Abstract
Background and objectives
This analysis used a population pharmacokinetic approach to identify covariates that influence plasma exposure of liraglutide 3.0 mg, a glucagon-like peptide-1 (GLP-1) receptor agonist approved for weight management in overweight and obese individuals.Methods
Samples for pharmacokinetic analysis were drawn at weeks 2, 12 and 28 of the phase IIIa SCALE Obesity and Prediabetes (N = 2339) and SCALE Diabetes (N = 584) trials. Dose proportionality of liraglutide in obese subjects was investigated using data from a phase II dose-finding study (N = 331).Results
Dose-proportional exposure of liraglutide up to and including 3.0 mg was confirmed. Body weight and sex influenced exposure of liraglutide 3.0 mg, while age ≥70 years, race, ethnicity and baseline glycaemic status did not. Compared with a reference subject weighing 100 kg, exposure of liraglutide 3.0 mg was 44 % lower for a subject weighing 234 kg (90 % CI 41-47), 41 % higher for a subject weighing 60 kg (90 % CI 37-46), and 32 % higher (90 % CI 28-35) in females than males with the same body weight. Neither injection site nor renal function significantly influenced exposure of liraglutide 3.0 mg (post hoc analysis).Conclusion
Population pharmacokinetics of liraglutide up to and including 3.0 mg daily in overweight and obese adults demonstrated dose-proportional exposure, and limited effect of covariates other than sex and body weight. These findings were similar to those previously observed with liraglutide up to 1.8 mg in subjects with type 2 diabetes mellitus. Further analysis of exposure-response relationship and its effect on dose requirements is addressed in a separate publication.Free full text
Liraglutide 3.0 mg for Weight Management: A Population Pharmacokinetic Analysis
Abstract
Background and Objectives
This analysis used a population pharmacokinetic approach to identify covariates that influence plasma exposure of liraglutide 3.0 mg, a glucagon-like peptide-1 (GLP-1) receptor agonist approved for weight management in overweight and obese individuals.
Methods
Samples for pharmacokinetic analysis were drawn at weeks 2, 12 and 28 of the phase IIIa SCALE Obesity and Prediabetes (N = 2339) and SCALE Diabetes (N = 584) trials. Dose proportionality of liraglutide in obese subjects was investigated using data from a phase II dose-finding study (N = 331).
Results
Dose-proportional exposure of liraglutide up to and including 3.0 mg was confirmed. Body weight and sex influenced exposure of liraglutide 3.0 mg, while age ≥70 years, race, ethnicity and baseline glycaemic status did not. Compared with a reference subject weighing 100 kg, exposure of liraglutide 3.0 mg was 44 % lower for a subject weighing 234 kg (90 % CI 41–47), 41 % higher for a subject weighing 60 kg (90 % CI 37–46), and 32 % higher (90 % CI 28–35) in females than males with the same body weight. Neither injection site nor renal function significantly influenced exposure of liraglutide 3.0 mg (post hoc analysis).
Conclusion
Population pharmacokinetics of liraglutide up to and including 3.0 mg daily in overweight and obese adults demonstrated dose-proportional exposure, and limited effect of covariates other than sex and body weight. These findings were similar to those previously observed with liraglutide up to 1.8 mg in subjects with type 2 diabetes mellitus. Further analysis of exposure–response relationship and its effect on dose requirements is addressed in a separate publication.
Electronic supplementary material
The online version of this article (10.1007/s40262-016-0410-7) contains supplementary material, which is available to authorized users.
Key Points
| In this analysis of obese/overweight subjects with and without type 2 diabetes mellitus, dose-proportional exposure of liraglutide (≤3.0 mg) was confirmed. |
| Body weight and sex influenced exposure of liraglutide 3.0 mg, while age ≥70 years, race, ethnicity and glycaemic status did not. |
| Moreover, neither injection site nor renal function influenced exposure of liraglutide 3.0 mg. |
Background
Liraglutide is an acylated human glucagon-like peptide-1 (GLP-1) receptor agonist with 97 % amino acid sequence homology to human GLP-1 (7–37). Liraglutide 1.8 mg daily (Victoza®; Novo Nordisk A/S, Bagsvaerd, Denmark) is widely approved for the treatment of type 2 diabetes mellitus (T2DM), and liraglutide 3.0 mg is approved in the US [1], Canada [2], Europe [3] and Mexico [4] for weight management.
In randomised clinical trials, liraglutide 3.0 mg led to significant weight loss, weight loss-dependent improvement in weight-related comorbidity, and improved glycaemic control [5, 6]. The mechanism for liraglutide-mediated weight loss has been shown to involve an increase in hypothalamic satiety signals coupled with a decrease in appetite-stimulating signals, resulting in reduced energy intake [7, 8].
Obesity, defined as a body mass index (BMI) ≥30 kg m−2 [9], is associated with multiple progressive comorbidities such as T2DM [10, 11], hypertension, high cholesterol, stroke, heart disease, several cancer types [12, 13] and a 5- to 10-year reduction in life expectancy [14]. Obese individuals are at greater risk for numerous physical symptoms [15–19] and psychosocial difficulties [20], and have poorer health-related quality of life than normal-weight individuals [21]. The individual and societal impact of obesity makes interventions to reduce its prevalence a public health priority [22].
