Abstract
Free full text

Human IL-3/GM-CSF knock-in mice support human alveolar macrophage development and human immune responses in the lung
Associated Data
Abstract
Mice with a functional human immune system have the potential to allow in vivo studies of human infectious diseases and to enable vaccine testing. To this end, mice need to fully support the development of human immune cells, allow infection with human pathogens, and be capable of mounting effective human immune responses. A major limitation of humanized mice is the poor development and function of human myeloid cells and the absence of human immune responses at mucosal surfaces, such as the lung. To overcome this, we generated human IL-3/GM-CSF knock-in (hIL-3/GM-CSF KI) mice. These mice faithfully expressed human GM-CSF and IL-3 and developed pulmonary alveolar proteinosis because of elimination of mouse GM-CSF. We demonstrate that hIL-3/GM-CSF KI mice engrafted with human CD34+ hematopoietic cells had improved human myeloid cell reconstitution in the lung. In particular, hIL-3/GM-CSF KI mice supported the development of human alveolar macrophages that partially rescued the pulmonary alveolar proteinosis syndrome. Moreover, human alveolar macrophages mounted correlates of a human innate immune response against influenza virus. The hIL-3/GM-CSF KI mice represent a unique mouse model that permits the study of human mucosal immune responses to lung pathogens.
Mice with components of the human immune system hold great promise for studying the human immune system in vivo and for proof-of-concept testing in vaccine and drug development (1–4). Human immune-system mice are generated by transplantation of a severely immunodeficient mouse strain [such as Rag2 KO IL-2R gamma (Il2rg) KO mice] with human hematopoietic stem and progenitor cells (5–10). Compared with nonhuman primates, human immune-system mice have the advantages of a small animal model: that is, they allow more versatile experimentation, are more accessible to the research community, and are ethically less debatable. Most importantly, experimental findings derived from these mice might be more relevant and applicable to humans as infection with human-specific pathogens and the study of human-specific immune responses are now becoming feasible (6, 11). Although much progress has been made in recent years, current human immune-system mice models have several major limitations, such as the poor development, maintenance, and function of human myeloid cells. As a consequence, human immune responses at mucosal surfaces, such as the lung, have rarely been observed.
The mouse host represents a nonphysiological environment for human cells. Several mouse cytokines, such as IL-3 and GM-CSF, do not act on the human cognate receptors. In addition, Rag2−/− Il2rg−/− mice have an intact mouse myeloid compartment, and human myeloid cells might have a competitive disadvantage relative to host cells. To overcome these limitations, we decided to generate human cytokine knock-in (KI) mice where mouse cytokines are replaced by their human counterparts. Criteria for cytokine replacement are: (i) mouse cytokine does not or weakly act on human cells; (ii) human cytokine does not or weakly act on mouse cells to confer competitive advantage to human cells; (iii) human cytokine is not exclusively produced by hematopoietic (transplanted) cells; and (iv) lack of mouse cytokine is not lethal to mouse host or human KI cytokine is sufficiently cross-reactive to rescue the mouse knockout (KO) phenotype. The KI strategy should allow faithful expression in appropriate organs and at physiologic concentrations. Importantly, in homozygous KI mice, human cognate receptor-expressing cells should gain a competitive advantage over the respective mouse cells.
IL-3 and GM-CSF are two cytokines crucial for myeloid cell development and function. Neither cytokine is cross-reactive between human and mouse (2). IL-3 stimulates early hematopoietic progenitors in vitro, but is dispensable for steady-state hematopoiesis in vivo (12). Similar to IL-3, GM-CSF is largely dispensable for steady-state hematopoiesis (13–15) and the same applies to mice lacking both cytokines (16, 17). In contrast, GM-CSF is required for inflammatory responses (such as the production of proinflammatory cytokines by macrophages) and host defense against pathogens (18). Moreover, GM-CSF is highly expressed in the lung and important for lung homeostasis in vivo (19), as demonstrated by the fact that GM-CSF KO mice develop pulmonary alveolar proteinosis (PAP), which is characterized by protein accumulation in the lung because of defective surfactant clearance (13, 14). Alveolar macrophages from GM-CSF KO mice have a defect in terminal differentiation, which leads to impaired innate immunity to pathogens in the lung (19, 20).
We thus hypothesized that generating hIL-3/GM-CSF KI mice would be valuable to support human myeloid cell reconstitution and function, as well as human innate immune responses to lung pathogens. We show here that these mice provide a substantial improvement over current models of human immune-system mice in terms of human alveolar macrophage development and human immune responses in the lung.
Results
Validation of hIL-3/GM-CSF KI Mice.
