Abstract
Free full text

Genetic counseling and testing for Alzheimer disease: Joint practice guidelines of the American College of Medical Genetics and the National Society of Genetic Counselors
Abstract
Alzheimer disease is the most common cause of dementia. It occurs worldwide and affects all ethnic groups. The incidence of Alzheimer disease is increasing due, in part, to increased life expectancy and the aging baby boomer generation. The average lifetime risk of developing Alzheimer disease is 10–12%. This risk at least doubles with the presence of a first-degree relative with the disorder. Despite its limited utility, patients express concern over their risk and, in some instances, request testing. Furthermore, research has demonstrated that testing individuals for apoli-poprotein E can be valuable and safe in certain contexts. However, because of the complicated genetic nature of the disorder, few clinicians are prepared to address the genetic risks of Alzheimer disease with their patients. Given the increased awareness in family history thanks to family history campaigns, the increasing incidence of Alzheimer disease, and the availability of direct to consumer testing, patient requests for information is increasing. This practice guideline provides clinicians with a framework for assessing their patients’ genetic risk for Alzheimer disease, identifying which individuals may benefit from genetic testing, and providing the key elements of genetic counseling for AD.
Alzheimer disease (AD) currently affects more than 5 million Americans.1 Although the majority of cases occur in the elderly, approximately 250,000 people have early-onset AD (EOAD) with onset of symptoms before age 65 years.1 Individuals with a family history of dementia often worry about their own risk of developing dementia and may be interested in learning about genetic testing options.2,3 Although genetic testing for AD has become more accessible through clinical laboratories and direct-to-consumer testing, the understanding of AD genetics continues to evolve, making it difficult for clinicians to effectively counsel their patients on hereditary risk and genetic testing.4 The purpose of this practice guideline is to provide clinicians with a framework for assessing their patients’ genetic risk for AD, identifying which individuals may benefit from genetic testing, and providing the key elements of genetic counseling for AD, which is an integral part of the testing protocol.
CLINICAL ASPECTS OF AD
AD is the most common form of dementia, accounting for two thirds of all dementia diagnoses.5 It is usually marked by slowly progressive episodic memory loss, which evolves into global loss of cognitive ability, psychiatric features, and involvement of other deeper brain areas such as the basal ganglia.6 Atypical presentations occur in 6–14% of autopsy confirmed cases.7–10 As the disease progresses, motor dysfunction, such as parkinsonism, myoclonus, spastic paraparesis, and seizures, may also accompany neurologic and neuropsychiatric symptoms.7,11 The variability in phenotype increases the challenges of clinical management and appropriate use of genetic testing.12
Current diagnostic criteria for AD are based on the Diagnostic and Statistical Manual for Mental Disorders, 4th Edition, and the National Institute of Neurological Disorders, Communicative Disorders and Stroke-Alzheimer Disease and Related Disorders Association working group.13,14 A definitive diagnosis of AD can only be made by pathologic confirmation (National Institute on Aging-Reagan criteria) after autopsy of a symptomatic individual or identification of a pathogenic mutation in a causal AD gene (see discussion later) in a symptomatic individual.7,15,16 The risk for developing AD is associated most heavily with genetic factors and age, but sex, level of education, and history of head trauma, among others under investigation, may also be contributing factors.1,17–19 Members of the general population are at approximately 10–12% risk of developing AD in their lifetime. More precise risk estimates are only available for those with a family history consistent with autosomal dominant EOAD and those with a first-degree relative with AD.