Behavioral intervention using diet and exercise is typically the initial approach for weight management, but when this is not sufficient to produce meaningful weight loss, pharmacotherapy may be a valuable adjunct [23–25]. The Satiety and Clinical Adiposity—Liraglutide Evidence in non-diabetic and diabetic people (SCALE) phase IIIa clinical trial programme investigated the efficacy and safety of liraglutide 3.0 mg (once-daily subcutaneous injection) as adjunct to a reduced-calorie diet and increased physical activity. After 56 weeks, mean body weight losses of 8.0 % (vs. 2.6 % with placebo) and 5.9 % (vs. 2.2 % with placebo) were observed in the SCALE Obesity and Prediabetes [5] and SCALE Diabetes [6] trials, respectively.
The efficacy of liraglutide 3.0 mg was consistent across various demographic subgroups. However, there was a tendency for less weight loss in subjects with a BMI >40 kg m−2 and greater weight loss in females versus males. Previously, a population pharmacokinetic analysis in patients with T2DM [26] demonstrated that body weight and sex were relevant factors for the exposure level of liraglutide (at doses up to 1.8 mg), suggesting that differences in clinical response to liraglutide may be associated with differences in exposure.
This analysis demonstrated that, in overweight and obese adults, population pharmacokinetics of liraglutide up to and including 3.0 mg daily was similar to that observed with liraglutide up to 1.8 mg in subjects with T2DM, with dose-proportional exposure and limited effect of covariates other than sex and body weight. Characterisation of individual exposure levels and key determinants of exposure allows for subsequent investigation of the exposure–response relationship, thereby informing dosing recommendations for liraglutide 3.0 mg in weight management.
Methods
Materials
Data Sources for Population Pharmacokinetic Analysis of Liraglutide 3.0 mg
SCALE Obesity and Prediabetes (Trial 1) was a randomised, double-blind, placebo-controlled, multicentre, phase IIIa trial examining the efficacy and safety of liraglutide 3.0 mg versus placebo, as adjunct to diet and exercise, in obese (BMI ≥30 kg m−2) or overweight (BMI ≥27–29.9 kg m−2) adults with at least one weight-related comorbidity (treated or untreated hypertension and/or dyslipidaemia) over 56 weeks. In this trial, 3731 subjects were randomised 2:1 to liraglutide 3.0 mg (N = 2487) or placebo (N = 1244) injections once daily, starting at 0.6 mg/day, with weekly dose increments of 0.6 mg up to a maximum of 3.0 mg daily (Trial 1 [5]). A total of 2339 subjects from the SCALE Obesity and Prediabetes trial were included in this population pharmacokinetic analysis.
A single blood sample for plasma liraglutide concentration measurement was drawn from all subjects included in the pharmacokinetic analysis from Trial 1, at weeks 2 (dose escalation period), 12 and 28 after randomisation. The date, time, liraglutide dose and injection site for the three injections prior to each blood sampling were recorded. In addition, week 16 data values were included from a substudy (N = 52; 50 maximum concentration [C max] values available) in which subjects who administered liraglutide in the evening had blood drawn for liraglutide bioanalysis at approximately 10, 11, 12 and 14 h after dosing, to obtain exposure values around C max for liraglutide 3.0 mg.
SCALE Diabetes (Trial 2) was a randomised, double-blind, placebo-controlled, parallel group, multicentre, phase IIIa trial examining the efficacy and safety of liraglutide 3.0 mg and 1.8 mg versus placebo in overweight or obese (BMI ≥27 kg m−2) adults with T2DM (glycated haemoglobin [HbA1c] 53–86 mmol mol−1 [7.0–10.0 %]), treated with diet and exercise alone or combined with one to three oral hypoglycaemic agents (OHAs), including metformin, a thiazolidinedione and/or a sulphonylurea. Subjects in Trial 2 (N = 846) were randomised 2:1:1 to liraglutide 3.0 mg (N = 423), liraglutide 1.8 mg (N = 211) or placebo (N = 212) injections once daily, starting at 0.6 mg/day, with weekly 0.6 mg dose increments up to a maximum of 3.0 mg/day (Trial 2 [6]).
Blood sampling was performed at weeks 2, 12 and 28 for all subjects included in the pharmacokinetic analysis from Trial 2, as described for subjects from Trial 1. The date, time, dose and injection site of liraglutide for the three injections occurring prior to each blood sampling were recorded.
Only records with a complete (all three doses) and unambiguous (constant dose level; only one daily dose) dosing history for the 3 days leading up to each visit were included; inadequate dosing history resulted in exclusion of 1185 of 8859 records from the main pharmacokinetic analysis. The available concentration data were used to estimate individual area under the curve (AUC) values, using the final population pharmacokinetic model (with the same population level parameter values as in the original analysis).
