronic cannabis exposure increased dose-dependent secretion of the stress hormones corticosterone and ACTH in rats. Another study indicated that increased Corticotropin-releasing hormone (CRH) mRNA expression in the rat central amydala may provide a possible mechanism for reported increased CFH release during withdrawal (Caberlotto, Rimondini, Hansson, Eriksson, & Heilig, 2004). Acute cannabis administration is also known to increase dopamine transmission in the nucleus accumbens (NAC) and mesolimbic reward systems via its action on central cannabinoid receptors (Cheer et al., 2004; Szabo et al., 1999) as well as increase prefrontal cortical catecholaminergic utilization function in rats (Jentsch et al., 1997). Many preclinical studies have also demonstrated the impact of cannabinoids on central noradrenergic function. Studies using synthetic cannabinoid agonists have shown that SR 141716A increases levels of norepinephrine in both the rat anterior hypothalamus and the frontal cortex (Tzavara et al., 2001; 2003). The cannabinoid receptor agonist WIN 55,212-2 has also been shown to dose-dependently increase the release of norepinephrine in the prefrontal region (Oropeza et al., 2005).
While there is a need to conduct more research in humans to support cannabis use related changes in stress responses, this line of research suggests that, in addition to being a response to stress, chronic cannabis consumption may impact brain development and sensitize individuals to the effects of subsequent life stressors. In effect, a vicious cycle may ensue with stress contributing as a risk factor to increase cannabis use and greater cannabis use altering brain stress and reward systems that enhance stress responses, decrease the capacity to cope with stress, and increase the salience of the drug and drug use behaviors (Sinha, 2001; 2005).
Conclusion
Numerous studies indicate that cannabis is commonly and consciously used as a stress-coping strategy. Stress-related factors including family dysfunction, negative life events, and traumatic stress are all associated with cannabis consumption. It appears that stressful life circumstances, especially those that occur early in life, may elevate distress, increase sensitivity to stress, and set individuals on a trajectory toward experimental cannabis use and a more severe course of addiction. Coping deficits that may develop from deficient care-giving and modeling of deviant peers may compound problems by reducing the coping-arsenal necessary to effectively overcome life stressors and modulate negative affect. In effect, cannabis use may be most likely in stress-vulnerable individuals as it supplies immediate stress-relief with relatively little effort. This is not to say that other factors do not influence cannabis use. Indeed, genetics may converge with psychosocial factors to influence cannabis consumption (Gruber & Pope, Jr., 2002; Lynskey et al., 2002).
While many people may be able to use cannabis socially and without consequence, there may be a subset of individuals who experience greater life stress, are more vulnerable to stress, and who may be more likely to use cannabis for stress-coping purposes. Importantly, these individuals may be at increased risk for earlier and heavier cannabis use and greater cannabis-related problems. This view is supported by a recent study that found that young adults who used cannabis primarily as a coping strategy had poorer mental health, greater pathology, more distress, and more life events than non-users whereas those with predominantly social reasons for use were not more distressed than non-users (Brodbeck, Matter, Page, & Moggi, 2007). Chronic cannabis use may further compound problems by altering brain stress and reward systems, thereby sensitizing individuals to the effects of stress. Together, these findings indicate that stress-coping focused interventions may be best applied if specifically targeted toward this subgroup of stress-vulnerable cannabis users.
A recent review indicated that cannabis dependence appears responsive to cognitive-behavioral, motivational enhancement, and contingency management interventions (McRae, Budney, & Brady, 2003). The literature we reviewed here suggests that enhanced cognitive-behavioral and pharmacological interventions specifically focused on reducing, planning for, tolerating, and coping appropriately with general life stress and traumatic stress may further improve treatment outcomes. Participation in stress-reducing activities outside of therapy, such as exercise and Yoga, may also be beneficial (Michalsen, Grossman, Acil, Langhorst, Ludtke, Esch, Stefano, & Dubos, 2005; Southwick et al., 2005; Tsatsoulis & Fountoulakis, 2006). However, given the varied reasons for cannabis use and misuse, the most effective prevention and interventions programs could benefit from incorporating stress-coping treatments with community and psychosocial interventions that enhance pleasurable activities, alter deviance-prone attitudes, and improve family, school, and social functioning. Harm reduction approaches focused on reducing the amount of cannabis ingested may also temper the stress-response, improve decision making capabilities, and lead to less aversive consequences. Reduced consequences, in turn, may translate to lower distress and less coping-related use of cannabis. Of course, randomized controlled trials are needed before any definitive conclusions or recommendations can be made.
Parents, teachers, and community and religious leaders should become more aware of the stressors children and adolescents face and implement strategies to prevent cannabis use. For instance, while childhood abuse is undoubtedly a stressful experience that necessitates immediate attention, social pressure may be a less obvious, but significant, form of stress to which adolescents must contend. The anxiety manifested in social pressure situations may lead to cannabis use as a stress-reduction strategy as well as a means to gain peer approval (Comeau, Stewart, & Loba, 2001). In all, early detection, intervention, and support for troubled adolescents may prevent experimental cannabis use and/or deter progression to problematic use (e.g., Butters, 2002). However, additional work is needed to understand the stress-related factors associated with the various stages of cannabis use and how to apply the findings to prevention and intervention programs. Further work is also needed to understand how chronic cannabis use influences brain-stress responding in humans.