Research on biomarkers for AD with the purpose of diagnosis, prediction of disease progression, presymptomatic predictive testing, and clinical trial use is proceeding around the world. Results indicate that cerebrospinal fluid (CSF) beta amyloid peptides (Aβ1-42), total tau, and phosphorylated tau levels have significant correlation with disease status, with evidence for decreased Aβ1-42 and increased total tau and phosphorylated tau in people with mild cognitive impairment (MCI) and AD, when compared with controls.20–22 Neuroimaging using magnetic resonance imaging, positron emission tomography, and Pittsburgh Compound B positron emission tomography improves the validity of the CSF markers.23 However, studies on these biomarkers did not use standardized assays and techniques, resulting in variability in measurements between different laboratories and within studies.22,24 Currently, CSF biomarkers are being used by some physicians in the differential diagnosis of dementia indicating the likelihood that a patient has AD rather than another form of dementia. Caution needs to be taken when interpreting these tests as results are not conclusive. Similarly, these test results cannot be used to predict the time of conversion from MCI to AD or as a definitive diagnostic test.22,25 Of note, studies indicate that apolipoprotein E (APOE) ε4 carriers with MCI have lower Aβ1-42 than noncarriers with MCI, indicating increased probability of conversion to AD compared with other APOE genotypes.22,26
At the current time, treatment of AD is focused on slowing the disease progression through two primary processes: cholinesterase inhibitors and N-methyl-d-aspartic acid receptor antagonists. Some studies suggest that a lifestyle promoting good cardiovascular health may be beneficial in reducing the risk or delaying the age of onset of AD.27,28 In addition, nonpharmacologic treatments (environment modification and caregiver training) can be effective in managing some of the behavior problems associated with AD, such as depression, agitation/ aggression, wandering, and sleep disturbance.29
GENETICS OF AD
Alzheimer genetics is traditionally subdivided into early onset (EOAD) and late onset (LOAD). EOAD has an onset before age 60–65 years and accounts for 1–5% of all cases. 30–32 LOAD has an onset after age 60–65 years and is the predominant form of AD. Additionally, family history may be consistent with autosomal dominant, familial, or sporadic AD.
Autosomal dominant
Families with autosomal dominant AD are characterized by disease that occurs in at least three individuals in two or more generations, with two of the individuals being first-degree relatives of the third (e.g., grandparent, parent, and child). This pattern can sometimes be masked by small families, premature death due to other causes, or, rarely, by incomplete penetrance. Autosomal dominant AD, which represents <5% of cases, is seen almost exclusively in EOAD families, thus the terms are often used interchangeably.30,31 It is important to note, however, that not all EOAD is inherited in an autosomal dominant pattern. Mutations in known causative genes in such families are identified approximately 40–80% of the time with variability likely due to inconsistency in criteria used to define autosomal dominant AD.31,33–35
Familial
Familial AD is characterized by disease that occurs in more than one individual, and at least two of the affected individuals are third-degree relatives or closer. Familial clustering represents approximately 15–25% of AD cases. Most often these are families with LOAD (15–25% of all LOAD cases), but familial clustering can be seen in approximately 47% of EOAD cases.31,36 These familial EOAD cases may represent hidden autosomal dominant AD due to small family size or cases of premature death.
Sporadic
Sporadic AD is characterized by an isolated case in the family or cases separated by more than three degrees of relationship. Sporadic AD represents approximately 75% of all cases. Typically, sporadic cases are LOAD, but approximately 40% of EOAD cases may be classified as sporadic possibly representing hidden familial or autosomal dominant disease, particularly if the family size is small and/or there are case(s) of premature death.31,37
