Abstract
Free full text

Targeted therapy against multi-resistant bacteria in leukemic and hematopoietic stem cell transplant recipients: guidelines of the 4th European Conference on Infections in Leukemia (ECIL-4, 2011)
Abstract
The detection of multi-resistant bacterial pathogens, particularly those to carbapenemases, in leukemic and stem cell transplant patients forces the use of old or non-conventional agents as the only remaining treatment options. These include colistin/polymyxin B, tigecycline, fosfomycin and various anti-gram-positive agents. Data on the use of these agents in leukemic patients are scanty, with only linezolid subjected to formal trials. The Expert Group of the 4th European Conference on Infections in Leukemia has developed guidelines for their use in these patient populations. Targeted therapy should be based on (i) in vitro susceptibility data, (ii) knowledge of the best treatment option against the particular species or phenotype of bacteria, (iii) pharmacokinetic/pharmacodynamic data, and (iv) careful assessment of the risk-benefit balance. For infections due to resistant Gram-negative bacteria, these agents should be preferably used in combination with other agents that remain active in vitro, because of suboptimal efficacy (e.g., tigecycline) and the risk of emergent resistance (e.g., fosfomycin). The paucity of new antibacterial drugs in the near future should lead us to limit the use of these drugs to situations where no alternative exists.
Introduction
There is a growing problem of antimicrobial resistance among the pathogens isolated from hematology patients and hematopoietic stem cell transplant (HSCT) recipients in many centers, and this increasingly influences the choice of empirical therapy.1 Resistance also affects the choice of ‘targeted’ therapy once a pathogen has been isolated, identified and subjected to susceptibility testing. In some cases, treatment options are very limited, and the emergence and proliferation of multiresistant Gram-negative organisms – both Enterobacteriaceae and non-fermenters – is forcing the renewed use of old antibiotics, notably colistin/polymyxin B and fosfomycin2–6 and of tigecycline. Similarly, the emergence of Gram-positive pathogens resistant to β-lactams and glycopeptides is leading to the use of linezolid, daptomycin and tigecycline in hematology patients.
These agents have not been extensively trialed in hematology patients; rather, their use is predicated on the lack of alternatives. Additional concern is that onco-hematological patients, and especially allogeneic HSCT recipients receive a lot of drugs (e.g., cyclosporine, mycophenolate mofetil, triazoles, antivirals) and they are likely more prone to drug-drug interactions than other populations. We should therefore reinforce the caution about the use of these antibiotics. For this reason, the European Conference on Infections in Leukemia (ECIL) group decided to review the published literature on the use of these non-conventional antibacterial agents for use against resistant Gram-negative and -positive pathogens in leukemic patients and HSCT recipients. The resulting draft guidelines, presented here, were discussed by the Expert Group at the ECIL-4 meeting in September 2011 and are based on published studies and expert opinion. Updated slide sets from ECIL-4 covering these aspects are available via the websites of the four organizations involved in ECIL (European Group for Blood and Marrow Transplantation, European Organization for Research and Treatment of Cancer, Immunocompromised Host Society, ECIL and European Leukaemia Net).7,8
Methods
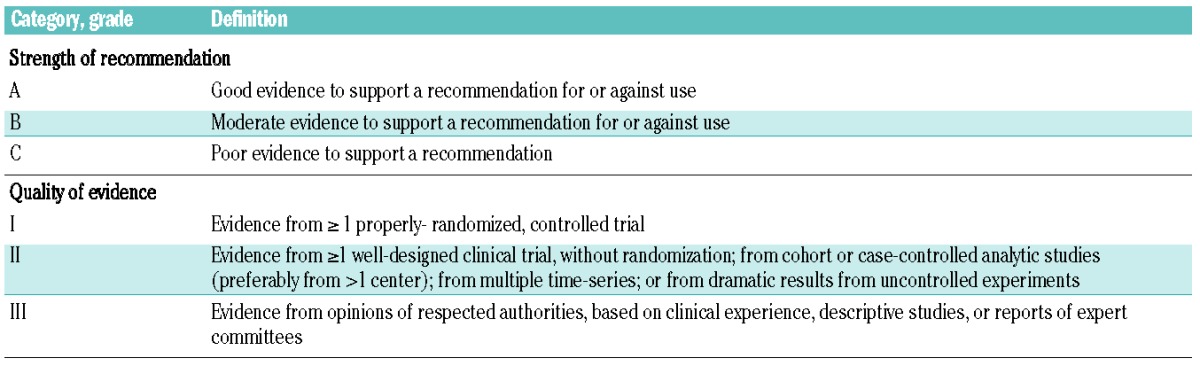
The methodology of the ECIL conferences was described previously;9 the quality of evidence and strength of recommendations were graded according to the criteria of the Infectious Disease Society of America (IDSA)10 (Table 1). A group leader (MA) was proposed by the organizing committee and experts were solicited to form the working group. The group reviewed the published English-language literature and prepared proposals on treatment options for infections due to resistant bacteria. Papers for review were sought using PubMed with the terms “linezolid”, “daptomycin”, “quinupristin/dalfopristin”, “colistin or polymyxin”, “tigecycline”, “fosfomycin”, “telavancin”, “ceftaroline” AND “stem cell transplantation or bone marrow transplant or leukemia or hematological malignancy or cancer”. References cited in the articles identified were also considered.
In respect of ‘Duration of therapy’, the main search terms used were “antibiotic therapy”; “stem cell transplantation or bone marrow transplantation or hematological malignancy or cancer”; “febrile neutropenia” and “duration therapy”, “discontinuation antibiotics” and “microbiologically documented infection”.
