Abstract
Aims
Coronary flow reserve (CFR) is a physiological index for the assessment of myocardial flow impairment due to focal or microcirculatory coronary artery disease (CAD). Coronary flow capacity (CFC) is another flow-based concept in diagnosing ischaemic heart disease, based on hyperaemic average peak velocity (hAPV) and CFR. We evaluated clinical and haemodynamic factors which potentially influence CFR and CFC in non-obstructed coronary arteries.Methods and results
Intracoronary Doppler flow velocity measurements to obtain CFR and CFC were performed after inducing hyperaemia in 390 non-obstructed vessels of patients who were scheduled for elective percutaneous coronary intervention (PCI) of another vessel. Akaike's information criterion (AIC) revealed age, female gender, history of myocardial infarction, hypercholesterolaemia, diastolic blood pressure, oral nitrates and rate pressure product as independent predictors of CFR and CFC. After regression analysis, age and female gender were associated with lower CFR and age was associated with worse CFC in angiographically non-obstructed vessels.Conclusions
Age and female gender are associated with lower CFR, and age with worse CFC in an angiographically non-obstructed coronary artery. CFC seems to be less sensitive to variations in clinical and haemodynamic parameters than CFR and is therefore a promising tool in contemporary clinical decision making in the cardiac catheterisation laboratory.Free full text

Impact of clinical and haemodynamic factors on coronary flow reserve and invasive coronary flow capacity in non-obstructed coronary arteries: a patient-level pooled analysis of the DEBATE and ILIAS studies
Associated Data
Abstract
Aims
Coronary flow reserve (CFR) is a physiological index for the assessment of myocardial flow impairment due to focal or microcirculatory coronary artery disease (CAD). Coronary flow capacity (CFC) is another flow-based concept in diagnosing ischaemic heart disease, based on hyperaemic average peak velocity (hAPV) and CFR. We evaluated clinical and haemodynamic factors which potentially influence CFR and CFC in non-obstructed coronary arteries.
Methods and results
Intracoronary Doppler flow velocity measurements to obtain CFR and CFC were performed after inducing hyperaemia in 390 non-obstructed vessels of patients who were scheduled for elective percutaneous coronary intervention (PCI) of another vessel. Akaike’s information criterion (AIC) revealed age, female gender, history of myocardial infarction, hypercholesterolaemia, diastolic blood pressure, oral nitrates and rate pressure product as independent predictors of CFR and CFC. After regression analysis, age and female gender were associated with lower CFR and age was associated with worse CFC in angiographically non-obstructed vessels.
Conclusions
Age and female gender are associated with lower CFR, and age with worse CFC in an angiographically non-obstructed coronary artery. CFC seems to be less sensitive to variations in clinical and haemodynamic parameters than CFR and is therefore a promising tool in contemporary clinical decision making in the cardiac catheterisation laboratory.
Introduction
Maximal coronary flow and coronary flow reserve (CFR), defined as the ratio of maximal to resting coronary flow, are the critical determinants of myocardial ischaemia and its clinical consequences1,2. Such direct measurements of coronary flow may therefore be a valuable adjunct to coronary angiography and coronary pressure measurements3,4,5. Impaired CFR in particular has been extensively documented to be associated with an importantly increased risk for adverse clinical outcome, regardless of the technique used for its assessment6. Nonetheless, the potential influence of haemodynamic and clinical variables on CFR documented in small studies has historically been considered a limitation to the clinical application of CFR; however, the magnitude and clinical relevance of such variables as encountered in clinical practice have not been evaluated in larger clinical studies7,8,9. Moreover, following these concerns regarding CFR, the concept of (invasive) coronary flow capacity (CFC) was introduced. By integrating both CFR and maximal flow, CFC aims to overcome the limitations of CFR related to its potential dependence on haemodynamic conditions10,11. CFC is expected to be less dependent on systemic and coronary haemodynamics than CFR, but this has not been systematically evaluated. Assessment of invasive coronary flow velocity in coronary arteries in the absence of angiographical epicardial stenosis allows the systematic evaluation of the impact of clinical and haemodynamic factors, as encountered in routine clinical practice, on CFR and CFC11,12. Therefore, the purpose of this analysis was to explore which clinical and haemodynamic parameters influence CFR and CFC in angiographically non-obstructed coronary arteries and to determine the clinical relevance for the use of CFR and CFC in clinical decision making.
Methods
PATIENTS
The study population consisted of a total of 390 reference vessels (angiographic diameter stenosis [DS] <30%) of 390 patients with stable or unstable angina pectoris (class 1 to 3 according to the Canadian Cardiovascular Society [CCS] or Braunwald’s classification I or II) and with normal left ventricular function, who were scheduled for percutaneous coronary intervention (PCI) in single-vessel or multivessel disease. Patients were evaluated in the setting of two multicentre studies, DEBATE II (Doppler Endpoints Balloon Angioplasty Trial Europe II)13 and ILIAS (Intermediate Lesions: Intracoronary Flow Assessment versus 99mTc-MIBI SPECT)3. Only patients for whom all relevant parameters were documented were included in the analysis. Common exclusion criteria were acute myocardial infarction (MI) less than one week prior to angioplasty, chronic total occlusion, left ventricular hypertrophy or cardiomyopathy. All patients gave written informed consent.
INTRACORONARY FLOW VELOCITY ASSESSMENT
Flow measurements were performed in a reference coronary artery (DS <30% on visual estimation) using a 0.014-inch Doppler sensor-tipped guidewire (FloWire; Endosonics, Rancho Cordova, CA, USA, currently ComboWire™ XT; Philips Volcano, San Diego, CA, USA). Doppler flow velocity measurements were obtained during resting conditions (baseline average peak flow velocity [bAPV]), as well as during hyperaemia (hyperaemic average peak flow velocity [hAPV]) induced by an intracoronary bolus injection of adenosine (12-15 μg for the right coronary artery and 18-20 μg for the left coronary artery). Doppler flow velocity signals were used to calculate CFR, defined as the ratio of hAPV to bAPV. The definition of CFC was described previously elsewhere11,14,15. In brief, normal CFC was defined as CFR ≥2.8, as encountered in patients with risk factors for ischaemic heart disease (IHD) without epicardial narrowing14, with its corresponding hAPV ≥49.0 cm/s. Mildly reduced CFC was defined as CFR <2.8 but >2.1, which reflects the upper limit of reported CFR cut-off values for inducible ischaemia, and the corresponding hAPV <49.0 and >33.0 cm/s, respectively. Moderately reduced CFC was defined as CFR ≤2.1 and >1.7, analogous to the reported range of CFR cut-off values for inducible myocardial ischaemia, and the corresponding hAPV ≤33.0 and >26.0 cm/s, respectively. Finally, severely reduced CFC was defined as CFR ≤1.7, and corresponding hAPV ≤26.0 cm/s.