The genes encoding GM-CSF (CSF2) and IL-3 (IL3) are closely linked (< 10 kb) on chromosomes 5 and 11 in humans and mice, respectively. This closeness allowed us to replace the mouse with the human loci for both genes to generate hIL-3/GM-CSF KI mice (Fig. S1). Although the human IL3 KI allele is under the control of mouse regulatory elements, the human CSF2 KI allele remains under the control of its human regulatory elements. We analyzed expression of mouse and human GM-CSF mRNA by RT-PCR in hIL-3/GM-CSF KI mice expressing one allele of each mouse and one allele of each human gene, referred to as IL-3/GM-CSF “human/mouse” (h/m) mice. Wild-type mice that only have the mouse alleles of Il3 and Csf2 are referred to as IL-3/GM-CSF “mouse/mouse” (m/m) mice. Human GM-CSF mRNA was expressed in a similar pattern to its mouse counterpart, with highest expression in the lung (Fig. 1A). To confer a competitive advantage to human hematopoietic cells, we generated homozygous KI mice that express two alleles of human IL3 and CSF2, referred to as IL-3/GM-CSF “human/human” (h/h) mice. Conventional and quantitative RT-PCR analysis of lung tissue showed that h/h mice express only human, but not mouse GM-CSF mRNA (Fig. 1 B and C). Human GM-CSF protein could be detected by ELISA in the bronchoalveolar lavage fluid of h/h mice (Fig. 1D). Both mouse and human IL-3 mRNA was highly expressed by activated splenocytes from h/m mice, with low expression in digested bone, but neither was expressed in the lung (Fig. S2A). Human IL-3 (and GM-CSF) protein could be detected in supernatants from activated splenocytes isolated from h/m mice (Fig. S2B). We conclude that hIL-3/GM-CSF KI mice faithfully express human GM-CSF and IL-3.
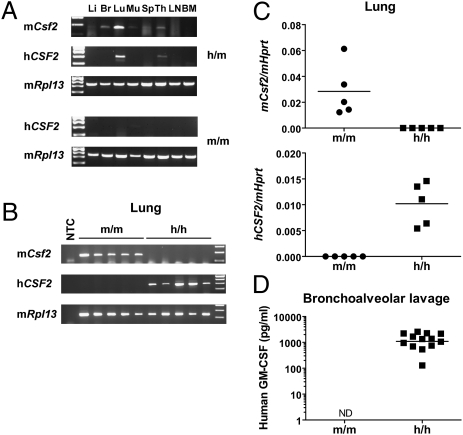
Validation of human GM-CSF expression in nonengrafted hIL-3/GM-CSF KI mice. (A) Representative RT-PCR analysis of GM-CSF mRNA expression in various tissues from KI mice with one allele of human and one allele of mouse Csf2 (h/m). Li, liver; Br, brain; Lu, lung; Mu, muscle; Sp, spleen; Th, thymus; LN, lymph node; BM, bone marrow. (Lower) Specificity of primers to detect human GM-CSF was verified by RT-PCR analysis of tissues from control mice (m/m). Mouse ribosomal protein L13 (Rpl13) served as an endogenous control. (B) RT-PCR analysis of GM-CSF mRNA expression in lungs from m/m mice or homozygous KI mice expressing two alleles of human CSF2 (h/h) (each n = 5). Mouse Rpl13 served as an endogenous control. NTC, no template control. (C) Quantitative RT-PCR analysis of GM-CSF mRNA expression as in B. GM-CSF expression was normalized to mouse Hprt (each n = 5). (D) ELISA of human GM-CSF protein in bronchoalveolar lavage fluid recovered from m/m or h/h KI mice (each n = 13). ND, not detectable. Each dot represents one mouse. Horizontal bars indicate mean values.
Enhanced Human Inflammatory Responses in Engrafted hIL-3/GM-CSF KI Mice.
