Abstract
Free full text

Concurrent hyperbaric oxygen therapy and intratympanic steroid application as salvage therapy after severe sudden sensorineural hearing loss
Key Clinical Message
Concurrent hyperbaric oxygen therapy (HBOT) and intratympanic steroid application (ITS) are beneficial as salvage therapy for therapy‐refractory sudden sensorineural hearing loss (SSNHL). The findings encourage further research on the treatment of noise‐induced and idiopathic SSNHL with concurrent use of HBOT and ITS respecting also patients with long‐term or therapy‐refractory SSNHL.
Introduction
Sudden sensorineural hearing loss (SSNHL) is defined as a loss of hearing of 30 dB or more over at least three contiguous frequencies. Usually, symptoms present unilaterally and suddenly within 24–72 h. Most of the cases are referred to as idiopathic sensorineural hearing loss (ISSNHL) since etiologies remain unclear in the majority of the patients. Sudden SNHL occurs in five to 20 cases per 100,000 per year in the United States 1, 2. A spontaneous recovery can be observed in up to 65% 3 of the patients. The rate of spontaneous recovery was rated between 25 and 89% according to recent publications 4. Different treatment regimens like antioxidants, corticosteroids, vasodilatators, hyperbaric oxygen (HBO), or carbogen therapy 5 have been described. Among these approaches, steroid treatment is the most common.
Steroids can be applied systemically (intravenously or orally) or by intratympanic injection. Intratympanic injection of steroids (ITS) is regarded as effective, safe, and well tolerated 6, and was shown to be as sufficient as orally applied steroids 7, 8. Although many studies have reported on the usefulness of steroids, the authors of a recent Cochrane review came to the conclusion that the value of steroids in the treatment of ISSNHL remains unclear 9.
For the treatment of ISSNHL, HBOT has been applied over decades either alone or in addition to other medical treatments 10. In combination with HBOT, the overall success rate of ITS was superior when compared to i.v. steroid application 11. However, HBOT in addition to application of a vitamin cocktail and dexamethasone, did not improve chronic ISSNHL in another study 12. Nevertheless, since benefits of HBO in the treatment of ISSNHL were demonstrated 13, the Committee of the Undersea and Hyperbaric Medical Society approved ISSNHL as indication for HBOT 14. These authors claim that best results are achieved when HBOT starts within 2 weeks and is combined with steroid treatment. The combination of HBOT with systemic steroid treatment was especially successful for patients with an initial hearing loss of more than 90 dB 15. Additionally, HBOT resulted in an improvement of thresholds especially in the low frequencies of patients with otherwise therapy‐refractory SSNHL 16. In another study, ITS was compared to HBOT and to a combination of both after unsuccessful systemic corticoid treatment of ISSNHL 17. All three modalities resulted in an improvement of word scores and pure tone audiometry (PTA). However, the highest success was achieved, especially at low frequencies, after the combined use of HBOT and ITS. Despite of the excellent results that can be achieved after treating patients with acute ISSNHL (duration max. 2 weeks) with HBO, data concerning the outcome of HBOT of patients with chronic (>6 months) ISSNHL have not been reported hitherto 18. We therefore present a case study on patients with severe ISSNHL receiving HBOT combined with ITS as salvage treatment after an unsuccessful attempt with systemic steroids application. In most of the cases, the delay between onset of hearing loss and start of the combined therapy was much more than the recommended maximum of 30 days 17.