STATISTICAL ANALYSIS
Variables are presented as mean±SD or frequency (percentage), as appropriate. The rate pressure product (RPP) was calculated by multiplying heart rate with systolic blood pressure. Akaike’s information criterion (AIC) was used to determine the model with the best goodness of fit for predicting CFR or CFC, with candidate covariates including baseline characteristics, and angiographic and haemodynamic parameters (Table 1, Supplementary Table 1, Supplementary Table 2). The variables identified from the best model of fit according to AIC were entered in a linear multivariable regression analysis to identify independent predictors of CFR and ordinal multivariable regression analysis for CFC. A p-value below the two-sided α level of 0.1 for univariate and 0.05 for multivariate regression analysis was considered statistically significant. The Stata software package, version 13.1 (StataCorp, College Station, TX, USA), was used for all statistical analyses.
Table 1
| Mean±SD or n (%) | |
| Age, years | 59.2±10.8 |
| Male | 289 (74.1) |
| Previous MI | 126 (32.3) |
| Hypertension | 152 (40) |
| Diabetes mellitus | 31 (8) |
| Hypercholesterolaemia | 216 (55.4) |
| Current or previous smoker | 167 (42.8) |
| Positive family history | 167 (42.8) |
| Acetylsalicylic acid | 355 (91) |
| Beta-blocker | 269 (67.9) |
| Calcium antagonist | 200 (51.3) |
| Oral nitrates | 255 (65.4) |
| Interrogated vessel | 390 |
| RCx | 195 (50) |
| LAD | 155 (39.7) |
| RCA | 40 (10.3) |
Results
PATIENT CHARACTERISTICS
Patient characteristics are listed in Table 1. Mean age was 59±11 years and 74% were male (n=289). A total of 390 unobstructed vessels were interrogated, with the majority in the ramus circumflex artery (RCx) (n=195), followed by the left anterior descending artery (LAD) (n=155) and the right coronary artery (RCA) (n=40). Detailed characteristics have been described elsewhere13,16.
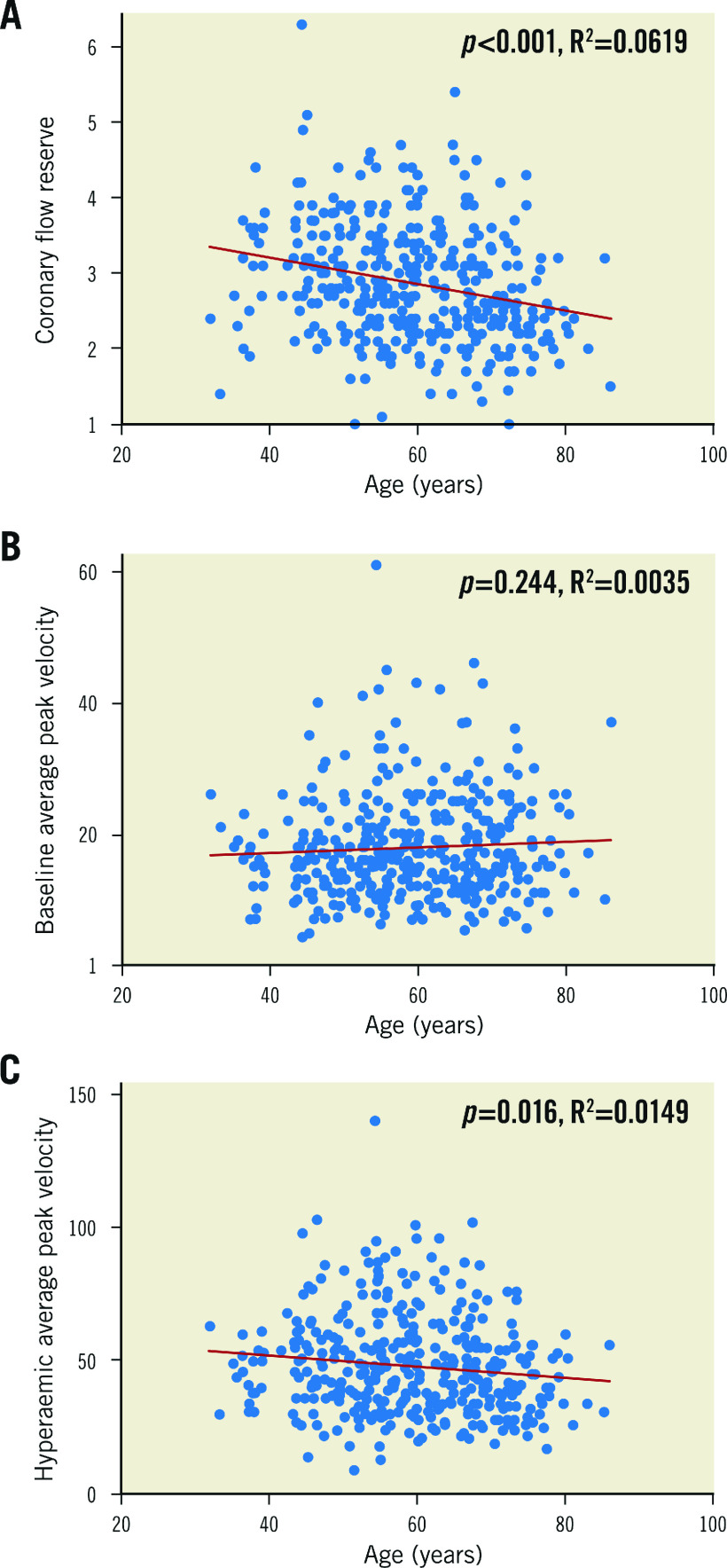
CFR AND CFC
Overall, mean CFR was 2.87±0.76 (Figure 1A). Men had higher mean CFR than women (2.96±0.04 versus 2.61±0.07, p=0.001). There was no significant difference in CFR between interrogated vessels: mean CFR was 2.83±0.79 for the RCx, 2.91±0.73 for the LAD and 2.90±0.75 for the RCA (p=0.16).
