Abstract
Purpose
There is limited data on radiotherapy (RT) for hepatocellular carcinoma (HCC) in patients with Child-Pugh classification B (CP-B). This study aimed to evaluate the treatment outcomes of fractionated conformal RT in HCC patients with CP-B.Materials and methods
We retrospectively reviewed the data of HCC patients with CP-B treated with RT between 2009 and 2014 at 13 institutions in Korea. HCC was diagnosed by the Korea guideline of 2009, and modern RT techniques were applied. Fraction size was ≤ 5 Gy and the biologically effective dose (BED) ≥ 40 Gy10 (α/β = 10 Gy). A total of 184 patients were included in this study.Results
Initial CP score was seven in 62.0% of patients, eight in 31.0%, and nine in 7.0%. Portal vein tumor thrombosis was present in 66.3% of patients. The BED ranged from 40.4 to 89.6 Gy10 (median, 56.0 Gy10). After RT completion, 48.4% of patients underwent additional treatment. The median overall survival (OS) was 9.4 months. The local progression-free survival and OS rates at 1 year were 58.9% and 39.8%, respectively. In the multivariate analysis, non-classic radiation-induced liver disease (RILD) (p < 0.001) and additional treatment (p < 0.001) were the most significant prognostic factors of OS. Among 132 evaluable patients without progressive disease, 19.7% experienced non-classic RILD. Normal liver volume was the most predictive dosimetric parameter of non-classic RILD.Conclusion
Fractionated conformal RT showed favorable OS with a moderate risk non-classic RILD. The individual radiotherapy for CP-B could be cautiously applied weighing the survival benefits and the RILD risks.Free full text

Treatment Outcome after Fractionated Conformal Radiotherapy for Hepatocellular Carcinoma in Patients with Child-Pugh Classification B in Korea (KROG 16-05)
Associated Data
Abstract
Purpose
There is limited data on radiotherapy (RT) for hepatocellular carcinoma (HCC) in patients with Child-Pugh classification B (CP-B). This study aimed to evaluate the treatment outcomes of fractionated conformal RT in HCC patients with CP-B.
Materials and Methods
We retrospectively reviewed the data of HCC patients with CP-B treated with RT between 2009 and 2014 at 13 institutions in Korea. HCC was diagnosed by the Korea guideline of 2009, and modern RT techniques were applied. Fraction size was ≤ 5 Gy and the biologically effective dose (BED) ≥ 40 Gy10 (α/β = 10 Gy). A total of 184 patients were included in this study.
Results
Initial CP score was seven in 62.0% of patients, eight in 31.0%, and nine in 7.0%. Portal vein tumor thrombosis was present in 66.3% of patients. The BED ranged from 40.4 to 89.6 Gy10 (median, 56.0 Gy10). After RT completion, 48.4% of patients underwent additional treatment. The median overall survival (OS) was 9.4 months. The local progression-free survival and OS rates at 1 year were 58.9% and 39.8%, respectively. In the multivariate analysis, non-classic radiation-induced liver disease (RILD) (p < 0.001) and additional treatment (p < 0.001) were the most significant prognostic factors of OS. Among 132 evaluable patients without progressive disease, 19.7% experienced non-classic RILD. Normal liver volume was the most predictive dosimetric parameter of non-classic RILD.
Conclusion
Fractionated conformal RT showed favorable OS with a moderate risk non-classic RILD. The individual radiotherapy for CP-B could be cautiously applied weighing the survival benefits and the RILD risks.
Introduction
Hepatocellular carcinoma (HCC) is one of the most common malignancies and the second leading cause of cancer-related death in the world [1]. Because HCC usually develops in patients with underlying liver cirrhosis, the coexistence of two life-threatening conditions of cancer itself and cirrhosis complicates the prognosis [2]. Child-Pugh classification (CP) is the most widely used system to assess the severity of underlying liver cirrhosis. In HCC patients with well-compensated liver function (CP class A, CP-A), the efficacy and safety of various treatment modalities according to the tumor extent are well documented. However, in cases of a borderline liver function (CP-B), liver cirrhosis further limits the applicability of certain treatment modalities because some standard therapies are a strain on the patients or can cause collateral damage to the non-cancerous liver tissue, thereby potentially further aggravating liver dysfunction [3]. A recent review article suggested that the best approach for treating HCC patients with CP-B would be to assess the prognostic weight of the HCC burden in the individual patient compared with that of cirrhosis severity and to adapt eventual tumor treatment to the liver function for tolerability and potential benefit [4].