Patients and Methods
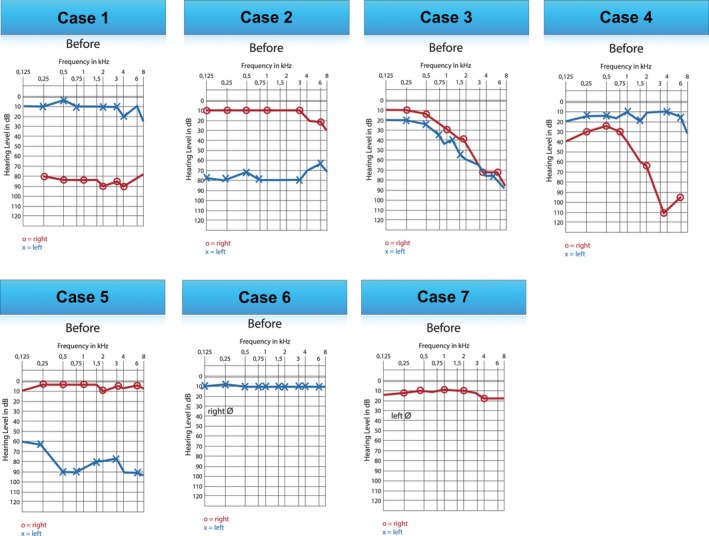
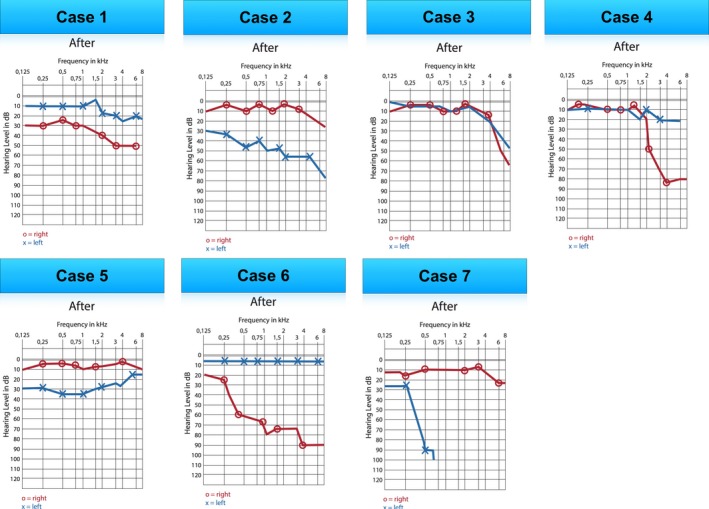
Over 4 months, we prospectively identified seven consecutive cases (three female and four male) with idiopathic (case 1, 2, 4, and 6), noise – (case 3 and 5), or barotrauma (case 7)‐induced SSNHL. Most of the patients presented after unsuccessful corticoid treatment with the symptoms persisting for up to 10 weeks (Table 1). In every patient, diagnostic tests were performed in order to rule out neurologic, vascular, or other etiologies for the hearing loss. Most of the patients were pretreated according to the guidelines of the German Society of Otorhinolaryngology for idiopathic hearing loss elsewhere. All patients, except for cases 3 and 7, had been subjected to unsuccessful treatment with systemic corticoids elsewhere prior to being referred to our institute (H. L, C.F. M‐K). Patients received bilateral paracentesis and ITS (dexamethasone with hyaluronic acid), and were immediately transferred to the HBO chamber (2.5 ATM for 2 × 30 min for each session). Thresholds were determined by PTA before the start and after finishing the salvage treatment at frequencies between 125 Hz and 8 kHz. In Figure Figure1,1, the PTAs of all seven patients at the time of their first presentation to our institute are depicted.