Human IL-3/GM-CSF KI mice were generated from ES cells with one allele of both Rag2 and Il2rg already deleted. Breeding onto the Rag2−/− Il2rg−/− (BALB/c × 129) background then allowed engraftment with human CD34+ hematopoietic cells. Human IL-3/GM-CSF h/m KI mice were engrafted with CD34+ cells from cord blood, and h/h KI mice were engrafted with CD34+ cells from fetal liver. Overall human CD45+ hematopoietic cell chimerism in bone marrow, blood, and spleen was not increased in hIL-3/GM-CSF KI mice (Fig. S3A). There were no major differences in human T-cell development in the thymus (Fig. S3B), as well as in the frequencies of human T, B, and natural killer (NK) cells in blood (Fig. S3C) and spleen (Fig. S3D). In addition, the frequencies of human CD34+ hematopoietic stem cells, CD34+CD33+ myeloid progenitor cells, total CD33+ myeloid cells, CD14+ monocytes/macrophages, and CD66+SSChi granulocytes in the bone marrow were not significantly increased in hIL-3/GM-CSF KI mice (Fig. S4A). The same was true for human CD14+ monocytes/macrophages, CD11c+ dendritic cells (DC), CD123+ plasmacytoid DC, and CD66+SSChi granulocytes in the blood (Fig. S4B). This finding applied to both h/m (engrafted with cord blood CD34+ cells) and h/h mice (engrafted with fetal liver CD34+ cells) under steady-state conditions. Finally, human bone marrow cells from engrafted hIL-3/GM-CSF KI mice had a similar capacity to form myeloid colonies in methylcellulose in vitro (Fig. S4C). Our findings are consistent with results from KO mouse studies showing that both IL-3 and GM-CSF are largely dispensable for steady-state myelopoiesis (12–17).
In contrast, GM-CSF plays an important role in mediating inflammatory responses (18). GM-CSF expression is induced by inflammatory stimuli, which leads to the production of inflammatory cytokines (such as IL-6) by monocytes/macrophages and to their recruitment to sites of inflammation. We observed that human CD14+ monocytes from engrafted hIL-3/GM-CSF KI mice had the highest expression of the GM-CSF receptor α-chain (CD116) (Fig. S5A). Therefore, we focused on human monocytes/macrophages in our analysis of engrafted hIL-3/GM-CSF KI mice. First, we analyzed the inflammatory response of human monocytes in engrafted hIL-3/GM-CSF KI mice. Systemic inflammation was induced by intraperitoneal injection of LPS. The frequency of circulating human CD14+ monocytes was significantly increased in h/m compared with control m/m mice after LPS injection (Fig. S5 B and C). Enhanced mobilization of human monocytes in h/m mice was associated with increased serum concentrations of human IL-6 after one and two injections of LPS (Fig. S5D). These data indicate that hIL-3/GM-CSF KI mice engrafted with human hematopoietic cells have enhanced human inflammatory responses mediated most likely by human myelo-monocytic cells.
Homozygous hIL-3/GM-CSF KI Mice Support the Development of Human Alveolar Macrophages.
The absence of mouse GM-CSF leads to impairment of mouse alveolar macrophages, which should favor reconstitution with human macrophages in homozygous hIL-3/GM-CSF KI mice. In support of this, human GM-CSF is highly expressed in the lung and bronchoalveolar lavage of h/h mice, but mouse GM-CSF is lacking (Fig. 1). Mouse alveolar macrophages from nonengrafted h/h mice were enlarged and had the typical “foamy” appearance (Fig. S6A), which has been described for alveolar macrophages from GM-CSF KO mice. GM-CSF KO mice develop PAP because of a defect in surfactant clearance by alveolar macrophages that have a block in terminal differentiation (19). Similarly to what has been reported for GM-CSF KO mice, nonengrafted h/h mice developed features of PAP, such as the subpleural accumulation of alveolar macrophages full of Periodic acid-Schiff (PAS)–positive material (Fig. S6B). We conclude that nonengrafted h/h mice show impaired differentiation of mouse alveolar macrophages and develop PAP, and are therefore functionally equivalent to GM-CSF KO mice.
Next, we examined the lung compartment of h/h mice after engraftment with human hematopoietic cells. FACS analysis showed that h/h mice had considerably more human CD45+ cells in the bronchoalveolar lavage (Fig. 2 A and B). Quantitative RT-PCR of lung tissue revealed that this increase in human cells consisted mainly of cells expressing mRNA for the human myeloid markers CD33, CD11b (ITGAM), CD11c (ITGAX), and CD14 (Fig. 2 C and D). Furthermore, mRNA expression of human CD68, a mature macrophage marker that is mainly expressed intracellularly, was markedly increased in engrafted h/h mice (Fig. 2E). This increase in h/h mice was associated with higher expression of two transcription factors that are expressed by alveolar macrophages, namely PU.1 (SPI1) and peroxisome proliferator-activated receptor-γ (PPARγ) (Fig. 2E). PU.1 is highly expressed in terminally differentiated alveolar macrophages in a GM-CSF–dependent manner (20). Importantly, transduction of GM-CSF KO alveolar macrophages with PU.1 in vitro reverses their functional impairment (20). PPARγ is also highly expressed in alveolar macrophages and, similarly to GM-CSF KO mice, PPARγ KO mice develop PAP (21). Immunohistological staining of lung sections revealed the presence of numerous hCD68+ cells with a typical intra-alveolar location, consistent with human alveolar macrophages, in engrafted h/h mice (Fig. 3). In contrast, very few human alveolar macrophages could be detected in engrafted m/m control mice. In summary, lungs of CD34+ hematopoietic cell transplanted h/h mice show markedly improved reconstitution with human macrophages.

