Abstract
Background
Hospitals rely on point-of-care (POC) blood glucose (BG) values to guide important decisions related to insulin administration and glycemic control. Evaluation of POC BG in hospitalized patients is associated with measurement and operator errors. Based on a previous quality improvement (QI) project we introduced an option for operators to delete and repeat POC BG values suspected as erroneous. The current project evaluated our experience with deleted POC BG values over a 2-year period.Method
A retrospective QI project included all patients hospitalized at two regional academic medical centers in the Pacific Northwest during 2014 and 2015. Laboratory Medicine POC BG data were reviewed to evaluate all inpatient episodes of deleted and repeated POC BG.Results
Inpatient operators choose to delete and repeat only 0.8% of all POC BG tests. Hypoglycemic and extreme hyperglycemic BG values are more likely to be deleted and repeated. Of initial values <40 mg/dL, 58% of deleted values (18% of all values) are errors. Of values >400 mg/dL, 40% of deleted values (5% of all values) are errors. Not all repeated POC BG values are first deleted. Optimal use of the option to delete and repeat POC BG values <40 mg/dL could decrease reported rates of severe hypoglycemia by as much as 40%.Conclusions
This project demonstrates that operators are frequently able to identify POC BG values that are measurement/operator errors. Eliminating these errors significantly reduces documented rates of severe hypoglycemia and hyperglycemia, and has the potential to improve patient safety.Free full text
What Can We Learn From Point-of-Care Blood Glucose Values Deleted and Repeated by Nurses?
Abstract
Background:
Hospitals rely on point-of-care (POC) blood glucose (BG) values to guide important decisions related to insulin administration and glycemic control. Evaluation of POC BG in hospitalized patients is associated with measurement and operator errors. Based on a previous quality improvement (QI) project we introduced an option for operators to delete and repeat POC BG values suspected as erroneous. The current project evaluated our experience with deleted POC BG values over a 2-year period.
Method:
A retrospective QI project included all patients hospitalized at two regional academic medical centers in the Pacific Northwest during 2014 and 2015. Laboratory Medicine POC BG data were reviewed to evaluate all inpatient episodes of deleted and repeated POC BG.
Results:
Inpatient operators choose to delete and repeat only 0.8% of all POC BG tests. Hypoglycemic and extreme hyperglycemic BG values are more likely to be deleted and repeated. Of initial values <40 mg/dL, 58% of deleted values (18% of all values) are errors. Of values >400 mg/dL, 40% of deleted values (5% of all values) are errors. Not all repeated POC BG values are first deleted. Optimal use of the option to delete and repeat POC BG values <40 mg/dL could decrease reported rates of severe hypoglycemia by as much as 40%.
Conclusions:
This project demonstrates that operators are frequently able to identify POC BG values that are measurement/operator errors. Eliminating these errors significantly reduces documented rates of severe hypoglycemia and hyperglycemia, and has the potential to improve patient safety.
Hospitals rely on point-of-care (POC) blood glucose (BG) meters to evaluate glycemic control in patients with diabetes mellitus or stress hyperglycemia.1 POC BG values guide critical insulin administration decisions, with many hospitals performing more than 100 000 POC BG tests per year.2 However, numerous studies have identified factors that make POC BG testing in hospitalized patients less accurate and reliable than would be expected based on glucose meter manufacturer’s data.3-5 Recent work from our large regional academic medical center demonstrated that POC BG measurement errors cause an overestimation of hypoglycemic events in critically ill patients.6 This work resulted in an ongoing quality improvement (QI) project at two regional academic medical hospitals to allow nurses (RNs) and assistive personnel (AP) trained to perform POC BG on patients to delete and repeat POC BG values that they believe may be measurement errors. The current work describes our findings from a 2-year evaluation of this QI project.