Currently, there are three known deterministic (causative) genes in which mutations are associated with autosomal dominant EOAD: PSEN1, PSEN2, and APP (Table 1).31,33,38–54 The major pathologic processes in AD seem to be the formation of neurofibrillary tangles and the deposition of Aβ42 into senile plaques in the brain. Thus, it should not be surprising that each of the known AD genes play a role in the production, trafficking, and clearance of Aβ42.55 Overall, however, mutations in the EOAD genes are rare, and account for only 1–5% of all cases of AD.30,31 Because not all families with autosomal dominant EOAD have identifiable mutations in PSEN1, PSEN2, or APP, it is likely there are additional genes that influence the pathophysiology of EOAD.31,49 Predictive/presymptomatic testing for autosomal dominant EOAD is most informative when a mutation has been confirmed in a symptomatic family member. Mutations in PSEN1 and APP are associated with complete penetrance, meaning that all individuals who have a PSEN1 or APP mutation will develop AD if they live a normal lifespan. In contrast, mutations in PSEN2 show 95% penetrance, meaning that not everyone with a PSEN2 mutation will develop AD.41,53 In general, clear genotype-phenotype correlations cannot typically be made for the three causative genes, and age of onset can vary more than 20 years within the same family. Although several mutations in PSEN1, PSEN2, and APP have been reported to demonstrate a distinct clinical or neuropathological phenotype, care must be taken when interpreting test results, as mutations may have variable expression both within and between families.56–58 Two other complicating factors are the ambiguity of a negative result in the absence of a known familial mutation and identifying a variant of uncertain significance.59
Table 1
Confirmed Alzheimer disease genes
| Gene | Protein name | Chromosomal locus | Testing is clinically available | Inheritance pattern | Age of onset | Penetrance |
|---|---|---|---|---|---|---|
| APP | Amyloid beta A4 Protein | 21q21.2 | Yes | Early-onset autosomal dominant | 40–60 yr | Complete |
| PSEN1 | Presenilin 1 | 14q24.3 | Yes | Early-onset autosomal dominant | 30–60 yr | Complete |
| PSEN2 | Presenilin 2 | 1q31-42 | Yes | Early-onset autosomal dominant | 40–75 yr | ~95% |
| APOE | Apolipoprotein E | 19q13.31 | Yes | Early- and late-onset familial/sporadic | 40–90 yr | N/A |
In contrast to these three deterministic genes, a fourth gene, APOE has been identified as a susceptibility gene for AD. APOE has three isoforms, ε2, ε3, and ε4. The ε4 variant of APOE is associated with an increased risk for AD, most notably in LOAD, but also EOAD.17,33,37,48,60,61 Approximately 50–70% of people with AD carry at least one ε4 allele.17,18,62,63 This percentage increases in those with AD who have a positive family history of disease.64 In addition, ε4 homozygotes are considerably more frequent among those with EOAD than LOAD.31,47,65 The presence of an ε4 allele increases the risk of AD in a dose-dependent fashion; individuals with two copies of the ε4 allele are at the highest risk. Estimates of the increased risk conferred by ε4 differ widely and also differ based on age and gender.31,66–68 Typical estimates suggest a 2–3-fold increased risk for ε4 heterozygotes, whereas estimates for homozygotes vary anywhere from a 2-fold to 10-fold increased risk.39,69–71 Many studies about the effects of the ε4 allele suggest that it influences the age at which AD occurs, rather than the overall lifetime risk for AD.17,61,72–75 Several studies have also suggested that the presence of an ε2 allele may play a protective role against developing AD.74,75 In addition to its role in AD, APOE has also been associated with risks of other diseases such as cardiovascular disease and macular degeneration.55,76 In the absence of APOE testing, first-degree relatives of an affected individual in sporadic or familial cases are estimated to have a 15–39% lifetime risk of developing AD, a 2–4-fold increase compared with the general population.77–83