Homozygous hIL-3/GM-CSF KI mice have enhanced human myeloid cell reconstitution in the lung. (A) Representative flow cytometry analysis of bronchoalveolar lavage cells from nonengrafted and engrafted m/m and h/h KI mice. Numbers next to outlined areas indicate the percentages of hCD45+ and mCD45+ hematopoietic cells. The mCD45+ cells have high autofluorescence and constitute F4/80+ mouse alveolar macrophages (Fig. S6A). (B) Numbers of human hematopoietic (hCD45+) cells in bronchoalveolar lavage from engrafted m/m and h/h KI mice. Results are combined from three independent experiment (total n = 15 per group). (C–E) Quantitative RT-PCR analysis of human lymphoid (C), myeloid (D), and macrophage (E) gene expression in lung tissue from engrafted m/m and h/h KI mice. Expression was normalized to mouse Hprt. Results are combined from three independent experiments (total, n = 10 per group). Each dot represents one mouse. Horizontal bars indicate mean values.
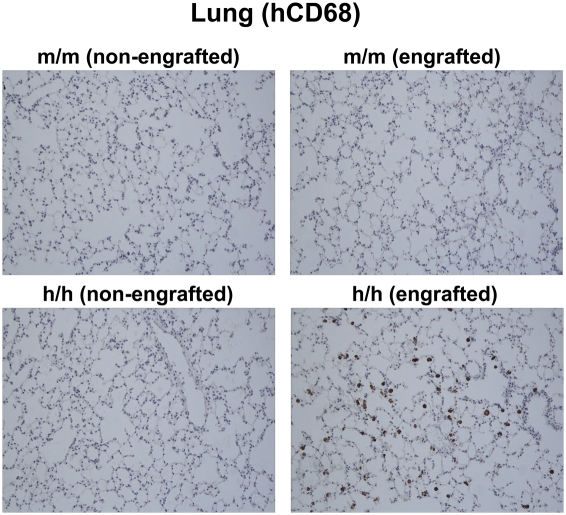
Homozygous hIL-3/GM-CSF KI mice support the development of human alveolar macrophages. Immunohistochemistry of lung tissue sections stained for human CD68 from nonengrafted and engrafted m/m and h/h KI mice. Magnification: 200×. One representative example of a total of 12 mice analyzed per group in two independent experiments is shown.
Human Hematopoietic Cells Partially Rescue PAP in Homozygous hIL-3/GM-CSF KI Mice.
We then asked if the increased engraftment of h/h mice with human macrophages leads to better human immune function in the lung. To demonstrate that human alveolar macrophages are functional, we first examined if human alveolar macrophages can rescue the PAP syndrome that is found in nonengrafted h/h mice. Although both type II alveolar epithelial cells and alveolar macrophages can respond to GM-CSF, PAP can be rescued by bone marrow transplantation (22). This finding indicates that hematopoietic cells, specifically alveolar macrophages, are the main cell type being able to reverse PAP. Therefore, we hypothesized that h/h mice engrafted with human hematopoietic cells should have less severe PAP. Consistent with our hypothesis, engrafted h/h mice had significantly lower amounts of total protein in the bronchoalveolar lavage fluid than nonengrafted h/h mice (Fig. 4A). In addition, although nonengrafted h/h mice showed intra-alveolar accumulation of PAS-positive material (Fig. 4B), which is a hallmark of PAP, engrafted h/h mice had less severe protein accumulation in the lung (Fig. 4B). These results indicate that engrafted human hematopoietic cells (presumably alveolar macrophages) are capable of at least partially rescuing PAP in homozygous hIL-3/GM-CSF KI mice, thereby contributing to lung homeostasis under steady-state conditions.