Accurate assessment of BG values in hospitalized patients is important because both hyperglycemia and hypoglycemia are associated with negative patient outcomes.7-9 Previous work has defined national benchmark data for hypoglycemia rates in critically ill and acutely ill hospitalized patients in the United States.2,10 While federal quality assurance organizations have removed hypoglycemia rates from their current quality measures, many state agencies including the Washington State Hospital Association publicly report hospital hypoglycemia rates to the consumer. In addition, the University HealthSystem Consortium (UHC/Vizient) is expected to begin tracking hypoglycemia metrics in 2018. In this context it is critical that reported hypoglycemia values represent true hypoglycemic events to ensure the greatest reliability of the data being presented to the public.
Data suggests that as many as 15-25% of hospitalized patients are treated with insulin during their admission to help optimize glycemic control.1,9,11 For these patients, hospital providers and nurses rely on POC BG values for important daily insulin administration decisions. Inaccurate hypoglycemic POC BG readings could lead to inappropriate administration of oral or IV rescue with sucrose or dextrose, or reduced doses of meal-time or basal insulin, both of which could lead to subsequent hyperglycemia. Even more important to patient safety, inaccurate hyperglycemic POC BG measurements could lead to administration of additional insulin to euglycemic patients potentially causing hypoglycemia. Thus, in addition to inaccurate quality and hospital performance data, POC BG measurement errors have the potential to cause patient harm through inappropriate insulin dosing.
Methods
Setting
This retrospective QI project was conducted at two reginal academic medical centers in the Pacific Northwest, the first a ~400-bed urban tertiary care center and Level 1 trauma center, and the second a ~350-bed urban tertiary care center. Both hospitals exclusively use the Accu-Chek Inform II glucose meter (Roche Diagnostics, Indianapolis, IN). Inform meters are automatically downloaded through Remote Automated Laboratory System-Plus (Medical Automation Systems, Charlottesville, Virginia), administered by Laboratory Medicine which then uploads POC BG values into the Electronic Health Record (EHR). All RNs and AP are trained to use the Inform glucose meter including options to add prepopulated comments to POC BG values. At the end of 2013 the prepopulated comments on the Inform glucose meter were changed to include “DeleteBG WillRetest” on the first page of comments. Operators were instructed to use this comment when POC BG result did not match BG trend, did not match symptoms, or for extreme high or low values, and other instances when the operator plans to repeat the POC BG test immediately.
Evaluated Data
All deleted and repeated POC BG values performed on inpatient units at both institutions during 2014 and 2015 were obtained from the Laboratory Medicine database. In 2016, after the end of the project period, all RNs and AP that perform inpatient glucose testing were invited via email to complete an online (Catalyst) survey titled POC BG Survey consisting of 10 questions which took less than 5 minutes to complete. Respondents were asked to identify reasons for deleting and repeating POC BG measurements and were allowed to choose more than one option. Emailed survey reminders were sent out after one week to staff who had not yet responded.
Statistical Analysis
Data are reported as mean ± standard deviation unless otherwise indicated. Means were compared using Student’s unpaired 2-sided t-tests or paired 2-sided t-tests. Categorical variables were analyzed using a chi-square test. For all comparisons the null hypothesis was rejected for a P value < .05.
Results
Survey to Assess Use of the POC Delete BG Option by Nurses
A survey of inpatient RNs and AP performed at the end of the project period evaluated use of the “DeleteBG WillRetest” option. The survey was sent to 2042 individuals and 489 (24%) responded. Of the respondents 443 (91%) were RNs and 46 (9%) were AP. Respondents estimated performing either an average of 0-10 POC BG tests weekly (63%) or >10 tests weekly (37%). Importantly, 59 (12%) of respondents were unaware of the “DeleteBG WillRetest” option, while 92 (19%) of respondents said they never used this option. Of the 338 (69%) respondents who used “DeleteBG WillRetest,” the reasons they identified for choosing this option are detailed in Table 1, consistent with teaching that operators had received just prior to the project period. Incidence of identifying any reason to delete and repeat a POC BG measurement was not significantly different between users who performed ≤10 or >10 POC BG tests per week. Only the choices “no reason” or “never” were more common for users who performed ≤10 POC BG per week compared to those who performed >10/week (P = .009 by chi-square). Thus, inpatient RNs and AP identify specific reasons to delete and repeat POC BG tests, however, nearly one-third of operators may not be using this QI opportunity optimally.