PEDIATRIC TESTING FOR AD
Given the great variability in both symptoms and age of onset, even in family members who share the same causative mutation, genotypic information provides very little in the way of anticipatory guidance for the child. In addition, because AD remains, at this time, a disease that can neither be prevented nor cured, it is difficult to argue that there is a medical or social benefit to knowing the genotype of the child.84,85
GENETIC TESTING FOR AUTOSOMAL DOMINANT AD IN ADULTS
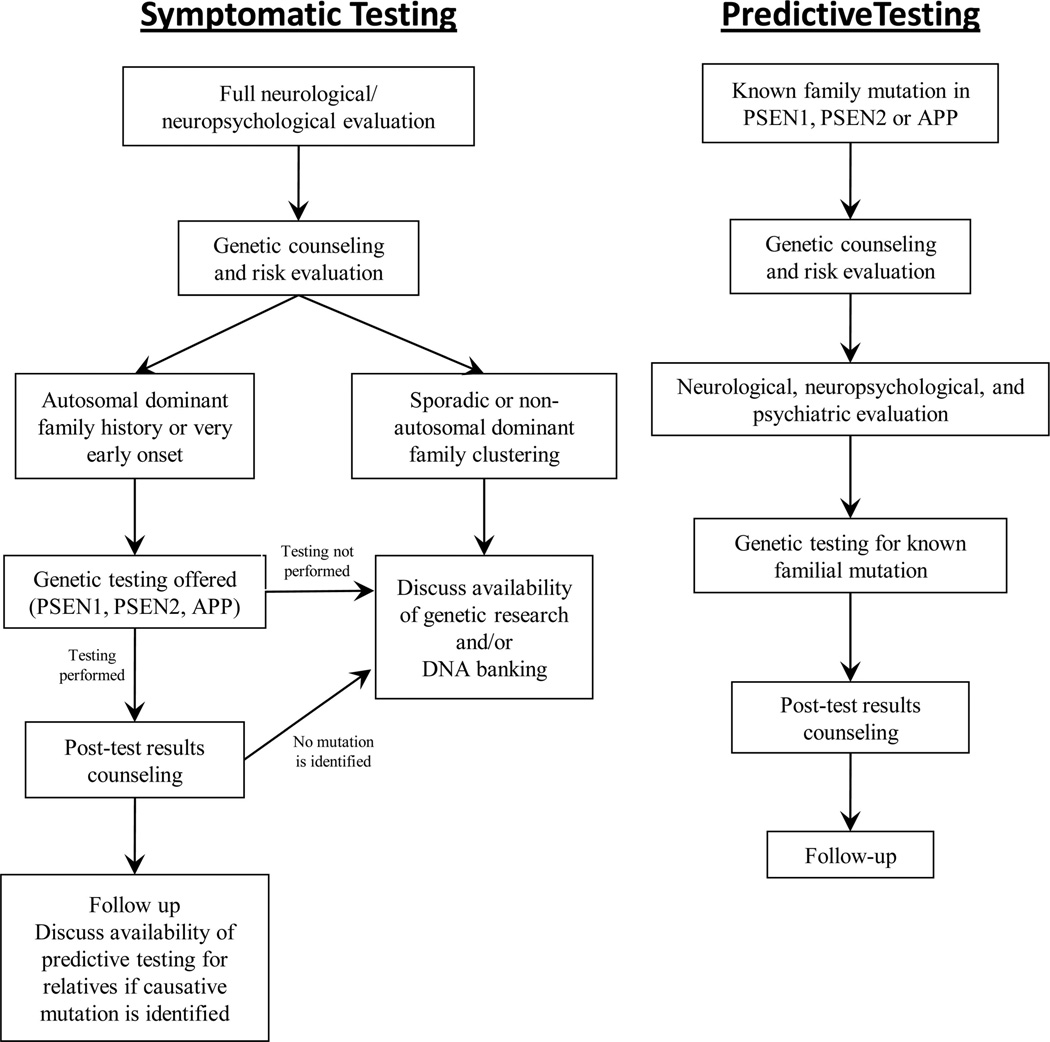
The use of genetic testing for diagnostic purposes in early-onset autosomal dominant AD has long been debated by clinicians in the dementia field.50,86,87 Although mutations are rare and testing may reveal variants of unknown significance, genetic testing may result in definitive diagnosis, improve understanding for the family, and allow at-risk relatives to have the option of predictive testing.88,89 Genetic counseling for symptomatic patients should be performed in the presence of the individual’s legal guardian or family member to help assess the level to which he/she is able to understand the purpose and possible results of the genetic test and to provide informed consent (Fig. 1).90
With respect to asymptomatic individuals, there are concerns genetic testing may trigger an untoward psychological response, such as severe depression, anxiety, or even suicidal ideation.91 However, research studies and clinical experience indicate that the majority of those tested using a standardized counseling protocol demonstrated effective coping skills and absence of negative psychological reactions after several months and found the testing to be beneficial, although the long-term effects of predictive testing for EOAD remain to be seen.92–95 Common reasons for testing included concern about early symptoms of dementia, financial or family planning, and relief from anxiety.92
The Huntington Disease Society of America’s Guidelines for Genetic Testing for Huntington Disease (HD) is considered by many to be the gold standard for genetic testing for adult onset conditions.96,97 This guideline uses a multidisciplinary approach to facilitate autonomous decision making. It includes a two-part pretest and one or more posttest/disclosure genetic counseling sessions conducted in person, in the presence of a patientselected support person who accompanies the patient to all genetic counseling visits. It also uses a neurologic evaluation and a psychiatric evaluation. Through this process, the various physical, psychological, social, and family history factors that influence the pretest decision-making process are brought to light, allowing the individual to make an informed decision about genetic testing while minimizing the risk of adverse outcome.
APOE SUSCEPTIBILITY TESTING
Although the association of the APOE ε4 allele with AD was identified in 1993, APOE genotyping for predictive purposes is not routinely offered in a clinical setting.98 Because the ε4 allele is neither necessary nor sufficient to cause AD, there have been numerous consensus statements and articles that have recommended against using APOE genotyping for predicting AD risk.6,15,16,99–102 The primary reasons for this recommendation include low sensitivity and specificity of testing, lack of preventive options, and the difficult nature of effectively conveying probabilistic risk.103 In addition, the association data indicate that risk conferred by APOE differs between genders and possibly by ethnic group.66–68 Because group differences in relative risk could result from differences in the prevalence of environmental exposures, modifier gene variants, or other factors (e.g., the effects of hormones in the case of gender differences), these differences complicate test result interpretation.