A limitation of our review is that we specifically focused on stress, negative life events, and maladaptive coping as stress-related factors implicated in cannabis consumption. Viewing the problem from another perspective, positive life events and adaptive forms of coping may be protective. Indeed, positive affect has been associated with lower levels of substance use in prospective studies (Wills et al. 1999), and more research is needed to address how individuals can obtain and enhance pleasant emotions in an effort to prevent drug addiction (Labouvie, 1986).
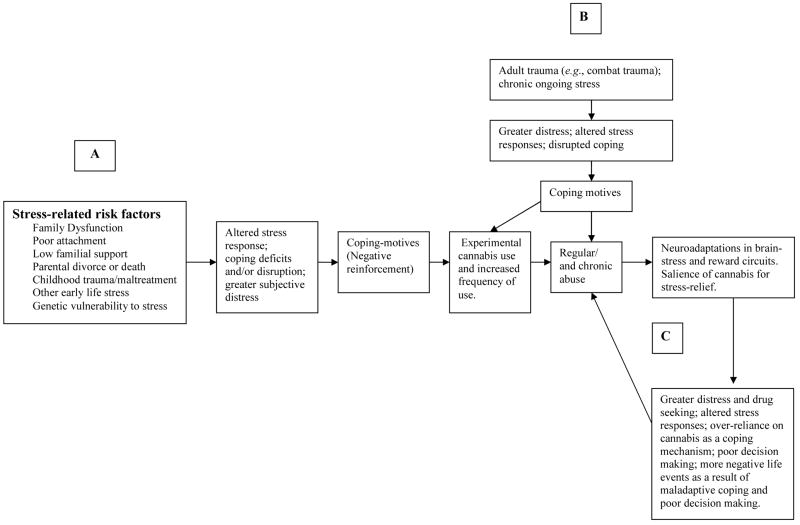
A schematic diagram depicting the vicious cycle by which stress increases the risk of experimental and chronic cannabis use and how alterations in brain stress and reward circuits resulting from chronic cannabis use perpetuates maladaptive stress responses and cannabis misuse. (A) Intense early life stress can alter the stress response, disrupt coping, increase distress, and lead to experimental and chronic cannabis use through coping motives (negative reinforcement). (B) Later trauma and other chronic life stressors can also alter the stress response, disrupt coping, increase distress and lead to experimental and chronic cannabis use through the same mechanism. (C) Neuroadaptations occurring in stress and reward circuits as a result of chronic cannabis use can promote maladaptive stress responding, thereby resulting in increased cannabis use for stress-coping purposes. Furthermore, chronic cannabis consumption can lead to decision making deficits and additional negative life events (e.g., arrest) which can further increase distress and perpetuate chronic cannabis consumption.
Acknowledgments
This research was supported by the National Institutes of Health (NIH) grants P50-DA16556 (RS) and K02-DA17232 (RS). The authors thank Raquel Andres-Hyman, Ph.D., Benjamin Toll, Ph.D., and Helen Fox, Ph.D. for their comments on an earlier draft of this manuscript.
Footnotes
1One theory postulates that refraining from engaging in a desired behavior such as cannabis consumption requires a considerable amount of effort and is not simply the product of inaction (Muraven & Baumeister, 2000). The strength needed to control behavior is depleted as various acts of self-control draw upon this limited energy source. Thus, after an initial difficult attempt at self-control (e.g., keeping oneself from crying or from lashing out in anger in response to a stressor), subsequent attempts at self control (e.g. refraining from cannabis use) should be more difficult and less likely to succeed. If circumstances such as chronic stress prevent adequate recuperation, individuals may become chronically deficient in resources needed for self-control. Thus, an adolescent, for example, who experiences ongoing family conflict and multiple problems at school, may spend a great deal of self-control strength to regulate negative affect. When later exposed to or pressured to use cannabis, this individual may have less self-control strength needed to refrain from use. The poorer an individual’s coping and affect regulation skills, the more distress he or she may feel when confronted with stressful situations. In effect, more strength may be needed to regulate associated negative affect, and less self-control strength may be available to resist urges or pressure to use cannabis in the future.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adinoff B, Junghanns K, Kiefer F, Krishnan-Sarin S. Suppression of the HPA axis stress-response: implications for relapse. Alcohol Clin Exp Res. 2005;29(7):1351–5. [Europe PMC free article] [Abstract] [Google Scholar]
- Baer PE, McLaughlin RJ, Burnside MA, Pokorny AD, Garmezy LB. Stress, family environment, and multiple substance use among seventh graders. Psychology of Addictive Behaviors. 1987;1(2):92–103. [Google Scholar]
- Barnes GE, Barnes MD, Patton D. Prevalence and predictors of “Heavy” marijuana use in a Canadian youth sample. Substance Use & Misuse. 2005;40:1849–1863. [Abstract] [Google Scholar]
- Bolla KI, Eldreth DA, Matochik JA, Cadet JL. Neural substrates of faulty decision-making in abstinent marijuana users. NeuroImage. 2005;26:480–492. [Abstract] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ, Bernstein A. Marijuana use motives: Concurrent relations to frequency of past 30-day use and anxiety sensitivity among young adult marijuana smokers. Addictive Behaviors. 2007;32:49–62. [Abstract] [Google Scholar]
- Boys A, Marsden J, Griffiths P, Fountain J, Stillwell G, Strang J. Substance use among young people: the relationship between perceived functions and intentions. Addiction. 1999;94(7):1043–1050. [Abstract] [Google Scholar]