Table 1.
Reasons to Delete and Repeat a POC BG Measurement in Hospitalized Patients Based on Questionnaire Answers Chosen by Inpatient Registered Nurses and Assistive Personnel.
| Reasons to delete and repeat a POC BG value | n of users (%) |
|---|---|
| Inadequate sample | 304 (90) |
| Does not match signs/symptoms | 267 (79) |
| Does not match trend | 243 (72) |
| Finger/sample not clean | 219 (65) |
| Value <40 mg/dL | 215 (64) |
| Value >300 mg/dL | 199 (59) |
| Patient requests recheck | 100 (30) |
| Hypoglycemia symptoms | 92 (27) |
Data shown as total number and percentage of respondents (users) who identified each reason (of the respondents who identified any reason). Respondents were able to choose more than one reason.
Deleted and Repeated POC BG Measurements
During the 24-month project period, 623, 327 inpatient POC BG measurements were performed at our two institutions. The “DeleteBG WillRetest” option was chosen 5119 (0.8%) times (Table 2). To determine if deleted and repeated POC BG values were targeted versus random we evaluated POC BG values in four groups based on the initial value: (1) <40 mg/dL, (2) 40-69 mg/dL, (3) 100-180 mg/dL, and (4) >400 mg/dL (Table 2). The percentage of deleted POC BG values within groups was significantly higher than predicted by chance (0.8%) for three groups, <40 mg/dL: 35%, 40-69 mg/dL: 10%, and >400 mg/dL: 14% (all P < .001, Table 2, % deleted), while for the fourth group, 100-180 mg/dL, only 0.2% of tests were deleted and repeated. Evaluated as a percentage of deleted values, all four groups were statistically different from expected based on the frequency of occurrence of these values among all POC BG tests (<40 mg/dL: 3.8% of deleted vs 0.1% of all, 40-69 mg/dL: 15% vs 1.2%, 100-180 mg/dL: 11% vs 62%, >400 mg/dL: 16% vs 0.9%, P < .001 for all, Table 2, %). These data support those from our survey demonstrating that RNs and AP are selecting POC BG measurements to be deleted and repeated based on specific criteria.
Table 2.
POC BG Values Groups.
| POC BG value group mg/dL | <40 | % | 40-69 | % | 100-180 | % | >400 | % | |
|---|---|---|---|---|---|---|---|---|---|
| All | 623 327 | 559 | 0.1 | 7657 | 1.2 | 383 888 | 62 | 5775 | 0.9 |
| Deleted | 5119 | 196 | 3.8* | 773 | 15* | 582 | 11* | 804 | 16* |
| % deleted | 0.8 | 35* | 10* | 0.2 | 14* |
The number and percentage of all and deleted POC BG values are shown for four groups of POC BG Value Ranges: (1) <40 mg/dL, (2) 40-69 mg/dL, (3) 100-180 mg/dL, and (4) >400 mg/dL. The percentage of all POC BG values deleted within each group is also shown (% deleted).
Evaluating Deleted POC BG Values Likely to Be Measurement/Operator Errors
Our initial work in this area identified likely POC BG measurement/operator errors that followed a consistent pattern, an extreme (high or low) POC BG value that was followed within 5 minutes by a POC BG that was normal or continued the previous POC BG trend for that patient without any documentation of intervention.6 This project confirms the frequency of these POC BG measurement/operator errors. Initial POC BG values <40 mg/dL, 40-69 mg/dL, or >400 mg/dL were commonly deleted and repeated (Table 2). Of the 196 deleted POC BG values <40 mg/dL, we evaluated 172/196 (88%) values that were repeated within 5 minutes of the initial, deleted POC BG measurement. While choosing the “DeleteBG WillRetest” option implies that the value is considered inaccurate and is not immediately acted on, this cutoff allows greater confidence that no intervention or clinical variable would have changed the BG value between the two measurements. Of these 172 initial values <40 mg/dL, 100 (58%) of the repeated values are ≥70 mg/dL with a mean increase of 108 ± 6 mg/dL even though the value was repeated nearly immediately (mean time to repeat 2:03 ± 0:05 minutes). Importantly, this represents 18% (100/559) of all POC BG values <40 mg/dL.