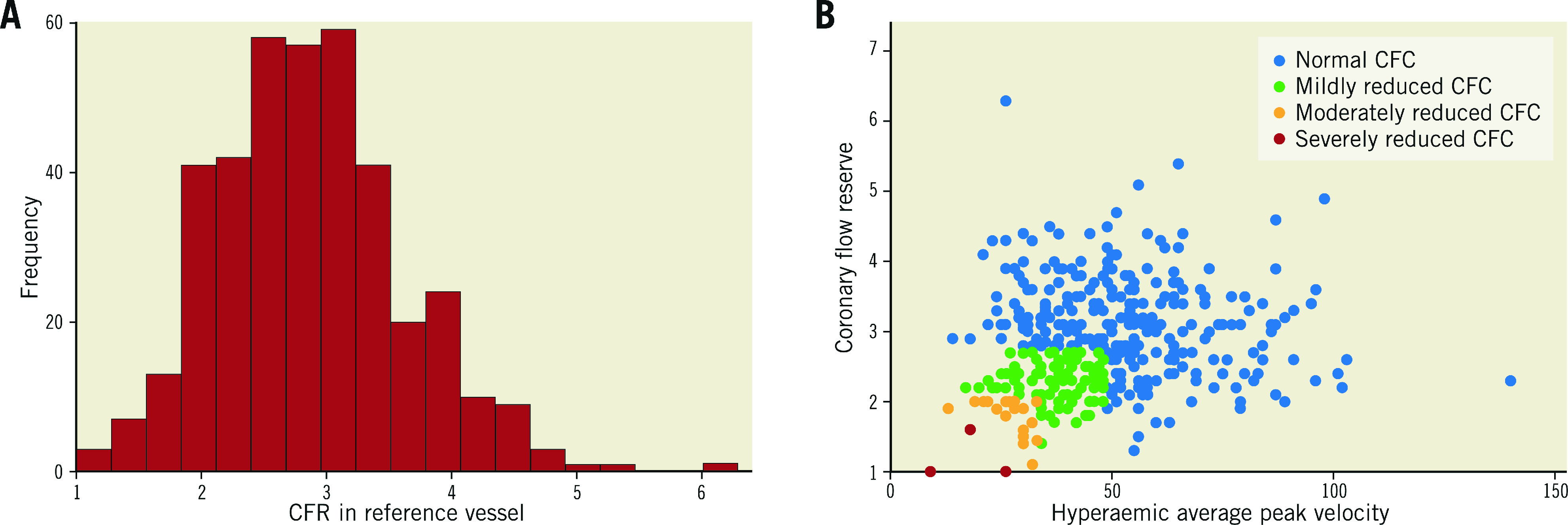
Overall CFR and CFC distribution. A) Overall CFR distribution. CFR mean±SD was 2.87±0.76. B) Overall CFC distribution based on CFR and hAPV.
Overall CFC distribution is shown in Figure 1B. Mean CFR, bAPV, and hAPV across the CFC categories are shown in Table 2. Mean CFR was 3.14±0.70 for normal CFC (n=278), 2.28±0.30 for mildly reduced CFC (n=90), 1.80±0.27 for moderately reduced CFC (n=19) and 1.2±0.35 for severely reduced CFC (n=3). CFR and CFC distribution per vessel is shown in Table 3.
Table 2
| CFC category | CFR | bAPV | hAPV |
| Normal (n=278) | 3.14±0.70 | 18.41±8.8 | 53.67±18.6 |
| Mildly reduced (n=90) | 2.28±0.30 | 16.53±3.9 | 36.9±7.0 |
| Moderately reduced (n=19) | 1.80±0.27 | 16.68±4.8 | 26.95±5.2 |
| Severely reduced (n=3) | 1.2±0.35 | 15.3±9.3 | 17.7±8.5 |
| bAPV: baseline average peak flow velocity; CFC: coronary flow capacity; CFR: coronary flow reserve; hAPV: hyperaemic average peak flow velocity | |||
Table 3
| Vessel | Normal CFC | Mildly reduced CFC | Moderately reduced CFC | Severely reduced CFC |
| RCx | 3.14±0.71 (n=136) | 2.30±0.28 (n=42) | 1.75±0.29 (n=14) | 1.2±0.35 (n=3) |
| LAD | 3.16±0.69 (n=112) | 2.29±0.31 (n=40) | 1.9 (n=3) | – |
| RCA | 3.15±0.70 (n=30) | 2.16±0.35 (n=8) | 2.0 n=2) | – |
| Total (n=390) | 278 | 90 | 19 | 3 |
DETERMINANTS OF CFR IN REFERENCE VESSELS
The best model for CFR identified by AIC included age, female gender, a history of MI, hypercholesterolaemia, diastolic blood pressure, oral nitrates and RPP. Univariate linear regression analysis and subsequent multivariate linear regression analysis (Table 4) revealed age (slope –0.014, 95% CI: –0.021 to –0.007, p<0.001), female gender (slope –0.212, 95% CI: –0.376 to –0.030, p=0.021) and oral nitrates (slope 0.162, 95% CI: 0.003 to 0.321, p=0.046) to be independently associated with CFR. The relationship between CFR and age is shown in Figure 2.