Finally, the risk associated with the ε4 allele not only varies widely between studies but also is often reported as an odds ratio, which is difficult to translate into meaningful figures for individual counseling.68,104–107 Cumulative risk curves for first-degree relatives of patients with AD stratified by APOE genotype and gender have been published but do not take into consideration multiple first- and second-degree relatives affected with AD and are based only on population studies of individuals of European or African American descent.106,108,109
A series of three successive multicenter, randomized, controlled trials, called the Risk Evaluation and Education for Alzheimer’s Disease (REVEAL) study was initiated to evaluate the potential benefits and harms of APOE genotyping in the clinical context.108,110 Findings indicated that disclosing APOE genotype status to adult children of parents diagnosed with AD did not result in significant short-term psychological risk to this population.110 In addition, findings showed that the degree to which participants recalled the information they were given was a reflection on both the manner in which the risk was communicated and the complexity of the information itself, indicating the importance of good counseling.111 Approximately half of participants who correctly recalled their risk information actually believed their risk was significantly different than what was disclosed to them.112 This finding suggests that counselors should recognize a possible “anchoring and adjustment” bias whereby test recipients adhere to baseline risk perceptions even in the face of disconfirming evidence. The most common reasons for undergoing testing were desire for information, desire to feel in control, arranging personal care, advance planning, emotional coping.113,114 Another finding was that participants with an ε4 allele were more likely than other groups to report health behavior changes, including the new use of dietary supplements.115 Although improvements in health behavior may be a beneficial outcome, there is concern such individuals will be vulnerable to marketing of treatments or supplements in the absence of evidence-based recommendations (e.g., direct to consumer [DTC] nutrigenomics testing).116 Another behavioral outcome is that participants receiving an ε4 result were significantly more likely than controls to report long-term care insurance changes during the 1-year follow-up period.117 From a policy perspective, these findings suggest the need to discuss issues of potential genetic discrimination in light of limitations to current state and federal genetic discrimination legislation.
It should be noted that the REVEAL study is not representative of a typical clinical setting. The cohort was a preselected (having a parent with AD), self-selecting (chose to participate), highly educated group. In addition, REVEAL participants obtained testing free of charge, and results were not included in their medical record.118
GUIDELINES
Pediatric testing for AD should not occur. Prenatal testing for AD is not advised if the patient intends to continue a pregnancy with a mutation.
Genetic testing for AD should only occur in the context of genetic counseling (in-person or through videoconference) and support by someone with expertise in this area.
Symptomatic patients: Genetic counseling for symptomatic patients should be performed in the presence of the individual’s legal guardian or family member.
Asymptomatic patients: A protocol based on the International Huntington Association and World Federation of Neurology Research Group on Huntington’s Chorea Guidelines is recommended.
DTC APOE testing is not advised.
A ≥3-generation family history should be obtained, with specific attention to the age of onset of any neurologic and/or psychiatric symptoms, type of dementia and method of diagnosis, current ages, or ages at death (especially unaffected relatives), and causes of death. Medical records should be used to confirm AD diagnosis when feasible. The history of additional relatives may prove useful, especially in small families or those with a preponderance of early death that may mask a history of dementia.
A risk assessment should be performed by pedigree analysis to determine whether the family history is consistent with EOAD or LOAD and with autosomal dominant (with or without complete penetrance), familial, or sporadic inheritance.
Patients should be informed that currently there are no proven pharmacologic or lifestyle choices that reduce the risk of developing AD or stop its progression.
The following potential genetic contributions to AD should be reviewed:
 The lifetime risk of AD in the general population is approximately 10–12% in a 75–80-year lifespan.
The lifetime risk of AD in the general population is approximately 10–12% in a 75–80-year lifespan. The effect(s) of ethnicity on risk is still unclear.
The effect(s) of ethnicity on risk is still unclear. Although some genes are known, there are very likely others (susceptibility, deterministic, and protective) whose presence and effects are currently unknown.