Data Source for Analysis of Dose Proportionality of Liraglutide at Doses Up to 3.0 mg
Data from 331 adults enrolled in a phase II dose-finding trial with liraglutide and an open-label orlistat comparator arm (Trial 3 [27]) were used in a dose-proportionality assessment. In this 20-week, randomised, double-blind, placebo-controlled, six-armed, parallel group, multicentre trial, the response to a range of liraglutide doses was examined in obese individuals (BMI ≥30 and ≤40 kg m−2) without T2DM. Subjects included in the dose-proportionality analysis were randomised 1:1:1:1:1:1 to receive liraglutide 1.2 mg (N = 88), 1.8 mg (N = 80), 2.4 mg (N = 77), 3.0 mg (N = 86) or placebo (N = 98) once daily (initiated at 0.6 mg/day, with weekly 0.6 mg increments up to the required dose) or orlistat (120 mg thrice daily).
Blood sampling for dose proportionality assessment was performed at week 20 during an oral glucose tolerance test visit, in the morning, 10–14 h after dose administration the previous evening. Samples were drawn at 0, 60 and 120 min following glucose ingestion. The time of blood sampling relative to the previous liraglutide dose was not recorded.
Population Pharmacokinetic Model
A prespecified approach [28] was used for the population pharmacokinetic analysis, which included estimation of a base model without covariates and a full model with all covariates included. Only the full covariate model is described here.
The population pharmacokinetic model was developed and validated according to the US FDA and European Medicines Agency (EMA) guidelines for pharmacokinetic modelling [29, 30]. Full details of the model qualification are included in the Online Resource, Sect. 1. This was a one-compartment model with first-order absorption and elimination. It was parameterised by absorption rate (Ka), apparent clearance (CL/F) and apparent volume (V/F), where covariate effects were implemented for clearance only, as:
where TVCL is the typical liraglutide apparent clearance for a reference subject profile (female; <70 years of age; 100 kg body weight [rounded value close to mean body weight]; White, non-Hispanic or -Latino, and without diabetes or prediabetes, taking liraglutide 3.0 mg once daily), and η describes the random interindividual variability, assumed to be normally distributed. To ensure identifiability of the model with the sparsely sampled data, the liraglutide absorption rate constant was set to a value (0.0806 L/h−1) estimated from a population pharmacokinetic model based on a multiple-dose clinical pharmacology study in obese subjects ([8]; data on file), and the assumption that this parameter can be fixed without affecting the conclusions was verified by sensitivity analyses. A proportional error model was used to describe the residual variability of liraglutide concentrations. Parameter estimates for the full covariate model are described in the Online Resource (Table S1).
The full covariate model was used to obtain parameter estimates and confidence intervals (CI) for the following covariates: age (< or ≥70 years), baseline body weight (minimum 60 kg; maximum 234 kg, relative to a 100 kg person), sex, race (White, Black or African American, Asian, Other [including American Indian or Alaskan native, native Hawaiian or other Pacific Islander]), ethnicity (Hispanic or Latino, non-Hispanic or -Latino), baseline glycaemic status (non-diabetic, prediabetic or with T2DM), and liraglutide dose (1.8 or 3.0 mg).
Likelihood profiling was used to determine geometric means and 90 % CI for each investigated covariate. Differences in pharmacokinetic parameters were considered relevant if the 90 % CI of the effect fell outside the standard bioequivalence limits (0.80–1.25).
Graphical data quality analyses, including goodness-of-fit plots, were conducted prior to performing the population pharmacokinetic analysis, as described in the Online Resource (Sect. 2; Figs. S1, S2).
Exposure Assessment for Dose Proportionality
The exposure data from Trial 3 were obtained by estimating the full population pharmacokinetic model (developed using data from Trials 1 and 2) on data from Trial 3, with all parameters fixed. This provided individual post hoc empirical Bayes estimates of the exposure level for subjects in Trial 3, which were used to evaluate dose proportionality.
Post Hoc Analysis
A post hoc analysis of the effect of (1) injection site and (2) renal function on CL/F of liraglutide was performed, using data from Trial 1 (injection site; renal function on CL/F of liraglutide) and Trial 2 (renal function on CL/F of liraglutide), by comparing individual values of covariate-adjusted CL/F. For injection-site analysis, values were obtained from subjects injecting into the abdomen, thigh or upper arm. Baseline renal function was determined by estimating creatinine clearance (CrCl) using the Chronic Kidney Disease–Epidemiology Collaboration (CKD–EPI) equation [31]. The effects of renal function and injection site were not part of the prespecified analysis; this post hoc analysis is therefore presented as the primary result for the influence of these parameters on CL/F of liraglutide.
Liraglutide Assay
Total liraglutide plasma concentration was determined using a validated enzyme-linked immunosorbent assay (ELISA) [32]. The lower limit of quantification (LLOQ) was 30 pmol L−1 for the ELISAs used in Trials 1 and 2, and 18 pmol L−1 for the ELISA used in the dose-finding trial (Trial 3). For Trials 1 and 2, the intra- and interassay precision was <12.9 and 9.4 %, respectively (data on file). For Trial 3, the intra- and interassay precision was <6.5 and 10.1 %, respectively [33].
Ethical Statements
The study protocols for all trials in this analysis were approved by local Institutional Review Boards and Ethics Committees. All trials were conducted in accordance with the Declaration of Helsinki [34] and Good Clinical Practice guidelines [35], and all patients provided written informed consent before participation.
Data Analysis Software
SPLUS, version 8.2 (TIBCO, Palo Alto, CA, USA) was used for data-file processing, exploratory-data analysis and plotting. NONMEM, version 7.1.2 (ICON Development Solutions, Ellicott City, MD, USA) was used for the population pharmacokinetic analysis and simulation.