- Boys A, Marsden J, Strang J. Understanding reasons for drug use amongst young people: a functional perspective. Health Education Research. 2001;16(4):457–469. [Abstract] [Google Scholar]
- Bremner DJ, Southwick SM, Darnell A, Charney DS. Chronic PTSD in Vietnam Combat Veterans: Course of Illness and Substance Abuse. The American Journal of Psychiatry. 1996;153(3):369–375. [Abstract] [Google Scholar]
- Brodbeck J, Matter M, Page J, Moggi F. Motives for cannabis use as a moderator variable of distress among young adults. Addictive Behaviors. 2007;32(8):1537–1545. [Abstract] [Google Scholar]
- Brown TT, Dobs AS. Endocrine effects of marijuana. Journal of Clinical Pharmacology. 2002;42:90S–96S. [Abstract] [Google Scholar]
- Budney AJ, Moore BA, Vandrey RG, Hughes JR. The time course and significance of cannabis withdrawal. Journal of Abnormal Psychology. 2003;112(3):393–402. [Abstract] [Google Scholar]
- Budney AJ, Novy PL, Hughes JR. Marijuana withdrawal among adults seeking treatment for marijuana dependence. Addiction. 1999;94:1311–1321. [Abstract] [Google Scholar]
- Bugental DB. Thriving in the face of early adversity. Journal of Social issues. 2004;60(1):219–235. [Google Scholar]
- Butters JE. Family stressors and adolescent cannabis use: a pathway to problem use. Journal of Adolescence. 2002;25:645–654. [Abstract] [Google Scholar]
- Caberlotto L, Rimondini R, Hansson A, Eriksson S, Heilig M. Corticotropin-releasing hormone (CRH) mRNA expression in rat central amygdale in cannabinoid tolerance and withdrawal: evidence for an allostatic shift? Neuropsychopharmacology. 2004;29(1):15–22. [Abstract] [Google Scholar]
- Chabrol H, Massot E, Mullet E. Factor structure of cannabis related beliefs in adolescents. Addictive Behaviors. 2004;29:929–933. [Abstract] [Google Scholar]
- Cheer JF, Wassum KM, Heien ML, Phillips PE, Wightman RM. Cannabinoids enhance subsecond dopamine release in the nucleus accumbens of awake rats. Journal of Neuroscience. 2004;24(18):4393–400. [Abstract] [Google Scholar]
- Chilcoat HD, Breslau N. Posttraumatic stress disorder and drug disorders: Testing causal pathways. Archives of General Psychiatry. 1998;55:913–917. [Abstract] [Google Scholar]
- Cicchetti D, Toth SL. Child maltreatment. Annual Review of Clinical Psychology. 2005;1:409–438. [Abstract] [Google Scholar]
- Copeland J, Swift W, Rees V. Clinical profile of participants in a brief intervention program for cannabis use disorder. Journal of Substance Abuse Treatment. 2001;20:45–52. [Abstract] [Google Scholar]
- Comeau N, Stewart SH, Loba P. The relations of trait anxiety, anxiety sensitivity, and sensation seeking to adolescents’ motivations for alcohol, cigarette, and marijuana use. Addictive Behaviors. 2001;26:803–825. [Abstract] [Google Scholar]
- Crutchfield RD, Gove WR. Determinants of drug use: A test of the coping hypothesis. Soc Sci Med. 1984;18(6):503–509. [Abstract] [Google Scholar]
- DeBellis MD. Developmental traumatology: a contributory mechanism for alcohol and substance use disorders. Psychoneuroendocrinology. 2002;27:155–170. [Abstract] [Google Scholar]
- de Fonseca FR, Carrera MRA, Navarro M, Koob GF, Weiss F. Activation of corticotrophin-releasing factor in the limbic system during cannabinoid withdrawal. Science. 1997;276:2050–2054. [Abstract] [Google Scholar]
- Dennis M, Babor TF, Roebuck MC, Donaldson J. Changing the focus: the case for recognizing and treating cannabis use disorders. Addiction. 2002;97(Suppl 1):4–15. [Abstract] [Google Scholar]
- Degenhardt L, Hall W. Is cannabis use a contributory cause of psychosis? Canadian Journal of Psychiatry. 2006;51(9):556–565. [Abstract] [Google Scholar]
- D’Souza D, Perry E, MacDougall L, Ammerman Y, Cooper TB, Wu YT, et al. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology. 2004;29:1558–1572. [Abstract] [Google Scholar]
- Eftekhari A, Turner AP, Larimer ME. Anger expression, coping, and substance use in adolescent offenders. Addictive Behaviors. 2004;29:1001–1008. [Abstract] [Google Scholar]
- Eldreth DA, Matochik JA, Cadet JL, Bolla KI. Abnormal brain activity in prefrontal brain regions in abstinent marijuana users. Neuroimage. 2004;23(3):914–20. [Abstract] [Google Scholar]
- Fergusson DM, Horwood LJ. Early onset cannabis use and psychosocial adjustment in young adults. Addiction. 1997;92(3):279–296. [Abstract] [Google Scholar]
- Fergusson DM, Horwoord LJ. Does cannabis use encourage other forms of illicit drug use? Addiction. 2000;95(4):505–520. [Abstract] [Google Scholar]