Although some genes are known, there are very likely others (susceptibility, deterministic, and protective) whose presence and effects are currently unknown.
For families in which an autosomal dominant AD gene mutation is a possibility
Discuss the risk of inheriting a mutation from a parent affected with autosomal dominant AD is 50%. In the absence of identifying a mutation in apparent autosomal dominant families, risk to offspring could be as high as 50% but may be less.
Testing for genes associated with early-onset autosomal dominant AD should be offered in the following situations:
 A symptomatic individual with EOAD in the setting of a family history of dementia or in the setting of an unknown family history (e.g., adoption).
A symptomatic individual with EOAD in the setting of a family history of dementia or in the setting of an unknown family history (e.g., adoption). Autosomal dominant family history of dementia with one or more cases of EOAD.
Autosomal dominant family history of dementia with one or more cases of EOAD. A relative with a mutation consistent with EOAD (currently PSEN1/2 or APP).
A relative with a mutation consistent with EOAD (currently PSEN1/2 or APP).
The Alzheimer Disease & Frontotemporal Dementia Mutation Database should be consulted (www.molgen.ua.ac.be/ADMutations/) before disclosure of genetic test results, and specific genotypes should not be used to predict the phenotype in diagnostic or predictive testing (Table 2).
Table 2
Alzheimer disease web-based resources
| Organization | Website | Purpose |
|---|---|---|
| Alzheimer Research Forum | www.alzforum.org | Presents scientific findings in AD research, including basic research and clinical trials. Maintains public databases of research data, including association studies and mutation databases |
| AD&FTD database | www.molgen.ua.ac.be/ADMutations | Compiles mutations and nonpathogenic coding variations in the genes related to Alzheimer disease (AD) and frontotemporal dementia |
| National Institute on Aging | www.nia.nih.gov | Supports research related to aging and age-related diseases |
| Alzheimer’s Disease Education and Referral Center (ADEAR) and Alzheimer Disease Research Centers (ADC) | www.nia.nih.gov/alzheimers | NIA-sponsored ADEAR provides clinical information and resources, research studies, and current news related to AD. ADCs provide diagnosis and management, volunteer research opportunities, and support services |
| Alzheimer’s Association | www.alz.org | Provides information, programs, and services for people with AD and their family members, caregivers, residential care staff, and healthcare providers. They also fund research |
| GeneReviews | www.genetests.org | Contains a comprehensive overview of early-onset and late-onset AD and provides details on genotype/phenotype correlations when available. Lists resources for patients and families dealing with AD |
Discuss the likelihood of identifying a mutation in PSEN1, PSEN2, or APP, noting that current experience indicates that this likelihood decreases with lower proportions of affected family members and/or older ages of onset.
Ideally, an affected family member should be tested first. If no affected family member is available for testing and an asymptomatic individual remains interested in testing despite counseling about the low likelihood of an informative result (a positive result for a pathogenic mutation), he/she should be counseled according to the recommended protocol. If the affected relative, or their next of kin, is uninterested in pursuing tested, the option of DNA banking should be discussed.
For families in which autosomal dominant AD is unlikely
Inform them why their family history is consistent with familial or sporadic AD.
Discuss that both sporadic and familial cases can be due to a genetic susceptibility. Risk estimates are only available for first-degree relatives of an affected individual in sporadic or familial cases.
Genetic testing for susceptibility loci (e.g., APOE) is not clinically recommended due to limited clinical utility and poor predictive value. If a patient wishes to pursue testing despite genetic counseling and recommendations to the contrary, testing may be considered at the clinician’s discretion. Testing performed should follow the HD genetic testing guidelines, with emphasis on genetic counseling with a qualified clinician. As such, DTC genetic testing is not advised.
Motives and considerations for pursuing genetic testing should be explored. This counseling should be an exploration of personal experiences, value and beliefs, and personal and family needs. Genetic testing should be discussed within the context of adapting to familial risk and when clients feel compelled to learn a more refined estimate of their risks to enhance their quality of life. As part of this, it is helpful to lead the individual through the scenario of receiving a positive test result and a negative test result, having them assess the ways these results would positively or adversely impact their psyche, life plans, and relationships.