Results
This population pharmacokinetic analysis used data from two phase IIIa trials to examine the effects of various covariates on plasma exposure of liraglutide 3.0 mg in overweight and obese individuals. Dose proportionality of liraglutide at doses up to 3.0 mg in obese subjects was also investigated using data from one phase II trial. In this study, we present the results of each analysis.
Demographics
Tables 1 and S2 (Online Resource) show baseline demographics in all three trial populations. Subjects in the population pharmacokinetic analysis (Table 1) had a mean age of 47 years, and 2.5 % (n = 73) were aged ≥70 years. Most subjects were female (72 %), White (85 %), and non-Hispanic or -Latino (90 %). Mean body weight and BMI were 106 ± 21 kg and 38 ± 7 kg m−2, respectively. In all, 20 % of subjects had T2DM (all in Trial 2), and the majority had normal renal function or mild renal impairment. In comparison, sex and age distribution in the dose-finding trial population was similar to that in the pharmacokinetic analysis population, although in the former trial almost all subjects were White (99 %), and mean body weight (98 ± 13 kg) and BMI (35 ± 3 kg m−2) were somewhat lower.
Table 1
Summary of baseline characteristics for subjects included in the pharmacokinetic evaluation
| Covariate | Trial 1 | Trial 2 | Total |
|---|---|---|---|
| [N = 2339] | [N = 584] | [N = 2923] | |
| Liraglutide dose, mg [ n (%)] | |||
| 1.8 | 0 (0) | 191 (32.5) | 191 (6.5) |
| 3.0 | 2339 (100) | 393 (67.5) | 2732 (93.5) |
| Sex [n (%)] | |||
| Female | 1831 (78) | 281 (48) | 2112 (72) |
| Male | 508 (22) | 303 (52) | 811 (28) |
| Age, years [ n (%)] | |||
| Mean (SD) | 45.2 (12.0) | 54.7 (10.5) | 47.1 (12.3) |
| ≥75 | 4 (0.2) | 9 (1.5) | 13 (0.4) |
| 70–74 | 32 (1.4) | 28 (4.8) | 60 (2.1) |
| 65–69 | 91 (3.9) | 67 (11.5) | 158 (5.4) |
| 18–64 | 2212 (94.5) | 480 (82.2) | 2692 (92.1) |
| Race [ n (%)] a | |||
| White | 1989 (85) | 493 (84.4) | 2482 (84.9) |
| Black/African American | 222 (9.5) | 61 (10.4) | 283 (9.7) |
| Asian | 82 (3.5) | 14 (2.4) | 96 (3.3) |
| Other | 46 (2.0) | 16 (2.8) | 62 (2.1) |
| Ethnic group [ n (%)] | |||
| Hispanic or Latino | 246 (10.5) | 60 (10.3) | 306 (10.5) |
| Non-Hispanic or -Latino | 2093 (89.5) | 524 (89.7) | 2617 (89.5) |
| Mean body weight, kg | |||
| Overall population | |||
| Mean (SD) | 106 (21) | 106 (22) | 106 (21) |
| Range | 65–234 | 60–199 | 30–234 |
| Females | |||
| Mean (SD) | 102 (19) | 100 (19) | 102 (19) |
| Range | 65–218 | 60–167 | 60–218 |
| Males | |||
| Mean (SD) | 121 (24) | 112 (22) | 118 (24) |
| Range | 79–234 | 75–199 | 75–234 |
| BMI, kg m −2 | |||
| Overall population | |||
| Mean (SD) | 38 (6) | 37 (7) | 38 (7) |
| Range | 27–77 | 27–68 | 27–77 |
| Females | |||
| Mean (SD) | 38 (6) | 38 (7) | 38 (6) |
| Range | 27–77 | 27–68 | 27–77 |
| Males | |||
| Mean (SD) | 38 (7) | 36 (7) | 38 (7) |
| Range | 27–70 | 27–61 | 27–70 |
| BMI categories [ n (%)] | |||
| <29.9 | 60 (2.6) | 77 (13.2) | 137 (4.7) |
| 30–34.9 | 765 (32.7) | 181 (31.0) | 946 (32.4) |
| 35–39.9 | 730 (31.2) | 148 (25.3) | 878 (30.0) |
| ≥40 | 784 (33.5) | 178 (30.5) | 962 (32.9) |
| Glycaemic status [ n (%)] | |||
| Normoglycaemic | 897 (38.3) | 0 (0) | 897 (30.7) |
| Prediabetic | 1442 (61.7) | 0 (0) | 1442 (49.3) |
| Type 2 diabetes | 0 (0) | 584 (100) | 584 (20.0) |
| Creatinine clearance, ml/min (degree of renal impairment) | |||
| ≥90 (normal) | 1194 (51) | 295 (51) | 1489 (51) |
| ≥60 and <90 (mild) | 1045 (45) | 236 (40) | 1281 (44) |
| ≥30 and <60 (moderate) | 99 (4) | 52 (9) | 151 (5) |
| <30 (severe) | 1 (0) | 1 (0) | 2 (0.0) |
| Injection site [ n (%)] b | |||
| Abdomen | 1768 (75.6) | NA | |
| Thigh | 452 (19.3) | ||
| Upper arm | 113 (4.8) | ||
| Other | 6 (0.3) | ||
BMI body mass index, NA not applicable, SD standard deviation
aThe ‘Other’ race group for the covariate analysis included ‘American Indian or Alaskan Native’, ‘Native Hawaiian or other Pacific Islander’ and any ‘Other’
bPost hoc analysis, analysed in Trials 1 and 2
Structural Model
Parameter estimates and qualifications of the pharmacokinetic model are available in the Online Resource, Sect. S1. The pharmacokinetics of liraglutide were adequately described by a one-compartment model with first-order absorption and first-order elimination, with CL/F ranging from 0.9 to 1.4 L/h. The apparent clearance was 0.9 and 1.0 L/h for a non-diabetic or diabetic female, respectively, and 1.1–1.4 L/h for a non-diabetic or diabetic male, with other covariate factors resembling those of the reference subject (100 kg body weight, White, non-Hispanic or -Latino, <70 years of age, taking liraglutide 3.0 mg once daily).