Table 4
| Univariate regression analysis | Multivariate regression analysis | |||||
| Slope | 95% CI | p-value | Slope | 95% CI | p-value | |
| Age | –0.018 | –0.024 to –0.011 | <0.001 | –0.014 | –0.021 to –0.007 | <0.001 |
| Female gender | –0.348 | –0.512 to –0.178 | <0.001 | –0.212 | –0.376 to –0.030 | 0.021 |
| RPP | –0.00007 | –0.0001 to 0.00004 | <0.001 | – | – | – |
| Hypercholesterolaemia | 0.19445 | 0.0429 to 0.346 | 0.012 | – | – | – |
| Oral nitrates | 0.1617 | 0.0028 to 0.3205 | 0.046 | 0.2202 | 0.031 to 0.409 | 0.023 |
RESTING AND HYPERAEMIC FLOW IN CFR CALCULATION
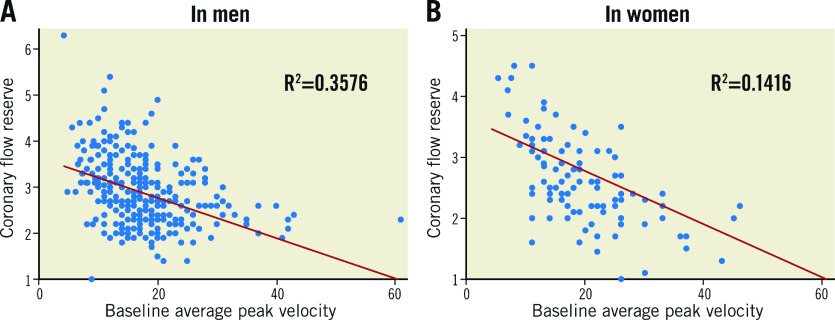
The parameters associated with CFR in angiographically non-obstructed vessels listed above were subsequently evaluated for their association with bAPV and hAPV to determine whether their impact on CFR derived from an effect on resting or hyperaemic flow (Table 5, Table 6). Increasing age was associated with a decrease in hAPV (slope –0.194, p=0.024), but not in bAPV (slope 0.044, p=0.223) (Figure 2). Gender was associated with bAPV, where women had higher bAPV than men (mean bAPV 19.4±8.3 cm/s versus 17.3±7.5 cm/s, slope 2.129, p=0.017) (Figure 3), but there was no association between gender and hAPV (slope –2.33; p=0.275). RPP was associated with bAPV (slope 0.0007; p<0.001), but not with hAPV (slope 0.0006; p=0.174). A history of MI, hypercholesterolaemia and current or prior smoking were not associated with bAPV (p=0.710, p=0.231 and p=0.271, respectively) or hAPV (p=0.576, p=0.915 and p=0.063, respectively).
Table 5
| Univariate regression analysis | Multivariate regression analysis | |||||
| Slope | 95% CI | p-value | Slope | 95% CI | p-value | |
| Female gender | 2.11 | 0.353 to 3.871 | 0.019 | – | – | – |
| RPP | 0.0007 | 0.0003 to 0.001 | <0.001 | 0.0005 | 0.0002 to 0.0009 | 0.002 |
| Diabetes mellitus | 2.87 | 0.013 to 5.723 | 0.049 | – | – | – |
| bAPV: baseline average peak flow velocity; RPP: rate pressure product | ||||||
Table 6
| Univariate regression analysis | Multivariate regression analysis | |||||
| Slope | 95% CI | p-value | Slope | 95% CI | p-value | |
| Age | –0.208 | –0.376 to –0.039 | 0.016 | –0.246 | –0.421 to –0.071 | 0.006 |
| Current or prior smoking | 3.883 | –0.189 to 7.173 | 0.039 | – | – | – |
| Acetylsalicylic acid | 6.052 | –0.334 to 12.44 | 0.063 | – | – | – |
DETERMINANTS OF CFC IN REFERENCE VESSELS
Univariate ordinal logistic regression analysis revealed age, RPP and oral nitrates to be associated with CFC. Subsequent multivariate ordinal logistic regression analysis revealed that age (slope 0.0397, 95% CI: 0.013 to 0.055, p=<0.001) was independently associated with worse CFC, whereas oral nitrate use (slope –0.577, 95% CI: –1.04 to –0.114; p=0.015) is associated with better CFC (Table 7).
Table 7
| Univariate regression analysis | Multivariate regression analysis | |||||
| Slope | 95% CI | p-value | Slope | 95% CI | p-value | |
| Age | 0.037 | 0.015 to 0.057 | 0.001 | 0.0397 | 0.013 to 0.055 | 0.001 |
| RPP | 0.0001 | 0.00001 to 0.00019 | 0.034 | – | – | – |
| Oral nitrates | –0.453 | –0.902 to –0.0031 | 0.048 | –0.5766 | –1.04 to –0.114 | 0.015 |
Discussion
This analysis from a large patient cohort consisting of two multicentre trials identified age and female gender as independent predictors of CFR in angiographically non-obstructed vessels. Age was the only independent predictor of a worse CFC in unobstructed coronary arteries. Oral nitrates are associated with both higher CFR and better CFC. This is therefore the first clinical study documenting that CFC is more independent of clinical and haemodynamic parameters as encountered in routine clinical practice compared with CFR, enhancing the diagnostic value of CFC over CFR alone.
ORIGIN OF ASSOCIATION BETWEEN CLINICAL AND HAEMODYNAMIC PARAMETERS AND FLOW ABNORMALITIES
CFR is a physiological parameter that has been extensively validated and is associated with improved risk stratification regarding major adverse cardiac events (MACE), regardless of the methodology used for its assessment6,17,18,19. However, in part due to its presumed sensitivity to variations in resting haemodynamics, its implementation in larger clinical practice has been limited. In the present study, age, female gender and oral nitrates significantly influenced CFR in a reference vessel. Interestingly, ageing was associated with lower CFR, mainly driven by a decrease in hAPV, as documented previously8,20. Female gender, in contrast, was associated with lower CFR, potentially due to a lower vascular tone and subsequently higher bAPV21. Cardiac workload estimated by RPP has generally been associated with an increase in both bAPV and hAPV22,23. Although a decrease in CFR is generally assumed with increases in cardiac workload, a simultaneous increase in maximal hyperaemic flow together with a proportional increase of baseline flow can result in a normal CFR24. Furthermore, de Bruyne et al25 found a significant association between CFR and haemodynamic changes in heart rate, blood pressure and contractility, but measured CFR under clinically challenging haemodynamic situations in which physiological assessment is usually not applied, since vasodilatory capacity is naturally impaired in these situations.
Oral nitrates induce vasodilation and a subsequent increase in coronary blood flow to the myocardium, resulting in higher CFR and CFC26.
Diabetes mellitus was not associated with lower CFR values in the present cohort. However, we found that diabetic patients had higher bAPV compared with non-diabetic patients (20.5±10.4 cm/s vs 17.6±7.5 cm/s, for diabetics and non-diabetics, respectively; p=0.046) but similar hAPV (52.6±18.4 cm/s vs 48.2±18.4 cm/s, for diabetics and non-diabetics, respectively; p=0.182). Higher bAPV in diabetics has been previously documented, and has been attributed to malfunctioning of the myocardial metabolism27,28, as well as impaired endothelial function, or even structural anatomical changes of the microcirculatory vasculature9,29. Although mean CFR values were not different between diabetics and non-diabetics in this study, higher resting flows evidently lead to lower CFR values in the individual patient and may impact on clinical decision making. Such an impact of diabetes on resting flow would be vanquished by using CFC.