Table 1
Patients demographics and case presentation
| Age | Gender | Vertigo/Tinnitus | Days from onset of HL to treatment | Previous treatment | |
|---|---|---|---|---|---|
| Case 1a | 62 | Male | no/no | 5 weeks | Syst. and oral corticoids, IST |
| Case 2 | 43 | Female | no/yes | 6 days | Syst. corticoids |
| Case 3b | 34 | Male | no/yes | 3 weeks | None |
| Case 4 | 54 | Male | no/no | 4 weeks | Syst. and oral corticoids |
| Case 5 | 30 | Male | no/no | 10 weeks | Syst. corticoids |
| Case 6 | 25 | Female | no/no | 4 weeks | Syst. corticoids |
| Case 7c | 49 | Female | no/no | 3 days | None |
Case 1 presented 5 weeks after SSNHL before salvage therapy, after unsuccessful treatment with systemic corticosteroids starting 3 days after the onset of unilateral ISSNHL and ITS (four injections) without HBOT, the patients was referred for salvage treatment to our institution. Case 2 experienced ISSNHL. Intravenous steroid application was initiated immediately after onset. Since no benefits of this therapy could be detected within 6 days, the patient was referred to our institute for ITS and HBOT. Case 3 experienced bilateral hearing loss and tinnitus after intense noise exposure over several hours. He was presented at our institute, 3 weeks after the onset of the symptoms without being subjected to any other treatment or diagnosis earlier. After other conditions than the noise exposure were excluded as causes for SSNHL, HBOT and intratympanic steroid application (ITS) were initiated. Case 4 received systemic followed by oral corticoid treatment after development of an ISSNHL. The therapy started 2 days after detection of the symptoms. However, his symptoms did not improve and he presented 4 weeks later to our institution. Case 5 developed combined hearing loss after noise trauma (explosion), accompanied by contusio labyrinthi. He was treated with systemic steroids immediately over a period of 10 days without success. Ten weeks after the noise incidence, the patient sought for salvage treatment in our institute and received concurrent HBOT with ITS. Case 6 received unsuccessful systemic corticoid treatment immediately after development of a profound ISSNHL at the right side. Approximately 4 weeks later, she was referred to our institute for salvage treatment. Case 7 experienced left sided complete hearing loss after lifting a heavy stone. Although she was advised for a tympanoscopy to rule out and treat a rupture of the round window membrane, she refused surgery and was referred to our institute 3 days after the incidence.
Results
Patients' demographics and history are summarized in Table 1. In this cases series, four male and four female patients with an age range from 25 to 62 years were included. All patients experienced unilateral SSNHL, except case 3 who presented with bilateral hearing loss and tinnitus after severe noise trauma. Hearing thresholds improved in all patients after the combination of ITS and HBOT. Audiograms for all cases after salvage treatment are provided for both ears in Figure Figure2.2. In case 1, after 10 courses of HBOT with three concurrent ITS, an improvement of hearing in the right ear could be achieved. Case 2 showed a significant recovery of hearing and vanishing of her tinnitus after 33 courses of HBOT, accompanied by six ITS. In case 3, combined HBOT and ITS lead to a dramatic improvement of hearing also in the higher frequencies. The tinnitus disappeared at both sides. Case 4 received 20 courses with HBOT with five ITS and his hearing recovered mainly in the lower frequencies. In case 5, combined HBOT (20×) and ITS (3×) resulted in dramatic improvement of the left‐sided hearing threshold. After 30 HBOT and five ITS, case 6 regained hearing especially in the lower frequencies. Case 7 achieved recovery of hearing only in the lower frequencies (33 × HBOT; 13 × ITS).
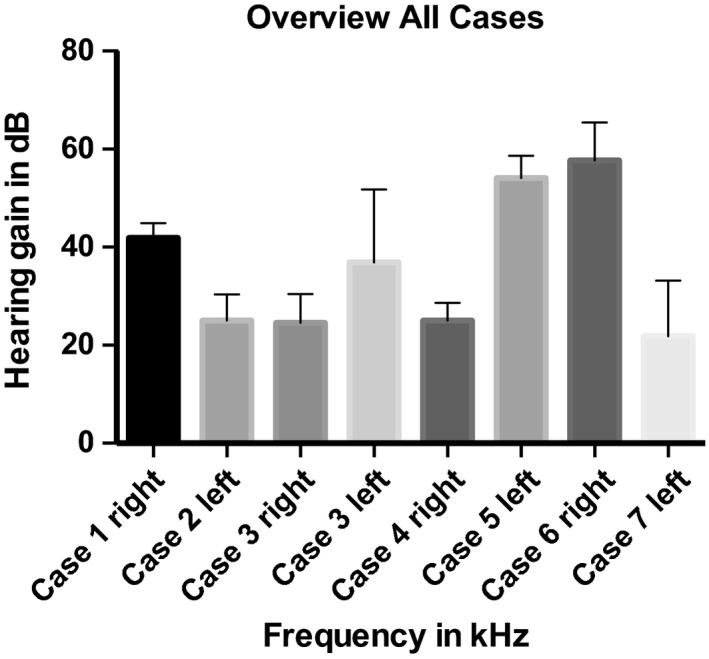
The PTA performed before treatment revealed pantonal hearing loss in all patients. In some of the patients, the hearing loss was more pronounced in the higher frequencies. All patients experienced an improvement of hearing. In addition, all patients experienced and reported substantial relieve from their symptoms during the course of the salvage therapy. The average gain in hearing for all cases (and for case 3 for each ear) is presented in Figure Figure3.3. The lowest gain (20 dB) was achieved in case 7 (barotrauma) even though treatment started already on day three after the trauma without any steroids as pretreatment. The mean improvements gained in patients suffering from noise‐induced SSNHL (37.2 dB) and ISSNHL (36.9 dB) were comparable. Some patients experienced huge benefits (more than 50 dB gain for case 5 and 6), whereas some only gained about 25 dB (case 2 and case 3r).