- Fergusson DM, Horwood LJ, Swain-Campbell NS. Cannabis use and psychosocial adjustment in adolescence and young adulthood. Addiction. 2002;97:1123–1135. [Abstract] [Google Scholar]
- Fishbein DH, et al. Mediators of the Stress-Substance-Use Relationship in Urban Male Adolescents. Prevention Science. 2006;7(2):113–126. [Abstract] [Google Scholar]
- Fox HC, Hong KA, Siedlarz K, Sinha R. Enhanced sensitivity to stress and drug/alcohol craving in abstinent cocaine dependent individuals compared to social drinkers. Neuropsychopharmacology. 2008;33(4):796–805. [Europe PMC free article] [Abstract] [Google Scholar]
- Glaser J, Os Jv, Portegijs PJM, Myin-Germeys I. Childhood trauma and emotional reactivity to daily life stress in adult frequent attenders of general practitioners. Journal of Psychosomatic Research. 2006;61:229–236. [Abstract] [Google Scholar]
- Gledhill-Hoyt J, Lee H, Strote J, Wechsler H. Increased use of marijuana and other illicit drugs at US colleges in the 1990s: results of three national surveys. Addiction. 2000;95(11):1655–1667. [Abstract] [Google Scholar]
- Goeders NE. The impact of stress on addiction. European Neuropsychopharmacology. 2003;13:435–441. [Abstract] [Google Scholar]
- Goeders NE. Stress, motivation, and drug addiction. Current Directions in Psychological Science. 2004;13(1):33–35. [Google Scholar]
- Gold SN. Not trauma alone: Therapy for child abuse survivors in family and social context. Lillington, NC: Taylor & Francis; 2000. [Google Scholar]
- Gold SN, Hyman SM, Andres-Hyman RC. Family of origin environments in two clinical samples of survivors of intra-familial, extra-familial, and both types of sexual abuse. Child Abuse & Neglect. 2004;28:1199–1212. [Abstract] [Google Scholar]
- Green B, Kavanagh D, Young R. Being stoned: a review of self-reported cannabis effects. Drug and Alcohol Review. 2003;22:453–460. [Abstract] [Google Scholar]
- Green B, Kavanagh DJ, Young R. Reasons for cannabis use in men with and without psychosis. Drug and Alcohol Review. 2004;23:445–453. [Abstract] [Google Scholar]
- Gruber AJ, Pope HG., Jr Marijuana use among adolescents. The Pediatric Clinics of North America. 2002;49:389–413. [Abstract] [Google Scholar]
- Hall W, Babor TF. Cannabis use and public health: assessing the burden. Addiction. 2000;95(4):485–490. [Abstract] [Google Scholar]
- Harkness KL, Bruce AE, Lumley MN. The role of childhood abuse and neglect in the sensitization to stressful life events in adolescent depression. Journal of Abnormal Psychology. 2006;115(4):730–741. [Abstract] [Google Scholar]
- Harrison PA, Fulkerson JA, Beebe TJ. Multiple substance use among adolescent physical and sexual abuse victims. Child Abuse & Neglect. 1997;21(6):529–539. [Abstract] [Google Scholar]
- Hathaway AD. Cannabis effects and dependency concerns in long-term frequent users: A missing piece of the public health puzzle. Addiction Research and Theory. 2003;11(6):441–458. [Google Scholar]
- Hayatbakhsh MR, Najman JM, Jamrozik K, Mamun AA, Alati R. Do parents’ marital circumstances predict young adults’ DSM-IV cannabis use disorders? A prospective study. Addiction. 2006;101:1778–1786. [Abstract] [Google Scholar]
- Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: Preclinical and clinical studies. Biological Psychiatry. 2001;49:1023–1039. [Abstract] [Google Scholar]
- Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, Miller AH, Nemeroff CB. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA. 2000;284(5):592–597. [Abstract] [Google Scholar]
- Hein D, Cohen L, Campbell A. Is traumatic stress a vulnerability factor for women with substance use disorders? Clinical Psychology Review. 2005;25:813–823. [Europe PMC free article] [Abstract] [Google Scholar]
- Hendlin H, Haas AP. The adaptive significance of chronic marijuana use for adolescents and adults. Advances in Alcohol and Substance Abuse. 1985;4(3–4):99–115. [Abstract] [Google Scholar]
- Hubbard JR, Franco SE, Onaivi ES. Marijuana: Medical implications. American Family Physician. 1999;60(9):2583–2588. [Abstract] [Google Scholar]
- Hundleby JD, Mercer GW. Family and friends as social environments and their relationship to young adolescents’ use of alcohol, tobacco, and marijuana. Journal of Marriage and the Family. 1987;49:151–164. [Google Scholar]
- Hyman SM, Fox H, Hong K, Doebrick C, Sinha R. Stress and drug-cue induced craving in opioid dependent individuals in naltrexone treatment. Experimental & Clinical Psychopharmacology. 2007;15(2):134–143. [Europe PMC free article] [Abstract] [Google Scholar]
- Jentsch JD, Andrusiak E, Tran A, Bowers MB, Jr, Roth RH. Delta 9-tetrahydrocannabinol increases prefrontal cortical catecholaminergic utilization and impairs spatial working memory in the rat: blockade of dopaminergic effects with HA966. Neuropsychopharmacology. 1997;16(6):426–32. [Abstract] [Google Scholar]