Dose Proportionality of Liraglutide at Doses Up to 3.0 mg
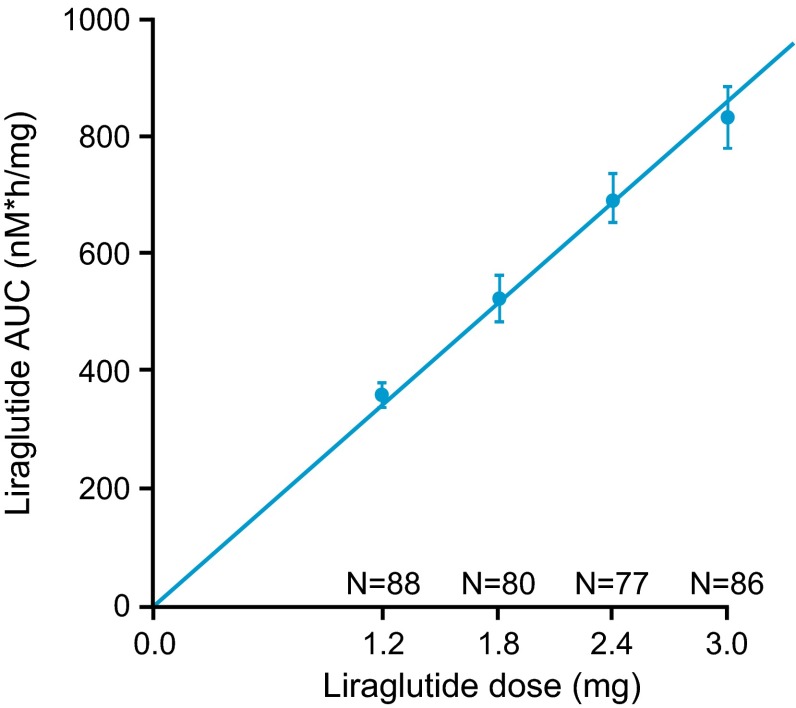
Model-derived AUCs by dose in this population supported dose proportionality of liraglutide up to and including 3.0 mg (Fig. 1). Demographics of subjects from the phase II dose-finding trial included in the dose-proportionality analysis are included in the Online Resource, Table S2.
Population Pharmacokinetic Analysis
Subject Baseline Characteristics
Table 1 describes the baseline demographics of subjects included in the population pharmacokinetic analysis. Mean body weight and BMI for all subjects were 106 kg and 38 kg m−2, respectively. As expected, despite similar baseline BMI in both sex groups, mean body weight was higher in men. Overall, the majority of subjects were White and non-Hispanic or -Latino. There was a higher proportion of females among subjects included in the pharmacokinetic analysis population from Trial 1.
Covariate Analysis
The covariate analysis results were summarised for steady-state liraglutide exposure (AUC24) relative to exposure for a reference subject (Table 1). The between-subject variability for liraglutide CL/F (hence dose-normalised AUC) was 34.8 % coefficient of variation (CV), which was reduced to 24.7 % CV when the predefined covariates for liraglutide CL/F were included in the population pharmacokinetic model.
Body weight and sex significantly impacted dose-normalised liraglutide exposure (Fig. 2), whereas age, race, ethnicity, glycaemic status, dose, injection site and renal function did not (additional data for exposure by renal function is included in Online Resource Fig. S3). The analysis also showed similar dose-normalised exposure for the liraglutide 3.0 mg and 1.8 mg groups, indicating dose proportionality in the dose range 1.8–3.0 mg, consistent with results from the phase II dose-finding trial (Fig. 1).