Despite these considerations, the prognostic value of CFR in angiographically non-obstructed coronary arteries remains undisputed. Several studies have documented that lower CFR is associated with an increased risk of MACE, both in vessels with6,30 and in those without31 obstructive CAD.
THE CONCEPT OF CFC: hAPV COMPLEMENTING CFR
The concept of CFC was originally validated using PET imaging12, and has been extrapolated to invasive coronary flow measurements11. These studies suggested an improved risk stratification by using CFC over the application of CFR alone, although more definitive data are required for confirmation of these findings. In the present study, we found that CFC is mostly independent of clinical and haemodynamic factors except for age, overcoming most of the potential limitations of using CFR alone. By integrating CFR and hAPV, CFC is less prone to variations in baseline flow compared with CFR. As documented in the present study, this applies to alterations in flow in diabetics, female patients, and increases in cardiac workload. In the present study, age was the only parameter associated with lower CFC, which is anticipated since age impacts on CFR through a solitary decrease in hAPV, leading to a decrease in CFC through impairment of both CFR and hyperaemic flow.
CLINICAL IMPLICATIONS
It is increasingly recognised that IHD has a multilevel origin, and that a stenosis-centred approach seems insufficient for optimal treatment of this complex syndrome. Current pressure-derived indices such as fractional flow reserve (FFR) and instantaneous wave-free ratio (iFR) are frequently used in contemporary clinical practice to estimate flow impairment of a stenosis, but remain an imperfect reference standard for inducible myocardial ischaemia32. In the FAME 2 study (Fractional Flow Reserve versus Angiography for Multivessel Evaluation), comparing FFR-guided PCI with angiography-guided PCI, 50% of patients with FFR ≤0.80 treated with optimal medical therapy did not require revascularisation and 70% did not suffer from MACE during five years of follow-up33. Subsequently, it has been well documented that coronary flow is fundamentally more important than coronary pressure in maintaining coronary function32,34, leading to a clear need for a robust flow-based approach to diagnosis and treatment of IHD. CFR, although a robust risk-stratification tool at the population level3,35, has been documented to be influenced by clinical and haemodynamic parameters unrelated to the extent of CAD that might lead to inadvertent alterations of CFR that can impact on clinical decision making in the individual patient. Furthermore, we found that CFC is largely independent of these variables that occur in clinical practice, and it has been documented to enhance risk stratification provided by CFR11,12. The latter, in corroboration with the findings in the present study, support further research towards the implementation of CFC as a coronary flow-based index of CAD severity in contemporary clinical practice.
Limitations
This study is based on a post hoc analysis of two multicentre studies13,16, in which all coronary flow measurements were performed by interventional cardiologists with ample experience in coronary flow velocity assessment. Only patients for whom all baseline clinical and haemodynamic variables were available were included in this analysis, leading to a limited number of analysed variables and patients. Administered adenosine doses were recommended for inducing hyperaemia in the two included studies, but these dosages induce sufficient vasodilation for physiological assessment36. Furthermore, these measurements were performed in vessels with DS <30% by visual estimation, which does not exclude the presence of subclinical atherosclerosis that may impact on coronary flow values37,38. Intravascular ultrasound (IVUS) was not routinely performed to improve the selection of patients. Oral nitrates were not discontinued before intracoronary flow assessment, potentially increasing CFR and CFC due to permanent vasodilation.
Conclusions
Age and female gender are independent predictors of lower CFR in an angiographically non-obstructed vessel. Age is associated with worse CFC; thus, CFC seems to be more independent of clinical and haemodynamic parameters compared with CFR. Therefore, the present findings may strengthen the value of invasive coronary flow assessment in contemporary clinical decision making in the cardiac catheterisation laboratory.
Impact on daily practice
Coronary flow is a critical determinant of myocardial ischaemia and plays an essential role in maintaining myocardial function. Widespread implementation of coronary flow assessment in the catheterisation laboratory is partially hampered due to the presumed sensitivity of coronary flow assessment to clinical and haemodynamic parameters. We demonstrate that age and female gender are weakly associated with coronary flow reserve and only age is associated with worse coronary flow capacity in angiographically non-obstructed vessels, strengthening the role of a flow-based diagnostic approach towards ischaemic heart disease in contemporary clinical decision making in the cardiac catheterisation laboratory.
Guest Editor
This paper was guest edited by Alec Vahanian, MD, PhD; Department of Cardiology, Hôpital Bichat-Claude Bernard, and University Paris VII, Paris, France.
Supplementary data
Akaike’s information criterion selection process for CFR.
Akaike’s information criterion selection process for CFC.
Funding
The ILIAS (Intermediate Lesions: Intracoronary flow Assessment versus 99mTc-MIBI SPECT) study was supported by the Dutch Health Insurance Board (grant 96-036) and by a grant from the Netherlands Heart Foundation (grant 2000.090).
Conflict of interest statement
J.J. Piek is a clinical investigator sponsored by the Netherlands Heart Foundation (grant nos. D96.020 and 2000.090). The other authors have no conflicts of interest to declare. The Guest Editor is a consultant for Edwards Lifesciences.
Abbreviations
| bAPV | baseline average peak flow velocity |
| CFC | coronary flow capacity |
| CFR | coronary flow reserve |
| FFR | fractional flow reserve |
| hAPV | hyperaemic average peak flow velocity |
| IVUS | intravascular ultrasound |
| MACE | major adverse cardiac events |
| MI | myocardial infarction |
| RPP | rate pressure product |
Contributor Information
Valérie E. Stegehuis, Amsterdam UMC, University of Amsterdam, Heart Center, Department of Clinical and Experimental Cardiology, Amsterdam Cardiovascular Sciences, Amsterdam, the Netherlands.
Gilbert Wijntjens, Amsterdam UMC, University of Amsterdam, Heart Center, Department of Clinical and Experimental Cardiology, Amsterdam Cardiovascular Sciences, Amsterdam, the Netherlands.