 Symptomatic patients: Because genetic testing of a symptomatic individual is typically requested by a relative concerned about his risk, the counselor must remain alert to any potential conflicts of interest, such as lack of interest of the symptomatic patient or of other at-risk family members. If the symptomatic patient gives any inclination of being averse to testing, it is not recommended. Instead, DNA banking should be explored.
Symptomatic patients: Because genetic testing of a symptomatic individual is typically requested by a relative concerned about his risk, the counselor must remain alert to any potential conflicts of interest, such as lack of interest of the symptomatic patient or of other at-risk family members. If the symptomatic patient gives any inclination of being averse to testing, it is not recommended. Instead, DNA banking should be explored.If there is disagreement within the family regarding whether testing should be performed, a family meeting is strongly encouraged (with or without the genetic counselor present). A family meeting would allow all interested parties to discuss the potential impact of the genetic testing on the family, how test results will be communicated, and how to respect the rights of those family members who do not wish to know the results.
Genetic testing: In the event testing is chosen, the following is recommended:
 Asymptomatic patients should receive a neurologic examination to assess for signs of dementia and to establish a baseline.
Asymptomatic patients should receive a neurologic examination to assess for signs of dementia and to establish a baseline. Assess patient’s and any accompanying family member’s psychological state of mind. In the case of presymptomatic testing, a consultation with a psychologist/psychiatrist may be recommended for the patient as part of the HD testing approach.
Assess patient’s and any accompanying family member’s psychological state of mind. In the case of presymptomatic testing, a consultation with a psychologist/psychiatrist may be recommended for the patient as part of the HD testing approach.- • If the patient seems to suffer from, or is potentially at risk for significant psychological/psychiatric problems, consider a psychotherapy referral before testing.
- • If the psychological assessment suggests testing is not in the person’s current best interest (e.g., untreated depression or recent death), these reservations should be shared openly, and an agreement should be made to revisit testing once the underlying condition and/or stressors have diminished. A referral for psychotherapy may also be appropriate.
 Assess and review the psychosocial impact of testing on the patient and his/her family.
Assess and review the psychosocial impact of testing on the patient and his/her family.- • Reinforce results cannot be “taken back” (although an individual can decide not to learn his or her test results after having the test performed.)
 Discuss testing logistics, associated costs, and possible outcomes.
Discuss testing logistics, associated costs, and possible outcomes.- • For EOAD genes, determine best approach to testing for patient (i.e., stepwise testing beginning with PSEN1 as the most likely gene or ordering a panel).
- • Discuss where results will be kept (e.g., medical record).
- • Determine who will accompany the patient to the result session for support.
- • Discuss possible test outcomes (positive, negative, or variant of uncertain significance). If testing for APOE, consider whether you will report other disease risk implications. If so, these should be included in the discussion of test outcomes with the patient. Also, it should be reiterated that APOE is a susceptibility gene and is not a predictive test. Thus, individuals with no copies of the ε4 allele still face a 2–4-fold increased lifetime risk of developing AD if they have a first-degree relative with AD.
 Assist the patient and participating family members with informed decision making regarding whom, if anyone, they plan to share the results with and how. Inform about the importance of discretion when discussing genetic testing and results.
Assist the patient and participating family members with informed decision making regarding whom, if anyone, they plan to share the results with and how. Inform about the importance of discretion when discussing genetic testing and results. Discuss the potential impact of genetic test results on insurance, and the benefits and limitations of existing state and federal genetic discrimination legislation.
Discuss the potential impact of genetic test results on insurance, and the benefits and limitations of existing state and federal genetic discrimination legislation. Obtain informed consent for all genetic testing for AD.
Obtain informed consent for all genetic testing for AD. After results disclosure, revisit the individual’s plans regarding with whom and how the results will be shared.
After results disclosure, revisit the individual’s plans regarding with whom and how the results will be shared. Arrange for a follow-up plan to “check in” with the patient and, if relevant, participating family member, and determine whether another genetic counseling session would be beneficial to the patient and/or the patient’s partner/family members/friends.
Arrange for a follow-up plan to “check in” with the patient and, if relevant, participating family member, and determine whether another genetic counseling session would be beneficial to the patient and/or the patient’s partner/family members/friends.
Discuss the availability and status of AD research and/or DNA banking.
Footnotes
Publisher's Disclaimer: Disclaimer: This document may not, in whole or in part, be reproduced, copied or disseminated, entered into or stored in a computer database or retrieval system, or otherwise utilized without the prior written consent of both the National Society of Genetic Counselors and American College of Medical Genetics.