Similarly, among the deleted POC BG measurements 40-69 mg/dL, we found that 634/773 (82%) were repeated within 5 minutes of the initial, deleted POC BG measurement. Of these, 110/634 (17%) were normal (100-180 mg/dL) with a mean increase of 73 ± 4 mg/dL (mean time to repeat 2:03 ± 0:05 minutes). This represents 1.4% of all POC BG values 40-69 mg/dL.
Finally, of the deleted POC BG measurements >400 mg/dL, we found that 644/804 (80%) were repeated within 5 minutes of the initial, deleted POC BG measurement. Of these, 156/644 (24%) were <180 mg/dL with a mean decrease of 410 ± 6 mg/dL (mean time to repeat 2:09 ± 0:05 minutes). Another 108/644 (17%) were between 180-300 mg/dL with a mean decrease of 297 ± 8 mg/dL (mean time to repeat 2:17 ± 0:06 minutes). Summed, these groups represent 40% of the deleted, and 5% of all POC BG values >400 mg/dL.
The total and percentage of POC BG values repeated in <5 minutes that were lower, the same, or higher than the deleted POC BG value are shown in Table 3.
Table 3.
Frequency of Repeated POC BG Values Being Lower, Equal, or Higher Than the Initial Deleted Value When Repeated in < 5 Minutes.
| Deleted POC BG value (n) | Repeated POC BG value < 5 minutes | ||
|---|---|---|---|
| Lower n (%) | Equal n (%) | Higher n (%) | |
| <40 mg/dL (172) | 20 (12) | 3 (2) | 149 (87) |
| 40-69 mg/dL (634) | 163 (26) | 37 (6) | 434 (68) |
| 100-180 mg/dL (373) | 188 (50) | 14 (4) | 171 (46) |
| >400 mg/dL (644) | 498 (77) | 44 (7) | 102 (16) |
Together, these data demonstrate that extreme POC BG values are commonly measurement/operator errors that can be identified and corrected by RNs and AP.
Evaluating Deleted POC BG Values Uncertain to Be Measurement/Operator Errors
In the same three groups of initial POC BG values we evaluated the deleted and repeated values that were not clearly measurement/operator errors based on the difference between the initial and repeated POC BG. For deleted POC BG values <40 mg/dL, 72/172 (42%) repeated values are <70 mg/dL, while for deleted POC BG values 40-69 mg/dL, 104/634 (16%) are between 70-99 mg/dL (mean time to repeat 1:58 ± 0:05 minutes, mean actual and absolute change +18 ± 1 mg/dL) and 404/634 (64%) of repeated values are <70 mg/dL (mean time to repeat 1:58 ± 0:02 minutes, mean actual change +1.0 ± 0.3 mg/dL, absolute POC BG change 4.0 ± 0.2 mg/dL). The number and percentage of repeated POC BG values that differed from the deleted value by more than 5, 10, 15, and 20 mg/dL are shown in Table 4.
Table 4.