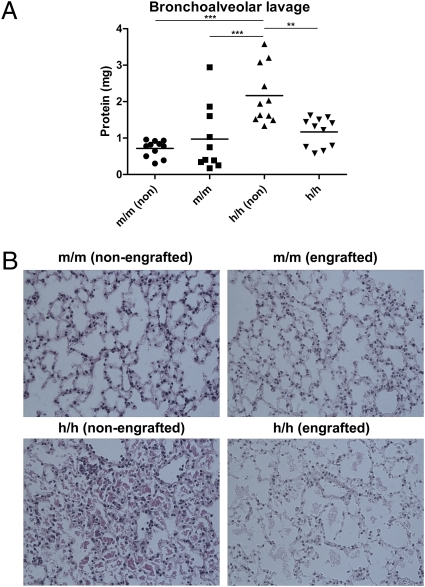
Human hematopoietic cells partially rescue PAP in homozygous hIL-3/GM-CSF KI mice. (A) Quantification of total protein in bronchoalveolar lavage fluid from nonengrafted (non) or engrafted m/m or h/h KI mice. Results are combined from two independent experiments (total n = 10–11 per group). P = 0.0004 (one-way ANOVA testing). Values of P as determined by Tukey's Multiple Comparison Test are indicated by asterisks (**P < 0.01, ***P < 0.001). (B) PAS staining of lung tissue sections from nonengrafted or engrafted m/m or h/h KI mice. Magnification: 400×. Representative examples of a total of 10 to 12 mice analyzed per group are shown.
Homozygous hIL-3/GM-CSF KI Mice Mount Correlates of a Human Innate Immune Response to Influenza A Virus.
In addition to their role in lung homeostasis, alveolar macrophages are essential for host defense in the lung. Alveolar macrophages are the main producers of type I IFN after infection with pulmonary viruses (23) and are required for an effective innate response to influenza A (24). Numerous studies have shown that GM-CSF KO mice are more susceptible to a variety of pathogens in the lung (19, 20). Furthermore, administration of recombinant human GM-CSF has a protective effect in mice infected with influenza A virus (25). To assess the contribution of engrafted human alveolar macrophages to lung host defense, we therefore infected engrafted h/h mice with influenza A/PR8 (H1N1) virus via the intranasal route and measured production of human cytokines. Consistent with enhanced human alveolar macrophage reconstitution, engrafted h/h mice expressed significant amounts of human GM-CSF, TNF-α, and IL-6 mRNA in the lung after infection with influenza A virus (Fig. 5A). Importantly, engrafted h/h mice had 100-fold higher expression of human IFN-β mRNA after infection and compared with engrafted m/m mice (Fig. 5A). In contrast, engrafted m/m mice showed no significant induction of human cytokine mRNA expression after influenza A infection compared with engrafted m/m mice that had received PBS intranasally (Fig. 5A). In addition, engrafted h/h mice expressed significantly higher amounts of human GM-CSF and IL-6 protein in the lung than engrafted m/m mice 72 h postinfection (Fig. 5B). The majority of engrafted h/h mice (9 of 14 mice) also had detectable levels of human IL-6 protein in the serum, but none of the engrafted m/m mice (0 of 10 mice) had detectable levels. IL-6 plays an important role in host defense against influenza virus, as shown by the increased mortality of IL-6 KO mice after influenza infection (26). Therefore, in contrast to m/m mice, engrafted h/h mice are capable of mounting a human innate immune response to influenza A virus. However, engrafted h/h mice did not show enhanced protection against influenza virus because viral burden was not reduced compared with engrafted m/m mice (Fig. S7). Taken together, these data show that homozygous hIL-3/GM-CSF KI mice allow better human macrophage chimerism in the lung, which leads to improved lung homeostasis under steady-state conditions and to enhanced human cytokine production in response to viral infection.
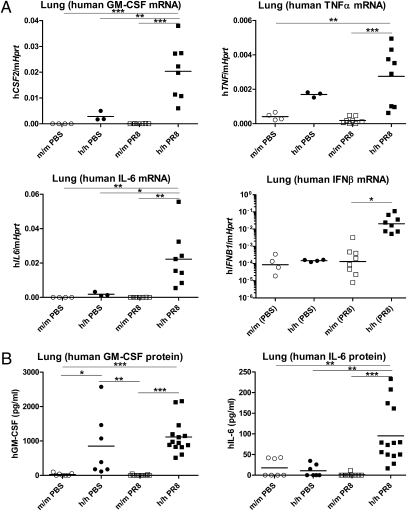
Homozygous hIL-3/GM-CSF KI mice mount correlates of a human innate immune response to influenza A virus. (A) Quantitative RT-PCR analysis of human gene expression in lung tissue from engrafted m/m and h/h KI mice 24 h after intranasal infection with influenza A (PR8) (each, n = 8). Intranasal application of PBS was used as a control (PBS) (each, n = 3–4). Expression was normalized to mouse Hprt. P < 0.0001 (hCSF2), P = 0.0004 (hTNF), P = 0.0007 (hIL6), P = 0.0171 (hIFNB1) (one-way ANOVA testing). (B) ELISA of human GM-CSF and IL-6 protein in lung tissue from engrafted m/m and h/h KI mice 72 h postinfection with influenza A (PR8) or intranasal application of PBS. Results are combined from two independent experiments (total, n = 7–14 per group). P < 0.0001 (hGM-CSF), P < 0.0001 (hIL-6) (one-way ANOVA testing). Each dot represents one mouse. Horizontal bars indicate mean values. Values of P as determined by Tukey's multiple comparison test are indicated by asterisks (*P < 0.05, **P < 0.01, ***P < 0.001).