Although radiotherapy (RT) was previously limited to HCC treatment owing to the low tolerance dose of the whole liver to RT [5], the developments in imaging and the introduction of 3-dimensional conformal radiotherapy (3DCRT) have enabled the delivery of conformal RT to the partial liver. In addition, further development of RT techniques, including intensity-modulated radiotherapy (IMRT), and stereotactic body radiotherapy (SBRT), have been expanded the role of RT for HCC [6]. Hepatic toxicity after RT is defined as radiation-induced liver disease (RILD), which typically occurs between 2 weeks to 3 months after RT, and the overall incidence has been reported to be 0%-20% [7,8]. Virtually all prospective and retrospective studies have included patients with CP-A and CP-B only, and the most of those with CP-B were classified as CP-B7 [9]. Culleton et al. [10] retrospectively reported that 63% of patients had a decline in CP score of ≥ 2 points after SBRT in HCC patients with CP-B or -C. In contrast, in subgroup analyses of ≤ 20 patients with CP-B in few studies, the incidence of RILD was 27%-63%. This suggest that SBRT should be used with caution or omitted for cases of severely impaired liver function.
Therefore, we performed a retrospective multi-institutional study with a large cohort obtained from 13 institutions of the Korean Radiation Oncology Group (KROG) to evaluate the efficacy and toxicity of fractionated conformal RT for HCC patients with CP-B.
Materials and Methods
1. Patient selection
We retrospectively reviewed the medical records of patients who received RT for HCC at 13 institutions of the KROG. The inclusion criteria were as follows: (1) HCC was diagnosed based on the Korean Liver Cancer Study Group (KLCSG) and the National Cancer Center (NCC) practice guideline of 2009 and was treated with RT between 2009 and 2014 [11]; (2) Eastern Cooperative Oncology Group performance score of 0-2; (3) CP-B; (4) treatment with modern RT techniques such as 3DCRT or IMRT; and (5) fraction size ≤ 5 Gy and the biologically effective dose (BED) ≥ 40 Gy10 when the α/β ratio was assumed to be 10 Gy. The exclusion criteria were as follows: (1) huge HCC beyond 60% of the total liver volume (TLV), for which RT was not feasible according to the KLCSG and NCC practice guideline of 2009; (2) extrahepatic spread beyond the regional lymph nodes; (3) history of previous RT to the liver; (4) history of additional RT for other HCC in the liver within 3 months; and (5) history of malignancies besides HCC within 5 years. A total of 184 patients were included in this study.
2. Evaluation of hepatic toxicity
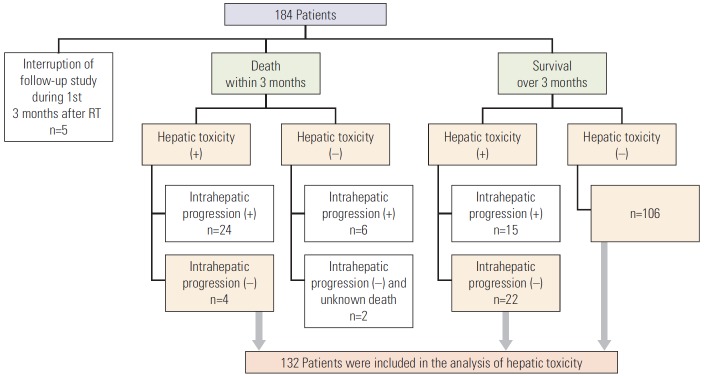
Patients underwent a physical examination, laboratory tests, and computed tomography and/or magnetic resonance imaging to assess hepatic function and evaluate the tumor extent before RT as well as to assess hepatic toxicity and the tumor response at follow-up visits. Hepatic toxicity was categorized as classic and non-classic RILD. Classic RILD included anicteric hepatomegaly, ascites, or elevated alkaline phosphatase more than twice the upper limit of normal value. Non-classic RILD included elevation of liver transaminases more than 5 times the upper limit of normal level or a worsening of CP score of ≥ 2 points. We defined the occurrence of non-classic RILD in the absence of documented progressive disease within 3 months after the end of RT as significant toxicity. Therefore, we subsequently excluded these patients from the entire study population as shown in Fig. 1 to minimize confounding factors. The remaining 132 patients were evaluated for hepatic toxicity.
For dosimetric analysis, the dose-volumetric values were calculated from dose-volume histograms. The normal liver volume (NLV) was defined as the TLV minus the gross tumor volume in seven institutions and as the TLV minus the planning target volume in six institutions. Doses delivered to specific volumes of the TLV and NLV were evaluated. Due to variations in the fractionation schemes among institutions, all doses were converted into the equivalent dose of 2 Gy per fraction (EQD2) using a linear-quadratic model when the α/β ratio for the normal liver was assumed to be 8 Gy (EQD2 with α/β ratio of 8 Gy=EQD28) [12]. This is applied to calculate the mean dose of the TLV (DTLV_mean EQD28) and NLV (DNLV_mean, EQD28), the percentage of the TLV ≥ 5 Gy (TLV5Gy EQD28), ≥ 10 Gy (TLV10Gy EQD28), ≥ 15 Gy (TLV15Gy EQD28), ≥ 20 Gy (TLV20Gy EQD28), ≥ 25 Gy (TLV25Gy EQD28), ≥ 30 Gy (TLV30Gy EQD28), ≥ 35 Gy (TLV35Gy EQD28), ≥ 40 Gy (TLV40Gy EQD28), the percentage of the NLV ≥ 5 Gy (NLV5Gy EQD28), ≥ 10 Gy (NLV10Gy EQD28), ≥ 15 Gy (NLV15Gy EQD28), ≥ 20 Gy (NLV20Gy EQD28), ≥ 25 Gy (NLV25Gy EQD28), ≥ 30 Gy (NLV30Gy EQD28), ≥ 35 Gy (NLV35Gy EQD28), and ≥ 40 Gy (NLV40Gy EQD28).