Variance of Deleted and Repeated POC BG Values.
| POC BG deleted (mg/dL) | POC BG repeated (mg/dL) | Value difference >5 mg/dL, n (%) | Value difference >10 mg/dL, n (%) | Value difference >15 mg/dL, n (%) | Value difference >20 mg/dL, n (%) |
|---|---|---|---|---|---|
| <40 | <70 | 27/72 (38) | 18/72 (25) | 13/72 (18) | 10/72 (14) |
| 40-69 | <70 | 103/404 (25) | 34/404 (8) | 15/404 (4) | 6/404 (1) |
| Value difference >5%, n (%) | Value difference >10%, n (%) | Value difference >15%, n (%) | Value difference >20%, n (%) | ||
| 100-180 | 100-180 | 158/323 (49) | 94/323 (29) | 61/323 (19) | 42/323 (13) |
| >400 | >300 | 171/389 (44) | 90/389 (23) | 7/389 (2) | 4/389 (1) |
Data shown for four POC BG value ranges (<40 mg/dL, 40-69 mg/dL, 100-180 mg/dL, and >400 mg/dL) with the corresponding BG value ranges for the repeated POC BG that were considered not to be a measurement/operator error. For hypoglycemic initial values, variance is shown at the >5, >10, >15, and >20 mg/dL levels as total and percentage (note each greater level of variance is a subset of the previous). For BG values >70 mg/dL the variance is shown as >5, >10, >15, and >20% between the initial and repeated POC BG value (each greater level is a subset of the previous).
For deleted POC BG values >400 mg/dL, 389/644 (60%) of repeated values are >300 mg/dL (mean time to repeat 2:00 ± 0:03 minutes, mean actual change –24 ± 3 mg/dL and absolute change +38 ± 3 mg/dL). The >300 mg/dL (rather than >400 mg/dL) group was chosen to evaluate repeated POC BG values that represent true severe hyperglycemia. Differences between deleted and repeated POC BG values are shown in Table 4 as >5, >10, >15, and >20% different from the initial POC BG value.
Together, these data show that the differences between the deleted and immediately repeated POC BG values are greater than would be expected based on manufacturer’s standards, suggesting that RNs and AP may be identifying some factor making the POC BG value unreliable, although we acknowledge that this project cannot determine which value more accurately reflects the plasma BG.
Evaluating Deleted POC BG Values 100-180 mg/dL
We evaluated POC BG values in the normal range that would have been repeated for reasons other than extreme POC BG value. In this group, 373/582 (72%) of deleted POC BG tests were repeated within 5 minutes—a lower percentage than for the other groups evaluated (P < .001 by chi-square). Of these, 323/373 (87%) are 100-180 mg/dL (mean time to repeat 1:41 ± 0:03 minutes, mean actual change –1 ± 1 mg/dL and absolute change 13 ± 1 mg/dL). Differences between deleted and repeated POC BG values are shown in Table 4.
Review of All Hypoglycemic POC BG Values <40 mg/dL During 6 Months
We manually reviewed all POC BG values for the last 6 months of the project period from one of the two institutions, evaluating 86 455 POC BG tests. During this time there were 131 POC BG values documented as <40 mg/dL, 0.2% of the total (Figure 1). Of these 31 (24%) are deleted and repeated, and consistent with data above more than half of these (18/31) are >70 mg/dL on repeat invalidating 17 potential false hypoglycemic events (1 instance had two tests deleted and repeated within 5 minutes) in the EHR (Figure 1, black bar, Del, Rep; false). Another 60 (46%) values are neither deleted nor repeated (Figure 1, white bar, Not Del, Not Rep). However, 40 (31%) of values are not deleted, but are repeated, of which, 34 (26%) are true hypoglycemia (repeating the value causing 15 additional values <40 mg/dL [2 values are 40-69 mg/dL and counted as true hypoglycemia] in the EHR, Figure 1, light gray bar, Not Del, Rep; true), and 6 (5%) are > 70 mg/dL and are false hypoglycemia (causing 6 additional values <40 mg/dL in the EHR; Figure 1, med gray bar, Not Del, Rep; false). Based on these data we generated 6-month severe hypoglycemia (POC BG <40 mg/dL) metrics including event rate, and patient-day rate variables separated into, 1) optimal use of the DeleteBG WillRetest option (assuming all repeated values are initially deleted), 2) actual use (current project data), and 3) no use (assuming no option to delete and repeat) (Table 5). Optimal use of DeleteBG WillRetest has the potential to decrease documented severe hypoglycemic events from 131 to 81 (38% decrease) and severe hypoglycemic patient days from 99 to 81 (18% decrease).