Definitions of resistance
A bacterial isolate was considered non-susceptible if it was categorized resistant, intermediate or non-susceptible when using clinical breakpoints of the European Committee on Antimicrobial Susceptibility Testing (EUCAST), Clinical and Laboratory Standards Institute (CLSI) or the US Food and Drug Administration (FDA). Definitions of ‘MDR’ vary among authors and usually presume resistance to at least two antibiotics used in empiric therapy (3rd4th -generation cephalosporins, carbapenems or piperacillin/tazobactam) or resistance to at least three of the following antibiotic classes: antipseudomonal penicillins, cephalosporins, carbapenems, aminoglycosides and fluoro-quinolones.11–15 According to the recent definition of the European Centre for Disease Prevention and Control (ECDC) and the Centers for Disease Control and Prevention (CDC), the isolate is considered MDR if it is non-susceptible to at least one agent in ≥3 therapeutically relevant antimicrobial categories.16
Results of the literature review
Resistant Gram-negative rods
Acquired resistance, now often encompassing carbapenems as well as other drug classes, is a growing problem in Enterobacteriaceae, Pseudomonas aeruginosa and Acinetobacter baumannii, whereas Stenotrophomonas maltophilia is inherently resistant to most antibiotics except co-trimoxazole (trimetoprim-sulfamethoxazole; TMP-SMX) and ticarcillin-clavulanate. The erosion of carbapenem activity against Enterobacteriaceae and A. baumannii largely reflects the spread of carbapenem-degrading enzymes, dubbed carbapenemases; these enzymes also occur in P. aeruginosa, although multi-resistance in this species, including to carbapenems, more often involves mutational reductions in permeability and up-regulation of efflux.17
Agents that retain some in vitro activity against most carbapenem-resistant Enterobacteriaceae isolates include tigecycline, colistin/polymyxin B, fosfomycin and – more variably – aminoglycosides. Interestingly, some carbapenemase-producing Enterobacteriaceae retain a degree of in vitro susceptibility to carbapenems and, if carbapenems are combined with other agents, they may still provide therapeutic benefit in these cases.18 In general, however, clinical data on the treatment of carbapenem-resistant Enterobacteriaceae infections are very limited and consist mainly of small case-series and brief reports.18–25 The prevalence of resistance in P. aeruginosa from HSCT patients varies across Europe, increasing as one moves south and eastward (ref. “Current etiology and resistance in bacterial bloodstream infections in hematology and oncology patients – literature review and ECIL-4 Surveillance Study.” M. Mikulska, C. Viscoli, C. Orasch, DM. Livermore, D. Averbuch, C. Cordonnier, M. Akova. Submitted for publication). In some centers, 25%–71% of P. aeruginosa isolates are MDR,11,14,15,26–30 leaving colistin/polymyxin B and (maybe) fosfomycin as the only treatment options.
Carbapenem-resistant A. baumannii may remain susceptible to sulbactam,31 a β–lactamase inhibitor that also has clinically relevant intrinsic antimicrobial activity against the organism.
Other antibiotics that show in vitro activity against some A. baumannii are colistin/polymyxin B and tigecycline.31 However, A. baumannii can develop resistance to tigecycline by mutation, with the trait sometimes selected in therapy;32–34 moreover some regionally prevalent MDR strains are non-susceptible to tigecycline.35
In the case of S. maltophilia, TMP-SMX is considered the treatment of choice, but resistance may arise and the sulfonamide component is poorly tolerated by some patients.36–39 Alternative agents against S. maltophilia proposed by some authors include the β-lactams, ticarcillin-clavulanate and ceftazidime; fluoroquinolones, with moxifloxacin reportedly active in vitro against some ciprofloxacin-resistant isolates from hematological patients;40 minocycline and chloramphenicol. Published cases series are small with variable success and drugs often in combination.37–39 The combination of TMP-SMX with either ticarcillin/clavulanate or with a third-generation cephalosporin (mainly ceftazidime) should be considered in neutropenic or severely ill patients.37,41,42 Review is further complicated because in vitro susceptibility testing for S. maltophilia is problematic, with results contingent on the medium (β-lactams) and temperature (aminoglycosides) used; the correlation with outcome is questionable.39
Treatment options against infections due to MDR Gram-negative rods in leukemic and HSCT patients are summarized in Table 2.
Table 2.
Main characteristics of the new or revisited antibacterial drugs for treatment of infections due to MDR Gram-negative bacteria.
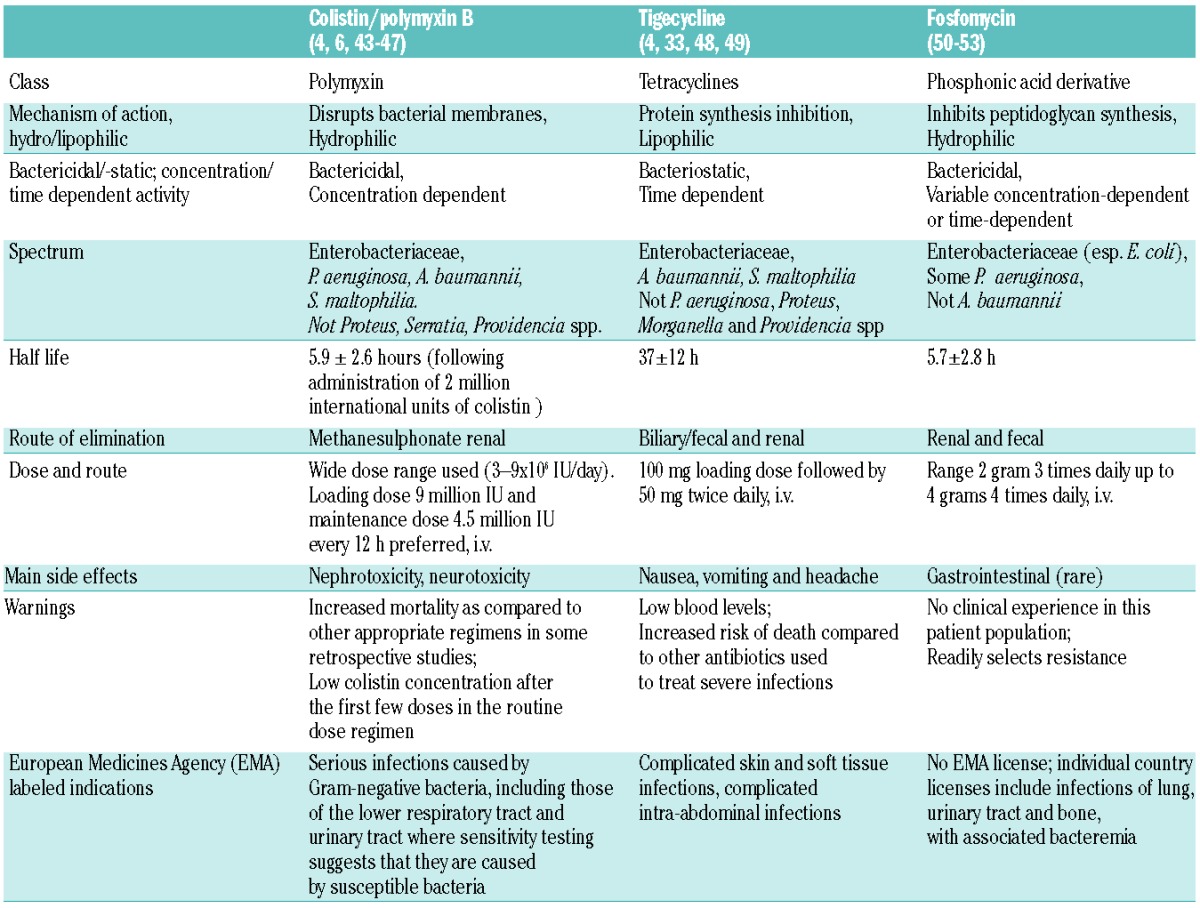
Tigecycline
Tigecycline has a broad-spectrum of in vitro activity against MDR Gram-positive and Gram-negative bacteria, excluding P. aeruginosa, Proteus spp., Providencia spp. and Morganella spp.22,38,54,55 However, evidence of increased mortality, compared to other antibiotic therapies, especially in ventilator-associated pneumonia48 leads to caution in its use. Moreover, a serious drawback, at least for monotherapy in bacteremia, is the low serum level obtained.33 Superinfections with pathogens inherently resistant to tigecycline (P. aeruginosa, Proteus spp., Providencia spp. and Morganella spp.) are another concern.32,56