- Johnston LD, O’Malley PM. Why do the nations’s students use drugs and alcohol? Self-reported reasons from nine national surveys. The Journal of Drug Issues. 1986;16(1):29–66. [Google Scholar]
- Junghanns K, Tietz U, Dibbelt L, Kuether M, Jurth R, Ehrenthal D, Blank S, Backhaus J. Attenuated salivary cortisol secretion under cue exposure is associated with early relapse. Alcohol and Alcoholism. 2005;40(1):80–85. [Abstract] [Google Scholar]
- Kalichman SC, Williams EA, Cherry C, Belcher L, Nachimson D. Sexual coercion, domestic violence, and negotiating condom use among low-income African American women. Journal of Women’s Health. 1998;7(3):371–378. [Abstract] [Google Scholar]
- Kandel DB. Does marijuana use cause the use of other drugs? JAMA. 2003;289(4):482–483. [Abstract] [Google Scholar]
- Kaplan HB, Martin SS, Johnson RJ, Robbins CA. Escalation of marijuana use: Application of a general theory of deviant behavior. Journal of Health and Social Behavior. 1986;27:44–61. [Abstract] [Google Scholar]
- Keinan G. Decision making under stress: Scanning of alternatives under controllable and uncontrollable threats. Journal of Personality and Social Psychology. 1987;52(3):639–644. [Abstract] [Google Scholar]
- Khalsa JH, Genser S, Francis H, Martin B. Clinical consequences of marijuana. Journal of Clinical Pharmacology. 2002;42(11 Suppl):7s–10s. [Abstract] [Google Scholar]
- Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology. 2000;68(1):19–30. [Abstract] [Google Scholar]
- Koenen KC, Lyons MJ, Goldberg J, Simpson J, Williams WM, Toomey R, Eisen SA, True W, Tsuang MT. Co-twin control study of relationships among combat exposure, combat-related PTSD, and other mental disorders. Journal of Traumatic Stress. 2003;16(5):433–438. [Abstract] [Google Scholar]
- Koob GF, Le Moal M. Drug abuse: hedonic homeostatic dysregulation. Science. 1997;278(5335):52–8. [Abstract] [Google Scholar]
- Koob GF, Le Moal M. Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology. 2001;24(2):97–129. [Abstract] [Google Scholar]
- Kumar MS, Chen CL. Effect of an acute dose of delta 9-THC on hypothalamic lutenizing hormone releasing hormone and met-enkephalin content and serum levels of testosterone and corticosterone in rats. Subst Alcohol Actions Misuse. 1983;4:37–43. [Abstract] [Google Scholar]
- Labouvie EW. Alcohol and marijuana use in relation to adolescent stress. The International Journal of the Addictions. 1986;21(3):335–345. [Abstract] [Google Scholar]
- Lane SD, Cherek DR, Tcheremissine OV, Lieving LM, Pietras CJ. Acute marijuana effects on human risk taking. Neuropsychopharmacology. 2005;30:800–809. [Abstract] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer; New York: 1984. [Google Scholar]
- Lee CM, Neighbors C, Woods BA. Marijuana motives: Young adults’ reasons for using marijuana. Addictive Behaviors. 2007;32(7):1384–1394. [Europe PMC free article] [Abstract] [Google Scholar]
- Li CS, Milivojevic V, Constable RT, Sinha R. Recent cannabis abuse decreased stress-induced BOLD signals in the frontal and cingulate cortices of cocaine dependent individuals. Psychiatry Res. 2005;140(3):271–80. [Abstract] [Google Scholar]
- Lipschitz DS, Rasmusson AM, Anyan W, Cromwell P, Southwick SM. Clinical and functional correlates of posttraumatic stress disorder in urban adolescent girls at a primary care clinic. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(9):1104–1111. [Abstract] [Google Scholar]
- Lipschitz DS, Rasmusson AM, Anyan W, Gueorguieva R, Billingslea EM, Cromwell PF, Southwick SM. Posttraumatic stress disorder and substance use in inner-city adolescent girls. The Journal of Nervous and Mental Disease. 2003;191(11):714–721. [Abstract] [Google Scholar]
- Lynskey MT, Heath AC, Bucholz KK, Slutske WS, Madden PAF, Nelson EC, Statham DJ, Martin NG. Escalation of drug use in early-onset cannabis users vs co-twin controls. JAMA. 2003;289(4):427–433. [Abstract] [Google Scholar]
- Lynskey MT, Heath AC, Nelson EC, Bucholz KK, Madden PAF, Slutske WS, Statham DJ, Martin NG. Genetic and environmental contributions to cannabis dependence in a national young adult twin sample. Psychological Medicine. 2002;32:195–207. [Abstract] [Google Scholar]
- Martin-Calderon JL, Munoz RM, Villanua MA, del Arco I, Moreno JL, de Fonseca FR, Navarro M. Characterization of the acute endocrine actions of (-)-11-hydroxy-delta8-tetrahydrocannabinol-dimethylheptyl (HU-210), a potent synthetic cannabinoid in rats. European Journal of Pharmacology. 1998;344(1):77–86. [Abstract] [Google Scholar]