3. Statistics
Local progression was defined as tumor growth or regrowth in any direction beyond that on pre-RT images of treated lesions by the modified Response Evaluation Criteria in Solid Tumor. Intrahepatic progression was defined as any progression within the liver. Local progression-free survival (LPFS), intrahepatic progression-free survival (IHPFS), and overall survival (OS) rates were estimated using the Kaplan-Meier method from the date of start of RT. Patients were censored at the date of death or at the date of last known follow-up, whichever came first. Prognostic factors affecting OS were analyzed using the Kaplan-Meier method for univariate analysis. Multivariate analysis was performed using a Cox proportional hazards model. A p-value < 0.05 was considered statistically significant.
To determine parameters affecting non-classic RILD in evaluable patients, clinical parameters were analyzed as categorical or continuous variables, and dosimetric parameters were analyzed as continuous variables. Univariate logistic regression analysis was performed to compare clinical and dosimetric parameters. In addition, a calculation of the area under the curve (AUC) of receiver operating characteristics (ROC) was used to determine the most predictive dosimetric parameter of non-classic RILD. As the AUC approximates 1.0, the parameter becomes more predictive of non-classic RILD. All calculations were performed using the Statistical Package for the Social Sciences software (SPSS ver. 20.0, IBM Corp., Armonk, NY).
4. Ethical statement
The current study was approved by the KROG (KROG 16-05) and the institutional review board of each participating institution (K-2016-2830). Written informed consent was waived due to the retrospective nature of the study.
Results
1. Patients’ characteristics
Patients’ characteristics at baseline are summarized in Table 1. Of 184 patients, the median age was 58 years. Viralassociated hepatitis due to hepatitis B or C virus was presented in 87.0% of patients. CP score was seven in 114 patients (62.0%), eight in 57 patients (31.0%), and nine in 13 patients (7.0%). The median tumor size was 5.4 cm. A single lesion was presented in 45.1% and portal vein tumor thrombosis (PVTT) was present in 66.3%. One hundred five patients (57.1%) had liver-directed therapy with 1-18 interventions (median, 2) before RT; 80.0% received transarterial chemoembolization (TACE). Combined treatment, defined as a treatment administered within 4 weeks of the start or end of RT, was conducted in 114 patients (62.0%); the most common modality was TACE in 81 patients, followed by transcatheter arterial chemotherapy infusion (TACI) in 32 patients. Most patients (87.5%) received 3DCRT, and 53.8% of patients received curative-intent RT, including all viable tumors. The total RT dose ranged from 31.5 to 64.0 Gy (median, 44.0 Gy), and the fraction size ranged from 1.5 to 5.0 Gy (median, 2.5 Gy). Eighty-nine patients (48.4%) underwent additional treatment after RT with 1-9 interventions (median, 2), including TACE (67 patients), TACI (15 patients), sorafenib (13 patients), systemic chemotherapy (6 patients), RT (5 patients), liver transplantation (5 patients), and radiofrequency ablation (1 patient).
Table 1.