Nevertheless, tigecycline was used at standard dosage, in combination with an anti-pseudomonal drug (β-lactams, quinolones, aminoglycosides) in 110 adult cancer patients (58% with hematological malignancies and 24% post-HSCT) as salvage therapy, for the treatment of refractory pneumonia (60%), bacteremia (17%) or other infections, which were microbiologically documented in 45% of the patients.57 Not all isolates were susceptible, or were tested to the antibiotics administered, concurrently with the tigecycline. Clinical response was achieved in 56% of transplant recipients, being higher in non-pseudomonas than pseudomonas infections (80% vs. 50%, P=0.06). Patients with pneumonia had lower response and higher mortality rates than those with bacteremia (51% vs. 79%, 44% vs. 16% respectively, both P<0.05).57 In another study, tigecycline was used at standard dosages for the treatment of serious hospital-acquired infections caused by MDR bacteria, including 50 patients (24%) with hematological malignancies. Alone or combined with other antibiotics, it showed efficacy in 16/23 (70%) of bacteremia cases and in 7/12 (58%) in whom it was used for empirical treatment of febrile neutropenia.58 Higher-dosage tigecycline regimens potentially may be advantageous in severe infections. A recent randomized study in patients with hospital-acquired pneumonia showed that clinical cure with tigecycline 100 mg twice daily after a loading dose of 200 mg (17/20, 85.0%) was numerically higher than with tigecycline 75 mg twice daily after a loading dose of 150 mg (16/23, 69.6%) and imipenem/cilastatin (18/24, 75.0%).59 Tigecycline may also benefit from combination. In a prospective multicenter trial of empirical for febrile neutropenic cancer patients, successful outcomes were reported in 126 of 164 (74%) treated with piperacillin-tazobactam plus tigecycline compared to 90 of 190 (47%) patients treated with piperacillin-tazobactam alone (P<0.01), although there was no difference in mortality. The success rate of the combined regimen was better than the piperacillin-tazobactam alone also in bacteremias (60% vs. 27%, P<0.01) and clinically documented infections (84% vs. 47%, P <0.01).60
Polymyxins
Colistin (polymyxin E) and polymyxin B, which were largely abandoned as systemic treatments from the 1960s and 70s, are now increasingly used as the last-resort treatment options against infections caused by MDR Gram-negative pathogens. Although several studies have presented case series with positive outcomes, treatment with colistin was associated with increased mortality as compared with other appropriate regimens in one retrospective study including a small number of onco-hematological patients.46 In another retrospective study, summarizing the efficacy of colistin in the treatment of infections due to MDR Gram-negative bacteria, multivariate analysis showed that presence of hematological disease, including malignancy, was itself associated with a decreased probability of survival.3 Two retrospective analyses that included patients with (mainly hematological) malignancies who were treated with colistin for MDR P. aeruginosa infections obtained differing results.5,61 In one study, 31-colistin-treated patients (45% with bacteremia, 55% with pneumonia) were compared to those (n= 64) treated with a non-colistin (β-lactam or quinolone) regimen. The colistin regimen achieved a higher rate of clinical response in multiple logistic regression analysis (P=0.026; odds ratio 2.9 (1.5, 7.6), whereas microbiological response (48% vs. 41%) and infection-related death rates (26% vs. 17%) were similar.5 The other study compared 26 patients (84% bacteremic) receiving colistin to 26 patients receiving anti-pseudomonal β–lactams and found similar rates of resolution of infection (77% vs. 65%) and mortality (11% in both groups).61 Nephrotoxicity, which was reported in up to 50% of patients receiving colistin/polymyxin B in older studies, is much less frequent in newer studies, with rates ranging from 10–30%.44 In the two Pseudomonas studies just cited, no significantly increased nephrotoxicity occurred in patients treated with colistin, as compared with other agents (including aminoglycosides), although one patient treated with colistin suffered from seizures.5,61 Among another 38 colistin treatment courses in adults and children with hematological malignancy or HSCT, nephrotoxicity developed in only 11%.62
The use of a 9-million-unit loading dose and high daily dosages (4.5 million units twice daily) of colistin47 may help to overcome the problem of low blood levels that may have been responsible for the suboptimal efficacy of polymyxins in some studies, leading to increased mortality, as well as to the selection of resistant strain variants.3,45,47,63 A recently-published prospective observational study in intensive care unit patients with severe infections due to Gram-negative bacteria susceptible only to colistin recorded clinical cures in 82% of cases when colistin was administered as a 9-million-unit loading dose followed by 9 million units daily, given in two doses, as maintenance therapy.64 Combination of colistin/polymyxin B with other agents to which the bacteria show in vitro sensitivity is strongly encouraged (e.g. with aminoglycosides and/or tigecycline for the treatment of infections due to Klebsiella pneumoniae with KPC carbapenemases).22–24 Nephrotoxicity following combination with aminoglycosides is of concern, though, and renal function should be monitored; moreover, most Enterobacteriaceae with NDM (rather than KPC) carbapenemases are broadly resistant to amino-glycosides.65