- McArdle PA. Cannabis use by children and young people. Arch Dis Child. 2006;91:692–695. [Europe PMC free article] [Abstract] [Google Scholar]
- McCubbin HI, Needle RH, Wilson M. Adolescent health risk behaviors: Family stress and adolescent coping as critical factors. Family Relations. 1985;34:51–62. [Google Scholar]
- McGee R, Williams S, Poulton R, Moffitt T. A longitudinal study of cannabis use and mental health from adolescence to early adulthood. Addiction. 2000;95(4):491–503. [Abstract] [Google Scholar]
- McIntosh J, Gannon M, McKeganey N, MacDonald F. Exposure to drugs among pre-teenage schoolchildren. Addiction. 2003;98:1615–1623. [Abstract] [Google Scholar]
- McKay JR, Murphy RT, McGuire J, Rivinus TR, Maisto SA. Incarcerated adolescents’ attributions for drug and alcohol use. Addictive Behaviors. 1992;17:227–235. [Abstract] [Google Scholar]
- McRae AL, Budney AJ, Brady KT. Treatment of marijuana dependence: a review of the literature. Journal of Substance Abuse Treatment. 2003;24:369–376. [Abstract] [Google Scholar]
- Michalsen A, Grossman P, Scil A, Langhorst J, Ludtke R, Esch T, Stefano GB, Dobos GJ. Rapid stress reduction and anxiolysis among distressed women as a consequence of a three-month intensive yoga program. Med Sci Monit. 2005;11(12):CR555–561. [Abstract] [Google Scholar]
- Muraven M, Baumeister RF. Self –regulation and depletion of limited resources: Does self-control resemble a muscle? . Psychological Bulletin. 2000;126(2):247–259. [Abstract] [Google Scholar]
- Nelson EC, Heath AC, Lynskey MT, Bucholz KK, Madden PAF, Statham DJ, Martin NG. Childhood sexual abuse and risks for licit and illicit drug-related outcomes: a twin study. Psychological Medicine. 2006;36(10):1473–1483. [Abstract] [Google Scholar]
- Office of National Drug Control Policy. Marijuana Myths and Facts: The Truth Behind 10 Popular Misperceptions 2004 [Google Scholar]
- Oropeza VC, Page ME, Van Bockstaele EJ. Systemic administration of WIN 55,212-2 increases norepinephrine release in the rat frontal cortex. Brain Res. 2005;1046(1–2):45–54. [Abstract] [Google Scholar]
- Puder M, Weidenfeld J, Chowers I, Nir I, Conforti N, Siegel RA. Corticotrophin and corticosterone secretion following delta 1-Tetrahhydrocannabinol in intact and in hypothalamic deafferentated male rats. Exp Brain Res. 1982;46(1):85–88. [Abstract] [Google Scholar]
- Reijneveld SA, Crone MR, Verhulst FC, Verloove-Vanhorick SP. The effect of a severe disaster on the mental health of adolescents: a controlled study. The Lancet. 2003;362:691–696. [Abstract] [Google Scholar]
- Reilly D, Didcott P, Swift W, Hall W. Long-term cannabis use: characteristics of users in an Australian rural area. Addiction. 1998;93(6):837–846. [Abstract] [Google Scholar]
- Rew L, Taylor-Seehafer M, Fitzgerald ML. Sexual abuse, alcohol and other drug use, and suicidal behaviors in homeless adolescents. Issues in Comprehensive Pediatric Nursing. 2001;24:225–240. [Abstract] [Google Scholar]
- Schafer J, Brown SA. Marijuana and cocaine effect expectancies and drug use patterns. Journal of Consulting and Clinical Psychology. 1991;59(4):558–565. [Abstract] [Google Scholar]
- Schiff M, Zweig HH, Benbenishty R, Hasin DS. Exposure to terrorism and Israeli youths’ cigarette, alcohol, and cannabis use. American Journal of Public Health. 2007;97(10):1852–1858. [Abstract] [Google Scholar]
- Segal B, Cromer F, Hobfoll SS, Wasserman PZ. Patterns of reasons for drug use among detained and adjudicated juveniles. The International Journal of the Addictions. 1982;17(7):1117–1130. [Abstract] [Google Scholar]
- Simons JS, Carey KB. Risk and vulnerability for marijuana use problems: The role of affect dysregulation. Psychology of Addictive Behaviors. 2002;16(1):72–75. [Abstract] [Google Scholar]
- Simons J, Correia CJ, Carey KB, Borsari BE. Validating a five-factor marijuana motives measure: Relations with use, problems, and alcohol motives. Journal of Counseling Psychology. 1998;45(3):265–273. [Google Scholar]
- Simons J, Correia CJ, Carey KB. A comparison of motives for marijuana and alcohol use among experienced users. Addictive Behaviors. 2000;25(1):153–160. [Abstract] [Google Scholar]
- Simons JS, Gaher RM, Correia CJ, Hansen CL, Christopher MS. An affective-motivational model of marijuana and alcohol problems among college students. Psychology of Addictive Behaviors. 2005;19(3):326–334. [Abstract] [Google Scholar]
- Sinha R. How does stress increase risk of drug abuse and relapse. Psychopharmacology. 2001;158(4):343–359. [Abstract] [Google Scholar]
- Sinha R. Stress and Drug Abuse. In: Steckler T, Kalin N, Reul JMHM, editors. Handbook on Stress and the Brain: Part 2: Stress: Integrative and Clinical Aspects. Elsevier Science; Amsterdam: 2005. pp. 333–356. [Google Scholar]