The practice guidelines of the National Society of Genetic Counselors (NSGC) and the American College of Medical Genetics (ACMG) are developed by members of the NSGC and ACMG to assist geneticists, genetic counselors, and other health care providers in making decisions about appropriate management of genetic concerns; including access to and/or delivery of services. Each practice guideline focuses on a clinical or practice-based issue, and is the result of a review and analysis of current professional literature believed to be reliable. As such, information and recommendations within the practice guidelines reflect the current scientific and clinical knowledge at the time of publication, are only current as of their publication date, and are subject to change without notice as advances emerge.
In addition, variations in practice, which take into account the needs of the individual patient and the resources and limitations unique to the institution or type of practice, may warrant approaches, treatments and/or procedures that differ from the recommendations outlined in this guideline. Therefore, these recommendations should not be construed as dictating an exclusive course of management, nor does the use of such recommendations guarantee a particular outcome. Genetic counseling practice guidelines are never intended to displace a health care provider’s best medical judgment based on the clinical circumstances of a particular patient or patient population. Practice guidelines are published by NSGC and ACMG for educational and informational purposes only, and NSGC and ACMG do not “approve” or “endorse” any specific methods, practices, or sources of information. It also would be prudent to consider whether intellectual property interests may restrict the performance of certain tests and other procedures.
Disclosure: The authors declare no conflict of interest.
REFERENCES
Full text links
Read article at publisher's site: https://doi.org/10.1097/gim.0b013e31821d69b8
Read article for free, from open access legal sources, via Unpaywall:
http://www.gimjournal.org/article/S1098360021048115/pdf
Citations & impact
Impact metrics
Article citations
Updates in Alzheimer's disease: from basic research to diagnosis and therapies.
Transl Neurodegener, 13(1):45, 04 Sep 2024
Cited by: 0 articles | PMID: 39232848 | PMCID: PMC11373277
Review Free full text in Europe PMC
Navigating the future of Alzheimer's care in Ireland - a service model for disease-modifying therapies in small and medium-sized healthcare systems.
BMC Health Serv Res, 24(1):705, 05 Jun 2024
Cited by: 0 articles | PMID: 38840115
Expanded genetic testing in familial hypercholesterolemia-A single center's experience.
Am J Prev Cardiol, 18:100683, 19 May 2024
Cited by: 0 articles | PMID: 38828125 | PMCID: PMC11139767
2024 Alzheimer's disease facts and figures.
Alzheimers Dement, 20(5):3708-3821, 30 Apr 2024
Cited by: 59 articles | PMID: 38689398 | PMCID: PMC11095490
Validation of the "Perceptions Regarding pRE-Symptomatic Alzheimer's Disease Screening" (PRE-ADS) Questionnaire in the German Population: Attitudes, Motivations, and Barriers to Pre-Symptomatic Dementia Screening.
J Alzheimers Dis, 97(1):309-325, 01 Jan 2024
Cited by: 1 article | PMID: 38189757 | PMCID: PMC10789340
Go to all (168) article citations
Other citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
ADDENDUM: Genetic counseling and testing for Alzheimer disease: joint practice guidelines of the American College of Medical Genetics and the National Society of Genetic Counselors.
Genet Med, 21(10):2404, 01 Oct 2019
Cited by: 2 articles | PMID: 31217590
Statement on use of apolipoprotein E testing for Alzheimer disease. American College of Medical Genetics/American Society of Human Genetics Working Group on ApoE and Alzheimer disease.
JAMA, 274(20):1627-1629, 01 Nov 1995
Cited by: 31 articles | PMID: 7474250
Review
Genetic testing for late-onset Alzheimer's disease. AGS Ethics Committee.
J Am Geriatr Soc, 49(2):225-226, 01 Feb 2001
Cited by: 3 articles | PMID: 11207878
Genetic Counseling and Testing for Alzheimer's Disease and Frontotemporal Lobar Degeneration: An Italian Consensus Protocol.
J Alzheimers Dis, 51(1):277-291, 01 Jan 2016
Cited by: 13 articles | PMID: 26901402
Funding
Funders who supported this work.
NIA NIH HHS (2)
Grant ID: P50 AG008702
Grant ID: P50 AG008702-22