Matthijs Bax, Haga Teaching Hospital, The Hague, the Netherlands.
Martijn Meuwissen, Amphia Hospital, Breda, the Netherlands.
Steven Chamuleau, Amsterdam UMC, University of Amsterdam, Heart Center, Department of Clinical and Experimental Cardiology, Amsterdam Cardiovascular Sciences, Amsterdam, the Netherlands.
Michiel Voskuil, University Medical Center Utrecht, Utrecht, the Netherlands.
Karel Koch, Amsterdam UMC, University of Amsterdam, Heart Center, Department of Clinical and Experimental Cardiology, Amsterdam Cardiovascular Sciences, Amsterdam, the Netherlands.
Carlo Di Mario, Careggi University Hospital, Florence, Italy.
Christiaan Vrints, University of Antwerp - Antwerp University Hospital, Antwerp, Belgium.
Michael Haude, Med. Klinik I, Städtische Kliniken Neuss, Lukaskrankenhaus GmbH, Neuss, Germany.
Eric Boersma, Erasmus Medical Center, Rotterdam, the Netherlands.
Patrick Serruys, Department of Cardiology, National University of Ireland, Galway (NUIG), Galway, Ireland. Imperial College London, London, United Kingdom.
Jan J. Piek, Amsterdam UMC, University of Amsterdam, Heart Center, Department of Clinical and Experimental Cardiology, Amsterdam Cardiovascular Sciences, Amsterdam, the Netherlands.
Tim van de Hoef, Amsterdam UMC, University of Amsterdam, Heart Center, Department of Clinical and Experimental Cardiology, Amsterdam Cardiovascular Sciences, Amsterdam, the Netherlands.
References
- Gould KL. Pressure-flow characteristics of coronary stenoses in unsedated dogs at rest and during coronary vasodilation. Circ Res. 1978;43:242–53. 10.1161/01.RES.43.2.242. [Abstract] [CrossRef] [Google Scholar]
- Uren NG, Melin JA, De Bruyne B, Wijns W, Baudhuin T, Camici PG. Relation between myocardial blood flow and the severity of coronary-artery stenosis. N Engl J Med. 1994;330:1782–8. 10.1056/NEJM199406233302503. [Abstract] [CrossRef] [Google Scholar]
- Chamuleau SA, Tio RA, de Cock CC, de Muinck ED, Pijls NH, Van Eck-Smit BL, Koch KT, Meuwissen M, Dijkgraaf MG, de Jong A, Verberne HJ, van Liebergen RA, Laarman GJ, Tijssen JG, Piek JJ. Prognostic value of coronary blood flow velocity and myocardial perfusion in intermediate coronary narrowings and multivessel disease. J Am Coll Cardiol. 2002;39:852–8. 10.1016/S0735-1097(01)01821-6. [Abstract] [CrossRef] [Google Scholar]
- Kern MJ, Donohue TJ, Aguirre FV, Bach RG, Caracciolo EA, Ofili E, Labovitz AJ. Assessment of angiographically intermediate coronary artery stenosis using the Doppler flowire. Am J Cardiol. 1993;71:26–33D. 10.1016/0002-9149(93)90131-U. [Abstract] [CrossRef] [Google Scholar]
- Naya M, Murthy VL, Taqueti VR, Foster CR, Klein J, Garber M, Dorbala S, Hainer J, Blankstein R, Resnic F, Di Carli MF. Preserved coronary flow reserve effectively excludes high-risk coronary artery disease on angiography. J Nucl Med. 2014;55:248–55. 10.2967/jnumed.113.121442. [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- van de Hoef TP, van Lavieren MA, Damman P, Delewi R, Piek MA, Chamuleau SA, Voskuil M, Henriques JP, Koch KT, de Winter RJ, Spaan JA, Siebes M, Tijssen JG, Meuwissen M, Piek JJ. Physiological basis and long-term clinical outcome of discordance between fractional flow reserve and coronary flow velocity reserve in coronary stenoses of intermediate severity. Circ Cardiovasc Interv. 2014;7:301–11. 10.1161/CIRCINTERVENTIONS.113.001049. [Abstract] [CrossRef] [Google Scholar]
- Kern MJ. Coronary physiology revisited: practical insights from the cardiac catheterization laboratory. Circulation. 2000;101:1344–51. 10.1161/01.CIR.101.11.1344. [Abstract] [CrossRef] [Google Scholar]
- Galderisi M, Rigo F, Gherardi S, Cortigiani L, Santoro C, Sicari R, Picano E. The impact of aging and atherosclerotic risk factors on transthoracic coronary flow reserve in subjects with normal coronary angiography. Cardiovasc Ultrasound. 2012;10:20. 10.1186/1476-7120-10-20. [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Nahser PJ Jr, Brown RE, Oskarsson H, Winniford MD, Rossen JD. Maximal coronary flow reserve and metabolic coronary vasodilation in patients with diabetes mellitus. Circulation. 1995;91:635–40. 10.1161/01.CIR.91.3.635. [Abstract] [CrossRef] [Google Scholar]
- van de Hoef TP, Echavarria-Pinto M, Escaned J, Piek JJ. Coronary flow capacity: concept, promises, and challenges. Int J Cardiovasc Imaging. 2017;33:1033–9. 10.1007/s10554-017-1125-z. [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- van de Hoef TP, Echavarria-Pinto M, van Lavieren MA, Meuwissen M, Serruys PW, Tijssen JG, Pocock SJ, Escaned J, Piek JJ. Diagnostic and Prognostic Implications of Coronary Flow Capacity: A Comprehensive Cross-Modality Physiological Concept in Ischemic Heart Disease. JACC Cardiovasc Interv. 2015;8:1670–80. 10.1016/j.jcin.2015.05.032. [Abstract] [CrossRef] [Google Scholar]
- Johnson NP, Gould KL. Integrating noninvasive absolute flow, coronary flow reserve, and ischemic thresholds into a comprehensive map of physiological severity. JACC Cardiovasc Imaging. 2012;5:430–40. 10.1016/j.jcmg.2011.12.014. [Abstract] [CrossRef] [Google Scholar]