Fosfomycin
Fosfomycin is another old, but increasingly revisited, antibiotic with broad-spectrum in vitro activity against Gram-positive and -negative bacteria, excluding Acinetobacter spp. It is used mainly as an oral treatment for community-acquired urinary tract infection (UTI), but intravenous formulations are available in some countries. Several studies estimate 80–90% of Enterobacteriaceae with extended-spectrum β–lactamases (ESBLs) and carbapenemases to be susceptible to fosfomycin,51,66 but other studies report that only 50% of Klebsiella spp. and fewer than 30% of MDR P. aeruginosa to be susceptible.2,6 There are no universally accepted specific species-related susceptibility breakpoints;2 EUCAST has no breakpoints for fosfomycin vs. P. aeruginosa, but notes anecdotal evidence that it may be efficacious, in combination, against strains with minimal inhibitory concentrations (MICs) <128 mg/L.67 Due to the possibility of resistance developing during therapy, fosfomycin should be used in combination with other agents, selected according to the susceptibility results.51,68 Data on the efficacy of intravenous fosfomycin are limited to case reports and small case series51 and there is no published experience of treating invasive infections in onco-hematological and HSCT patients. A retrospective study in HSCT patients showed, that in a multivariate analysis, exposure to fosfomycin (route of administration not specified) was associated with a significantly decreased incidence of veno-occlusive liver disease.69
Sulbactam
Although sulbactam is conventionally used as a β-lactamase inhibitor, it also has inherent antibiotic activity against Acinetobacter spp.31 The package insert of sulbactam says that the maximum daily dose of sulbactam should not exceed 4 g. However, there are reports on dosages of sulbactam (combined with β lactams) of at least 6 g IV in divided dosages, assuming normal renal function.31,70 Furthermore, doses of up to 9–12 g/day were administered for ventilator-associated pneumonia with MDR Acinetobacter.71
Combination therapy in infections due to resistant Gram-negative bacteria
Several meta-analyses of randomized controlled studies, some of them done before the present era of increasing resistance, concluded that there was similar all-cause mortality in febrile neutropenic patients treated with a β-lactam vs. the same β-lactam plus an aminoglycoside as empirical or definitive therapy.72–74 However, owing to the small numbers of cases of infection due to resistant bacteria, a benefit of combination therapy could not be ruled out for those patients who were critically ill or were infected with P. aeruginosa or some other resistant pathogen.72–74
Combination antibiotic therapy also may simply improve the likelihood that at least one component agent is active.75 A retrospective study reviewed patients with hematological malignancies or post-HSCT, who were infected by ESBL- or AmpC-producing Enterobacteriaceae or resistant pseudomonas, most of whom were empirically treated with combination of a β-lactam and an aminoglycoside. Mortality was lower among those patients whose pathogen was sensitive in vitro to either the β-lactam or the aminoglycoside, compared with those whose pathogen was resistant to both (OR, 1.8; 95% CI, 1.3 to 2.5).76
Nevertheless, and in contrast, an early prospective randomized trial in non-neutropenic patients, in the era prior to the emergence of significant imipenem resistance, showed that the combination of imipenem plus netilmicin was no more efficacious than imipenem monotherapy for the treatment of severe infections, but did have increased nephrotoxicity, and did not prevent the emergence of imipenem-resistant P. aeruginosa.77
Some in-vitro data suggest synergy in combining two agents against carbapenemase-producing K. pneumoniae, even when the pathogen is resistant to one of these agents.78,79 Synergy was claimed for a combination of polymyxin B and either rifampin or doxycycline, resulting in at least a four-fold decrease in the MIC of polymyxin B when both drugs were used at physiologically achievable concentrations in one study.78 In another study a combination of fosfomycin with meropenem or colistin was asserted to be synergistic, based on 100-fold more extensive killing than with the more active single agent.79 Nevertheless there is a profound lack of clarity on when and how the various different measures of synergy used in vitro translate into clinical advantage; moreover there must be a concern about publication bias: studies that detect synergy are more likely to be reported and published than those that fail to do so.
Carbapenem-containing regimens were associated with significantly reduced mortality compared to non-carbapenem-containing regimens in a retrospective analysis of 138 patients who received treatment for infections due to carbapenemase-producing K. pneumoniae that showed susceptibility to carbapenems in vitro. Carbapenems may be a reasonable treatment option against carbapenemase-producing K. pneumoniae provided that: (i) the carbapenem MIC for the infecting organism is ≤4 mg/L; (ii) a high-dose prolonged-infusion regimen is administered to drive the pharmacokinetic/pharmacodynamic profile to acceptable exposures; and (iii) this class of agent is administered in combination with another active compound.21 The caveat is that many carbapenemase producers are more substantially resistant, precluding such strategies.