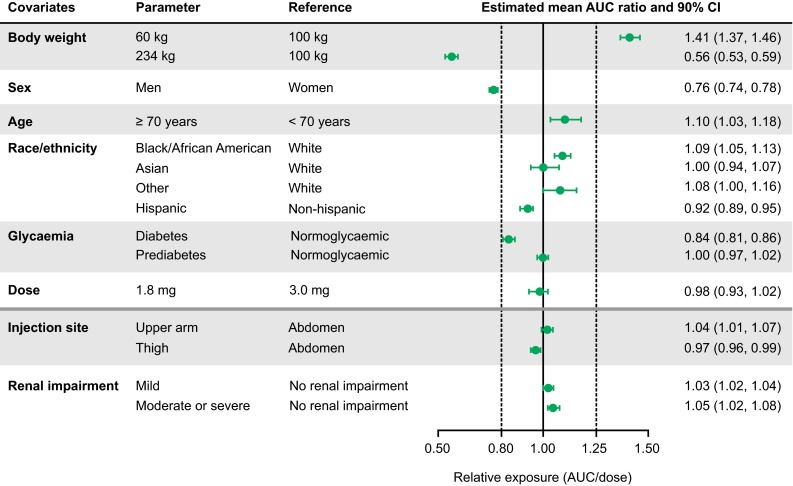
Influence of covariates on exposure expressed as change in relative steady-state dose-normalised liraglutide exposure (AUC24/dose). Reference subject profile: female, below 70 years of age, 100 kg body weight, White, non-Hispanic or -Latino, without diabetes or prediabetes, dosed by liraglutide 3.0 mg once daily. The parameter ‘body weight’ shows the highest and lowest in the dataset. Mild and moderate/severe renal impairment were defined as ≥60 and <90 ml min−1 and ≥30 and <60 ml min−1, respectively, and ‘no renal impairment’ was defined as ≥90 ml/min. Dotted lines indicate the interval used for bioequivalence testing, for comparison. The column to the right shows geometric mean relative exposures with 90 % CI obtained by likelihood profiling. Covariates above the solid horizontal line were prespecified, and parameters below the solid line were analyzed post hoc. CI confidence interval, AUC area under the curve
Effect of Body weight
Mean liraglutide exposure appeared to decrease with increasing body weight (Online Resource Fig. S1), and this was confirmed in the population pharmacokinetic analysis (Fig. 2). Compared with a reference subject weighing 100 kg, higher body weight was associated with decreased liraglutide exposure, and lower body weight was associated with increased exposure; for a 234 kg subject (the highest observed body weight in the dataset), liraglutide exposure was 44 % lower (78 % higher CL/F). Conversely, for a 60 kg subject (the lowest observed body weight in the dataset), liraglutide exposure was 41 % higher (29 % lower CL/F). The 90 % CI values were outside of the predefined limits for bioequivalence for both the highest (234 kg) and lowest (60 kg) body weight values, indicating an effect of body weight on liraglutide exposure. Exposure by baseline BMI revealed a less clear relationship. Graphical analysis demonstrated negligible difference between subjects with high and low BMI when body weight was matched (data not shown). Additional statistical analyses based on post hoc estimates confirmed that, for simultaneous investigation of body weight and BMI, the influence of body weight on exposure was highly significant (p < 0.0001), and of similar magnitude as in the main analysis. By contrast, the BMI influence was small and of borderline significance (p ~ 0.03). These findings suggest that absolute bodyweight, rather than obesity per se, is the better predictor of liraglutide exposure.
Effect of Sex
Liraglutide exposure was 24 % lower in males than in females of comparable body weight (Fig. 2), which corresponds to 32 % greater exposure in females compared with males at comparable body weight. The effect of sex on exposure was independent of the effect of body weight (Online Resource Fig. S4). Since the 90 % CI for this effect was outside of the bioequivalence limits, sex was considered to have a pharmacokinetically relevant effect on liraglutide exposure.
Effect of Trial: Glycaemic Status
Subjects with T2DM were found to have 16 % lower liraglutide exposure than normoglycaemic subjects, while subjects with prediabetes had similar mean exposure to normoglycaemic subjects (Fig. 2). The 90 % CI for subjects with T2DM versus normoglycaemic subjects fell narrowly within the bioequivalence limits and were therefore not considered pharmacokinetically relevant. However, glycaemic status was confounded by trial as all subjects with T2DM originated from Trial 2. Therefore, a trial effect cannot be excluded. Conversely, subjects with prediabetes had similar liraglutide exposure to normoglycaemic subjects; however, in this case both groups originated from Trial 1.
The geometric mean of the individual apparent clearance estimates in the three studies was 0.94, 1.22 and 0.93 L/h for Trials 1, 2 and 3, respectively. This confirms similarity between the trials in subjects without diabetes (Trials 1 and 3), and higher clearance values for Trial 2, in subjects with diabetes. The covariate-adjusted clearance estimate was similar across the three trials (geometric mean 0.86, 0.86, and 0.88 L/h, respectively), confirming that the estimated covariate factors adequately accounted for differences between trials.
Effect of Body Weight on Exposure: By Sex and Baseline Glycaemic Status
Exposure levels at steady-state concentrations of liraglutide 3.0 mg overlapped in male and female subjects. However, in general, males are heavier than females and therefore the combined effects of sex and body weight contribute to a generally lower exposure in males versus females. The relationship among exposure, body weight and sex is shown in Fig. 3a. Likewise, individuals with T2DM generally had lower exposure than those with normoglycaemia or prediabetes at all body weights (Fig. 3b).