Patients’ characteristics at baseline
| Characteristic | No. of patients (%) |
|---|---|
| Age, median (range, yr) | 58 (39-85) |
| Sex | |
 Male Male | 158 (85.9) |
 Female Female | 26 (14.1) |
| ECOG score | |
 0 0 | 54 (29.3) |
 1 1 | 80 (43.5) |
 2 2 | 50 (27.2) |
| Hepatitis | |
 No No | 11 (6.0) |
 HBV HBV | 135 (73.4) |
 HCV HCV | 25 (13.6) |
 Alcoholic Alcoholic | 13 (7.0) |
| Initial CP score | |
 7 7 | 114 (62.0) |
 8 8 | 57 (31.0) |
 9 9 | 13 (7.0) |
| Tumor size, median (range, cm) | 5.4 (1-21) |
| No. of tumors | |
 1 1 | 83 (45.1) |
 2-3 2-3 | 54 (29.4) |
 4-9 4-9 | 23 (12.5) |
 ≥ 10 ≥ 10 | 24 (13.0) |
| Tumor location | |
 One lobe One lobe | 131 (71.2) |
 Both lobes Both lobes | 53 (28.8) |
| Bile duct invasion | |
 No No | 150 (81.5) |
 Yes Yes | 34 (18.5) |
| PVTT | |
 No No | 62 (33.7) |
 Yes Yes | 122 (66.3) |
  Main PVTT Main PVTT | 54 (44.3) |
  Branched PVTT Branched PVTT | 68 (55.7) |
| mUICC_T | |
 1 1 | 10 (5.4) |
 2 2 | 21 (11.4) |
 3 3 | 61 (33.2) |
 4 4 | 92 (50.0) |
| mUICC_N | |
 0 0 | 158 (85.9) |
 1 1 | 26 (14.1) |
| Previous liver-directed therapy | |
 No No | 79 (42.9) |
 Yes Yes | 105 (57.1) |
| Combined treatment | |
 No No | 70 (38.0) |
 Yes Yes | 114 (62.0) |
| Fraction size, median (range, Gy) | 2.5 (1.5-5) |
| BED, median (range, Gy10) | 56.0 (40.4-89.6) |
| RT completion | |
 Yes Yes | 179 (97.3) |
 No No | 5 (2.7)a) |
| AFP, median (range, IU/mL) | 242.7 (0.7-1136990) |
| Additional treatment | |
 No No | 95 (51.6) |
 Yes Yes | 89 (48.4) |
ECOG, Eastern Cooperative Oncology Group; HBV, hepatitis B virus; HCV, hepatitis C virus; CP, Child-Pugh; PVTT, portal vein tumor thrombosis; mUICC, the modified International Union Against Cancer stage; T, tumor; N, lymph nodes; BED, biologically effective dose when the α/β ratio was assumed to be 10 Gy; AFP, α-fetoprotein.
2. Outcomes
The median follow-up period was 7.3 months (range, 0.7 to 67.7 months). The median OS was 9.4 months, and the actuarial 6-month and 1-year LPFS, IHPFS, and OS rates were 78.0% and 58.9%, 43.1% and 22.1%, and 70.8% and 39.8%, respectively (Fig. 2). Hepatic toxicity occurred in 80 patients (43.5%) within 3 months after the end of RT; 22 patients (12.0%) experienced classic RILD and 66 (35.9%) experienced non-classic RILD (Fig. 3A). After the occurrence of classic RILD, 15 patients (68.2%) recovered their own liver function: three patients (13.6%) suffered from persistent hepatic dysfunction; four patients (18.2%) experienced intrahepatic progression and were impossible to assess. Among patients with non-classic RILD, 10 patients (15.2%) recovered their own liver function: 17 patients (25.8%) suffered from persistent hepatic dysfunction; 39 patients (59.0%) experienced intrahepatic progression and were impossible to assess. The results of the univariate and multivariate analysis for prognostic factors affecting OS are summarized in Table 2. In multivariate analysis, non-classic RILD (hazard ratio [HR], 2.674; 95% confidence interval [CI], 1.826 to 3.916; p < 0.001) and additional treatment (HR, 2.159; 95% CI, 1.479 to 3.152; p < 0.001) were the most significant factors affecting OS.
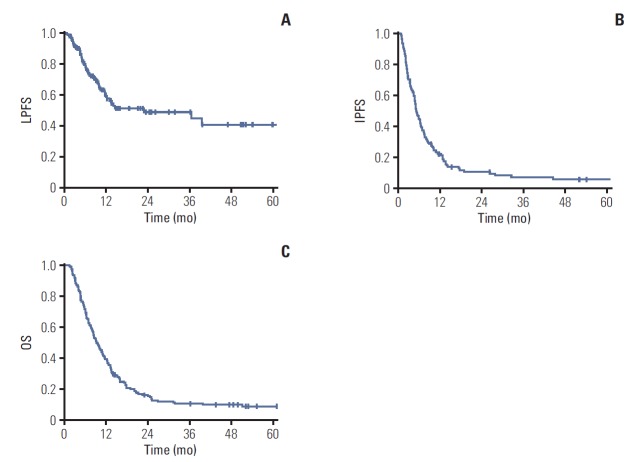
Local progression-free survival (LPFS) (A), intrahepatic progression-free survival (IPFS) (B), and overall survival (OS) (C) curves.
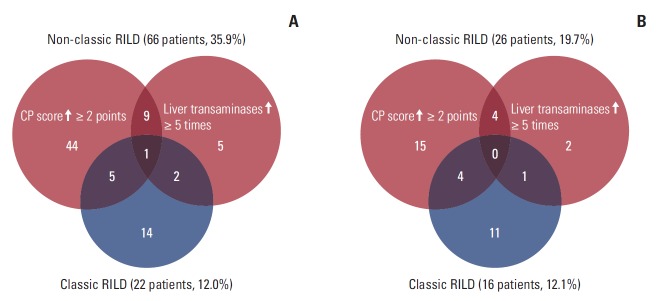
Hepatic toxicity defined as classic and non-classic radiation-induced liver disease (RILD) within 3 months after the end of radiotherapy in 184 patients (entire cohort, A) and in 132 patients (evaluable cohort, B). CP, Child-Pugh classification.