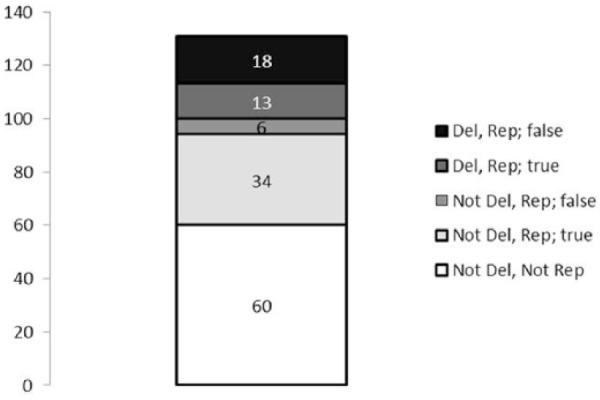
Analysis of all POC BG values <40 mg/dL at one institution over a 6-month period divided into 5 categories: (1) initial BG deleted and repeated value is ≥70 mg/dL (black bar, Del, Rep; false), (2) initial BG deleted and repeat value is <70 mg/dL (dark gray bar, Del, Rep; true), (3) initial BG not deleted and repeated value is ≥70 mg/dL (med gray bar, Not Del, Rep; false), (4) initial BG not deleted and repeated value <70 mg/dL (light gray bar, No Del, Rep; true), and (5) initial BG not deleted and not repeated (white bar, Not Del, Not Rep).
Table 5.
Analysis of All POC BG Values <40 mg/dL Over a 6-Month Period.
| Severe hypoglycemia (SevHypo) <40 mg/dL | Use of DeleteBG WillRest glucose meter option | ||
|---|---|---|---|
| Optimal | Actual | None | |
| SevHypo values | 81 | 106 | 131 |
| SevHypo rate (%) | 0.09 | 0.12 | 0.15 |
| SevHypo patient-days | 81 | 88 | 99 |
Glycemic metrics for severe hypoglycemia POC BG values <40 mg/dL (SevHypo) are shown as total number of values (SevHypo values) in the electronic health record, as percentage of all POC BG values (SevHypo rate), and patient days (SevHypo patient days). Outcomes are shown for three groups based on use of the option to delete and repeat POC BG values: (1) optimal (all repeated tests are initially deleted, theoretical), (2) actual (our current data), and (3) none (the option does not exist or is not used, theoretical).
Discussion
Accurate POC BG values are critical to support effective glycemic management strategies for hospitalized patients. Erroneous POC BG values affect common clinical decisions related to insulin administration, which may result in hypoglycemia or hyperglycemia, and related morbidities and mortality, excess costs and greater length of stay.12 Our current project shows that operators performing inpatient POC BG measurements frequently correctly identify POC BG values that are erroneous, and the option to delete and repeat POC BG values significantly reduces the number of extreme POC BG values documented in the EHR.
While our previously published QI project provided evidence for the hypothesis that erroneous POC BG values are frequently included in the EHR for ICU patients at one institution,6 this project proves this hypothesis conclusively for all hospitalized patients at two large tertiary care hospitals. While untested, it is likely that our findings are applicable beyond our own institutions and that other hospitals may want to explore the option to give RNs and AP the opportunity to delete and repeat POC BG values that they believe are erroneous to prevent these values from being uploaded permanently into the EHR.
Based on this project we plan to recommend that all POC BG values <40 mg/dL at our institutions be deleted and repeated unless the patient has clear clinical evidence of hypoglycemia, acknowledging (and teaching) that patients with true hypoglycemia may be asymptomatic making the rapidly repeated POC BG value of critical importance.