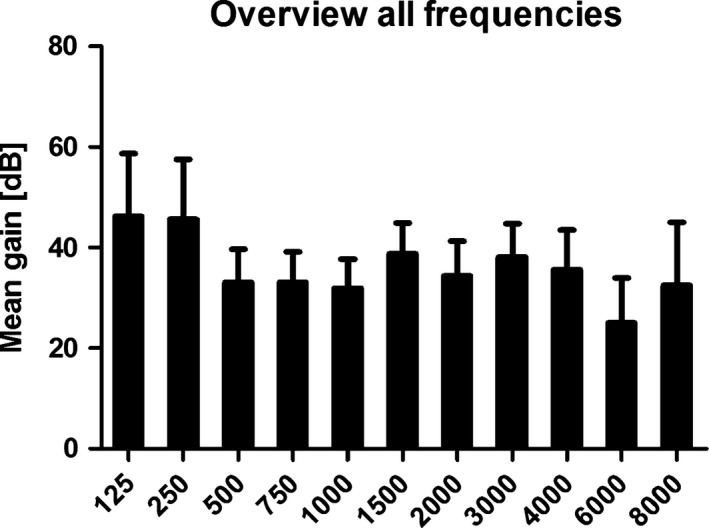
In general, the improvement was larger at low frequencies (Figure (Figure4),4), whereas at high frequencies, not all patients could benefit. The average gain ranged between 15 dB for 8 kHz and 46.4 dB for 0.125 kHz. For all patients, no side effects due to HBOT or other applied therapies could be observed.
Discussion
Randomized controlled trials concerning the benefit of anti‐inflammatory treatment with corticoids in patients with SSHL are contradictory in outcome. A meta‐analysis published and recently updated in the Cochrane library concludes that the value of steroids in the treatment of ISSNHL still remains unclear 9, even though oral or systemic steroid application is recommended as treatment of SSNHL by the Guidelines of the American Academy of Otolaryngology‐Head and Neck Surgery 19. Intratympanic injection of steroids (ITS) for the local application has recently emerged to a promising treatment modality for SSNHL 6, 11. This is favorable as it minimizes systemic side effects 20 especially in patients with contraindications for the systemic application of corticosteroids, e.g., diabetic patients 21.
In recent years, combined application of steroids and HBOT for the treatment of SSNHL as salvage therapy has become more popular since promising results were achieved 17, 22. Only in one of these studies, HBOT and ITS were applied concurrently in patients refractory to other treatment regimen, and partial or even full hearing recovery in the low frequencies was achieved in most of the patients 17. In this study, the salvage therapy was started <1 week after the onset of hearing loss in all patients included. By contrast, in the herein presented series of patients, most of them with chronic SSNHL, we have shown that concurrent application of both ITS and HBOT can alleviate the symptoms even if the onset of the symptoms was several months ago. The highest mean gain was achieved in the low frequencies. The lowest recovery rate was achieved in a patient with barotrauma, even though treatment started as early as 3 days after the onset of hearing loss (case 7). Here, other effects might have contributed to the hearing loss, for example, the rupture of the round window. Nevertheless, some low‐frequency hearing was regained even in this case.