- Sinha R, Fox HC, Hong KA, Bergquist K, Bhagwagar Z, Siedlarz K. Enhanced negative emotion and alcohol craving and altered physiological responses to stress and alcohol cues in alcohol dependent individuals. Neuropsychopharmacology. 2008 (epub online) [Europe PMC free article] [Abstract] [Google Scholar]
- Sinha R, Garcia M, Paliwal P, Kreek MJ, Rounsaville BJ. Stress-induced cocaine craving and hypothalamic-pituitary-adrenal responses are predictive of cocaine relapse outcomes. Arch Gen Psychiatry. 2006;63(3):324–31. [Abstract] [Google Scholar]
- Sinha R, Talih M, Malison R, Cooney N, Anderson GM, Kreek MJ. Hypothalamic-pituitary-adrenal axis and sympatho-adreno-medullary responses during stress-induced and drug cue-induced cocaine craving states. Psychopharmacology (Berl) 2003;170:62–72. [Abstract] [Google Scholar]
- Siqueira L, Diab M, Bodian C, Rolnitzky L. The relationship of stress and coping methods to adolescent marijuana use. Substance Abuse. 2001;22(3):157–166. [Abstract] [Google Scholar]
- Southwick SM, Vythilingam M, Charney DS. The psychobiology of depression and resilience to stress: Implications for prevention and treatment. Annual Review of Clinical Psychology. 2005;1:255–291. [Abstract] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2002 National Survey on Drug Use and Health: National Findings (NHSDA Series H-22, DHHS Publication No. SMA 03–3836) Office of Applied Studies; Rockville, MD: 2003. [Google Scholar]
- Szabo B, Muller T, Koch H. Effects of cannabinoids on dopamine release in the corpus striatum and the nucleus accumbens in vitro. J Neurochem. 1999;73(3):1084–9. [Abstract] [Google Scholar]
- Turner RJ, Lloyd DA. Cumulative adversity and drug dependence in young adults: racial/ethnic contrasts. Addiction. 2003;98:305–315. [Abstract] [Google Scholar]
- Tsatsoulis A, Fountoulakis S. The protective role of exercise on stress system dysregulation and comorbidities. Ann NY Acad Sci. 2006;1083:196–213. [Abstract] [Google Scholar]
- Tschann JM, Adler NE, Irwin CE, Millstein SG, Turner RA, Kegeles SM. Initiation of substance use in early adolescence: The roles of pubertal timing and emotional distress. Health Psychology. 1994;13:326–333. [Abstract] [Google Scholar]
- Tzavara ET, Perry KW, Rodriguez DE, Bymaster FP, Nomikos GG. The cannabinoid CB(1) receptor antagonist SR141716A increases norepinephrine outflow in the rat anterior hypothalamus. Eur J Pharmacol. 2001;426(3):R3–4. [Abstract] [Google Scholar]
- Tzavara ET, Wade M, Nomikos GG. Biphasic effects of cannabinoids on acetylcholine release in the hippocampus: site and mechanism of action. J Neurosci. 2003;23(28):9374–84. [Abstract] [Google Scholar]
- Unger JB, Sussman S, Dent CW. Interpersonal conflict tactics and substance use among high-risk adolescents. Addictive Behaviors. 2003;28:979–987. [Abstract] [Google Scholar]
- Van den Bree MBM, Pickworth WB. Risk factors predicting changes in marijuana involvement in teenagers. Archives of General Psychiatry. 2005;62:311–319. [Abstract] [Google Scholar]
- Vlahov D, Galea S, Ahern J, Resnick H, Kilpatrick D. Sustained increased consumption of cigarettes, alcohol, and marijuana among Manhattan residents after September 11, 2001. American Journal of Public Health. 2004;94(2):253–254. [Abstract] [Google Scholar]
- Vlahov D, Galea S, Resnick H, Ahern J, Boscarino JA, Bucuvalas M, Gold J, Kilpatrick D. Increased use of cigarettes, alcohol, and marijuana among Manhattan, New York, residents after the September 11thterrorist attacks. American Journal of Epidemiology. 2002;155(11):988–996. [Abstract] [Google Scholar]
- von Sydow K, Lieb R, Pfister H, Hofler M, Wittchen H. What predicts incident use of cannabis and progression to abuse and dependence? A 4-year prospective examination of risk factors in a community sample of adolescents and young adults. Drug and Alcohol Dependence. 2002;68:49–64. [Abstract] [Google Scholar]
- Weidenfeld J, Feldman S, Mechoulam R. Effect of the brain constituent anandamide, a cannabinoid receptor agonist, on the hypothalamo-pituitary-adrenal axis in the rat. Neuroendocrinology. 1994;59(2):110–112. [Abstract] [Google Scholar]
- Whitlow, et al. Long-term heavy marijuana users make costly decisions on a gambling task. Drug and Alcohol Dependence. 2004;76:107–111. [Abstract] [Google Scholar]
- Widom CS, Marmorstein NR, White HE. Childhood victimization and illicit drug use in middle adulthood. Psychology of Addictive Behaviors. 2006;20(4):394–403. [Abstract] [Google Scholar]