This strategy may also be warranted for POC BG values >400 mg/dL or POC BG values of 40-69 mg/dL since our data demonstrate high rates of measurement errors for these tests, though we did not manually evaluate repeated tests that are not deleted within those categories. While a policy to repeat values POC BG values >400 mg/dL would involve more repeated tests than for values <40 mg/dL (with material cost, operator time and patient discomfort), nonetheless, measurement errors >400 mg/dL in patients receiving correctional insulin are the most likely to result in inappropriate insulin doses and potential patient harm from hypoglycemia. This project did not determine patient harm related to measurement errors and, thus, a definitive policy will depend on further work. We suggest that RNs and AP delete and repeat POC BG values >400 or 40-69 mg/dL if symptoms do not match BG values or if the BG values are significantly different from previous trends.
Health care institutions and regulatory bodies continue to increase their emphasis on measuring quality of care.13 The inclusion of erroneous POC BG values in the EHR has the potential to skew both hypoglycemia and hyperglycemia metrics leading to an inaccurate assessment of hospital quality related to glycemic control as conclusively demonstrated by this project.
This project estimates that common hospital-reported hypoglycemia rates (either as a percentage of all POC measures or as hypoglycemic patient days)14 could be reduced by as much as 40% at hospitals implementing this QI strategy optimally; however, we found that at our own institutions, up to a third of glucose meter operators are not using the option to delete and repeat POC BG values.
The impact of erroneous severe hypoglycemic POC BG on hospital inpatient metrics should not be underestimated even though these are rare events. The Centers for Medicare and Medicaid Services (CMS) is in the process of revising and endorsing their metric for severe inpatient hypoglycemia (National Quality Foundation [NQF] 2363) related to treatment with medications to reduce BG. This metric, which documents rates of inpatient hypoglycemia <40 mg/dL, now includes instructions to ignore values that are followed by a POC BG >80 mg/dL obtained within 5 minutes of the initial hypoglycemic measurement. Inpatient metrics being proposed by Vizient or already implemented by the Washington State Hospital Association (WSHA) track hospital performance related to inpatient hypoglycemia focusing on values <50 mg/dL. In contrast to the NQF, these protocols eliminate duplicate values (lab or POC BG) within 30 minutes prior to the last hypoglycemic value to avoid inflating hypoglycemia statistics due to rechecks, but do not assess for inaccurate values that are normal when repeated within 5 minutes. Based on our data, hospitals that delete and repeat suspected erroneous hypoglycemic POC BG values would have significantly lower severe hypoglycemia rates than hospitals that do not delete and repeat POC BG values using the WSHA and proposed Vizient criteria, but not the proposed CMS-NQF criteria. Based on our data the CMS-NQF strategy to eliminate false hypoglycemic values will capture the majority of erroneous POC BG values for hospitals that do not adopt a strategy to delete and repeat POC BG values, but this would only be effective if inpatient hypoglycemia protocols mandate immediate reevaluation of severe hypoglycemic POC BG values in asymptomatic patients.
While the impact of erroneous POC BG values on hospital glycemic metrics is supported by data from this project, we cannot make conclusions about possible impact on patient safety. It is certainly likely that low POC BG values are acted on by giving IV dextrose or oral carbohydrates and holding prescribed insulin, while high POC BG are acted on by giving additional insulin—and either intervention could result in significant dysglycemia if the POC BG value was erroneous. Evaluating potential patient harm due to either hypo- or hyperglycemia caused by measurement error was out of the scope of this project, and would require a carefully designed and supported clinical study to be performed.