Table 2.
Univariate analysis and multivariate analysis for prognostic factors affecting OS
| Factor | No. of patients | 1-Year OS (%) | Median OS (mo) | UVA p-value | MVA HR (95% CI) | MVA p-value |
|---|---|---|---|---|---|---|
| Age (yr) | ||||||
 ≤ 60 ≤ 60 | 107 | 30.8 | 8.3 | 0.154 | 0.722 | 0.104 |
 > 60 > 60 | 77 | 51.3 | 12.2 | (0.487-1.069) | ||
| Sex | ||||||
 Male Male | 158 | 35.8 | 9.1 | 0.055 | 1.174 | 0.622 |
 Female Female | 26 | 60.6 | 13.4 | (0.621-2.219) | ||
| ECOG score | ||||||
 0-1 0-1 | 134 | 40.2 | 9.4 | 0.817 | - | - |
 2 2 | 50 | 37.2 | 9.7 | |||
| Hepatitis | ||||||
 No No | 10 | 57.1 | 20.7 | 0.020 | Reference | 0.011 |
 HBV/HCV HBV/HCV | 160 | 40.0 | 9.5 | 1.970 (0.829-4.683) | 0.125 | |
 Alcoholic Alcoholic | 14 | 19.0 | 5.3 | 4.559 (1.570-13.235) | 0.005 | |
| Initial CP score | ||||||
 7 7 | 114 | 43.2 | 10.7 | 0.381 | - | - |
 8 8 | 57 | 35.5 | 9.1 | |||
 9 9 | 13 | 23.1 | 5.6 | |||
| Tumor size (cm) | ||||||
 ≤ 5 ≤ 5 | 85 | 48.7 | 11.1 | 0.019 | - | - |
 > 5 > 5 | 99 | 31.4 | 8.0 | |||
| No. of tumors | ||||||
 1-3 1-3 | 137 | 43.6 | 10.1 | 0.014 | - | - |
 ≥ 4 ≥ 4 | 47 | 26.7 | 8.0 | |||
| Tumor location | ||||||
 One lobe One lobe | 131 | 42.1 | 10.1 | 0.052 | - | - |
 Both lobes Both lobes | 53 | 32.6 | 8.2 | |||
| PVTT | ||||||
 No No | 62 | 55.1 | 13.2 | < 0.001 | 1.022 | 0.928 |
 Yes Yes | 122 | 31.6 | 8.0 | (0.636-1.643) | ||
| mUICC_T | ||||||
 1, 2 1, 2 | 31 | 72.7 | 24.1 | < 0.001 | 3.277 | 0.002 |
 3, 4 3, 4 | 153 | 32.5 | 8.3 | (1.546-6.944) | ||
| mUICC_N | ||||||
 0 0 | 158 | 41.8 | 10.0 | 0.031 | 1.355 | 0.242 |
 1 1 | 26 | 22.8 | 6.4 | (0.815-2.254) | ||
| Initial AFP (IU/mL) | ||||||
 ≤ 200 ≤ 200 | 87 | 47.1 | 11.1 | 0.003 | 1.875 | 0.005 |
 > 200 > 200 | 92 | 29.2 | 8.0 | (1.207-2.911) | ||
| RT aima) | ||||||
 Curative Curative | 99 | 43.2 | 10.1 | 0.044 | 0.876 | 0.486 |
 Palliative Palliative | 85 | 34.8 | 8.3 | (0.604-1.271) | ||
| BED (Gy10) | ||||||
 ≤ 53 ≤ 53 | 75 | 31.4 | 8.3 | 0.029 | 0.946 | 0.760 |
 > 53 > 53 | 109 | 45.1 | 10.1 | (0.664-1.349) | ||
| AFP responseb) | ||||||
 Yes Yes | 79 | 44.4 | 9.8 | 0.012 | 0.593 | 0.013 |
 No No | 81 | 24.2 | 6.6 | (0.393-0.894) | ||
| Classic RILD | ||||||
 No No | 162 | 41.2 | 9.7 | 0.582 | - | - |
 Yes Yes | 22 | 27.3 | 7.7 | |||
| Non-classic RILD | ||||||
 No No | 118 | 51.3 | 12.2 | < 0.001 | 2.674 | < 0.001 |
 Yes Yes | 66 | 17.2 | 5.1 | (1.826-3.916) | ||
| Additional treatment | ||||||
 No No | 95 | 27.0 | 7.0 | 0.001 | 2.159 | < 0.001 |
 Yes Yes | 89 | 51.7 | 12.2 | (1.479-3.152) |
OS, overall survival; UVA, univariate analysis; MVA, multivariate analysis; HR, hazard ratio; CI, confidence interval; ECOG, Eastern Cooperative Oncology Group; HBV, hepatitis B virus; HCV, hepatitis C virus; CP, Child-Pugh; PVTT, portal vein tumor thrombosis; mUICC, the modified International Union Against Cancer stage; T, tumor; N, lymph nodes; AFP, α-fetoprotein; RT, radiotherapy; BED, biologically effective dose when the α/β ratio was assumed to be 10 Gy; RILD, radiation-induced liver disease.