- Wills TA. Stress and coping factors in the epidemiology of substance use. In: Kozlowski, et al., editors. Research Advances in Alcohol and Drug Problems. Vol. 10. New York: Plenum Press; 1990. pp. 215–250. [Google Scholar]
- Wills TA, Hirky AE. Coping and substance abuse: A theoretical model and review of the evidence. In: Zeichnec M, Eudler NS, editors. Handbook of Coping: Theory, research, and applications. New York: Wiley; 1996. pp. 279–302. [Google Scholar]
- Wills TA, Sandy JM, Shinar O, Yaeger A. Contributions of positive and negative affect to adolescent substance use: Test of a bi-dimensional model in a longitudinal study. Psychology of Addictive Behaviors. 1999;13(4):327–338. [Google Scholar]
- Wills TA, Sandy JM, Yaeger AM, Cleary SD, Shinar O. Coping dimensions, life stress, and adolescent substance use: A latent growth analysis. Journal of Abnormal Psychology. 2001;110(2):309–323. [Abstract] [Google Scholar]
- Wills TA, Stoolmiller M. The role of self-control in early escalation of substance use: A time-varying analysis. Journal of Consulting and Clinical Psychology. 2002;70(4):986–997. [Abstract] [Google Scholar]
- Wills TA, Walker C, Mendoza D, Ainette MG. Behavioral and emotional self-control: Relations to substance use in samples of middle and high school students. Psychology of Addictive Behaviors. 2006;20(3):265–278. [Abstract] [Google Scholar]
- Windle M, Wiesner M. Trajectories of marijuana use from adolescence to young adulthood: Predictors and outcomes. Development and Psychopathology. 2004;16:1007–1027. [Abstract] [Google Scholar]
- Wingood GM, DiClemente RJ, Raj A. Adverse consequences of intimate partner abuse among women in non-urban domestic violence shelters. American Journal of Preventative Medicine. 2000;19(4):270–275. [Abstract] [Google Scholar]
- Yager T, Laufer R, Gallops M. Some problems associated with war experience in men of the Vietnam generation. Archives of General Psychiatry. 1984;41(4):327–333. [Abstract] [Google Scholar]
- Zimmer L, Morgan JP. Marijuana Myths Marijuana Facts: A Review of the Scientific Evidence. New York: The Lindesmith Centre; 1997. [Google Scholar]
Full text links
Read article at publisher's site: https://doi.org/10.1016/j.jsat.2008.08.005
Read article for free, from open access legal sources, via Unpaywall:
https://europepmc.org/articles/pmc2696937?pdf=render
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1016/j.jsat.2008.08.005
Article citations
Directional associations between posttraumatic stress disorder symptoms and cannabis use in young adults: Uncovering variation by sex, race, and ethnicity.
Psychol Addict Behav, 37(8):1052-1065, 01 Dec 2023
Cited by: 0 articles | PMID: 38108802
A pilot trial of a brief intervention for cannabis use supplemented with a substance-free activity session or relaxation training.
Psychol Addict Behav, 38(3):255-268, 25 Jan 2024
Cited by: 0 articles | PMID: 38271079
Neural correlates of negative life events and their relationships with alcohol and cannabis use initiation.
Dialogues Clin Neurosci, 25(1):112-121, 02 Nov 2023
Cited by: 1 article | PMID: 37916739 | PMCID: PMC10623894
Mental and Physical Health-Related Cannabis Motives Mediate the Relationship between Childhood Trauma and Problematic Cannabis Use over Time among Emerging Adult Cannabis Users.
Subst Use Misuse, 59(2):193-207, 28 Dec 2023
Cited by: 0 articles | PMID: 37822106
"I've smoked weed with my daughter": Cannabis Use within Families Affected by Parental Opioid Misuse.
Child Youth Serv Rev, 155:107235, 15 Oct 2023
Cited by: 0 articles | PMID: 37982095
Go to all (131) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Symptoms of obsessive-compulsive disorder predict cannabis misuse.
Addict Behav, 72:159-164, 31 Mar 2017
Cited by: 11 articles | PMID: 28453999
The association between distress tolerance and cannabis use-related problems: the mediating and moderating roles of coping motives and gender.
Addict Behav, 37(10):1181-1184, 02 Jun 2012
Cited by: 70 articles | PMID: 22698896
[Motivations for cannabis cessation, coping and adaptation strategies, and perceived benefits: impact on cannabis use relapse and abstinence].
Encephale, 39(6):385-392, 05 Aug 2013
Cited by: 4 articles | PMID: 23928064
Cannabis abuse and addiction: a contemporary literature review.
Niger J Med, 18(2):128-133, 01 Apr 2009
Cited by: 4 articles | PMID: 19630315
Review
Funding
Funders who supported this work.
NIDA NIH HHS (8)
Grant ID: K02 DA017232-01
Grant ID: P50 DA016556
Grant ID: PL1 DA024859-02
Grant ID: K02 DA017232
Grant ID: K02-DA17232
Grant ID: P50 DA016556-01
Grant ID: P50-DA16556
Grant ID: PL1 DA024859
National Institutes of Health (2)
Grant ID: K02-DA17232
Grant ID: P50-DA16556