Discussion
The ability to study human tissue in an in vivo setting in mice has opened a wide range of possible avenues of research. Major limitations have hindered the application of the approach, and of these one of the most important deficiencies has been the inability of mouse factors to support human cells. Indeed, in the immune system many essential factors required for human immune cell development and function are species-specific and cannot be effectively provided by the mouse. We therefore decided to follow a strategy of replacing the mouse genes with their human counterparts, enabling the better development and function of human cells and potentially disabling the same of the corresponding mouse cells. By applying this concept to human cytokine KI mice, we provide here proof of concept that replacement of immune genes in the mouse host with human genes improves human immune-system mice.
Human cytokines can be delivered to human immune-system mice by intravenous injection; for example, to boost human NK cell and T-cell reconstitution by injections of IL-15/IL-15Rα complexes (27) and IL-7 (28), respectively. Systemic expression of human cytokines can also be achieved using a lentivirus-based delivery system; for example, to enhance human T-cell reconstitution by the expression of IL-7 (29). Another approach is the hydrodynamic injection of plasmid DNA-expressing human cytokines, which leads to transient expression in the liver. This approach has recently been used to improve reconstitution of human DC by hydrodynamic delivery of GM-CSF and IL-4 (30). Finally, human cytokines can also be overexpressed as transgenes in human immune-system mice. This approach has been used to generate human IL-3/GM-CSF/stem cell-factor transgenic mice (31). In these mice, human cytokine expression is driven by the cytomegalovirus promoter, which leads to ubiquitous expression. However, hIL-3/GM-CSF/stem cell-factor transgenic human immune-system mice are hampered by reduced maintenance of human hematopoietic stem cells in bone marrow and expanded terminal myelopoiesis. In contrast to our study, no functional responses of myeloid cells or in vivo responses to pathogens were evaluated in the last two reports.
The hIL-3/GM-CSF KI mice described in this study represent a considerable improvement over previous human immune-system mice and the alternative approaches discussed above. First, delivery of human IL-3 and GM-CSF by our KI strategy leads to long-term cytokine expression, which circumvents the need for repeated injections of expensive cytokines. Second, faithful expression in organs where IL-3 and GM-CSF are normally expressed, is achieved. Under physiological conditions, GM-CSF is mainly expressed in the lung (Fig. 1). In contrast, hydrodynamic delivery leads to predominant expression in the liver and in the circulation (30). In both liver and blood GM-CSF is not normally expressed in steady-state conditions. Third, physiological amounts of IL-3 and GM-CSF are expressed in KI mice in contrast to delivery by hydrodynamic injection or ubiquitous overexpression in hIL-3/GM-CSF/stem cell-factor transgenic mice. Fourth, homozygous hIL-3/GM-CSF KI mice allow the simultaneous impairment of the mouse myeloid compartment because mouse IL-3 and GM-CSF are not expressed in homozygous mice, which leads to a competitive advantage for human myeloid cells, as shown in the present study.
Despite increased human cytokine production, engrafted hIL-3/GM-CSF KI mice did not show enhanced protection against infection with influenza virus. This is likely because of several reasons: (i) Influenza virus affects both human and mouse cells and in humanized mice the lung epithelium is of mouse origin, but the immune system consists of mouse (myeloid) and human (myeloid and lymphoid) cells. Furthermore, our mouse strain (BALB/c × 129 background) lacks a functional Mx gene, an important IFN-induced resistance factor against influenza virus (32). Therefore, although the (human) innate immune response to influenza is enhanced in hIL-3/GM-CSF KI mice, this may not lead to better protection because the mouse lung epithelium lacks the antiviral Mx gene. (ii) Recovery from influenza infection in mice is dependent on a functional adaptive immune system. In current humanized mouse models (including hIL-3/GM-CSF KI mice), human T- and B-cell responses are still suboptimal. This could be another reason why the enhanced human innate immune response in hIL-3/GM-CSF KI mice does not translate into better protection. Future improvements of our model by additional genetic modifications of the mouse host (human cytokine and HLA KI) should lead to a humanized mouse model with enhanced protection against influenza.