The duration of the therapy was dictated by the improvement of the symptoms. These were documented by PTA and were also based on the subjective improvement as reported by the patients at each consultation. However, evaluation of patients' satisfaction using standardized measures such as visual analog scala was not performed.
Regarding possible mechanisms for the positive results achieved, some further aspects will be discussed. Permeability of the round window membrane, clearance as well as the longitudinal perilymph flow rate are interindividual factors that influence accumulation of pharmacologically active substances from the cavum tympani to the perilymph. After ITS, a rapid loss of the drug may occur due to the clearing functions of the eustachian tube 23. In order to accumulate in the perilymph, the round window seems to be the dominant route to the inner ear 24. The size, concentration, solubility, and electrical charge of the drug affect its permeation through the round window membrane 25, 26. In addition, the thickness and the state of the round window membrane strongly influence the permeability of the drug. After transtympanic administration of gadolinium and monitoring of the three‐dimensional distribution using magnetic resonance imaging, permeability of the round window membrane was impaired in approximately 20% of the patients 27. Therefore, it is not surprising that some of the patients with SSNHL remain unresponsive to both systemic and intratympanic steroid application. For these patients, concurrent application of ITS and HBOT might present a successful treatment regimen.
We speculate that higher concentrations of corticoids may accumulate in the perilymph under HBOT due to a potentially increased permeability of the round window membrane and that increased partial oxygen pressure may account for the benefits experienced by the patients included in our study. However, there is hitherto no evidence available to support this hypothesis. Trying to understand the mechanisms that are involved, a closer look to the round window membrane is important. The round window membrane is known to be semipermeable. For example, substances like gentamycin and dexamethasone are able to pass the membrane under normal conditions, whereas bigger molecules, such as albumin, are not 28. The permeability of the round window membrane changes under pathological conditions, for example, middle ear infection, and larger molecules are then able to penetrate to the inner ear 29. After application via the cavum tympani, substances (e. g., glucocorticoids) penetrate through the round window membrane and generate a gradient in the cochlea 30. For dexamethasone, baso‐apical differences in concentration up to a factor of 1000 have been measured in guinea pigs 30. These results show that the delivered substances mainly accumulate in the basal turn of the cochlea 30. Since permeability of the round window membrane can be modulated by pathological conditions, it seems likely that HBOT may also influence its properties. To sufficiently explain the results obtained under this regimen, many pathophysiological mechanisms have to be considered and further investigations need to be performed. A hyperbaric environment may facilitate the diffusion rate of chemicals in solution, such as of corticoids into the perilymph through the round window membrane. Transport functions via gap junctions and the mechanism behind could also play a role in the transport of substances into the cochlea. Gap junctions allow the passage of molecules up to a size of approximately 2 nm 31. Some of them are mechanosensitive 32 and their state can be influenced, for example, by temperature. Kniggendorf et al. 33. postulate that in lower temperature ranges, only small molecules can pass. At higher temperature ranges, beginning with 23°C, the passage of bigger molecules becomes possible. Considering these data, pressure‐dependent behavior seems to be likely.
A synergistic effect of ITS and HBOT has been proposed in order to explain the gain of threshold: on the one side, steroids reduce inflammation in the inner ear that may be contributing to hearing loss, on the other side, HBOT increases the intracochlear aiding in the recovery of hearing 17. However, based on our experience, the hearing recovery may be achievable even if the onset of SSNHL was several weeks to months ago, if the patients were attributed to HBOT immediately after ITS. In addition to the synergistic effort in reducing edema in the inner ear, we assume that HBOT changes the permeability of the round window membrane allowing increased influx of steroids into the perilymph, especially into the basal turn of the cochlea, where dexamethasone levels can be expected to be the highest. This may explain the recovery of hearing not only in the low frequencies but also in the high frequencies that are more refractory to recovery treatment.