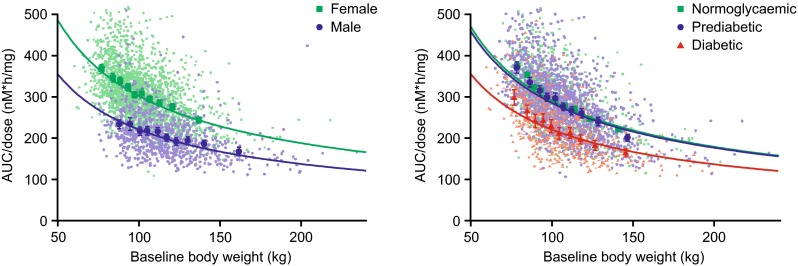
Liraglutide exposure versus body weight stratified by a sex and b glycaemic status. Data are dose-normalised mean AUC values with 95 % CI for quantiles of baseline body weight (large symbols) and individual exposure estimates (small symbols). Lines are model-based relationships adjusted for other covariate effects. AUC area under the curve, CI confidence interval
High and Low Exposure Scenarios Including Additional Covariates
A ‘high-exposure scenario’ was generated using a female of body weight 60 kg (lowest observed body weight in the pharmacokinetic dataset) without T2DM using injection site ‘upper arm’ and additional covariates expected to give the highest exposure (≥70 years of age, Black, non-Hispanic). A ‘low-exposure scenario’ was generated using a male with body weight 234 kg (highest observed body weight in the pharmacokinetic dataset) with T2DM using injection site ‘thigh’, and additional covariates expected to give the lowest exposure (<70 years of age, White, Hispanic). Predicted liraglutide exposure values (AUC) for the high- and low-exposure scenarios were 1631 and 297 nM h, respectively. These predicted exposure levels were covered by the actual observed exposure levels.
Exposure Comparison: Liraglutide 3.0 mg in Overweight/Obese Subjects Versus 1.8 mg in Subjects with Type 2 Diabetes Mellitus
Liraglutide 1.8 mg is approved for use in subjects with T2DM, and safety data are available both from the clinical trial programme and postmarketing experience. To evaluate the applicability of safety data for liraglutide 1.8 mg in subjects with T2DM with liraglutide 3.0 mg in overweight/obese subjects, an exposure comparison was undertaken.
The predicted estimated exposure distribution associated with liraglutide 3.0 mg in overweight/obese subjects in Trials 1 and 2 was compared with the estimated exposure of liraglutide 1.8 mg in subjects with T2DM in a previous phase III trial [26]. As shown in Fig. 4, there is substantial overlap in exposures with liraglutide 3.0 and 1.8 mg when used for weight management and treatment of T2DM, respectively, in overweight/obese subjects with and without T2DM; approximately 16 % of the overweight/obese population receiving 3.0 mg reach exposures higher than any exposure in subjects with T2DM treated with 1.8 mg. Approximately one-third of the difference in exposure between Trials 1 and 2 (29 % higher exposure in Trial 1) could be explained by the higher proportion of females in Trial 1 (78 vs. 48 %). The remaining 19 % may be attributed to differences in exposure in subjects with and without T2DM.
Discussion
This analysis demonstrated that exposure of liraglutide, within the dose range 1.2–3.0 mg, is dose proportional in obese adults. Furthermore, the population pharmacokinetic assessment established a plasma clearance value for liraglutide 3.0 mg in overweight and obese adults of between 0.9 and 1.4 L/h, and demonstrated that exposure of liraglutide 3.0 mg in an overweight or obese population is mainly impacted by two key covariates—body weight and sex.
These findings are consistent with the established pharmacokinetic properties of liraglutide at lower doses [36]. Dose-proportional exposure has been demonstrated in the 0.6–1.8 mg dose range in healthy adults [37, 38] and those with T2DM [39, 40]. Furthermore, body weight and sex (but not age, race or ethnicity) were previously found to be relevant covariates for liraglutide (1.2–1.8 mg) clearance, and hence exposure, in a population pharmacokinetic analysis in subjects with T2DM and mean body weight of 90 kg [26].
Reasons for the lower weight-adjusted clearance of liraglutide in females than males, and the effects of differences in body composition and other factors, have yet to be determined. Further analysis of the exposure–response relationship demonstrated increasing weight loss response at increasing exposure levels throughout the exposure range, with clear effects apparent in the low exposure range. With the exception of gastrointestinal tolerability, safety and tolerability were not exposure-dependent [41]. Therefore, exposure–response analysis supported use of the highest tested dose of liraglutide (3.0 mg) in all subpopulations, and did not support differential dosing in males versus females or in heavier versus lighter individuals [41].
Liraglutide is endogenously metabolised without a specific organ as a major route of elimination [42]. In accordance with this, post hoc analysis demonstrated that clearance of liraglutide 3.0 mg is not impacted by mild (CrCl ≥60 and <90 ml min−1) or moderate (CrCl ≥30 and <60 ml min−1) renal impairment, although we recognise that use of epidermal growth factor receptor (eGFR) may have led to overestimation of true GFR in this obese population [43]. While this suggests that dose adjustment of liraglutide 3.0 mg is not required in renal impairment (as is also the case for liraglutide 1.8 mg) [44, 45], experience with liraglutide 3.0 mg in patients with severe renal impairment (CrCl <30 ml min−1), including end-stage renal disease, is limited. Use in this group is therefore not recommended [1], and caution is advised when initiating or escalating doses of liraglutide in these patients [1]. The post hoc analysis also found no difference in CL/F values for liraglutide across injection sites (abdomen, thigh or upper arm), suggesting that injection site can be guided by patient preference. Since the effects of adding renal function and/or injection site to the model are minimal, and the shrinkage in clearance is small, these effects would remain eligible if the prespecified model was revised to include these parameters.