- Chamuleau SA, Meuwissen M, Van Eck-Smit BL, Koch KT, de Jong A, de Winter RJ, Schotborgh CE, Bax M, Verberne HJ, Tijssen JG, Piek JJ. Fractional flow reserve, absolute and relative coronary blood flow velocity reserve in relation to the results of technetium-99m sestamibi single-photon emission computed tomography in patients with two-vessel coronary artery disease. J Am Coll Cardiol. 2001;37:1316–22. 10.1016/S0735-1097(01)01173-1. [Abstract] [CrossRef] [Google Scholar]
- Kern MJ, Bach RG, Mechem CJ, Caracciolo EA, Aguirre FV, Miller LW, Donohue TJ. Variations in normal coronary vasodilatory reserve stratified by artery, gender, heart transplantation and coronary artery disease. J Am Coll Cardiol. 1996;28:1154–60. 10.1016/S0735-1097(96)00327-0. [Abstract] [CrossRef] [Google Scholar]
- Meuwissen M, Siebes M, Chamuleau SAJ, Verhoeff BJ, Henriques JPS, Spaan JAE, Piek JJ. Role of fractional and coronary flow reserve in clinical decision making in intermediate coronary lesions. Interventional Cardiology. 2009;1:237–55. 10.2217/ica.09.33. [CrossRef] [Google Scholar]
- Serruys PW, De Bruyne B, Carlier S, Sousa JE, Piek J, Muramatsu T, Vrints C, Probst P, Seabra-Gomes R, Simpson I, Voudris V, Gurne O, Pijls N, Belardi J, van Es GA, Boersma E, Morel MA, van Hout B. Randomized comparison of primary stenting and provisional balloon angioplasty guided by flow velocity measurement. Doppler Endpoints Balloon Angioplasty Trial Europe (DEBATE) II Study Group. Circulation. 2000;102:2930–7. 10.1161/01.CIR.102.24.2930. [Abstract] [CrossRef] [Google Scholar]
- Meuwissen M, Chamuleau SA, Siebes M, de Winter RJ, Koch KT, Dijksman LM, van den Berg AJ, Tijssen JG, Spaan JA, Piek JJ. The prognostic value of combined intracoronary pressure and blood flow velocity measurements after deferral of percutaneous coronary intervention. Catheter Cardiovasc Interv. 2008;71:291–7. 10.1002/ccd.21331. [Abstract] [CrossRef] [Google Scholar]
- Murthy VL, Naya M, Foster CR, Gaber M, Hainer J, Klein J, Dorbala S, Blankstein R, Di Carli MF. Association between coronary vascular dysfunction and cardiac mortality in patients with and without diabetes mellitus. Circulation. 2012;126:1858–68. 10.1161/CIRCULATIONAHA.112.120402. [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Murthy VL, Naya M, Foster CR, Hainer J, Gaber M, Di Carli G, Blankstein R, Dorbala S, Sitek A, Pencina MJ, Di Carli MF. Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation. 2011;124:2215–24. 10.1161/CIRCULATIONAHA.111.050427. [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- Sara JD, Widmer RJ, Matsuzawa Y, Lennon RJ, Lerman LO, Lerman A. Prevalence of Coronary Microvascular Dysfunction Among Patients With Chest Pain and Nonobstructive Coronary Artery Disease. JACC Cardiovasc Interv. 2015;8:1445–553. 10.1016/j.jcin.2015.06.017. [Abstract] [CrossRef] [Google Scholar]
- Forte P, Kneale BJ, Milne E, Chowienczyk PJ, Johnston A, Benjamin N, Ritter JM. Evidence for a difference in nitric oxide biosynthesis between healthy women and men. Hypertension. 1998;32:730–4. 10.1161/01.HYP.32.4.730. [Abstract] [CrossRef] [Google Scholar]
- Czernin J, Muller P, Chan S, Brunken RC, Porenta G, Krivokapich J, Chen K, Chan A, Phelps ME, Schelbert HR. Influence of age and hemodynamics on myocardial blood flow and flow reserve. Circulation. 1993;88:62–9. 10.1161/01.CIR.88.1.62. [Abstract] [CrossRef] [Google Scholar]
- Rimoldi O, Rosen SD, Camici PG. The blunting of coronary flow reserve in hypertension with left ventricular hypertrophy is transmural and correlates with systolic blood pressure. J Hypertens. 2014;32:2465–71. 10.1097/HJH.0000000000000338. [Abstract] [CrossRef] [Google Scholar]
- Hoffman JI. Maximal coronary flow and the concept of coronary vascular reserve. Circulation. 1984;70:153–9. 10.1161/01.CIR.70.2.153. [Abstract] [CrossRef] [Google Scholar]
- De Bruyne B, Bartunek J, Sys SU, Pijls NH, Heyndrickx GR, Wijns W. Simultaneous coronary pressure and flow velocity measurements in humans. Feasibility, reproducibility, and hemodynamic dependence of coronary flow velocity reserve, hyperemic flow versus pressure slope index, and fractional flow reserve. Circulation. 1996;94:1842–9. 10.1161/01.CIR.94.8.1842. [Abstract] [CrossRef] [Google Scholar]
- Parker JD, Parker JO. Nitrate therapy for stable angina pectoris. N Engl J Med. 1998;338:520–31. 10.1056/NEJM199802193380807. [Abstract] [CrossRef] [Google Scholar]
- Akasaka T, Yoshida K, Hozumi T, Takagi T, Kaji S, Kawamoto T, Morioka S, Yoshikawa J. Retinopathy identifies marked restriction of coronary flow reserve in patients with diabetes mellitus. J Am Coll Cardiol. 1997;30:935–41. 10.1016/S0735-1097(97)00242-8. [Abstract] [CrossRef] [Google Scholar]
- Nitenberg A, Ledoux S, Valensi P, Sachs R, Attali JR, Antony I. Impairment of coronary microvascular dilation in response to cold pressor--induced sympathetic stimulation in type 2 diabetic patients with abnormal stress thallium imaging. Diabetes. 2001;50:1180–5. 10.2337/diabetes.50.5.1180. [Abstract] [CrossRef] [Google Scholar]
- Papaioannou GI, Kasapis C, Seip RL, Grey NJ, Katten D, Wackers FJ, Inzucchi SE, Engel S, Taylor A, Young LH, Chyun DA, Davey JA, Iskandrian AE, Ratner RE, Robinson EC, Carolan S, Heller GV. Value of peripheral vascular endothelial function in the detection of relative myocardial ischemia in asymptomatic type 2 diabetic patients who underwent myocardial perfusion imaging. J Nucl Cardiol. 2006;13:362–8. 10.1016/j.nuclcard.2006.01.022. [Abstract] [CrossRef] [Google Scholar]