Earlier studies have reported on the role of HBOT in order to enhance results achieved by systemic or oral steroid application 15, 22. The partial pressure of oxygen in the scala tympani in an experimental setting increased resulting in the protection of neurosensory cells and restoration of the oxidative metabolism in the vascular strip 34. In addition, HBOT improves rheology and microcirculation by lowering the blood viscosity and improving erythrocyte elasticity 35.
The Guidelines of the American Academy of Otolaryngology–Head and Neck Surgery 19 state that the evidence supports a possible benefit of HBOT as an adjuvant treatment, in cases of acute SSNHL when used within 3 months of the onset of the hearing loss. Nonetheless, a recent review points out that the costs and the limited availability of HBOT as well as the lack of high quality evidence make it impractical for most patients 36. The findings of the herein presented study encourage further research on the treatment of noise‐induced SSNHL and ISSNHL with the concurrent use of HBOT and ITS respecting also patients with long‐term or therapy‐refractory SSNHL.
Notes
Clinical Case Reports 2016; 4(3): 287–293 [Europe PMC free article] [Abstract] [Google Scholar]
References
Articles from Clinical Case Reports are provided here courtesy of Wiley
Full text links
Read article at publisher's site: https://doi.org/10.1002/ccr3.510
Read article for free, from open access legal sources, via Unpaywall:
https://onlinelibrary.wiley.com/doi/pdfdirect/10.1002/ccr3.510
Citations & impact
Impact metrics
Citations of article over time
Article citations
Altered static and dynamic intrinsic brain activity in unilateral sudden sensorineural hearing loss.
Front Neurosci, 17:1257729, 31 Aug 2023
Cited by: 0 articles | PMID: 37719156 | PMCID: PMC10500124
Effects of Oxygen Therapies in Experimental Acute Acoustic Trauma.
J Int Adv Otol, 17(6):508-513, 01 Nov 2021
Cited by: 0 articles | PMID: 35177387 | PMCID: PMC8975416
The Effectiveness of Hyperbaric Oxygen Therapy as Salvage Treatment for Sudden Sensorineural Hearing Loss: A Retrospective Study.
Cureus, 12(10):e10819, 06 Oct 2020
Cited by: 2 articles | PMID: 33173627 | PMCID: PMC7645304
The use of hyperbaric oxygen therapy in acute hearing loss: a narrative review.
Eur Arch Otorhinolaryngol, 276(7):1859-1880, 20 May 2019
Cited by: 16 articles | PMID: 31111252 | PMCID: PMC6581929
Review Free full text in Europe PMC
Diagnostics and therapy of sudden hearing loss.
GMS Curr Top Otorhinolaryngol Head Neck Surg, 16:Doc05, 01 Jan 2017
Cited by: 13 articles | PMID: 29503670 | PMCID: PMC5818684
Review Free full text in Europe PMC
Go to all (6) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Addition of intratympanic steroid or hyperbaric oxygen treatment to systemic steroid treatment in sudden idiopathic sensorineural hearing loss treatment, and long-term results of salvage treatment
Turk J Med Sci, 50(1):177-183, 13 Feb 2020
Cited by: 4 articles | PMID: 31865663 | PMCID: PMC7080352
The Effectiveness of Salvage Hyperbaric Oxygen Therapy Following Combined Steroid Therapy for Refractory Sudden Sensorineural Hearing Loss.
Ann Otol Rhinol Laryngol, 133(4):400-405, 10 Jan 2024
Cited by: 0 articles | PMID: 38197374
The therapeutic effect of hyperbaric oxygen therapy in patients with severe to profound idiopathic sudden sensorineural hearing loss.
Sci Rep, 14(1):3321, 09 Feb 2024
Cited by: 2 articles | PMID: 38337013 | PMCID: PMC10858205
Controversies in the management of sudden sensorineural hearing loss: an evidence-based review.
Clin Otolaryngol, 40(3):176-182, 01 Jun 2015
Cited by: 30 articles | PMID: 25521864
Review

 1
1