3. Predictors for non-classic RILD
In 132 evaluable patients described in Fig. 1, hepatic toxicity occurred in 37 patients (28.0%) within 3 months after the end of RT. The characteristics are listed in S1 Table. Classic RILD occurred in 16 patients (12.1%) and non-classic RILD occurred in 26 patients (19.7%); among patients with non-classic RILD, 23 patients experienced a worsening of CP score by ≥ 2 points (Fig. 3B). Univariate logistic regression analysis was conducted to determine clinical and dosimetric parameters affecting non-classic RILD, which was the most significant prognostic factor for OS in both univariate and multivariate analysis. Of the clinical parameters, only the RT technique was associated with the risk of non-classic RILD (p=0.007) (S2 Table). Of the dosimetric parameters, NLV, DTLV_mean EQD28, TLV15Gy EQD28, TLV20Gy EQD28, TLV35Gy EQD28, and TLV40Gy EQD28 were associated with the risk of non-classic RILD (Table 3). NLV was the most predictive dosimetric parameter based on compared values from the AUC of ROC.
Table 3.
Univariate analysis for dosimetric parameters affecting non-classic radiation-induced liver disease
| Parameter | Mean±standard deviation | p-value | ROC AUC |
|---|---|---|---|
| GTV (mL) | 287.7±585.7 | 0.211 | 0.666 |
| TLV (mL) | 1,555.8±758.7 | 0.311 | 0.571 |
| NLV (mL) | 1,184.4±442.2 | 0.013 | 0.694 |
| DTLV_mean EQD28 (Gy)a) | 18.1±8.8 | 0.041 | 0.593 |
| TLV5Gy EQD28 (%)b) | 71.8±17.3 | 0.120 | 0.582 |
| TLV10Gy EQD28 (%) | 58.9±18.3 | 0.082 | 0.607 |
| TLV15Gy EQD28 (%) | 50.0±18.9 | 0.023 | 0.644 |
| TLV20Gy EQD28 (%) | 43.2±19.6 | 0.019 | 0.648 |
| TLV25Gy EQD28 (%) | 37.6±19.6 | 0.051 | 0.618 |
| TLV30Gy EQD28 (%) | 32.7±19.9 | 0.051 | 0.594 |
| TLV35Gy EQD28 (%) | 28.5±19.3 | 0.039 | 0.595 |
| TLV40Gy EQD28 (%) | 21.8±19.5 | 0.003 | 0.635 |
| DNLV_mean EQD28 (Gy) | 13.9±5.4 | 0.794 | 0.508 |
| NLV5Gy EQD28 (%)c) | 68.7±17.4 | 0.203 | 0.582 |
| NLV10Gy EQD28 (%) | 53.0±16.2 | 0.373 | 0.560 |
| NLV15Gy EQD28 (%) | 42.0±15.2 | 0.190 | 0.592 |
| NLV20Gy EQD28 (%) | 34.1±14.4 | 0.143 | 0.606 |
| NLV25Gy EQD28 (%) | 27.7±13.4 | 0.495 | 0.551 |
| NLV30Gy EQD28 (%) | 22.4±12.4 | 0.470 | 0.551 |
| NLV35Gy EQD28 (%) | 17.9±11.3 | 0.205 | 0.577 |
| NLV40Gy EQD28 (%) | 12.1±10.8 | 0.057 | 0.591 |
ROC, receiver operator characteristics; AUC, area under the curve; GTV, gross tumor volume; TLV, total liver volume; NLV, normal liver volume, which was defined as the total liver volume minus GTV in seven institutions and as the TLV minus the planning target volume in six institutions; EQD2, equivalent dose of 2 Gy per fraction.