An ertapenem-doripenem combination may be of potential usefulness against KPC-producing K. pneumoniae based on a study in an immunocompetent murine thigh infection model based on the notion that the high affinity of KPC for ertapenem would “trap” the enzyme thus enhancing the activity of doripenem.80
Others have found that various combinations of rifampin, β–lactams, aminoglycosides, quinolones, colistin/polymyxin B, fosfomycin or other agents are synergistic in vitro, or in animal models, against MDR Pseudomonas or Acinetobacter spp.2,31,81,82 Many authors argue that rifampin should be considered for addition to other active antibiotics in the treatment of uncontrolled infection due to MDR bacteria,31,55,78,83–85 though there is little evidence of why rifampicin should improve outcome and no randomized trials to show that it does improve these outcomes. Further obstacles include: (a) there is no relevant in vitro breakpoint for susceptibility to rifampin against Gram-negative bacteria; (b) toxic potential of rifampin; (c) multitude of drug interactions between rifampin and other agents, a main concern especially in onco-hematological patients and allogeneic HSCT recipients who receive a lot of other drugs concomitantly (such as cyclosporine, mycophenolate mofetil, antifungals, antivirals).86
Notably, a randomized, open-label recently published clinical trial, which enrolled 210 patients with life-threatening infections due A. baumannii that were susceptible only to colistin showed that 30-day mortality was not reduced by addition of rifampicin.86
Publication of further observational studies assessing different monotherapies and combinations against MDR Acinetobacter or carbapenem-resistant Gram-negative bacteria is pending.87,88
Resistant Gram-positive pathogens
Treatment options against infections due to resistant Gram-positive bacteria in leukemic and HSCT patients are summarized in Table 3.
Table 3.
Main characteristics of the new or revisited antibacterial drugs for treatment of resistant Gram-positive bacteria.
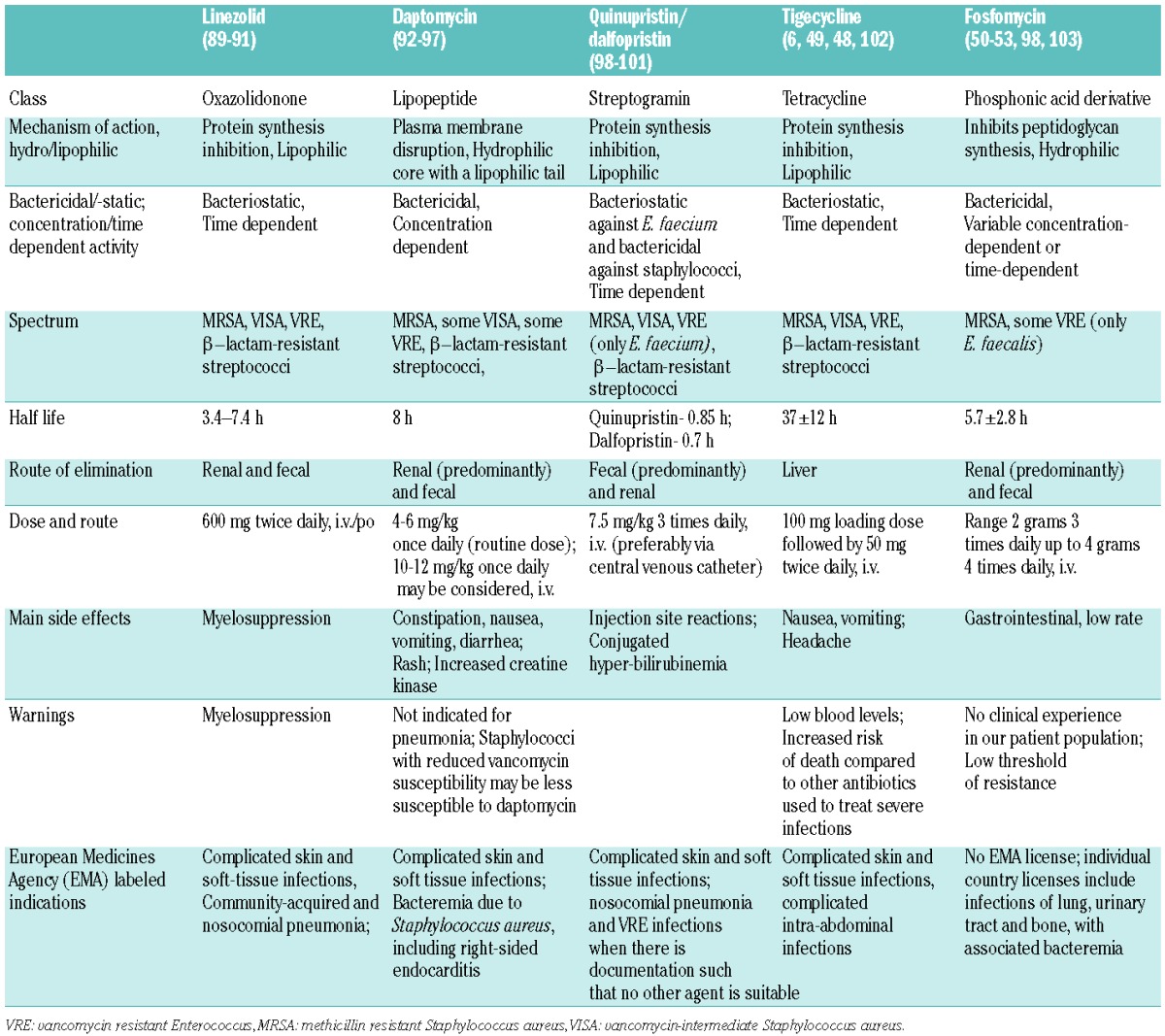
Glycopeptide non-susceptible Gram-positive bacteria include vancomycin-resistant enterococci (VRE) and vancomycin-intermediate and hetero-resistant Staphylococcus aureus (VISA and hVISA). There is also evidence that vancomycin MICs at the high end of the normal range for MRSA (2 mg/L) are associated with worse outcomes than MIC of <1 mg/L.104 Infections with VRE are prevalent in onco-hematological and HSCT patients in some countries105–110 but, until now, infections with VISA or hVISA remain rare in this patient population.111–113
Agents showing activity against some glycopeptide non-susceptible Gram-positive pathogens include linezolid, daptomycin, quinupristin/dalfopristin, tigecycline and fosfomycin, as well as the new agents telavancin and ceftaroline. The exact spectra of these agents vary and should be considered before use. Linezolid and tigecycline are almost universally active, whereas quinupristin/dalfopristin for example, does not cover E. faecalis, telavancin is inactive against VanA enterococci and ceftaroline lacks activity against E. faecium and is variable against E. faecalis.