Apart from being a model for human immune responses to lung pathogens, hIL-3/GM-CSF KI mice may be useful for studying human autoimmune and inflammatory responses in the lung that occur, for example, in asthma. Alveolar macrophages have been implicated in preventing excessive immune responses to inhaled antigens (24), and other cells that are important for the immunopathology in asthma are also regulated by IL-3 and GM-CSF: IL-3 plays a role in the biology of mast cells (33) and GM-CSF regulates the differentiation of NKT cells (34). Future refinements, such as the improvement of human T-cell (Th2) responses and reconstitution of human lung epithelium (35) in the mouse host, should therefore make a mouse model that closely mimics human asthma a real possibility.
In summary, the hIL-3/GM-CSF KI mice presented in the current study represent a considerable improved human immune system mouse model that should serve as a versatile tool for future studies.
Materials and Methods
Generation of hIL-3/GM-CSF KI Mice.
For details see SI Materials and Methods.
RT-PCR.
Total RNA was extracted from homogenized tissues with TRIzol reagent (Invitrogen) according to the manufacturer's instructions. Equal amounts of DNase-treated RNA were used for cDNA synthesis with the SuperScript First-Strand Synthesis System (Invitrogen). Conventional RT-PCR was performed with the following primers: (i) Mouse Csf2: forward, CCAGTCCAAAAATGAGGAAGC; reverse, CAGCGTTTTCAGAGGGCTAT. (ii) Human CSF2: forward, GGCGTCTCCTGAACCTGAGT; reverse, GGGGATGACAAGCAGAAAGT. (iii) Mouse Rpl13: forward, GTACGCTGTGAAGGCATCAA; reverse, ATCCCATCCAACACCTTGAG. Quantitative RT-PCR was performed on a 7500 Fast Real-Time PCR system with primer-probe sets purchased from ABI. Expression values were calculated using the comparative threshold cycle method and normalized to mouse Hprt.
Bronchoalveolar Lavage.
Lungs were inflated with 1 mL PBS via a catheter inserted into the trachea. This process was repeated twice and the recovered lavage pooled. After centrifugation, cell-free supernatants were saved for determination of GM-CSF protein concentration by ELISA or for total protein content with the BCA Protein Assay Kit (Pierce) according to the manufacturer's instructions. After RBC lysis with ACK lysis buffer (Lonza), cell pellets were counted and either used for flow cytometry as above or for cytospin preparations. Cells were spun onto slides and stained with Diff-Quik Stain Set (Dade Behring) according to the manufacturer's instructions.
Engraftment of Mice with Human Hematopoietic CD34+ Stem and Progenitor Cells.
Human cord blood and fetal liver samples were obtained under approval from the Yale University Human Investigation Committee from Yale-New Haven Hospital and Albert Einstein Medical College, New York, respectively. CD34+ cells were purified by density gradient centrifugation and immunomagnetic selection using CD34 microbeads (Miltenyi Biotec). Newborn pups were engrafted with human CD34+ cells as previously described (6). Engraftment with human hematopoietic cells was determined 8 to 12 wk posttransplantation by retro-orbital bleeding and flow cytometry, as described below. Mice used for experiments had blood engraftment levels of ≥4% hCD45+ cells unless indicated otherwise. Matched mice (i.e., mice engrafted with the same batch of CD34+ cells) were used for experiments. Human IL-3/GM-CSF h/m KI mice were engrafted with CD34+ cells from cord blood, and h/h KI mice were engrafted with CD34+ cells from fetal liver. Mice were maintained under specific pathogen-free conditions and received prophylactic antibiotics (Sulfatrim) in the drinking water to prevent opportunistic infections. All animal work was approved by the Yale University Institutional Animal Care and Use Committee and conducted in accordance with its regulations.
Histology and Immunohistochemistry.
After perfusion with 10 mL cold PBS lungs were harvested and fixed in 10% neutral-buffered formalin or Zinc Fixative (BD Biosciences) for histological analysis. Paraffin-embedded tissues sections were prepared, stained with H&E or PAS, or processed for immunohistochemistry by the Yale Pathology Tissue Services. Anti-human Ab CD68 (PG-M1) (Dako) was used for immunohistochemistry.
Influenza A Infection.