- van de Hoef TP, Bax M, Meuwissen M, Damman P, Delewi R, de Winter RJ, Koch KT, Schotborgh C, Henriques JP, Tijssen JG, Piek JJ. Impact of coronary microvascular function on long-term cardiac mortality in patients with acute ST-segment-elevation myocardial infarction. Circ Cardiovasc Interv. 2013;6:207–15. 10.1161/CIRCINTERVENTIONS.112.000168. [Abstract] [CrossRef] [Google Scholar]
- Britten MB, Zeiher AM, Schachinger V. Microvascular dysfunction in angiographically normal or mildly diseased coronary arteries predicts adverse cardiovascular long-term outcome. Coron Artery Dis. 2004;15:259–64. 10.1097/01.mca.0000134590.99841.81. [Abstract] [CrossRef] [Google Scholar]
- van de Hoef TP, Siebes M, Spaan JA, Piek JJ. Fundamentals in clinical coronary physiology: why coronary flow is more important than coronary pressure. Eur Heart J. 2015;36:3312–9a. 10.1093/eurheartj/ehv235. [Abstract] [CrossRef] [Google Scholar]
- Xaplanteris P, Fournier S, Pijls NHJ, Fearon WF, Barbato E, Tonino PAL, Engstrøm T, Kääb S, Dambrink JH, Rioufol G, Toth GG, Piroth Z, Witt N, Fröbert O, Kala P, Linke A, Jagic N, Mates M, Mavromatis K, Samady H, Irimpen A, Oldroyd K, Campo G, Rothenbuhler M, Jüni P, De Bruyne B FAME 2 Investigators. Five-Year Outcomes with PCI Guided by Fractional Flow Reserve. N Engl J Med. 2018;379:250–9. [Abstract] [Google Scholar]
- Smalling RW, Kelley K, Kirkeeide RL, Fisher DJ. Regional myocardial function is not affected by severe coronary depressurization provided coronary blood flow is maintained. J Am Coll Cardiol. 1985;5:948–55. 10.1016/S0735-1097(85)80438-1. [Abstract] [CrossRef] [Google Scholar]
- Taqueti VR, Hachamovitch R, Murthy VL, Naya M, Foster CR, Hainer J, Dorbala S, Blankstein R, Di Carli MF. Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation. 2015;131:19–27. 10.1161/CIRCULATIONAHA.114.011939. [Europe PMC free article] [Abstract] [CrossRef] [Google Scholar]
- De Luca G, Venegoni L, Iorio S, Giuliani L, Marino P. Effects of increasing doses of intracoronary adenosine on the assessment of fractional flow reserve. JACC Cardiovasc Interv. 2011;4:1079–84. 10.1016/j.jcin.2011.08.004. [Abstract] [CrossRef] [Google Scholar]
- Gould KL, Kirkeeide RL, Buchi M. Coronary flow reserve as a physiologic measure of stenosis severity. J Am Coll Cardiol. 1990;15:459–74. 10.1016/S0735-1097(10)80078-6. [Abstract] [CrossRef] [Google Scholar]
- Gould KL, Lipscomb K, Hamilton GW. Physiologic basis for assessing critical coronary stenosis. Instantaneous flow response and regional distribution during coronary hyperemia as measures of coronary flow reserve. Am J Cardiol. 1974;33:87–94. 10.1016/0002-9149(74)90743-7. [Abstract] [CrossRef] [Google Scholar]
Articles from EuroIntervention are provided here courtesy of Europa Group
Full text links
Read article at publisher's site: https://doi.org/10.4244/eij-d-19-00774
Read article for free, from open access legal sources, via Unpaywall:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9724860
Citations & impact
Impact metrics
Article citations
The role of coronary microcirculation in heart failure with preserved ejection fraction: An unceasing odyssey.
Heart Fail Rev, 03 Oct 2024
Cited by: 0 articles | PMID: 39358622
Review
Going beyond summed stress scores: Correlating global and territorial coronary flow reserve by single photon emission tomography with routine myocardial perfusion imaging.
Heliyon, 10(8):e29629, 14 Apr 2024
Cited by: 0 articles | PMID: 38660292 | PMCID: PMC11040110
Rate pressure product as a novel predictor of long-term adverse outcomes in patients after percutaneous coronary intervention: a retrospective cohort study.
BMJ Open, 13(4):e067951, 04 Apr 2023
Cited by: 1 article | PMID: 37015792 | PMCID: PMC10083747
Factors Associated with Impaired Resistive Reserve Ratio and Microvascular Resistance Reserve.
Diagnostics (Basel), 13(5):950, 02 Mar 2023
Cited by: 3 articles | PMID: 36900097 | PMCID: PMC10000988
Coronary flow reserve and coronary flow capacity at a time of shifting paradigms of ischaemic heart disease.
EuroIntervention, 16(18):e1463-e1465, 02 Apr 2021
Cited by: 0 articles | PMID: 33792541 | PMCID: PMC9707477
Go to all (8) article citations
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Diagnostic and Prognostic Implications of Coronary Flow Capacity: A Comprehensive Cross-Modality Physiological Concept in Ischemic Heart Disease.
JACC Cardiovasc Interv, 8(13):1670-1680, 01 Nov 2015
Cited by: 55 articles | PMID: 26585617
Differential Impact of Coronary Revascularization on Long-Term Clinical Outcome According to Coronary Flow Characteristics: Analysis of the International ILIAS Registry.
Circ Cardiovasc Interv, 15(6):e011948, 23 May 2022
Cited by: 0 articles | PMID: 35603622
Clinical outcomes of Fractional Flow Reserve-Guided Percutaneous Coronary Intervention By Coronary Flow Capacity Status in Stable Lesions.
EuroIntervention, 17(4):e301-e308, 20 Jul 2021
Cited by: 2 articles | PMID: 32624458 | PMCID: PMC9724928
Coronary flow capacity: concept, promises, and challenges.
Int J Cardiovasc Imaging, 33(7):1033-1039, 28 Mar 2017
Cited by: 8 articles | PMID: 28353034 | PMCID: PMC5489577
Review Free full text in Europe PMC