Linezolid is the only one of these antibiotics that has been compared to vancomycin in a relevant prospective double-blind, multicenter equivalence study. This was performed in 605 febrile neutropenic cancer patients with proven (24%) or suspected Gram-positive infections: 94% had hematological malignancy. The study showed equivalent efficacy between vancomycin and linezolid in achieving clinical (87% vs. 86%) and microbiological (58% vs. 50%) success. Mortality rates, too, were similar (5.6% vs. 7.6%), though there were fewer drug-related adverse events with linezolid (17.2% vs. 24%; P=0.04).114 Another prospective, multicenter, open-label, non-comparative, non-randomized study examined the performance of linezolid in 103 neutropenic cancer patients with serious Gram-positive infections, mainly bacteremia. Most patients had VRE resistant to other therapies, or had a history of failure or intolerance to available agents. Linezolid achieved 79% clinical and 86% microbiological cure rates.115
Despite these positive findings, there is a concern about the thrombocytopenia and/or neutropenia found in some studies with linezolid. This side effect was seen in 2–11% of patients,115,116 although two further studies suggested that the incidence was similar to that with vancomycin.114,117 Other uncommon but serious adverse effects associated with linezolid include lactic acidosis, serotonin syndrome, and peripheral and optic neuropathies.118–120
Quinupristin/dalfopristin (QD) was compared to linezolid in a prospective randomized trial in 40 patients with hematological malignancies (a third were post-HSCT, 20% neutropenic) with VRE infections, predominantly bacteremia. Both regimens achieve comparable clinical (43% vs. 58%) and microbiological (71% vs. 90%) cure rates, with similar mortality (10% vs.16%).116 Comparable results were achieved in treating staphylococcal line-associated bacteremia with quinupristin/dalfopristin or vancomycin in a prospective randomized comparative study that included cancer patients.121 The response rate in vancomycin-resistant E. faecium infections, mainly bacteremias, was 55%-68% in two studies that largely included leukemia patients, including those with HSCT and neutropenia,122,123 in one of these studies quinupristin/dalfopristin was combined with minocycline.123 Arthralgia or myalgia developed in 6–36% of patients.99,122 Quinupristin/dalfopristin should preferably be administered via central venous catheter.99,122
Daptomycin treatment of probable or definite catheter-related bacteremia caused by Gram-positive bacteria resulted in a better overall response rate as compared with matched historical controls treated with vancomycin −68% vs. 32% (P=0.003);124 70% of these patients had hematological malignancy and 13% were post-HSCT. In another retrospective study, treatment with daptomycin led to improvement in 90% of 72 febrile cancer patients (82% with hematologic malignancies, 47% neutropenic) with infections, predominantly bacteremias, due to Gram-positive organisms.125 None of the patients required discontinuation of the daptomycin due to adverse effects.125 The MIC of daptomycin should be checked for staphylococci previously exposed or resistant to glycopeptides, as cross-resistance is possible, due to the thickened cell wall trapping daptomycin.93,95,126 Use in enterococcal bacteremia is off-label and MICs should be carefully checked, as those for E. faecium are commonly around 2–4 mg/L, well above the staphylococcal breakpoint.95 In a small report, only four of nine febrile neutropenic patients with vancomycin-resistant E. faecium bacteremia had clinical and microbiological cure with daptomycin, and only five survived for 30 days.127 In this context the use of daptomycin at 10–12 mg/kg daily-well above the currently licensed 4–6 mg/kg dose - may be justified, especially for high inoculum infections, but clinical data are limited and side effects remain to be evaluated in large-scale clinical trials.95,128,129
Tigecycline shows in vitro activity against glycopeptide-non-susceptible Gram-positive bacteria; studies that considered its activity were outlined above in the section on Gram-negative pathogens.57,58
Other new agents active against some resistant Gram-positive bacteria include lipoglycopeptides (e.g., telavancin) and anti-MRSA β-lactams (e.g. ceftaroline), whilst fosfomycin – an old agent - is active against many MRSA and VRE, especially E. faecalis, at least in vitro.103 As yet, though, there is no published experience with these agents in hematological and neutropenic patients.
Duration of targeted therapy
There are several studies reporting that the duration of treatment for microbiologically documented infections (MDI) is at least 7 days.130–137 Others reported on 10–14 days of therapy.138,139 Some studies required some evidence of bone marrow recovery.138–141 Repeated blood cultures had to be sterile, and control of local infection, if any, needed to be achieved. In a few of the studies patients were afebrile for at least 24 hours138–142 while in the other reports the patients were afebrile for at least 4–5 days.130,133,134,136,143
ECIL-4 recommendations
Based on in vitro susceptibility, the options for targeted treatment of infections due to resistant Gram-negative and Gram-positive bacteria are shown in Table 4. As most of these options have not been assessed in large randomized, prospective studies, at least in hematology populations, their use should be approached with caution and should be carefully discussed with the microbiologists or infectious diseases specialist, taking in account also the risk/benefit balance and safety profile of each drug on an individual basis.
Table 4.
ECIL4 Recommendations: targeted treatment of infections due to resistant Gram-negative and -positive bacteria (based on in vitro susceptibility).