Our project has limitations. Glucose meter operators determined POC BG values to be deleted and repeated; thus, selection of deleted POC BG values was not randomized. Therefore, we need to rely on published manufacturer data for the expected variance in repeated POC BG would have been if deleted values were randomly chosen. This limitation has little impact on our conclusions related to measurement/operator error as extreme (low or high) values normalizing within 2 minutes is extremely unlikely to be due to chance, treatment or clinical change. However, for the remaining deleted values we cannot determine whether the initial or repeated value is more accurate. We can say that the variance between the two results is greater than expected based on manufacturer standards. However, previous studies have shown that POC BG performed in hospitalized patients may be less accurate than expected.3,15 Thus greater than expected variance could be due to RNs and AP correctly identifying inaccurate POC BG values, but other factors including, a statistical regression to the mean for extreme values, meter/strip inaccuracy, or specific factors in hospitalized patients cannot be excluded.4,5,15 Again, a randomized study would be the best method to answer this question.
In summary, this QI project demonstrates that giving operators the option to delete and repeat suspect POC BG values improves the quality of hospital glycemic metrics, has a significant impact on hospital performance related to hypoglycemia, and has the potential to improve patient safety by making operators more aware of POC BG measurement errors.
Acknowledgments
We are grateful for resources and time provided by Clinical Education, Laboratory Medicine and Quality Improvement personnel.
Footnotes
Abbreviations: AP, assistive personnel; BG, blood glucose; CMS, Centers for Medicare and Medicaid Services; EHR, electronic health record; NQF, National Quality Foundation; POC, point of care; QI, quality improvement; RN, registered nurse; UHC, University HealthSystem Consortium; WSHA, Washington State Hospital Association.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: BEW is a consultant for TransformativeMedicine (T4M).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
Articles from Journal of Diabetes Science and Technology are provided here courtesy of Diabetes Technology Society
Full text links
Read article at publisher's site: https://doi.org/10.1177/1932296818763891
Read article for free, from open access legal sources, via Unpaywall:
https://journals.sagepub.com/doi/pdf/10.1177/1932296818763891
Citations & impact
Impact metrics
Article citations
Adverse Event Data for Years 2018 to 2020 for Diabetes Devices.
J Diabetes Sci Technol, 16(5):1299-1302, 08 May 2021
Cited by: 3 articles | PMID: 33969718 | PMCID: PMC9445356
More Focus is Needed to Reduce Adverse Events for Diabetes Devices.
J Diabetes Sci Technol, 16(2):498-499, 08 Sep 2020
Cited by: 3 articles | PMID: 32900228 | PMCID: PMC8861793
Inpatient Hypoglycemia: The Challenge Remains.
J Diabetes Sci Technol, 14(3):560-566, 01 May 2020
Cited by: 9 articles | PMID: 32389071 | PMCID: PMC7576945
Review Free full text in Europe PMC
Predictors of Time-to-Repeat Point-of-Care Glucose Following Hypoglycemic Events in Hospitalized Patients.
J Diabetes Sci Technol, 14(3):526-534, 23 Oct 2019
Cited by: 0 articles | PMID: 31640421 | PMCID: PMC7576943
Getting More Information From Glucose Meter Evaluations.
J Diabetes Sci Technol, 13(6):1175-1177, 07 May 2019
Cited by: 1 article | PMID: 31064212 | PMCID: PMC6835175
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Reliability of Inpatient CGM: Comparison to Standard of Care.
J Diabetes Sci Technol, 17(2):329-335, 15 Dec 2021
Cited by: 8 articles | PMID: 34911384 | PMCID: PMC10012376
Addressing Hospital-Acquired Hypoglycemia.
Am J Nurs, 121(5):56-61, 01 May 2021
Cited by: 1 article | PMID: 33872265
Inpatient point-of-care bedside glucose testing: preliminary data on use of connectivity informatics to measure hospital glycemic control.
Diabetes Technol Ther, 9(6):493-500, 01 Dec 2007
Cited by: 24 articles | PMID: 18034603
Reexamining the evidence for inpatient glucose control: new recommendations for glycemic targets.
Am J Health Syst Pharm, 67(16 suppl 8):S3-8, 01 Aug 2010
Cited by: 19 articles | PMID: 20689151
Review