Mice were infected with 2 × 104 PFU of influenza A/PR8 (H1N1) virus via the intranasal route. Infection was performed by the intranasal application of 50 μL virus stock diluted in PBS (or an equal volume of PBS as a control) to mice that had been deeply anesthetized with anafane (Ivesco). Lungs were harvested 24 h after infection for RNA extraction and quantitative RT-PCR analysis as described above. Lung homogenates were prepared in 1 mL 0.1% BSA/PBS for cytokine measurements by ELISA 72 h postinfection.
Statistical Analysis.
The nonparametric Mann-Whitney U test was used to determine statistical significance between two groups (α = 0.05). For multigroup comparisons, we applied one-way ANOVA with post hoc testing using Tukey's Multiple Comparison Test (α = 0.05). For data plotted on a logarithmic scale the geometric mean is depicted, otherwise the arithmetic mean is shown.
Acknowledgments
The authors thank A. M. Franco for isolation of CD34+ cells, P. Ranney for mouse breeding, R. Webber for mouse breeding and engraftment, A. Brooks for histology and immunohistochemistry, and J. Alderman for organizational support; we also thank our colleagues at Regeneron's VelociGene for their excellent technical contributions to this work, L. Zenewicz, S. Sanjabi, and F. Sutterwala for critically reading the manuscript, and F. Manzo for manuscript submission. This work was supported by grants from the Bill and Melinda Gates Foundation (Grand Challenges in Global Health Initiative) and the Juvenile Diabetes Research Foundation. R.A.F. is an investigator of The Howard Hughes Medical Institute.
Footnotes
Conflict of interest statement: G.D.Y., D.M.V., A.J.M., and W.A. are employees of Regeneron Pharmaceuticals. S.S. was an employee of Regeneron Pharmaceuticals and is currently an employee of AnaptysBio Inc.
This article contains supporting information online at www.pnas.org/lookup/suppl/10.1073/pnas.1019682108/-/DCSupplemental.
References
Articles from Proceedings of the National Academy of Sciences of the United States of America are provided here courtesy of National Academy of Sciences
Full text links
Read article at publisher's site: https://doi.org/10.1073/pnas.1019682108
Read article for free, from open access legal sources, via Unpaywall:
https://www.pnas.org/content/pnas/108/6/2390.full.pdf
Free after 6 months at www.pnas.org
http://www.pnas.org/cgi/content/abstract/108/6/2390
Free after 6 months at www.pnas.org
http://www.pnas.org/cgi/content/full/108/6/2390
Free after 6 months at www.pnas.org
http://www.pnas.org/cgi/reprint/108/6/2390.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Article citations
Emerging and reemerging infectious diseases: global trends and new strategies for their prevention and control.
Signal Transduct Target Ther, 9(1):223, 11 Sep 2024
Cited by: 0 articles | PMID: 39256346 | PMCID: PMC11412324
Review Free full text in Europe PMC
Advancing Human Vaccine Development Using Humanized Mouse Models.
Vaccines (Basel), 12(9):1012, 04 Sep 2024
Cited by: 0 articles | PMID: 39340042 | PMCID: PMC11436046
Review Free full text in Europe PMC
Cross-tissue organization of myeloid cells in scleroderma and related fibrotic diseases.
Curr Opin Rheumatol, 23 Aug 2024
Cited by: 0 articles | PMID: 39171604 | PMCID: PMC11451931
T-cell responses in colorectal peritoneal metastases are recapitulated in a humanized immune system mouse model.
Front Immunol, 15:1415457, 09 Jul 2024
Cited by: 0 articles | PMID: 39044825 | PMCID: PMC11263213
Protocol to construct humanized mice with adult CD34+ hematopoietic stem and progenitor cells.
STAR Protoc, 5(3):103155, 26 Jun 2024
Cited by: 0 articles | PMID: 38935509 | PMCID: PMC11260840
Go to all (138) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
GM-CSF in the lung protects against lethal influenza infection.
Am J Respir Crit Care Med, 184(2):259-268, 07 Apr 2011
Cited by: 110 articles | PMID: 21474645 | PMCID: PMC6938174
Delivery of GM-CSF to Protect against Influenza Pneumonia.
PLoS One, 10(4):e0124593, 29 Apr 2015
Cited by: 28 articles | PMID: 25923215 | PMCID: PMC4414562
GM-CSF modulates pulmonary resistance to influenza A infection.
Antiviral Res, 92(2):319-328, 08 Sep 2011
Cited by: 41 articles | PMID: 21925209 | PMCID: PMC4894852
Gm-CSF regulates pulmonary surfactant homeostasis and alveolar macrophage-mediated innate host defense.
Annu Rev Physiol, 64:775-802, 01 Jan 2002
Cited by: 214 articles | PMID: 11826288
Review
Funding
Funders who supported this work.