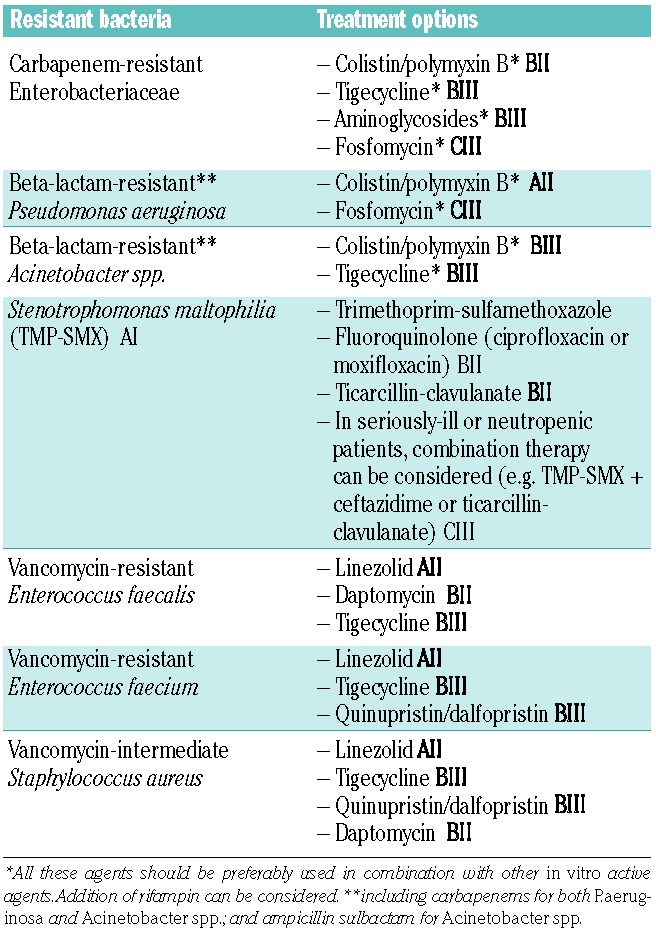
As shown in Table 4, colistin/polymyxin B are the preferred agents for treatment of infections due to β–lactam-resistant Enterobacteriaceae, so long as the organism is susceptible in vitro. A loading dose and high maintenance dose may be required.
Tigecycline has wide in vitro activity, but should be used with caution in bacteremia, as it achieves low blood levels. Alternatives should be considered in patients with severe infections, especially ventilator-associated pneumonia, due to the higher mortality seen in the tigecycline arms of comparative trials,48,144 Resistance can develop on treatment.
Combination therapy, based on in vitro susceptibility tests, should be considered when colistin/polymyxin B, tigecycline, aminoglycosides and fosfomycin are used for the treatment of infections due to resistant Gram-negatives. Addition of rifampin can be considered.
The options for targeted treatment of infections due to resistant Gram-positive bacteria are wider than against Gram-negative bacteria. If linezolid is used, monitoring of bone marrow recovery is important because of the possibility of myelosuppression. Patients with suspected or overt pneumonia should not be treated with daptomycin, which is inactivated in lungs.
In general, the patient should be treated using narrower-spectrum agents active against the pathogen identified, if it is plausible and/or clinically significant, guided by in vitro susceptibility tests, including MICs when available, and based on knowledge on drugs with specific activities (e.g. TMP-SMX for S. maltophilia) AI.
Penicillins and penicillin/β-lactamase inhibitors should be preferred over cephalosporins and carbapenems if they have comparable in vitro activity, spectrum of coverage and drug concentration at site of infection BII. A more drastic narrowing of the antibiotics could be envisaged if a fully-susceptible organism is documented from blood cultures of a stable patient under hospital observation, e.g. step down to an amino- or ureido- penicillin (ampicillin or piperacillin) when an α-haemolytic streptococcus is isolated BIII.
Duration of targeted therapy for microbiologically documented infections
Antibiotic treatment should be continued for at least 7 days, until the infection is microbiologically eradicated and all clinical signs of infection are resolved, with the patient afebrile for at least 4 days BIII. If the patient is still neutropenic and antibiotic therapy is stopped, (s)he should be kept hospitalized under close observation for at least 24–48 hours. If fever recurs, antibiotics should be restarted urgently after obtaining blood cultures and performing other relevant evaluation based on clinical judgment.
Centers that give prophylactic antibacterial agents should consider renewing this regimen upon discontinuation of targeted antibiotic therapy, if the patient is still neutropenic CIII.
Discussion
BSI develops in 13% to 60% of HSCT recipients14,26,108,145–147 and in 21–36% of neutropenic leukemia patients.131,136,146,148–151 Rates in other hematology patients are less well documented.
It is of utmost importance to recognize infections due to resistant bacteria and to target the therapy appropriately, based on: (i) in vitro susceptibility, (ii) knowledge of the best treatment option against the particular species and resistance phenotypes, and (iii) a careful assessment of the risk-benefit balance, according to the expected toxicity of the drug(s). Narrower-spectrum agents should be used whenever possible, so long as they have equivalent activity and efficacy. Pharmacokinetic and pharmacodynamic data in individual situations should also be taken in account.
Combinations of antibiotics are often required, as resistance can develop on treatment (e.g., fosfomycin), or because of suboptimal efficacy as monotherapy (e.g., tigecycline). Nevertheless the evidence that combinations improve outcomes or prevent the emergence of resistance is scanty at best, and the relationship of in vitro and in vivo synergy is unclear.
The paucity of new antibacterial drugs expected in the near future should lead us to limit the use of the drugs discussed here to documented infection where there is no other alternative. In this context, a strong collaboration is needed between the hematologist, microbiologist, antimicrobial pharmacist and infectious disease specialist. The best treatment option is uncertain in many cases, and many combinations have not been formally assessed, precluding recommendations based on the principles of “evidence-based medicine”. There is a great need to study and monitor the efficacy of these non-conventional antibiotics in the leukemic population.
Whilst current increases in bacterial resistance among leukemic and HSCT patients restrict treatment choices and force the use of the compounds discussed here, it should never been forgotten that they are poorer therapies than the compounds they replace, with clear evidence that colistin and tigecycline are inferior to other antibiotics if the pathogen is susceptible to them.46,48,144 If the underlying problem is the spread of resistant clones of bacterial among the patients in a unit, the best answer is the reinforcement of infection control, not the use of more exotic and complex antimicrobial chemotherapy. Antimicrobial stewardship, aiming to minimize unnecessary broad spectrum antibiotic use and its associated collateral damage and resistance selection is likewise crucial in the present era of growing resistance.