Discussion
RT is mostly administered to HCC patients with CP-A, and only a few studies have examined the efficacy of RT for CP-B [13,14]. Culleton et al. [10] reported a median OS of 7.9 months in CP-B or -C patients treated with SBRT for HCC: 9.9 months in CP-B7 patients and 2.8 months in CP ≥ 8. In contrast, Nabavizadeh et al. [15] reported a superior survival rate of 11.8 months after SBRT or accelerated hypofractionated RT (AHRT). The authors suggested that favorable patients’ characteristics, such as a unifocal tumor, smaller tumor size, and PVTT in 10% of patients, may have contributed to the improvement in OS. Our fractionated conformal RT showed a comparable survival of 9.4 months, despite the inclusion of patients with unfavorable characteristics, e.g., T3/T4, multiple HCCs, large tumor size, and PVTT. However, local control (LC) was suboptimal compared with SBRT studies with a 1-year LPFS rate of 58.9%. Ohri et al. [16] found that there was no clear evidence for a dose-response relationship with a BED of 60-180 Gy10 for SBRT to primary liver tumors and suggested that SBRT with 60-72 Gy10 was a reasonable fractionation scheme, with a 2-year LPFS of 90%. In addition, Nabavizadeh et al. [15] showed statistically significant superior LC rates for SBRT group compared to AHRT group, with a 2-year LC rate of 94% versus 65%. However, a nationwide survey in Korea reported that SBRT was selectively used for small-sized HCC with CP-A and that RT was mainly considered for advanced HCC and combined treatment using fractionated conformal RT was common clinical practice patterns [17,18]. In addition, HCC occurs in developing countries, especially in Asia where there are limited health resources. Therefore, we suggest that fractionated conformal RT as a practical alternative to SBRT, although further prospective studies to improve its efficacy are required.
The incidence of RILD after RT is higher in HCC patients with CP-B than with CP-A. An SBRT study for HCC in 29 patients with CP-B or -C reported the highest toxicity rate of 63%, resulting in a worsening of CP score by ≥ 2 points after a median dose of 30 Gy in six fractions [10]. They suggested SBRT for selected CP-B7 patients but did not recommend it for patients with CP ≥ 8 outside of studies. Another study using SBRT (50 Gy in 5 fractions) or AHRT (45 Gy in 18 fractions) presented a worsening of CP score by ≥ 2 points in 27 out of 95 patients (28%) with CP-A or -B7 and in 18 out of 51 patients (35%) with CP-B8, -B9, or -C [15]. As the true tolerability of RT in patients with CP-B or -C is unknown, the authors proposed further prospective trials. In a hypofractionated 3DCRT study using 40-60 Gy with a fraction size of 4-8 Gy, classic or non-classic RILD occurred in 12 out of 20 patients (60%) with CP-B, compared to 7 out of 108 (6%) with CP-A [19]. They stated that CP-B patients did not tolerate the hypofractionated RT. On the other hand, conventional fractionated RT may be more tolerable. A 3DCRT study using 66 Gy in 33 fractions reported that three out of 11 patients (27%) with CP-B experienced grade 4 hepatic toxicity [20]. However, as all of these patients had grade 3 abnormalities before RT, the correlation of toxicity to the RT is not entirely clear. In the current study, non-classic RILD was observed in 19.7% of 132 evaluable patients after fractionated conformal RT with a median fraction size of 2.5 Gy. Considering that normal tissue toxicity is more greatly impacted by fraction size in terms of radiobiology, we suggested the use of fractionated conformal RT for HCC in CP-B patients to minimize toxicity [21]. Because most patients were CP-B7 or -B8, however, the safety of fractionated conformal RT for patients with CP-B9 has still undetermined and we should treat them with considerable caution.
To the best of our knowledge, this is the largest study in published data evaluating predictors for non-classic RILD in HCC patients with CP-B treated with fractionated conformal RT. Although several dosimetric parameters were statistically significant in univariate analysis, we were unable to identify the definite dosimetric constraints because values from the AUC of ROC were suboptimal for the selections of cut-off points. Other recent studies have attempted to obtain the definitive constraints in CP-B patients but did not succeed [15,22]. There are some practical limitations to identify dosimetric predictors. Firstly, our study applied various NLV definitions according to different institutions because plan data which was already approved before RT were retrospectively reviewed. In addition, we defined the α/β ratio of the normal liver as 8 to compare different fractionation schedules among institutions, based on the Korean data reflecting similarities in the underlying disease, applied fraction schemes, and combined modalities [12]. However, the α/β ratio of the normal liver is still unknown, and it ranges between 2, 2.5, 3, 8, and 10 [23-26]. These variances may confound the importance of dosimetric parameters. Secondly, RT for CP-B patients have a higher probability of RILD, especially non-classic RILD: however, the underlying pathology of non-classic RILD remains unclear [7]. Thirdly, CP-B, as a preexisting liver dysfunction, has the intrinsic morbidity. In a randomized trial in advanced HCC patients, the rate of serious adverse events among the placebo group because of progression of cirrhosis or HCC was 52% [27]. However, it is impossible to distinguish between RILD and the natural progression of underlying cirrhosis in a clinical setting. Therefore, further prospective studies are required to minimize confounding factors and obtain practical constraints.