Covariate analysis showed that subjects with low body weight will achieve higher liraglutide exposure than subjects with high body weight. Therefore, the liraglutide exposure level was compared between the weight management programme (with the higher dose 3.0 mg and heavier subjects [body weight range 60–234 kg]) and liraglutide 1.8 mg in subjects with T2DM (phase III trial with body weight range 40–160 kg [26]). The substantial overlap in exposures in the two programmes indicates that safety data obtained with liraglutide 1.8 mg can usefully inform dosing with liraglutide 3.0 mg. To further evaluate the safe use of liraglutide in subjects with overweight/obesity, in particular for exposure levels exceeding the range obtained with 1.8 mg, an exposure–response evaluation was conducted for selected safety parameters and has been published separately [41].
Conclusions
Exposure of liraglutide up to and including 3.0 mg in overweight and obese adults is dose proportional. For liraglutide 3.0 mg, sex and body weight are the main baseline covariates influencing exposure, while age ≥70 years, race, ethnicity, glycaemic status, mild-to-moderate renal impairment, injection site and dose are not considered pharmacokinetically relevant. Further exposure–response analyses in relevant subgroups are required to support dosing recommendations of liraglutide 3.0 mg for weight management.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
Medical writing assistance was provided by Rosalyn Ferguson and Esther Nathanson at Watermeadow Medical, UK, supported by Novo Nordisk A/S.
Author Contributions
Rune V. Overgaard participated in planning and conducting the analyses, data interpretation, and drafting of this article. Kristin C. Petri participated in planning and conducting the analyses, data interpretation, and drafting of this article. Lisbeth V. Jacobsen participated in planning of the analyses, data interpretation and drafting of this article. Christine B. Jensen participated in trial design, trial conduct, planning of the analyses, data interpretation, and drafting of this article. All authors had full access to all the data used in the analyses and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors approved the final version.
Compliance with Ethical Standards
Conflict of interest
Rune V. Overgaard, Kristin C. Petri, Lisbeth V. Jacobsen and Christine B. Jensen are all employees of, and shareholders in, Novo Nordisk A/S. No other relationships or activities appear to have influenced the submitted work.
References
Full text links
Read article at publisher's site: https://doi.org/10.1007/s40262-016-0410-7
Read article for free, from open access legal sources, via Unpaywall:
https://link.springer.com/content/pdf/10.1007%2Fs40262-016-0410-7.pdf
Citations & impact
Impact metrics
Citations of article over time
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.1007/s40262-016-0410-7
Article citations
Adipose Tissue: A Novel Target of the Incretin Axis? A Paradigm Shift in Obesity-Linked Insulin Resistance.
Int J Mol Sci, 25(16):8650, 08 Aug 2024
Cited by: 0 articles | PMID: 39201336 | PMCID: PMC11354636
Review Free full text in Europe PMC
Sex-Differences in Response to Treatment with Liraglutide 3.0 mg.
J Clin Med, 13(12):3369, 07 Jun 2024
Cited by: 1 article | PMID: 38929898
Obesity management: sex-specific considerations.
Arch Gynecol Obstet, 309(5):1745-1752, 08 Feb 2024
Cited by: 1 article | PMID: 38329549 | PMCID: PMC11018683
Review Free full text in Europe PMC
Sex Differences in the Preventive Effect of Cardiovascular and Metabolic Therapeutics on Dementia.
Biomol Ther (Seoul), 31(6):583-598, 01 Nov 2023
Cited by: 0 articles | PMID: 37899743 | PMCID: PMC10616511
Review Free full text in Europe PMC
Obesity: a gender-view.
J Endocrinol Invest, 47(2):299-306, 23 Sep 2023
Cited by: 17 articles | PMID: 37740888 | PMCID: PMC10859324
Review Free full text in Europe PMC
Go to all (20) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
One-year follow-up on liraglutide treatment for prediabetes and overweight/obesity in clozapine- or olanzapine-treated patients.
Acta Psychiatr Scand, 139(1):26-36, 28 Nov 2018
Cited by: 13 articles | PMID: 30374965
Exposure-response analyses of liraglutide 3.0 mg for weight management.
Diabetes Obes Metab, 18(5):491-499, 01 Mar 2016
Cited by: 35 articles | PMID: 26833744 | PMCID: PMC5069568
Comparable liraglutide pharmacokinetics in pediatric and adult populations with type 2 diabetes: a population pharmacokinetic analysis.
Clin Pharmacokinet, 54(6):663-670, 01 Jun 2015
Cited by: 17 articles | PMID: 25603819 | PMCID: PMC4449373
Liraglutide in Type 2 Diabetes Mellitus: Clinical Pharmacokinetics and Pharmacodynamics.
Clin Pharmacokinet, 55(6):657-672, 01 Jun 2016
Cited by: 72 articles | PMID: 26597252 | PMCID: PMC4875959
Review Free full text in Europe PMC
Funding
Funders who supported this work.