Acknowledgments
The authors would like to thank the participants of the ECIL 4 meeting:
Hamdi Akan, Murat Akova, Turkey; Diana Averbuch, Israel; Rose-Mary Barnes, United Kingdom; Nicole Blijlevens, The Netherlands; Thierry Calandra, Switzerland; Elio Castagnola, Simone Cesaro, Italy; Catherine Cordonnier, France; Oliver Cornely, Germany; Jean-Hughes Dalle, France; Rafael de la Camara, Spain; Emma Dellow (Gilead Sciences) United Kingdom; Peter Donnelly, The Netherlands; Lubos Dgrona, Slovakia; Hermann Einsele, Germany; Dan Engelhard, Israel; Bertrand Gachot, France; Corrado Girmenia, Italy; Andreas Groll, Germany; Ingeborg Gyssens, The Netherlands; Werner Heinz, Germany; Raoul Herbrecht, France; Hans Hirsch, Switzerland; William Hope, United Kingdom; Petr Hubacek, Czech Republic; Chris Kibbler, United Kingdom; Galina Klyasova, Russia; Sean Knox (Astellas Pharma), United Kingdom; Michal Kouba, Czech Republic; Catherine Lagrou, Belgium; Thomas Lernbecher, Germany; Per Ljungman, Sweden; Johan Maertens, Belgium; Oscar Marchetti, Switzerland; Rodrigo Martino, Spain; Georg Maschmeyer, Germany; Tamas Masszi, Hungary; Suzanne Matthes-Martin, Austria; Małgorzata Mikulska, Alessandra Micozzi, Italy; Bilal Mohty, Switzerland; Patricia Munoz, Spain; David Nadal, Christina Orasch, Switzerland; Zdenek Racil, Czech Republic; Patricia Ribaud, France; Valérie Rizzi-Puechal (Pfizer), France; Emmanouil Roilidis, Greece; Janos Sinko, Hungary; Jan Styzynski, Poland; Alina Tanase, Hungary; Mario Tumbarello, Italy; Paul Verweij, The Netherlands; Claudio Viscoli, Italy; Kate-Nora Ward, United Kingdom; Aafje Warris, The Netherlands; Craig Wood (Merck), USA.
The authors would like to thank Jean-Michel Gosset and the staff of KOBE, group GL Events, Lyon, France, for the organization of the meeting.
Footnotes
Funding
The ECIL-4 meeting has been supported by unrestricted educational grants from Astellas Pharma, Gilead Sciences, Merck, Novartis and Pfizer.
Companion papers
European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of emerging resistance: summary of the 4th European Conference on Infections in Leukemia (ECIL-4, 2011). Diana Averbuch, Christina Orasch, Catherine Cordonnier, David M Livermore, Małgorzata Mikulska, Claudio Viscoli, Inge C. Gyssens, Galina Klyasova, Oscar Marchetti, Dan Engelhard, Murat Akova.
The role of antibiotic stewardship in limiting antibacterial resistance among hematology patients. Inge C. Gyssens, Winfried V. Kern and David M. Livermore.
Authorship and Disclosures
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version of this article at www.haematologica.org.
References
Articles from Haematologica are provided here courtesy of Ferrata Storti Foundation
Full text links
Read article at publisher's site: https://doi.org/10.3324/haematol.2013.091330
Read article for free, from open access legal sources, via Unpaywall:
https://haematologica.org/article/download/6858/39705
Citations & impact
Impact metrics
Article citations
Carbapenem Versus Non-carbapenem Therapy in Hematology Patients: Extended-Spectrum Beta-Lactamase Positive Enterobacteriaceae Colonization Impact.
Cureus, 16(7):e63570, 01 Jul 2024
Cited by: 0 articles | PMID: 39087172 | PMCID: PMC11289854
Reactivation of cytomegalovirus and bloodstream infection and its impact on early survival after allogeneic haematopoietic stem cell transplantation: a multicentre retrospective study.
Front Microbiol, 15:1405652, 19 Jun 2024
Cited by: 0 articles | PMID: 38962143 | PMCID: PMC11219566
Short-term chemotherapy-related complications and undernutrition in children diagnosed with cancer at Korle Bu Teaching Hospital, Accra, Ghana: A prospective cohort study.
PLoS One, 19(3):e0301208, 28 Mar 2024
Cited by: 0 articles | PMID: 38547211 | PMCID: PMC10977704
Rare tuberculosis in recipients of allogeneic hematopoietic stem cell transplantation successfully treated with contezolid-a typical case report and literature review.
Front Cell Infect Microbiol, 13:1258561, 16 Oct 2023
Cited by: 1 article | PMID: 37908760 | PMCID: PMC10614019
Review Free full text in Europe PMC
Hospital survival following pediatric HSCT: changes in complications, ICU therapies and outcomes over 10 years.
Front Pediatr, 11:1247792, 12 Oct 2023
Cited by: 1 article | PMID: 37900687 | PMCID: PMC10601648
Go to all (71) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Retrospective evaluation of intravenous fosfomycin in multi-drug resistant infections at a tertiary care hospital in Lebanon.
J Infect Dev Ctries, 15(9):1308-1313, 30 Sep 2021
Cited by: 3 articles | PMID: 34669601
European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance: summary of the 2011 4th European Conference on Infections in Leukemia.
Haematologica, 98(12):1826-1835, 01 Dec 2013
Cited by: 250 articles | PMID: 24323983 | PMCID: PMC3856957
Multidrug-resistant Gram-negative infections: what are the treatment options?
Drugs, 69(14):1879-1901, 01 Oct 2009
Cited by: 161 articles | PMID: 19747006
Review
Antibiotic resistance in cancer patients.
Expert Rev Anti Infect Ther, 12(8):1003-1016, 16 May 2014
Cited by: 37 articles | PMID: 24834465
Review