There were some limitations to the current study. Firstly, there was the interinstitutional heterogeneity of HCC management, because the KLCSG and NCC practice guidelinerecommended RT only for HCC patients with well-preserved liver function (CP-A or upper B) and could not encompass all possible clinical situations. However, a certain degree of heterogeneity among institutions mirrors clinical practice in the real world, providing results more representative of what can be achieved in everyday practice than findings from an ideal setting [28]. This is particularly important for HCC as a large gap exists between applied practice and evidence-based treatment, making our multicenter study more representative [29]. Secondly, as we only included patients who received RT ≥ 40 Gy10, patients who could not complete RT or decreased the total dose due to acute toxicities or other possible causes would be excluded. This may overestimate the efficacy of RT for patients with CP-B. Thirdly, this study was a retrospective analysis. Therefore, selection and confounding biases may have occurred, and the rates of hepatic toxicity may have been underestimated. To minimize the effect of these limitations, we only analyzed cases with completed follow-up during the 3 months after RT without disease progression.
In conclusions, fractionated conformal RT showed favorable OS when compared to other published studies in HCC patients with CP-B and a moderate risk of non-classic RILD even if it was lower than that reported in previous SBRT studies. The individual RT for CP-B could be cautiously applied considering that non-classic RILD was the most significant factor affecting OS. In Korea, IMRT and proton beam therapy have been approved by the National Health Insurance Service from 2015. The application of these advanced RT techniques using fractionated RT might provide some answers to improve the efficacy of RT without increasing the incidence of non-classic RILD for HCC patients with CP-B.
Acknowledgments
This work was supported by the Soonchunhyang University Research Fund.
Footnotes
Conflict of interest relevant to this article was not reported.
Electronic Supplementary Material
Supplementary materials are available at Cancer Research and Treatment website (https://www.e-crt.org).
S2 Table.
Univariate analysis for clinical parameters affecting non-classic radiation-induced liver disease
References
Articles from Cancer Research and Treatment : Official Journal of Korean Cancer Association are provided here courtesy of Korean Cancer Association
Full text links
Read article at publisher's site: https://doi.org/10.4143/crt.2018.687
Read article for free, from open access legal sources, via Unpaywall:
http://www.e-crt.org/upload/pdf/crt-2018-687.pdf
Citations & impact
Impact metrics
Citations of article over time
Alternative metrics
Smart citations by scite.ai
Explore citation contexts and check if this article has been
supported or disputed.
https://scite.ai/reports/10.4143/crt.2018.687
Article citations
Development and validation of a nomogram for radiation-induced hepatic toxicity after intensity modulated radiotherapy for hepatocellular carcinoma: a retrospective study.
Jpn J Clin Oncol, 54(6):699-707, 01 Jun 2024
Cited by: 0 articles | PMID: 38376811 | PMCID: PMC11144290
Managing hepatocellular carcinoma across the stages: efficacy and outcomes of stereotactic body radiotherapy : A retrospective study.
Strahlenther Onkol, 200(8):715-724, 30 Apr 2024
Cited by: 0 articles | PMID: 38689147 | PMCID: PMC11272809
Low-dose radiotherapy combined with dual PD-L1 and VEGFA blockade elicits antitumor response in hepatocellular carcinoma mediated by activated intratumoral CD8+ exhausted-like T cells.
Nat Commun, 14(1):7709, 24 Nov 2023
Cited by: 5 articles | PMID: 38001101 | PMCID: PMC10673920
Radiotherapy plus anti-PD1 versus radiotherapy for hepatic toxicity in patients with hepatocellular carcinoma.
Radiat Oncol, 18(1):129, 04 Aug 2023
Cited by: 1 article | PMID: 37542246 | PMCID: PMC10403970
Radiotherapy trend in elderly hepatocellular carcinoma: retrospective analysis of patients diagnosed between 2005 and 2017.
Radiat Oncol J, 41(2):98-107, 22 Jun 2023
Cited by: 2 articles | PMID: 37403352 | PMCID: PMC10326507
Go to all (13) article citations
Data
Data behind the article
This data has been text mined from the article, or deposited into data resources.
BioStudies: supplemental material and supporting data
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Radiation-induced liver disease after three-dimensional conformal radiotherapy for patients with hepatocellular carcinoma: dosimetric analysis and implication.
Int J Radiat Oncol Biol Phys, 54(1):156-162, 01 Sep 2002
Cited by: 107 articles | PMID: 12182986
Advanced radiotherapy technique in hepatocellular carcinoma with portal vein thrombosis: Feasibility and clinical outcomes.
PLoS One, 16(9):e0257556, 23 Sep 2021
Cited by: 3 articles | PMID: 34555075 | PMCID: PMC8460041
Investigation of dosimetric variations of liver radiotherapy using deformable registration of planning CT and cone-beam CT.
J Appl Clin Med Phys, 18(1):66-75, 05 Dec 2016
Cited by: 2 articles | PMID: 28291931 | PMCID: PMC5689896
Radiation-Induced Liver Toxicity.
Semin Radiat Oncol, 27(4):350-357, 01 Oct 2017
Cited by: 35 articles | PMID: 28865518
Review
Funding
Funders who supported this work.